Abstract
Objectives
To determine the effects of a brief psychological intervention (brief psychodynamic interpersonal therapy) for patients after deliberate self poisoning compared with usual treatment. To compare the impact of the active intervention and usual treatment on patients' satisfaction with care.
Design
Randomised controlled trial.
Participants
119 adults who had deliberately poisoned themselves and presented to the emergency department of a teaching hospital.
Setting
Community based study.
Intervention
Four sessions of therapy delivered in the patient's home. Control patients received “treatment as usual,” which in most cases consisted of referral back to their general practitioner.
Outcome measures
Severity of suicidal ideation six months after treatment as assessed by the Beck scale for suicidal ideation. Secondary outcome measures at six month follow up included depressive symptoms as measured by the Beck depression inventory, patient satisfaction with treatment, and self reported subsequent attempts at self harm.
Results
Participants randomised to the intervention had a significantly greater reduction in suicidal ideation at six month follow up compared with those in the control group (reduction in the mean (SD) Beck scale 8.0 v 1.5). They were more satisfied with their treatment and were less likely to report repeated attempts to harm themselves at follow up (proportion repeating 9% v 28% in control group; difference 19%, 95% confidence interval 9% to 30 %, P=0.009).
Conclusion
Brief psychodynamic interpersonal therapy may be a valuable treatment after people have deliberately tried to poison themselves.
What is already known on this topic
Deliberate self poisoning is one of the commonest reasons for admission to hospital in the United Kingdom and up to 15% of patients who poison themselves eventually kill themselves
There are no interventions of proved efficacy for these patients
Most episodes of self poisoning are precipitated by some form of interpersonal problem
What this study adds
Compared with usual treatment four sessions of psychodynamic interpersonal therapy reduced suicidal ideation and self reported attempts at self harm
The intervention also improved patients' satisfaction with care
Introduction
Deliberate self poisoning is one of the commonest reasons for medical admission in the United Kingdom.1 Of patients presenting to hospital with deliberate self poisoning, 3% to 15% eventually kill themselves.2–4 However, services for this problem remain poorly organised,5 probably because there are no interventions of proved efficacy. A recent systematic review concluded that while some treatments showed promise, further randomised intervention trials were required.6
About 70% of all episodes of deliberate self harm are precipitated by an interpersonal problem,7 so there is a strong rationale for investigating the efficacy of an interpersonal intervention. We used a randomised controlled trial to determine whether a brief psychological treatment compared with usual treatment for deliberate self poisoning results in decreased suicidal ideation, reduced severity of depressive symptoms, and a reduction in further episodes of self harm.
Methods
The study was conducted at the emergency department of a university hospital. Patients between the ages of 18-65 years were considered eligible for the study if they presented with an episode of deliberate self poisoning.8 Participants had to be able to read and write English, be living within the catchment area of the hospital, be registered with a general practitioner, and not need inpatient psychiatric treatment.
Consecutive patients meeting inclusion criteria were invited to take part in the study by the emergency department doctor who assessed them at the time of presentation. The study was then explained in detail by one of the research team (FM-F, EM), who was not involved in any other aspect of their treatment. After the patient gave signed consent, the recruiting member of the research team referred to a allocation sequence, provided by the trial statistician (BT) and based on a computer generated list of random numbers, to assign patients to the psychotherapy intervention or usual treatment in blocks of 12 participants. The groups were stratified according to whether or not they had a history of self harm.
Psychotherapy intervention
Patients in the intervention group were offered four sessions of psychodynamic interpersonal therapy within one week of presentation. This therapy entails identifying and helping to resolve interpersonal difficulties which cause or exacerbate psychological distress. The model was developed by Hobson9 and is described in a standardised manual.10 It has proved efficacy in the treatment of depression11,12 and has been shown to be cost effective.13
The therapy was adapted for use with patients who have harmed themselves and was delivered by nurse therapists (CT, GB, SS) in the patient's home. Sessions were offered weekly and lasted 50 minutes. Treatment fidelity and adherence was ensured by weekly supervision, audiotaping of interviews, and use of a standardised rating scale.10 During each session the therapists assessed the risk of suicide and liaised with the patient's general practitioner.
Usual care
Patients who were randomised to the “treatment as usual” arm received routine care. In most cases this consists of an assessment by a casualty doctor or a junior psychiatrist in the emergency department, on the basis of which about one third patients are referred for follow up as a psychiatry outpatient, a small number are referred to addiction services, and the remainder are advised to consult their own general practitioner.5 No patients are routinely referred to psychotherapy or psychology services.
