Abstract
BACKGROUND
Kidney transplantation (KT) is a life-prolonging therapy in certain older end-stage renal disease (ESRD) patients, but concerns regarding peri-transplant morbidity remain. We estimate the relative increase in time spent hospitalized in the year post-KT for older versus younger ESRD patients.
METHODS
This was a retrospective analysis of 27,247 Medicare-primary KT recipients from 2000–2005 using United States Renal Data System and Organ Procurement and Transplantation Network data. Time spent hospitalized was enumerated in the year pre- and post-KT from Medicare Part A claims. Excess inpatient days were the difference in an individual’s post-KT and pre-KT hospital and skilled nursing facility days, standardized by time spent alive in the year post-KT.
RESULTS
Median excess inpatient days were similar by age group (9 in recipients ≥65 years vs. 7 in recipients < 65 years); however, the distribution was skewed, such that many more older adults had large increases in inpatient time (8.6% totaled > 120 excess inpatient days vs. 4.2% in younger recipients). Among older recipients, risk factors for poor outcomes included recipient age, donor age, longer dialysis vintage, diabetic nephropathy, and congestive heart failure. Reasons for post-transplant hospitalization were similar by age with the exception of rehabilitation, which was common only in the 65+ age group. Mean inpatient costs were equivalent pre-transplant by age but significantly higher post-transplant among older KT recipients.
CONCLUSIONS
Post-transplant morbidity may not be so different in the majority of older individuals selected for KT; however, a minority fares much worse.
Keywords: kidney transplantation, costs, older adults
INTRODUCTION
Older adults are increasingly referred for kidney transplantation.1, 2 In 2008, adults ages 65 and older comprised 17% of the kidney transplant waiting list, up from 8% a decade earlier.1 However, older adults make up nearly half of incident ESRD patients,1 and access to transplantation remains exceedingly low.3 Although there is a clear survival advantage associated with kidney transplantation for the appropriately selected older transplant candidate compared with remaining on dialysis,4 less is known about the tolerance of kidney transplantation in an older population, or whether the impact of transplant-related morbidity differs by recipient age.
Older ESRD patients may have distinct risk-benefit considerations for kidney transplantation. Older adults have smaller gains in expected life-years associated with transplantation compared with younger kidney transplant recipients,5 and their peri-operative morbidity may be higher. For example, older adults may experience higher infection rates after standard immunosuppression protocols given age-related changes in immune response.6 Steroid therapy may predispose already frail older transplant candidates to increased rates of fracture.7 Finally, older adults generally shoulder a higher burden of comorbid conditions, and they may face longer post-transplant recovery times and higher surgical complication rates.8 These hypothetical increases in transplant-related morbidity among older transplant recipients may result in decreased quality of life – an important consideration in patients with relatively short expected survival. 9
Hospitalizations are an important and underutilized proxy for comparing post-transplant morbidity across age groups. Careful interpretation is required: greater time spent hospitalized post-transplant may be attributable to poorer tolerance of the transplant itself, but it may also be attributable to pre-existing medical conditions. In other words, older patients might be expected to spend more time in the hospital than a younger patient regardless of whether they received a transplant. Using a novel method to adjust for this baseline non-transplant morbidity, the aim of this study was to compare post-transplant hospitalization patterns between older and younger recipients, benchmarking to an individual’s pre-transplant hospitalization pattern.
RESULTS
Baseline and transplant characteristics
From 2000 to 2005, there were 4,807 Medicare-primary transplant recipients ages 65 and over, and 22,440 between the ages of 18 and 64 (Table 1). There were smaller proportions of female and black recipients among older age groups. Except for drug abuse and current smoking, older recipients had a greater burden of comorbid conditions than their younger counterparts (mean number of comorbidities, 2.1 vs. 1.7, p<0.001). Older adults had slightly shorter pre-transplant time on dialysis (3.3 years vs. 3.9 years, p<0.001) and they more often received expanded criteria donor organs (27.1% vs. 15.8%, p<0.001). The rate of live donor transplantation was lower for older recipients vs. younger recipients overall (18.3% vs. 20.6%, p<0.001), although this was driven mostly by the high live donor rates in 18–39 year-olds.
Table 1.
