Abstract
We used a longitudinal twin design to examine the causal association between sexual, emotional, and physical abuse in childhood (before age 18) and borderline personality disorder (BPD) traits at age 24 using a discordant twin design and biometric modeling. Additionally, we examined the mediating and moderating effects of symptoms of childhood externalizing and internalizing disorders on the link between childhood abuse and BPD traits. Although childhood abuse, BPD traits, and internalizing and externalizing symptoms were all correlated, the discordant twin analyses and biometric modeling showed little to no evidence that consistent with a causal effect of childhood abuse on BPD traits. Instead, our results indicate that the association between childhood abuse and BPD traits stems from common genetic influences that, in some cases, also overlap with internalizing and externalizing disorders. These findings are inconsistent with the widely held assumption that childhood abuse causes BPD, and suggests that BPD traits in adulthood are better accounted for by heritable vulnerabilities to internalizing and externalizing disorders.
Borderline personality disorder (BPD) is a severe personality disorder characterized by a pattern of unstable interpersonal relationships, self-image, and affect, as well as impulsivity in a variety of contexts (APA, 2000). Although the prevalence of BPD in the general population is estimated to range from 1% to 5.9% (Grant et al., 2008; Torgersen, Kringlen, & Cramer, 2001), approximately 10% of mental health outpatients and 20% of psychiatric inpatients have a BPD diagnosis (APA, 2000). Additionally, BPD is highly comorbid with both Axis I (Skodol et al., 2002) and Axis II disorders (Zanarini et al., 1998), including major depressive disorder, post-traumatic stress disorder, substance use disorders, and antisocial personality disorder (Skodol et al., 2002; Zanarini et al., 1998). Finally, a large proportion of BPD patients engage in deliberate self-injury and parasuicidal behavior (Shearer, 1994), and 1 in 10 of those with the diagnosis will commit suicide (Paris, 2002). To reduce the burden of this disorder on individuals and society, it is necessary to explore the etiological origins of BPD.
Maladaptive childhood environments such as parental criticism (Cheavens et al., 2005; Crowell, Beauchaine, & Linehan, 2009; Linehan, 1993), witnessing domestic violence (Zanarini, 2000), emotional and physical neglect (Widom, Czaja, & Paris, 2009; Zanarini & Frankenburg, 1997), and sexual, physical, or emotional abuse (Ball & Links, 2009; Beauchaine, Klein, Crowell, Derbidge, & Gatzke-Kopp, 2009; Bornovalova, Gratz, Delany-Brumsey, Paulson, & Lejuez, 2006; Carlson, Egeland, & Sroufe, 2009; Johnson, Cohen, Brown, Smailes, & Bernstein, 1999; Trull, 2001; Zanarini, 2000) have long been considered important etiologic factors in the development of BPD. Childhood abuse (CA) – defined as sexual, physical, or emotional abuse that occurred before the age of 18 (Dinwiddie et al., 2000; Johnson et al., 1999; Nelson et al., 2002; Silverman, Reinherz, & Giaconia, 1996)—has received perhaps the greatest attention in the BPD literature as a potential pathogenic factor. In cross-sectional studies using retrospective reports, 30 to 90% of BPD patients report childhood sexual, physical, or emotional abuse (Ball & Links, 2009; Bornovalova et al., 2006; Carlson et al., 2009; Golier et al., 2003; Laporte & Guttman, 1996; Zanarini, 2000). This association has been documented in a variety of samples including psychiatric inpatients (Bradley, Jenei, & Westen, 2005), psychiatric outpatients (Golier et al., 2003), urban drug users (Bornovalova et al., 2006), and community adolescents (Rogosch & Cicchetti, 2005). Additionally, CA shows a dose-response relationship with BPD such that the more severe the abuse, the higher the level of BPD symptoms and overall severity of psychosocial impairment (Sansone, Songer, & Miller, 2005; Silk, Lee, Hill, & Lohr, 1995; Zanarini et al., 2002).
The diathesis-stress model is an alternative to CA having a direct and causal effect on BPD. This model postulates that the temperamental traits of behavioral disinhibition or externalizing [EXT; impulsivity and inability to inhibit undesirable actions (Iacono, Malone, & McGue, 2008)] and negative emotionality or internalizing [INT; predisposition to experience depression, anger, and anxiety, (Watson & Clark, 1984)] serve as pre-existing vulnerabilities, while CA functions as an environmental risk factor (Beauchaine et al., 2009; Cheavens et al., 2005; Crowell et al., 2009; Linehan, 1993; Paris, 2002; Zanarini & Frankenburg, 1997). The underlying INT and EXT vulnerabilities (diathesis) interacting with CA (environmental stressor) then produces BPD traits. Stated otherwise, in a diathesis-stress or interaction model, CA would contribute to BPD traits only in the context of high INT or EXT. Despite some indirect support (Arens, Grabe, Spitzer, & Barnow, 2011; Distel et al., 2011; Wagner, Baskaya, Dahmen, Lieb, & Tadic, 2010; Wagner, Baskaya, Lieb, Dahmen, & Tadic, 2009, 2010), there are no direct tests of the diathesis-stress interaction model.
In both the direct causal and diathesis-stress models, CA is often assumed to have a causal effect on BPD. The association between CA and BPD, however, might be accounted for by common genetic or environmental risk factors (i.e., environmental factors that contribute to similarity among relatives). For instance, the CA-BPD association could be accounted for by parental genotypes contributing to both inherited (e.g., child’s temperament traits) and environmental risk factors (e.g., chaotic home environment, abuse, exposure to domestic violence). Alternatively, it is possible that a child’s inherited characteristics (e.g., disinhibited temperament) elicit reactions from others that then increase exposure to environmental risk factors (e.g., harsh punishment). Both of these scenarios are examples of gene-environment (G-E) correlations (passive and evocative, respectively), also termed genetic mediation. If genetic mediation accounts for the CA-BPD association, then INT and EXT are heritable characteristics that might account for the CA-BPD association. Twin studies have shown that INT, EXT, and CA are each influenced by both genetic and shared environment factors (Bergen, Gardner, & Kendler, 2007; Bornovalova, Hicks, Iacono, & McGue, 2010; Burt, Krueger, McGue, & Iacono, 2001, 2003; Burt, McGue, Krueger, & Iacono, 2005a; Gjone, Stevenson, Sundet, & Eilertsen, 1996; Hicks, Krueger, Iacono, McGue, & Patrick, 2004; Kendler, Prescott, Myers, & Neale, 2003; Schulz-Heik et al., 2010) with heritability being moderate to high for INT and EXT and modest for CA (Jaffee, Caspi, Moffitt, & Taylor, 2004; Lyons et al., 1993; Schulz-Heik et al., 2010; Stein, Jang, Taylor, Vernon, & Livesley, 2002). Research has also demonstrated that genetic mediation can account for the association between childhood EXT and maladaptive parenting practices and abuse (Burt et al., 2003; Burt et al., 2005a; Schulz-Heik et al., 2010), and between adult violence and stress exposure with BPD (Distel et al., 2011). A viable hypothesis then is that genetic mediation rather than a direct causal effect may account for the association between CA and BPD.
Disentangling Causal Effects and Genetic Mediation
Two methods for examining the genetic and environmental influences on the association between CA on BPD are discordant twin design and biometric modeling. Both methods compare the similarity of members of monozygotic (MZ) and dizygotic (DZ) twin pairs. The logic of these designs is that twin similarity is due to additive genetic effects—which are shared completely by MZ twins but only 50% on average by DZ twins—and shared environmental effects (environmental effects that contribute to twin similarity) that are shared equally and completely by both MZ and DZ twins. Environmental exposures experienced by one twin but not the other are called non-shared environmental influences, and contribute to differences between twins. The discordant twin design involves a comparison of members of MZ and DZ twin pairs that differ on the experience of CA, the logic being if the effect of CA on BPD is causal, then members of both MZ and DZ twin pairs discordant for CA are expected to be significantly different on BPD traits. That is, the twin who experienced CA is expected to exhibit more BPD traits than the twin who did not experience CA. If common genetic influences account for the association between CA and BPD, however, MZ twin pairs discordant for CA should exhibit similar levels of BPD traits. For discordant DZ pairs, however, the twin who experienced CA should exhibit more BPD traits than the twin who did not experience CA, because DZ twin pairs provide only partial control for genetic influences. Alternatively, if common shared environment effects account for the association between CA and BPD, then for both MZ and DZ pairs, the twin who experienced CA would not exhibit more BPD traits because both types of twins are equally matched on shared environmental factors (McGue, Osler, & Christensen, 2010).
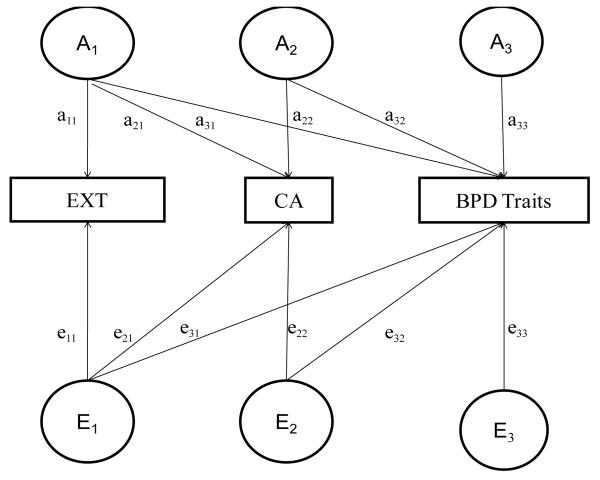
Biometric modeling is a second method to examine the genetic and environmental influences on the association between CA and BPD. This method estimates the amount of overlapping genetic and environmental variance across CA and BPD traits. Evidence consistent with a causal effect of CA on BPD (i.e., an effect of CA on BPD even after controlling for common genetic and shared environmental risk factors) would be significant overlap between the nonshared environmental influences on CA and BPD (nonshared environmental correlation). In contrast, substantial overlap in the genetic influences on CA and BPD would be consistent with genetic mediation. Additionally, biometric modeling provides a method for examining potential genetic mediators such as INT and EXT (Figure 1). Specifically, if childhood INT and EXT vulnerabilities account for the genetic overlap between CA and BPD, then adjusting for INT or EXT should reduce the genetic overlap to non-significance.
Figure 1. Visual Representation of Cholesky Decomposition.
Note: CA, Childhood abuse; BPD, Borderline personality disorder traits; A = additive genetic influences; C = shared environmental influences; E = non-shared environmental influences. In this model, path a32 and path e32 is the path of interest (coefficients for these paths are reported in Table 6). This path shows the regression effect of CA on BPD traits after adjusting for EXT. The same model is used to adjust for the effect of INT or INT-EXT.
