We describe three patients who all underwent elective surgery and had acute haemorrhage after the operation. All three patients had hypotension but did not develop the typically associated sign of tachycardia. The assumption that occult bleeding is always associated with tachycardia is incorrect and may lead to a delay in diagnosis.
The accepted and traditional cardiovascular signs of acute blood loss are tachycardia, hypotension, and poor peripheral perfusion. In a healthy adult, tachycardia is a heart rate of more than 100 beats/min. The maximum heart rate a person can sustain is generally accepted to be 220 minus the patient's age. Tachycardia occurs in the initial stage of a biphasic cardiovascular response, which attempts to maintain cardiac output in the face of hypovolaemia and a decreased stroke volume. Neural and hormonal mechanisms mediate this tachycardia after arterial baroreceptors are stimulated. In some patients with acute haemorrhage, however, this initial tachycardic response is absent; this may lead to confusion or a delay in diagnosis. The phenomenon has been called relative bradycardia,1-4 absence of tachycardic response,1-5 or paradoxical bradycardia.6 We describe three patients for whom doctors did not see initial tachycardia during acute haemorrhage.
Case reports
Case 1
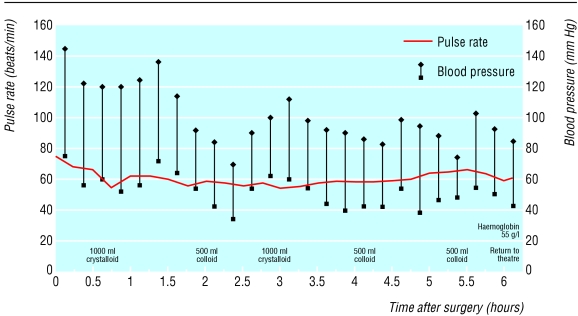
A 59 year old woman had an elective total abdominal hysterectomy and bilateral salpingo-oophorectomy. Apart from mild asthma, for which she took a ventolin inhaler, she was otherwise fit and well. She was taking no regular drugs. Her preoperative blood pressure was 145/75 mm Hg, pulse rate was 76 beats/min, and haemoglobin concentration was 147 g/l. Surgery was uneventful. In the recovery room, the woman's blood pressure fell to 70/34, 84/42, and 78/48 mm Hg at 2.5, 4, and 5.5 hours after the operation. At each occasion, doctors prescribed a fluid bolus, which increased systolic blood pressure to greater than 100 mm Hg. Her pulse rate never exceeded 70 beats/min (fig 1). Six hours after the operation, her haemoglobin concentration was 55 g/l. During laparotomy, doctors drained 1500 ml of blood from her peritoneal cavity, securing haemostasis. Subsequent recovery was uneventful.
Fig 1.
Case 1: pulse rate and blood pressure every 15 minutes after total abdominal hysterectomy and bilateral salpingo-oophorectomy
Case 2
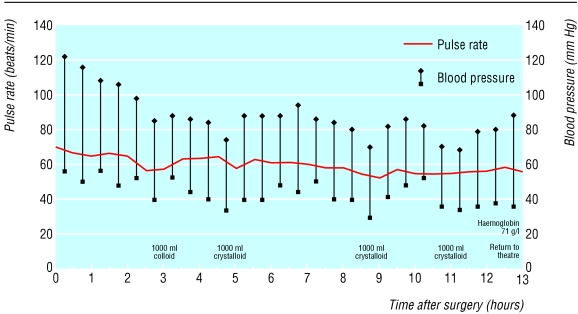
A 54 year old woman had an elective laparoscopic cholecystectomy. She was fit and well and taking no regular drugs. Before the operation, her blood pressure was 122/56 mm Hg, pulse rate was 72 beats/min, and haemoglobin concentration was 111 g/l. Surgery was uneventful. Three hours after the operation, she had a blood pressure of 85/40 mm Hg and a pulse rate of 70 beats/min. Despite having fluids replaced, her systolic blood pressure did not exceed 90 mm Hg and her pulse rate remained fewer than 70 beats/min over the next nine hours (fig 2).
Fig 2.
