Abstract
Background
Simultaneous resistance to aminoglycosides and fluoroquinolones in carbapeneme non-susceptible (CNS) isolates will inevitably create problems. The present study was performed to characterize the prevalence of the plasmid-mediated quinolone resistance determinants (QRDs) and aminoglycoside resistance determinants (ARDs) among the CNS Enterobacter cloacae (E. cloacae) isolates in a Chinese teaching hospital, and to acquire their molecular epidemiological characteristics.
Methods
The β-lactamases genes (including class A carbapenemase genes blaKPC and blaSME, metallo-β-lactamase genes (MBLs) blaIMP, blaVIM and blaNDM, and extended spectrum β-lactamases (ESBLs),blaCTX-M, blaTEM and blaSHV), QRDs (including qnrA, qnrB, qnrS and aac(6′)-Ib-cr) and ARDs (including aac(6′)-Ib, armA and rmtB) of these 35 isolates were determined by PCR and sequenced bidirectionally. The clonal relatedness was investigated by pulsed-field gel electrophoresis (PFGE).
Results
Of the 35 isolates, 9 (25.7%) harbored a carbapenemase gene; 23 (65.7%) carried ESBLs; 24 (68.6%) were QRD positive; and 27 (77.1%) were ARD positive. Among the 5 blaIMP-8 positive strains, 4 (80%) contained both ESBL and QRD genes, and all the 5 (100%) harbored ARD genes. Of the 23 ESBLs positive isolates, 6 (26.1%) were carbapenemase positive, 14 (60.9%) were QRD positive, and 18 (78.3%) were ARD positive. PFGE revealed genetic diversity among the 35 isolates, indicating that the high prevalence of CNS E. cloacae isolates was not caused by clonal dissemination.
Conclusion
QRD and ARD genes were highly prevalent among the CNS E. cloacae isolates. Multiple resistant genes were co-expressed in the same isolates. The CNS E. cloacae isolate co-expressing blaNDM-1, blaIMP-26, qnrA1 and qnrS1 was first reported.
Introduction
Enterobacter cloacae (E. cloacae) has recently emerged as an important hospital pathogen [1]. Increasingly reported extended-spectrum β-lactamases (ESBLs) and carbapenemases in E. cloacae represent an emerging public health concern [2]. The vast majority of ESBLs belong to the TEM-, SHV- and CTX-M-type enzymes [3]. Since ESBL-producing bacteria are often multidrug resistant (MDR), carbapenems represent one of the therapeutic options of last resort for life-threatening infections due to these organisms [4]. Although several mechanisms of carbapenem resistance have been reported, most of the mechanisms are related to the spread of plasmid-mediated acquired carbapenemases belonging to Ambler class A (KPCs) and class B (VIMs, IMPs, and NDM-1) β-lactamases [5]. These enzymes compromise the clinical efficacy of almost the whole armamentarium of antimicrobial drugs, leaving clinicians with only a limited number of “last-line” agents such as colistin [6]. Detection of infected patients and carriers with carbapenemase producers is therefore becoming a major health issue to prevent their spread [5].
Of note, the ESBLs and carbapenemases are often encoded by genes located on large plasmids and these also carry genes for resistance to other antimicrobial agents such as aminoglycosides [7], [8] and fluoroquinolones [8], [9]. Thus, very broad antibiotic resistance extending to multiple antibiotic classes is now a frequent characteristic of ESBL- and/or carbapenemase-producing enterobacterial isolates [1], [10].
Quinolone resistance may be conferred by plasmid-mediated quinolone resistance (PMQR) determinants, including the qnr genes, qnrA, qnrB and qnrS [11], and the recently identified aac(6′)-Ib-cr [12]. Although the PMQR determine relatively small increases in the MICs of quinolones, these changes are sufficient to facilitate the selection of mutants with higher levels of resistance [13], and the penetration of PMQR into the population of Enterobacter spp. were found to be coincided with a rapid increase in fluoroquinolone resistance [14]. More importantly, they were shown to be associated with other resistance elements, for instance, qnr genes were found to be co-carried with various ESBLs genes on the same plasmid [15], as well as with metallo-β-lactamase (MBLs) genes [16] and the class A carbapenemase gene blaKPC [17].
Aminoglycosides are an important class of antimicrobial agents for the treatment of life-threatening bacterial infections. Several mechanisms for aminoglycoside resistance have been described previously, with bacterial expression of drug-metabolizing enzymes, such as the clinically widespread aminoglycoside N-6'-acetyltransferase-Ib (AAC(6')-Ib) being the most common mechanism of resistance to aminoglycoside antibiotics, especially in Gram-negative clinical isolates [18]. Moreover, 16S rRNA methyltransferases, such as ArmA and RmtB, are especially troublesome due to their wide target range and their ability to confer high levels of resistance [19]. Of note, they were shown to be associated with other resistance elements. For instance, 16S RNA methylase genes have been demonstrated to be co-expressed with various ESBLs [20] and carbapenemases genes such as blaNDM-1 [21], blaIMP [22] and blaKPC-2 [23] on the same plasmid.
