Abstract
Background:
There is uncertainty about the optimal approach to screen for clinically important cervical spine (C-spine) injury following blunt trauma. We conducted a systematic review to investigate the diagnostic accuracy of the Canadian C-spine rule and the National Emergency X-Radiography Utilization Study (NEXUS) criteria, 2 rules that are available to assist emergency physicians to assess the need for cervical spine imaging.
Methods:
We identified studies by an electronic search of CINAHL, Embase and MEDLINE. We included articles that reported on a cohort of patients who experienced blunt trauma and for whom clinically important cervical spine injury detectable by diagnostic imaging was the differential diagnosis; evaluated the diagnostic accuracy of the Canadian C-spine rule or NEXUS or both; and used an adequate reference standard. We assessed the methodologic quality using the Quality Assessment of Diagnostic Accuracy Studies criteria. We used the extracted data to calculate sensitivity, specificity, likelihood ratios and post-test probabilities.
Results:
We included 15 studies of modest methodologic quality. For the Canadian C-spine rule, sensitivity ranged from 0.90 to 1.00 and specificity ranged from 0.01 to 0.77. For NEXUS, sensitivity ranged from 0.83 to 1.00 and specificity ranged from 0.02 to 0.46. One study directly compared the accuracy of these 2 rules using the same cohort and found that the Canadian C-spine rule had better accuracy. For both rules, a negative test was more informative for reducing the probability of a clinically important cervical spine injury.
Interpretation:
Based on studies with modest methodologic quality and only one direct comparison, we found that the Canadian C-spine rule appears to have better diagnostic accuracy than the NEXUS criteria. Future studies need to follow rigorous methodologic procedures to ensure that the findings are as free of bias as possible.
A clinically important cervical spine injury is defined as any fracture, dislocation or ligamentous instability detectable by diagnostic imaging and requiring surgical or specialist follow-up.1,2 These injuries can have disastrous consequences including spinal cord injury and death if the diagnosis is delayed or missed.3 Despite the low prevalence (< 3%) of clinically important cervical spinal injury following blunt trauma (e.g., motor vehicle collision), accurate diagnosis is imperative for safe, effective management.4 Currently, uncertainty exists about the optimal diagnostic approach. Some guidelines5,6 advocate using screening tools to identify patients with a higher likelihood of clinically important cervical spinal injury; these patients are then sent for imaging to establish the diagnosis. In other more conservative settings, all patients with blunt trauma are sent for imaging. The first approach, involving screening, is arguably preferable because it optimizes resources and time, while reducing unnecessary costs, radiation exposure and psychological stress for the patient.7 For screening to be safe and effective, the screening tools must have high sensitivity, a low negative likelihood ratio and a low rate of false positives. This assures clinicians that a clinically important cervical spine injury is unlikely and reduces the number of referrals for imaging.
Clinical decision rules synthesize 3 or more findings from the patient’s history, physical examination or simple diagnostic tests to guide diagnostic and treatment decisions.8,9 Two clinical decision rules, the Canadian C-spine rule2 and the National Emergency X-Radiography Utilization Study (NEXUS; Box 1),10 are available to assess the need for imaging in patients with cervical spine injury following blunt trauma. These rules aim to reduce unnecessary imaging by reserving these investigations for patients with a higher likelihood of clinically important cervical spinal injury. Developed independently and validated using large cohorts of patients, these 2 decision rules are recommended in many international guidelines.5,11,12 However, no consensus exists as to which rule should be endorsed.12–14 Therefore, the purpose of our systematic review was to describe the quality of research evaluating the Canadian C-spine rule and NEXUS; describe the diagnostic accuracy of the Canadian C-spine rule and NEXUS; and compare the diagnostic accuracy of the Canadian C-spine rule to that of NEXUS.
Box 1: National Emergency X-Radiography Utilization Study (NEXUS) low-risk criteria10.
