Abstract
Purpose
Single port laparoscopic surgery is a rapidly evolving laparoscopic surgical approach. We report a comparison of transumbilical single port laparoscopic appendectomy (TUSPLA) and conventional laparoscopic appendectomy (CLA) in a Korean military hospital.
Methods
This single-center retrospective study of 63 patients who received laparoscopic appendectomy was conducted between May 2011 and October 2011. Nineteen patients received TUSPLA and 44 patients received CLA. Clinical outcomes such as operation time, hospital stay, postoperative pain, diet, and postoperative complication were reviewed.
Results
There were no statistically significant differences between TUSPLA and CLA patients, respectively, in operation time (58.9 minutes vs. 52.3 minutes, P = 0.262), duration of hospitalization (10.2 days vs. 10.6 days, P = 0.782), mean visual analogue scale score (2.6 vs. 2.5, P = 0.894), and return to diet (1.6 days vs. 1.7 days, P = 0.776). There were two cases (10.5%) of short-term complications in the TUSPLA group and four cases (9.1%) of short-term complications in the CLA group. All patients were fully recovered at discharge.
Conclusion
TUSPLA is a feasible alternative for CLA. When a glove port is used, no special instruments are needed. Thus, it can be performed in a hospital equipped with basic laparoscopic surgical instruments.
Keywords: Laparoscopy, Appendectomy, Single-port, Transumbilical, Scarless
INTRODUCTION
Since its first description in 1983 [1], laparoscopic appendectomy has gained acceptance as a treatment modality for acute appendicitis. Compared with open surgery, it has been proven to be less painful with better cosmesis [2,3]. When laparoscopic appendectomy is performed, the laparoscope is usually introduced into the abdominal cavity through a periumbilical incision and two additional laparoscopic instruments are inserted through 5-mm incisions and placed in a triangular fashion. This allows a completely intracorporeal appendectomy. With the advent of minimal invasive surgery, the number of ports has been reduced to further improve cosmetic outcome [4-8]. Single port laparoscopic appendectomy that requires only a single incision is becoming more popular. Various methods have been reported, from a single incision at the right iliac fossa [9] to use of a single suprapubic incision that can be concealed in the pubic hair [10]. A recent study concluded that the single port method is technically feasible even in children [11].
Among these methods, a single incision at the umbilicus is virtually scarless. There have been successful reports of the use of this transumbilical procedure in appendectomy, cholecystectomy, and other operations [12-15]. Transumbilical single port laparoscopic appendectomy (TUSPLA) is a form of single incision laparoscopic appendectomy that utilizes the transumbilical incision. Because the umbilicus has natural skin folds, has virtually no subcutaneous fat, and has a natural depression, TUSPLA can be performed easily even in obese patients.
We report a comparison of TUSPLA and three ports laparoscopic appendectomy (TLA) performed in a Korean military hospital.
METHODS
Patients
The retrospective study involved patients who received laparoscopic appendectomy between May 2011 and October 2011. A total of 63 patients were treated for acute appendicitis. Nineteen patients received TUSPLA and 44 patients received TLA. All 63 patients were fully informed concerning the TUSPLA surgery and other possible therapeutic options, including TLA and open appendectomy. Of the 63 patients, written informed consent was provided by 19 patients for TUSPLA and by 44 to receive TLA.
Reviewed patient factors were age, sex, weight, height, body mass index, and comorbidities. Outcome variables were operation time, duration of hospital stay, patient pain according to the visual analogue scale (VAS), return to diet, and postoperative complications. Postoperative pain at rest was recorded 24 ± 3 hours after surgery, using a 1 to 10 VAS scale.
The study was approved by the hospital's Institutional Review Board of the Ethical Committee.