Current Study
We employed a series of discordant twin and biometric models to evaluate the genetic and environmental influences underlying the link between CA, INT and EXT in childhood (present before age 18) and BPD traits in adulthood (age 24). To do so, we used a large sample of twins (over 1300 pairs) followed longitudinally from age 11 to 24. Consistent with previous research, we predicted a main effect of CA, INT, and EXT on BPD traits. In the light of recent evidence that INT and EXT may have an additive and/or interactive effect on BPD and BPD-like behaviors (deliberate self-injury, suicide) (Gratz et al., 2009; Sprague, Javdani, Sadeh, Newman, & Verona, 2011; Sprague & Verona, 2010), we also examined the additive effect of INT and EXT (termed INT-EXT) on the CA-BPD relationship. Our hypotheses were:
If the link between CA and BPD is consistent with a causal model, then a) within discordant MZ twin pairs, the twin exposed to CA would have significantly higher BPD traits than the non-exposed twin, and b) there would be significant nonshared environmental overlap between CA and BPD.
If CA has a causal effect on BPD only in the context of high INT or EXT, the discordant twin models would reveal a significant discordance × INT or discordance × EXT interaction. This pattern of results would be consistent with a diathesis-stress model.
If common genetic influences account for the association between CA and BPD, then a) MZ twins discordant for CA would not differ on BPD traits (but discordant DZ twins would), and b) there would be significant genetic overlap between the two phenotypes. This pattern of results would be consistent with a genetic mediation model.
If the association between CA and BPD is consistent with a genetic mediation model and the genetic mediation is due to common genetic risk for INT and EXT, then the inclusion of INT, EXT, or the additive effect of INT and EXT in the biometric model should account for the genetic overlap.
Method
Sample
Participants were same-sex twin pairs taking part in the ongoing, longitudinal Minnesota Twin Family Study (MTFS) (Iacono, Carlson, Taylor, Elkins, & McGue, 1999). Birth records and public databases were used to locate more than 90% of the families that included a twin birth in the state of Minnesota from 1972 to 1984. Eligible twins and their families a) lived within a day’s drive of Minneapolis with at least one biological parent, and b) had no mental or physical handicap precluding participation. All protocols were approved by the University of Minnesota Institutional Review Board. Parents and children gave informed consent or assent as appropriate. Typical follow-up rates are extremely high, with typical retention rates ~90% (Elkins, McGue, & Iacono, 2007; Hicks, Durbin, Blonigen, Iacono, 2011; Klahr, Rueter, McGue, Iacono, & Burt, 2011). A full description of the design of the MTFS has been provided elsewhere (Iacono et al., 1999).
The MTFS intake sample includes an 11-year-old and a 17-year-old cohort of male and female twins. Intake and follow-up assessments are scheduled to coincide with major transitions in the lives of adolescents and young adults. The current study utilized data from the intake (age 11 for the younger cohort and age 17 for the older) and age 24 assessment data (both cohorts). INT and EXT were assessed at intake, and BPD traits were assessed at age 24.
The final sample included 756 twin pairs from the 11-year old and 626 twin pairs from the 17-year old cohort. Of these 1382 pairs, 896 were MZ (50.8% female) and 486 were DZ (54.5% female). Over 95% of the twins were Caucasian, reflecting the ethnic composition of Minnesota for the birth years sampled. The mean age of participants at the age-24 assessment was 24.92 years (SD = .90 years). Because mean-level BPD traits decline throughout young adulthood (Bornovalova, Hicks, Iacono, & McGue, 2009), BPD traits were centered at age 24.
Measures
Minnesota Borderline Personality Disorder scale (Bornovalova, Hicks, Patrick, Iacono, & McGue, 2011). The MBPD is a 19-item scale developed using items from the Multidimensional Personality Questionnaire (MPQ) (Tellegen, 1982), a well-validated omnibus measure of normal personality. In its development, the MBPD underwent a thorough validation procedure in five separate samples. Candidate items were identified in two samples—inner-city drug users and undergraduates—by examining correlations between all MPQ items and diagnostic and self-report measures of BPD. Candidate items that were significantly correlated with BPD measures in both samples were retained for further analyses in a third sample of community young adults. When selecting items for the MBPD a special emphasis was placed on items providing incremental prediction over general negative affect as measured by the MPQ Stress Reaction scale. The final 19 items were drawn from the MPQ Stress Reaction, Alienation, Control, Aggression, Well-Being, and Absorption scales. In the undergraduate sample, MBPD scores were strongly correlated (r = .80) with scores on the Personality Assessment Inventory-Borderline scale (PAI-BOR) (Morey, 1991). In the substance user sample, MBPD scores were strongly correlated with the self-report Inventory for Interpersonal Problems-BPD scale (r = .60) (Lejuez et al., 2003; Pilkonis, Yookung, Proietti, & Barkham, 1996), and with a DSM-IV interview-based diagnosis of BPD (r = .65). The association between MBPD scores and the self-report and diagnostic BPD scales did not differ by gender, suggesting MBPD scores assess the same construct in males and females.
Bornovalova et al. (2011) also examined the association between MBPD scores and external criterion variables in the community and drug user samples, as well as a sample of male and female prisoners. As evidence of convergent validity, MBPD scores were associated with several known correlates of BPD including history of traumatic exposure (r = .27), symptoms of post-traumatic stress disorder (r = .56), and measures of antisocial behavior (rs = .19-.42), internalizing distress (rs = .31-.48), and drug/alcohol use severity (rs = .25-.42). MBPD scores also exhibited incremental validity over MPQ Negative Emotionality scores in predicting these external criterion variables. MBPD scores also exhibited theoretically coherent associations with multiple measures tapping the normal-range personality constructs of negative affect (rs = .47-.64), positive affect (r = −.39), and disinhibition (rs = .26-.32). Internal consistency was high across the five study samples (α =.81 to.83). MBPD scores also exhibited adequate discriminant validity: MBPD scores exhibited stronger correlations with interview-based symptoms BPD than symptoms of adult antisocial behavior, conduct disorder, and self-reported depressive symptoms. Similarly, in a sample of male and female prisoners, MBPD scores showed higher correlations with a regression-estimated PAI-BOR scale than with interview-based symptoms of conduct disorder and adult antisocial behavior.
To further assuage any concerns about the MBPD, we conducted supplementary analyses utilizing data from the ongoing age-20 assessment (N = 127) of the MTFS Enrichment Sample, a separate cohort of twins that lags the original MTFS (Keyes et al., 2009). Participants completed both the PAI-BOR and the BPD section of the Structured Interview for DSM-IV Personality Disorders (Pfohl, Blum, & Zimmerman, 1997), and were assessed for symptoms of adult antisocial behavior and major depressive disorder using modified version of the Structured Clinical Interview for DSM-III-R (SCID-II, Spitzer, Williams, Gibbons, & First, 1987). MBPD scores at age 17 were strongly related to total BPD DSM-IV symptoms (r = .48) and PAI-BOR scores (r = .56) at age 20. After correcting for attenuation due to measurement error (Spearman, 1904) using the 3-year stability of MBPD scores (r = .63) (Bornovalova et al., 2009), the correlations with MBPD scores increased to .66 with BPD symptoms and .89 with PAI-BOR scores. The slightly smaller correlation with BPD symptoms is due to the differences in method of assessment (interview vs. questionnaire). In support of its discriminant validity, MBPD scores were significantly but less strongly related to symptoms of adult antisocial behavior (r = .35) and major depressive disorder (r = .17).
Exposure to emotional, physical, and sexual abuse
Table 1 provides the assessment schedule of what participants received at which time point. At ages 20, 24, and 29, participants completed the Trauma Assessment for Adults (TAA) (Resnick, Falsetti, Kilpatrick, & Freedy, 1966), an interview to assess traumatic life events related to posttraumatic stress disorder. Questions on the TAA were preceded by the statement, “Some people experience unwanted sexual advances in their lives. This can come from multiple sources: strangers, a friend, a date, or a family member. Not everyone reports these experiences to family, friends, or the police. These types of experiences might happen in any time in a person’s life, including when a person is a child. We would like to know if you have experienced unwanted sexual advances that involved sexual contact. This means any contact between your genitals, breasts or anus and someone else or between their genitals, breasts or anus and you.” After this statement, the TAA asks two questions about sexual abuse, namely: whether the participant has ever had sexual contact with anyone five or more years older than him/her before age 13, and whether anyone (friend, relative, etc) ever used pressure, force, or physical threats to make the participant engage in some sort of unwanted sexual contact. 1
Table 1. Schedule of Assessments.
| Age | 11 | 14 | 17 | 20 | 24 | 29 | Total Outcome Pairs |
|
|---|---|---|---|---|---|---|---|---|
| Intake | FU1 | FU2 | FU3 | FU4 | FU5 | |||
| Younger Cohort | Males | Lifetime INT & EXT |
TAA | TAA CEQ MBPD |
TAA | 376 | ||
| Females | Lifetime INT & EXT |
TAA | TAA CEQ MBPD |
380 | ||||
| Older Cohort | Intake | FU1 | FU2 | FU3 | ||||
| Males | Lifetime INT & EXT |
TAA SocAdj |
TAA MBPD |
289 | ||||
| Females | Lifetime INT & EXT |
TAA | TAA MBPD |
CEQ | 337 |
Abbreviations: FU, Follow-up. MBPD, Minnesota Borderline Personality Disorder Scale. INT, Internalizing psychopathology. EXT, Externalizing Psychopathology. TAA, Trauma Assessment for Adults. SocAdj, Social Adjustment Interview. CEQ, Childhood Experiences Questionnaire.
For female participants in both the 11- and 17-year old cohorts and males in the younger cohort only, the TAA was supplemented by the Childhood Experiences Questionnaire (CEQ), a 26-item inventory with items adapted from the Childhood Life Events Interview (Sher, Gershuny, Peterson, & Raskin, 1997), the Colorado Adolescent Rearing Interview (Crowley, Mikulich, Ehlers, Hall, & Whitmore, 2003), and the Childhood Trauma Questionnaire (Bernstein et al., 2003). The CEQ was administered at ages 24 and 29 and included a detailed retrospective report of sexual abuse occurring before age 18 (7 items including genital fondling and vaginal or anal intercourse). The age-18 definition is consistent with ones used in other studies (Dinwiddie et al., 2000; Johnson et al., 1999; Nelson et al., 2002; Silverman et al., 1996). The CEQ also includes a retrospective report of harsh discipline (2-items; hit with a hand or fist more than once, hit with an object more than once), physical abuse (2-items; hit with a weapon; kicking, biting, or burning), and emotional abuse (6-items including insult, ridicule, humiliation, tormenting with scary things) occurring before age 18. For male twins in the older cohort, harsh discipline only was assessed as part of a larger social adjustment interview completed at age 20, in which participants were asked whether typical discipline while growing up included being “hit in the face” or “hit with an object.” There was good agreement between TAA- and the CEQ-reported sexual abuse (tetrachoric r =.90, kappa=.63).