Study population characteristics, by recipient age
| Ages 18–39 (N=6,233) | Ages 40–49 (N=5,771) | Ages 50–64 (N=10,436) | Ages 65+ (N=4,807) | |
|---|---|---|---|---|
| Recipient characteristics | ||||
| Female (%) | 41.2 | 39.6 | 39.2 | 37.3 |
| Age (years, mean) | 32.2 | 45.3 | 57.2 | 69.8 |
| Race (%): | ||||
| White | 50.9 | 53.8 | 57.7 | 72.7 |
| Black | 40.4 | 38.5 | 34.3 | 21.2 |
| Other | 8.7 | 7.8 | 8.0 | 6.1 |
| BMI (mean) | 26.2 | 27.6 | 27.9 | 27.0 |
| Total comorbidities (mean) | 1.2 | 1.6 | 2.0 | 2.1 |
| History of cancer | 0.3 | 0.9 | 1.8 | 4.3 |
| Congestive heart failure | 6.9 | 9.6 | 15.9 | 18.1 |
| Cerebrovascular accident | 1.2 | 2.5 | 4.0 | 4.9 |
| Diabetic nephropathy | 14.2 | 28.1 | 45.0 | 42.7 |
| Drug abuse | 1.0 | 1.8 | 0.6 | 0.0 |
| History of arrhythmia | 0.6 | 0.9 | 1.6 | 3.6 |
| Hypertension | 76.0 | 81.9 | 83.2 | 83.9 |
| Ischemic heart disease | 1.0 | 4.2 | 11.4 | 18.2 |
| Myocardial infarction | 0.4 | 1.5 | 3.7 | 5.0 |
| Chronic pulmonary disease | 0.4 | 1.2 | 2.1 | 3.0 |
| Peripheral vascular disease | 1.3 | 3.1 | 5.9 | 6.9 |
| Current smoker | 5.4 | 6.6 | 5.2 | 2.2 |
| Years on dialysis pre-transplant | 3.7 | 4.0 | 4.0 | 3.3 |
| Transplant characteristics | ||||
| Transplant year (%): | ||||
| 2000 | 14.6 | 12.7 | 11.0 | 11.6 |
| 2001 | 15.7 | 15.6 | 14.1 | 12.8 |
| 2002 | 16.4 | 15.9 | 16.8 | 15.8 |
| 2003 | 17.1 | 17.4 | 17.7 | 17.3 |
| 2004 | 18.6 | 19.1 | 19.9 | 19.5 |
| 2005 | 17.6 | 19.2 | 20.4 | 23.0 |
| Live donor (%) | 27.9 | 18.7 | 17.2 | 18.3 |
| Extended criteria donor (%) | 5.3 | 9.4 | 16.9 | 27.1 |
| Cold ischemia time (hours, mean) | 15.4 | 16.6 | 16.8 | 16.6 |
Peri-transplant hospitalization
In the year pre-transplant, older recipients spent – on average – slightly less time hospitalized than younger recipients (mean, 5.4 days vs. 5.8 days, p=0.03) but slightly more time in skilled nursing facilities (mean, 0.5 days versus 0.3 days, p=0.004). There was no difference in the median pre-transplant days spent hospitalized or in skilled nursing facilities by age group (2 days and 0 days, respectively), reflecting a skew in the distribution (Table 2). On average, older recipients spent significantly more days in the hospital for the transplant itself (mean, 7.9 days vs. 6.9 days, p<0.001) and more time in skilled nursing facilities in the year post-transplant (mean, 3.7 days vs. 1.2 days, p<0.001); again, medians were similar by age category, with the exception of days spent hospitalized for reasons other than the transplant (Table 2).
Table 2.
Pre- and post- transplant hospitalization and skilled nursing facility time, by age at transplantation
