Abstract
Objective
To report methods and results from a national sample mortality surveillance programme implemented in Viet Nam in 2009.
Methods
A national sample of 192 communes located in 16 provinces and covering a population of approximately 2.6 million was selected using multi-stage cluster sampling. Deaths for 2009 were identified from several local data sources. Record reconciliation and capture–recapture methods were used to compile data and assess completeness of the records. Life tables were computed using reported and adjusted age-specific death rates. Each death was followed up by verbal autopsy to ascertain the probable cause(s) of death. Underlying causes were certified and coded according to international guidelines.
Findings
A total of 9921 deaths were identified in the sample population. Completeness of death records was estimated to be 81%. Adjusted life expectancies at birth were 70.4 and 78.7 years for males and females, respectively. Stroke was the leading cause of death in both sexes. Other prominent causes were road traffic accidents, cancers and HIV infection in males, and cardiovascular conditions, pneumonia and diabetes in females.
Conclusion
Viet Nam is undergoing the epidemiological transition. Although data are relatively complete, they could be further improved through strengthened local collaboration. Medical certification for deaths in hospitals, and shorter recall periods for verbal autopsy interviews would improve cause of death ascertainment.
Résumé
Objectif
Rapporter les méthodes et les résultats d'un programme national de surveillance de la mortalité basée sur l’échantillonnage, mis en place au Viet Nam en 2009.
Méthodes
Un échantillon national de 192 communes situées dans 16 provinces et couvrant une population d'environ 2,6 millions de personnes a été sélectionné par échantillonnage en grappes à plusieurs degrés. Pour l’année 2009, les décès ont été identifiés sur la base de plusieurs sources d’informations locales. Le recoupement des dossiers ainsi que des méthodes de capture-recapture ont été utilisés pour compiler les informations et évaluer l'exhaustivité des dossiers. Les tables de mortalité ont été calculées en utilisant les taux de mortalité présentés et ajustés par âge. Chaque décès a été suivi d'une autopsie orale pour déterminer la ou les causes probables de la mort. Les causes sous-jacentes ont été certifiées et codées selon les normes internationales.
Résultats
Un nombre total de 9921 décès a été identifié dans la population de l'échantillon. L’exhaustivité des dossiers de décès a été estimée à 81%. Les espérances de vie à la naissance étaient, après ajustement, de respectivement 70,4 et 78,7 ans pour les hommes et les femmes. L’accident vasculaire cérébral représentait la principale cause de décès pour les deux sexes. D'autres causes importantes comprenaient les accidents de la route, les cancers et l’infection par le VIH chez les hommes, et les maladies cardiovasculaires, la pneumonie et le diabète chez les femmes.
Conclusion
Le Viet Nam est en pleine transition épidémiologique. Bien que les données soient relativement complètes, elles pourraient être encore améliorées par une collaboration locale renforcée. Une certification médicale des décès dans les hôpitaux ainsi que des délais de rappel plus courts pour les entretiens d'autopsie orale permettraient d'améliorer la constatation de la cause de la mort.
Resumen
Objectivo
Informar de métodos y resultados de un programa nacional de vigilancia de la mortalidad mediante muestras realizado en Viet Nam en 2009.
Métodos
Se seleccionó una muestra nacional de 192 municipios localizados en 16 provincias y que abarcan una población de aproximadamente 2,6 millones mediante muestreo por conglomerados multietápico. Las muertes de 2009 se identificaron por varias fuentes de datos locales. Se emplearon métodos de captura-recaptura y reconciliación de registros para recopilar datos y evaluar la integridad de los registros. Se computaron las tablas de mortalidad mediante tasas de mortalidad por edad registradas y ajustadas. Cada muerte iba acompañada de una autopsia verbal para establecer la(s) probable(s) causa(s) de la muerte. Las causas subyacentes se certificaron y codificaron según las directrices internacionales.
Resultados
Se identificó un total de 9921 muertes en la población del muestreo. Se calculó que la integridad de los registros de mortalidad fue del 81%. La esperanza de vida ajustada al nacer fue de 70,4 y 78,7 años para hombres y mujeres, respectivamente. Los accidentes cerebrovasculares fueron la principal causa en ambos sexos. Otras causas destacadas fueron los accidentes de tránsito, el cáncer y la infección por el VIH en hombres, y las enfermedades cardiovasculares, la neumonía y la diabetes en las mujeres.
Conclusión
Viet Nam está experimentando una transición epidemiológica. Aunque los datos son relativamente completos, podrían mejorarse considerablemente mediante una mayor colaboración local. Los certificados médicos de las defunciones en los hospitales y periodos recordatorios más breves para las entrevistas de las autopsias verbales mejorarían la causa de la comprobación de las muertes.
ملخص
الغرض
تقديم تقرير عن طرق ونتائج البرنامج الوطني لترصد معدل وفيات العينة الذي تم تنفيذه في فييت نام في عام 2009.
الطريقة
تم انتقاء عينة وطنية مؤلفة من 192 مجتمعاً محلياً تقع في 16 مقاطعة وتغطي حوالي 2.6 مليون نسمة باستخدام أخذ العينات العنقودي متعدد المراحل. وتم تحديد حالات الوفاة لعام 2009 من مصادر البيانات المحلية المتعددة. وتم استخدام تسوية السجلات وطرق الالتقاط-الاسترداد لتجميع البيانات وتقييم اكتمال السجلات. وتم حوسبة جداول الحياة باستخدام معدلات الوفاة التي تم الإبلاغ عنها والخاصة بالسن المصحح. وتم متابعة كل حالة وفاة من خلال التشريح الشفوي للتحقق من السبب (الأسباب) المحتملة للوفاة. وتم توثيق أسبابها الأساسية وترميزها وفقاً للمبادئ التوجيهية الدولية.