Outcome measures
We considered suicidal ideation as our primary outcome measure because it is an important predictor of successful suicide.14 We took a difference of 5 points on the Beck scale for suicidal ideation to be clinically significant.15 The standard deviation (SD) of this scale in a previous study was 7.7.16 Assuming α=0.05 and β=0.2 and allowing for a one third drop out rate, we calculated we would need to recruit 60 patients to each group. We considered depressive symptoms, patients' satisfaction with their treatment, and repetition of deliberate self harm as secondary outcome measures.
Patients were assessed on entry to the study, at the end of the one month treatment phase, and six months later. Patients completed the Beck scale for suicidal ideation.17 This is a 19 item instrument which measures the intensity, duration, and specificity of a patient's thoughts about committing suicide. Participants also completed the Beck depression inventory,18 which is a 21 item scale measuring symptoms of depression. Higher scores on the scales indicate greater suicidal intent and greater severity of depression. We assessed patient satisfaction at the end of treatment and at six month follow up using a 10 point scale (responses ranging from 0=not satisfied to 10=extremely satisfied).
Episodes of self harm
Patients were asked to give a detailed description of further episodes of self harm at one month and six month assessments. Episodes were included if they met a standard definition.8 In addition, a separate check of the hospital database was carried out by a researcher (NK), blind to the trial groups, to determine whether patients lost to follow up had presented with deliberate self harm during the study period. We recorded all methods of self harm, including self poisoning.
Resource utilisation
We collected information on use of health services at each assessment on the basis of a well established method for recording data on health economics.19 Follow up assessments were conducted by one of two research assistants (EM, FM-F), who were blind to treatment groups. The study was granted ethical approval from the Central Manchester ethics committee.
Data analysis
We included in the analysis all patients who completed the assessments at the end of treatment or at six month follow up assessments. Comparisons between groups were made on an intention to treat basis. Patients were included in the groups to which they were allocated after randomisation regardless of how long, or even whether, they received the treatment assigned. We compared normally distributed variables using t tests and used analysis of covariance in the comparisons at follow up to adjust for baseline differences.
Results
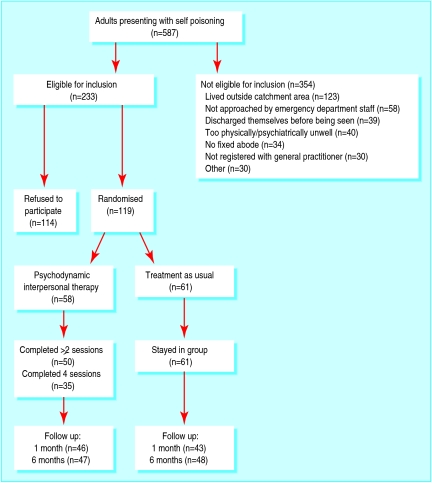
During the recruitment phase of the study 587 adults presented with deliberate self poisoning. Of these, 354 were ineligible. The figure shows progress through the study. Of the 233 patients eligible for the study, 119 (51%) agreed to participate. They were similar to those who declined in terms of sex and employment status but were more likely to have a history of self harm (59% v 45%), to have left a suicide note at the time of the current episode (23% v 5%), and to express a wish to die (76% v 46%).
Of the 119 participants, 66 (56%) were women and the mean (SD) age was 31.2 (1.5) years. Thirty three patients (28%) were married or cohabiting, and 19 (16%) were in paid employment. Paracetamol was the drug most commonly chosen for self poisoning (36% of patients). Seventy one (60%) had a history of self harm, and 67 (56%) had a history of psychiatric treatment. The intervention and usual treatment groups were similar in terms of baseline characteristics with the exception of marital status (table 1).
Table 1.
Demographic and clinical characteristics of patients admitted for deliberate self poisoning according to treatment group at baseline. Figure are numbers of participants
| Intervention group (n=58) | Treatment as usual group (n=61) | |
|---|---|---|
| Women | 33 | 33 |
| Married | 8 | 25 |
| Employed | 8 | 11 |
| Incapable of work | 21 | 22 |
| Evidence of planning | 15 | 12 |
| Suicide note | 14 | 8 |
| Avoided discovery | 14 | 13 |
| Wanted to die | 47 | 44 |
| Alcohol with overdose | 34 | 35 |
| Psychiatric history | 28 | 37 |
| History of deliberate self harm | 33 | 38 |
Psychological assessments were completed on 89 (75%) patients at the end of the treatment phase and 95 (80%) patients at six month follow up. Patients assessed at follow up were similar to those lost to follow up in terms of baseline clinical and demographic characteristics. The mean (SD) baseline score on the Beck scale for suicidal ideation for those who completed questionnaires at six months was 15.9 (10.5) compared with 11.7 (9.3) for those who did not complete a questionnaire at six months.
