Abstract
Background
Non-exercise algorithms are cost-effective methods to estimate cardiorespiratory fitness (CRF) in healthcare settings. The limitation of current non-exercise models is that they were developed with cross-sectional data.
Purpose
To extend the non-exercise research by developing algorithms for men and women using longitudinal data on indicators available in healthcare settings.
Methods
The sample included 1325 women (aged 20–78 years) and 10,040 men (aged 20–86 years) who completed from two to 21 maximal treadmill tests between 1977 and 2005. The data were analyzed in 2011 and 2012. The dependent variable was CRF measured by treadmill test. The independent variables were age, body composition (percentage fat or BMI); waist circumference, self-reported physical activity; resting heart rate; and smoking behavior.
Results
Linear mixed-models regression showed that all variables were independently related to CRF. There was a positive association between CRF and physical activity. Higher levels of body composition were linked to lower CRF. High resting heart rate and smoking resulted in lower estimates of CRF. The error estimates of the percentage fat algorithms were: women, 1.41 METs (95% CI=1.35, 1.47); and men, METs 1.54 (95% CI=1.51, 1.55). The BMI models were somewhat less accurate: women, METs 1.51 (95% CI=1.45, 1.58); and men, 1.66 METs (95% CI=1.63, 1.68).
Conclusions
These results showed that the CRF of women and men can be estimated from easily obtained health indicators. The longitudinal non-exercise algorithms provide models to accurately estimate CRF changes associated with aging and provide cost-effective algorithms to track CRF over time with health indicators available in healthcare settings.
Introduction
Low cardiorespiratory fitness (CRF) is associated with increased risk of cardiovascular disease, type 2 diabetes and all-cause mortality.1–12 Unlike other important risk factors, CRF is not routinely measured in most healthcare or fitness settings. Measuring CRF requires trained personnel to administer a maximal or submaximal exercise test using specialized equipment. The most valid measure of CRF is a maximal exercise test with oxygen consumption measured by indirect calorimetry. A common alternative is a submaximal test in which maximal oxygen uptake (VO2max) is estimated from heart rate response to submaximal exercise.13,14 With the publication of non-exercise algorithms, it is now feasible to estimate CRF without administering an exercise test.15–24
The non-exercise method estimates CRF using health indicators typically available in healthcare settings. The variables used include age and gender in combination with body composition, and self-reported physical activity. The concurrent validity correlations for the first published non-exercise equations17 ranged from 0.78 to 0.81 and the SEs of estimate (SEE) ranged from 1.51 to 1.60 METs (5.3 to 5.6 ml/kg/minute). The non-exercise estimates were found to be more accurate than commonly used submaximal CRF estimates of maximal capacity.13 Post hoc analysis revealed that the non-exercise models accurately estimated the CRF of individuals who had a positive exercise electrocardiogram (ECG) or were taking hypertension medication. Several investigators15–24 have published non-exercise algorithms.
The advantage of the non-exercise method is that it makes it possible to estimate a patient’s CRF with reasonable accuracy using health indicators commonly available in field and healthcare settings. Published non-exercise algorithms have two limitations. First, the non-exercise algorithms were developed with cross-sectional data. Although non-exercise cross-sectional models provide accurate estimates at the population level, the accuracy of the cross-sectional models to estimate CRF changes is not known. Second, age was included as a linear term in the cross-sectional models and recent longitudinal data25,26 demonstrated that CRF declines at a nonlinearly with aging. In the current study, these two limitations were addressed. The purpose was to develop longitudinal non-exercise algorithms for men and women that estimated CRF changes associated with aging.
Methods
Study Population
The sample included 1325 women and 10,040 men who completed at least two comprehensive medical examinations at the Cooper Clinic in Dallas TX between 1977 and 2005. The women ranged in age from 20 years to 78 years and the men from 20 years to 86 years. The women completed 2–14 tests (M=2.9) for a total of 3816 observations; and 25% completed three or more tests, and 5% did six or more. The men completed 2–21 tests (M=3.9) for a total of 38,716 observations; 25% of the men completed four or more tests, and 5% did nine or more. All participants had normal resting or exercising ECGs, a BMI ≥18.5, and were able to reach 85% of their age-predicted maximal heart rate during the exercise tests. Those who reported a history of myocardial infarction, stroke, or cancer were excluded. Patients with physician-diagnosed diabetes or those who used insulin were also excluded. The patients were relatively healthy women and men.
Participants came to the clinic for periodic preventive health examinations and for counseling regarding diet, exercise, and other lifestyle factors associated with increased risk of chronic diseases. Participants were unpaid volunteers and were not recruited to the study. Many were sent by their employers for the examination, some were referred by their physicians, and others were self-referred. Participants were predominantly white, well-educated, and of middle and upper SES; all had access to health care.
