Abstract
Patients with multiple myeloma are at an increased risk of venous thromboembolism and arterial thrombosis. We assessed the impact of venous and arterial thrombosis on survival in a population-based study of 9,399 multiple myeloma patients diagnosed in Sweden from 1987 to 2005. We found multiple myeloma patients with venous thromboembolism to have a higher mortality at 1-, 5-, and 10-years of follow up compared with those without, with hazard ratios of 2.9 (95% confidence interval (CI) 2.4-3.5), 1.6 (95% CI: 1.5-1.8), and 1.6 (95% CI: 1.4-1.7), respectively. There was an increase in risk of death among multiple myeloma patients with arterial thrombosis, with hazard ratios of 3.4 (95% CI: 3.0-3.8), 2.2 (95% CI: 2.0-2.3), and 2.1 (95% CI: 1.9-2.1), respectively. In landmark analyses at six months, early arterial but not venous thromboembolism was associated with a higher risk of death. Thus, in contrast to prior smaller studies, we found the development of thrombosis to be associated with significantly poorer survival. The prevention of thrombosis in multiple myeloma is an important goal in the management of these patients.
Key words: multiple myeloma, venous thromboembolism, survival, arterial thrombosis, thalidomide, lenalidomide, aspirin, low-molecular weight heparin, warfarin, prophylaxis
Introduction
Multiple myeloma is a plasma cell malignancy characterized by osteolytic lesions, anemia, hypercalcemia and renal failure.1 Several population-based studies have shown that overall survival of patients with multiple myeloma has improved since the introduction of novel agents such as the immunomodulatory drugs (IMiDs) thalidomide and lenalidomide, bortezomib, as well as high-dose melphalan with stem cell transplantation.2-5 However, during the same time period, venous thromboembolism (VTE) has been increasingly observed in patients with multiple myeloma, primarily those who were treated with thalidomide and lenalidomide, in combination with dexamethasone and/or combination chemotherapy.6-8 Recently, we showed that the risk of VTE and arterial thrombosis is increased in multiple myeloma as well as its precursor state monoclonal gammopathy of undetermined significance (MGUS), suggesting that non-treatment related factors play a role in the development of VTE in plasma cell disorders.9-10 In further support of this observation, compared to the general population, we observed a significantly higher risk of VTE in multiple myeloma patients before the introduction of the novel agents.9-10
In the general population, the occurrence of VTE is associated with a decrease in survival.11 Three studies have addressed the impact of VTE in relation to survival in multiple myeloma. In the first study, a retrospective analysis of data from a clinical trial including 668 newly diagnosed patients treated with or without thalidomide, survival was similar among patients who developed VTE compared to those who did not.12 In the second study, also a retrospective analysis of a clinical trial including 353 relapsed/refractory multiple myeloma patients treated with lenalidomide, there was again no difference in survival in relation to thromboembolic episodes.13 Lastly, in a retrospective analysis including 535 multiple myeloma patients treated with thalidomide combined with cytotoxic chemotherapy treated in different clinical trials, development of a deep vein thrombosis (DVT) was not associated with poorer survival.14
We conducted the first population-based study designed to evaluate whether thrombosis influences survival in multiple myeloma. In the largest study to date, using high-quality data from Sweden, we assessed the impact of both venous and arterial thrombosis on survival in almost 10,000 multiple myeloma patients.
Design and Methods
The details of the study population have been described previously.10 All physicians and pathologists/cytologists in Sweden are obliged by law to report each case of cancer they diagnose or treat to the centralized nationwide Swedish Cancer Registry, which has a very high diagnostic accuracy and completeness.15 Using the Swedish Cancer Registry, we identified all multiple myeloma patients diagnosed between 1987 and 2005.
The centralized Swedish Patient Registry captures information on individual patient-based discharge diagnoses and discharge listings from inpatient (since 1964) and outpatient (since 2000) care, with a very high coverage. Information on occurrence and date of arterial (coronary artery disease and cerebrovascular disease) and VTE (DVT and pulmonary embolism) was obtained. All conditions were analyzed both individually and grouped into categories. Through linkage with the Cause of Death Register and the Register of Total Population, we collected information on vital status until 31st December 2006. From the Swedish Medical Products Agency, we gathered information on the number of patients who were prescribed thalidomide and lenalidomide in Sweden during the study period.
This study was approved by the Karolinska Institutional Review Board.