Case 2: pulse rate and blood pressure every 30 minutes after laparoscopic cholecystectomy
At 12 hours after the operation, the patient had increasing pain in her right shoulder and abdomen. Examination showed diffuse abdominal tenderness. Her haemoglobin was 71 g/l. At laparotomy, surgeons removed 600 ml of blood together with large clots. Her bleeding point was a tear at the insertion of the falciform ligament into the liver. Doctors secured haemostasis, and subsequent recovery was uneventful.
Case 3
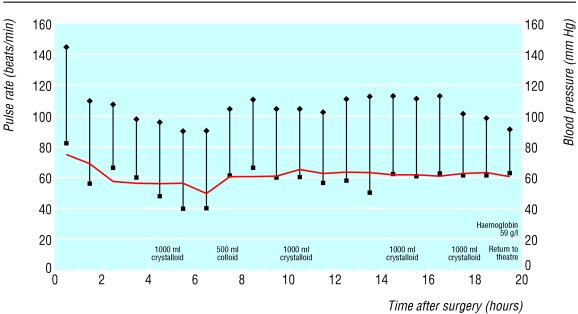
A 46 year old woman had an elective abdominal hysterectomy and bilateral salpingo-oophorectomy. She was fit and well and taking no regular drugs. Before surgery, her blood pressure was 145/82 mm Hg, pulse rate was 84 beats/min, and haemoglobin concentration was 139 g/l. After uneventful surgery, she was persistently oliguric with a systolic blood pressure of about 100 mm Hg. Doctors gave 4500 ml of crystalloid and colloid over 18 hours, during which the woman's pulse rate remained fewer than 80 beats/min (fig 3). Her haemoglobin concentration was 59 g/l. At laparotomy, surgeons removed 700 ml of blood and removed large clots. Surgeons identified the source of bleeding as venous ooze from the edge of her vagina and secured haemostasis. Transient renal failure and myocardial ischaemia complicated recovery.
Fig 3.
Case 3: pulse rate and blood pressure every hour after abdominal hysterectomy and bilateral salpingo-oophorectomy
Discussion
Patients with acute haemorrhage may not show the expected initial tachycardic response. Clinicians should consider a diagnosis of acute haemorrhage for patients with hypotension and a normal or low heart rate after surgery. The three patients presented to us in a single year; for patients with acute haemorrhage, lack of initial tachycardia may be more common than previously thought.
Experimental evidence and clinical observations show that, without resuscitation, the response of heart rate to a reduction in the volume of circulating blood is usually biphasic. In the first phase, baroreceptor mediated reflex vasoconstriction and cardio-acceleration maintain arterial pressure despite falling cardiac output. This phase is therefore characterised by tachycardia and normotension. The second phase occurs when about a third of the volume of circulating blood has been lost. Sympathetically mediated vasoconstriction and cardiac drive fall abruptly, and cardiac vagal drive increases. This simultaneously reduces mean arterial pressure and heart rate. Early recognition of this vasodepressor-cardioinhibitory reaction to a reduced circulating volume is vital; the associated bradycardia and hypotension precede circulatory collapse. These phases, seen with progressive central hypovolaemia, are reversed during resuscitation of circulatory volume. The distinction between a bradycardia seen in the second phase of a normal response to acute haemorrhage and a relative bradycardia is that patients with relative bradycardia do not exhibit the initial tachycardia in the first phase.
Bradycardic responses to acute haemorrhage need early recognition and prompt replacement of circulatory volume. About a third of patients with traumatic haemorrhage will present with a bradycardia; “normal heart rate or even bradycardia can be associated with an acute reduction in blood volume.”7 A retrospective study of patients with isolated extremity trauma or isolated penetrating abdominal trauma found that of the 71 patients presenting with systolic blood pressure of less than 100 mm Hg, 25 (35%) had a pulse rate of fewer than 100 beats/min.8 A retrospective study of patients at a trauma centre found that of 750 patients who presented with a systolic blood pressure of less than 90 mm Hg, 217 (28.9%) had a pulse rate of fewer than 90 beats/min.9 The authors of the study also suggested that bradycardia was associated with a better prognosis in certain subgroups of patients.