| Ages 18–39 (N=6,233) | Ages 40–49 (N=5,771) | Ages 50–64 (N=10,436) | Ages 65+ (N=4,807) | |
|---|---|---|---|---|
| Measured over the year pre-transplant (median, IQR) | ||||
| Days in skilled nursing facility | 0 (0-0) | 0 (0-0) | 0 (0-0) | 0 (0-0) |
| Days in hospital | 2 (1–6) | 2 (1–6) | 2 (1–6) | 2 (1–6) |
| Measured over the year post-transplant (median, IQR) | ||||
| Days in skilled nursing facility | 0 (0-0) | 0 (0-0) | 0 (0-0) | 0 (0-0) |
| Days in hospital for transplant | 5 (3–7) | 5 (4–8) | 5 (4–8) | 6 (4–9) |
| Days in hospital other than transplant | 3 (0–10) | 3 (0–12) | 4 (0–15) | 5 (0–18) |
| Comparison of post- to pre-transplant (median, IQR) | ||||
| Excess inpatient days* | 5 (2–12) | 6 (2–16) | 7 (2–19) | 9 (3–24) |
| Excess inpatient days, no transplant** | −1 (−2–5) | 0 (−2–8) | 1 (−2–11) | 1 (−2–15) |
| Standardized excess inpatient days*** | 5 (2–13) | 6 (2–16) | 8 (2–22) | 9 (3–29) |
| Post-transplant mortality (%) | ||||
| One year mortality | 2.2 | 3.8 | 7.3 | 11.1 |
| Three year mortality | 5.5 | 8.6 | 15.6 | 23.1 |
Excess inpatient days: days hospitalized or in skilled nursing facility in the year post-transplant - days hospitalized or in skilled nursing facility in the year pre-transplant
Excess inpatients days, no transplant: excess inpatient days – days hospitalized for transplant
Standardized excess inpatient days: inpatient days in the year post-transplant (standardized to one year survival) - inpatient days in the year pre-transplant
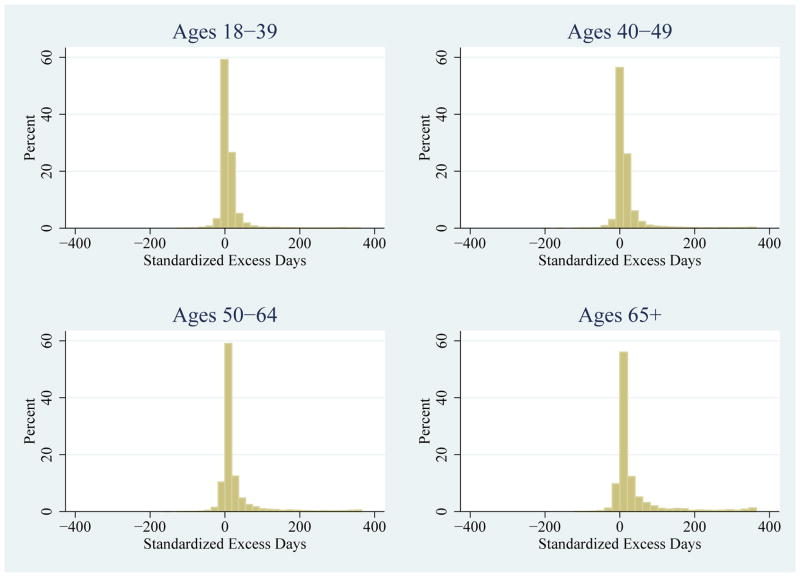
When benchmarked to an individual recipient’s hospitalization pattern in the year pre-transplant, differences in inpatient time (“excess inpatient days”) between the older and younger age groups were more pronounced (Table 2). While median excess inpatient days remained similar (5, 6, 7, and 9 days in the 18–39, 40–49, 50–64, and 65+ age groups, respectively), the interquartile range of excess inpatient days increased with age (2–12, 2–16, 2–19, and 3–24, respectively); this increase in interquartile range was greater still when excess inpatient days were standardized to the time spent alive in the year post-transplant (Table 2). Similarly, the distribution of standardized excess inpatient days was markedly different by age group (Figure 1A). Older adults were more likely to spend more than 120 standardized excess inpatient days post-transplant than any other age group (1.4%, 2.7%, 5.4%, and 8.6% of the 18–39, 40–49, 50–64, and 65+ age groups, respectively).
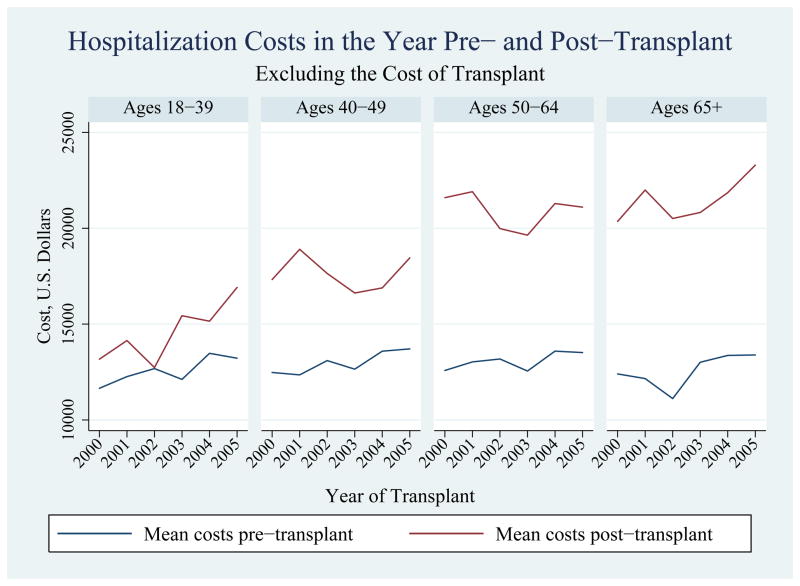
Figure 1.