Of concern, both PMAR and PMQR genes are not yet being taken into account in resistance screening by clinical microbiology laboratories. However, on the other hand, analysis of the drug resistance profiles of the recent carbapenem-non-susceptible (CNS) E. cloacae isolates from our hospital showed that most of the CNS E. cloacae strains (32/35, 91.4%) were resistant to both fluoroquinolones (CIP and LEV) and aminoglycosides (GM, TOB and AK) according to the 2012 CLSI breakpoints. Simultaneous resistance to quinolone and aminoglycosides in CNS isolates will inevitably create problems, as many carbapenemase producers may carry unrelated drug-resistance genes such as the quinolone resistance determinants (QRDs) and aminoglycoside resistance determinants (ARDs), and selection pressure with structurally unrelated antibacterial drugs (for instance, aminoglycosides and fluoroquinolone) may contribute to their spread. Thus, the present study was initiated to explore the prevalence of PMQR and PMAR Determinants among the 35 CNS E. cloacae isolates collected from Sep 2009 to Feb 2012 in our hospital. ESBL genes, carbapenemase genes, QRD genes and ARD genes of the CNS E. cloacae isolates were detected to observe the complex genotypes, and all of the strains were characterized by antibiotic resistance phenotyping and pulsed-field gel electrophoresis (PFGE) to understand whether the strains were epidemiologically related.
Materials and Methods
Bacterial Isolates
Between September 2009 and February 2012, 986 clinical isolates of E. cloacae, as identified by VITEK2 compact and API system (bioMerieux, Hazelwood, MO, France) were isolated in our laboratory, 35 (3.55%) of which were non-susceptible to ertapenem (ETP) or imipenem (IMP) according to the 2012 MIC interpretive criteria recommended by the Clinical and Laboratory Standards Institute (CLSI).
Antimicrobial Susceptibility Test
MICs of ceftazidime (CAZ), ceftriaxone (CRO), cefepime (FEP), imipenem (IMP), ertapenem (ETP), gentamycin (GM), tobramycin (TOB), amikacin (AK), ciprofloxacin (CIP) and levofloxacin (LEV) were determined for all isolates using a microbroth dilution method and interpreted based on the 2012 MIC interpretive criteria recommended by the CLSI.
Detection and Sequencing of β-lactamases, ARD and QRD Genes
All the 35 E. cloacae isolates with reduced susceptibility to imipenem (MIC≥2 µg/ml) or ertapenem (MIC≥1 µg/ml) were defined as CNS isolates, which were than PCR screened using custom primers (Table 1) targeting β-lactamases genes, QRD and ARD genes. PCR amplicons were sequenced for both strands by Invitrogen (Invitrogen, Shanghai), and sequences were analyzed.
Table 1. PCR primers for β-lactams, quinolinones and aminoglycosides resistance genes.
| Genes | Primers | Sequences (5′-3′)’) | Amplicon length(bp) |
| blaKPC | F | ATGTCACTGTATCGCCGTCT | 892 |
| R | TTTTCAGAGCCTTACTGCCC | ||
| blaSME | F | AACGGCTTCATTTTTGTTTAG | 820 |
| R | GCTTCCGCAATAGTTTTATCA | ||
| blaVIM | F | TTATGGAGCAGCAACGATGT | 920 |
| R | CAAAAGTCCCGCTCCAACGA | ||
| blaIMP | F | CATGGTTTGGTGGTTCTTGT | 488 |
| R | ATAATTTGGCGGACTTTGGC | ||
| blaNDM-1 | 1-F | CAGCACACT TCCTATCTC | 292 |
| 1-R | CCGCAACCATCCCCTCTT | ||
| 2-F | GGCGGAATGGCTCATCACGA | 287 | |
| 2-R | CGCAACACAGCCTGACTTTC | ||
| blaTEM | F | GTGCGCGGAACCCCTATT | 919 |
| R | TTACCAATGCTTAATCAGTGAGGC | ||
| blaSHV | F | CTTTACTCGCCTTTATCGGC | 1031 |
| R | TTACCGACCGGCATCTTTCC | ||
| blaCTX-M-3′ | F | AATCACTGCGCCAGTTCACGCT | 479 |
| R | GAACGTTTCGTCTCCCAGCTGT | ||
| blaCTX-M-14′ | F | TACCGCAGATAATACGCAGGTG | 355 |
| R | CAGCGTAGGTTCAGTGCGATCC | ||
| qnrA | F | ATTTCTCACGCCAGGATTTG | 413 |
| R | GAGATTGGCATTGCTCCAGT | ||
| qnrB | F | GATCGTGAAAGCCAGAAAGG | 469 |
| R | ACGATGCCTGGTAGTTGTCC | ||
| qnrS | F | GCAAGTTCATTGAACAGGGT | 428 |
| R | TCTAAACCGTCGAGTTCGGCG | ||
| aac(6′)-Ib-cr | F | ATATGCGGATCCAATGAGCAACGCAAAAACAAAGTTAG | 544 |
| R | ATAGCGAATTCTTAGGCATCACTG CGTGTTCGCTC | ||
| aac(6′)-Ib | F | TATGAGTGGCTAAATCGAT | 395 |
| R | CCCGCTTTCTCGTAGCA | ||
| armA | F | CCGAAATGACAGTTCCTATC | 846 |
| R | GAAAATGAGTGCCTTGGAGG | ||
| rmtB | F | ATGAACATCAACGATGCCCT | 769 |
| R | CCTTCTGATTGGCTTATCCA | ||
| IntI 1 | F | GGTCAAGGATCTGGATTTCG | 480 |
| R | ACATGCGTGTAAATCATCGTC |
Conjugation Experiment and Antimicrobial Susceptibility Test by VITEK2 Compact System
Conjugation transfer assay was performed in broth culture with E. coli EC600 as the recipient. Donor and recipient cells were mixed at a ratio of 1∶1. Transconjugants were selected on MacConkey agar containing ampicillin (100 mg/L) supplemented with rifampicin (1500 mg/L; Sigma Chemical Co.). The colonies grown on the selecting medium were selected, identified and tested for antimicrobial susceptibility by the VITEK2 compact system (bioMerieux, Hazelwood, MO, France).