Because individuals were excluded if they had major chronic diseases, failed to achieve at least 85% of their estimated maximal heart rate on the treadmill test, or had abnormal exercise tests, the study population was healthier than the general population. Participants signed an informed consent for the clinical examinations and follow-up, and the study was reviewed, approved and had ethical approval from the IRB of the Cooper Institute. A detailed description of the Aerobics Center Longitudinal Study (ACLS) cohort with multiple tests is provided in other sources.8,25
Clinical Examinations
The clinical examinations were completed after an overnight fast of at least 12 hours and included a physician examination, clinical evaluations such as blood chemistry analyses and blood pressure measurements, questionnaires on personal health history and smoking behavior, and a maximal treadmill exercise test. Smoking status (current smoker or not), and physical activity habits were obtained from a standardized questionnaire. Height and weight were measured on a physician’s scale and stadiometer. BMI was computed by standard formula from measured height and weight. Waist circumference was measured level with the umbilicus. Percentage fat was measured by either hydrostatic weighing27 or skinfold thickness28,29; 22% of women and 49% of men had hydrostatic data. The method used to measure percentage fat is described in detail elsewhere.30
Cardiorespiratory fitness was quantified as the duration of a symptom-limited maximal treadmill exercise test using a modified Balke protocol.31 Patients were encouraged to give maximal effort, and the test endpoint was volitional exhaustion or termination by the physician for medical reasons. The mean (±SD) percentage of age-predicted maximal heart rate achieved during exercise was 103.6% (±6.5%). The speed and elevation of the final minute of the treadmill test was used to convert treadmill performance to METs using the American College of Sports Medicine (ACSM) equation.32 Exercise treadmill duration on this protocol with adults is highly correlated (r ≥0.92) with measured peak oxygen uptake.33,34
Self-reported aerobic exercise (physical activity) was assessed with a five-level physical activity index (PAI) based on patient response to questions in the medical history questionnaire about their regular physical activity habits during the past 3 months.35,36 If participation in an activity was reported, the patient was asked to provide additional information about the type of activity, number of times per week, duration of each exercise session, and distance or time spent in the activity. Table 1 provides the ACLS criteria used to define the individual’s PAI. Walking and jogging were chosen as the basis for the PAI used herein because it was the most common activity for this population. The PAI data were treated as a categoric variable; the referent category was PAI 0: “no regular activity.”
Table 1.
Criteria for defining level of physical activity for the previous 30 days
| Physical activity index | Five-level physical activity criteria | Two-level physical activity criteria | |
|---|---|---|---|
| 0 | No regular activity | 0 | Inactive |
| 1 | Other: Participated in some other regular physical activity such as bicycling, swimming, racquet sports, and other strenuous sports, but not walking or jogging | ||
| 2 | Low: Walked or jogged <10 miles per week | ||
| 3 | Moderate: Walked or jogged 10–20 miles per week | 1 | Active |
| 4 | High: Walked or jogged >20 miles per week |
The five-level model was used to develop a second physical activity variable defined as inactive and active. Active was walking or jogging ≥10 miles per week.37,38 The referent for the two-level model was “inactive.” The guide for the inactive and active criteria was the DHHS consensus exercise recommendation of “at least 150 minutes of moderate-intensity aerobic activity (i.e., brisk walking) every week.38 Assuming that individuals walked at a rate of 3.3 mph, walking or jogging ≥10 miles per week represents aerobic exercise of ≥200 minutes per week. The active category is slightly higher than the DHHS consensus recommendation of “at least 150 minutes of moderate-intensity aerobic activity (i.e., brisk walking) every week.”
Statistical Analyses
Linear mixed-models (LMM) regression using a random longitudinal growth model was used to analyze the data.39,40 Stata 12 xtmixed program was used for all LMM analyses, which were completed in 2012. The dependent variable was CRF scaled in METs. The independent variables were age, age,2 body composition, physical activity, resting heart rate, and smoking behavior.
Combinations of independent variables were used to develop four gender-specific prediction models. The models included percentage fat or BMI and either the five-level or two-level physical activity variables in combination with the other independent variables. Each regression coefficient was tested with a z-statistic to determine if it was different from 0. Only variables with regression weights significantly greater than 0 were included in the model. The accuracy of the non-exercise models was defined by the SEE for the fixed model, which was computed as the square root of the sum of the random intercept and residual variances.39–41
Results
Table 2 provides the descriptive statistics for the women and men at their first test (baseline) and for all tests (total observations). Ages ranged from 20 years to 78 years for women and from 20 years to 86 years for men. The data exhibited the well-documented gender differences in body composition and CRF. The mean CRF of men was about 20% higher than that for women, and the mean percentage fat of women was about 6% higher than that for men. The total observations in Table 2 showed that 25% of women and 31% of men walked or jogged ≥10 miles per week. The percentage of men who reported that they currently smoked was 11.3% compared to 6% for women.
Table 2.