Finally, participants reported the age at which the abuse first occurred on both the TAA and the CEQ. We defined sexual abuse to include any endorsement of sexual exploitation occurring before age 18. Physical abuse was defined as any report of either harsh discipline or physical maltreatment occurring before age 18. Emotional abuse was defined as any endorsement of emotional cruelty occurring before age 18. All types of CA were coded dichotomously (0 = absent, 1 = present). Participants were classified as having CA if they reported CA on any of the three measures described above. Based on this definition, 27.5% of the sample was exposed to any CA; 16.1% were exposed to emotional CA; 19.0% exposed to physical CA; and 7.3% exposed to sexual CA (See Table 3 for prevalence rates across gender). These rates are consistent with estimates from large representative samples (Hanson et al., 2006; MacMillan et al., 1997; Scher, Forde, McQuaid, & Stein, 2004). Additionally, preliminary analyses of our data indicated that all abuse indices were related significantly to adult antisocial behavior, alcohol and nicotine dependence, and major depression symptoms in both males and females at age 24, providing evidence for the validity of the CA indices (Derringer, Krueger, Irons, & Iacono, 2010).
Table 3. Number of Discordant MZ and DZ Twin Pairs across CA Types.
| # Discordant MZ Pairs |
# Discordant DZ Pairs |
% Reporting CA |
||
|---|---|---|---|---|
| Any CA | Males | 93 | 55 | 24.4% |
| Females | 104 | 82 | 30.1% | |
| All | 197 | 137 | 27.5% | |
| Emotional CA | Males | 34 | 25 | 14.4% |
| Females | 60 | 52 | 16.9% | |
| All | 94 | 77 | 16.1% | |
| Physical CA | Males | 66 | 37 | 21.4% |
| Females | 65 | 44 | 16.9% | |
| Total | 131 | 81 | 19.0% | |
| Sexual CA | Males | 13 | 16 | 3.0% |
| Females | 52 | 41 | 11.1% | |
| All | 65 | 57 | 7.3% |
Note: CA, Childhood abuse; MZ, Monozygotic; DZ, Dizygotic.
EXT and INT symptoms
EXT and INT were assessed at the intake assessment (age 11 for the younger cohort, age 17 for the older cohort) via a combination of interview and self-report measures that were administered to the twins, their mothers, and teachers. Trained interviewers with either a bachelor’s or a master’s degree in psychology administered structured interviews to twins and mothers. Twins were assessed for attention deficit/hyperactivity disorder, conduct disorder, oppositional defiant disorder, major depressive disorder, separation anxiety disorder (younger cohort only) and social phobia and specific phobia (older cohort only) using the Diagnostic Interview for Children and Adolescents – Revised (DICA-R) (Reich & Welner, 1988) and the Structured Clinical Interview for DSM-III-R (Spitzer, Williams, Gibbon, & First, 1992). Mothers also reported on symptoms present in their children using the parent version of the DICA. We also administered a supplemental psychiatric onset section, in which both the mother and twin were queried about the onset of each symptom, allowing us to examine the effect of INT and EXT symptoms that preceded versus followed CA. A “best-estimate” approach was taken such that a symptom was considered present if reported by either the mother or twin. An established diagnostic consensus procedure was used to optimize the likely accuracy of symptom assignment, yielding kappa reliabilities of .71 or greater for all the disorders assessed. Finally, up to 3 teachers completed ratings of childhood disruptive behavior disorders and internalizing distress (anxious, moody, and dysthymic temperament) using the Teacher Rating Form (Sherman, McGue, & Iacono, 1997). If multiple teacher ratings were available, the mean of the teacher ratings was used. The state of Minnesota has a policy of placing members of a twin pair in separate classrooms whenever possible, which should minimize any bias due to twin contrast or comparison on the teacher ratings.
Similar to many previous studies (Achenbach, McConaughy, & Howell, 1987; Burt, McGue, Krueger, & Iacono, 2005b; Sherman et al., 1997), the cross-informant correlations hovered around .3 (mean inter-informant r = .29). While it is possible that findings might differ as a function of informant, previous studies indicate that each type of informant contributes a considerable amount of valid information not contributed by other informants, allowing for a more complete assessment of psychopathology (Achenbach et al., 1987; Burt et al., 2001). Thus, an EXT composite was calculated using the mean z-score of best-estimate symptom counts and teacher ratings of attention deficit/hyperactivity disorder, conduct disorder, and oppositional defiant disorder. For the younger cohort, INT was calculated as the mean z-score of symptoms of major depressive disorder and separation anxiety disorder and the teacher rating of internalizing distress. For the older cohort, INT was the mean z-score of symptoms of major depressive disorder, social phobia and simple phobia (currently known as specific phobia) and the teacher rating of internalizing distress. Finally, we computed a score that reflected the combined effect of INT and EXT (termed INT-EXT)2. In this case, we summed across individual mean-z-scored childhood disorders. Using procedures similar to those used here, past work with this sample has documented the high reliability and construct validity of INT and EXT (Bornovalova et al., 2010; Burt et al., 2003; Burt, McGue, Iacono, & Krueger, 2006; Burt et al., 2005a, 2005b; Hicks, South, DiRago, Iacono, & McGue, 2009; Hicks, DiRago, Iacono, & McGue, 2009; Walden, McGue, Iacono, Burt, & Elkins, 2004).
Phenotypic Analyses: Main effects and Interactions
For our initial analyses, we examined the phenotypic associations between CA, BPD, and INT, EXT and INT-EXT using correlation and regression analysis. First, we examined the CA-BPD association by fitting a regression model that included the effects of CA and Sex in the full sample and separately by gender (in order to test if the effect of CA on BPD trait variables differed for males and females). If the regression weights of CA on BPD traits were significantly different for males and females, discordant twin and biometric models would be computed separately by gender. Next, we tested the CA × INT, CA × EXT, and CA × INT-EXT interactions, examining if those with high levels of INT, EXT, or INT-EXT who were exposed to CA exhibited greater levels BPD traits in adulthood. Analyses were conducted for each type of abuse (emotional, physical, and sexual), and any type of CA. For all analyses we used PROC MIXED in SAS 9.2 (SAS Institute Inc, 2008) that adjusts all statistics for the correlated twin observations.
Discordant twin analysis
A mixed-level regression framework (Begg & Parides, 2003; McGue et al., 2010) predicting BPD traits was used to investigate whether the association between CA and BPD was consistent a causal effect. In the discordant-twin analysis, the regression of BPD traits on CA is decomposed into a within pair effect and a between pair effect (Begg & Parides, 2003), with zygosity as a moderator. The CAW or within-pair effect gives the difference in outcome for the members of a twin pair who are discordant for CA. The within-pair effect is the main interest of this study as it measures the similarity in BPD among twins discordant for CA. All twins were included in the regression analysis regardless of concordance status to estimate both between-pair effects (for which both discordant and concordant pairs are informative) as well as within-pair effects (for which only the discordant pairs are informative). Number of discordant twin pairs by each CA type and by zygosity is presented in Table 3.
For each type of CA, we fit a series of mixed-level regression models using PROC MIXED in SAS. Specifically, we tested whether the twin who experienced CA had higher levels of BPD traits than the non-CA twin after controlling for gender and cohort. Next, if there were significant CA × INT, CA × EXT, or CA × INT-EXT interactions in the phenotypic models, we fit the CAW × INT, CAW × EXT, or CAW × INT-EXT in the genetically-informed discordant twin models (see Huibregtse et al, 2011 for an example of this approach).
Biometric modeling
Standard biometric models were used to examine the influence of additive genetic, shared environmental, and non-shared environmental influences on all variables of interest. The additive genetic component (a2) refers to the additive effect of individual genes summed over loci on trait variance. Genetic influences are inferred if the MZ correlation is greater than the DZ correlation for a given trait. Shared environmental (c2) effects refer to environmental influences that increase similarity between members of a twin pair. Shared environmental effects are inferred if the DZ correlation is more than 1/2 the MZ correlation. Non-shared environmental (e2) effects refer to environmental factors that contribute to differences between members of a twin pair and are inferred when the MZ correlation is less than 1. Measurement error is also included in the estimate of e2.
Next, we estimated the extent to which genetic and environmental influences on CA also influenced BPD traits. To do so, we fit a series of bivariate Cholesky decompositions to CA and BPD that parse both the variance of each phenotype and the covariance between phenotypes into their respective genetic and environmental components (Neale & Cardon, 1992). Specifically, we decomposed the standardized coefficient in the regression of BPD traits on each form of CA into their constituent genetic and environmental components. Subsequently, we tested whether genetic and environmental risk in INT, EXT, or INT-EXT could account for the association between CA and BPD traits. To do so, we fit a series of three-variable Cholesky decomposition models to INT, EXT, or INT-EXT, CA, and BPD traits (see Figure 1 for visual representation). If INT, EXT, or INT-EXT contributes to both CA and BPD, then the CA-BPD genetic and environmental regression coefficient should be reduced in these models. The difference in the parameters accounting for the CA-BPD association from before to after accounting for INT and EXT or their joint effect allowed us to examine the degree to which these variables account for genetic and environmental overlap between CA and BPD. All biometric analyses were conducted using the computer program Mx (Neale, Boker, Xie, & Maes, 2002).
Results
Preliminary Analyses: Conceptual Distinction between INT, EXT, and adult BPD Traits
First, we conducted several analyses to ensure conceptual distinctions between INT and EXT and adult BPD. First, we focused on INT and EXT symptoms that generally onset in childhood. These behaviors do not overlap with the diagnostic criteria for BPD (APA, 1994, 2000) or the MBPD scale. Second, we found that the average age of first EXT and INT symptom was 7.03 (SD = 3.91) years and 8.21 (SD = 4.31) years, respectively. Ninety two percent of those reporting any EXT behaviors and 70% of those reporting INT behaviors reported the expression of earliest symptom prior to age 123. Finally, as shown in Table 2, INT and EXT showed relatively modest correlations with BPD at age 24. All of these factors indicate INT and EXT can be clearly be adequately distinguished from BPD traits in this sample.
Table 2. Correlations among Variables.
| BPD Traits | EXT | INT | INT-EXT | Any CA | Emotional CA | Physical CA | Sexual CA | |
|---|---|---|---|---|---|---|---|---|
| Sex | −.11*** | −.32*** | .33*** | −.07** | .11** | .06 | −.10* | .39*** |
| BPD Traits | --- | .27*** | .20*** | .29*** | .18*** | .24*** | .12*** | .15*** |
| EXT | --- | .41*** | .90*** | .21*** | .17*** | .27*** | .16*** | |
| INT | --- | .70*** | .25*** | .18*** | .17*** | .32*** | ||
| INT-EXT | --- | .27*** | .20*** | .30*** | .29*** | |||
| Any CA | --- | .97*** | .93*** | .99*** | ||||
| Emotional CA | --- | .48*** | .29*** | |||||
| Physical CA | --- | .20*** |
Note: CA, Childhood abuse; BPD, Borderline personality disorder traits; EXT, Childhood externalizing psychopathology; INT, childhood internalizing psychopathology; INT-EXT, combined childhood internalizing and externalizing psychopathology. Sex coded 1= male, 2 = female.
p<.05;
p<.01;
p<.001.
