Given the remarkable pace at which technological change alters the economy and society, it was only a matter of time before it eventually made inroads in the cloistered world of medical education.
Change in the hallowed halls of dry medical pedagogy, though, may finally be in the offing as educators explore a new model of instruction — called the “flipped classroom” — that slashes student exposure to mind-numbing lectures and frees class time for discussions and interactive exercises in hopes of better preparing future physicians to be lifelong learners.
The traditional lecture may have been an efficient format for transferring information 100 years ago, but it’s no longer practical in an era of exploding medical knowledge, says Dr. David Snadden, executive associate dean of education for the faculty of medicine at the University of British Columbia in Vancouver. “We’ve actually reached a stage where we can’t fit [in] all the curriculum. It’s just not possible.”
“The thing that’s becoming really critical for us is helping our students understand how to manage information, access and sift information” as they’ll need to do as practising physicians, he adds.
Shifting course material onto the Internet offers a solution to both these challenges, Snadden says. In addition to freeing class time for more active learning, the model allows students to control the pace of their learning and “skip the things that don’t seem relevant or that they already know.”
It’s senseless to waste time verbally transmitting information that’s more effectively delivered online, says Dr. Charles Prober, senior associate dean for medical education at Stanford University in California. “If the information is a series of facts and concepts, it might as well be delivered in a more digestible way.”
It also allows for pedagogical innovation, Prober adds. An instructor, for example, might embed quizzes or links to ancillary materials within a video to engage students and provide context in ways that would not be possible in a traditional lecture.
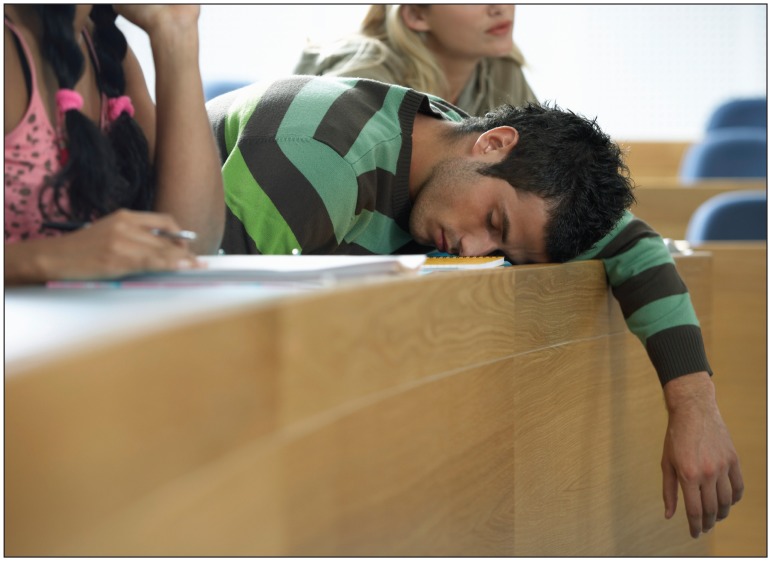
Is sitting through endless hours of lectures the most effective way for medical students to learn in an era of exploding medical knowledge?
Image courtesy of © 2012 Thinkstock
A professor can also better utilize class time to engage students in case-, problem- and team-based exercises to support knowledge retention, Prober adds. “So it’s the discussion and embedding of the course material in stories that ultimately makes the material relevant and therefore sustained by students.”
Stanford utilized the approach in a core biochemistry course this year, repackaging lectures into short, online presentations for students to view at their leisure and reserving class time for interactive discussions of clinical vignettes and frequent low-stakes quizzes. Prober says student reviews were positive and although attendance was optional, it jumped from 30% to 80%.
Medical educators at Queen’s University in Kingston, Ontario, have similarly noted improved student participation now that instructors spend less than 50% of class time on lectures, says Lewis Tomalty, vice dean of medical education at the school. “They’re much more engaged learners.”
The flipped classroom model builds on an already successful tradition of Canadian medical schools using video conferencing and other digital media to provide off-site instruction to students at satellite learning centres — a model pioneered by the University of British Columbia in 2004 — although such programs still primarily broadcast digital content in real-time during class hours, Snadden says.
The next step in that evolution will be “moving to what we would call synchronous learning, whereby all the students in a second-year lecture right across the province are listening to or looking at a video at the same time, to asynchronous learning,” whereby students are able to access digital content whenever and wherever they like.
Thus far, however, Tomalty notes that students have embraced the transition to such a model more readily than their instructors. “Students are comfortable with it. They’ll engage and they’re getting very comfortable working together, speaking out and problem solving in these large venues. But one of the big issues is telling the teacher who may have been teaching a session for the past 20 years that they can’t do it in a standard lecture format anymore.”
“We’ve known for decades that active learning enhances retention and understanding, but it’s hard to do and the model we were brought up with was that professors stood at the front of the class and taught at you,” he adds.
According to Snadden, the time and “intensity of effort” required to develop interactive materials pose further obstacles for even the most tech-savvy faculty. “The real challenge is the instructional design of what that material will look like and how it’s put together. I don’t think you could just take a video camera into a class and say to the lecturer: ‘Do the lecture and we’ll put it on the web-site.’ I personally don’t think that works.”
To that end, Queen’s University is developing a cadre of support staff for faculty including “educational developers who will go into the classroom with you, will help you plan your sessions and help you learn how to use different kinds of teaching methods,” as well as a technology team to assist instructors in developing electronic ancillary materials, Tomalty says. “There’s not a formula here. The idea is you really have to sit down and plan the whole teaching arena. And that’s where it becomes difficult because physicians are very busy people and proper teaching takes a lot of time.”