Descriptive statistics of women and men for baseline and all observations, M (SD) unless otherwise noted
| Variable | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline (n=1325) | Total observations (n=3816) | Baseline (n=10,040) | Total observations (n=38,716) | |||||
| Age, years | 44.4 (9.2) | 47.8 | 9.7 | 43.8 | 9.0 | 48.2 | 9.7 | |
| Height, cm | 164.4 | 5.9 | 164.3 | 5.9 | 179.2 | 6.4 | 179.0 | 6.4 |
| Weight, kg | 60.9 | 9.3 | 60.9 | 9.1 | 82.8 | 11.7 | 82.3 | 11.4 |
| BMI | 22.5 | 3.2 | 22.6 | 3.1 | 25.8 | 3.1 | 25.7 | 3.1 |
| Waist circumference, cm | 71.5 | 8.5 | 71.6 | 9.0 | 92.0 | 9.4 | 91.9 | 9.1 |
| Percentage fat, % | 26.4 | 6.2 | 26.0 | 6.1 | 20.5 | 5.8 | 20.5 | 5.6 |
| Resting heart rate, bpm | 62.9 | 10.2 | 61.8 | 10.1 | 58.5 | 10.3 | 56.9 | 9.8 |
| Maximal heart rate, bpm | 177.3 | 12.2 | 176.0 | 12.6 | 179.5 | 12.3 | 177.0 | 12.6 |
| Treadmill time, minutes | 14.6 | 4.2 | 14.9 | 4.2 | 19.6 | 4.5 | 20.2 | 4.5 |
| CRF (METs) | 10.1 | 1.9 | 10.2 | 1.9 | 12.4 | 2.3 | 12.7 | 2.3 |
| Physical activity index | ||||||||
| 0 | 16.2 | 19.4 | 18.8 | 17.8 | ||||
| 1 | 26.7 | 25.7 | 22.5 | 22.1 | ||||
| 2 | 33.7 | 29.6 | 32.5 | 29.2 | ||||
| 3 | 16.0 | 18.4 | 17.0 | 20.8 | ||||
| 4 | 7.4 | 7.0 | 9.2 | 10.1 | ||||
| Active, % | 23.4 | 25.3 | 26.1 | 30.9 | ||||
| Current smoker, % | 7.8 | 6.0 | 14.8 | 11.3 | ||||
CRF, cardiorespiratory fitness
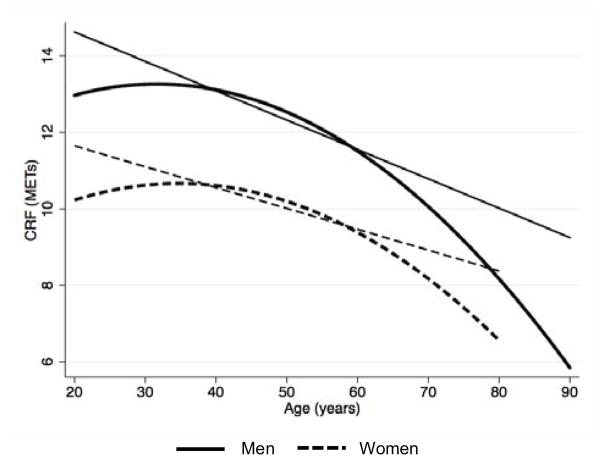
The first step was to examine and define the linearity of longitudinal change in CRF with aging. Figure 1 provides the linear and quadratic LMM age-CRF regression lines for women and men. The analyses found that the relationship was not linear but quadratic (p<0.001). Figure 1 shows that at about age 45 years, CRF of both women and men started to decline, and the trajectory of change accelerated with aging. After about age 60 years, the linear model systematically underestimated the quadratic trend, and this bias increased with aging.
Figure 1.
The linear and quadratic LMM regression lines for women and men
Note: The linear model defined the yearly decline in CRF at −0.0545/year for women and for men, −0.0767/year. The LMM quadratic models are: women, CRF=8.2475 + (age × 0.1391) − (age2 × 0.0020); and men, CRF=11.0850 + (age × 0.1378) − (age2 × 0.0022).
Tables 3 and 4 provide the women and men’s longitudinal non-exercise algorithms and the SEE (95% CI). Provided are four, gender-specific prediction models that include percentage fat or BMI and either the five-level or two-level physical activity variables in combination with waist circumference, resting heart rate, and smoking behavior. All regression coefficients were significant (p<0.001).
Table 3.