Transformation Experiment and Antimicrobial Susceptibility Test by VITEK2 Compact System
Plasmid DNAs isolated from the clinical No. 35 E. Cloacae strain were transformed by electroporation into E. Coli DH5Θ (Invitrogen, Auckland, New Zealand). The possible NDM-producing transformants were selected on Luria–Bertani agar supplemented with ampicillin (100 mg/L). The colonies grown on the selecting medium were selected, identified and tested for antimicrobial susceptibility by the VITEK2 compact system (bioMerieux, Hazelwood, MO, France).
Plasmid Analysis
Plasmid DNAs isolated from the clinical No. 35 E. Cloacae strain (donor strain), E. coli EC600, representative transconjugant, E. Coli DH5Θ and representative transformant were obtained by the alkaline lysis method and were used as a template in PCR analyses with primers that are specific for qnrA1, qnrS1, AAC(6′)-Ib, AAC(6′)-Ib-cr, bla DNM-1 and bla IMP-26. The PCR products were purified and sequenced twice on both strands by Invitrogen (Invitrogen, Shanghai).
PFGE Fingerprinting
Chromosomal DNA was digested with Xba I and subjected to pulsed-field gel electrophoresis (PFGE) as previously reported [24]. A lambda ladder (Bio-Rad, France) was used as the molecular weight marker. DNA macro restriction patterns were analyzed by visual inspection, based on the criteria of relatedness proposed by Tenover [25].
Results
Prevalence of the QRD Genes and their Associations with Carbapenemases and ESBLs Production
The qnrA, qnrB, qnrS and aac(6′)-Ib-cr genes were detected in 4 (11.4%), 8 (22.9%), 13 (37.1%) and 14(15.3%) of the isolates, respectively, including 2 with qnrA1, 2 with qnrA2, 2 with qnrB2, 6 with qnrB6, and 13 with qnrS1. The prevalence of any QRD genes was 68.6% (24/35).
The qnrA, qnrB, qnrS and aac(6′)-Ib-cr genes and any QRD genes were detected in 13.0% (3/23), 30.4% (7/23), 26.1% (6/23), 30.4% (7/23) and 60.9% (14/23) of the ESBL positive isolates, respectively. Interestingly, 10 of the 24 QRD positive isolates (41.7%) expressed the blaTEM-6 gene.
Among the 9 carbapenemase-producers, 2 (22.2%) qnrA-positive, 4 (44.4%) qnrB-positive, 2 (22.2%) qnrS-positive, 3 (33.3%) aac(6′)-Ib-cr-positive, and 5 (55.5%) any QRD-positive strains were observed. Notably, while all the 3 blaKPC-2 positive strains were shown not to express any QRD genes, 4 of the 5 blaIMP-8 positive isolates (80.0%) expressed one or more QRD genes, and the only one strain co-expressing the blaIMP-26 and blaNDM-1 MBL genes was demonstrated to co-harbor qnrA1, qnrS1 and aac(6′)-Ib-cr.
Moreover, the prevalence rates of QRDs among ESBL and carbapenemase co-producers and both of them non-producers were 66.7% (4/6) and 100.0% (9/9), respectively. Of note, only one was found in the ESBL- and carbapenemase+ group (Table 2).
Table 2. Relevant phenotypic and genotypic characteristics of the 35 carbapeneme non-susceptible (CNS) Enterobacter cloacae (E. cloacae) strains.
| No. | MIC(mg/ml) | Drug resistance profiles | detection of resistance genes | PFGE pattern | ||||
| IMP | ETP | Carbape-nemase | ESBL | QRD | ARD | |||
| 1 | 2 | 16 | CRO, CAZ, FEP, CIP, LEV, AK | blaIMP-8 | - | - | aac(6‘) -Ib | A1 |
| 2 | 2 | 16 | CRO, CAZ, FEP, CIP,LEV, GM, TOB, AK | blaIMP-8 | blaTEM-6 | qnrB6 | aac(6‘) -Ib | A2 |
| 3 | 2 | 16 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | blaIMP-8 | blaTEM-6, blaCTX-M- | qnrB6, aac(6′)-Ib-cr | aac(6‘) -Ib | A1 |
| 4 | 0.25 | 4 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | blaTEM-6 | - | armA, aac(6‘) -Ib | E1 |
| 5 | 2 | 16 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | blaIMP-8 | blaTEM-6 | qnrB6 | aac(6‘) -Ib | A2 |
| 6 | 0.25 | 4 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | blaTEM-6 | qnrA2 | - | K |
| 7 | 8 | 8 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | - | qnrS1 | aac(6‘)-Ib | F |
| 8 | 8 | 2 | CRO, CAZ, FEP, GM, TOB, AK | blaIMP-8 | blaTEM-6, blaSHV-12,blaCTX-M-14 | qnrA2, qnrB6, qnrS1, aac(6′)-Ib-cr | rmtB, aac(6‘) -Ib | G |
| 9 | 1 | 16 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | blaTEM-6, blaSHV-12,blaCTX-M-3 | aac(6′)-Ib-cr, qnrS1 | armA | B1 |