Symptom measures
Patients who received psychotherapy showed greater improvement on the outcome measures than patients in the control group at six month assessment (table 2). When we adjusted for differences in marital status between the groups, the differences in the scores on the Beck scale for suicidal ideation remained significant (P=0.027) but the scores for the Beck depression inventory did not (P=0.11).
Table 2.
Mean scores for two Beck scales at baseline, end of treatment, and six month follow up. Scores at end of treatment and six month follow up adjusted for baseline differences with analysis of covariance. Figures are means (SD)
| Outcome measures (No with data) | Intervention group | Treatment as usual group | Difference between means (95% CI) | P value |
|---|---|---|---|---|
| Beck scale for suicidal ideation | ||||
| Baseline (n=119) | 15.9 (9.9) | 14.3 (10.8) | 1.6 (−2.2 to 5.4) | 0.40* |
| End of treatment phase (n=88) | 10.3 (8.6) | 12.4 (9.9) | −2.1 (−5.6 to 1.4) | 0.22† |
| Six month follow up (n=95) | 7.9 (8.6) | 12.8 (10.4) | −4.9 (−8.2 to −1.6) | 0.005† |
| Beck depression inventory | ||||
| Baseline (n=119) | 30.2 (12.2) | 28.5 (11.6) | 1.7 (−2.6 to 6.0) | 0.43* |
| End of treatment phase (n=89) | 21.3 (13.1) | 22.8 (13.3) | −1.4 (−6.2 to 3.4) | 0.55† |
| Six month follow up (n=95) | 18.8 (13.5) | 23.7 (12.6) | −5.0 (−9.7 to −0.3) | 0.037† |
Independent samples t test.
Analysis of covariance.
Satisfaction
Patients who received the intervention were more satisfied with their treatment at the end of therapy (mean (SD) satisfaction scores 6.56 (3.42) v 4.40 (3.08), 95% confidence interval for difference in means 0.73 to 3.58, P=0.003, t test) and at six month follow up (5.46 (3.38) v 3.89 (2.76), 0.31 to 2.83, P=0.015).
Further episodes of self harm
Twenty nine patients harmed themselves again during the study period. Twenty one patients reported doing so without seeking hospital treatment, and six reported attending hospital. We found data on two further patients on the computerised database. At six month follow up five patients (9%) in the intervention group had harmed themselves again compared with 17 patients (28%) in the usual treatment group (P=0.009, Fisher's exact test, difference in proportion 19.3%, 8.6% to 30.0%). There were no successful suicide attempts in either group during the follow up period.
Resource utilisation
During the treatment phase of the study the two groups were similar in terms of contact with psychiatrists, but patients in the intervention group had more contact with a psychiatric nurse than those in the usual treatment group (mean number (range) of contacts 2 (1-4) v 0.16 (0-3)). Table 3 shows health service contacts for the six months after the intervention.
Table 3.
Number of health service contacts in 46 patients allocated to intervention and 48 patients allocated to usual treatment between end of treatment phase and six month follow up
| Type of contact | Intervention
|
Treatment as usual
|
P value for difference* | |||
|---|---|---|---|---|---|---|
| Mean (SD) | Median (range) | Mean (SD) | Median (range) | |||
| Inpatient | 0.2 (0.62) | 0 (0-3) | 0.35 (1.7) | 0 (0-12) | 0.86 | |
| Outpatient | 1.0 (2.6) | 0 (0-13) | 0.5 (1.3) | 0 (0-5) | 0.30 | |
| Accident and emergency | 0.52 (0.78) | 0 (0-3) | 0.4 (0.76) | 0 (0-3) | 0.31 | |
| Other mental health professionals | 4.0 (11.5) | 0 (0-72) | 3.1 (8.1) | 0 (0-43) | 0.93 | |
| General practitioner | 4.7 (5.9) | 2 (0-27) | 4.7 (5.9) | 3 (0-26) | 0.91 | |
Mann-Whitney U test.