النتائج
تم تحديد ما إجماليه 9921 حالة وفاة في العينة السكانية. وتم تقدير اكتمال سجلات الوفاة بنسبة 81 %. وبلغ متوسط سنوات العمر المصححة عند الميلاد 70.4 سنة و78.7 سنة للذكور والإناث، على التوالي. وكانت السكتة الدماغية السبب الرئيسي للوفاة في كلا الجنسين. وكان من بين الأسباب الرئيسية الأخرى حوادث المرور وأمراض السرطان وعدوى فيروس العوز المناعي البشري لدى الذكور والحالات القلبية الوعائية والالتهاب الرئوي وداء السكري لدى الإناث.
الاستنتاج
تشهد فييت نام تغيراً في الأوضاع الوبائية. وبرغم اكتمال البيانات نسبياً، إلا أنه يمكن تحسينها من خلال تعزيز التعاون المحلي. ومن شأن التوثيق الطبي لحالات الوفاة في المستشفيات وقصر فترات الاستدعاء لإجراء مقابلات التشريح الشفوي أن يؤدي إلى تحسين سبب التحقق من الوفاة.
摘要
目的
报告2009 年在越南实施的全国抽样死亡率监测方案的方法和结果。
方法
使用多阶段整群抽样,选择分布在16 个省,覆盖人口约260 万的192 个市镇的全国抽样。由数个本地数据源确定2009 年的死亡人数。使用记录对账和获取-再获取方法编译数据并评估记录的完整性。使用报告和调整后的特定年龄死亡率计算生命表。每例死亡之后执行口头尸检,以确定可能的死因。按照国际准则,对根本原因进行认证和编码。
结果
抽样人口中确定共有9921 例死亡。死亡记录的完整性估计为81%。男性和女性调整后的出生时预期寿命分别为70.4 年和78.7 年。中风是导致男女死亡的主要原因。其他突出的原因:男性为道路交通事故、癌症和艾滋病感染;女性为心血管疾病、肺炎和糖尿病。
结论
越南正在经历流行病学转变。虽然数据相对完整,但可以通过加强地方合作进一步完善。医院中死亡的医学证明和更短的口头尸检面谈回忆期将会改进对死因的确认。
Резюме
Цель
Представить отчет по методам и результатам национальной программы выборочного эпиднадзора за смертностью, осуществленной во Вьетнаме в 2009 году.
Методы
Было проведено национальное выборочное исследование 192 общин, расположенных в 16 провинциях, с приблизительной численностью населения 2,6 миллиона человек с применением многоступенчатой групповой выборки. Из нескольких местных источников данных были выявлены смертельные исходы за 2009 год. Применялись методы соотнесения данных и двойного охвата в целях сопоставления данных и оценки полноты задокументированных данных. Были рассчитаны таблицы вероятности дожития с использованием зарегистрированных и скорректированных повозрастных показателей смертности. Каждая смерть сопровождалась опросом об обстоятельствах смерти в целях установления вероятных причин(-ы) смерти. Истинные причины были освидетельствованы и зашифрованы в соответствии с международными правилами.
Результаты
В выборочной совокупности выявлена 9921 смерть. Полнота регистрации количества смертей оценена в 81 %. Уточненная вероятная продолжительность жизни при рождении составляла 70,4 и 78,7 лет у мужчин и женщин соответственно. Инсульт являлся основной причиной смерти у обоих полов. Другими значимыми причинами являлись дорожно-транспортные происшествия, онкологические заболевания и ВИЧ-инфекции у мужчин, и сердечно-сосудистые заболевания, пневмония и диабет у женщин.
Вывод
Вьетнам подвержен эпидемиологическому переходу. Несмотря на относительную полноту данных, они могли быть далее улучшены через укрепление сотрудничества на местном уровне. Медицинское освидетельствование смертей в лечебных учреждениях и более короткие периоды проведения опросов об обстоятельствах смерти улучшили бы установление причины смерти.
Introduction
Key mortality indicators, such as age-specific death rates, life expectancy at birth and the leading causes of death in a population, are essential for population health assessment. Data on these standard international mortality indicators are needed in developing countries for comparative analysis, health policy, monitoring and evaluation, and epidemiological research. However, in such countries vital registration systems, which are the optimal source of these data, are seldom fully functional.1 This is the case in Viet Nam, a densely populated developing country of 88 million people located in south-eastern Asia whose population structure is rapidly changing because of declining fertility and mortality and a transition in causes of death.2 The country’s population distribution is also changing as a result of socioeconomic development and rapid urbanization. Thus, accurate measures of mortality by age, sex and cause of death from death registration systems are urgently needed to assess the on-going demographic and epidemiological transition, plan the provision of health care and design effective prevention strategies.
In light of the absence of vital registration data for Viet Nam, we undertook a detailed review of the national Vietnamese vital registration system in 2006 using a mixed-methods approach.3 The review found highly incomplete death registration and a failure to conform to international standards for reporting the cause of death. We recommended implementing a capacity-building initiative to improve the vital registration system, especially the death registration process. In response, activities have been conducted over the past four years to establish a national sample mortality surveillance system in Viet Nam consisting of passive surveillance to identify deaths from routine local data sources at the commune level, followed by a household verbal autopsy interview to ascertain the cause of each identified death. This paper reports the overall and cause-specific mortality measures generated during the first wave of these activities and discusses ways to move forward and improve the availability of local mortality data throughout the country.
Methods
Population sampling plan
Viet Nam has approximately 11 000 communes distributed across 63 provinces. We used multi-stage cluster sampling to select the surveillance population. Based on prior age-specific mortality estimates for Viet Nam, we calculated that the population under surveillance would need to yield approximately 11 000 deaths to allow us to measure age- and sex-specific mortality rates within a 15% tolerable margin of error for three broad cause of death groups: Group 1, communicable, maternal, perinatal and nutritional disorders; Group 2, non-communicable diseases; Group 3, injuries.4 This translated into an estimated total surveillance population of approximately 2.5 million people.
