Abstract
Asthma is a chronic inflammatory lung disease that results in airflow limitation, hyperreactivity, and airway remodeling. There is strong evidence that an imbalance between the reducing and oxidizing systems favoring a more oxidative state is present in asthma. Endogenous and exogenous reactive oxygen species, such as superoxide anion, hydroxyl radical, hypohalite radical, and hydrogen peroxide, and reactive nitrogen species, such as nitric oxide, peroxynitrite, and nitrite, play a major role in the airway inflammation and are determinants of asthma severity. Asthma is also associated with decreased antioxidant defenses, such as superoxide dismutase, catalase, and glutathione. In this review, we will summarize the current knowledge and discuss the current and future strategies for the modulation of oxidative stress in asthma.
Key Words: asthma, oxidative stress, reactive oxygen species, redox
THE LINK BETWEEN INFLAMMATION OF ASTHMA AND OXIDATIVE STRESS
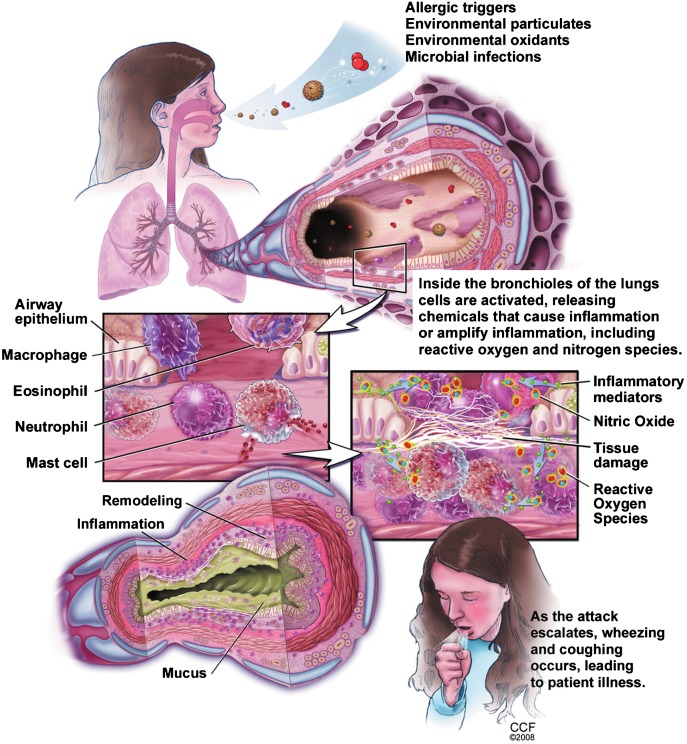
Asthma is a chronic inflammatory lung disease involving complex interactions between numerous cell types and mediators that result in airway reactivity and airflow limitation.1–5 There is strong evidence that the endogenous and exogenous reactive oxygen and nitrogen species play a major role in the airway inflammation and are determinants of asthma severity1–6 (Fig. 1).
FIGURE 1.
Asthma pathophysiology. Adapted with permission from Comhair and Erzurum.7
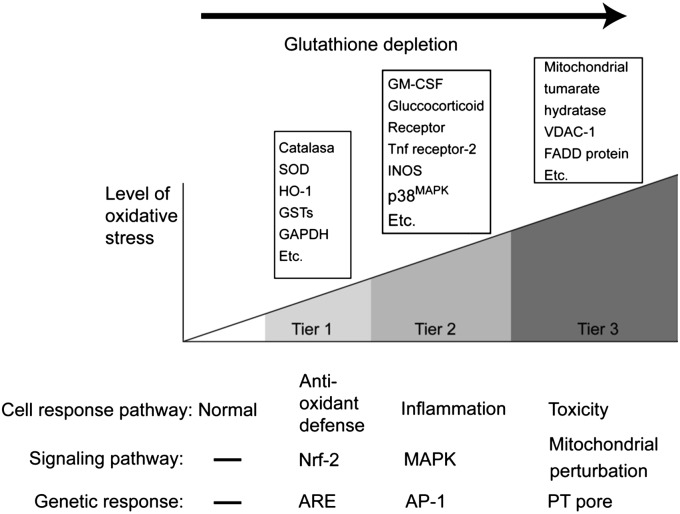
According to a recently proposed hierarchical oxidative stress model,8,9 a low level of oxidative stress, such as exposure to diesel exhaust products for 6 hours at a concentration of 10 to 50 μg/mL,10 leads to the activation of the transcription factor, nuclear erythroid 2 p45-related factor 2 (Nrf2), which encodes more than 200 genes. These gene products are responsible for a wide range of antioxidant, anti-inflammatory, cytoprotective, and detoxification functions and include catalase, superoxide dismutase (SOD)-3, heme oxygenase-1, glutathione-S-transferases, NAD(P)H-quinone oxidoreductase (NQO1), glutathione peroxidase, and glucuronosyltransferase-1a6 (UGT-1a6).11 At low level of oxidative stress, antioxidants can restore cellular redox homeostasis. When high levels of oxidative stimuli are present, additional sets of intracellular signaling cascades are triggered that are potentially proinflammatory. These include mitogen-activated protein kinase and nuclear factor-κB (NF-κB), which lead to the expression of inflammatory cytokines, chemokines, and adhesion molecules. A further increase in the level of oxidative stress could ultimately trigger a cytotoxic response originating in the mitochondria and lead to cellular apoptosis or necrosis (Fig. 2).
FIGURE 2.
The hierarchial oxidative stress model. Adapted with permission from Riedl and Nel.9
ENDOGENOUS PRODUCTION OF REACTIVE OXYGEN SPECIES AND ITS BIOLOGICAL EFFECTS IN ASTHMA
Inflammatory cells (such as activated eosinophils, neutrophils, monocytes, and macrophages) and resident cells (such as epithelial and smooth muscle cells) can generate reactive oxygen species (ROS).12–14 Sources of  include primarily nicotinamide adenine dinucleotide phosphate (NADP) oxidase–dependent complex, the cytosolic xanthine oxidase system, and the mitochondrial respiratory chain.
include primarily nicotinamide adenine dinucleotide phosphate (NADP) oxidase–dependent complex, the cytosolic xanthine oxidase system, and the mitochondrial respiratory chain.  spontaneously or enzymatically dismutates to hydrogen peroxide (H2O2). Both
spontaneously or enzymatically dismutates to hydrogen peroxide (H2O2). Both  and H2O2 interact with iron and other metal ions and form OH- in biological systems.15–17 Eosinophils, neutrophils, and monocytes contain peroxidases that catalyze the interaction between H2O2 and halides leading to the formation of hypohalides, such as HOCl. In addition, superoxide anion may also react with nitric oxide (NO) to form peroxynitrite (ONOO-), a potent ROS.13–17
and H2O2 interact with iron and other metal ions and form OH- in biological systems.15–17 Eosinophils, neutrophils, and monocytes contain peroxidases that catalyze the interaction between H2O2 and halides leading to the formation of hypohalides, such as HOCl. In addition, superoxide anion may also react with nitric oxide (NO) to form peroxynitrite (ONOO-), a potent ROS.13–17
ROS can attack proteins to form carbonyls and react with nitrogen species and tyrosine to form nitrotyrosine. In murine and human studies, tyrosine nitration was shown to increase after allergen exposure in sensitized mice or atopic asthmatic humans.18 ROS also reacts with lipids to liberate isoprostane and ethane.19–21 As a result, 8-isoprostane, a biomarker of lipid peroxidation, is elevated in the exhaled breath condensate in adults and children with asthma.20 Similar to the airways and systemic circulation, urinary levels of bromotyrosine and F2-isoprostanes are elevated in patients with asthma22 and are associated with an increased risk of having asthma.