By age group: (A) distribution of standardized excess inpatient days*, (B) mean costs
* Standardized excess inpatient days: inpatient days in the year post-transplant (standardized to one year survival) - inpatient days in the year pre-transplant
Stratification by donor type
Among live donor recipients, the disparities in outcomes by age group were attenuated. The proportion of recipients with more than 120 standardized excess inpatient days was 1.1%, 1.7%, 3.5%, and 5.1% in the 18–39, 40–49, 50–64, and 65+ age groups, respectively. The one-year mortality rates were also lower among live donor recipients, at 1.8 %, 3.0 %, 5.1 %, and 6.6 % by increasing age group. The median standardized excess inpatient days were similar (4, 4, 4, and 5 days among recipients ages 18–39, 40–49, 50–64, and 65+, respectively), as were the corresponding distributions (interquartile range of standardized excess inpatient days, 1–10, 0–12, 1–13, and 1–16 by increasing age group). Compared with deceased donor recipients, live donor recipients spent more time hospitalized in the year pre-transplant (mean, 6.8 days among live donors vs. 5.4 days among deceased donors, p<0.001; median, 2 days for both groups); this was true within each age group. Conversely, live donor recipients spent less time hospitalized in the year post-transplant than their deceased donor counterparts (inpatient days among all ages: mean, 15.0, median, 8, interquartile range 4–17 among live donor recipients; mean, 19.6, median, 11, interquartile range 6–23 among deceased donor recipients).
Poor outcome among older adults
Recipient characteristics significantly associated with poor outcome (>120 excess inpatient days or death in the year post-transplant) among recipients ages 65 years and older included age (adjusted odds ratio (aOR) 1.42 per decade, 95% CI: 1.11–1.81, p=0.005), time on dialysis pre-transplant (aOR 1.11 per year, 95% CI: 1.05–1.17, p<0.001), time spent hospitalized in the year pre-transplant (aOR 1.08 per week, 95% CI: 1.02–1.16, p=0.01), diabetes (aOR 1.49, 95% CI: 1.11–2.01, p=0.008) or hypertension (aOR 1.46, 95% CI: 1.07–1.99, p=0.02) as the primary cause of renal disease, and the presence of congestive heart failure (aOR 1.27, 95% CI: 1.02–1.58, p=0.03) (Table 3). Transplant characteristics associated with poor outcome were donor age (aOR 1.11 per decade, 95% CI: 1.03–1.19, p=0.005); live donor (aOR 0.59, 0.44–0.79, p<0.001) and later transplant year (aOR 0.93 per year, 95% CI: 0.88–0.98, p=0.007) were protective. Expanded criteria donor organs had no independent association with outcome (aOR 1.11, 95% CI: 0.85–1.45, p=0.4), likely because of the collinearity between donor age and expanded criteria donor status. When the entire transplant recipient population was included, there was a statistically significant interaction between age category and diabetes as a cause of renal failure, with diabetes conferring higher odds of poor outcomes among younger age groups (ages 18–39, aOR 2.55, 95% CI: 1.75–3.79, p<0.001; ages 40–49, aOR 2.01, 95% CI: 1.50–2.70, p<0.001; ages 50–64, aOR 1.83, 95% CI: 1.50–2.22, p<0.001; ages 65+, aOR 1.39, 95% CI: 1.12–1.72, p=0.003).
Table 3.
Factors associated with poor outcomes (≥33% of the year post-KT spent hospitalized or death) among older transplant recipients, multivariable model
| Characteristic | Adjusted odds ratio (95% confidence interval) | P-value |
|---|---|---|
| Age (per 10 years) | 1.42 (1.11–1.81) | 0.005 |
| Race: | ||
| White | Reference | |
| Black | 0.88 (0.70–1.11) | 0.3 |
| Other | 0.91 (0.63–1.32) | 0.6 |
| Female sex | 0.89 (0.74–1.07) | 0.2 |
| BMI: | ||
| >30 | Reference | |
| <20 | 0.86 (0.55–1.36) | 0.5 |
| 20≤BMI <25 | 0.86 (0.68–1.10) | 0.2 |
| 25≤BMI <30 | 0.88 (0.70–1.09) | 0.2 |
| Years on dialysis pre-transplant | 1.11 (1.05–1.17) | <0.001 |
| Live donor | 0.59 (0.44–0.79) | <0.001 |
| ECD donor | 1.11 (0.85–1.45) | 0.4 |
| Donor age (per 10 years) | 1.11 (1.03–1.19) | 0.005 |
| Year pre-KT hospitalization (per week) | 1.08 (1.02–1.16) | 0.01 |
| Etiology of renal disease | ||
| Glomerulonephritis | Reference | |
| Diabetes | 1.49 (1.11–2.01) | 0.008 |
| Hypertension | 1.46 (1.07–1.99) | 0.02 |
| Polycystic kidney disease | 0.71 (0.43–1.16) | 0.2 |
| All others | 1.32 (0.93–1.89) | 0.1 |
| History of cancer | 0.73 (0.45–1.18) | 0.2 |
| Congestive heart failure | 1.27 (1.02–1.58) | 0.03 |
| Cerebrovascular accident | 1.26 (0.87–1.83) | 0.2 |
| Insulin-dependent diabetes | 1.09 (0.85–1.40) | 0.5 |
| History of arrhythmia | 1.39 (0.92–2.10) | 0.1 |
| Hypertension | 0.98 (0.76–1.26) | 0.9 |
| Ischemic heart disease | 1.20 (0.95–1.51) | 0.1 |
| Myocardial infarction | 0.92 (0.62–1.38) | 0.7 |
| Chronic pulmonary disease | 1.18 (0.74–1.89) | 0.5 |
| Peripheral vascular disease | 1.24 (0.90–1.70) | 0.2 |
| Current smoker | 1.57 (0.93–2.64) | 0.09 |
| Transplant Year | 0.93 (0.88–0.98) | 0.007 |
Causes of hospitalization post-transplant
The top five reasons for hospitalization in the year post-transplant (excluding the hospitalization for the transplant itself) were fairly similar across age groups (Table 4). The two most common causes of hospitalization were genitourinary system symptoms/procedures (including kidney, ureter, bladder procedures, prostatectomy, kidney stones, and other kidney and urinary tract signs and symptoms) and infection (most commonly infectious disease, septicemia, urinary tract infection, and pneumonia). Circulatory disorders were the third most common reason for hospitalization in recipients ages 40 and older. Despite the higher prevalence of diabetes in older adults, endocrine hospitalizations were not among the top 5 reasons for hospitalizations in older adults, although they were in the younger transplant recipient population. Rehabilitation was among the top 5 reasons for hospitalization only in older recipients.