Statistical analysis
To assess the impact of thrombosis on overall survival, we treated thrombosis as a time dependent covariate in Cox’s proportional hazard models and computed hazard ratios (HRs) and 95% confidence intervals (CIs) for association (PROC PHREG, SAS, version 9.1; SAS Institute). Follow-up time started at the later of diagnosis of multiple myeloma or 1st January 1987. The delayed entry was accommodated by the entry time option in PROC PHREG. Follow up ended at time of death or at time of censoring. Censoring events were emigration, and the end of the data acquisition period (31st December 2006). We analyzed 1-, 5-, and 10-year overall survival. We estimated HRs for any thrombosis, and also estimated separate effects by grouping them according to arterial thrombosis and VTE. Models were adjusted for age at diagnosis, sex and year of diagnosis. Models were stratified by sex and by year of multiple myeloma diagnosis (before or after 2000). P values for interaction are based on Wald tests.
We also performed landmark analyses in which follow up started six months after diagnosis, and assessed the impact of any thrombotic event during the first six months on overall survival. Thrombotic episodes that were diagnosed after the first six months were not considered in this analysis.
Results and Discussion
A total of 9,399 multiple myeloma patients were diagnosed in Sweden from 1987 to 2005. The median age at diagnosis was 71 years, with almost equal sex distribution. A total of 1,756 patients (mostly multiple myeloma) received thalidomide in Sweden from 2000 to 2005 compared to fewer than 100 before the year 2000. Lenalidomide was prescribed to 103 patients (mostly multiple myeloma) from 2003 to 2005. A total of 724 multiple myeloma patients developed VTE and 1,572 arterial thrombosis during follow up.