The Viet Nam General Statistics Office selected the communes to be included in the sample according to a stratified multi-stage cluster design. In the first stage of sampling, the 63 provinces were stratified across the eight socioeconomic regions of Viet Nam. Next, 16 provinces were selected proportionate to the size of their populations, and 12 communes were then selected from each of the 16 provinces proportionate to the number of households in each commune. In total, the sample consisted of 192 communes, 668 142 households and 2 616 056 people (approximately 3% of the national population).
Data collection
A network of five medical universities coordinated the field operations, and data were compiled for calendar years 2008 and 2009. Extensive capacity building was undertaken to train staff at the provincial, district and commune levels in data collection, management and quality control. In this manuscript, we report on deaths that had occurred in 2009. As ascertained from previous research, Viet Nam has two parallel official reporting systems for vital events at the commune level: the Justice Department and the Commune Health Centre (CHC).5 In addition, the Commune Population and Family Planning Committee (CPFPC) also maintains registers of vital events at the local level, although in most instances the records are regularly matched with and updated from CHC records.
Initially, trained commune health staff compiled a list of deaths for the reference period from each of the main sources of death data at the commune level. These sources were later collated into a single list of unique records for the reference period. The variables used to determine matched or unique records were name(s), sex, age and month of death. A range of 5 years was allowed for matching age at death and a range of 1 month for matching date of death. The correct age at death as verified at the verbal autopsy interview was used for all further analysis. At the first stage of collation, death records from the CHC and CPFPC were merged into a single list because these sources are not independent (i.e. reporting in one source influences reporting in the other). Records from the Justice Department were treated as an independent source and were matched with the CHC/CPFPC records. In the second stage of collation, the records from the Justice Department and the CHC/CPFPC data source were merged to create a single list of unique reconciled death records. This reconciled list showed the deceased individuals’ age, sex and address, as well as the source(s) of each record.
In certain rural communes, farmers’, women’s or senior citizens’ unions constitute additional sources of death records. Hence, in the third stage of collation we drew from these additional sources any deaths not identified during the second stage, and this yielded a list of all deaths for the reference calendar year.
For each death on the final list, a household interview was conducted and the Vietnamese version of the verbal autopsy questionnaire was used to explore in detail the symptoms and clinical events that preceded the death, as witnessed by the respondent.6 The detailed verbal autopsy protocols are described in an earlier manuscript.7 Briefly, household interviews were conducted by trained paramedical staff from local commune health stations. Completed questionnaires were subsequently reviewed by trained physicians who assigned the cause(s) of death using the standard International Medical Certificate of Cause of Death, as recommended by the World Health Organization (WHO).8,9 Physician reviewers were guided by a manual describing key aspects of cause-of-death assignment from verbal autopsy.10 Subsequently, a team of physicians trained in applying the coding rules in the International statistical classification of diseases and health-related problems, 10th revision (ICD-10) selected an underlying cause for each death following prescribed international guidelines.8 Causes were aggregated to the ICD-10’s Mortality tabulation list 1 for descriptive analysis.11
Data analysis
We assessed the completeness of death reporting by applying the two-source capture–recapture method proposed by Chandrasekar and Deming in 194912 to the two sources analysed at the second stage of collation (i.e. to the list derived by reconciling the Justice Department list and the combined CHC/CPFPC list). The probability of reporting a death to the Justice Department is independent of the probability of the death being recorded in the CHC/CPFPC list, and this administrative independence of the systems is a necessary condition for applying the capture–recapture method to estimate data completeness. Capture–recapture analysis was undertaken with the full set of data, and subgroup analyses were performed with the same data broken down by sex and into four age groups: 0–14, 15–59, 60–74 and 75+ years. Based on these analyses, we estimated the deaths missed by both sources in each age and sex group and summed them to the rest of the deaths to obtain the overall estimated number of deaths in the sample population. Data completeness was estimated as the proportion of all estimated deaths derived from the reconciled list.
The 95% confidence intervals (CIs) of completeness estimates were derived using the bootstrapping method in the SAS analytical software version 9.3 (SAS Institute, Cary, United States of America). The reciprocals of these measures of completeness were used to adjust the numbers of deaths from the reconciled list, and these numbers were then used to compute age-specific death rates and develop life tables for the sample population. Age- and sex-specific population counts for the sample communes were obtained from the 2009 census.
During our analyses, we noted that the deaths in the reconciled list for the 0–4 year age group were so few that they would yield implausibly low mortality rates. On closer review of the data we found that all sources were equally deficient in recording early childhood deaths (data not shown). Hence, in generating Vietnamese life tables we used WHO’s 2009 national under-five mortality estimates for Viet Nam (24.6 and 22.6 deaths per 1000 for males and females, respectively).13 We calculated the CIs for life expectancy at birth using the Chiang Silcocks method,14 and we constructed logarithmic plots to assess the plausibility of the age-specific death rates.15
Summary mortality measures derived from the routine continuous data collection process described above were compared with those from adjusted life tables developed with population data from the 2009 Vietnamese census, which employed 12-month annual recall of household deaths to estimate mortality. Census data were adjusted for data completeness using the Preston-Coale method,16 an indirect demographic technique previously used to estimate census-based mortality for Viet Nam.17 Our mortality results were also compared with modelled mortality estimates published by WHO for 200913 and by the United Nations Population Division (UNPD) for 2005–2010.18 Finally, we used descriptive analysis of leading causes of death to develop tables of the leading causes of death, by sex, for three broad age groups: 0–14, 15–59 and 60+ years. Causes of deaths identified from additional sources were included in these tables.