Discussion
Inpatients who poison themselves deliberately we have shown that suicidal ideation and self reported self harm were reduced after brief psychological intervention. Patients who received the therapy also reported higher levels of satisfaction with their treatment. There was no evidence from the data on use of health services that the intervention resulted in a reduction in such use. Our previous research suggests that a more intensive therapeutic intervention may be required to effect such a change.13
Methodological considerations
We made no attempt to control for the non-specific effects of psychotherapy in this study as the trial was a pragmatic one. We aimed to compare a specific intervention with the usual treatment in the United Kingdom for patients who harm themselves.20 Effects of treatment may have resulted from non-specific factors, such as increased contact with nurses for patients in the intervention group. However, previous studies that have involved a similar or greater intensity of clinical contact have failed to show benefit on several outcomes,21,22 and psychodynamic interpersonal therapy has already been found to be superior to a psychological placebo in other patient groups.23
Our inclusion criteria may have resulted in the exclusion of people who were at somewhat higher risk of suicidal behaviour in the future. However, such patients might be unlikely to engage in treatment in any case. Only half of the eligible participants agreed to participate, but our recruitment rate is comparable with that in previous studies21,22 and reflects the difficulty of engaging such patients in intervention programmes. The participants in this study had high levels of psychological morbidity compared with other patients who poison themselves.1,5,21 Our results may therefore not be generalisable to other groups of people who poison themselves but may have less severe psychological problems. Nevertheless, the effectiveness of a low intensity intervention in this group of patients is encouraging.
The data regarding further episodes of self harm should be interpreted cautiously as they are based on reports from the patients themselves. This allowed us to include 21 episodes in the patients who had not attended hospital, an outcome which has been relatively neglected in research to date. This finding may be affected by reporting or interpretation bias, though episodes were included only if they met a standardised definition.8
Possible explanations for treatment effects
Why has the current study shown clear treatment effects, in contrast with previous research? The intervention in the current study focused specifically on interpersonal problems, which are an important antecedent of many episodes of self harm.7 Our sample included a high proportion of patients with a history of self harm, who may particularly benefit from psychological treatments.6 Lastly, our measure of repetition included episodes of self harm when the patient did not present to hospital.
Conclusion
These results are promising, but larger studies of interpersonal psychotherapies in different settings are needed to establish the potential costs and benefits of such treatments for patients who poison themselves. Studies comparing psychodynamic interpersonal therapy with placebo treatments and other psychological interventions may help to identify the active components of the therapy. Such research would inform our future approaches to a problem which is both difficult to manage and widespread.
Figure.
Progress of participants through trial
Acknowledgments
We thank the following people for supporting the project: Dr Rosemary Morton, (consultant in accident and emergency medicine), Simon Brown (nursing manager, accident and emergency), Drs David Hughes, Damien Longson, Amanda Poynton, Judy Harrison, Ian Anderson, Andrew Procter, Sarah Davies, and Richard Gater (consultant psychiatrists, community mental health team), and Frank Hanily and Mary Lord (managers in the directorate of psychiatry, community mental health team). We also thank Professor Francis Creed for his comments on the manuscript.
Footnotes
Competing interests: None declared.
Funding: North West Regional Health Authority and the NHS Research and Development Levy.
References
- 1.NHS Centre for Reviews and Dissemination. Deliberate self harm. Effective Health Care. 1998;4:1–12. [Google Scholar]
- 2.Hawton K, Fagg J. Suicide and other causes of death following attempted suicide. Br J Psychiatry. 1988;152:359–366. doi: 10.1192/bjp.152.3.359. [DOI] [PubMed] [Google Scholar]
- 3.Hall DJ, O'Brien F, Stark C, Pelosi A, Smith H. Thirteen-year follow-up of deliberate self-harm, using linked data. Br J Psychiatry. 1998;172:239–242. doi: 10.1192/bjp.172.3.239. [DOI] [PubMed] [Google Scholar]