In the face of severe hypovolaemia, the bradycardia seen in the second phase of cardiovascular response to acute haemorrhage allows for a longer time for diastolic ventricular filling leading to an increased stroke volume.10 This bradycardia may result from the activation of a vagally mediated reflex arc originating from mechanoreceptors in the left ventricle.11 The bradycardic response may also be the result of a parasympathetic reflex mediated via the vagus nerve triggered by blood in the peritoneum.1,12 Vagus involvement is suggested by the fact that after cooling or cutting of the vagus nerves after rapid external haemorrhage in cats the fall in blood pressure was not affected, but the bradycardic response was absent.10 Why some patients do not show initial tachycardia is unknown.
Conclusion
Bradycardia in patients presenting with acute haemorrhage is common, either as part of a normal physiological response or as a relative bradycardia. The assumption that initial tachycardia is the only haemodynamic response to acute central hypovolaemia is incorrect, and a failure to recognise bradycardia as a sign of acute haemorrhage is potentially dangerous. Increasing circulatory volume in these critically ill patients should not be delayed.
Patients with acute haemorrhage may not exhibit the typically associated initial tachycardia
Contributors: IT and JD collected the data. IT wrote the paper. JD reviewed and redrafted the paper. JD is guarantor.
Funding: No additional funding.
Competing interests: None declared.
References
- 1.Jansen RPS. Relative bradycardia: a sign of acute intraperitoneal bleeding. Aust NZ Obstet Gynaecol 1978;18: 206-8. [DOI] [PubMed] [Google Scholar]
- 2.Secher NH, Sander Jensen K, Werner C, Warberg J, Bie P. Bradycardia during severe but reversible hypovolemic shock in man. Circ Shock 1984;14: 267-74. [PubMed] [Google Scholar]
- 3.Adams SL, Greene JS. Absence of a tachycardic response to intraperitoneal haemorrhage. J Emerg Med 1986;4: 383-9. [DOI] [PubMed] [Google Scholar]
- 4.Snyder HS, Dresnick SJ. Lack of tachycardic response to hypotension in penetrating abdominal injuries. J Emerg Med 1989;7: 335-9. [DOI] [PubMed] [Google Scholar]
- 5.Vayer JS, Henderson JV, Bellamy RF, Galper AR. Absence of a tachycardic response to shock in penetrating intraperitoneal injury. Ann Emerg Med 1988;17: 227-31. [DOI] [PubMed] [Google Scholar]
- 6.Barriot P, Riou B. Haemorrhagic shock with paradoxical bradycardia. Intens Care Med 1987;13: 203-7. [DOI] [PubMed] [Google Scholar]
- 7.American College of Surgeons. Advanced Trauma Life Support for Doctors. (ATLS) Instructor Course Manual. Chicago: ACoS, 1997.
- 8.Thompson D, Adams SL, Barrett J. Relative bradycardia in patients with isolated penetrating abdominal trauma and isolated extremity trauma. Ann Emerg Med 1990;19: 268-75. [DOI] [PubMed] [Google Scholar]
- 9.Demetriades D, Chan LS, Bhasin P, Berne TV, Ramicone E, Huicochea F, et al. Relative bradycardia in patients with traumatic hypotension. J Trauma 1998;45: 534-9. [DOI] [PubMed] [Google Scholar]
- 10.Oberg P, Thoren P. Increased activity in vagal cardiac afferents correlated to the appearance of reflex bradycardia during severe haemorrhage in cats. Acta Physiol Scand 1970;80(suppl): 22A-23A. [DOI] [PubMed] [Google Scholar]
- 11.Oberg B, Thoren P. Increased activity in left ventricular receptors during haemorrhage or occlusion of caval veins in the cat. Acta Physiol Scand 1972;85: 164-3. [DOI] [PubMed] [Google Scholar]
- 12.Snyder HS. Lack of a tachycardic response to hypotension with ruptured ectopic pregnancy. Am J Emerg Med 1990;8: 23-6. [DOI] [PubMed] [Google Scholar]