Cervical spine radiography is indicated for patients with neck trauma unless they meet ALL of the following criteria:
No posterior midline cervical-spine tenderness
No evidence of intoxication
A normal level of alertness (score of 15 on the Glasgow Coma Scale)
No focal neurologic deficit
No painful distracting injuries
Methods
Data sources
Three electronic databases (CINAHL, Embase, MEDLINE) were searched from inception until Sept. 12, 2011. The search strategy consisted of terms describing the Canadian C-spine rule and NEXUS (Appendix 1, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.120675/-/DC1). We did not use a diagnostic search filter because even sensitive filters can miss relevant studies and perform inconsistently.15 We screened the reference lists of included studies and related systematic reviews to identify diagnostic studies missed by the database search.
Study selection
Two reviewers (Z.M and C.M., A.V., T.R. or C.-W.L.) independently applied selection criteria to titles and abstracts and then full papers. We included articles that met the following criteria: reported on a cohort of patients presenting with symptoms of cervical spine injury following blunt trauma and clinically important cervical spine injury was a differential diagnosis; evaluated the diagnostic performance of the Canadian C-spine rule or NEXUS criteria; confirmed the diagnosis of clinically important spinal injury with an adequate reference standard (e.g., plain radiographs, computed tomography, magnetic resonance imaging); and reported results in sufficient detail to allow reconstruction of contingency tables. No language restriction was applied.
Quality assessment
Two reviewers (Z.M. and A.V., T.R. or C.-W.L.) assessed the methodologic quality of studies using the 11-item Quality Assessment of Diagnostic Accuracy Studies (QUADAS) criteria.16 Studies were included regardless of their risk of bias.16 Disagreements were resolved first in discussion (Z.M. and A.V., T.R. or C.-W.L.), and then by an independent third reviewer if necessary (C.M.). The inter-rater reliability of the quality assessment was evaluated using percentage agreement and Kappa (k) statistics.
Data extraction and analysis
Two authors (Z.M. and C.M., A.V., T.R. or C.-W.L) independently extracted data, including the number of participants, setting, characteristics of the index test and reference standard, prevalence of clinically important cervical spinal injury, and raw data to enable reconstruction of contingency tables. We added 0.5 to the empty cells in the contingency table when a computational problem existed and calculated sensitivity, specificity, likelihood ratios, post-test probabilities and percentage of true negative test results. We planned to pool sensitivity and specificity using a bivariate model if included studies showed sufficient clinical and statistical homogeneity.17,18 We conducted a sensitivity analysis to evaluate the diagnostic performance of the Canadian C-spine rule and NEXUS using studies that assessed the rule prospectively and in their entirety.
Results
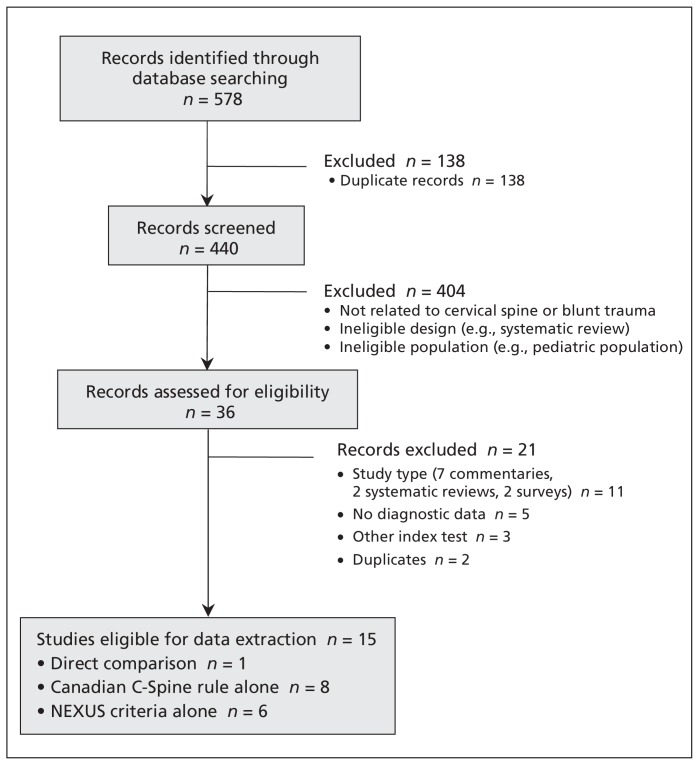