Preliminary Analyses: Cohort Effects
To rule out cohort effects, we first examined cohort differences in the effects of CA on BPD traits by cohort. The effects of CA on BPD traits did not differ by cohort for overall CA [B (SE) = .07 (.09), p = .47)], emotional CA [.02 (.13), p = .86)], physical CA [.05 (.12), p = .63)], or sexual CA [.08 (.16), p = .62)]. Moreover, there were no differences in mean BPD levels between cohorts [mean (SD) = 35.72 (7.62) v. 36.01 (7.98) for the 11-year old and 17-year old cohorts, respectively, B (SE) = −0.04 (.05), p = .40]. There were also no cohort differences in the rates of any CA [26.2% v. 29.0% for 11-year old and 17-year old cohorts, respectively, B (SE) = −0.14 (.10), p = .17] or physical CA [17.4% v. 20.8%, B (SE) = −0.21 (.12), p = .09]. However, the older cohort reported higher frequencies of emotional [14.1% v. 20.1%, B (SE) = −0.42 (.15), p < .01] and sexual [5.3% v. 9.8%, B (SE) = −0.67 (.17), p < .001] CA. To be conservative, we controlled for cohort status in all analyses below.
Phenotypic Analyses: Main effects and Interactions
Pearson, biserial and tetrachoric correlations among the variables of interest indicated that all types of CA were modestly related to BPD (see Table 2). Additionally, BPD and all types of CA were moderately related to INT, EXT, and INT-EXT. Finally, all types of CA were moderately interrelated Next, we tested if there were any curvilinear trends that might suggest that the CA-BPD association changes at very high levels of BPD. To do so, we fit a series of regression models that included gender, cohort, the centered linear BPD traits term and a centered quadratic BPD traits term as predictor variables and various abuse types as criterion variables. Results failed to indicate any quadratic effects of BPD in the overall sample. Examining males and females separately also failed to yield quadratic effects of BPD on CA. This indicates that the relationship between BPD traits and CA functions on a dose-response relationship, such that as BPD traits increase in severity, the probability of abuse increases4.
Third, we estimated the main effects of CA, Sex, and the CA × Sex, CA × INT, CA × EXT, and CA × INT-EXT interactions in a series of mixed-level regressions (Table 4). Each type of CA had a significant effect on BPD traits, such that exposed individuals showed more BPD traits than the non-exposed individuals. Gender was also a significant predictor of BPD. Surprisingly, men reported slightly more BPD traits than women, though this difference was small (d = .17). Next, we entered INT and INT × CA effects (the EXT and EXT × CA and INT-EXT and INT-EXT × CA effects were entered in separate models) into the regression model. INT, EXT, and INT-EXT had significant effects on BPD traits. Moreover, Sobel tests (Sobel, 1982) indicated that INT, EXT, or INT-EXT mediated the relationship between CA and BPD traits in 27 of 30 models, with full mediation in 13 models (effect of CA dropped to nonsignificance) (Baron & Kenny, 1986). This suggests that INT, EXT, and their combination contribute importantly to the relationship between BPD traits and physical and sexual CA. However, none of the CA × Sex interactions were significant; therefore, the CA × Sex interaction term was excluded from any additional regression models. Because the CA × INT, CA × EXT, and CA × INT-EXT interaction effects did not reach significance at the phenotypic level, we do not present tests for these effects in the discordant twin analyses5
Table 4. Regression Models of the Effects of Sex, CA, and Internalizing and Externalizing Symptoms on BPD traits at age 24. Unstandardized regression coefficients [B (SE)] are presented.
| Outcome: BPD Traits at age 24 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Males | Females | All | ||||||||||
|
| ||||||||||||
| Any | Emotional | Physical | Sexual | Any | Emotional | Physical | Sexual | Any | Emotional | Physical | Sexual | |
| Effect of CA Considered Alone | ||||||||||||
| Sex | ---- | ---- | ---- | ---- | ---- | ---- | ---- | ---- | −.19 (.05)* | −.17 (.06)* | −.17 (.05)* | −.21(.05)* |
| CA | .21 (.07)* | .40 (.11)* | .13 (.08) | .40 (.18) | .36 (.06)* | .42 (.08)* | .27 (.08)* | .28 (.09)* | .29 (.05)* | .42 (.06)* | .20 (.05)* | .30 (.08)* |
| Sex Diff? (contrast z)a |
---- | ---- | ---- | ---- | ---- | ---- | ---- | ---- | No (1.63) |
No (0.15) |
No (1.24) |
No (.60) |
| Effects of CA Considered with INT | ||||||||||||
| CA | .17 (.07) | .38 (.11)* | .08 (.08) | .32 (.18) | .28 (.06)* | .36 ( .07)* | .20 (.08)* | .16 (.09) | .23 (.05)* | .37 (.06)* | .14 (.05) | .19 (.08) |
| INT | .20 (.04)* | .19 (.05)* | .21 (.04)* | .20 (.04)* | .23 (.03)* | .24 (.03)* | .25 (.03)* | .25 (.03)* | .22 (.02)* | .23 (.02)* | .23 (.02)* | .23 (.02)* |
| CA*INT | −.15 (.07) | −.12 (.11) | −.20 (.08) | .15 (.18) | .04 (.06) | −.01 (.07) | .02 (.07) | .14 (.07) | −.01 (.04) | −.03 (.06) | −.06 (.05) | .13 (.06) |
| Mediation Significant? (critical z) bc |
Yes (3.32) |
No (1.16) |
N/A | N/A | Yes (4.96) |
Yes (3.97) |
Yes (3.42) |
Yes (5.36) |
Yes (6.85) |
Yes (3.92) |
Yes (5.32) |
Yes (6.49) |
| Effects of CA Considered with EXT | ||||||||||||
| CA | .13 (.07) | .36 (.11)* | .02 (.08) | .26 (.18) | .26 (.06)* | .35 (.07)* | .15 (.08) | .15 (.09) | .21 (.05)* | .36 (.06)* | .09 (.06) | .19 (.08) |
| EXT | .22 (.03)* | .17 (.04)* | .23 (.03)* | .22 (.03)* | .26 (.06)* | .28 (.04)* | .28 (.04)* | .30 (.04)* | .24 (.02)* | .23 (.03)* | .25 (.02)* | .26 (.02)* |
| CA*EXT | −.04 (.06) | −.02 (.09) | −.04 (.07) | .13 (.19) | −.03 (.07) | −.03 (.08) | .02 (.08) | −.06 (.08) | −.05 (.04) | −.02 (.06) | −.03 (.05) | .01 (.07) |
| Mediation Significant? |
Yes (4.22) |
No (1.88) |
N/A | N/A | Yes (3.75) |
Yes (3.25) |
Yes (4.56) |
Yes (4.60) |
Yes (6.21) |
Yes (3.68) |
Yes (7.17) |
Yes (5.69) |
| Effects of CA Considered with Joint Effects of INT and EXT | ||||||||||||
| CA | .13 (.07) | .37 (.11)* | .02 (.08) | .25 (.18) | .24 (.06)* | .34 (.07)* | .14 (.08) | .12 (.09) | .19 (.05)* | .35 (.06)* | .08 (.05) | .16 (.08) |
| INT-EXT | .23 (.03)* | .19 (.04)* | .24 (.03)* | .23 (.03)* | .30 (.03)* | .30 (.03)* | .31 (.03)* | .32 (.03)* | .26 (.02)* | .25 (.03)* | .27 (.02)* | .28 (.02)* |
| CA* INT-EXT | −.07 (.06) | −.04 (.09) | −.08 (.07) | .23 (.21) | .04 (.06) | .02 (.08) | .08 (.09) | .09 (.09) | −.02 (.05) | −.00 (.06) | −.03 (.05) | .13 (.08) |
| Mediation Significant? |
Yes (4.64) |
No (1.52) |
N/A | N/A | Yes (5.95) |
Yes (4.10) |
Yes (5.60) |
Yes (5.42) |
Yes (7.26) |
Yes (3.89) |
Yes (6.62) |
Yes (6.05) |
Note: In all models, BPD is the criterion variable. CA, Childhood abuse; BPD, Borderline personality disorder traits; EXT, Childhood externalizing psychopathology; INT, childhood internalizing psychopathology; INT-EXT, combined childhood internalizing and externalizing psychopathology. Table is organized as follows. The variables in each model are named on the far left. For each column, CA represents any, emotional, physical and sexual CA.
Significance level was set to p<.01 due to multiple tests.
Sex was coded as 1 (male) and 2 (female). Significance of sex differences was tested by comparing regression coefficients between males and females. This provides a contrast z value. If z value was higher than 2.58 (two-tailed significance at .01 level), this would be evidence for significant sex differences. Because the effect of CA on BPD traits failed to come out in the initial model (Effect of CA Alone), we did not consider it in the analyses that consider INT and EXT.
The significance of mediation of the CA-BPD association by INT, EXT, or INT-EXT was tested using the Sobel test (Sobel, 1982) which provides a critical z value. If z value was higher than 2.58 (two-tailed significance at .01 level), mediation was considered significant.
Mediation was tested only if there was a univariate effect of CA in the first model (otherwise, denoted as n/a) (see Baron & Kenny, 1986).
Discordant Twin Models
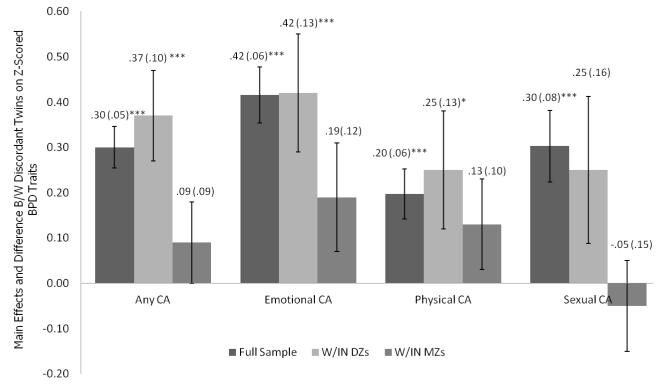
We fit discordant twin models to compare the effects of CA on BPD traits within MZ and DZ pairs. The results for the models testing the effect of CA are shown in Figure 2. First, all four MZ within-pair effects (CAW) failed to reach statistical significance. This indicates that CA-affected and CA-nonaffected twins within an MZ pair did not differ significantly in BPD traits, regardless of the abuse category. The DZ within-pair effects were significant for any CA, emotional CA, and physical CA, but not sexual CA – indicating that CA-affected and CA-nonaffected DZ twins differed significantly in BPD traits for three of the four types of CA. The fact that the MZ effects were nonsignificant but the DZ effects were is consistent with genetic mediation effect of the CA-BPD association. In the case of sexual CA, both the MZ and DZ within-pair effects were nonsignificant; however, the DZ effect was considerably larger than the MZ effect – a pattern also consistent with genetic influences.
Figure 2. Within Twin Pair Differences in BPD Trait Scores for Pairs Discordant for Child Abuse.