Surgical technique
All patients received a 1st generation cephalosporin intravenously at induction of anesthesia. After surgery, patients were administered with two or more further doses of antibiotics. Preoperative preparation and anesthesia were performed in the standard manner. When performing TUSPLA, the umbilicus was cleaned thoroughly using cotton swabs. Manual evacuation of debris was done routinely. Three 5-mm trocars were attached to the digits of a small surgical glove before beginning surgery (Fig. 1). A midline incision was made inside the depression of the umbilicus. The underlying fascia was divided and the fasciotomy was widened after retracting the skin incision cranially and then caudally. The adequacy of the fasciotomy was tested by inserting the index finger into the wound. An extra-small wound retractor (ALEXIS wound retractor XS, Applied Medical, Rancho Santa Margarita, CA, USA) was applied, and the prepared surgical glove was fitted over the wound retractor. After the single port was placed into the abdominal wall, the patient was placed in the Trendelenburg position left-side down. A 30 degree 5-mm laparoscope was used as the optic instrument. Standard rigid 5-mm laparoscopic instruments or a 5-mm roticulator (Roticulator Endo Grasp, Covidien, Mansfield, MA, USA) were used. Laparoscopic appendectomy was performed conventionally. There was no need of a vinyl bag to remove the resected appendix, since the wound retractor protected the entire circumference of the incision from contamination. The appendix was pulled out of the abdominal cavity and put inside one of the free digits of the glove. The digit was tied with silk to prevent spillage (Fig. 1). The fascia was closed using absorbable suture material (Vicryl, Ethicon, Somerville, NJ, USA). Usually, two sutures were sufficient for fascia closure, and no additional skin sutures were necessary. After adequate closure, the immediate cosmetic effect was excellent (Fig. 2A). A gauze ball was placed on the depression of the umbilicus.
Fig. 1.

To make the glove port, three 5-mm trocars were attached to the digits of a small surgical glove. After appendectomy, the resected appendix was put inside one of the digits (red arrow).
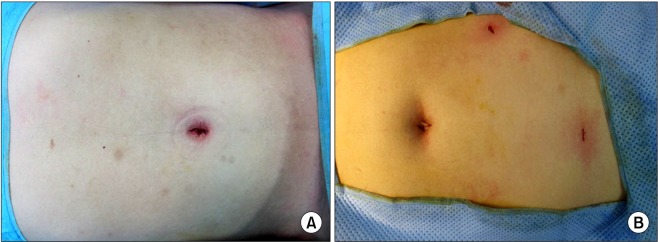
Fig. 2.
Comparison of the cosmetic effects of transumbilical single port laparoscopic appendectomy (TUSPLA) and three ports laparoscopic appendectomy (TLA) immediately after surgery. (A) After TUSPLA, the scar is concealed in the umbilicus. (B) After TLA, although a transumbilical incision was used to reduce the umbilical scar, the other two 5-mm incisions were clearly visible.
When TLA was performed, a transumbilical incision or a periumbilical incision was used for the initial approach of the laparoscope into the abdominal cavity. Under direct visualization, two more 5-mm trocars were inserted in a triangular fashion. Appendectomy was performed using conventional methods and a vinyl bag was used for specimen retrieval. The fascia at the umbilical incision and the subcutaneous fat and skin at the 5-mm incisions were closed using absorbable sutures. After closure, the 5-mm incisions were clearly visible (Fig. 2B).