Results
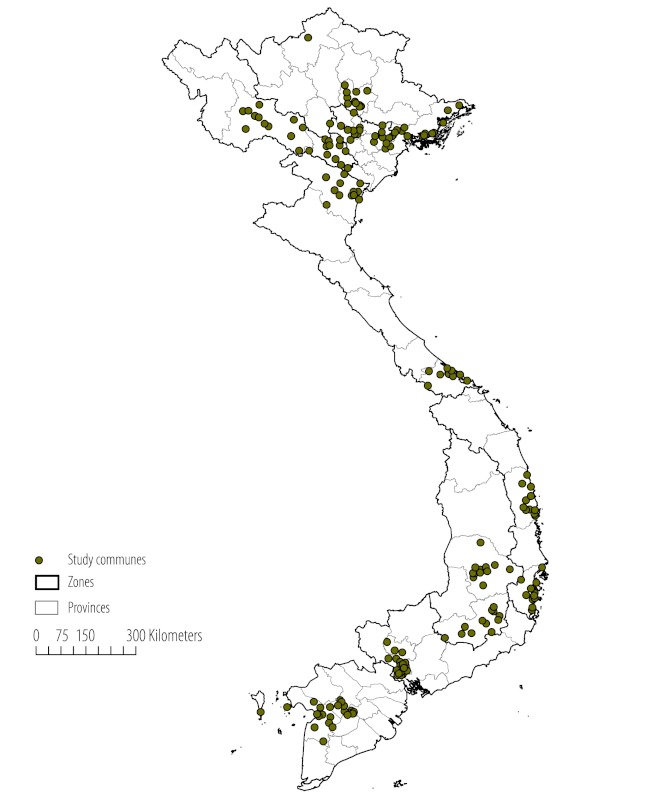
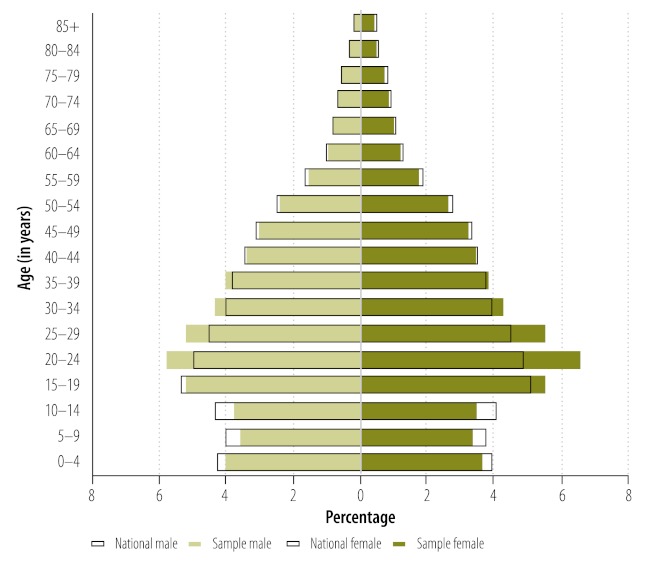
Fig. 1 shows the geographical distribution of the communes representing the sample population. Fig. 2 shows the age and sex structure of the national population and the study population. The study population had a higher proportion of people, especially females, in the 20–34 year age category than the national population. The population aged 15 years or less was slightly under-represented in the sample. More detailed analysis showed that the sample population was slightly more urban than the national population (39% versus 30%, urban communes, respectively). This may explain the differences in age structure.
Fig. 1.
Geographic distribution of communes included in the sample mortality surveillance system, Viet Nam, 2009
Source of shapefile: www.diva-gis.org
Fig. 2.
Population pyramid for the national population and study sample, Viet Nam, 2009
Table 1 shows the distribution of observed and estimated deaths from each source by age and sex. In 2009, 9921 deaths were observed in the sample population, as compared to the estimated total of 11 719 deaths from the two-source capture recapture analysis, yielding an overall completeness of 81.3% (95% CI: 74.4 to 87.1) for the reconciled list. Analyses of subgroups by sex and age showed that completeness varied very little for ages 15 and above (range: 80–83%). Completeness was only marginally different in urban and rural communes: 81.9% and 81.1%, respectively.
Table 1. Age- and sex-specific observed and estimated deathsa and completeness of mortality data, Viet Nam, 2009.
| Sex-specific age group (in years) | Sample | ab | bc | cd | xe | Other source only | Deaths |
Per cent completenessf (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|
| Observed (a + b + c + additional) | Estimated (a + b + c + x) | ||||||||
| Males | 1 239 937 | 2138 | 1984 | 1363 | 1265 | 215 | 5700 | 6750 | 81.2 (74.1–87.1) |
| 15–59 | 873 727 | 903 | 873 | 597 | 577 | 92 | 2465 | 2950 | 80.4 (72.2–80.3) |
| 60–74 | 53 985 | 453 | 414 | 274 | 250 | 38 | 1179 | 1391 | 82.0 (74.9–87.9) |
| 75+ | 22 852 | 710 | 629 | 453 | 401 | 77 | 1869 | 2193 | 81.7 (74.7–87.4) |
| Females | 1 309 462 | 1572 | 1413 | 1026 | 922 | 181 | 4192 | 4933 | 81.3 (74.4–87.1) |
| 15–59 | 929 773 | 373 | 350 | 251 | 236 | 56 | 1030 | 1210 | 80.5 (72.5–87.1) |
| 60–74 | 72 999 | 342 | 271 | 213 | 169 | 41 | 867 | 995 | 83.0 (75.4–89.0) |
| 75+ | 37 684 | 812 | 734 | 539 | 487 | 80 | 2165 | 2572 | 81.0 (73.9–87.0) |
CI, confidence interval.
a Age- and sex-specific deaths deviate slightly from the totals reported in the text because 27 deaths had no age data.
b Number of deaths reported by the Commune Health Centre, the Commune Population and Family Planning Committee (CHC/CPFPC) and the Justice Department.
c Number of deaths reported by the CHC/CPFPC but not by the Justice Department.
d Number of deaths reported by the Justice Department but not by the CHC/CPFPC.
e Estimated number of deaths missing from CHC/CPFPC and Justice Department sources.
f Proportion of estimated deaths derived from the list obtained by reconciling the Justice Department and combined CHC/CPFPC lists. Derived with the following formula: (a + b + c) ÷ (a + b + c + x) × 100.
The completeness estimates obtained with the Preston-Coale indirect demographics method were 65.6% for males and 57.8% for females (Table 2), both higher than estimates from the 1989 Vietnamese census (55% for males and 47% for females)17 but markedly lower than our direct estimates of completeness based on capture–recapture analysis.