Longitudinal algorithms for estimating maximal CRF (METs) for women
| Model | Women’s equations | SE estimate (95% CI) |
|---|---|---|
|
Percentage fat Five-level |
CRF(METs) = 13.4967 + (Age × 0.1200) − (Age2 × 0.0017) − (%fat × 0.0817) − (WC × 0.0140) − (RHR × 0.0342) + (PAI-1 × 0.2402) + (PAI-2 × 0.2735) + (PAI-3 × 0.7432) + (PAI-4 × 1.0346) − (CS × 0.3207) | 1.41 (1.35, 1.47) |
| Two-Level | CRF(METs) = 13.7415 + (Age × 0.1223) − (Age2 × 0.0018) − (%fat × 0.0819) − (WC × 0.0141) − (RHR × 0.0349) + (Active × 0.6061) − (CS × 0.3188) | 1.43 (1.37, 1.49) |
|
BMI Five-level |
CRF(METs) = 14.5493 = (Age × 0.1136) − (Age2 × 0.0016) − (BMI × 0.1500) − (WC × 0.0088) − (RHR × 0.0359) + (PAI-1 × 0.2091) + (PAI-2 × 0.2275) + (PAI-3 × 0.7021) + (PAI-4 × 1.0070) − (CS × 0.3005) | 1.51 (1.45, 1.58) |
| Two-level | CRF(METs) = 14.7873 = (Age × 0.1159) − (Age2 × 0.0017) − (BMI × 0.1534) − (WC × 0.0088) − (RHR × 0.0364) + (Active × 0.5987) − (CS × 0.2994) | 1.53 (1.47, 1.59) |
%fat, percentage body fat; CRF, cardiorespiratory fitness; CS, currently smoke; PAI, physical activity index; RHR, resting heart rate; WC, waist circumference
Table 4.
Longitudinal algorithms for estimating maximal CRF (METs) for men
| Model | Men’s Equations | SE estimate (95% CI) |
|---|---|---|
|
%fat Five-level |
CRF(METs) = 17.7357 + (Age × 0.1620) − (Age2 × 0.0021) − (%fat × 0.1057) − (WC × 0.0422) − (RHR × 0.0363) + (PAI-1 × 0.2153) + (PAI-2 × 0.3655) + (PAI-3 × 0.8092) + (PAI-4 × 1.1989) − (CS × 0.4378) | 1.54 (1.51, 1.55) |
| Two-level | CRF(METs) = 18.1395 + (Age × 0.1662) − (Age2 × 0.0022) − (%fat × 0.1077) − (WC × 0.0431) − (RHR × 0.0380) + (Actve × 0.6429) − (CS × 0.4339) | 1.56 (1.54, 1.59) |
|
BMI Five-level |
CRF(METs) = 20.8013 + (Age × 0.1610) − (Age2 × 0.0022) − (BMI × 0.2240) − (WC × 0.0334) − (RHR × 0.0375) + (PAI-1 × 0.2163) + (PAI-2 × 0.3447) + (PAI-3 × 0.7877) + (PAI-4 × 1.1961) − (CS × 0.4306) | 1.66 (1.63, 1.68) |
| Two-level | CRF(METs) = 21.2870 + (Age × 0.1654) − (Age2 × 0.0023) − (BMI × 0.2318) − (WC × 0.0337) − (RHR × 0.0390) + (Active × 0.6351) − (CS × 0.4263) | 1.69 (1.67, 1.72) |
%fat, percentage body fat; CRF, cardiorespiratory fitness; CS, currently smoke; PAI, physical activity index; RHR, resting heart rate; WC, waist circumference
Although the women’s and men’s models exhibited the same general trend, the SEE of women’s models was lower (0.13 METs vs 0.16 METs) than that for the men’s models. There was an inverse relationship between CRF and resting heart rate and body composition. The significant relationship between CRF and the physical activity variables was positive. Each of the physical activity coefficients for the five-level models was different from 0, the referent. The two-level models (inactive, active) were slightly less accurate (≈0.02 METs) than the five-level physical activity models. The most accurate models were those that included percentage fat and the five-level physical activity variables. The SEEs of the percentage fat models were ≈0.10 METs lower than those for the BMI models.
Discussion
These results established that CRF could be estimated by modeling longitudinal health indicators typically measured at fitness and healthcare settings. The error estimates of the algorithms ranged from 1.41 to 1.69 METs, within the range reported with cross-sectional models.15–24 The percentage fat and the five-level physical activity algorithms were more accurate than the BMI models, but BMI has greater utility, as percentage fat estimates are often not available in healthcare settings. The error estimates for the BMI models were ≈0.12 METs higher than those for the percentage fat algorithms.