Excess production of ROS correlates with the degree of airway hyperresponsiveness as quantified by methacholine challenge.22–24 Asthma attacks and experimental antigen challenges are both associated with immediate formation of  , being high at the sites of antigen challenge that persists throughout the late asthmatic phase.22
, being high at the sites of antigen challenge that persists throughout the late asthmatic phase.22
The main nitrogen species produced in the lung is NO. Autoxidation of NO with oxygen results in the formation of nitrite, a substrate for eosinophil peroxidase (EPO) and myeloperoxidase (MPO).25 Nitric oxide reacts with superoxide to form ONOO-, which can nitrate tyrosine residues and thus damage enzymes, and structural and functional proteins.13–15,25 Higher NO levels are associated with higher risk of asthma, asthma severity, and greater response to bronchodilator agents.22,26
A link also exists between the increase in ROS and the asthma severity. ROS production by neutrophils correlates with the severity of the reactivity of airways.27 Increased levels of EPO and MPO correlate with the numbers and activation of eosinophils and neutrophils, respectively.28–30 The level of 3-bromotyrosine, a unique product of EPO and eosinophils, was found to be 3 times higher in the bronchoalveolar lavage (BAL) fluid of individuals with asthma compared with that in the control subjects.31 In the intensive care unit, the level of 3-bromotyrosine in airways of severe asthma patients was 100-fold higher than that in individuals hospitalized for nonasthma causes.32 MPO-mediated oxidation is also related to asthma severity.30 Two to 3-fold elevations in chlorotyrosine are detected from allergen-challenged subsegments in asthmatic subjects.31 Similarly, children with asthma have increased levels of malondialdehyde, a marker of lipid peroxidation, and lower than normal levels of glutathione. Furthermore, the higher levels of malondialdehyde correlated with the severity of the asthma.33
EXPOSURE TO EXOGENOUS ROS AND ASTHMA
Respiratory system has a large surface area that is in contact with the environment. Cigarette smoke, inhalation of airborne pollutants (ozone, nitrogen dioxide, sulfur dioxide), or particulate matter in the air can trigger symptoms of asthma.34 Recently, a clear relationship between traffic density and asthma exacerbations was demonstrated.35 Ultrafine particles with a diameter of <0.1 μm may directly induce mitochondrial damage and make it difficult for the lungs to cope with oxidative stress.36 Cigarette smoke is related to asthma exacerbations, especially in young children, and there is a dose-dependent relationship between exposure to cigarette smoke and rates of asthma.37 Cigarette smoke is a highly complex mixture of more than 4000 chemical compounds that are distributed in aqueous, gas, and the tar phase of the smoke. In the gas phase, the smoke contains high concentrations of  and nitric oxide. They immediately react to form highly reactive peroxynitrite.38 The tar phase of the cigarette smoke contains organic radicals that react with molecular oxygen to form
and nitric oxide. They immediately react to form highly reactive peroxynitrite.38 The tar phase of the cigarette smoke contains organic radicals that react with molecular oxygen to form  , OH-, and H2O2. The tar phase is an effective metal chelator that chelates iron and generates H2O2 continuously. Aqueous phase of the cigarette smoke may undergo redox recycling for a period in the epithelial lining of the lungs.39
, OH-, and H2O2. The tar phase is an effective metal chelator that chelates iron and generates H2O2 continuously. Aqueous phase of the cigarette smoke may undergo redox recycling for a period in the epithelial lining of the lungs.39
IMBALANCE BETWEEN OXIDANTS AND ANTIOXIDANT SYSTEMS IN ASTHMA
Homeostasis of cellular functions during oxidative stress depends on the appropriate induction of protective antioxidant mechanisms. Antioxidants are major in vivo and in situ defense mechanisms of the cells against oxidative stress.9,13,15–17 Naturally occurring antioxidants work to protect cells and tissues against the continuous production of reactive oxygen and reactive nitrogen species during normal metabolism.40 Disequilibrium of the airway reducing state is a determinant of asthma initiation and severity.1,4–6
The nonenzymatic antioxidants include ascorbic acid, glutathione, albumin, α-tocopherol, uric acid, and β-carotene.41–44 The major enzymatic antioxidants of the lungs are SODs, catalase, and glutathione peroxidases as well as heme oxygenase-1, thioredoxins, peroxiredoxins, and glutaredoxins.41 Asthma is characterized by the loss of antioxidant activities.7
We evaluated the enzymatic and nonenzymatic antioxidant systems in children with asthma.45 Levels of the enzymes glutathione peroxidase and SOD and of the nonenzymatic components of the antioxidant system including reduced glutathione, ascorbic acid, α-tocopherol, lycopene, and β-carotene were significantly lower in children with asthma compared with the healthy controls. In addition, of the amino acids contributing to glutathione synthesis, glycine, and glutamine were significantly lower in children with asthma. The majority of the amino acids susceptible to oxidative stress displayed lower levels in children with asthma. The results of this study clearly show that childhood asthma is associated with significant decreases in various components of both enzymatic and nonenzymatic antioxidant defenses.45
Because superoxide is the primary ROS produced from a variety of sources, its dismutation by SOD is of primary importance for each cell. All 3 forms of SOD (CuZn-SOD, Mn-SOD, and EC-SOD) are widely expressed in the human lung.46,47 SOD activity is significantly lower in epithelial lining fluid and airway epithelial cells in asthma patients compared with that in the healthy controls.7 Studies in large populations showed that the airway reactivity is inversely related to SOD activity.5,48 Transgenic mice that overexpress SOD had decreased allergen-induced physiologic changes in the airways compared with controls.49 It seems that the lower SOD activity is partly a consequence of the increased oxidative and nitrative stress in the asthmatic airway and serves as a sensitive marker of airway redox and asthma severity.7
In addition to lower SOD activity, CuZn-SOD protein is decreased in asthmatic airway epithelium.50 Oxidation and nitration of Mn-SOD are also present in the asthmatic airway, correlating with the severity of the asthma.48,51 Overall, the loss of SOD activity reflects oxidant stress in the airway.48
Catalase is a metalloprotein enzyme and the main scavenger of H2O2. It is effective in high concentrations of H2O2. Under prolonged oxidative stress, NADPH binds to the enzyme and stabilizes the structure and protects catalase from inactivation. This leads to the decrease in catalase activity.52 Both animal and human studies have shown that catalase activity in BAL fluid is lower in patients with asthma as compared with that in healthy controls.53 The lower catalase activity is due to nitration and oxidation, which identifies oxidative inactivation as the mechanism of activity loss in vivo.53
Extracellular glutathione peroxidase is higher than normal in the lungs of patients with asthma. Although ozone decreased the levels of glutathione peroxidase protein and activity, no change was detected with exposure to NO2.6,54 During acute asthma exacerbations, glutathione levels in the exhaled breath condensate of children were found to be lower than those in the control subjects. In addition, the glutathione levels in exhaled breath condensate increased after oral steroid treatment compared with pretreatment levels.55 Glutathione depletion leads to the inhibition of Th1-associated cytokine production and favors Th2-associated response.56 In other words, reduction in glutathione levels supports the maintenance of Th2 response in asthma.