Table 2. Summary sex-specific measures of mortality based on WHO, UNPD and Viet Nam census data for the 16 study provinces, Viet Nam, 2009.
| Data source | Per cent data completeness (95% CI) | Life expectancy at birth (95% CI) [e0] | Risk of death in children under 5 (deaths per 1000) [5q0] | Risk of death at ages 15–59 (deaths per 1000) [45q15] | Remaining years of life at age 60 [e60] |
|---|---|---|---|---|---|
| Males | |||||
| Surveillance sample (unadjusted) | – | 74.4 (74.0–74.8) | 7.4 | 163 | 20.9 |
| Surveillance sample (adjusted)a | 81.1 (74.1–87.1) | 70.4 (70.1–70.8) | 24.6c | 199 | 19.4 |
| Viet Nam census (unadjusted) | – | 75.2 (75.0–75.4) | 10.9 | 157 | 22.1 |
| Viet Nam census (adjusted)b | 65.6 (–) | 68.8 (68.6–69.0) | 16.5 | 230 | 17.9 |
| WHO (2009) | NA (modelled) | 69.8 (–) | 24.6 | 173 | 17 |
| UNPD (2005–2010) | NA (modelled) | 72.3 (–) | No data | 139 | No data |
| Females | |||||
| Surveillance sample (unadjusted) | – | 82.3 (82.0–82.7) | 5.8 | 57 | 25.1 |
| Surveillance sample (adjusted)a | 81.3 (74.4–87.1) | 78.7 (78.4–79.0) | 22.5c | 71 | 23.6 |
| Viet Nam census (unadjusted) | – | 85.2 (85.0–85.6) | 8.8 | 50 | 28.4 |
| Viet Nam census (adjusted)b | 57.8 (–) | 77.8 (77.5–78.0) | 15.7 | 86 | 22.4 |
| WHO (2009) | NA (modelled) | 74.5 (–) | 22.6 | 107 | 19.8 |
| UNPD (2005–2010) | NA (modelled) | 76.2 (–) | No data | 96 | No data |
CI, confidence interval; NA, not applicable; UNPD, United Nations Population Division; WHO, World Health Organization.
a Adjusted for data incompleteness and mortality in children under 5 years of age.
b Adjustment by the Preston-Coale method.
c WHO estimate.
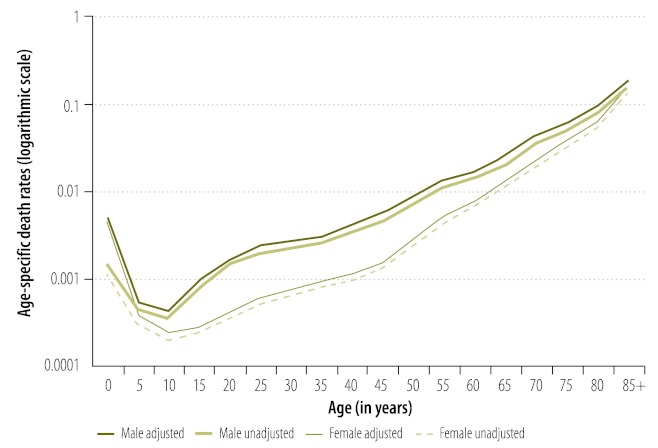
Logarithmic plots of age- and sex-specific mortality rates for both unadjusted and adjusted local data demonstrated a smooth exponential increase in groups older than 15 years, which suggests that stated age was accurate and that sample size was adequate (Fig. 3). Table 2 presents the summary mortality measures for Viet Nam derived from different sources. The adjusted life expectancy at birth for males as calculated from our data fell within the range of the estimates derived from Vietnamese census data and WHO/UNPD model life tables. However, life expectancy at birth for females as calculated from our data was substantially higher than UNPD model life table estimates because in our data the observed risk of death for adult females was lower. There are two possible reasons for this difference. First, WHO/UNPD model life tables are based on historical data sets whose corresponding female adult mortality rates may have been higher than current rates as estimated from the local data presented here. On the other hand, our sample population, which was more urban than the national population, may have had lower female adult mortality. These differences between adjusted local data and model life tables data merit future reappraisal using improved data from nationally representative samples.
Fig. 3.
Logarithmic plots of age- and sex-specific mortality rates (unadjusted and adjusted), Viet Nam, 2009
Table 3 shows the leading causes of death in 2009. Stroke was the leading cause in both males and females, as observed in other Asian countries, notably China, Indonesia and Thailand.19–22 In males, transport accidents, infectious diseases (particularly HIV infection and tuberculosis), and tobacco- and alcohol-related conditions (especially lung cancer, chronic obstructive pulmonary disease and liver diseases) were among the leading causes. In women, diseases of the circulatory system accounted for four of the five leading causes of death. In women, diseases of the circulatory system account for four of the five leading causes of death. Of these, stroke and ischaemic heart disease are specific conditions, but the categories ranking third and fifth (i.e. hypertensive disease and “other heart disease”, which includes cardiac arrest and heart failure) are relatively non-specific. In addition, one quarter of all female deaths were assigned to ill-defined causes. However, in terms of age distribution, only 5.5% of deaths among females aged 15 to 59 years were assigned to ill-defined causes, in contrast to 31% of the deaths among women aged 60 years or older (data not shown). This illustrates the poor quality of cause-of-death attribution among elderly females.