Thrombosis and risk of death
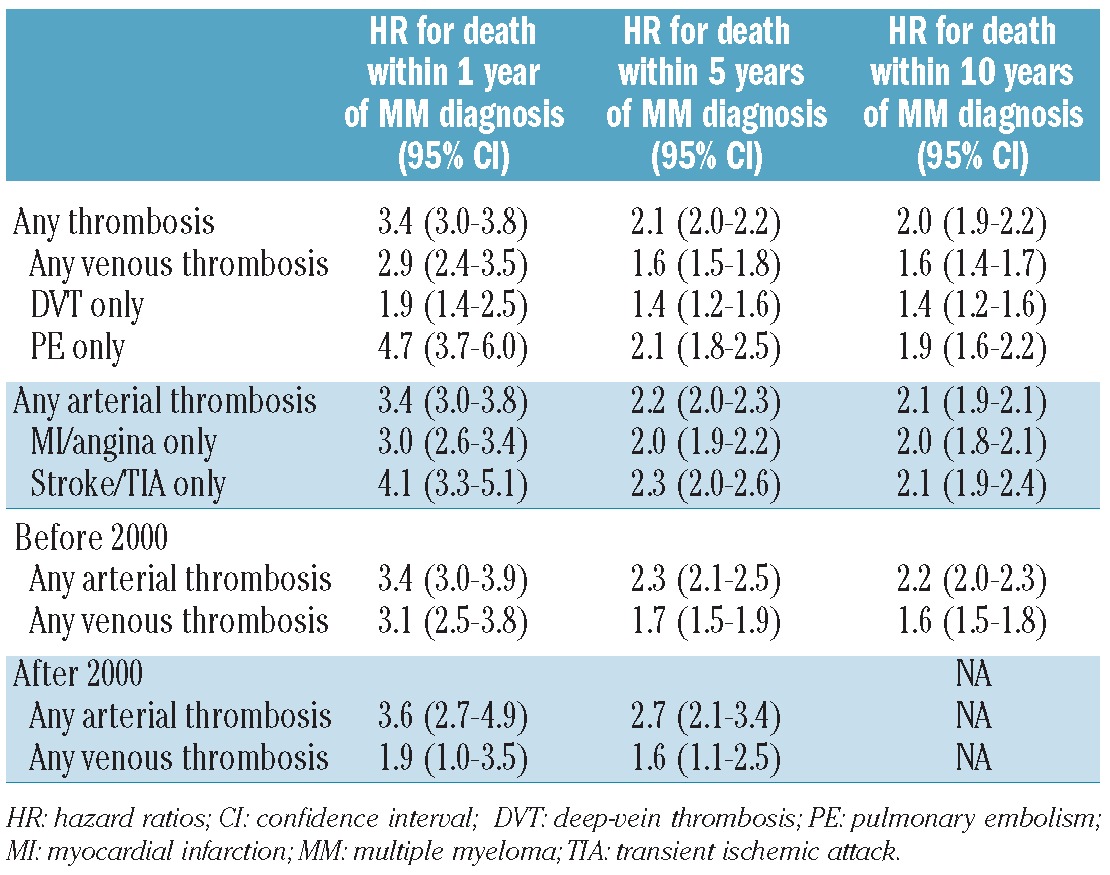
Multiple myeloma patients with any thrombosis after diagnosis had higher mortality rates compared to those without, at 1-, 5-, and 10-year follow up, with HR of 3.4 (95% CI: 3.0-3.8), HR 2.1 (95% CI: 2.0-2.2), and HR 2.0 (95% CI: 1.9-2.2), respectively (Table 1). The risk of death during the 1-, 5-, and 10-year follow up was significantly higher with diagnosis of any VTE, HR 2.9 (95% CI: 2.4-3.5), 1.6 (95% CI: 1.5-1.8), and 1.6 (95% CI: 1.4-1.7), respectively, as well as with arterial thrombosis, HR 3.4 (95% CI: 3.0-3.8), 2.2 (95% CI: 2.0-2.3), and 2.1 (95% CI: 1.9-2.1), respectively. There were no significant differences in the effect of thrombosis on mortality for multiple myeloma patients diagnosed before 2000 compared to those diagnosed after this date (Table 1), according to sex or to age of diagnosis (above/below 70 years of age). These findings are important as they confirm that thrombosis in multiple myeloma is a serious complication, increasing morbidity and even mortality, also in the era of novel anti-tumor agents.
Table 1.
Risk of death among multiple myeloma patients with thrombosis compared to those without.
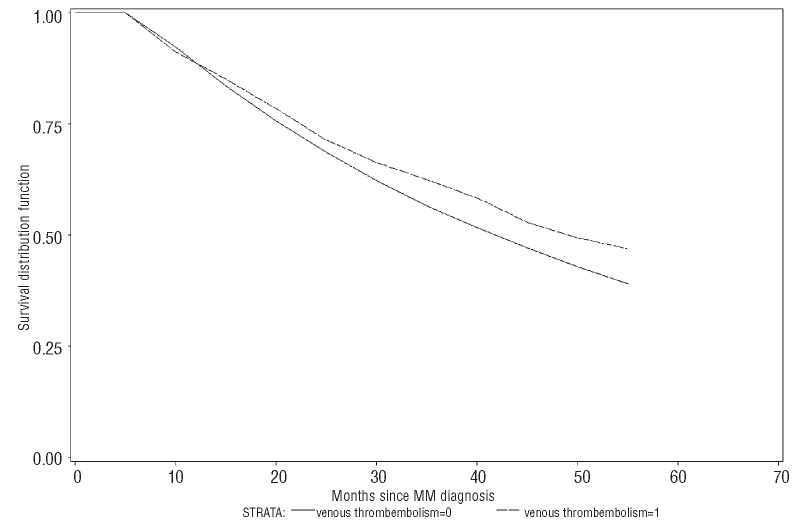
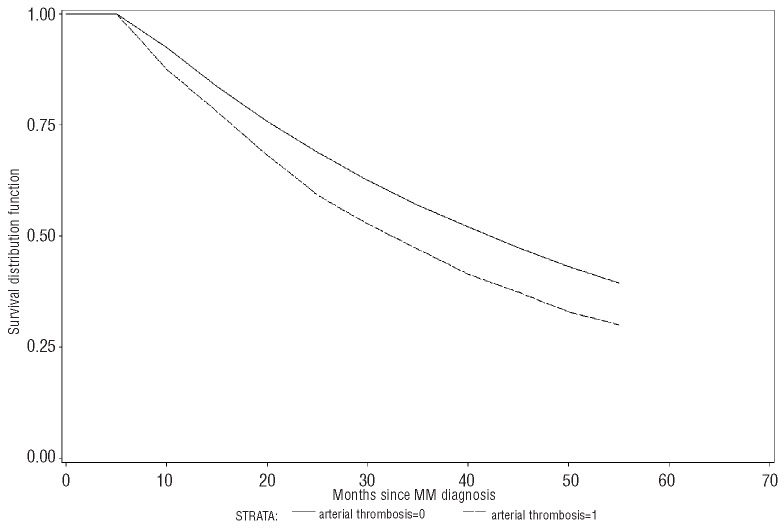
Given that a multiple myeloma patient survived the first six months following diagnosis (landmark analyses), early VTE (within six months) was not associated with a higher risk of death at one year (HR 1.4; 95% CI: 0.9-2.0), five years (HR 1.1; 95% CI: 0.9-1.3), or ten years (HR 1.0; 95% CI: 0.9-1.2) (Figure 1). In contrast, in a landmark analysis, early arterial thrombosis was associated with a significantly higher risk of death at one year (Hr 1.5; 95% CI: 1.1-2.0), five years (HR 1.4; 95% CI: 1.2-1.6), and ten years (HR 1.4; 95% CI: 1.2-1.6) (Figure 2).