Table 4.
Top five reasons for hospitalization post-transplant, by age
| Percent of time hospitalized in the year post-transplant | |
|---|---|
| Ages 18–39 | |
| Kidney/ureter/pelvis/bladder procedures | 19.5 |
| Infection | 9.1 |
| Miscellaneous | 2.8 |
| Endocrine | 2.7 |
| Gastrointestinal disorder | 2.6 |
| Ages 40–49 | |
| Kidney/ureter/pelvis/bladder procedures | 17.2 |
| Infection | 9.9 |
| Circulatory disorders | 3.1 |
| Endocrine | 2.8 |
| Gastrointestinal disorder | 2.4 |
| Ages 50–64 | |
| Kidney/ureter/pelvis/bladder procedures | 15.5 |
| Infection | 10.7 |
| Circulatory disorders | 3.0 |
| Endocrine | 2.9 |
| Respiratory | 2.4 |
| Ages 65+ | |
| Kidney/ureter/pelvis/bladder procedures | 15.3 |
| Infection | 10.9 |
| Circulatory disorders | 3.3 |
| Rehabilitation | 3.3 |
| Miscellaneous | 2.7 |
Costs before and after transplantation
Overall, Medicare costs were similar in the year pre-transplant when stratified by age group, and these costs increased slightly over time (p<0.001, Figure 1B). There was no difference in costs in the year post-transplant between recipients 50–64 and 65+ (p=0.3); however, they were both significantly larger than post-transplant costs in the 18–39 and 40–49 age groups. Post-transplant costs increased significantly over time in both the 18–39 and 65+ age groups (p<0.001).
DISCUSSION
This national study of hospitalization patterns before and after kidney transplantation further supports the growing body of evidence that appropriately selected older adults can and do thrive after kidney transplantation.10, 11 Compared with younger transplant recipients, older transplant recipients had similar median – yet higher mean – inpatient days in the year following transplantation, both before and after adjustment for baseline hospitalization patterns and mortality. Post-transplant hospitalization burden for the majority of older adults was relatively comparable to their younger counterparts; a minority of older recipients, however, fared much worse. Better tools to risk-stratify older kidney transplant candidates are needed.
Renal replacement therapy – even dialysis initiation – among older adults remains somewhat controversial. Therapeutic nihilism is common and not without evidence: studies from the United Kingdom indicate that older ESRD patients choosing conservative (non-dialysis) therapy may have equivalent survival to matched controls initiating dialysis.12, 13 Deceased donor kidney transplantation in older adults places a limited resource in a population with a reduced life expectancy.2, 14 While older kidney transplant recipients report higher quality of life than their counterparts on dialysis,15 the expected gains in quality of life after transplantation may be offset by a complicated post-transplant course.16 Factors associated with poor transplant outcomes, such as malnutrition, depression, and poor functional status, are disproportionately prevalent in the older ESRD population.17–19 Our study suggests that most older adults’ pre- and post- transplant hospitalizations – both important predictors of quality of life among older adults16 – are similar to those experienced in younger transplant recipients. However, poor outcomes after transplantation may be magnified in the older population: the upper range of post-transplant inpatient days and short-term mortality was much higher.