Note: CA, Childhood abuse; BPD, Borderline personality disorder traits. The BPD index was z-scored, and unstandardized regression weights [B (SE)] are presented above the bar.
Biometric modeling
Table 5 presents the twin correlations and estimates of genetic and environmental contributions to the BPD traits and CA. BPD evidenced moderate heritability, a small and non-significant effect of shared environment, and large non-shared environmental effects. INT, EXT, and INT-EXT showed a moderate-to-large influence of genetic factors and a small influence of shared and non-shared environmental factors (shared environmental effects were not significant for INT or INT-EXT). All types of CA showed small but significant genetic effects, moderate to large shared environmental influences, and moderate and significant nonshared environmental influences6. Our results are consistent with previous reports on the heritability of BPD, CA, and INT and EXT (Bornovalova et al., 2009; Distel et al., 2008; Hicks et al, 2009, a, b; Schulz-Heik et al., 2010; Stein et al., 2002; Torgersen et al., 2008). Notably, although there was no CA × Sex interaction on BPD traits, results were unchanged when we re-ran the discordant and biometric analyses separately for male and female twins.
Table 5. Heritability of BPD and CA by CA Type.
| MZ | DZ | A | C | E | |
|---|---|---|---|---|---|
| BPD Traits | .44 | .28 | .35 (.14, .50) | .10 (.00, .28) | .56 (.50,.62) |
| EXT | .78 | .52 | .56 (.45,.69) | .22 (.09,.33) | .22 (.19,.24) |
| INT | .50 | .31 | .43 (.27,.57) | .09 (.00,.24) | .47 (.43, .52) |
| INT-EXT | .71 | .45 | .59 (.45,.73) | .14 (.00, .26) | .28 (.25,.31) |
| Any CA | .57 | .49 | .13 (.04, .33) | .46 (.28,.57) | .41(.35,.46) |
| Emotional CA | .53 | .36 | .13 (.03,.31) | .43 (.27,.55) | .44 (.38,.49) |
| Physical CA | .61 | .56 | .10 (.01,.25) | .51 (.38,.62) | .39 (.34,.44) |
| Sexual CA | .60 | .58 | .05 (.03,.08) | .65 (.61,.70) | .30 (.25,.34) |
Note: A = additive genetic influences; C = shared environmental influences; E = non-shared environmental influences. CA, Childhood abuse; BPD, Borderline personality disorder traits. EXT, childhood externalizing psychopathology; INT, childhood internalizing psychopathology; INT-EXT, combined childhood internalizing and externalizing psychopathology. BPD, Borderline personality disorder.
Genetic and Environmental Influences on Covariation between CA and BPD
Table 6 presents the genetic and nonshared environmental influences on BPD and CA. Notably, all shared environmental influences common to both BPD and CA were dropped. This resulted in significant improvements in model fit as indexed by changes in the Bayesian Information Criterion (Raftery, 1995). There were moderate to large genetic effects on the association between each type of CA and BPD traits. These results are consistent with those from the discordant twin models that also suggested genetic effects on the CA-BPD relationship. The nonshared environmental effects were all small but significant; however, these effects were negative for sexual CA.
Table 6. Models Examining Genetic and Environmental Influences on the association between BPD and CA before and after adjusting for INT and EXT.
| Genetic Correlation (CI) | Nonshared Environmental Correlation (CI) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| CA Type | Unadjusted | Adjusted For EXT |
Adjusted For INT |
Adjusted For INT- EXT |
Unadjusted | Adjusted For EXT |
Adjusted For INT |
Adjusted For INT-EXT |
| Any | .78 (.45, 1.0) |
.67 (.35,.95) |
.74 (.38,1.0) |
.59 (.26, .92) |
.08 (.04,.12) |
.06 (.02,.09) |
.06 (.02,.10) |
.06 (.03, .10) |
| Emotional | .44 (.31,.67) |
.43 (.30,.65) |
.40 (.27,.60) |
.39 (.24, .94) |
.18 (.14,.21) |
.15 (.12,.19) |
.17 (.14,.20) |
.16 (.13, .20) |
| Physical | .31 (.07,.79) |
.17 (−.04,.92) |
.08 (−.77,.98) |
.05 (−.22, .30) |
.10 (.07,.14) |
.08 (.04,.11) |
.09 (.06,.13) |
.07 (.03, .11) |
| Sexual | .97 (.62,1.0) |
.88 (.44,.93) |
.97 (.69,.99) |
.90 (.68, .94) |
−.06 (−.09,−.02) |
−.06 (−.10,−.03) |
−.05 (−.08,−.02) |
−.06 (−.09, −.04) |
Note. CA, Childhood abuse; BPD, Borderline personality disorder traits. EXT, Childhood externalizing psychopathology; INT, childhood internalizing psychopathology; INT-EXT, combined childhood internalizing and externalizing psychopathology. Table reports the effect of each CA type on BPD when unadjusted, adjusted for EXT and adjusted for INT (all are standardized regression coefficients). These effects represent the coefficients for paths a32 and e32 in Figure 1.
Genetic and Environmental Influences on Covariation between Abuse and BPD after Adjusting for INT, EXT, and INT-EXT
Results of three-variable Cholesky models examining the effects of all types of CA on BPD traits after adjusting for EXT, INT, and INT-EXT are presented in Table 6. After adjusting for EXT, there were small reductions in the genetic overlap between any CA and sexual CA and BPD traits. The genetic effect of emotional CA on BPD remained almost entirely unchanged, as did all nonshared environmental effects. Finally, the effect of physical CA on BPD traits had a moderate reduction to nonsignificance.
After adjusting for INT, there was a slight drop in the genetic effects for any CA and emotional CA, and a moderate drop for physical CA. Moreover, the genetic influence of physical CA on BPD traits dropped to nonsignificance after accounting for INT. The genetic influence of sexual CA on BPD traits did not change after adjusting for INT. Finally, the nonshared environmental influences of all CA types on BPD traits showed little change after accounting for INT.
Finally, after adjusting for INT-EXT, there were small reductions in the genetic effects of any CA and sexual CA on BPD traits; a negligible reduction in the genetic effect of emotional CA on BPD traits; and a large drop for physical CA. Also, the genetic influence of physical CA on BPD traits dropped to nonsignificance. Finally, the nonshared environmental influences of all types of CA on BPD traits showed little change after accounting for INT-EXT. These results indicate that INT, EXT, and INT-EXT do not account for much of the genetic relationship between any, emotional, and sexual CA and BPD traits. Instead, there are common genetic risk for BPD traits and CA that are independent of INT or EXT. However, INT, EXT, and their joint effect account for nearly all the common genetic risk factors contributing to both physical CA and BPD traits.
More Restrictive Tests of the CA and BPD relationship
We also fit more restrictive models to test if the influence of CA on BPD traits is consistent with a causal model. Because sample size showed some drop-off in these subsample analyses, they had less power to address the aims of the study (although they were sufficiently powered to detect a moderate effect size). Nevertheless, in each analysis, the pattern of results supported the findings obtained with the full sample.
First, several studies suggest that the age of onset of CA is inversely related to BPD symptoms (McLean & Gallop, 2003; Yen et al., 2002; Zanarini et al., 2002). Thus, we repeated the analyses with CA categorized as “before age 13”, and then, as “before age 7” – a definition used previously (McLean & Gallop, 2003). The “before age 13” analysis included 170 discordant MZ twin pairs and 117 discordant DZ pairs (with 20.6% of the sample reporting any abuse). The “before age 7” analysis included 156 discordant MZ twin pairs and 100 discordant DZ pairs (with 16.9% of the sample reporting any abuse). The pattern of results was identical to those for the full sample. Specifically, all MZ within-pair effects were nonsignificant and the nonshared environmental correlations were small and/or nonsignificant. Additionally, we considered that the interaction model is a “diathesis-stress” model only when the diathesis comes before CA. Thus, we re-ran the analyses including only individuals who reported that their youngest onset of INT or EXT symptoms preceded the earliest occurrence of abuse. Again, the pattern of results was identical to the findings reported for the full sample.
Discussion
We examined the mechanisms underlying the relationship between emotional, physical, and sexual CA and BPD traits by testing 3 models. First, we tested if the effects of CA on BPD traits were direct and consistent with a causal relationship (direct causal model). Second, we tested if CA influences BPD traits only in combination with INT, EXT, or pooled INT and EXT symptoms (diathesis-stress model). Finally, we tested an alternative model that the CA-BPD association is better accounted for by common genetic risk factors (genetic mediation model). Within this latter model, we tested if INT, EXT, or additive INT and EXT psychopathology could account for genetic or environmental influences common to CA and BPD. Using two genetically informed methods (discordant twin design and the modeling of genetic and nonshared environmental correlations), we were able to begin to disentangle these competing hypotheses.
First, consistent with previous work (Carlson et al., 2009; Golier et al., 2003; Trull, 2001; Zanarini et al., 2002), we found evidence for the interrelationship of all our key variables. Importantly, the relationship between all types of CA and BPD was linear (rather than quadratic), indicating that as BPD traits increase, so does the probability of CA. This is consistent with previous studies indicating that BPD is best conceptualized as a dimensional construct (Ayers, Haslam, Bernstein, Tryon, & Handelsman, 1999; Edens et al., 2008; Rothschild, Cleland, Haslam, & Zimmerman, 2003; Trull, Widiger, Lynam, & Costa, 2003; Wilberg, Urnes, Friis, Pedersen, & Karterud, 1999). Next, we failed to find evidence for any of the CA × INT, CA × EXT, or CA × INT-EXT interactions. This argues against the idea that CA has an especially strong effect on BPD among those with an INT and EXT vulnerability, or even among those with both INT and EXT problems. Next, discordant twin analyses found that MZ twins discordant for CA were similar in BPD traits, but discordant DZ twins differed significantly. This pattern of results suggests that the association between CA and BPD traits is likely mediated by common genetic factors. Stated otherwise, our data are inconsistent with either a direct causal or a diathesis-stress model. Rather, they are consistent with the genetic mediation model.
Biometric analysis provided corroborating evidence for genetic mediation effects in the association between CA and BPD. First, although CA is generally thought of as a purely environmental effect, our results suggest that genetic effects accounted for a small but statistically significant amount of variance in CA - a result consistent with other investigations [(Bemmels, Burt, Legrand, Iacono, & McGue, 2008; Distel et al., 2011; Schulz-Heik et al., 2010; Stein et al., 2002; Thapar, Harold, & McGuffin, 1998; Thapar & McGuffin, 1996); but see Jaffee & Price (2007) for contradictory findings]. And, though the genetic effect on CA was modest, genetic factors accounted for most the association between BPD and CA. These results are consistent with a recent study (Distel et al., 2011) reporting that BPD had moderate genetic and small (and in some cases non-significant) nonshared environmental correlations with adult violent assault, adult sexual assault, robbery, divorce, and job loss. Thus, both our and the Distel et al. (2011) results provide evidence that the association between exposure to traumatic events and BPD may be better accounted for by common genetic influences rather than the former causally influencing the latter.