A new finding was that the models that used the two-level, inactive–active scale were nearly as accurate as the five-level physical activity scale. The advantages of the inactive–active scale are that it provides an easier method to estimate physical activity and is consistent with the level of aerobic activity recommended for American adults.38 These longitudinal analyses revealed that waist circumference, resting heart rate, and smoking behavior were predictors of CRF, independent of gender, age, physical activity, and body composition, which are the variables that comprise cross-sectional models.15–24 Because of the well-documented gender differences in body composition28,29 and the large sample sizes, gender-specific longitudinal algorithms were developed. The error estimates for the women’s models were ≈0.13 METs lower than those for the men, which has been reported with cross-sectional models.17,21
An important aspect of this study was the use of serial data and statistical modeling to build the longitudinal algorithms. Cross-sectional algorithms use age and CRF as a linear relationship.15,17,21–23 These longitudinal results are consistent with published data 25, 26 showing that the trend for measured CRF is quadratic, not linear. Figure 1 documents the bias. At age 70 years, the quadratic trend was ≈0.75 METs lower than the linear estimate, and the systematic bias grew to ≈2 METs at age 80 years, and over 3 METs for men aged 85 years. A likely reason for the linearity difference between cross-sectional and longitudinal analyses is that the upper age limit of the cross-sectional subjects was ≤70 years, whereas the age ranges for these ACLS samples were 20–78 years for women and 20–86 years for men.
Although cross-sectional models15–24 provide accurate estimates of CRF at the population level, they do not furnish information concerning the model’s utility to assess changes in CRF. Since the serial tests were the random part of the modeled data, the LMM algorithms give unbiased estimates of changes in CRF with aging. The residuals (measured CRF–estimated CRF) of all models were contrasted by age (Appendix A, available online at www.ajpmonline.org). The bivariate graph documented that slopes of the age by residual regressions lines did not differ from 0 (p>0.05), and the residuals for both the fixed and random models were evenly distributed across the age range studied. An important feature of these longitudinal findings over cross-sectional models15– 24 is that the algorithms can be used to track fitness over time with health indicators commonly available in healthcare settings.
Measured CRF is a strong independent predictor of all-cause and cause-specific mortality in asymptomatic individuals as well as those with existing metabolic or cardiovascular disease.1,2,4,6–8,11,12,36,37,42 Although the relationship between measured CRF and health risk is well documented, the validity of non-exercise CRF to estimate health risk is just starting to evolve. Stamatakis43 reported that non-exercise CRF18 was associated with all-cause and CVD mortality in men and women aged 35–70 years in the United Kingdom. Although research documenting health risk with non-exercise CRF is lacking, there is evidence linking variables that comprise non-exercise algorithms to health risk.
Numerous investigators7–9,44–47 have linked obesity to health risk. Talbot and associates12 examined the associations between self-reported leisure-time physical activity and VO2peak with the risk of coronary events in healthy younger (aged ≤65 years) and older (aged ≥65 years) men. They reported that for younger men, higher CRF, but not physical activity, was associated with a reduced risk of coronary heart disease. In older men, both high-intensity (≥6 METs) leisure-time activity and measured CRF reduced coronary risk. In a longitudinal study of men and women without documented cardiovascular disease (CVD) at baseline, Nauman et al.48 reported that an increase in resting heart rate over 10 years was associated with all-cause and heart-disease mortality. Mailey et al.20 reported that aggregated cardiovascular disease conditions reported by older men and women (aged ≥60 years) were inversely associated with non-exercise estimated fitness.
The major strengths of this study are the use of large samples of women and men with serial data measured across the adult life span and CRF measured with a maximal exercise test. LMM is an ideal method to model longitudinal data because it accommodates unbalanced, unequally spaced observations over time.39,40 Compared to published cross-sectional algorithms,15–24 the advantages of the longitudinal models are that the gender-specific algorithms: (1) account for the quadratic aging trend; (2) provide unbiased estimates of changes in CRF with aging; and (3) included smoking, waist circumference, and resting heart rate as independent variables. To our knowledge, these are the only longitudinal non-exercise models currently available to estimate CRF, and they provide a cost-effective method to track fitness over time.
The ACLS consisted mostly of white patients who were well educated, of middle and upper SES, and had access to health care. Although the overall ACLS cohort is similar to the general population for many risk factors, the multi-visit cohort studied is more fit than the overall ACLS cohort.49 The mean CRF of the overall ACLS cohort, aged 40–49 years, was 8.3 METs for women and 10.9 METs for men,1 about 2 METs lower than for these multi-visit men and women. Lee and associates9 reported that changes in measured CRF were associated with health risk over 11.4 years of follow-up of ACLS men who had at least two medical examinations. To further validate these longitudinal models, research is needed to determine if the algorithms identify health risk when applied to patients who differ in race and have major chronic diseases.
Finally, research is needed to determine if the longitudinal algorithms predict health risk and if changes in non-exercise CRF are associated with health risk.
Table 5 illustrates scenarios that apply the algorithms to estimate CRF from clinical data. It is cumbersome to make these calculations by hand and it is recommended that it be accomplished using computer technology. The scenarios illustrate the basic calculations of the models that differ in body composition, physical activity and gender. Provided next are suggestions designed to integrate the algorithms with existing computer technology.
Table 5.