- 4.Nordentoft M, Breum L, Munck L, Nordestgaard A, Hunding A, Bjaedager P. High mortality by natural and unnatural causes: a 10 year follow up study of patients admitted to a poisoning treatment centre after suicide attempts. BMJ. 1993;306:1637–1641. doi: 10.1136/bmj.306.6893.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kapur N, House A, Creed F, Feldman E, Friedman T, Guthrie E. Management of deliberate self poisoning in adults in four teaching hospitals: descriptive study. BMJ. 1998;316:831–832. doi: 10.1136/bmj.316.7134.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hawton K, Arensman E, Townsend E, Bremner S, Feldman E, Goldney R, et al. Deliberate self harm: systematic review of efficacy of psychosocial and pharmacological treatments in preventing repetition. BMJ. 1998;317:441–447. doi: 10.1136/bmj.317.7156.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bancroft J, Skrimshire A, Casson J, Harvard-Watts O, Reynolds F. People who deliberately poison or injure themselves: their problems and their contacts with helping agencies. Psychol Med. 1977;7:289–303. doi: 10.1017/s0033291700029391. [DOI] [PubMed] [Google Scholar]
- 8.Schmidtke A, Bille-Brahe U, DeLeo D, Kerkhof A, Bjerke T, Crepet P, et al. Attempted suicide in Europe: rates, trends and sociodemographic characteristics of suicide attempters during the period 1989-1992. Results of the WHO/EURO multicentre study on parasuicide. Acta Psychiatr Scand. 1996;935:327–338. doi: 10.1111/j.1600-0447.1996.tb10656.x. [DOI] [PubMed] [Google Scholar]
- 9.Hobson RF. Forms of feeling. London: Tavistock Publications; 1985. [Google Scholar]
- 10.Shapiro DA, Startup MJ. Raters' manual for the Sheffield psychotherapy rating scale. Sheffield: MRC/ESRC Social and Applied Psychology Unit, University of Sheffield; 1990. (Memo No 1154). [Google Scholar]
- 11.Shapiro DA, Barkham M, Rees A, Hardy GE, Reynolds S, Startup M. Effects of treatment duration and severity of depression on the effectiveness of congnitive-behavioral therapy and psychodynamic-interpersonal psychotherapy. J Consult Clin Psychol. 1994;62:522–528. doi: 10.1037/0022-006x.62.3.522. [DOI] [PubMed] [Google Scholar]
- 12.Shapiro DA, Rees A, Barkham M. Effects of treatment duration and severity of depression on the maintenance of gains following congnitive-behavioral therapy and psychodynamic-interpersonal psychotherapy. J Consult Clin Psychol. 1995;63:378–387. doi: 10.1037//0022-006x.63.3.378. [DOI] [PubMed] [Google Scholar]
- 13.Guthrie E, Moorey J, Margison F, Barker H, Palmer S, McGrath G, et al. Cost-effectiveness of brief psychodynamic-interpersonal therapy in high utilizers of psychiatric services. Arch Gen Psychiatry. 1999;56:519–526. doi: 10.1001/archpsyc.56.6.519. [DOI] [PubMed] [Google Scholar]
- 14.Beck AT, Steer RA, Kovacs M, Garrison B. Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry. 1985;142:559–563. doi: 10.1176/ajp.142.5.559. [DOI] [PubMed] [Google Scholar]
- 15.Beck AT, Kovacs M, Weissman A. Assessment of suicide intention: the scale for suicide ideation. J Consult Clin Psychol. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 16.Steer RA, Rissmiller DJ, Ranieri WF, Beck AT. Dimensions of suicidal ideation in psychiatric inpatients. Behav Res Ther. 1993;31:229–236. doi: 10.1016/0005-7967(93)90090-h. [DOI] [PubMed] [Google Scholar]
- 17.Beck AT, Steer RA, Ranieri WF. Scale for suicidal ideation: psychometric properties of a self report version. J Clin Psychol. 1988;44:499–505. doi: 10.1002/1097-4679(198807)44:4<499::aid-jclp2270440404>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 18.Beck AT, Ward CH, Mendelsohn M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 19.Beecham J, Knapp N. Costing psychiatric interventions. In: Thornicroft G, Brewin CR, Wing J, editors. Measuring mental health needs. London: Royal College of Psychiatrists; 1992. pp. 163–183. [Google Scholar]
- 20.Slinn R, King A, Evans J. A national survey of the hospital services for the management of adult deliberate self-harm. Psychiatric Bull. 2001;25:53–55. [Google Scholar]
- 21.Hawton K, McKeown S, Day A, Martin P, O'Connor M, Yule J. Evaluation of out-patient counselling compared with general practitioner care following overdoses. Psychol Med. 1987;17:751–761. doi: 10.1017/s0033291700025988. [DOI] [PubMed] [Google Scholar]
- 22.Van der Sande R, Van Rooijen L, Buskens E, Allart E, Hawton K, Van Der Grafe Y, et al. Intensive in-patient and community intervention versus routine care after attempted suicide. A randomized intervention study. Br J Psychiatry. 1997;171:35–41. doi: 10.1192/bjp.171.1.35. [DOI] [PubMed] [Google Scholar]
- 23.Guthrie E, Creed F, Dawson D, Tomenson B. A controlled trial of psychological treatment for the irritable bowel syndrome. Gastroenterology. 1991;100:450–457. doi: 10.1016/0016-5085(91)90215-7. [DOI] [PubMed] [Google Scholar]