| 10 | 1 | 16 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | blaTEM-6, blaSHV-12,blaCTX-M-3 | aac(6′)-Ib-cr | armA | B1 |
| 11 | 0.25 | 4 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | blaTEM-6, blaCTX-M-3,blaCTX-M-14 | - | armA | C2 |
| 12 | 0.25 | 4 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | blaTEM-6, blaCTX-M-3,blaCTX-M-14 | aac(6′)-Ib-cr | armA, aac(6‘) -Ib | C1 |
| 13 | 0.25 | 4 | CRO, CAZ, FEP | - | - | aac(6′)-Ib-cr | - | J |
| 14 | 0.25 | 2 | CRO, CAZ, FEP, CIP, LEV, GM, TOB | - | blaTEM-6, blaSHV-12,blaCTX-M-3 | - | aac(6′) -Ib | I |
| 15 | 8 | 8 | CRO, CAZ, FEP | - | - | aac(6′)-Ib-cr | - | H |
| 16 | 0.25 | 4 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | blaTEM-6, blaCTX-M-3 | qnrB6, aac(6′)-Ib-cr | armA | D2 |
| 17 | 0.25 | 4 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | blaTEM-6, blaCTX-M-3 | qnrB6, qnrS1 | armA | D1 |
| 18 | 1 | 16 | CRO, CAZ, CIP, LEV, GM, TOB | - | blaSHV-12 | - | - | B2 |
| 19 | 0.25 | 2 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | - | aac(6′)-Ib-cr | armA, aac(6‘) -Ib | E2 |
| 20 | 2 | 16 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | - | qnrS1, aac(6′)-Ib-cr | armA, aac(6‘) -Ib | E3 |
| 21 | 0.25 | 2 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | blaSHV-12 | qnrS1 | aac(6‘) -Ib | E1 |
| 22 | 2 | 16 | CRO, CAZ, FEP, CIP, LEV, GM, TOB, AK | - | - | qnrS1, aac(6′)-Ib-cr | armA, aac(6‘) -Ib | E3 |
| 23 | 16 | 16 | CRO, FEP, CAZ, CIP, LEV, GM, TOB | - | blaSHV-12 | - | - | L1 |
| 24 | 64 | 32 | CRO, FEP, CAZ, CIP, LEV, GM, TOB | blaKPC-2 | blaSHV-12 | - | - | L2 |
| 25 | 32 | 32 | CRO, FEP, CAZ, CIP, LEV, GM, TOB, AK | blaKPC-2 | blaSHV-12, blaCTX-M-14 | - | aac(6‘) -Ib | L1 |
| 26 | 2 | 16 | CRO, FEP, CAZ, CIP, LEV, GM, TOB, AK | - | blaCTX-M-14 | qnrA1 | - | O |
| 27 | 32 | 16 | CRO, FEP, CAZ, CIP, LEV, GM, TOB | blaKPC-2 | - | - | - | N |
| 28 | 0.5 | 8 | CRO, FEP, CAZ, CIP, LEV, GM, TOB, AK | - | blaCTX-M-14 | - | armA | P |
| 29 | 0.125 | 4 | CRO, FEP, CAZ, CIP, LEV, GM, TOB, AK | - | blaCTX-M-14 | qnrB2, qnrS1 | armA, aac(6‘) -Ib | ND* |
| 30 | 0.25 | 4 | CRO, FEP, CAZ, CIP, LEV, GM, TOB, AK | - | - | qnrB2, qnrS1 | aac(6′) -Ib | ND* |
| 31 | 0.25 | 4 | CRO, FEP, CAZ, CIP, LEV, GM, TOB | - | blaCTX-M-14 | - | aac(6′) -Ib | M |
| 32 | 0.125 | 4 | CRO, FEP, CAZ, CIP, LEV | - | blaCTX-M-3 | qnrS1, aac(6′)-Ib-cr | aac(6′) -Ib | Q |
| 33 | 4 | 8 | CRO, CAZ, CIP, LEV, GM, TOB, AK | - | - | qnrS1 | aac(6‘) -Ib | E3 |
| 34 | 0.125 | 1 | CRO, FEP, CAZ, CIP,LEV, GM, TOB, AK | - | - | qnrS1, aac(6′)-Ib-cr | aac(6‘) -Ib | E2 |
| 35 | 64 | 32 | CRO, FEP, CAZ, CIP, LEV, GM,TOB | blaNDM-1, blaMP-26 | - | qnrA1, qnrS1, aac(6′)-Ib-cr | aac(6‘) -Ib | O |
ND: not determined.
Prevalence of the ARD Genes and their Associations with Carbapenemases and ESBLs Production
The aac(6′)-Ib, armA and rmtB genes were detected in 21 (60.0%), 12 (34.3%), and 1 (2.9%) of the 35 isolates, respectively. Since 6 isolates carried both aac(6′)-Ib and armA, one isolate carried both aac(6′)-Ib and rmtB, the prevalence of any ARD genes was 27 (87.1%) of all isolates. The aac(6′)-Ib, armA and rmtB genes were detected in 52.2% (12/23), 39.1% (9/23), and 4.3% (1/23) of the ESBLs positive isolates, respectively. Of note, 17 (63.0%) strains of the 27 ARD positive isolates expressed blaTEM-6 or blaCTX-M-like genes.
Interestingly, while only 1 of the 3 blaKPC-2 positive strains was shown to express the aac(6′)-Ib gene, all the 5 blaIMP-8 positive isolates (100.0%) expressed the aac(6′)-Ib gene, and the only one strain co-expressing the blaIMP-26 and blaNDM-1 MBL genes was also demonstrated to harbor the aac(6′)-Ib gene, that is to say, 7 carbapenemase positive strains co-expressed the aac(6′)-Ib gene.
Moreover, the prevalence rates of ARD among ESBL and carbapenemase co-producers and both of them non-producers were 83.3% (5/6) and 77.8% (7/9), respectively. Notably, most of the ESBL+ and carbapenemase- strains (13/17, 76.5%) were shown to be ARD-positive (Table 2).