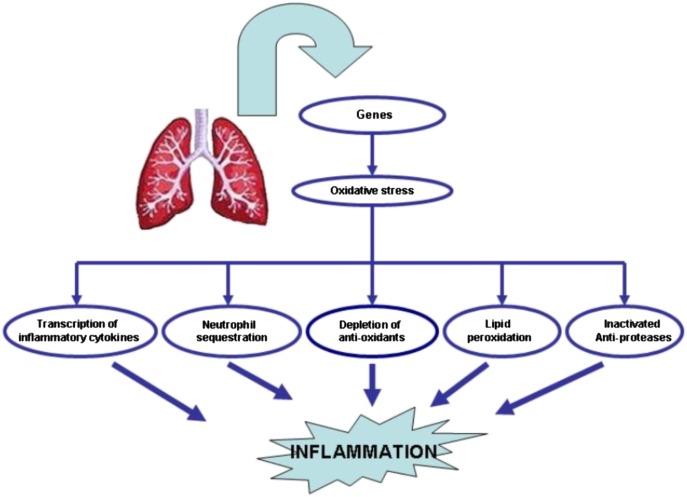
GENES AND OXIDATIVE STRESS IN ASTHMA
Glutathione S-transferases (GST) include a number of subclasses, such as GST-P1 and GST-M1, that are expressed in the lungs and have been implicated in the pathogenesis of asthma. Children with GSTM1 null or GSTP1 val/val genotypes had increased respiratory symptoms upon exposure to ozone.33,57,58 The same genotypes were associated with higher nasal IgE and histamine response.59 Because these polymorphisms have a high frequency,60 they may have a substantial effect at the population level. GSTCD gene at 4q24 location was identified as one of the primary genes that determine lung function.61
We genotyped patients with asthma and healthy individuals for null variants of GSTT1 and GSTM1 and ile105val variant of GSTP1. Children with asthma possessing the GSTP1 val/val genotype had higher malondialdehyde and lower glutathione levels compared with other genotypes in the systemic circulation but not in the airways.33,62 This particular genotype was independently associated with the severity of childhood asthma.
Similar genetic effects have been reported for SOD. Ala16Val mutation in Mn-SOD changes the secondary structure of the protein, which may affect the targeting of the protein to mitochondria.63 The EC-SOD R213G polymorphism is associated with reduced exacerbations in chronic obstructive pulmonary disease (COPD) and lower rates of hospitalization.64 However, neither R213G (EC-SOD) nor Ala16Val of Mn-SOD was associated with a genetic susceptibility to develop asthma.63 This is an area that needs further research (Fig. 3).
FIGURE 3.
Genetic polymorphisms lead to pathophysiological changes that result in the inflammation of the airways.
CLINICAL MONITORING OF OXIDATIVE STRESS IN ASTHMA
Oxidants are produced at higher amounts either spontaneously or after the stimulation in patients with asthma compared with healthy subjects. EPO and MPO are increased in the peripheral blood, induced sputum, and BAL fluid of patients with asthma.65–68 Many direct or indirect markers of oxidative stress, including malondialdehyde, thiobarbituric acid, and glutathione disulfide, have been found in urine, plasma, sputum, and BAL fluid of patients with asthma, and the level of the markers correlated with the severity of the disease.67–69 Analysis of exhaled breath condensate has allowed direct measurements of H2O2 and NO and the measurement of several indirect by-products of oxidation like isoprostane and ethane.20,21 Despite the difficulties to quantify the ROS because of their labile nature, the stable end products of the reactive pathways may be used as reliable markers of oxidative stress in patients with asthma.7
One clinically useful biomarker of airway inflammation is exhaled NO.7 During an asthma exacerbation and in the case of uncontrolled asthma, the airway environment becomes more acidic and oxidizing that leads to the release of NO from S-nitrosoglutathione (GSN), which leads to high levels of exhaled NO.2
FUTURE PERSPECTIVES FOR ANTI-OXIDANT TREATMENT
Even though it is apparent that treatment modalities targeting the oxidant stress has a great potential for the treatment of many diseases including asthma, so far, human studies have failed to reveal a clear benefit.
Thiol Antioxidants
Thiol antioxidants that are metabolically converted to glutathione precursors are popular alternatives as antioxidant therapeutics. N-acetyl cysteine (NAC) is the most commonly used thiol precursor. NAC was found to suppress airway inflammation and hyperreactivity in animals70 and inhibit ROS production in human peripheral blood eosinophils.71 In animal models, oral NAC exerted an antioxidant protective effect and attenuated pulmonary inflammation.70,72
In humans, according to meta-analyses, NAC is able to decrease the exacerbation rate in patients with COPD by more than 20%.73–75 However, in a controlled randomized study, NAC was found to be ineffective in preventing the deterioration in lung function and exacerbations in patients with COPD.76 In a recent study, NAC produced no significant benefit when added to conventional treatment during an asthma attack.77 The lack of clear benefit in human studies may be related to the relative instability of NAC.78,79
In addition to NAC, a more potent and orally available thiol antioxidant is bucillamine. It stimulates the production of precursors necessary for glutathione synthesis and induces Nrf2 release into the nucleus. Thus, it might function as Nrf2 agonist.80 Bucillamine was shown to be safe in humans but not tested yet for the reduction of oxidative stress in the respiratory system of patients.81
Vitamins and Nutrients
The results of the studies evaluating the effects of vitamins and nutrients on asthma have been controversial.82–88 In a murine study, it was shown that the administration of vitamins C and E caused decreases in ragweed extract–induced ROS levels and is associated with lower airway allergic inflammation.82 In an ovalbumin-sensitized rat model, 4 days of oral treatment with γ-tocopherol diminished eosinophil infiltration in the nose, sinuses, and nasolacrimal duct but not in the lung after allergen challenge.83
Even though epidemiological studies have suggested that children with low dietary intake of vitamins and C E, and other antioxidants have in general more symptoms,85,89 the results of the clinical studies have been largely disappointing.86–88 Interestingly, a recent study has even suggested that vitamin supplements may increase the oxidant stress. In this study, the investigators have hypothesized that the intake of antioxidant vitamins would augment the beneficial effects of exercise in patients with type 2 diabetes. In contrast to their expectations, the results have shown that daily supplementation with vitamin C and vitamin A for 4 weeks not only failed to improve the insulin responsiveness but also decreased the expression of ROS-sensitive transcriptional regulators, molecular mediators of ROS defense (SOD 1 and 2, glutathione peroxidase).90 Thus, antioxidant supplement seems to have blocked endogenous defenses rather than counteract the oxidant stress. This emphasizes that exogeneous antioxidants need to block the oxidant pathways without suppressing the endogenous antioxidant mechanisms.
The Nrf2 pathway is a negative regulator of inflammation according to the hierarchical oxidative stress model.8,9 Sulforaphane is a potent Nrf2 agonist, which is found in high amounts in broccoli. Studies using human bronchial epithelial cells confirm that sulforaphane is effective in suppressing the proinflammatory effects of diesel exhaust particles. It effectively upregulates GSTM1 and blocks interleukin (IL)-8, granulocyte-macrophage colony-stimulating factor (GM-CSF), IL-1β production in the bronchial epithelial cells.91
Quercetin is a flavonoid molecule found in a variety of foods especially in apples and has antioxidant and anti-inflammatory properties.92,93 Quercetin was shown to inhibit proinflammatory cytokines and NO production through MAP kinases and NF-κB pathway in lipopolysaccharide-stimulated cells.93 Dietary intake of the soy isoflavone genistein was associated with reduced allergic respiratory symptoms.94 In animal models, genistein blocks allergen-induced airway inflammation in ex vivo allergen-challenged guinea-pig bronchi and lung specimens. Intratracheal instillation of genistein was shown to reduce leukotriene and histamine levels.89 In support of these studies, asthma patients with high dietary genistein consumption had less severe airflow obstruction than those who consume little or no genistein.95
α-Lipoic acid is a nonenzymatic antioxidant and is present in various foods and oral supplements. In an animal model, α-lipoic acid treatment was associated with reduced airway hyperresponsiveness, lower eosinophil counts, and IL-4 and IL-5 concentrations in BAL, improved pathology of the lungs, and lower intracellular ROS and NF-κB DNA-binding activity.96 Recently, Metha et al84 reported that choline and α-lipoic acid treatment reduces ROS production and isoprostanes in BAL fluid and thus suppresses oxidative stress.