A notable finding of our study was the relative success of living donor transplantation among older persons. One-year survival among older living donor transplant recipients was high at 93.3%, and the post-transplant hospitalization experience was minimally different from younger living donor transplant recipients. A priori, we thought providers might be uneasy listing an older adult “to the detriment” of a potential younger candidate, given the length of the deceased donor waiting list. If this were true, providers might be more willing to refer marginal candidates with a potential live donor. We did observe that live donor recipients spent more time hospitalized in the year pre-transplant than deceased donor recipients, suggesting that this differential consideration may play a role in transplant candidate selection. However, even if older living donor recipients were in poorer health at the time of transplant than their age-matched deceased donor counterparts, they appeared to tolerate live donor transplantation similar to younger age groups.
Existing literature on transplant-associated morbidity among older adults is limited. In a single-center study of 271 patents, adults over the age of 60 had post-transplant experiences similar to younger transplant recipients in terms of perioperative morbidity, length of stay, and hospital readmissions.20 In another single-center study of 527 living donor transplant recipients, older adults had significantly higher rates of readmission but not length of stay.21 However, these studies are small, lack the power to detect some clinically meaningful differences, and potentially lack generalizability. The observation in our large, national study that kidney transplant lengths of stay are slightly higher for older adults is consistent with trends seen in the general U.S. population, where all-cause hospital rates and lengths of stay are increased among adults over the age of 65.22
The strengths of this study include the large sample size, the novel method for determining (and standardizing) post-transplant hospitalizations, and the likely generalizability to the overall kidney transplant candidate population. Our study population captures much of the US kidney transplant recipient pool and is over 50 times larger than previous studies. We use excess hospital days as a novel measure of hospitalizations post-transplant with an “internal control” for expected (i.e., pre-transplant) hospitalizations. Hospitalization records were extracted from administrative data, likely yielding a more accurate quantification of hospital days than that possible from a single transplant center source, where outside hospitalizations may be missed.
However, several important limitations merit consideration. Claims data may have low sensitivity in identifying hospitalization complications.23, 24 We limited our population to Medicare-primary patients, a criterion which could differentially affect older and younger patients. Given that all ESRD patients requiring dialysis therapy are eligible for Medicare, this is a common inclusion criterion in studies of ESRD patients,17, 25, 26 and one in which we believe should only minimally bias the results. Also, there may be a differential threshold for hospitalization admissions among younger and older transplant recipients. If so, however, we would expect older adults to be more readily hospitalized, and inferences from the existing study would be conservative.
In conclusion, this study provides national data regarding the hospitalization experience in the year before and after kidney transplantation in younger and older recipients. Time spent hospitalized in the year post-transplant and excess inpatient days are novel measures which may serve as important proxies for inferior quality of life and severe post-transplant morbidity. We demonstrate that, despite a substantially increased burden of comorbid conditions and inferior graft characteristics, the majority of older transplant recipients have similar post-transplant hospitalization patterns to their younger counterparts, although a minority of older transplant recipients fared very poorly. Based on these findings, we support continued efforts to improve access to transplantation for older end stage renal disease patients. However, older candidates should be counseled about their higher risk of severe morbidity and death in the year following kidney transplantation, and efforts should be intensified to improve the prediction of poor transplant outcomes within the older transplant candidate population. Better identification of transplant recipients at risk for prolonged hospital stays could spur development of surveillance protocols to improve post-transplant outcomes and reduce rehospitalization rates.
MATERIALS AND METHODS
The study population was composed of 27,247 adult first-time kidney-only transplant recipients between January 1, 2000 and December 31, 2005, as reported to the Organ Procurement and Transplantation Network (OPTN). The population was limited to those recipients with Medicare as their primary insurer continuously over the two-year peri-transplant period (encompassing 365 days pre- and post-kidney transplant). Donor, recipient, and transplant characteristics were gleaned from United States Renal Data System (USRDS), OPTN transplant candidate and recipient registration forms (TCR and TRR), and the Centers for Medicare & Medicaid Services (CMS) claims. Mortality information was augmented with the Social Security Death Master File (SSDMF).
The outcome of interest was number of days spent hospitalized in the year following transplant (including the hospitalization for the transplant itself), estimated from Medicare Part A claims. Excess inpatient days were calculated as the number of inpatient days (either in a skilled nursing facility or in a hospital) over the year post-transplant minus the number of inpatient days over the year pre-transplant. In order to account for the higher rates of death in the older age groups (and thus fewer days at risk for hospitalization), a standardized measure of excess inpatient days was constructed by scaling post-transplant inpatient days by the time spent alive in the year post-transplant. Hospitalizations were classified by International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes into 35 broad categories. Inpatient Medicare costs were also analyzed as a secondary outcome.
Comparisons of baseline variables between younger and older transplant recipients were performed using χ2 and t-tests as appropriate. Logistic regression was used to study factors associated with a “poor outcome”, namely ≥ 120 days excess inpatient days or death within a year post-transplant; factors evaluated included patient sex, ethnicity, years on dialysis pre-transplant, cause of ESRD, body mass index (BMI), Form 2728 comorbidities, donor age, donor type (living/deceased, expanded criteria donor) and hospital days in the year pre-transplant. To determine whether the effect of diabetic nephropathy on poor outcomes differed by age, an interaction term between the two variables was also tested. All statistical analyses were performed using Stata 11.0/MP (StataCorp, College Station, TX).