Table 3. Leading causes of death, all ages, Viet Nam, 2009.
| Ranking of causes | Males |
Females |
|||||
|---|---|---|---|---|---|---|---|
| Cause (ICD-10 code) | No. | %a | Cause (ICD-10 code) | No. | %a | ||
| 1 | Cerebrovascular disease (I60–169) | 951 | 16.6 | Cerebrovascular disease (I60–169) | 760 | 18.0 | |
| 2 | Transport accident (V00–V99) | 433 | 7.6 | Pneumonia (J12–J18) | 169 | 4.0 | |
| 3 | Liver cancer (C22) | 369 | 6.4 | Hypertensive disease (I10–I14) | 147 | 3.5 | |
| 4 | Lung cancer (C33–C34) | 270 | 4.7 | Ischaemic heart disease (I20–I25) | 147 | 3.5 | |
| 5 | Pneumonia (J12–J18) | 211 | 3.7 | Other heart diseases (I26–I51) | 126 | 3.0 | |
| 6 | Ischaemic heart disease (I20–I25) | 209 | 3.7 | Liver cancer (C22) | 125 | 3.0 | |
| 7 | HIV disease (B20–B24) | 206 | 3.6 | Chronic respiratory disease (J40–47) | 122 | 2.9 | |
| 8 | Non-malignant liver disease (K70–76) | 197 | 3.4 | Diabetes mellitus (E10–E14) | 119 | 2.8 | |
| 9 | Chronic respiratory disease (J40–J47) | 193 | 3.4 | Transport accident (V00–V99) | 102 | 2.4 | |
| 10 | Respiratory tuberculosis (A15–A19) | 187 | 3.3 | Lung cancer (C33–C34) | 92 | 2.2 | |
| Ill-defined condition (R00–R99) | 656 | 11.5 | Ill-defined condition (R00–R99) | 1048 | 24.9 | ||
| All other causes | 1822 | 31.9 | All other causes | 1259 | 29.9 | ||
| Total | 5704 | 99.8b | Total | 4215 | 100.1b | ||
ICD-10, International statistical classification of diseases and related health problems, tenth revision.
a Percentage of all deaths.
b These totals deviate from 100% due to rounding.
Discussion
The mortality patterns reported here for Viet Nam are based on empirical observations. The life tables were derived from observed age-specific mortality rates adjusted for completeness, unlike previous model life tables, which were derived from summary input parameters. Furthermore, verbal autopsies yielded individual causes of death that were summed to derive mortality ranks by cause at the population level. In a broader context, these local data conform to the standard international indicators used to measure and compare mortality patterns. In addition, local data are necessary to understand prevailing epidemiological conditions and are politically relevant for public health policy as well as clinical intervention programmes. This is particularly relevant because previous cause-specific mortality estimates for Viet Nam were based on models derived from a combination of Chinese, Indian and Thai data.23 This sample-based passive mortality surveillance system using routine local data sources in a national set of population clusters provides a basis for the continued availability of international standard mortality measures for Viet Nam.
The adjusted life expectancies at birth and risks of death in adults, together with mortality rates in children less than 5 years of age (from the Demographic and Health Survey), suggest that Viet Nam has lower mortality rates than other developing countries in south-eastern Asia.13 Also, non-communicable diseases account for a large proportion of the deaths, as reported in Table 3. However, communicable diseases continue to cause considerable mortality in Viet Nam, but largely among adults; populations in earlier stages of epidemiological transition have high mortality from childhood infectious diseases. Furthermore, although liver cancer is a leading cause of death in both males and females, chronic hepatitis B among adults probably accounts for a large proportion of liver cancers in Viet Nam.24 Although these mortality indicators suggest that Viet Nam is experiencing an epidemiological transition, the country’s current mixed burden of communicable and non-communicable diseases, as well as injuries, illustrates that the country’s health sector priorities cover a broad range.
The absence of maternal conditions among the leading causes of death among women 15 to 59 years of age (data not shown) probably stems from Viet Nam’s very low fertility rate, measured at 2.03 from the 2009 census.25 However, we may have failed to adequately capture rural maternal deaths in our data set because of the relatively large proportion of urban communes in our sample. As mentioned, stroke was the leading cause of death in both males and females, and mortality from cardiovascular disease was high in women. Research has indicated that deaths attributed to non-specific cardiovascular categories, such as hypertensive disease, heart failure and cardiac arrest, could in reality be misclassified deaths from ischaemic heart disease.26,27 However, from a more general perspective, attribution to such non-specific categories limits the public health utility of cause-of-death data.28 More efforts to assess the validity and reliability of cause-of-death attribution in Viet Nam are needed. A national non-communicable-disease surveillance framework has been developed in Viet Nam,29 and a routine mortality data programme with suitable data quality control mechanisms, such as the one reported here, is needed in the country to provide important information on chronic disease outcomes.
The data presented here have several limitations, as does the operation of the surveillance system. First, reporting practices for all three sources vary widely in different parts of the country. For example, in Thai Nguyen province, the CHC and the Justice Department sources capture 85% and 15% of the deaths, respectively, in the reconciled list, whereas in Ho Chi Minh, the CHC captures only 17% of the deaths and the Justice Department captures 76%. Hence, reconciling the data across sources was necessary to estimate total mortality in the population. Given the need to closely monitor and follow up the deaths recorded in different sources, our mortality statistical compilation process from routine data sources may be described as passive surveillance, as distinct from the active and more costly door-to-door surveillance operations in demographic data collection programmes.
We have shown that the reconciled list captured 80% of deaths in the sample population, more than any individual source. Higher completeness could thus be achieved through stronger local collaboration between different recording systems at the point of registration. However, such collaboration would make routine application of capture–recapture methods to assess completeness impossible, since the different data sources would no longer be independent of each other. Although indirect demographic techniques (such as the Preston-Coale method) could also be used to estimate completeness, such techniques have limitations30 that make direct measurement of completeness using the capture–recapture method, as reported here, the recommended approach. In such a situation, periodic sample household surveys could provide an additional set of independent data with which to assess completeness using the capture–recapture method, as previously used elsewhere in Asia.31–33
Data recorded in local maternal and child health registers in Viet Nam and in routine reproductive health statistical returns are potentially useful supplementary data sources for improving data completeness.34,35 However, health facilities, especially in urban areas, need to make birth and death records available to improve measures of infant mortality.