Finally, the current results indicated that, by and large, controlling for INT, EXT, or INT-EXT had little if any effect on the genetic overlap between BPD and any, emotional, or sexual CA. In contrast, controlling for EXT, INT, and INT-EXT accounted for most of the genetic overlap between physical abuse and BPD (adjusted genetic correlation was not significant). These results suggest that the genetic risk for INT and EXT accounts for much the genetic risk underlying the association between BPD and physical abuse. However, factors other than INT or EXT must account for the genetic overlap between BPD with any, emotional, and sexual CA.
Potential Mechanisms Explaining the CA-BPD Link
Genetic mediation is played out via passive, evocative, or active gene-environment correlations (Plomin, DeFries, & Loehlin, 1977; Scarr & McCartney, 1983). In the case of a passive gene-environment correlation, parents transmit their genotype to their offspring as well as help create that offspring’s rearing environment. As applied to the relationship between physical abuse and BPD, a child who shares a genetic predisposition to impulsivity, aggression or negative emotionality with his or her parents is also more likely to be reared in a hostile and abusive family environment. In the case of an evocative gene-environmental correlation, an individual’s genotype elicits specific responses from others. For example, a child’s genetic disposition towards behavioral disinhibition or oppositionality may elicit physical aggression from the parents. Similarly, a child’s genetic predisposition to depression or anxiety may place greater demand on the parents’ coping resources, thereby reducing patience and increasing frustration. The possibility of gene-environment correlations is also a likely explanation for the genetic overlap between sexual and emotional abuse with BPD traits. However, the actual vulnerability factor that accounts for the genetic overlap in these cases remains unknown.
Several lines of research may be useful to understand what processes account for the genetic overlap among CA and BPD. First, it is necessary to identify the developmental precursors to BPD in childhood and adolescence. For instance, one might test what childhood and adolescent manifestations of INT and EXT are related to adult BPD. Also, one might test if factors not tested in the current study - such as the inability to withstand psychological distress, difficulties in interpersonal situations, or emotion-regulatory skills might be developmental precursors to BPD. Identifying additional developmental precursors might also assist in identifying the factors that account for the genetic overlap between BPD and sexual and emotional CA. Once the developmental trajectory of BPD is established, it may be worthwhile exploring how gene-environment correlations play out at different developmental stages. Both biometric modeling and experimental studies would be useful explorations into this hypothesized relationship. For example, one might test if particular characteristics are more evocative of maladaptive parenting responses at one age versus another. Additionally, observations of parent-offspring interactions in childhood and adolescence could provide tests of evocative gene-environment correlations. Finally, exploring the predisposition to engage in maladaptive parenting among parents with underlying vulnerabilities may provide evidence for a passive gene-environment correlation.
Beyond research implications, our study has several implications for BPD prevention. First, we emphasize that the results do not support the idea that CA is inevitable, justified, or without harm. Along with the subjective trauma of experiencing abuse, CA is linked with multiple mental and physical health consequences (Hussey, Chang, & Kotch, 2006; Irish, Kobayashi, & Delahanty, 2010; Springer, Sheridan, Kuo, & Carnes, 2007). And, as we note in the results, the nonshared environmental overlap between CA and BPD was significant (albeit small) for any, emotional, and physical CA, suggesting that there might be small causal effects of CA on BPD. Thus, increasing prevention efforts for childhood abuse will be undoubtedly beneficial. However, the current data also suggests that targeting maladaptive behaviors associated with pre-existing vulnerabilities (while simultaneously targeting maladaptive parenting or parental psychopathology) may be successful in preventing the development of later BPD.
The current study has several limitations. First, the study used a sample of mostly Caucasian twins. Second, the retrospective reporting of CA with no independent corroboration could have introduced a retrospective bias. Third, we examined a number of abuse subcategories (i.e. emotional, physical, and sexual). However, follow-up studies may also consider other sub-categories including perpetrator type (e.g. biological vs. non-biological perpetrator; sex of perpetrator) and the characteristics of abuse itself (e.g., genital v. non-genital contact in sexual abuse; duration, frequency, and psychological impact of abuse). Fourth, the current study used a self-report questionnaire to measure BPD traits. Future studies would benefit from the use of a multi-assessment, multi-informer design, as previous work suggests that different assessment methods and informants provide unique information about BPD traits (Hopwood et al., 2008; Oltmanns & Turkheimer, 2009). Fifth, measures of CA were obtained from several different instruments and at several time points rather than using one standard measure. On the other hand, the multiple assessment instruments administered at multiple time points are a strength as well as a limitation. Specifically, rather than relying on one instrument, the multiple measures and multiple time points provide convergent validity data for our assessment of CA. Finally, although less of a limitation than a future direction, it is important to cross-validate the current findings by replicating our study in larger and/or separate datasets that use different measures of CA and BPD characteristics to assure that the current findings are not a function of sample or measurement.
Despite these caveats, the current research has utilized a series of powerful methods testing the nature of the CA-BPD relationship, and the results are compelling. Future research can extend these findings by providing insight into the factors that do causally contribute to BPD, which can then be used to inform the design of interventions that ultimately reduce the suffering associated with this form of psychopathology.
Acknowledgments
Data for this project were collected at the University of Minnesota. This work was supported by National Institute of Drug Abuse Grant DA05147 and DA028807 and National Institute on Alcohol Abuse and Alcoholism grants AA09367 and AA015621. Brian M. Hicks was supported by DA025868. All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. No conflict of interest exists for any of the authors.
Footnotes
The preceding statement and questions have been reworded to protect instrument copyright.
We also considered utilizing a variable reflecting the interaction between INT and EXT in the genetically-informed analyses. However, preliminary phenotypic analyses indicated that the INT × EXT interaction term is not related to BPD traits (neither in the full sample nor in males or females when examined separately). As such, we focused on the additive effect of INT and EXT in all analyses. Combining the two variables also yields more power to the phenotypic and biometric mediation analyses than using INT and EXT variables separately.
We replicated all analyses removing individuals who reported an onset of INT or EXT after age 12. The results were unchanged.
An additional reason to use a dimensional measure of BPD comes from previous work showing that BPD is best thought of as a dimensional construct (Edens, Marcus, & Ruiz, 2008). Also, dimensional measures of personality disorders possess substantially greater statistical power than categorical measures (Markon, Chmielewski, & Miller, 2011)
Nevertheless, even when tested, all discordant twin models failed to show a within-pair × INT, within-pair × EXT, or within-pair × INT-EXT effect.
Estimates obtained using the three-variable Cholesky decomposition
References
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: implications of cross-informant correlations. Psychological Bulletin. 1987;101(2):213–232. [PubMed] [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: 2000. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders (4th ed) Washington, DC: 1994. [Google Scholar]
- Arens EA, Grabe HJ, Spitzer C, Barnow S. Testing the biosocial model of borderline personality disorder: Results of a prospective 5-year longitudinal study. Personality and Mental Health. 2011;5(1):29–42. [Google Scholar]
- Ayers W, Haslam N, Bernstein DP, Tryon WT, Handelsman L. Categorical vs Dimensional models of personality disorders in substance abusers: A taxometric analysis; Annual Meeting of American Psychiatric Association.1999. [Google Scholar]
- Ball JS, Links PS. Borderline personality disorder and childhood trauma: evidence for a causal relationship. Current Psychiatry Reports. 2009;11(1):63–68. doi: 10.1007/s11920-009-0010-4. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge C, Gatzke-Kopp L. Multifinality in the development of personality disorders: A biology × sex × environment interaction model of antisocial and borderline traits. Development and Psychopathology. 2009;21(3):735–770. doi: 10.1017/S0954579409000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begg MD, Parides MK. Separation of individual-level and cluster-level covariate effects in regression analysis of correlated data. Statistics in Medicine. 2003;22(16):2591–2602. doi: 10.1002/sim.1524. [DOI] [PubMed] [Google Scholar]
- Bemmels HR, Burt SA, Legrand LN, Iacono WG, McGue M. The heritability of life events: An adolescent twin and adoption study. Twin Research and Human Genetics. 2008;11(3):257–265. doi: 10.1375/twin.11.3.257. [DOI] [PubMed] [Google Scholar]
- Bergen SE, Gardner CO, Kendler KS. Age-related changes in heritability of behavioral phenotypes over adolescence and young adulthood: A meta-analysis. Twin Research and Human Genetics. 2007;10(3):423–433. doi: 10.1375/twin.10.3.423. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Gratz KL, Delany-Brumsey A, Paulson A, Lejuez CW. Temperamental and environmental risk factors for borderline personality disorder among inner-city substance users in residential treatment. Journal of Personality Disorders. 2006;20(3):218–231. doi: 10.1521/pedi.2006.20.3.218. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Iacono WG, McGue M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: A longitudinal twin study. Development and Psychopathology. 2009;21(4):1335–1353. doi: 10.1017/S0954579409990186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Iacono WG, McGue M. Familia transmission and heritability of childhood disruptive disorders. American Journal of Psychiatry. 2010;167:1066–1074. doi: 10.1176/appi.ajp.2010.09091272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Patrick CJ, Iacono WG, McGue M. Development and validation of the Minnesota Borderline Personality Disorder scale. Assessment. 2011;18(2):234–252. doi: 10.1177/1073191111398320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley R, Jenei J, Westen D. Etiology of borderline personality disorder - Disentangling the contributions of intercorrelated antecedents. Journal of Nervous and Mental Disease. 2005;193(1):24–31. doi: 10.1097/01.nmd.0000149215.88020.7c. [DOI] [PubMed] [Google Scholar]