Acknowledgments
The authors thank the Organ Procurement and Transplantation Network (OPTN) and the United States Renal Disease System (USRDS) for provision of the data. The OPTN is supported by Health Resources and Services Administration contract 234-2005-370011C. The analyses described here are the responsibility of the authors alone and do not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Funding sources: Morgan Grams, National Kidney Foundation of Maryland; Dorry Segev, NIH grants K23AG032885 (co-funded by the American Federation of Aging Research) and R21DK085409.
ABBREVIATIONS
- CMS
Centers for Medicare & Medicaid Services
- ICD-9-CM
International Classification of Diseases, 9th Revision, Clinical Modification
- KT
kidney transplantation
- OPTN
Organ Procurement and Transplantation Network
- TCR
Transplant candidate registration form
- TRR
Transplant registration form
- SSDMF
Social Security Death Master File
- USRDS
United States Renal Data System
Footnotes
Author contributions:
MG: Research design, data analysis, first draft of the manuscript
MMD: Data analysis, manuscript revision and editing
LK: Data analysis, manuscript revision and editing
DS: Research design, data analysis, manuscript revision and editing
Related presentations: Presented in part at the American Transplant Congress, April 30, 2011; Philadelphia, PA.
References
- 1.US Renal Data System. USRDS 2010 annual data report: Atlas of chronic kidney disease and end-stage renal disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2010. [Google Scholar]
- 2.Huang E, Segev DL, Rabb H. Kidney transplantation in the elderly. Semin Nephrol. 2009;29:621–635. doi: 10.1016/j.semnephrol.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grams ME, Kucirka LM, Hanrahan CF, Montgomery RA, Massie AB, Segev DL. Candidacy for kidney transplantation of older adults. J Am Geriatr Soc. 2012;60:1–7. doi: 10.1111/j.1532-5415.2011.03652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, Held PJ, Port FK. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–1730. doi: 10.1056/NEJM199912023412303. [DOI] [PubMed] [Google Scholar]
- 5.Wolfe RA, McCullough KP, Leichtman AB. Predictability of survival models for waiting list and transplant patients: Calculating LYFT. Am J Transplant. 2009;9:1523–1527. doi: 10.1111/j.1600-6143.2009.02708.x. [DOI] [PubMed] [Google Scholar]
- 6.Meier-Kriesche HU, Ojo A, Hanson J, Cibrik D, Lake K, Agodoa LY, Leichtman A, Kaplan B. Increased immunosuppressive vulnerability in elderly renal transplant recipients. Transplantation. 2000;69:885–889. doi: 10.1097/00007890-200003150-00037. [DOI] [PubMed] [Google Scholar]
- 7.Pichette V, Bonnardeaux A, Prudhomme L, Gagne M, Cardinal J, Ouimet D. Long-term bone loss in kidney transplant recipients: A cross-sectional and longitudinal study. Am J Kidney Dis. 1996;28:105–114. doi: 10.1016/s0272-6386(96)90138-9. [DOI] [PubMed] [Google Scholar]
- 8.Kauffman HM, McBride MA, Cors CS, Roza AM, Wynn JJ. Early mortality rates in older kidney recipients with comorbid risk factors. Transplantation. 2007;83:404–410. doi: 10.1097/01.tp.0000251780.01031.81. [DOI] [PubMed] [Google Scholar]
- 9.Brown EA. Can quality of life be improved for the increasing numbers of older patients with end-stage kidney disease? Expert Rev Pharmacoecon Outcomes Res. 2010;10:661–666. doi: 10.1586/erp.10.78. [DOI] [PubMed] [Google Scholar]
- 10.Rao PS, Merion RM, Ashby VB, Port FK, Wolfe RA, Kayler LK. Renal transplantation in elderly patients older than 70 years of age: Results from the Scientific Registry of Transplant Recipients. Transplantation. 2007;83:1069–1074. doi: 10.1097/01.tp.0000259621.56861.31. [DOI] [PubMed] [Google Scholar]
- 11.Tullius SG, Tran H, Guleria I, Malek SK, Tilney NL, Milford E. The combination of donor and recipient age is critical in determining host immunoresponsiveness and renal transplant outcome. Ann Surg. 2010;252:662–674. doi: 10.1097/SLA.0b013e3181f65c7d. [DOI] [PubMed] [Google Scholar]