Illustration of using the algorithms to estimate CRF from routinely collected clinical data
| Men, %fat, five-level | Women, BMI, two-level | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Value | Regular weight | Result | Variable | Value | Regular weight | Result |
| Constant | 17.7357 | Constant | 14.7873 | ||||
| Age | 50.0 | 0.1620 | 8.1 | Age | 40 | 0.1159 | 4.636 |
| Age2 | 2500.0 | −0.0021 | −5.25 | Age2 | 1600 | 0.0017 | −2.72 |
| %fat | 20.0 | −0.1057 | −2.114 | BMI | 24 | 0.1534 | −3.6816 |
| Waist circumference | 92.0 | −0.0422 | −3.8824 | Waist circumference | 70 | 0.0088 | −0.616 |
| Resting HR | 60.0 | −0.0363 | −2.178 | Resting HR | 62 | 0.0364 | −2.2568 |
| PAI-1 | 0 | 0.2153 | 0 | Active Yes | 1 | 0.5987 | 0.5987 |
| PAI-2 | 0 | 0.3655 | 0 | Smoker Yes | 0 | −0.2994 | 0 |
| PAI-3 | 1 | 0.8092 | 0.8092 | Estimated CRF (METs) | 10.7476 | ||
| PAI-4 | 0 | 1.1989 | 0 | ||||
| Smoker yes | 1 | 0.4378 | −0.4378 | ||||
| Estimated CRF (METs) | 2729.7851 | ||||||
Note: Provided is the %fat, five physical activity algorithm for men and the BMI, and two-level algorithm for women. The values for the clinical data were arbitrarily selected. To estimate CRF with a given algorithm, first multiply the patient’s clinical value by the model’s regression weight, and second, sum the obtained results with the algorithm’s constant.
CRF, cardiorespiratory fitness; HR, heart rate; PAI, physical activity index; %fat, percentage fat
Select the equations that are most suitable for a clinical setting.
Develop a computer database to enter and store the clinical variables. Designing software or using commercial database software such as Microsoft Excel can accomplish this.
Program the database to estimate CRF using the selected equation.
Provide a means to put the CRF estimates into a report that can be the focus of individual counseling on current level of fitness, and if serial measures are available, changes in fitness over time.
In summary, the longitudinal non-exercise models are cost-effective algorithms with functions to estimate CRF. The longitudinal prediction models account for the nonlinear age–CRF relationship and provide unbiased estimates of changes in CRF. The longitudinal algorithms provide a cost-effective method to track changes in CRF with health indicators available in fitness and healthcare settings.
Acknowledgments
The authors thank the Cooper Clinic physicians and technicians for collecting the baseline data, and the staff at the Cooper Institute for data entry and data management.
Supported by NIH grants AG06945, HL62508, and R21DK088195; and an unrestricted research grant from the Coca Cola Company.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Blair SN, Kohl HW, 3rd, Paffenbarger RS, Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality: a prospective study of healthy men and women. JAMA. 1989;262:2395–401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- 2.Blair SN, Kampert J, Kohl HW, 3rd, et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA. 1996;276:205–10. [PubMed] [Google Scholar]
- 3.Ekelund LG, Haskell WL, Johnson JL, Whaley FS, Criqui MH, Sheps DS. Physical fitness as a predictor of cardiovascular mortality in asymptomatic North American men: the Lipid Research Clinic’s mortality follow-up study. N Engl J Med. 1988;319:1379–84. doi: 10.1056/NEJM198811243192104. [DOI] [PubMed] [Google Scholar]
- 4.Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301:2024–35. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 5.Lakka TA, Vemalainen JM, Rauramaa R, Salonen R, Tuomilehto J, Salonen JT. Relation of leisure-time physical activity and cardiorespiratory fitness to the risk of acute myocardial infarction in men. N Engl J Med. 1994;330:1549–54. doi: 10.1056/NEJM199406023302201. [DOI] [PubMed] [Google Scholar]
- 6.Laukkanen JA, Kurl S, Salonen R, Rauramaa R, Salonen JT. The predictive value of cardiorespiratory fitness for cardiovascular events in men with various risk profiles: a prospective population-based cohort study. Eur Heart J. 2004;25:1428–37. doi: 10.1016/j.ehj.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 7.Lee CD, Blair SN, Jackson AS. Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men. Am J Clin Nutr. 1999;69:373–80. doi: 10.1093/ajcn/69.3.373. [DOI] [PubMed] [Google Scholar]