Figure 1.
Survival among multiple myeloma patients with and without early venous thrombembolism (landmark analysis).
Figure 2.
Survival among multiple myeloma patients with and without early arterial thrombosis (landmark analysis).
Thrombosis is a frequent complication in patients with cancer and patients with various types of cancer have a two times higher mortality if diagnosed with VTE and three times higher during the first year.16 The occurrence of DVT or pulmonary embolism in the general population is associated with a decreased survival during the first six months, and in cases of unprovoked VTE, up to three years after diagnosis.11 Our study is the first to evaluate the impact of VTE on survival in a large population-based cohort of multiple myeloma patients. In accordance with the findings from studies on other cancers,16 we show that multiple myeloma patients with VTE have an almost 3- fold higher risk of dying within one year after diagnosis of thrombosis (compared to multiple myeloma patients without a thrombosis) and 1.6-fold higher risk within the first ten years. This is in contrast to the three previously published retrospective clinical studies based on 668, 535, and 353 patients, which reported that multiple myeloma patients with VTE have a similar survival to those without.12-14
There are some important differences between these studies and ours. Firstly, we included all patients diagnosed with multiple myeloma in a whole population and followed them for a long time period. Secondly, the other studies are based on data from clinical trials, with some patients excluded, for example, because of poor performance status and reduced cardiopulmonary function.12-13 Furthermore, two of the studies included relapsed/refractory patients and it is well known that these have a lower risk of thrombosis compared to newly diagnosed patients.17-20 Accordingly, we found the risk of death in multiple myeloma patients with VTE to be highest during the first year following diagnosis of the disease. Thirdly, the patients in two clinical trials were younger than the patients in our study (median age 57 and 63 years vs. 71 years, respectively).14,15 Age is a strong predictor for VTE and this can, therefore, influence the outcome.9,21 Finally, and perhaps most importantly, not all patients in our study were treated with thalidomide or lenalidomide as these agents were not available during the largest part of the study period. We conclude that VTE in multiple myeloma is a serious complication with a considerable impact on overall survival.
Interestingly, based on landmark analyses, survival rates for multiple myeloma patients with an early VTE who survived their first six months were similar to multiple myeloma patients without VTE during the first six months. Based on data from the Total Therapy 2 study, 95% of the VTEs were diagnosed within the first 12 months.12 In their study into the impact of VTE on survival, a 12-month landmark analysis was used and early mortality was, therefore, not evaluated. In the study based on data on relapsed/refractory multiple myeloma patients treated with lenalidomide, 96.7% of thrombotic events occurred in the first 12 months from start of treatment, and a 6-month landmark was used.15 Taken together, VTE is associated with higher mortality; however, the findings from our study, as well as those from the previously published studies, show that those patients who survive a VTE within the first 6-12 months do not seem to have a poorer survival. There are several potential mechanisms to explain these findings. Firstly, it has been suggested that the occurrence of thrombosis is partly related to the response to the treatment, and that patients who respond have an increased risk of VTE. Furthermore, the impact of low-molecular weight heparin (LMWH) on survival needs to be evaluated as this is usually used to treat VTE, and has been shown to have anti-tumoral activity.22 In addition, it is possible that multiple myeloma patients who survive their early thrombosis are in some way healthier than those who do not, introducing a bias contributing to an observed improvement in long-term survival.
This is the first study to our knowledge to evaluate the impact of arterial thrombosis on survival in multiple myeloma patients. Overall, diagnosis of arterial thrombosis was associated with a 3.4-fold higher risk of death within one year following multiple myeloma (compared to multiple myeloma patients without an arterial event) and a 2.1-fold risk within the first ten years. In contrast to VTE, we found early arterial thrombosis to be associated with a higher risk of death also in those surviving their first six months. This confirms that arterial thrombosis (myocardial infarction, angina, stroke, and TIA) is a very serious complication in multiple myeloma patients and is associated with immediate morbidity, and early and long-term mortality.23-24 One explanation might also be that patients with arterial thrombosis are treated as aggressively as other multiple myeloma patients.