- Burt SA, Krueger RF, McGue M, Iacono WG. Sources of covariation among attention-deficit/hyperactivity disorder, oppositional defiant disorder, and conduct disorder: The importance of shared environment. Journal of Abnormal Psychology. 2001;110(4):516–525. doi: 10.1037/0021-843X.110.4.516. [DOI] [PubMed] [Google Scholar]
- Burt SA, Krueger RF, McGue M, Iacono WG. Parent-child conflict and the comorbidity among childhood externalizing disorders. Archives of General Psychiatry. 2003;60(5):505–513. doi: 10.1001/archpsyc.60.5.505. [DOI] [PubMed] [Google Scholar]
- Burt SA, McGue M, Iacono WG, Krueger RF. Differential parent-child relationships and adolescent externalizing symptoms: Cross-lagged analyses within a monozygotic twin differences design. Developmental Psychology. 2006;42(6):1289–1298. doi: 10.1037/0012-1649.42.6.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt SA, McGue M, Krueger RF, Iacono WG. How are parent-child conflict and childhood externalizing symptoms related over time? Results from a genetically informative cross-lagged study. Development and Psychopathology. 2005a;17(01):145–165. doi: 10.1017/S095457940505008X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt SA, McGue M, Krueger RF, Iacono WG. Sources of covariation among the child-externalizing disorders: informant effects and the shared environment. Psychological Medicine. 2005b;35(8):1133–1144. doi: 10.1017/S0033291705004770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson EA, Egeland B, Sroufe LA. A prospective investigation of the development of borderline personality symptoms. Development and Psychopathology. 2009;21(4):1311–1334. doi: 10.1017/S0954579409990174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheavens JS, Zachary Rosenthal M, Daughters SB, Nowak J, Kosson D, Lynch TR, et al. An analogue investigation of the relationships among perceived parental criticism, negative affect, and borderline personality disorder features: the role of thought suppression. Behaviour Research and Therapy. 2005;43(2):257–268. doi: 10.1016/j.brat.2004.01.006. [DOI] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: elaborating and extending Linehan’s theory. Psychological Bulletin. 2009;135(3):495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley TJ, Mikulich SK, Ehlers KM, Hall SK, Whitmore EA. Discriminative validity and clinical utility of an abuse-neglect interview for adolescents with conduct and substance use problems. American Journal of Psychiatry. 2003;160(8):1461–1469. doi: 10.1176/appi.ajp.160.8.1461. [DOI] [PubMed] [Google Scholar]
- Derringer J, Krueger RF, Irons DE, Iacono WG. Harsh discipline, childhood sexual assault, and MAOA genotype: An investigation of main and interactive effects on diverse clinical externalizing outcomes. Behavior Genetics. 2010;40(5):639–648. doi: 10.1007/s10519-010-9358-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinwiddie S, Heath AC, Dunne MP, Bucholz KK, Madden PAF, Slutske WS, et al. Early sexual abuse and lifetime psychopathology: A co-twin-control study. Psychological Medicine. 2000;30(1):41–52. doi: 10.1017/s0033291799001373. [DOI] [PubMed] [Google Scholar]
- Distel MA, Middeldorp CM, Trull TJ, Derom CA, Willemsen G, Boomsma DI. Life events and borderline personality features: the influence of gene-environment interaction and gene-environment correlation. Psychological Medicine. 2011;41(4):849–860. doi: 10.1017/S0033291710001297. [DOI] [PubMed] [Google Scholar]
- Distel MA, Trull TJ, Derom CA, Thiery EW, Grimmer MA, Martin NG, et al. Heritability of borderline personality disorder features is similar across three countries. Psychological Medicine. 2008;38(9):1219–1229. doi: 10.1017/S0033291707002024. [DOI] [PubMed] [Google Scholar]
- Edens JF, Marcus DK, Ruiz MA. Taxometric analyses of borderline personality features in a large-scale male and female offender sample. Journal of Abnormal Psychology. 2008;117(3):705–711. doi: 10.1037/0021-843X.117.3.705. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Archives of General Psychiatry. 2007;64(10):1145–1152. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- Gjone H, Stevenson J, Sundet JM, Eilertsen DE. Changes in heritability across increasing levels of behavior problems in young twins. Behavior Genetics. 1996;26(4):419–426. doi: 10.1007/BF02359486. [DOI] [PubMed] [Google Scholar]
- Golier J, Yehuda R, Bierer L, Mitropoulou V, New AS, Schmeidler J, et al. The relationship of borderline personality disorder to posttraumatic stress and traumatic events. American Journal of Psychiatry. 2003;160:2018–2024. doi: 10.1176/appi.ajp.160.11.2018. [DOI] [PubMed] [Google Scholar]
- Grant B, Chou S, Goldstein R, Huang B, Stinson F, Saha T, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinincal Psychology. 2008;69:533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Reynolds EK, Bagge CL, Latzman RD, Daughters SB, et al. Extending extant models of the pathogenesis of borderline personality disorder to childhood borderline personality symptoms: The roles of affective dysfunction, disinhibition, and self- and emotion-regulation deficits. Development and Psychopathology. 2009;21(4):1263–1291. doi: 10.1017/S0954579409990150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson RF, Self-Brown S, Fricker-Elhai AE, Kilpatrick DG, Saunders BE, Resnick HS. The relations between family environment and violence exposure among youth: Findings from the national survey of adolescents. Child Maltreatment. 2006;11(1):3–15. doi: 10.1177/1077559505279295. [DOI] [PubMed] [Google Scholar]
- Hicks BM, DiRago AC, Iacono WG, McGue M. Gene-environment interplay in internalizing disorders: consistent findings across six environmental risk factors. Journal of Child Psychology and Psychiatry. 2009;50(10):1309–1317. doi: 10.1111/j.1469-7610.2009.02100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks BM, Durbin CE, Blonigen DM, Iacono WG. Relationship between personality change and the onset and course of alcohol dependence in young adulthood. Addiction. 2011;107:540–548. doi: 10.1111/j.1360-0443.2011.03617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks BM, Krueger RF, Iacono WG, McGue M, Patrick CJ. Family transmission and heritability of externalizing disorders - A twin-family study. Archives of General Psychiatry. 2004;61(9):922–928. doi: 10.1001/archpsyc.61.9.922. [DOI] [PubMed] [Google Scholar]
- Hicks BM, South SC, DiRago AC, Iacono WG, McGue M. Environmental adversity and increasing genetic risk for externalizing disorders. Archives of General Psychiatry. 2009;66(6):640–648. doi: 10.1001/archgenpsychiatry.2008.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Morey LC, Edelen MO, Shea MT, Grilo CM, Sanislow CA, et al. A comparison of interview and self-report methods for the assessment of borderline personality disorder criteria. Psychological Assessment. 2008;20(1):81–85. doi: 10.1037/1040-3590.20.1.81. [DOI] [PubMed] [Google Scholar]
- Huibregtse BM, Bornovalova MA, Hicks BM, McGue M, Iacono WG. Testing the causal role of adolescent sexual initiation in later-life sexual risk behavior: A longitudinal twin design. Psychological Science. 2011;22:924–933. doi: 10.1177/0956797611410982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussey JM, Chang JJ, Kotch JB. Child maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatrics. 2006;118(3):933–942. doi: 10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-case disorders: Findings from the Minnesota Twin Family Study. Development and Psychopathology. 1999;11(4):869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Malone SM, McGue M. Behavioral dishinhibition and the development of early-onset addiction: Common and specific influences. Annual Review of Clinical Psychology. 2008;4:325–348. doi: 10.1146/annurev.clinpsy.4.022007.141157. [DOI] [PubMed] [Google Scholar]
- Irish L, Kobayashi I, Delahanty DL. Long-term physical health consequences of childhood sexual abuse: A meta-analytic review. Journal of Pediatric Psychology. 2010;35(5):450–461. doi: 10.1093/jpepsy/jsp118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffee SR, Price TS. Gene-environment correlations: A review of the evidence and implications for prevention of mental illness. Molecular Psychiatry. 2007;12(5):432–442. doi: 10.1038/sj.mp.4001950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffee SR, Caspi A, Moffitt TE, Taylor A. Physical maltreatment victim to antisocial child: Evidence of an environmentally mediated process. Journal of Abnormal Psychology. 2004;113(1):44–55. doi: 10.1037/0021-843X.113.1.44. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Brown J, Smailes EM, Bernstein DP. Childhood maltreatment increases risk for personality disorders during early adulthood. Archives of General Psychiatry. 1999;56(7):600–606. doi: 10.1001/archpsyc.56.7.600. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60(9):929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Keyes MA, Malone SM, Elkins IJ, Legrand LN, McGue M, Iacono WG. The enrichment study of the minnesota twin family study: increasing the yield of twin families at high risk for externalizing psychopathology. Twin Research and Human Genetics. 2009;12(5):489–501. doi: 10.1375/twin.12.5.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klahr AM, Rueter MA, McGue M, Iacono WG, Burt SA. The relationship between parent-child conflict and adolescent antisocial behavior: confirming shared environmental mediation. Journal of Abnormal Child Psychology. 2011;39(5):683–694. doi: 10.1007/s10802-011-9505-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laporte L, Guttman H. Traumatic childhood experiences as risk factors for borderline and other personality disorders. Journal of Personality Disorders. 1996;10(3):247–259. [Google Scholar]
- Lejuez CW, Daughters SB, Nowak JA, Lynch T, Rosenthal MZ, Kosson D. Examining the inventory of interpersonal problems as a tool for conducting analogue studies of mechanisms underlying borderline personality disorder. Journal of Behavior Therapy and Experimental Psychiatry. 2003;34:313–324. doi: 10.1016/j.jbtep.2003.11.002. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. Guilford Press; New York,NY: 1993. [Google Scholar]
- Lyons MJ, Goldberg J, Eisen SA, True W, Tsuang MT, Meyer JM, et al. Do genes influence exposure to trauma? A twin study of combat. American Journal of Medical Genetics. 1993;48(1):22–27. doi: 10.1002/ajmg.1320480107. [DOI] [PubMed] [Google Scholar]
- MacMillan HL, Fleming JE, Troome N, Boyle MH, Wong M, Racine YA, et al. Prevalence of child physical and sexual abuse in the community - Results from the Ontario health supplement. Jama-Journal of the American Medical Association. 1997;278(2):131–135. [PubMed] [Google Scholar]
- Markon KE, Chmielewski M, Miller CJ. The Reliability and Validity of Discrete and Continuous Measures of Psychopathology: A Quantitative Review (vol 137, pg 856, 2011) Psychological Bulletin. 2011;137(6):1093–1093. doi: 10.1037/a0023678. [DOI] [PubMed] [Google Scholar]
- McGue M, Osler M, Christensen K. Causal inference and observational aging research: the utility of twins. Perspectives in Psychological Science. 2010;5:546–556. doi: 10.1177/1745691610383511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean LM, Gallop R. Implications of childhood sexual abuse for adult borderline personality disorder and complex posttraumatic stress disorder. American Journal of Psychiatry. 2003;160(2):369–371. doi: 10.1176/appi.ajp.160.2.369. [DOI] [PubMed] [Google Scholar]
- Morey LC. Personality Assessment Inventory: Professional manual. Psychological Assessment Resources; Odessa, FL: 1991. [Google Scholar]
- Neale MC, Cardon LR. Methodology For Genetic Studies of Twins and Families. Kluwer Academic Publishers; Dordrecht: 1992. [Google Scholar]