Plasmid Analysis
Firstly, using E. coli EC600 (rifampicin resistant) as the recipient, a conjugation experiment was performed to investigate whether the drug resistance genes identified in the clinical No. 35 E. Cloacae strain were located on plasmids and whether the transfer of these genes contributed to the reduced susceptibility of the recipient E. coli EC600 towards antibiotics. The transconjugants showed a multidrug resistance phenotype that included resistance to ampicillin, ampicillin/sulbactam, piperacillin/tazobactam, cefazolin, cefotetan, ceftazidime, ceftriaxone, ertapenem, imipenem and ciprofloxacin, intermediate susceptible to cefepime and levofloxacin. However, all the transconjugants were susceptible to aztreonam, amikacin, gentamicin and tobramycin (Table 3). For the β-lactam antibiotics or β-lactam/β-lactamase inhibitor combinations, the transconjugants showed ≥2-, 8-, 32-, 16-, 16-, 64-, 64-, 16-, 16- and 16-fold increases in the MICs of ampicillin, ampicillin/sulbactam, piperacillin/tazobactam, cefazolin, cefotetan, ceftriaxone, ceftazidime,cefepime, ertapenem and imipenem, respectively, when compared with the recipient E. coli EC600 strain. For quinolone antibiotics, the transconjugants showed ≥16- and 8-fold increases in the MICs of ciprofloxacin and levofloxacin, respectively, when compared with the recipient strain. With regard to the MICs of aztreonam, amikacin, gentamicin, and tobramycin, they showed no increases. More notably, eight transconjugants were randomly chosen and detected to harbour qnrA1, qnrS1, aac(6′)-Ib-cr, bla DNM-1 and bla IMP-26 simultaneously, while aac(6′)-Ib was not detected in all the transconjugants (Table 4).
Table 3. MICs of antibiotics for the clinical No. 35 E. Cloacae strain (donor strain), E. coli EC600, representative transconjugant, E. Coli DH5? and representative transformant.
| antibiotics | MIC (µg/ml) | ||||
| EC No.35 | EC600 | Transconjugant* | DH5? | Transformant* | |
| AMP | ≥32 | 16 | ≥32 | ≤2 | ≥32 |
| AMS | ≥32/16 | 4/2 | ≥32/16 | ≤2/1 | ≥32/16 |
| PTZ | ≥128/4 | ≤4/0.125 | ≥128/4 | ≤4/0.125 | 64/2 |
| CFZ | ≥64 | ≤4 | ≥64 | ≤4 | ≥64 |
| CTT | ≥64 | ≤4 | ≥64 | ≤4 | 32 |
| CRO | ≥64 | ≤1 | ≥64 | ≤1 | ≥64 |
| CAZ | ≥64 | ≤1 | ≥64 | ≤1 | ≥64 |
| FEP | ≥64 | ≤1 | 16 | ≤1 | 8 |
| AZT | ≥64 | ≤1 | ≤1 | ≤1 | ≤1 |
| IMP | ≥16 | ≤1 | ≥16 | ≤1 | ≥16 |
| ETP | ≥8 | ≤0.5 | ≥8 | ≤0.5 | ≥8 |
| CIP | ≥4 | ≤0.25 | ≥4 | ≤0.25 | 0.5 |
| LEV | ≥8 | 0.5 | 4 | ≤0.25 | 1 |
| GM | ≥16 | ≤1 | ≤1 | ≤1 | ≤1 |
| TOB | 8 | ≤1 | ≤1 | ≤1 | ≤1 |
| AK | ≤2 | ≤2 | ≤2 | ≤2 | ≤2 |
Eight representative transconjugants and transformants were respectively collected for antibiotic susceptibility test by the AST GN-13 card, and the representative results were shown.
Abbreviations used: ampicillin (AMP), ampicillin/sulbactam (AMS), piperacillin/tazobactam (PTZ), cefazolin (CFZ), cefotetan (CTT), ceftazidime (CAZ), ceftriaxone (CRO), cefepime (FEP), aztreonam (AZT), ertapenem (ETP), imipenem (IMP), ciprofloxacin (CIP), levofloxacin (LEV), amikacin (AK), gentamicin (GM), tobramycin (TOB).
Table 4. Drug resistance genes detected from the clinical No. 35 E. Cloacae strain (donor strain), E. coli EC600, transconjugants, E. Coli DH5? and transformants using their plasmids as PCR templates.
| Genes | Stains | ||||
| EC No.35 | EC600 | transconjugant | DH5? | transformant | |
| bla IMP-26 | • | • | • | ||
| bla DNM-1 | • | • | • | ||
| qnrA1 | • | • | |||
| qnrS1 | • | • | • | ||
| AAC(6′)-Ib | • | • | |||
| AAC(6′)-Ib-cr | • | ||||
•denotes positive.
Secondly, using E. coli DH5Θ as the recipient, a transformation experiment was performed to further investigate whether these genes were located on plasmids and whether the transfer of these genes contributed to the reduced susceptibility of the recipient E. coli DH5Θ towards antibiotics. The E. Coli DH5Θ transformants showed resistance to ampicillin/inhibitor combinations, broad-spectrum cephalosporins and carbapenems (Table 3). Similar to those of the transconjugants, all the transformants were also susceptible to aztreonam, amikacin, gentamicin, and tobramycin. However, on the other hand, although the transformants were still susceptible to ciprofloxacin and levofloxacin, they showed ≥2- and 4-fold increases in the MICs of ciprofloxacin and levofloxacin, respectively, when compared with the recipient E. Coli DH5Θ strain. More notably, transformation assays allowed to transfer the qnrS1, bla DNM-1 and bla IMP-26 gene simultaneously in all the transformants tested (Table 4).