Our study has several strengths, including its large size and the application of high-quality data from Sweden, a country with a stable population who had access to standardized medical care during the entire study period. In our study, we used a register-based cohort design that ensured a population-based setting and the generalizability of our findings. In a recent validation study, we reported that ascertainment and diagnostic accuracy for multiple myeloma is very high in Sweden (>90-95%).15 Study limitations are the lack of detailed clinical data, including information on anti-multiple myeloma therapy, subtype of multiple myeloma, underlying diseases and risk factors for thrombosis. Another limitation is the potential inaccuracy and lack of independent validation of thrombotic diagnosis obtained from the centralized Patient Registry.
In summary, in this large population-based study based on over 9,000 multiple myeloma patients, we found, in contrast to previously published studies, that the occurrence of any thrombosis was associated with a significantly poorer survival. Multiple myeloma patients with an early arterial or venous thrombosis had a higher risk of death than patients without. However, multiple myeloma patients with an early VTE who survived their first six months had similar survival rates to those without VTE. Therefore, our findings confirm that thrombosis in multiple myeloma patients is a serious complication, and that it increases mortality, also in the era of novel agents. It is important to investigate whether more effective prevention of thromboembolism can improve the survival of multiple myeloma patients.
Supplementary Material
Acknowledgments
the authors thank Lynn Goldin for important work in constructing the database, Ms. Shiva Ayobi, The National Board of Health and Welfare, Stockholm, Sweden; Medical Products Agency, Uppsala, Sweden; and Ms. Susanne Dahllöf, Statistics Sweden, Örebro, Sweden.
Funding: this research was supported by grants from the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and Karolinska Institutet, the Cancer Society in Stockholm, and the Intramural Research Program of the NIH, NCI. The authors thank the Medical Product Agency in Sweden.
Footnotes
Authorship and Disclosures: The information provided by the authors about contributions from persons listed as authors and in acknowledgments is available with the full text of this paper at www.haematologica.org.
Financial and other disclosures provided by the authors using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are also available at www.haematologica.org.
References
- 1.Kyle RA, Rajkumar SV. Multiple myeloma. N Engl J Med. 2004;351(18):1860-73 [DOI] [PubMed] [Google Scholar]
- 2.Waxman AJ, Mink PJ, Devesa SS, Anderson WF, Weiss BM, Kristinsson SY, et al. Racial disparities in incidence and outcome in multiple myeloma: a population-based study. Blood. 2010;116(25):5501-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Turesson I, Velez R, Kristinsson SY, Landgren O. Patterns of improved survival in patients with multiple myeloma in the twenty-first century: a population-based study. J Clin Oncol. 2010;28(5):830-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kristinsson SY, Landgren O, Dickman PW, Derolf AR, Bjorkholm M. Patterns of survival in multiple myeloma: a population-based study of patients diagnosed in Sweden from 1973 to 2003. J Clin Oncol. 2007;25(15):1993-9 [DOI] [PubMed] [Google Scholar]
- 5.Kumar SK, Rajkumar SV, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK, et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood. 2008;111(5):2516-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dimopoulos M, Spencer A, Attal M, Prince HM, Harousseau JL, Dmoszynska A, et al. Lenalidomide plus dexamethasone for relapsed or refractory multiple myeloma. N Engl J Med. 2007;357(21):2123-32 [DOI] [PubMed] [Google Scholar]
- 7.Rajkumar SV, Blood E, Vesole D, Fonseca R, Greipp PR. Phase III clinical trial of thalidomide plus dexamethasone compared with dexamethasone alone in newly diagnosed multiple myeloma: a clinical trial coordinated by the Eastern Cooperative Oncology Group. J Clin Oncol. 2006;24(3):431-6 [DOI] [PubMed] [Google Scholar]