RESULTS
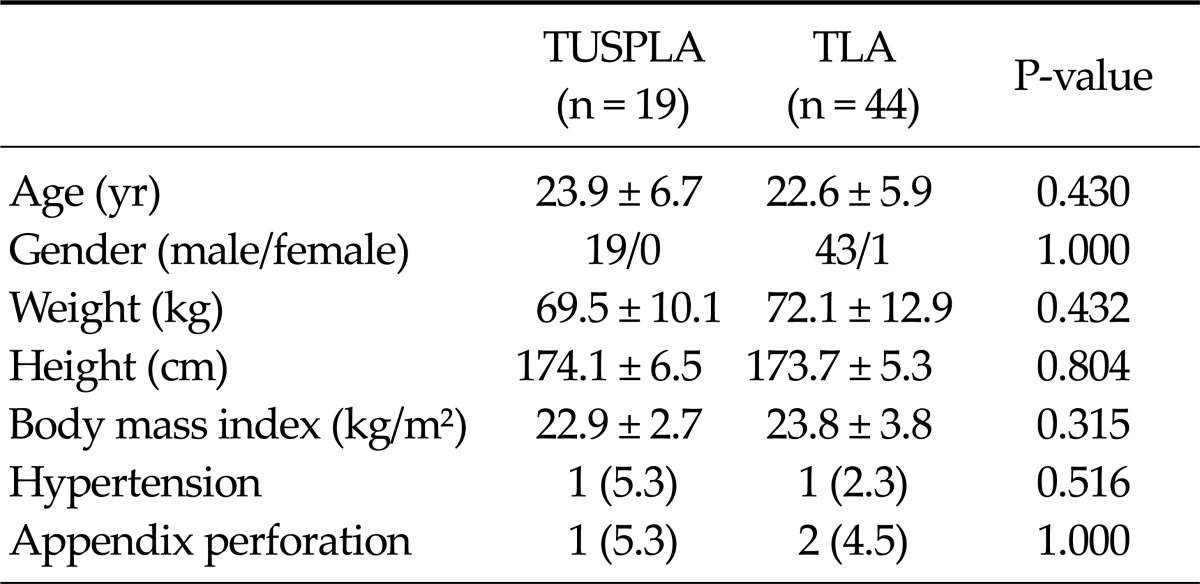
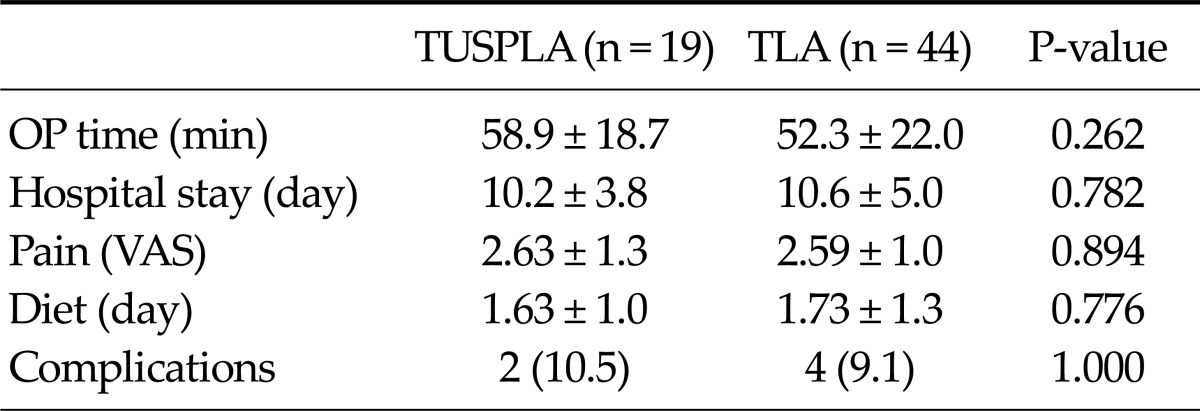
A total of 63 patients were reviewed. TUSPLA was performed on 19 patients and TLA was performed on 44 patients. There were no statistically significant differences in patient demographics (Table 1). One patient (5.3%) in the TUSPLA group and one patient (2.3%) in the TLA group had hypertension. There were no patients with diabetes, coronary artery disease, or chronic obstructive pulmonary disease in either group. One patient (5.3%) in the TUSPLA group and two patients (4.5%) in the TLA group had perforated appendicitis. The difference in patient number was not significant. TUSPLA was successfully performed in all 19 patients in the TUSPLA group, and conversion to three ports laparoscopic surgery was not necessary in any of the cases. There were no statistically significant differences in clinical data between the two groups (Table 2). There was no difference in operation time between the TUSPLA group (58.9 minutes) and the TLA group (52.3 minutes) (P = 0.262). Duration of hospital stay was 10.2 days in the TUSPLA group and 10.6 days in the TLA group (P = 0.782). The mean VAS score was 2.6 in the TUSPLA group and 2.5 in the TLA group (P = 0.894), and return to diet required 1.6 days in the TUSPLA group and 1.7 days in the TLA group (P = 0.776).
Table 1.
Patient demographics
Values are presented as mean ± standard deviation or number (%). TUSPLA, transumbilical single-port laparoscopic appendectomy; TLA, three ports laparoscopic appendectomy.
Table 2.
Postoperative clinical data
Values are presented as mean ± standard deviation or number (%). TUSPLA, transumbilical single-port laparoscopic appendectomy; TLA, three ports laparoscopic appendectomy; OP, operation; VAS, visual analogue scale.
Two patients (10.5%) in the TUSPLA group experienced short-term complications. One patient had bladder injury. This patient had an appendix perforation and an additional trocar was inserted in the suprapubic area for drainage. The bladder injury was caused by the trocar insertion. One patient developed wound infection. Both patients were successfully treated with conservative care. Four patients (9.1%) in the TLA group experienced short-term complications. One patient developed postoperative ileus. One patient developed an abscess at the appendectomy site, and reoperation was performed 6 days after the initial surgery. Two patients developed wound infection at the periumbilical incision. There were no intraoperative complications or long-term complications. Short-term complication rates showed no significant difference between the two groups. All patients recovered well and were discharged in good condition without any further complications.