Molecular Epidemiology
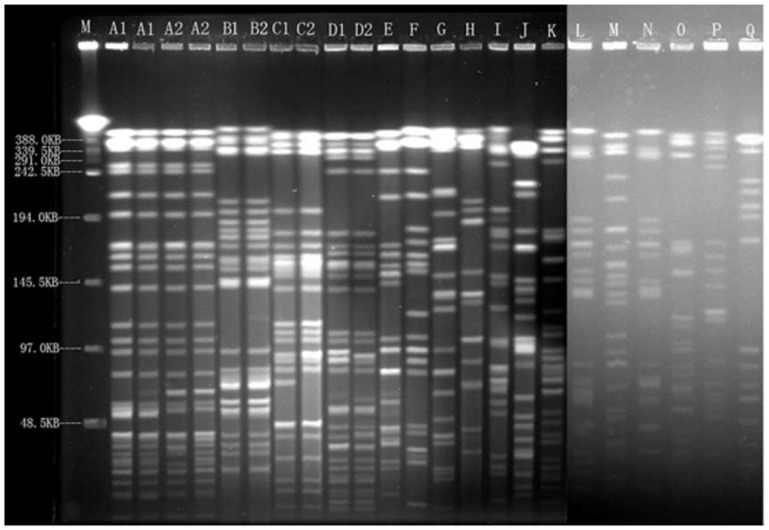
Seventeen Xba I patterns, named A to Q, were found among the 35 E. cloacae isolates. Between Sep 2009 and Feb 2011, the major epidemic pattern A comprised of 4 isolates genetically related to subtypes A1 and A2. All of the pattern A isolates were blaIMP-8 positive and were all collected from different wards. However, the fifth blaIMP-8 positive isolate, identified nine months after the fourth IMP-8 producer was isolated, was collected in another ward and was found to be totally different from pattern A and were grouped into pattern G. The isolates collected from Sep 2011 to Feb 2012 were categorized into eight clusters. The major epidemic pattern E comprised of 6 isolates genetically related to subtypes E1, E2 and E3 (Figure 1 and Table 2). These data indicate that the high prevalence of CNS E. cloacae isolates was not caused by clonal dissemination.
Figure 1. PFGE patterns of 35 CNS E. cloacae isolates.
PFGE fingerprinting was performed according to the “methods” section. Chromosomal DNA restriction patterns were interpreted by the Tenover's criteria. M: Lambda DNA Ladder; A1-Q: representative isolates with different genotype from A to Q.
Discussion
In the present study, the prevalence of the PMQRs and PMARs among the 35 CNS E. cloacae isolates in a Chinese teaching hospital was characterized and their molecular epidemiological characteristics were also achieved. Of the 35 isolates, 9 harbored carbapenemase genes, 23 carried ESBLs, 24 were QRD positive and 27 were ARD-producers. Among the 5 blaIMP-8 positive strains, 4 contained QRD genes, and 5 harbored ARD genes. Among the 23 ESBLs positive isolates, 14 were QRD positive and 18 were ARD positive. Molecular typing by PFGE revealed genetic diversity among the 35 isolates, indicating that the CNS E. cloacae isolates were epidemiologically unrelated. Of note, multiple resistant genes were found to be co-expressed in the same CNS E. cloacae isolates.
The increasing frequency of quinolone resistance in Enterobacteriaceae was associated with an increasing prevalence of PMQR genes, and this change involved an increase in the diversity of the PMQR genes and also an increase in the prevalence of the mutations in gyrA, parC, or both in PMQR-positive strains but not PMQR-negative strains [26]. The present study demonstrated high prevalence (24/35, 68.6%) of QRDs among CNS E. cloacae isolates in a Chinese teaching hospital. The association of QRD with blaIMP-8 or ESBLs should be investigated further.
Three common plasmid-borne qnr genes, qnrA, qnrB and qnrS were detected, with qnrS (37.1%, 13/35) being the most common among the three. Moreover, the low rates of qnrA have been observed in most surveillance studies [16], while in some countries, qnrA were more common [27]. Interestingly, isolate 8 co-carrying qnrA2, qnrB6, qnrS1 and aac(6′)-Ib-cr, was found to be sensitive to both CIP and LEV. Qnr determinants alone may not confer resistance to quinolones, but they can supplement other quinolone resistance mechanisms. In our study, one isolate (isolate 8) carrying qnrA2, qnrB6, aac(6′)-Ib-cr and qnrS1 and 2 isolates (isolate 13 and 15) harboring aac(6′)-Ib-cr were classified as Ciprofloxacin (CIP) and levofloxacin (LEV) susceptible by CLSI 2012 criteria. Thus, treatment with a fluoroquinolone might easily select for resistant strains, and it will be interesting to find out whether the existence of the qnr genes is sufficient to facilitate the selection of mutants with higher levels of quinolone resistance. Most importantly, this is the first report of the co-expression of qnrA1 and qnrS1 with blaDNM-1 and blaIMP-26 carbapenemases in E. cloacae.