- 8.Lee DC, Artero EG, Lee IM, et al. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the aerobics center longitudinal study. Circulation. 2011;124(23):2483–90. doi: 10.1161/CIRCULATIONAHA.111.038422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee DC, Sui X, Church TS, Lavie CJ, Jackson AS, Blair SN. Changes in Fitness and Fatness on the Development of Cardiovascular Disease Risk Factors. J Am Coll Cardiol. 2012;59:665–72. doi: 10.1016/j.jacc.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lynch J, Helmrich SP, Lakka TA, et al. Moderately intense physical activities and high levels of cardiorespiratory fitness reduce the risk of non–insulin-dependent diabetes mellitus in middle-aged men. Arch Intern Med. 1996;156:1307–14. [PubMed] [Google Scholar]
- 11.Meyers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 12.Talbot LA, Morrell CH, Metter EJ, Fleg JL. Comparison of cardiorespiratory fitness versus leisure time physical activity as predictors of coronary events in men aged < or = 65 years and > 65 years. Am J Cardiol. 2002;89:1187–92. doi: 10.1016/s0002-9149(02)02302-0. [DOI] [PubMed] [Google Scholar]
- 13.Åstrand P-O, Ryhming I. A nomogram for calculation of aerobic capacity (physical fitness) from pulse rate during submaximal work. J Appl Physiol. 1954;7:218–21. doi: 10.1152/jappl.1954.7.2.218. [DOI] [PubMed] [Google Scholar]
- 14.Baumgartner TA, Jackson AS, Mahar MT, Rowe DA. Measurement for Evaluation in Physical Education and Exercise Science. 8. New York: McGraw-Hill; 2007. [Google Scholar]
- 15.George JD, Stone WJ, Burkett LN. Non-exercise VO2max estimation for physically active college students. Med Sci Sports Exerc. 1997;29:415–23. doi: 10.1097/00005768-199703000-00019. [DOI] [PubMed] [Google Scholar]
- 16.Heil DP, Freedson PS, Ahlquist LE, Price J, Rippe JM. Non-exercise regression models to estimate peak oxygen consumption. Med Sci Sports Exerc. 1995;27:599–606. [PubMed] [Google Scholar]
- 17.Jackson AS, Blair SN, Mahar MT, Wier LT, Ross RM, Stuteville JE. Prediction of functional aerobic capacity without exercise testing. Med Sci Sports Exerc. 1990;22:863–70. doi: 10.1249/00005768-199012000-00021. [DOI] [PubMed] [Google Scholar]
- 18.Jurca R, Jackson AS, LaMonte MJ, et al. Assessing cardiorespiratory fitness without performing exercise testing. Am J Prev Med. 2005;29:185–93. doi: 10.1016/j.amepre.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Matthews CE, Heil DP, Freedson PS, Pastides H. Classification of cardiorespiratory fitness without exercise testing. Med Sci Sports Exerc. 1999;31:486–9. doi: 10.1097/00005768-199903000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Mailey EL, White SM, Wojcicki TR, Szabo AN, Kramer AF, McAuley E. Construct validation of a non-exercise measure of cardiorespiratory fitness in older adults. BMC Public Health. 2010;10:59. doi: 10.1186/1471-2458-10-59. Published online 2010 Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nes BM, Janszky I, Vatten LJ, Nilsen TI, Aspenes ST, Wisløff U. Estimating VO2peak from a Non-Exercise Prediction Model; the HUNT Study, Norway. Med Sci Sports Exerc. 2011 Apr 14; doi: 10.1249/MSS.0b013e31821d3f6f. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Suminski RR, Weir LT, Poston W, Arenare B, Randles A, Jackson AS. The effect of habitual smoking on measured and predicted VO2(max) J Phys Act Health. 2009;6:667–73. doi: 10.1123/jpah.6.5.667. [DOI] [PubMed] [Google Scholar]
- 23.Wier LT, Jackson AS, Ayers GW, Arenare B. Noneexercise models for estimating VO2max with waist girth, percent fat or BMI. Med Sci Sports Exerc. 2006;238:555–561. doi: 10.1249/01.mss.0000193561.64152. [DOI] [PubMed] [Google Scholar]
- 24.Williford HN, Scjarff-Olson M, Wang N, Blessing DL, Smith FH, Duey WJ. Cross-validation of non-exercise predictions of VO2peak in women. Med Sci Sports Exerc. 1996;28:926–30. doi: 10.1097/00005768-199607000-00022. [DOI] [PubMed] [Google Scholar]
- 25.Fleg JL, Morrell CH, Bos AG, et al. Accelerated longitudinal decline of aerobic capacity in healthy older adults. Circulation. 2005;112:674–82. doi: 10.1161/CIRCULATIONAHA.105.545459. [DOI] [PubMed] [Google Scholar]
- 26.Jackson AS, Sui X, Hébert JR, Church TS, Blair SN. Role of Lifestyle and Aging on the Longitudinal Change in Cardiorespiratory Fitness. Arch Intern Med. 2009;169:1781–7. doi: 10.1001/archinternmed.2009.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Going SB. Chapter 2 Densitometry. In: Heymsfield SB, Lohnman TG, Wang Z, Going SB, editors. Human Body Composition. 2. Champaign: Human Kinetics; 2005. pp. 17–34. [Google Scholar]