Another food derivative, epigallocatechin 3 gallate, a component of polyphenols derived from green tea, was shown to be a potent inhibitor of IL-1β–induced MUC5AC gene expression and MUC5AC secretion97 and has antioxidant activity.98
SOD Mimetics
Transgenic mice that over express SOD have decreased allergen induced physiologic changes in the airway compared with controls.49 A number of SOD mimetics have been developed possessing antioxidant properties in vivo99,100 and their benefits have been identified in animal models.101 SOD mimetic (SODm) M40403 was shown to decrease the physiological and histopathological lung abnormalities in the ovalbumin model of allergic asthma reaction in sensitized guinea pigs.101
Molecules Affecting Glutathione System
Ebselen, a nontoxic, seleno-organic drug, is an effective reductant of hydroperoxides. It mimics glutathione peroxidase. In animal models, it inhibits airway inflammation by reducing neutrophil chemotaxis and chemokine expression.102
Resveratrol, a phytoalexin found in seeds of grapes, has antioxidant and anti-inflammatory effects. It effectively inhibits oxidative damage and scavenges free radicals. It induces glutathione (GSH) synthesis and attenuates GSH depletion in lung epithelial cells during the oxidative stress.103 Most studies done thus far on resveratrol was performed on either animal models or in vitro systems. In a recent study, resveratrol blocked the release of both IL-8 and GM-CSF from alveolar macrophages of patients with COPD both at basal state and after stimulation with IL-1β and cigarette smoke.104 Resveratrol was shown to decrease IL-1 and tumor necrosis factor-α105 expression and reduce iNOS expression, COX-2 messenger RNA, and production of IL-8 and GM-CSF106 in human lung epithelial cells More studies need be done to understand how resveratrol fits into inflammatory pathways in the development of novel therapies for the treatment of asthma.
Nanomaterials
Nanotechnology provides fullerene nanomaterials, which are soccer ball–shaped carbon cages that are among the most potent free radical scavengers due to their capacity to absorb electrons. They have been shown to inhibit IgE-mediated human mast cell and peripheral blood basophils mediator release in vitro.107 The clinical applications of these products in humans have not yet been investigated.
CURRENT ASTHMA THERAPY AND OXIDATIVE STRESS
Anti-inflammatory therapy using corticosteroids remains to be the mainstay of treatment and is emphasized in all guidelines.108,109 The efficacy of current asthma therapy in preventing the effects of oxidative stress is not yet clear and sometimes controversial.
Corticosteroids may have direct effects on oxidative stress by decreasing the number and/or activity of cells involved in ROS.110 Even though some studies have suggested that they may also increase the antioxidant enzyme levels,111 this observation was not supported by others.112
Clinical studies have produced some challenging results as well. In a recent study, it was shown that patients with asthma who were well controlled with inhaled corticosteroids and long-acting β2 agonists had higher lipid peroxide levels compared with healthy controls.113 Similarly, intranasal corticosteroids failed to prevent the oxidative burden produced by intranasal ragweed allergen challenge.114 It is also important to remember that ROS may inactivate histone deacetylase-2, an essential factor for corticosteroid inhibition of the inflammatory response.115
CONCLUSION
Asthma is associated with a strong oxidant stress that is a result of both increased oxidant forces and decreased antioxidant capacity. Even though modulation of this system offers great promise in the treatment of inflammatory diseases, such as asthma, more work is needed to discover a clinically useful compound.
REFERENCES
- 1.Dweik RA, Comhair SA, Gaston B, Thunnissen FB, Farver C, et al. NO chemical events in the human airway during the immediate and late antigen-induced asthmatic response. Proc Natl Acad Sci U S A. 2001;98:2622–2627. doi: 10.1073/pnas.051629498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaston B, Drazen JM, Loscalzo J, Stamler JS. The biology of nitrogen oxides in the airways. Am J Respir Crit Care Med. 1994;149:538–551. doi: 10.1164/ajrccm.149.2.7508323. [DOI] [PubMed] [Google Scholar]
- 3.Haahtela T. Airway remodelling takes place in asthma—what are the clinical implications? Clin Exp Allergy. 1997;27:351–353. [PubMed] [Google Scholar]
- 4.Calhoun WJ, Reed HE, Moest DR, Stevens CA. Enhanced superoxide production by alveolar macrophages and air-space cells, airway inflammation, and alveolar macrophage density changes after segmental antigen bronchoprovocation in allergic subjects. Am Rev Respir Dis. 1992;145:317–325. doi: 10.1164/ajrccm/145.2_Pt_1.317. [DOI] [PubMed] [Google Scholar]
- 5.Comhair SA, Bhathena PR, Dweik RA, Kavuru M, Erzurum SC. Rapid loss of superoxide dismutase activity during antigen-induced asthmatic response. Lancet. 2000;355:624. doi: 10.1016/S0140-6736(99)04736-4. [DOI] [PubMed] [Google Scholar]
- 6.Comhair SA, Bhathena PR, Farver C, Thunnissen FB, Erzurum SC. Extracellular glutathione peroxidase induction in asthmatic lungs: evidence for redox regulation of expression in human airway epithelial cells. FASEB J. 2001;15:70–78. doi: 10.1096/fj.00-0085com. [DOI] [PubMed] [Google Scholar]
- 7.Comhair SA, Erzurum SC. Redox control of asthma: molecular mechanisms and therapeutic opportunities. Antioxid Redox Signal. 2010;12:93–124. doi: 10.1089/ars.2008.2425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li N, Hao M, Phalen RF, Hinds WC, Nel AE. Particulate air pollutants and asthma. A paradigm for the role of oxidative stress in PM-induced adverse health effects. Clin Immunol. 2003;109:250–265. doi: 10.1016/j.clim.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Riedl MA, Nel AE. Importance of oxidative stress in the pathogenesis and treatment of asthma. Curr Opin Allergy Clin Immunol. 2008;8:49–56. doi: 10.1097/ACI.0b013e3282f3d913. [DOI] [PubMed] [Google Scholar]
- 10.Li N, Alam J, Venkatesan MI, Eiguren-Fernandez A, Schmitz D, et al. Nrf2 is a key transcription factor that regulates antioxidant defense in macrophages and epithelial cells: protecting against the proinflammatory and oxidizing effects of diesel exhaust chemicals. J Immunol. 2004;1(173):3467–3481. doi: 10.4049/jimmunol.173.5.3467. [DOI] [PubMed] [Google Scholar]