Many carbapenemase-producing Enterobacteriaceae are highly multiresistant, but may remain susceptible to one or more aminoglycosides [28]. In the present study, 11 (31.4%) strains were found to be sensitive to at least one of the aminoglycosides tested. Three common ARD genes, aac(6′)-Ib, armA and rmtB were detected, with aac(6′)-Ib being the most common (60.0%, 21/35) among the three. The extremely high prevalence (27/35, 77.1%) of ARD among CNS E. Cloacae in our hospital may be due mainly to the intrahospital spread of a few clones and the dissemination of plasmids containing both aac(6′)-Ib or armA and ESBLs, presumably by means of transposons, insertion sequences or recombination. The semisynthetic aminoglycoside amikacin (AK) is very useful in the treatment of multiresistant infections because only a limited number of modifying enzymes, such as AAC(6′)-I-type acetyltransferases, are able to inactivate it. Unfortunately, the rise in multiresistant strains harboring aac(6′)-Ib has seriously limited the successful use of aminoglycosides including AK [29]. Notably, although all the 3 bla KPC-2 positive carbapenem-resistant E. cloacae strains included in this study were found not to carry any QRDs, and only one showed the co-expression of one kind of ARD, aac(6′)-Ib, they were shown to be resistant to both quinolones (CIP and LEV) and aminoglycosides (GM and TOB), and notably, the only one co-harboring blaKPC-2 and aac(6′)-Ib demonstrated to be resistant to GM, TOB and AK, while the other two without aac(6′)-Ib were AK-susceptible.
The emergence and spread of carbapenem-resistant Enterobacteriaceae in the world are a major concern. Q Wu et al. [30] demonstrated 5 isolates of E. cloacae from Shanghai, China, that were resistant to all clinically available antimicrobial agents co-expressing blaKPC-2, blaSHV-12, blaCTX-M-14 and armA 16S rRNA methylase. We reported for the first time an E. cloacae strain co-harboring blaKPC-2, blaSHV-12, blaCTX-M-14 and aac(6′)-Ib that was also resistant to all clinically available antimicrobial agents from Chongqing.
To our knowledge, this is the first description of the coexistence of the qnrA1, qnrS1, aac(6′)-Ib, aac(6′)-Ib-cr, bla DNM-1 and bla IMP-26 resistance genes in one enterobacterial strain. The association of these resistance determinants is worrisome, because it may facilitate the selection of high-level multidrug-resistant strains in some communities and this process may be promoted by the co-selection of various antimicrobial agents under subinhibitory concentrations. There is a great need to obtain more detailed knowledge on the association of various resistance genes in enterobacterial strain, and more studies should be carried out in this field. We suggest that an effective surveillance and strict infection control strategies should be implemented soon to prevent potential outbreaks of nosocomial infections by such pathogens in China.
In conclusion, QRD and ARD genes were highly prevalent among the CNS E. cloacae isolates, and multiple resistant genes were co-expressed in the same isolates. Most importantly, the CIP- and LEV-susceptible CNS E. cloacae isolate co-expressing blaIMP-8, blaTEM-6, blaSHV-12, blaCTX-M-14, qnrA2, qnrB6, qnrS1, aac(6′)-Ib-cr, rmtB and aac(6′)-Ib and the CNS E. cloacae isolate co-expressing qnrA1, qnrS1, AAC(6′)-Ib, AAC(6′)-Ib-cr, bla DNM-1 and bla IMP-26 were first reported to the best of our knowledge. Southern blot experiments are currently underway to reveal the the possible co-existence of blaNDM-1, blaIMP-26 and qnrS1 on the same transferred plasmid in the clinical No. 35 E. Cloacae strain.
Acknowledgments
We thank the staffs in the Center for Hospital Infection Control, Daping hospital, Research Insititute of surgery, Third Military Medical University, Chongqing, China, for the help in the PFGE work. Especially, we appreciate professor Ding Liu and technician Zheng Wang for the very useful advice.
Funding Statement
This work was supported in part by the National Science Foundation of China (Grant No. 81071621 and No.30973378; http://www.nsfc.gov.cn/Portal0/default152.htm). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Yang FC, Yan JJ, Hung KH, Wu JJ (2012) Characterization of Ertapenem-resistant Enterobacter cloacae in a Taiwanese University Hospital. J Clin Microbiol 50: 223–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bush K (2010) Alarming β-lactamase-mediated resistance in multidrug-resistant Enterobacteriaceae . Curr Opin Microbiol 13: 558–564. [DOI] [PubMed] [Google Scholar]
- 3. Paterson DL, Bonomo RA (2005) Extended-spectrum β-lactamases: a clinical update. Clin Microbiol Rev 18: 657–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cornaglia G, Giamarellou H, Rossolini GM (2011) Metallo-β-lactamases: a last frontier for β-lactams? Lancet Infect Dis11: 381–393. [DOI] [PubMed] [Google Scholar]
- 5. Miriagou V, Cornaglia G, Edelstein M, Galani I, Giske CG, et al. (2010) Acquired carbapenemases in Gram-negative bacterial pathogens: detection and surveillance issues. Clin Microbiol Infect 16: 112–122. [DOI] [PubMed] [Google Scholar]
- 6. Naas T, Cuzon G, Bogaerts P, Glupczynski Y, Nordmann P (2011) Evaluation of a DNA Microarray (Check-MDR CT102) for Rapid Detection of TEM, SHV, and CTX-M Extended-Spectrum β-Lactamases and of KPC, OXA-48, VIM, IMP, and NDM-1 Carbapenemases. J Clin Microbiol 49: 1608–1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paterson DL (2000) Recommendation for treatment of severe infections caused by Enterobacteriaceae producing extended-spectrum β-lactamases (ESBLs). Clin Microbiol Infect 6: 460–463. [DOI] [PubMed] [Google Scholar]