DISCUSSION
Laparoscopic appendectomy is widely performed for the treatment of acute appendicitis. Single port laparoscopic appendectomy is rapidly gaining momentum due to improved cosmesis and reduced parietal trauma. TUSPLA is one type of single port laparoscopic appendectomy that yields very satisfactory cosmetic results. In our study, the clinical data of TUSPLA was comparable to that of conventional laparoscopic appendectomy. There were no significant differences in operation time, postoperative hospital stay, postoperative pain, return to diet, or complication rates. This type of surgery can be a very attractive alternative to patients, especially in the younger population.
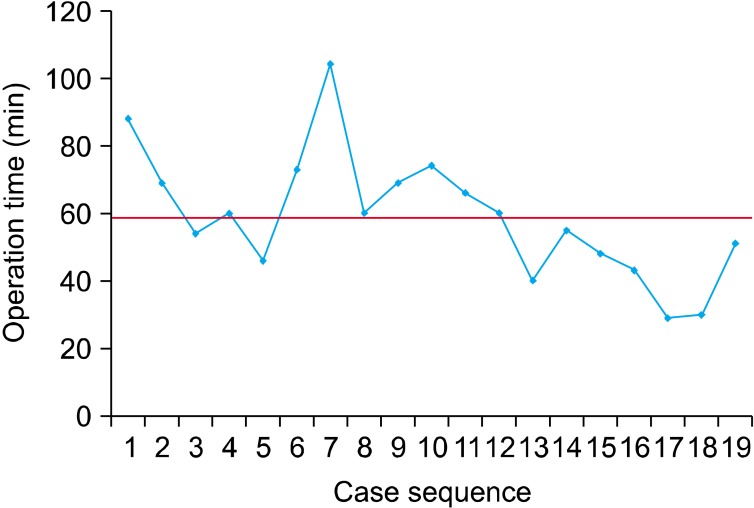
Performing TUSPLA requires experience in laparoscopic surgery, and a certain number of cases must be performed to overcome the learning curve. In our study, the mean operation time was 58.9 minutes. The cases in the beginning phase took longer than average. As the cases accumulated and operator experience was gained, the operation time tended to shorten. The last seven cases took less than the average 58.9 minutes (Fig. 3). The learning curve for single port cholecystectomy has been reported to be approximately five cases [16]. Further studies are needed to better determine the learning curve for TUSPLA.
Fig. 3.
Decreasing operation time according to surgical experience in transumbilical single port laparoscopic appendectomy group. Red line indicates the mean operation time.
Some cases may require drainage, making the term 'single port' meaningless. Even without obvious signs of perforation preoperatively, some cases show perforation when the laparoscope is inserted. In our study, there was one such case. Although there have been reports of drainage catheters put through the umbilicus, we chose to add a suprapubic incision. Even though the suprapubic port was added under direct visualization, bladder injury was discovered upon removal of the catheter. Fluorescent cystoscopy showed only extraperitoneal leakage, so the patient was treated conservatively, and was discharged in good condition 18 days after surgery.
It may be assumed that with the wider fasciotomy of the transumbilical incision, there will be more pain. Indeed, a recent study showed that pain scores measured 24 hours after surgery in patients who had received single port appendectomy were significantly higher than those of the patients who had received conventional laparoscopic appendectomy [17]. When the fasciotomy is insufficient, vigorous manipulation is needed to place the wound retractor. This may be the cause of the excess pain in single port appendectomy cases. In our study, when TUSPLA was performed, the adequacy of the fasciotomy was tested by inserting the index finger. With a sufficient fasciotomy, insertion of the wound retractor was easy, and manipulation around the umbilicus was minimal. There was no difference in VAS score or umbilical complications between the two groups. Further studies with more cases are needed to conclusively assess this issue.
Several single port systems have been used to introduce laparoscopic instruments into the abdominal cavity. Some authors have reported on the use of pre-manufactured one port systems [18-21]. Others have reported on the glove port method [22,23]. All of our patients in the TUSPLA group were operated on using the glove port. This approach offered several advantages. First, a wound retractor is the only additional material needed. All the other components are conventional material used in the operating room. Second, as noted earlier, the glove port is cost-effective. Instead of using a disposable trocar, a suction tube can be used. Also, a vinyl specimen retrieval bag is not required. Therefore, a relatively small number of disposable instruments is used, and the total cost of surgery is reduced [22]. Third, it can prevent subcutaneous emphysema, as well as port-site infection and bleeding, due to the tamponade effect of the two flanges of the wound retractor.