- 11.Cho HY, Jedlicka AE, Reddy SP, Kensler TW, Yamamoto M, Zhang LY, Kleeberger SR. Role of NRF2 in protection against hyperoxic lung injury in mice. Am J Respir Cell Mol Biol. 2002;26:175. doi: 10.1165/ajrcmb.26.2.4501. [DOI] [PubMed] [Google Scholar]
- 12.Barnes PJ. Reactive oxygen species and airway inflammation. Free Radic Biol Med. 1990;9:235–243. doi: 10.1016/0891-5849(90)90034-g. [DOI] [PubMed] [Google Scholar]
- 13.Dworski R. Oxidant stress in asthma. Thorax. 2000;55(suppl 2):S51–S53. doi: 10.1136/thorax.55.suppl_2.S51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henricks PA, Nijkamp FP. Reactive oxygen species as mediators in asthma. Pulm Pharmacol Ther. 2001;14:409–420. doi: 10.1006/pupt.2001.0319. [DOI] [PubMed] [Google Scholar]
- 15.Bowler RP. Oxidative stress in the pathogenesis of asthma. Curr Allergy Asthma Rep. 2004;4:116–122. doi: 10.1007/s11882-004-0056-7. [DOI] [PubMed] [Google Scholar]
- 16.Caramori G, Papi A. Oxidants and asthma. Thorax. 2004;59:170–173. doi: 10.1136/thorax.2002.002477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mak JC, Chan-Yeung MM. Reactive oxidant species in asthma. Curr Opin Pulm Med. 2006;12:7–11. doi: 10.1097/01.mcp.0000198067.50457.71. [DOI] [PubMed] [Google Scholar]
- 18.Iijima H, Duguet A, Eum SY, Hamid Q, Eidelman DH. Nitric oxide and protein nitration are eosinophil dependent in allergen-challenged mice. Am J Respir Crit Care Med. 2001;163:1233–1240. doi: 10.1164/ajrccm.163.5.2003145. [DOI] [PubMed] [Google Scholar]
- 19.Hanazawa T, Kharitonov SA, Barnes PJ. Increased nitrotyrosine in exhaled breath condensate of patients with asthma. Am J Respir Crit Care Med. 2000;162:1273–1276. doi: 10.1164/ajrccm.162.4.9912064. [DOI] [PubMed] [Google Scholar]
- 20.Dworski R, Roberts LJ, II, Murray JJ, Morrow JD, Hartert TV, Sheller JR. Assessment of oxidant stress in allergic asthma by measurement of the major urinary metabolite of F2-isoprostane, 15-F2t-IsoP (8-iso-PGF2alpha). Clin Exp Allergy. 2001;31:387–390. doi: 10.1046/j.1365-2222.2001.01055.x. [DOI] [PubMed] [Google Scholar]
- 21.Pardi P, Kharitonov SA, Barnes PJ. Elevation of exhaled ethane concentration in asthma. Am J Respir Crit Care Med. 2000;162:1450–1454. doi: 10.1164/ajrccm.162.4.2003064. [DOI] [PubMed] [Google Scholar]
- 22.Wedes SH, Khatri SB, Zhang R, Wu W, Comhair SA, et al. Noninvasive markers of airway inflammation in asthma. Clin Transl Sci. 2009;2:112–117. doi: 10.1111/j.1752-8062.2009.00095.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dong CC, Yin XJ, Ma JY, Millecchia L, Wu ZX, et al. Effect of diesel exhaust particles on allergic reactions and airway responsiveness in ovalbumin-sensitized brown Norway rats. Toxicol Sci. 2005;88:202–212. doi: 10.1093/toxsci/kfi280. [DOI] [PubMed] [Google Scholar]
- 24.de Boer J, Meurs H, Flendrig L, Koopal M, Zaagsma J. Role of nitric oxide and superoxide in allergen-induced airway hyperreactivity after the late asthmatic reaction in guinea-pigs. Br J Pharmacol. 2001;133:1235–1242. doi: 10.1038/sj.bjp.0704191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abu-Soud HM, Hazen SL. Nitric oxide is a physiological substrate for mammalian peroxidases. J Biol Chem. 2000;275:37524–37532. doi: 10.1074/jbc.275.48.37524. [DOI] [PubMed] [Google Scholar]
- 26.Sanders SP. Nitric oxide in asthma. Pathogenic, therapeutic, or diagnostic? Am J Respir Cell Mol Biol. 1999;21:147–149. doi: 10.1165/ajrcmb.21.2.f158. [DOI] [PubMed] [Google Scholar]
- 27.Sanders SP, Zweier JL, Harrison SJ, Trush MA, Rembish SJ, Liu MC. Spontaneous oxygen radical production at sites of antigen challenge in allergic subjects. Am J Respir Crit Care Med. 1995;151:1725–1733. doi: 10.1164/ajrccm.151.6.7767513. [DOI] [PubMed] [Google Scholar]
- 28.Carlson MG, Peterson CG, Venge P. Human eosinophil peroxidase: purification and characterization. J Immunol. 1985;134:1875–1879. [PubMed] [Google Scholar]
- 29.Cramer R, Soranzo MR, Patriarca P. Evidence that eosinophils catalyze the bromide-dependent decarboxylation of amino acids. Blood. 1981;58:1112–1118. [PubMed] [Google Scholar]
- 30.Jatakanon A, Uasuf C, Maziak W, Lim S, Chung KF, Barnes PJ. Neutrophilic inflammation in severe persistent asthma. Am J Respir Crit Care Med. 1999;160:1532–1539. doi: 10.1164/ajrccm.160.5.9806170. [DOI] [PubMed] [Google Scholar]
- 31.Wu W, Samoszuk MK, Comhair SA, Thomassen MJ, Farver CF, et al. Eosinophils generate brominating oxidants in allergen induced asthma. J Clin Invest. 2000;105:1455–1463. doi: 10.1172/JCI9702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MacPherson JC, Comhair SA, Erzurum SC, Klein DF, Lipscomb MF, et al. Eosinophils are a major source of nitric oxide-derived oxidants in severe asthma: characterization of pathways available to eosinophils for generating reactive nitrogen species. J Immunol. 2001;166:5763–5772. doi: 10.4049/jimmunol.166.9.5763. [DOI] [PubMed] [Google Scholar]
- 33.Ercan H, Birben E, Dizdar EA, Keskin O, Karaaslan C, et al. Oxidative stress and genetic and epidemiologic determinants of oxidant injury in childhood asthma. J Allergy Clin Immunol. 2006;118:1097–1104. doi: 10.1016/j.jaci.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 34.Liu L, Poon R, Chen L, Frescura AM, Montuschi P, et al. Acute effects of air pollution on pulmonary function, airway inflammation, and oxidative stress in asthmatic children. Environ. Health Perspect. 2009;117:668–674. doi: 10.1289/ehp11813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Migliore E, Berti G, Galassi C, Pearce N, Forastiere F, et al. SIDRIA-2 Collaborative Group. Respiratory symptoms in children living near busy roads and their relationship to vehicular traffic: results of an Italian multicenter study (SIDRIA 2). Environ Health. 2009;8:27. doi: 10.1186/1476-069X-8-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li N, Sioutas C, Cho A, Schmitz D, Misra C, et al. Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ Health Perspect. 2003;111:455–460. doi: 10.1289/ehp.6000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gilmour MI, Jaakkola MS, London SJ, Nel AE, Rogers CA. How exposure to environmental tobacco smoke, outdoor air pollutants, and increased pollen burdens influences the incidence of asthma. Environ Health Perspect. 2006;114:627–633. doi: 10.1289/ehp.8380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Church DF, Pryor WA. Free-radical chemistry of cigarette smoke and ts toxicological implications. Environ Health Perspect. 1985;64:111–126. doi: 10.1289/ehp.8564111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakayama T, Church DF, Pryor WA. Quantitative analysis of the hydrogen peroxide formed in aqueous cigarette tar extracts. Free Radic Biol Med. 1989;7:9–15. doi: 10.1016/0891-5849(89)90094-4. [DOI] [PubMed] [Google Scholar]