- 12.Murtagh FE, Marsh JE, Donohoe P, Ekbal NJ, Sheerin NS, Harris FE. Dialysis or not? A comparative survival study of patients over 75 years with chronic kidney disease stage 5. Nephrol Dial Transplant. 2007;22:1955–1962. doi: 10.1093/ndt/gfm153. [DOI] [PubMed] [Google Scholar]
- 13.Chandna SM, Da Silva-Gane M, Marshall C, Warwicker P, Greenwood RN, Farrington K. Survival of elderly patients with stage 5 CKD: Comparison of conservative management and renal replacement therapy. Nephrol Dial Transplant. 2011;26:1608–1614. doi: 10.1093/ndt/gfq630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fabrizii V, Winkelmayer WC, Klauser R, Kletzmayr J, Saemann MD, Steininger R, Kramar R, Horl WH, Kovarik J. Patient and graft survival in older kidney transplant recipients: Does age matter? J Am Soc Nephrol. 2004;15:1052–1060. doi: 10.1097/01.asn.0000120370.35927.40. [DOI] [PubMed] [Google Scholar]
- 15.Apostolou T, Hutchison AJ, Boulton AJ, Chak W, Vileikyte L, Uttley L, Gokal R. Quality of life in CAPD, transplant, and chronic renal failure patients with diabetes. Ren Fail. 2007;29:189–197. doi: 10.1080/08860220601098862. [DOI] [PubMed] [Google Scholar]
- 16.Rosenberger J, van Dijk JP, Nagyova I, Zezula I, Geckova AM, Roland R, van den Heuvel WJ, Groothoff JW. Predictors of perceived health status in patients after kidney transplantation. Transplantation. 2006;81:1306–1310. doi: 10.1097/01.tp.0000209596.01164.c9. [DOI] [PubMed] [Google Scholar]
- 17.Dobbels F, Skeans MA, Snyder JJ, Tuomari AV, Maclean JR, Kasiske BL. Depressive disorder in renal transplantation: An analysis of Medicare claims. Am J Kidney Dis. 2008;51:819–828. doi: 10.1053/j.ajkd.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 18.Guijarro C, Massy ZA, Wiederkehr MR, Ma JZ, Kasiske BL. Serum albumin and mortality after renal transplantation. Am J Kidney Dis. 1996;27:117–123. doi: 10.1016/s0272-6386(96)90038-4. [DOI] [PubMed] [Google Scholar]
- 19.Molnar MZ, Kovesdy CP, Bunnapradist S, Streja E, Mehrotra R, Krishnan M, Nissenson AR, Kalantar-Zadeh K. Associations of pretransplant serum albumin with post-transplant outcomes in kidney transplant recipients. Am J Transplant. 2011 doi: 10.1111/j.1600-6143.2011.03480.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saidi RF, Kennealey PT, Elias N, Kawai T, Hertl M, Farrell M, Goes N, Hartono C, Tolkoff-Rubin N, Cosimi AB, Ko DS. Deceased donor kidney transplantation in elderly patients: Is there a difference in outcomes? Transplant Proc. 2008;40:3413–3417. doi: 10.1016/j.transproceed.2008.08.127. [DOI] [PubMed] [Google Scholar]
- 21.Chuang FP, Novick AC, Sun GH, Kleeman M, Flechner S, Krishnamurthi V, Modlin C, Shoskes D, Goldfarb DA. Graft outcomes of living donor renal transplantations in elderly recipients. Transplant Proc. 2008;40:2299–2302. doi: 10.1016/j.transproceed.2008.06.017. [DOI] [PubMed] [Google Scholar]
- 22.U.S. Department of Health & Human Services. Agency for healthcare research and quality: Healthcare cost and utilization project. [Electronic version] 2011. [Google Scholar]
- 23.Grams ME, Plantinga LC, Hedgeman E, Saran R, Myers GL, Williams DE, Powe NR CDC CKD Surveillance Team. Validation of CKD and related conditions in existing data sets: A systematic review. Am J Kidney Dis. 2011;57:44–54. doi: 10.1053/j.ajkd.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leibson CL, Needleman J, Buerhaus P, Heit JA, Melton LJ, 3rd, Naessens JM, Bailey KR, Petterson TM, Ransom JE, Harris MR. Identifying in-hospital venous thromboembolism (VTE): A comparison of claims-based approaches with the Rochester Epidemiology Project VTE Cohort. Med Care. 2008;46:127–132. doi: 10.1097/MLR.0b013e3181589b92. [DOI] [PubMed] [Google Scholar]
- 25.Weinhandl ED, Snyder JJ, Israni AK, Kasiske BL. Effect of comorbidity adjustment on CMS criteria for kidney transplant center performance. Am J Transplant. 2009;9:506–516. doi: 10.1111/j.1600-6143.2008.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Snyder JJ, Israni AK, Peng Y, Zhang L, Simon TA, Kasiske BL. Rates of first infection following kidney transplant in the United States. Kidney Int. 2009;75:317–326. doi: 10.1038/ki.2008.580. [DOI] [PubMed] [Google Scholar]