- 8. Patrick MG, Jun H, Robert JC, Yu Y, Yoon IK, et al. (2012) Complete Sequence of a Novel 178-Kilobase Plasmid Carrying blaNDM-1 in a Providencia stuartii Strain Isolated in Afghanistan. Antimicrob Agents Chemother 56: 1673–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mammeri H, Van De Loo M, Poirel L, Martinez-Martinez L, Nordmann P (2005) Emergence of plasmid-mediated quinolone resistance in Escherichia coli in Europe. Antimicrob Agents Chemother 49: 71–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Johann D-DP, Patrice N, Kevin BL, Laurent P (2005) Emergence of Enterobacteriaceae producing extended-spectrum β-lactamases (ESBLs) in the community. Antimicrob Chemother 56: 52–59. [DOI] [PubMed] [Google Scholar]
- 11. Strahilevitz J, Jacoby GA, Hooper DC, Robicsek A (2009) Plasmid-Mediated Quinolone Resistance: a Multifaceted Threat. Clin Microbiol Rev 22: 664–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Robicsek A, Strahilevitz J, Jacoby GA, Macielag M, Abbanat D, et al. (2006) Fluoroquinolone-modifying enzyme: a new adaptation of a common aminoglycoside acetyltransferase. Nat Med 12: 83–88. [DOI] [PubMed] [Google Scholar]
- 13. Cano LM-M, Pascual A (2007) Mutant prevention concentrations of fluoroquinolones for Enterobacteriaceae expressing the plasmid-carried quinolone resistance determinant qnrA1 . Antimicrob Agents Chemother 51: 2236–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Strahilevitz J, Engelstein D, Adler A, Temper V, Moses AE, et al. (2007) Changes in qnr prevalence and fluoroquinolone resistance in clinical isolates of Klebsiella pneumoniae and Enterobacter spp. collected from 1990 to 2005. Antimicrob Agents Chemother 51: 3001–3003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Robicsek A, Jacoby GA, Hooper DC (2006) The worldwide emergence of plasmid-mediated quinolone resistance. Lancet Infect Dis 6: 629–640. [DOI] [PubMed] [Google Scholar]
- 16. Wu JJ, Ko WC, Tsai SH, Yan JJ (2007) Prevalence of plasmid-mediated quinolone resistance determinants QnrA, QnrB, and QnrS among clinical isolates of Enterobacter cloacae in a Taiwanese hospital. Antimicrob Agents Chemother 51: 1223–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chmelnitsky I, Navon-Venezia S, Strahilevitz J, Carmeli Y (2008) Plasmid-Mediated qnrB2 and Carbapenemase Gene bla KPC-2 Carried on the Same Plasmid in Carbapenem-Resistant Ciprofloxacin-Susceptible Enterobacter cloacae Isolates. Antimicrob Agents Chemother 52: 2962–2965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. O'Neill AJ (2008) New antibacterial agents for treating infections caused by multi-drug resistant Gram-negative bacteria. Expert Opin Investig Drugs 17: 297–302. [DOI] [PubMed] [Google Scholar]
- 19. Folster JP, Rickert R, Barzilay EJ, Whichard JM (2009) Identification of the Aminoglycoside Resistance Determinants armA and rmtC among Non-Typhi Salmonella Isolates from Humans in the United States. Antimicrob Agents Chemother 53: 4563–4564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ma L, Lin CJ, Chen JH, Fung CP, Chang FY, et al. (2009) Widespread Dissemination of Aminoglycoside Resistance Genes armA and rmtB in Klebsiella pneumoniae Isolates in Taiwan Producing CTX-M-Type Extended-Spectrum β-Lactamases. Antimicrob Agents Chemother 53: 104–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Poirel L, Dortet L, Bernabeu, Nordmann P (2011) Genetic Features of bla NDM-1-Positive Enterobacteriaceae . Antimicrob Agents Chemother 55: 5403–5407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liu Y, Zhang B, Cao Q, Huang WC, Shen LS, et al. (2009) Two Clinical Strains of Klebsiella pneumoniae Carrying Plasmid-Borne blaIMP-4, blaSHV-12, and armA Isolated at a Pediatric Center in Shanghai, China. Antimicrob Agents Chemother 53: 1642–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zacharczuk K, Piekarska K, Szych J, Zawidzka E, Sulikowska A, et al. (2011) Emergence of Klebsiella pneumoniae Coproducing KPC-2 and 16S rRNA Methylase ArmA in Poland. Antimicrob Agents Chemother 55: 443–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yang H, Chen H, Yang Q, Chen M, Wang H (2008) High prevalence of plasmid-mediated quinolone resistance genes qnr and aac(6′)-Ib-cr in clinical isolates of Enterobacteriaceae from nine teaching hospitals in China. Antimicrob Agents Chemother 52: 4268–4273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, et al. (1995) Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 33: 2233–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kim HB, Park CH, Kim CJ, Kim EC, Jacoby GA, et al. (2009) Prevalence of Plasmid-Mediated Quinolone Resistance Determinants over a 9-Year Period. Antimicrob Agents Chemother 53: 639–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Robicsek A, Strahilevitz J, Sahm DF, Jacoby GA, Hooper DC (2006) qnr Prevalence in Ceftazidime-Resistant Enterobacteriaceae Isolates from the United States. Antimicrob Agents Chemother 50: 2872–2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Livermore DM, Mushtaq S, Warner M, Zhang JC, Maharjan S, et al. (2011) Activity of aminoglycosides, including ACHN-490, against carbapenem-resistant Enterobacteriaceae isolates. J Antimicrob Chemother 66: 48–53. [DOI] [PubMed] [Google Scholar]
- 29. Vakulenko SB, Mobashery S (2003) Versatility of aminoglycosides and prospects for their future. Clin Microbiol Rev 16: 430–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wu Q, Liu Q, Han L, Sun J, Ni Y (2010) Plasmid-mediated carbapenem-hydrolyzing enzyme KPC-2 and ArmA 16S rRNA methylase conferring high-level aminoglycoside resistance in carbapenem-resistant Enterobacter cloacae in China. Diagn Microbiol Infect Dis 66: 326–328. [DOI] [PubMed] [Google Scholar]