- 40.Heffner JE, Repine JE. Pulmonary strategies of antioxidant defense. Am Rev Respir Dis. 1989;140:531–554. doi: 10.1164/ajrccm/140.2.531. [DOI] [PubMed] [Google Scholar]
- 41.Rahman I, Biswas SK, Kode A. Oxidant and antioxidant balance in the airways and airway diseases. Eur J Pharmacol. 2006;533:222–239. doi: 10.1016/j.ejphar.2005.12.087. [DOI] [PubMed] [Google Scholar]
- 42.Comhair SA, Erzurum SC. Antioxidant responses to oxidant mediated lung diseases. Am J Physiol Lung Cell Mol Physiol. 2002;283:L246–L255. doi: 10.1152/ajplung.00491.2001. [DOI] [PubMed] [Google Scholar]
- 43.McFadden SL, Woo JM, Michalak N, Ding D. Dietary vitamin C supplementation reduces noise-induced hearing loss in guinea pigs. Hear Res. 2005;202:200–208. doi: 10.1016/j.heares.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 44.Rock CL, Rodriguez JL, Khilnani R, Lown DA, Parker RS. Carotenoids and antioxidant nutrients following burn injury. Ann NY Acad Sci. 1993;691:274–276. doi: 10.1111/j.1749-6632.1993.tb26193.x. [DOI] [PubMed] [Google Scholar]
- 45.Sackesen C, Ercan H, Dizdar E, Soyer O, Gumus P, et al. A comprehensive evaluation of the enzymatic and nonenzymatic antioxidant systems in childhood asthma. J Allergy Clin Immunol. 2008;122:78–85. doi: 10.1016/j.jaci.2008.03.035. [DOI] [PubMed] [Google Scholar]
- 46.Kinnula VL, Crapo JD. Superoxide dismutases in the lung and human lung diseases. Am J Respir Crit Care Med. 2003;167:1600–1619. doi: 10.1164/rccm.200212-1479SO. [DOI] [PubMed] [Google Scholar]
- 47.Kinnula VL. Production and degradation of oxygen metabolites during inflammatory states in the human lung. Curr Drug Targets Inflamm Allergy. 2005;4:465–470. doi: 10.2174/1568010054526368. [DOI] [PubMed] [Google Scholar]
- 48.Comhair SA, Xu W, Ghosh S, Thunnissen FB, Almasan A, et al. Superoxide dismutase inactivation in pathophysiology of asthmatic airway remodeling and reactivity. Am J Pathol. 2005;166:663–674. doi: 10.1016/S0002-9440(10)62288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Larsen GL, White CW, Takeda K, Loader JE, Nguyen DD, et al. Mice that over express Cu=Zn superoxide dismutase are resistant to allergen-induced changes in airway control. Am J Physiol Lung Cell Mol Physiol. 2000;279:L350–L359. doi: 10.1152/ajplung.2000.279.2.L350. [DOI] [PubMed] [Google Scholar]
- 50.Smith LJ, Shamsuddin M, Sporn PH, Denenberg M, Anderson J. Reduced superoxide dismutase in lung cells of patients with asthma. Free Radic Biol Med. 1997;22:1301–1307. doi: 10.1016/s0891-5849(96)00550-3. [DOI] [PubMed] [Google Scholar]
- 51.Comhair SA, Ricci KS, Arroliga M, Lara AR, Dweik RA, et al. Correlation of systemic superoxide dismutase deficiency to airflow obstruction in asthma. Am J Respir Crit Care Med. 2005;172:306–313. doi: 10.1164/rccm.200502-180OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kirkman HN, Rolfo M, Ferraris AM, Gaetani GF. Mechanisms of protection of catalase by NADPH. Kinetics and stoichiometry. J Biol Chem. 1999;274:13908–13914. doi: 10.1074/jbc.274.20.13908. [DOI] [PubMed] [Google Scholar]
- 53.Ghosh S, Masri F, Comhair S, Andreadis A, Swaidani S, et al. Nitration of proteins in murine model of asthma. Am J Respir Crit Care Med. 2003;167:A889. [Google Scholar]
- 54.Comhair SA, Thomassen MJ, Erzurum SC. Differential induction of extracellular glutathione peroxidase and nitric oxide synthase 2 in airways of healthy individuals exposed to 100% O(2) or cigarette smoke. Am J Respir Cell Mol Biol. 2000;23:350–354. doi: 10.1165/ajrcmb.23.3.4076. [DOI] [PubMed] [Google Scholar]
- 55.Corradi M, Folesani G, Andreoli R, Manini P, Bodini A, et al. Aldehydes and glutathione in exhaled breath condensate of children with asthma exacerbation. Am J Resp Crit Care Med. 2003;167:395–399. doi: 10.1164/rccm.200206-507OC. [DOI] [PubMed] [Google Scholar]
- 56.Peterson JD, Herzenberg LA, Vasquez K, Waltenbaugh C. Glutathione levels in antigen-presenting cells modulate Th1 versus Th2 response patterns. Proc Natl Acad Sci U S A. 1998;95:3071–3076. doi: 10.1073/pnas.95.6.3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kamada F, Mashimo Y, Inoue H, Shao C, Hirota T, et al. The GSTP1 gene is a susceptibility gene for childhood asthma and the GSTM1 gene is a modifier of the GSTP1 gene. Int Arch Allergy Immunol. 2007;144:275–286. doi: 10.1159/000106316. [DOI] [PubMed] [Google Scholar]
- 58.Romieu I, Ramirez-Aguilar M, Sienra-Monge JJ, Moreno-Macías H, del Rio-Navarro BE, et al. GSTM1 and GSTP1 and respiratory health in asthmatic children exposed to ozone. Eur Respir J. 2006;28:953–959. doi: 10.1183/09031936.06.00114905. [DOI] [PubMed] [Google Scholar]
- 59.Gilliland FD, Li YF, Gong H, Jr., Diaz-Sanchez D. Glutathione s-transferases M1 and P1 prevent aggravation of allergic responses by secondhand smoke. Am J Respir Crit Care Med. 2006;174:1335–1341. doi: 10.1164/rccm.200509-1424OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Garte S, Gaspari L, Alexandrie AK, Ambrosone C, Autrup H, et al. Metabolic gene polymorphism frequencies in control populations. Cancer Epidemiol Biomarkers Prev. 2001;10:1239–1248. [PubMed] [Google Scholar]
- 61.Repapi E, Sayers I, Wain LV, Burton PR, Johnson T, et al. Genome-wide association study identifies five loci associated with lung function. Nat Genet. 2010;42:36–44. doi: 10.1038/ng.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dut R, Dizdar EA, Birben E, Sackesen C, Soyer OU, Besler T, Kalayci O. Oxidative stress and its determinants in the airways of children with asthma. Allergy. 2008;63:1605–1609. doi: 10.1111/j.1398-9995.2008.01766.x. [DOI] [PubMed] [Google Scholar]
- 63.Kinnula VL, Lehtonen S, Koistinen P, Kakko S, Savolainen M, et al. Two functional variants of the superoxide dismutase genes in Finnish families with asthma. Thorax. 2004;59:116–119. doi: 10.1136/thorax.2003.005611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Juul K, Tybjaerg-Hansen A, Marklund S, Lange P, Nordestgaard BG. Genetically increased antioxidative protection and decreased chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;173:858–864. doi: 10.1164/rccm.200509-1387OC. [DOI] [PubMed] [Google Scholar]
- 65.Monteseirin J, Bonilla I, Camacho J, Conde J, Sobrino F. Elevated secretion of myeloperoxidase by neutrophils from asthmatic patients: the effect of immunotherapy. J Allergy Clin Immunol. 2001;107:623–626. doi: 10.1067/mai.2001.113566. [DOI] [PubMed] [Google Scholar]