- 28.Jackson AS, Pollock ML. Generalized equations for predicting body density of men. Br J Nutr. 1978;40:497–504. doi: 10.1079/bjn19780152. [DOI] [PubMed] [Google Scholar]
- 29.Jackson AS, Pollock ML, Ward A. Generalized equations for predicting body density of women. Med Sci Sports Exerc. 1980;12:175–82. [PubMed] [Google Scholar]
- 30.Jackson AS, Janssen I, Sui X, Church TS, Blair SN. Longitudinal changes in body composition associated with healthy ageing: men, aged 20–96 years. Br J Nutr. 2011;107:1085–91. doi: 10.1017/S0007114511003886. [DOI] [PubMed] [Google Scholar]
- 31.Balke B. A simple field test for assessment of physical fitness. Civil Aeromedical Research Report. 1963:63–66. [PubMed] [Google Scholar]
- 32.ACSM. Guidelines for Exercise Testing and Prescription. 6. Philadelphia: Lippincott, Williams and Wilkins; 2000. [Google Scholar]
- 33.Pollock ML, Bohannon RL, Cooper KH, et al. A comparative analysis of four protocols for maximal treadmill stress testing. Am Heart J. 1976;92:39–42. doi: 10.1016/s0002-8703(76)80401-2. [DOI] [PubMed] [Google Scholar]
- 34.Pollock ML, Foster C, Schmidt D, Hellman C, Linnerud AC, Ward A. Comparative analysis of physiologic responses to three different maximal graded exercise test protocols in healthy women. Am Heart J. 1982;103:363–73. doi: 10.1016/0002-8703(82)90275-7. [DOI] [PubMed] [Google Scholar]
- 35.Cheng Y, Macera CA, Davis DR, Ainsworth BE, Troped PJ, Blair SN. Physical activity and self-reported, physician-diagnosed osteoarthritis: is physical activity a risk factor? J Clin Epidemiol. 2000;53:315–22. doi: 10.1016/s0895-4356(99)00168-7. [DOI] [PubMed] [Google Scholar]
- 36.Kampert JB, Blair SN, Barlow CE, Kohl HW., 3rd Physical activity, physical fitness, and all-cause and cancer mortality: a prospective study of men and women. Ann Epidemiol. 1996;5:452–7. doi: 10.1016/s1047-2797(96)00059-2. [DOI] [PubMed] [Google Scholar]
- 37.Lee DC, Sui X, Ortega FB, et al. Comparisons of leisure-time physical activity and cardiorespiratory fitness as predictors of all-cause mortality in men and women. Br J Sports Med. 2011;45(6):504–10. doi: 10.1136/bjsm.2009.066209. [DOI] [PubMed] [Google Scholar]
- 38.DHHS. Physical Activity Guidelines for Americans. 2008 www.health.gov/paguidelines, editor.
- 39.Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. 2. College Station: Stata Press; 2008. [Google Scholar]
- 40.West B, Welch KB, Gatecki AT. Linear Mixed Models. New York: Chapman & Hall/CRC; 2007. [Google Scholar]
- 41.O’Connor DP, Bray MS, McFarlin BK, Sailors MH, Ellis KJ, Jackson AS. Generalized equations for estimating DXA percent fat of diverse young women and men: the TIGER study. Med Sci Sports Exerc. 2010;42:1959–65. doi: 10.1249/MSS.0b013e3181dc2e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sui X, LaMonte MJ, Laditka JN, et al. Cardiorespiratory fitness and adiposity as mortality predictors in older adults. JAMA. 2007;298:2507–16. doi: 10.1001/jama.298.21.2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stamatakis E. Associations between a Non-Exercise Testing Algorithm for Estimating Cardiorespiratory Fitness and All-Cause and CVD Mortality. In: Katzmarzyk PT, editor. 3rd International Congress on Physical Activity and Public Health; Toronto: JPAH, Human Kinetics; 2010. p. 29. [Google Scholar]
- 44.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 45.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298:2028–37. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 46.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289(2):187–93. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 47.Neovius M, Sundstrom J, Rasmussen F. Combined effects of overweight and smoking in late adolescence on subsequent mortality: nationwide cohort study. BMJ. 2009;38:338, b496. doi: 10.1136/bmj.b496. doi:0.1136/bmj.b496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nauman J, Janszky I, Vatten LJ, Wisløff U. Temporal changes in resting heart rate and deaths from ischemic heart disease. JAMA. 2011;306(23):2579–87. doi: 10.1001/jama.2011.1826. [DOI] [PubMed] [Google Scholar]
- 49.Wang CY, Haskell WL, Farrell SW, et al. Cardiorespiratory Fitness Levels among U.S. adults 20–49 years of age: Findings from the 1999–2004 National Health and Nutrition Examination Survey. Am J Epidemiol. 2010;171:426–35. doi: 10.1093/aje/kwp412. [DOI] [PubMed] [Google Scholar]