The sample population resembles the national population in terms of age structure, but the group composed of females aged 20–34 years was an exception, perhaps because we selected the sample from a pre-census mapping list of households in communes, rather than actual population data. The fact that, as a result, the sample population had a higher fraction of urban communes than the country as a whole could have led to an underestimation of national mortality rates, since urban communities in Viet Nam probably enjoy better health care and health status than rural ones. The sample size, on the other hand, appears adequate for measuring mortality at the national level but would need to be increased to achieve representativeness at the regional level. Any future enlargement of the surveillance sample should take into account the country’s urban–rural ratio and the age and sex composition of the population.
Concerning cause-of-death ascertainment, household enquiries have resulted in more detailed diagnoses than those afforded by the rudimentary four-category classification used for statistical compilation in Viet Nam’s routine death registration system: disease or old age; accident, suicide and “other”.3 Nevertheless, the high proportions of deaths classified to non-specific causes among the elderly and in women signals the need for improvement. For deaths in 2009, verbal autopsy recall periods ranged from 8 to 18 months, which could have undermined the accuracy of questionnaire responses, particularly with respect to symptoms and clinical events among the elderly. The choice of respondents in terms of education and closeness to the deceased during the terminal illness could also affect the quality of verbal autopsy interviews and limit the information physician reviewers have to draw on to formulate specific diagnoses. To counter this, the household enquiry process should be conducted closer to the date on which the death is notified, while allowing enough time for bereavement,36 and training on choosing respondents should be intensified.
The inherent weaknesses of verbal autopsy led us to realize that it is essential to establish medical certification of causes for deaths occurring in health facilities in Viet Nam. We therefore used balance funds from the main project to develop medical death certification protocols for institutional deaths, and we conducted a pilot study in five hospitals in 2010 (unpublished report). This experience demonstrated the feasibility of implementing medical death certification in hospitals in Viet Nam, and efforts to broaden coverage beyond those facilities are under way. Verification of the occurrence of death and its cause through local disease-specific programme data would enhance the completeness and quality of sample mortality surveillance data. Maintenance of medical records in commune and district-level health facilities would also improve access to more reliable medical inputs for ascertaining the cause of death.
Conclusion
The epidemiological findings from this research suggest a mixed mortality burden from both communicable and non-communicable diseases and from road traffic accidents in Viet Nam, and they illustrate the complex epidemiological transition currently taking place in the country. Such data provide baseline evidence for designing public health interventions and programmes. Sustained follow-up activities are required to maintain this data collection platform, as well as to conduct additional research to assess and improve data quality for monitoring mortality indicators. Given the size and distribution of the population in Viet Nam, the surveillance system must enlarge its sample. Sample mortality surveillance in a developing country like Viet Nam is beneficial provided appropriate attention is paid to design and operations.
Acknowledgements
This research was partially supported by a grant from the Atlantic Philanthropies. We acknowledge the guidance provided by Gail Williams at the School of Population Health, University of Queensland, in conducting the bootstrap analysis to derive uncertainty bounds for the completeness estimates.
Competing interests:
None declared.
References
- 1.Mahapatra P, Shibuya K, Lopez AD, Coullare F, Notzon FC, Rao C, et al. Civil registration systems and vital statistics: successes and missed opportunities. Lancet. 2007;370:1653–63. doi: 10.1016/S0140-6736(07)61308-7. [DOI] [PubMed] [Google Scholar]
- 2.Minh HV, Byass P, Wall S. Mortality from cardiovascular diseases in Bavi District, Vietnam. Scand J Public Health Suppl. 2003;62:26–31. doi: 10.1080/14034950310015077. [DOI] [PubMed] [Google Scholar]
- 3.Rao C, Osterberger B, Anh TD, MacDonald M, Chuc NT, Hill PS. Compiling mortality statistics from civil registration systems in Viet Nam: the long road ahead. Bull World Health Organ. 2010;88:58–65. doi: 10.2471/BLT.08.061630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Begg S, Rao C, Lopez AD. Design options for sample-based mortality surveillance. Int J Epidemiol. 2005;34:1080–7. doi: 10.1093/ije/dyi101. [DOI] [PubMed] [Google Scholar]
- 5.Huy TQ, Johansson A, Long NH. Reasons for not reporting deaths: a qualitative study in rural Vietnam. World Health Popul. 2007;9:14–23. doi: 10.12927/whp.2007.18739. [DOI] [PubMed] [Google Scholar]
- 6.Nguyen TKC, Nguyen PH, Rao C, Ngo DA. Xác đinh nguyên nhân cái chet bang cách su dung các cuoc phong van: tài lieu đào tao cho nguoi phong van [Identification of cause of death using interviews: training document for interviewers]. Hanoi: Viet Nam Ministry of Health; 2011. Vietnamese. [Google Scholar]
- 7.Ngo AD, Rao C, Hoa NP, Adair T, Chuc NTK. Mortality patterns in Vietnam, 2006: findings from a national verbal autopsy survey. BMC Res Notes. 2010;3:78. doi: 10.1186/1756-0500-3-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mortality: guidelines for certification and rules for coding. In: Vol. 2, International statistical classification of diseases and related health problems, tenth revision Geneva: World Health Organization; 1993. pp. 30-65. [Google Scholar]
- 9.Verbal autopsy standards: ascertaining and attributing cause of death. Geneva: World Health Organization; 2007. [Google Scholar]
- 10.Nguyen TKC, Nguyen PH, Rao C, Ngo DA. Xác đinh nguyên nhân cái chet bang cách su dụng các cuoc phong van: đào tao tài lieu cho các bác sĩ và các nhà nghiên cuu [Identification of cause of death using interviews: training document for doctors and researchers]. Hanoi: Viet Nam Ministry of Health; 2011. Vietnamese. [Google Scholar]
- 11.Special tabulation lists for mortality and morbidity: mortality tabulation list 1. In: Vol. 1, International statistical classification of diseases and related health problems, tenth revision Geneva: World Health Organization; 1993. pp. 1207-10. [Google Scholar]
- 12.Chandrasekar C, Deming WE. On a method of estimating birth and death rates and the extent of registration. J Am Stat Assoc. 1949;44:101–15. [Google Scholar]
- 13.World Health Organization [Internet]. Life tables for WHO Member States. Geneva: WHO; 2012. Available from: http://www.who.int/healthinfo/statistics/mortality_life_tables/en/ [accessed 19 July 2012].