- 66.Aldridge RE, Chan T, van Dalen CJ, Senthilmohan R, Winn M, et al. Eosinophil peroxidase produces hypobromous acid in the airways of stable asthmatics. Free Radic Biol Med. 2002;33:847–856. doi: 10.1016/s0891-5849(02)00976-0. [DOI] [PubMed] [Google Scholar]
- 67.Nadeem A, Chhabra SK, Masood A, Raj HG. Increased oxidative stress and altered levels of antioxidants in asthma. J Allergy Clin Immunol. 2003;111:72–78. doi: 10.1067/mai.2003.17. [DOI] [PubMed] [Google Scholar]
- 68.Mak JC, Leung HC, Ho SP, Law BK, Lam WK, et al. Systemic oxidative and antioxidative status in Chinese patients with asthma. J Allergy Clin Immunol. 2004;114:260–264. doi: 10.1016/j.jaci.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 69.Beier J, Beech KM, Semmler D, Beike N, Buhl R. Increased concentrations of glutathione in induced sputum of patients with mild or moderate allergic asthma. Ann Allergy Asthma Immunol. 2004;92:459–463. doi: 10.1016/S1081-1206(10)61783-8. [DOI] [PubMed] [Google Scholar]
- 70.Blesa S, Cortijo J, Mata M, Serrano A, Closa D, et al. Oral N-acetylcysteine attenuates the rat pulmonary inflammatory response to antigen. Eur Respir J. 2003;21:394–400. doi: 10.1183/09031936.03.00039602. [DOI] [PubMed] [Google Scholar]
- 71.Whitekus MJ, Li N, Zhang M, Wang M, Horwitz MA, et al. Thiol antioxidants inhibit the adjuvant effects of aerosolized diesel exhaust particles in a murine model for ovalbumin sensitization. J Immunol. 2002;168:2560–2567. doi: 10.4049/jimmunol.168.5.2560. [DOI] [PubMed] [Google Scholar]
- 72.Blesa S, Cortijo J, Martinez-Losa M, Mata M, Seda E, Santangelo F, Morcillo EJ. Effectiveness of oral N -acetylcysteine in a rat experimental model of asthma. Pharmacol Res. 2002;45:135–140. doi: 10.1006/phrs.2001.0917. [DOI] [PubMed] [Google Scholar]
- 73.Grandjean EM, Berthet P, Ruffman R, Leuenberger P. Efficacy of oral long-term N-acetylcysteine in bronchopulmonary disease: a meta-analysis of published double-blind placebo-controlled clinical trials. Clin Ther. 2000;22:209–221. doi: 10.1016/S0149-2918(00)88479-9. [DOI] [PubMed] [Google Scholar]
- 74.Stey C, Steurer J, Bachmann S, Medici TC, Tramer MR. The effect of oral N-acetylcysteine in chronic bronchitis: a quantitative systematic review. Eur Respir J. 2000;16:253–262. doi: 10.1034/j.1399-3003.2000.16b12.x. [DOI] [PubMed] [Google Scholar]
- 75.Poole PJ, Black PN. Oral mucolytic drugs for exacerbations of chronic obstructive pulmonary disease: systematic review. BMJ. 2001;322:1271–1274. doi: 10.1136/bmj.322.7297.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Decramer M, Rutten-van Mölken M, Dekhuijzen PN, Troosters T, van Herwaarden C, et al. Effects of N-acetylcysteine on outcomes in chronic obstructive pulmonary disease (Bronchitis Randomized on NAC Cost-Utility Study, BRONCUS): a randomised placebo-controlled trial. Lancet. 2005;365:1552–1560. doi: 10.1016/S0140-6736(05)66456-2. [DOI] [PubMed] [Google Scholar]
- 77.Aliyali M, Poorhasan Amiri A, Sharifpoor A, Zalli F. Effects of N-acetylcysteine on asthma exacerbation. Iran J Allergy Asthma Immunol. 2010;9:103–109. [PubMed] [Google Scholar]
- 78.Kurtoglu YE, Navath RS, Wang B, Kannan S, Romero R, Kannan RM. Poly(amidoamine) dendrimer-drug conjugates with disulfide linkages for intracellular drug delivery. Biomaterials. 2009;30:2112–2121. doi: 10.1016/j.biomaterials.2008.12.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Navath RS, Kurtoglu YE, Wang B, Kannan S, Romero R, Kannan RM. Dendrimer-drug conjugates for tailored intracellular drug release based on glutathione levels. Bioconjug Chem. 2008;19:2446–2455. doi: 10.1021/bc800342d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mazor D, Greenberg L, Shamir D, Meyerstein D, Meyerstein N. Antioxidant properties of bucillamine: possible mode of action. Biochem Biophys Res Commun. 2006;349:1171–1175. doi: 10.1016/j.bbrc.2006.08.155. [DOI] [PubMed] [Google Scholar]
- 81.Sekiguchi N, Kameda H, Amano K, Takeuchi T. Efficacy and safety of bucillamine, a D-penicillamine analogue, in patients with active rheumatoid arthritis. Mod Rheumatol. 2006;16:85–91. doi: 10.1007/s10165-005-0466-y. [DOI] [PubMed] [Google Scholar]
- 82.Dharajiya N, Choudhury BK, Bacsi A, Boldogh I, Alam R, Sur S. Inhibiting pollen reduced nicotinamide adenine dinucleotide phosphate oxidase-induced signal by intrapulmonary administration of antioxidants blocks allergic airway inflammation. J Allergy Clin Immunol. 2007;119:646–653. doi: 10.1016/j.jaci.2006.11.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wagner JG, Jiang Q, Harkema JR, Ames BN, Illek B, Roubey RA, Peden DB. Gamma-tocopherol prevents airway eosinophilia and mucous cell hyperplasia in experimentally induced allergic rhinitis and asthma. Clin Exp Allergy. 2008;38:501–511. doi: 10.1111/j.1365-2222.2007.02855.x. [DOI] [PubMed] [Google Scholar]
- 84.Mehta AK, Arora N, Gaur SN, Singh BP. Choline supplementation reduces oxidative stress in mouse model of allergic airway disease. Eur J Clin Invest. 2009;39:934–941. doi: 10.1111/j.1365-2362.2009.02190.x. [DOI] [PubMed] [Google Scholar]
- 85.Burns JS, Dockery DW, Neas LM, Schwartz J, Coull BA, Raizenne M, Speizer FE. Low dietary nutrient intakes and respiratory health in adolescents. Chest. 2007;132:238–245. doi: 10.1378/chest.07-0038. [DOI] [PubMed] [Google Scholar]
- 86.Riccioni G, Barbara M, Bucciarelli T, di Ilio C, D'Orazio N. Antioxidant vitamin supplementation in asthma. Ann Clin Lab Sci. 2007;37:96–101. [PubMed] [Google Scholar]
- 87.Fogarty A, Lewis SA, Scrivener SL, Antoniak M, Pacey S, Pringle M, Britton J. Oral magnesium and vitamin C supplements in asthma: a parallel group randomized placebo controlled trial. Clin Experimental Allergy. 2003;33:1355–1359. doi: 10.1046/j.1365-2222.2003.01777.x. [DOI] [PubMed] [Google Scholar]
- 88.Pearson PJ, Lewis SA, Britton J, Fogarty A. Vitamin E supplements in asthma: a parallel group randomised placebo controlled trial. Thorax. 2004;59:652–656. doi: 10.1136/thx.2004.022616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ristow M, Zarse K, Oberbach A, Klöting N, Birringer M, et al. Antioxidants prevent health-promoting effects of physical exercise in humans. Proc Natl Acad Sci U S A. 2009;106:8665–8670. doi: 10.1073/pnas.0903485106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ritz SA, Wan J, Diaz-Sanchez D. Sulforaphane-stimulated phase II enzyme induction inhibits cytokine production by airway epithelial cells stimulated with diesel extract. Am J Physiol Lung Cell Mol Physiol. 2007;292:L33–L39. doi: 10.1152/ajplung.00170.2006. [DOI] [PubMed] [Google Scholar]