However, when using the glove port, clashing of the surgical instruments may lengthen the operation time. Of course, this is better when roticulating instruments are used. The use of roticulators enable triangulation of the instruments inside the abdominal cavity provides the operator a surgical field similar to that of conventional laparoscopic surgery. Also, adequate positioning of the instruments can reduce clashing. We found that inserting the optic instrument in the middle and inserting the two working instruments laterally at each side of the optic instrument helped reduce the clashing. Using various methods to reduce instrument clashing, the operation time can be reduced so it is comparable to that of conventional laparoscopic surgery. In our study, there was no difference in operation time.
Many patients diagnosed with acute appendicitis at a military hospital choose to be transferred to civilian hospitals, due to lack of trust in the operative facilities. Laparoscopic surgery is one factor that can give patients faith in the medical personnel. Although open appendectomy is still being performed, laparoscopic surgery is widely accepted as a treatment modality for acute appendicitis. When surgery methods are explained to a patient without obvious perforation, it is anticipated that the patient will choose laparoscopic surgery.
In our study, we did not use a selection criteria for choosing the surgical method. Both methods were explained to all patients admitted during the study period, and TUSPLA was performed on all patients who agreed to receiving TUSPLA. 44 of 63 patients chose to receive TLA. Although the feasibility of TUSPLA was explained in detail, since it is relatively unknown to the general population, it may have seemed more dangerous. With further integration of single port surgery, the capability of the surgeon to perform TUSPLA may have the effect of giving trust to the patients, and may reduce transfer rates to civilian hospitals.
In military hospitals, it is more difficult to introduce new operation procedures and materials into the operating room, and only basic laparoscopic equipment are available. Even with these conditions, TUSPLA was easily done using the glove port and conventional laparoscopic instruments. In many cases, the only additional operation material was the wound retractor, and the clinical data were similar to the three ports method. It seems TUSPLA can be started and performed in smaller hospitals with basic laparoscopic surgery equipment. Moreover, the clinical data of the TUSPLA group is comparable to that of other studies describing TUSPLA, with the exception of longer hospital stay. The literatures show an operation time of approximately 40 to 75 minutes, a VAS score of 2 to 3, a postoperative hospital stay of 2 to 3 days, and a complication rate ranging from 0 to 9% [14-17]. Unlike civilians, patients admitted at military hospitals are required to return immediately to active military duty immediately after discharge. For this reason admission periods tend to be longer. But, there was no significant difference in hospital stay between the TUSPLA group and the TLA group.
This study has an inherent limitation in that it is a retrospective study, and the two groups were not randomized. Also, both groups mainly consist of relatively young patients with little comorbidities, with only one female subject in the entire study. A randomized study with more cases that better represent the general population is needed for confirmation.
In conclusion, we report a comparison of TUSPLA and TLA in a Korean military hospital. TUSPLA is a safe and feasible procedure with good cosmetic results that can be considered as an alternative for laparoscopic appendectomy. It is possible to perform in a hospital equipped with laparoscopic instruments, with a minimum of additional material.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Semm K. Endoscopic appendectomy. Endoscopy. 1983;15:59–64. doi: 10.1055/s-2007-1021466. [DOI] [PubMed] [Google Scholar]
- 2.Chung RS, Rowland DY, Li P, Diaz J. A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg. 1999;177:250–256. doi: 10.1016/s0002-9610(99)00017-3. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen NT, Zainabadi K, Mavandadi S, Paya M, Stevens CM, Root J, et al. Trends in utilization and outcomes of laparoscopic versus open appendectomy. Am J Surg. 2004;188:813–820. doi: 10.1016/j.amjsurg.2004.08.047. [DOI] [PubMed] [Google Scholar]