- 8.Osman K, Comenzo R, Rajkumar SV. Deep venous thrombosis and thalidomide therapy for multiple myeloma. N Engl J Med. 2001;344(25):1951-2 [DOI] [PubMed] [Google Scholar]
- 9.Kristinsson SY, Fears TR, Gridley G, Turesson I, Mellqvist UH, Bjorkholm M, et al. Deep vein thrombosis after monoclonal gammopathy of undetermined significance and multiple myeloma. Blood. 2008;112(9):3582-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kristinsson SY, Pfeiffer RM, Bjorkholm M, Goldin LR, Schulman S, Blimark C, et al. Arterial and venous thrombosis in monoclonal gammopathy of undetermined significance and multiple myeloma: a population-based study. Blood. 2010;115(24):4991-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naess IA, Christiansen SC, Romundstad P, Cannegieter SC, Rosendaal FR, Hammerstrom J. Incidence and mortality of venous thrombosis: a population-based study. J Thromb Haemost. 2007;5(4):692-9 [DOI] [PubMed] [Google Scholar]
- 12.Zangari M, Barlogie B, Cavallo F, Bolejack V, Fink L, Tricot G. Effect on survival of treatment-associated venous thromboembolism in newly diagnosed multiple myeloma patients. Blood Coagul Fibrinolysis. 2007;18(7):595-8 [DOI] [PubMed] [Google Scholar]
- 13.Zangari M, Tricot G, Polavaram L, Zhan F, Finlayson A, Knight R, et al. Survival effect of venous thromboembolism in patients with multiple myeloma treated with lenalidomide and high-dose dexamethasone. J Clin Oncol. 2010;28(1):132-5 [DOI] [PubMed] [Google Scholar]
- 14.Zangari M, Barlogie B, Thertulien R, Jacobson J, Eddleman P, Fink L, et al. Thalidomide and deep vein thrombosis in multiple myeloma: risk factors and effect on survival. Clin Lymphoma. 2003;4(1):32-5 [DOI] [PubMed] [Google Scholar]
- 15.Turesson I, Linet MS, Bjorkholm M, Kristinsson SY, Goldin LR, Caporaso NE, et al. Ascertainment and diagnostic accuracy for hematopoietic lymphoproliferative malignancies in Sweden 1964-2003. Int J Cancer. 2007;121(10):2260-6 [DOI] [PubMed] [Google Scholar]
- 16.Sorensen HT, Mellemkjaer L, Olsen JH, Baron JA. Prognosis of cancers associated with venous thromboembolism. N Engl J Med. 2000;343(25):1846-50 [DOI] [PubMed] [Google Scholar]
- 17.Cavo M, Zamagni E, Tosi P, Cellini C, Cangini D, Tacchetti P, et al. First-line therapy with thalidomide and dexamethasone in preparation for autologous stem cell transplantation for multiple myeloma. Haematologica. 2004;89(7):826-31 [PubMed] [Google Scholar]
- 18.Zonder JA, Barlogie B, Durie BG, McCoy J, Crowley J, Hussein MA. Thrombotic complications in patients with newly diagnosed multiple myeloma treated with lenalidomide and dexamethasone: benefit of aspirin prophylaxis. Blood. 2006;108(1):403; author reply 4. [DOI] [PubMed] [Google Scholar]
- 19.Richardson PG, Schlossman RL, Weller E, Hideshima T, Mitsiades C, Davies F, et al. Immunomodulatory drug CC-5013 overcomes drug resistance and is well tolerated in patients with relapsed multiple myeloma. Blood. 2002;100(9):3063-7 [DOI] [PubMed] [Google Scholar]
- 20.Morgan GJ, Schey SA, Wu P, Srikanth M, Phekoo KJ, Jenner M, et al. Lenalidomide (Revlimid), in combination with cyclophosphamide and dexamethasone (RCD), is an effective and tolerated regimen for myeloma patients. Br J Haematol. 2007;137(3):268-9 [DOI] [PubMed] [Google Scholar]
- 21.Hansson PO, Welin L, Tibblin G, Eriksson H. Deep vein thrombosis and pulmonary embolism in the general population. 'The Study of Men Born in 1913'. Arch Intern Med. 1997;157(15):1665-70 [PubMed] [Google Scholar]
- 22.Mousa SA, Linhardt R, Francis JL, Amirkhosravi A. Anti-metastatic effect of a non-anticoagulant low-molecular-weight heparin versus the standard low-molecular-weight heparin, enoxaparin. Thromb Haemost. 2006;96(6):816-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kristinsson SY. Thrombosis in multiple myeloma. Hematology Am Soc Hematol Educ Program. 2010;2010:437-44 [DOI] [PubMed] [Google Scholar]
- 24.Libourel EJ, Sonneveld P, van der Holt B, de Maat MP, Leebeek FW. High incidence of arterial thrombosis in young patients treated for multiple myeloma: results of a prospective cohort study. Blood. 2010;116 (1):22-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.