- 91.Mainardi T, Kapoor S, Bielory L. Complementary and alternative medicine: herbs, phytochemicals and vitamins and their immunologic effects. J Allergy Clin Immunol. 2009;123:283–294. doi: 10.1016/j.jaci.2008.12.023. [DOI] [PubMed] [Google Scholar]
- 92.Cho SY, Park SJ, Kwon MJ, Jeong TS, Bok SH, et al. Quercetin suppresses proinflammatory cytokines production through MAP kinases and NF-kappaB pathway in lipopolysaccharide-stimulated macrophage. Mol Cell Biochem. 2003;243:153–160. doi: 10.1023/a:1021624520740. [DOI] [PubMed] [Google Scholar]
- 93.Butler LM, Koh W-P, Lee H-P, Yu MC, London SJ. Dietary fiber and reduced cough with phlegm: a cohort study in Singapore. Am J Respir Crit Care Med. 2004;170:279–287. doi: 10.1164/rccm.200306-789OC. [DOI] [PubMed] [Google Scholar]
- 94.Tsang F, Wong W. Inhibitors of tyrosine kinase signaling cascade attenuated antigen challenge of guinea-pig airways in vitro. Am J Respir Crit Care Med. 2000;162:126–133. doi: 10.1164/ajrccm.162.1.9908105. [DOI] [PubMed] [Google Scholar]
- 95.Smith LJ, Holbrook JT, Wise R, Blumenthal M, Dozor AJ, Mastronarde J, Williams L. Dietary intake of soy genistein is associated with lung function in patients with asthma. J Asthma. 2004;41:833–843. doi: 10.1081/jas-200038447. [DOI] [PubMed] [Google Scholar]
- 96.Cho YS, Lee J, Lee TH, Lee EY, Lee KU, Park JY, Moon HB. Alpha-lipoic acid inhibits airway inflammation and hyperresponsiveness in a mouse model of asthma. J Allergy Clin Immunol. 2004;114:429–435. doi: 10.1016/j.jaci.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 97.Kim HJ, Park SH, Park SY, Moon UY, Lee BD, et al. Epigallocatechin-3-gallate inhibits interleukin-1beta-induced MUC5AC gene expression and MUC5AC secretion in normal human nasal epithelial cells. J Nutr Biochem. 2008;19:536–544. doi: 10.1016/j.jnutbio.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 98.Song KS, Lee WJ, Chung KC, Koo JS, Yang EJ, Choi JY, Yoon JH. Interleukin-1 beta and tumor necrosis factor-alpha induce MUC5AC overexpression through a mechanism involving ERK/p38 mitogen-activated protein kinases-MSK1-CREB activation in human airway epithelial cells. J Biol Chem. 2003;278:23243–23250. doi: 10.1074/jbc.M300096200. [DOI] [PubMed] [Google Scholar]
- 99.Salvemini D, Wang ZQ, Zweier JL, Samouilov A, Macarthur H, et al. A nonpeptidyl mimic of superoxide dismutase with therapeutic activity in rats. Science. 1999;286:304–306. doi: 10.1126/science.286.5438.304. [DOI] [PubMed] [Google Scholar]
- 100.Melov S, Ravenscroft J, Malik S, Gill MS, Walker DW, et al. Extension of life-span with superoxide dismutase=catalase mimetics. Science. 2000;289:1567–1569. doi: 10.1126/science.289.5484.1567. [DOI] [PubMed] [Google Scholar]
- 101.Masini E, Bani D, Vannacci A, Pierpaoli S, Mannaioni PF, et al. Reduction of antigen-induced respiratory abnormalities and airway inflammation in sensitized guinea pigs by a superoxide dismutase mimetic. Free Radic Biol Med. 2005;39:520–531. doi: 10.1016/j.freeradbiomed.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 102.Matsue H, Edelbaum D, Shalhevet D, Mizumoto N, Yang C, et al. Generation and function of reactive oxygen species in dendritic cells during antigen presentation. J Immunol. 2003;171:3010–3018. doi: 10.4049/jimmunol.171.6.3010. [DOI] [PubMed] [Google Scholar]
- 103.Kode A, Rajendrasozhan S, Caito S, Yang SR, Megson IL, Rahman I. Resveratrol induces glutathione synthesis by activation of Nrf2 and protects against cigarette smoke-mediated oxidative stress in human lung epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2008;294:L478–L488. doi: 10.1152/ajplung.00361.2007. [DOI] [PubMed] [Google Scholar]
- 104.Culpitt SV, Rogers DF, Fenwick PS, Shah P, De Matos C, et al. Inhibition by red wine extract, resveratrol, of cytokine release by alveolar macrophages in COPD. Thorax. 2003;58:942–946. doi: 10.1136/thorax.58.11.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Richard N, Porath D, Radspieler A, Schwager J. Effects of resveratrol, piceatannol, tri-acetoxystilbene, and genistein on the inflammatory response of human peripheral blood leukocytes. Mol Nutr Food Res. 2005;49:431–442. doi: 10.1002/mnfr.200400099. [DOI] [PubMed] [Google Scholar]
- 106.Donnelly LE, Newton R, Kennedy GE, Fenwick PS, Leung RH, et al. Anti-inflammatory effects of resveratrol in lung epithelial cells: molecular mechanisms. Am J Physiol Lung Cell Mol Physiol. 2004;287:L774–L783. doi: 10.1152/ajplung.00110.2004. [DOI] [PubMed] [Google Scholar]
- 107.Ryan JJ, Bateman HR, Stover A, Gomez G, Norton SK, Zhao W, et al. Fullerene nanomaterials inhibit the allergic response. J Immunol. 2007;179:665–672. doi: 10.4049/jimmunol.179.1.665. [DOI] [PubMed] [Google Scholar]
- 108.Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007;120:S94–S138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 109.Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31:143–178. doi: 10.1183/09031936.00138707. [DOI] [PubMed] [Google Scholar]
- 110.Majori M, Vachier I, Godard P, Farce M, Bousquet J, Chanez P. Superoxide anion production by monocytes of corticosteroid-treated asthmatic patients. Eur Respir J. 1998;11:133–138. doi: 10.1183/09031936.98.11010133. [DOI] [PubMed] [Google Scholar]
- 111.De Raeve HR, Thunnissen FB, Kaneko FT, Guo FH, Lewis M, et al. Decreased Cu, Zn-SOD activity in asthmatic airway epithelium: correction by inhaled corticosteroid in vivo. Am J Physiol. 1997;272:L148–L154. doi: 10.1152/ajplung.1997.272.1.L148. [DOI] [PubMed] [Google Scholar]
- 112.Fenech AG, Ellul-Micallef R. Selenium glutathione peroxidase and superoxide dismutase in maltese asthmatic patients: effect of glucocorticoid administration. Pulm Pharmacol Ther. 1998;11:301–308. doi: 10.1006/pupt.1998.0122. [DOI] [PubMed] [Google Scholar]
- 113.Alzoghaibi MA, Bahammam AS. Lipid peroxides in stable asthmatics receiving inhaled steroids and long-acting beta2-agonists. Respirology. 2007;12:439–442. doi: 10.1111/j.1440-1843.2007.01034.x. [DOI] [PubMed] [Google Scholar]
- 114.Diaz-Sanchez D, Tsien A, Fleming J, Saxon A. Effect of topical fluticasone propionate on the mucosal allergic response induced by ragweed allergen and diesel exhaust particle challenge. Clin Immunol. 1999;90:313–322. doi: 10.1006/clim.1998.4676. [DOI] [PubMed] [Google Scholar]
- 115.Ito K, Hanazawa T, Tomita K, Barnes PJ, Adcock IM. Oxidative stress reduces histone deacetylase-2 activity and enhances IL-8 gene expression: role of tyrosine nitration. Biochem Biophys Res Commun. 2004;315:240–245. doi: 10.1016/j.bbrc.2004.01.046. [DOI] [PubMed] [Google Scholar]