- 4.Esposito C. One-trocar appendectomy in pediatric surgery. Surg Endosc. 1998;12:177–178. doi: 10.1007/s004649900624. [DOI] [PubMed] [Google Scholar]
- 5.Rispoli G, Armellino MF, Esposito C. One-trocar appendectomy. Surg Endosc. 2002;16:833–835. doi: 10.1007/s00464-001-9107-5. [DOI] [PubMed] [Google Scholar]
- 6.Tekin A, Kurtoglu HC. Video-assisted extracorporeal appendectomy. J Laparoendosc Adv Surg Tech A. 2002;12:57–60. doi: 10.1089/109264202753486948. [DOI] [PubMed] [Google Scholar]
- 7.Fazili FM, Al-Bouq Y, El-Hassan OM, Gaffar HF. Laparoscope-assisted appendectomy in adults: the two-trocar technique. Ann Saudi Med. 2006;26:100–104. doi: 10.5144/0256-4947.2006.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Panait L, Bell RL, Duffy AJ, Roberts KE. Two-port laparoscopic appendectomy: minimizing the minimally invasive approach. J Surg Res. 2009;153:167–171. doi: 10.1016/j.jss.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 9.Ng PC. One-puncture laparoscopic appendectomy. Surg Laparosc Endosc. 1997;7:22–24. [PubMed] [Google Scholar]
- 10.Vidal O, Ginesta C, Valentini M, Marti J, Benarroch G, Garcia-Valdecasas JC. Suprapubic single-incision laparoscopic appendectomy: a nonvisible-scar surgical option. Surg Endosc. 2011;25:1019–1023. doi: 10.1007/s00464-010-1307-4. [DOI] [PubMed] [Google Scholar]
- 11.Kang DB, Lee SH, Lee SY, Oh JT, Park DE, Lee C, et al. Application of single incision laparoscopic surgery for appendectomy in children. J Korean Surg Soc. 2012;82:110–115. doi: 10.4174/jkss.2012.82.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong TH, Kim HL, Lee YS, Kim JJ, Lee KH, You YK, et al. Transumbilical single-port laparoscopic appendectomy (TUSPLA): scarless intracorporeal appendectomy. J Laparoendosc Adv Surg Tech A. 2009;19:75–78. doi: 10.1089/lap.2008.0338. [DOI] [PubMed] [Google Scholar]
- 13.Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. Surg Endosc. 2009;23:1393–1397. doi: 10.1007/s00464-008-0252-y. [DOI] [PubMed] [Google Scholar]
- 14.Lee J, Baek J, Kim W. Laparoscopic transumbilical single-port appendectomy: initial experience and comparison with three-port appendectomy. Surg Laparosc Endosc Percutan Tech. 2010;20:100–103. doi: 10.1097/SLE.0b013e3181d84922. [DOI] [PubMed] [Google Scholar]
- 15.Chow A, Purkayastha S, Nehme J, Darzi LA, Paraskeva P. Single incision laparoscopic surgery for appendicectomy: a retrospective comparative analysis. Surg Endosc. 2010;24:2567–2574. doi: 10.1007/s00464-010-1004-3. [DOI] [PubMed] [Google Scholar]
- 16.Kravetz AJ, Iddings D, Basson MD, Kia MA. The learning curve with single-port cholecystectomy. JSLS. 2009;13:332–336. [PMC free article] [PubMed] [Google Scholar]
- 17.Kim HO, Yoo CH, Lee SR, Son BH, Park YL, Shin JH, et al. Pain after laparoscopic appendectomy: a comparison of transumbilical single-port and conventional laparoscopic surgery. J Korean Surg Soc. 2012;82:172–178. doi: 10.4174/jkss.2012.82.3.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ito M, Asano Y, Horiguchi A, Shimizu T, Yamamoto T, Uyama I, et al. Cholecystectomy using single-incision laparoscopic surgery with a new SILS port. J Hepatobiliary Pancreat Sci. 2010;17:688–691. doi: 10.1007/s00534-010-0266-4. [DOI] [PubMed] [Google Scholar]
- 19.Song T, Kim TJ, Kang HJ, Choi CH, Lee JW, Bae DS, et al. Single-port access laparoscopic surgery using a novel laparoscopic port (Octo-Port) Taiwan J Obstet Gynecol. 2011;50:436–440. doi: 10.1016/j.tjog.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 20.Saber AA, El-Ghazaly TH. Early experience with single incision transumbilical laparoscopic adjustable gastric banding using the SILS Port. Int J Surg. 2009;7:456–459. doi: 10.1016/j.ijsu.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 21.Saber AA, El-Ghazaly TH. Single-incision transumbilical laparoscopic right hemicolectomy using SILS Port. Am Surg. 2011;77:252–253. [PubMed] [Google Scholar]
- 22.Lee YS, Kim JH, Moon EJ, Kim JJ, Lee KH, Oh SJ, et al. Comparative study on surgical outcomes and operative costs of transumbilical single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy in adult patients. Surg Laparosc Endosc Percutan Tech. 2009;19:493–496. doi: 10.1097/SLE.0b013e3181c15493. [DOI] [PubMed] [Google Scholar]
- 23.Kim HJ, Lee JI, Lee YS, Lee IK, Park JH, Lee SK, et al. Single-port transumbilical laparoscopic appendectomy: 43 consecutive cases. Surg Endosc. 2010;24:2765–2769. doi: 10.1007/s00464-010-1043-9. [DOI] [PubMed] [Google Scholar]