- Neale MC, Boker SM, Xie G, Maes HH. Mx: Statistical modelling. 6th ed. Department of Psychiatry; Richmond, VA: 2002. [Google Scholar]
- Nelson EC, Heath AC, Madden PAF, Cooper ML, Dinwiddie SH, Bucholz KK, et al. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes - Results from a twin study. Archives of General Psychiatry. 2002;59(2):139–145. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- Oltmanns TF, Turkheimer E. Person perception and personality pathology. Current Directions in Psychological Science. 2009;18(1):32–36. doi: 10.1111/j.1467-8721.2009.01601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paris J. Chronic suicidality among patients with borderline personality disorder. Psychiatric Services. 2002;53(6):738–742. doi: 10.1176/appi.ps.53.6.738. [DOI] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M. Structured Interview for DSM-IV Personality (SIDP-IV) American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- Pilkonis P, Yookung K, Proietti JM, Barkham M. Scales for personality disorders developed from the Inventory of Interpersonal Problems. Journal of Personality Disorders. 1996;10:355–369. [Google Scholar]
- Plomin R, DeFries JC, Loehlin JC. Genotype-environment interaction and correlation in the analysis of human behavior. Psychological Bulletin. 1977;84(2):309–322. [PubMed] [Google Scholar]
- Raftery AE. Bayesian model selection in social research. Sociological Methodology 1995. 1995;25(25):111–163. [Google Scholar]
- Reich W, Welner Z. Revised version of the Diagnostic Interview for Children and Adolescents (DICA-R) Department of Psychiatry, Washington University School; St Louis, MO: 1988. [Google Scholar]
- Resnick HS, Falsetti SA, Kilpatrick DG, Freedy JR. Assessment of rape and other civilian trauma-related post-traumatic stress disorder: Emphasis on assessment of potentially traumatic events. In: Miller TW, editor. Stressful life events. International Universities Press; Madison: 1966. [Google Scholar]
- Rogosch FA, Cicchetti D. Child maltreatment, attention networks, and potential precursors to borderline personality disorder. Development and Psychopathology. 2005;17(4):1071–1089. doi: 10.1017/s0954579405050509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothschild L, Cleland C, Haslam N, Zimmerman M. A taxometric study of borderline personality disorder. Journal of Abnormal Psychology. 2003;112(4):657–666. doi: 10.1037/0021-843X.112.4.657. [DOI] [PubMed] [Google Scholar]
- Sansone RA, Songer DA, Miller KA. Child abuse, mental healthcare utilization, self-harm behavior, and multiple psychiatric diagnoses among inpatients with and without a borderline diagnosis. Comprehensive Psychiatry. 2005;46:117–120. doi: 10.1016/j.comppsych.2004.07.033. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS ® 9.2 CDISC Procedure: User’s Guide. SAS Institute Inc; Cary, NC: 2008. [Google Scholar]
- Scarr S, McCartney K. How people make their own environments: A theory of genotype-> environment effects. Child Development. 1983;54(2):424–435. doi: 10.1111/j.1467-8624.1983.tb03884.x. [DOI] [PubMed] [Google Scholar]
- Scher CD, Forde DR, McQuaid JR, Stein MB. Prevalence and demographic correlates of childhood maltreatment in an adult community sample. Child Abuse & Neglect. 2004;28(2):167–180. doi: 10.1016/j.chiabu.2003.09.012. [DOI] [PubMed] [Google Scholar]
- Schulz-Heik RJ, Rhee SH, Silvern LE, Haberstick BC, Hopfer C, Lessem JM, et al. The association between conduct problems and maltreatment: testing genetic and environmental mediation. Behavior Genetics. 2010;40(3):338–348. doi: 10.1007/s10519-009-9324-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shearer SL. Phenomenology of self-injury among inpatient women with borderline personality disorders. Journal of Nervous and Mental Disease. 1994;182(9):524–526. [PubMed] [Google Scholar]
- Sher KJ, Gershuny BS, Peterson L, Raskin G. The role of childhood stressors in the intergenerational transmission of alcohol use disorders. Journal of Studies on Alcohol. 1997;58(4):414–427. doi: 10.15288/jsa.1997.58.414. [DOI] [PubMed] [Google Scholar]
- Sherman D, McGue M, Iacono WG. Twin concordance for attention deficit hyperactivity disorder: A comparison of teacher’s and mother’s reports. American Journal of Psychiatry. 1997;155:532–535. doi: 10.1176/ajp.154.4.532. [DOI] [PubMed] [Google Scholar]
- Silk KR, Lee S, Hill EM, Lohr NE. Borderline personality disorder symptoms and severity of sexual abuse. American Journal of Psychiatry. 1995;152(7):1059–1064. doi: 10.1176/ajp.152.7.1059. [DOI] [PubMed] [Google Scholar]
- Silverman AB, Reinherz HZ, Giaconia RM. The long-term sequelae of child and adolescent abuse: A longitudinal community study. Child Abuse & Neglect. 1996;20(8):709–723. doi: 10.1016/0145-2134(96)00059-2. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ. The borderline diagnosis I: psychopathology, comorbidity, and personality structure. Biological Psychiatry. 2002;51(12):936–950. doi: 10.1016/s0006-3223(02)01324-0. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological methodology. Jossey-Bass; San Francisco: 1982. pp. 290–312. [Google Scholar]
- Spearman C. The Proof and Measurement of Association between Two Things. The American Journal of Psychology. 1904;15(1):72–101. [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. The structured clinical interview for DSM-III-R (SCID) I: History, rationale, and description. Archives of General Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbons M, First MB. Structured clinical interview for DSM-III-R personality disorders (SCID II) Biometrics Research Division, New York State Psychiatric Institute; NY: 1987. [Google Scholar]
- Sprague J, Verona E. Emotional conditions disrupt behavioral control among individuals with dysregulated personality traits. Journal of Abnormal Psychology. 2010;119(2):409–419. doi: 10.1037/a0019194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprague J, Javdani S, Sadeh N, Newman JP, Verona E. Borderline personality disorder as a female phenotypic expression of psychopathy. Personality Disorders: Theory, Research, and Treatment. 2011;11:1–13. doi: 10.1037/a0024134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer KW, Sheridan J, Kuo D, Carnes M. Long-term physical and mental health consequences of childhood physical abuse: Results from a large population-based sample of men and women. Child Abuse & Neglect. 2007;31(5):517–530. doi: 10.1016/j.chiabu.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MB, Jang KL, Taylor S, Vernon PA, Livesley WJ. Genetic and environmental influences on trauma exposure and posttraumatic stress disorder symptoms: A twin study. American Journal of Psychiatry. 2002;159(10):1675–1681. doi: 10.1176/appi.ajp.159.10.1675. [DOI] [PubMed] [Google Scholar]
- Tellegen A. Brief manual for the Multidimensional Personality Questionnaire. Minneapolis, MN: 1982. Unpublished manuscript. [Google Scholar]
- Thapar A, McGuffin P. Genetic influences on life events in childhood. Psychological Medicine. 1996;26(4):813–820. doi: 10.1017/s0033291700037831. [DOI] [PubMed] [Google Scholar]
- Thapar A, Harold G, McGuffin P. Life events and depressive symptoms in childhood - Shared genes or shared adversity? A research note. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1998;39(8):1153–1158. [PubMed] [Google Scholar]
- Torgersen S, Czajkowski N, Jacobson K, Reichborn-Kjennerud T, Roysamb E, Neale MC, et al. Dimensional representations of DSM-IV cluster B personality disorders in a population-based sample of Norwegian twins: A multivariate study. Psychological Medicine. 2008;38(11):1617–1625. doi: 10.1017/S0033291708002924. [DOI] [PubMed] [Google Scholar]
- Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Archives of General Psychiatry. 2001;58(6):590–596. doi: 10.1001/archpsyc.58.6.590. [DOI] [PubMed] [Google Scholar]
- Trull TJ. Structural relations between borderline personality disorder features and putative etiological correlates. Journal of Abnormal Psychology. 2001;110(3):471–481. doi: 10.1037//0021-843x.110.3.471. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Widiger TA, Lynam DR, Costa PT. Borderline personality disorder from the perspective of general personality functioning. Journal of Abnormal Psychology. 2003;112(2):193–202. doi: 10.1037/0021-843x.112.2.193. [DOI] [PubMed] [Google Scholar]
- Wagner S, Baskaya O, Dahmen N, Lieb K, Tadic A. Modulatory role of the brain-derived neurotrophic factor Val(66)Met polymorphism on the effects of serious life events on impulsive aggression in borderline personality disorder. Genes Brain and Behavior. 2010;9(1):97–102. doi: 10.1111/j.1601-183X.2009.00539.x. [DOI] [PubMed] [Google Scholar]
- Wagner S, Baskaya O, Lieb K, Dahmen N, Tadic A. The 5-HTTLPR polymorphism modulates the association of Serious Life Events and impulsivity in patients with borderline personality disorder. Pharmacopsychiatry. 2009;42(5):246–246. doi: 10.1016/j.jpsychires.2009.03.004. [DOI] [PubMed] [Google Scholar]
- Wagner S, Baskaya O, Lieb K, Dahmen N, Tadic A. Lack of modulating effects of the COMT Val(158)Met polymorphism on the association of serious life events (SLE) and impulsivity in patients with borderline personality disorder. Journal of Psychiatric Research. 2010;44(2):121–122. doi: 10.1016/j.jpsychires.2009.06.008. [DOI] [PubMed] [Google Scholar]
- Walden B, McGue M, Iacono WG, Burt SA, Elkins I. Identifying shared environmental contributions to early substance use: The respective roles of peers and parents. Journal of Abnormal Psychology. 2004;113(3):440–450. doi: 10.1037/0021-843X.113.3.440. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Negative affectivity: The disposition to experience negative aversive emotional states. Psychological Bulletin. 1984;96(3):465–490. [PubMed] [Google Scholar]
- Widom CS, Czaja SJ, Paris J. A prospective investigation of borderline personality disorder in abused and neglected children followed up into adulthood. Journal of Personality Disorders. 2009;23(5):433–446. doi: 10.1521/pedi.2009.23.5.433. [DOI] [PubMed] [Google Scholar]
- Wilberg T, Urnes O, Friis S, Pedersen G, Karterud S. Borderline and avoidant personality disorders and the five-factor model of personality: A comparison between DSM-IV diagnoses and NEO-PI-R. Journal of Personality Disorders. 1999;13(3):226–240. doi: 10.1521/pedi.1999.13.3.226. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea MT, Battle CL, Johnson DM, Zlotnick C, Dolan-Sewell R, et al. Traumatic exposure and posttraumatic stress disorder in borderline, schizotypal, avoidant, and obsessive-compulsive personality disorders: Findings from the collaborative longitudinal personality disorders study. Journal of Nervous and Mental Disease. 2002;190(8):510–518. doi: 10.1097/00005053-200208000-00003. [DOI] [PubMed] [Google Scholar]
- Zanarini MC. Childhood experiences associated with the development of borderline personality disorder. Psychiatric Clinics of North America. 2000;23(1):89–101. doi: 10.1016/s0193-953x(05)70145-3. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR. Pathways to the development of borderline personality disorder. Journal of Personality Disorders. 1997;11(1):93–104. doi: 10.1521/pedi.1997.11.1.93. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis II comorbidity of borderline personality disorder. Comprehensive Psychiatry. 1998;39(5):296–302. doi: 10.1016/s0010-440x(98)90038-4. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Yong L, Frankenburg FR, Hennen J, Reich DB, Marino MF, et al. Severity of reported childhood sexual abuse and its relationship to severity of borderline psychopathology and psychosocial impairment among borderline inpatients. Journal of Nervous and Mental Disease. 2002;190(6):381–387. doi: 10.1097/00005053-200206000-00006. [DOI] [PubMed] [Google Scholar]