- 14.Schoen R. Calculating life tables by estimating Chiang's a from observed rates. Demography. 1978;15:625–35. doi: 10.2307/2061212. [DOI] [PubMed] [Google Scholar]
- 15.Gompertz B. On the nature of the function expressive of the law of human mortality, and on a new mode of determining the value of life contingencies. Philos Trans R Soc Lond. 1825;115:513–83. doi: 10.1098/rstl.1825.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Preston S, Coale AJ, Trussell J, Weinstein M. Estimating the completeness of reporting of adult deaths in populations that are approximately stable. Popul Index. 1980;46:179–202. doi: 10.2307/2736122. [DOI] [PubMed] [Google Scholar]
- 17.Merli MG. Mortality in Vietnam, 1979-1989. Demography. 1998;35:345–60. doi: 10.2307/3004042. [DOI] [PubMed] [Google Scholar]
- 18.United Nations. Department of Economic and Social Affairs, Population Division [Internet]. World population prospects, the 2010 revision. New York: UNPD; 2011. Available from: http://esa.un.org/unpd/wpp/Excel-Data/mortality.htm [accessed 19 July 2012]. [Google Scholar]
- 19.Porapakkham Y, Rao C, Pattaraarchachai J, Polprasert W, Vos T, Adair T, et al. Estimated causes of death in Thailand, 2005: implications for health policy. Popul Health Metr. 2010;8:14. doi: 10.1186/1478-7954-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rao C, Soemantri S, Djaja S, Suhardi S, Adair T, Wiryawan Y, et al. Mortality in Central Java: results from the indonesian mortality registration system strengthening project. BMC Res Notes. 2010;3:325. doi: 10.1186/1756-0500-3-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rao C, Yang G, Hu J, Ma J, Xia W, Lopez AD. Validation of cause-of-death statistics in urban China. Int J Epidemiol. 2007;36:642–51. doi: 10.1093/ije/dym003. [DOI] [PubMed] [Google Scholar]
- 22.Wang L, Yang G, Jiemin M, Rao C, Wan X, Dubrovsky G, et al. Evaluation of the quality of cause of death statistics in rural China using verbal autopsies. J Epidemiol Community Health. 2007;61:519–26. doi: 10.1136/jech.2005.043927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The global burden of disease: 2004 update Geneva: World Health Organization; 2008. Available from: http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf [accessed 19 July 2012].
- 24.Gish RG, Bui TD, Nguyen CT, Nguyen DT, Tran HV, Tran DM, et al. Liver disease in Viet Nam: screening, surveillance, management and education: a 5-year plan and call to action. J Gastroenterol Hepatol. 2012;27:238–47. doi: 10.1111/j.1440-1746.2011.06974.x. [DOI] [PubMed] [Google Scholar]
- 25.United Nations Viet Nam [Internet]. Sample results from census show fertility rate in Viet Nam remains below replacement level. Ha Noi: UN; 2012: Available from: http://www.un.org.vn/en/feature-articles-press-centre-submenu-252/1080-sample-results-from-census-show-fertility-rate-in-viet-nam-remains-below-replacement-level-.html [accessed 19 July 2012].
- 26.Khosravi A, Rao C, Naghavi M, Taylor R, Jafari N, Lopez AD. Impact of misclassification on measures of cardiovascular disease mortality in the Islamic Republic of Iran: a cross-sectional study. Bull World Health Organ. 2008;86:688–96. doi: 10.2471/BLT.07.046532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahern RM, Lozano R, Naghavi M, Foreman K, Gakidou E, Murray CJ. Improving the public health utility of global cardiovascular mortality data: the rise of ischemic heart disease. Popul Health Metr. 2011;9:8. doi: 10.1186/1478-7954-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Naghavi M, Makela S, Foreman K, O'Brien J, Pourmalek F, Lozano R. Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metr. 2010;8:9. doi: 10.1186/1478-7954-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization. Representative Office in Viet Nam [Internet]. Noncommunicable diseases. Hanoi: World Health Organization; 2009. Available from: http://www.wpro.who.int/vietnam/sites/dhp/ncd/background.htm [accessed 19 July 2012]. [Google Scholar]
- 30.Murray CJ, Rajaratnam JK, Marcus J, Laakso T, Lopez AD. What can we conclude from death registration? Improved methods for evaluating completeness. PLoS Med. 2010;7:e1000262. doi: 10.1371/journal.pmed.1000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang G, Hu J, Rao KQ, Ma J, Rao C, Lopez AD. Mortality registration and surveillance in China: history, current situation and challenges. Popul Health Metr. 2005;3:3. doi: 10.1186/1478-7954-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vapattanawong P, Prasartkul P. Under-registration of deaths in Thailand in 2005–2006: results of cross-matching data from two sources. Bull World Health Organ. 2011;89:806–12. doi: 10.2471/BLT.10.083931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rao C, Kosen S, Bisara D, Usman Y, Adair T, Djaja S, et al. Tuberculosis mortality differentials in Indonesia during 2007-2008: evidence for health policy and monitoring. Int J Tuberc Lung Dis. 2011;15:1608–14. doi: 10.5588/ijtld.11.0018. [DOI] [PubMed] [Google Scholar]
- 34.Nguyen L. Evaluating completeness of antenatal, delivery and immunization registers to measure mortality in children under one year in the central region of Vietnam Brisbane: University of Queensland; 2011. [Google Scholar]
- 35.Diep T. The completeness of the infant mortality recording system in rural northern Vietnam: potential for improvement Brisbane: University of Queensland; 2011. [Google Scholar]
- 36.Chandramohan D, Maude GH, Rodrigues LC, Hayes RJ. Verbal autopsies for adult deaths: issues in their development and validation. Int J Epidemiol. 1994;23:213–22. doi: 10.1093/ije/23.2.213. [DOI] [PubMed] [Google Scholar]