Our search retrieved 578 articles. Fifteen studies were included after screening (Figure 1) and all were published in English. Eight studies evaluated the Canadian C-spine rule alone2,19–25 and 6 studies evaluated NEXUS alone.7,10,26–29 We considered only one of the studies to be a direct comparison, because the diagnostic accuracy of both rules were evaluated prospectively in the same patients and by the same physicians.13 The other comparison was reported in 2 separate studies and evaluated the rules using different study designs and assessors.2,26 We did not consider this to be an accurate direct comparison of the 2 rules, hence we presented these studies individually.2,26 The prevalence of clinically important spinal injury ranged from 0.4%19 to 6%25,28 (median 1.95%, interquartile range [IQR] 1.13–2.74) and included injuries such as C1 arch fracture, C2 hangman’s fracture and C6/7 fracture/subluxation, all of which required surgical intervention, specialist follow-up, or both. Table 1 outlines the characteristics of the included studies. Based on visual inspection of forest plots and statistical testing (a statistically significant χ2 and moderate-to-high I2 value), we determined that the included studies were too heterogeneous to pool.
Figure 1:
Flow diagram of studies selected for inclusion.
Table 1:
Characteristics of the included studies
| Study | Design | Country | N | %Male | MOI | Index test | Reference standard (% of patients who received it) | No. of patients lost to follow-up (%) |
|---|---|---|---|---|---|---|---|---|
| Hoffman et al., 200010 | Prospective cross-sectional | US | 34 069 | 64.8 | NR |
|
|
0 |
| Stiell et al., 20012 | Prospective cross-sectional | Canada | 8 924 | 51.5 | MVC 67% |
|
|
577 (6.5) |
| Stiell et al., 200313 | Prospective cross-sectional | Canada | 8 283 | 52.3 | MVC 67.2% |
|
|
854 (10.3) indeterminate cases not included in the analysis |
| Dickinson et al., 200426 | Retrospective analysis of data from Stiell 200112 | Canada | 8 924 | 51.5 | MVC 67% |
|
|
577 (6.5) |
| Miller et al., 200619 | Prospective cross-sectional | UK | 460 | NR | NR |
|
|
NR |
| Rethnam et al., 200820 | Retrospective review | UK | 114 | NR | NR |
|
|
N/A, patients were included if radiography was conducted |
| Mahler et al., 200927 | Prospective cross-sectional | US | 202 | NR | NR |
|
|
0 |
| Stiell et al, 200921 | Prospective cross-sectional | Canada | 3 628 | 51.0 | MVC 70.1% |
|
|
Radiography conducted in 47.2% of patients |
| Vaillancourt et al., 200922 | Prospective cross-sectional | Canada | 2 393 | 50.2 | MVC 62.5% |
|
|
444 (18.6) |
| Coffey et al., 201023 | Prospective cross-sectional | UK | 1 420 | 50.4 | MVC 75.8% |
|
|
178 (12.5) |
| Stiell et al., 201024 | Prospective cross-sectional | Canada | 3 633 | 46.4 | MVC 63% |
|
|
Radiography conducted in 47.2% of patients |
| Duane et al., 201125 | Prospective cross-sectional | US | 3 201 | 64 | NR |
|
|
0 |
| Duane et al., 201128 | Prospective cross-sectional | US | 2 606 | 65 | MVC, % NR |
|
|
0 |
| Griffith et al., 20117 | Retrospective analysis from radiology information record system | US | 1 589 | 59.3 | MVC 37.7% |
|
|
NA, patients were included if computed tomography was conducted |
| Migliore et al., 201129 | Prospective cross-sectional | US | 80 | NR | NR |
|
|
10 (15) |
Note: CT = computed tomography, ED = Emergency department, MOI = Mechanism of injury, MVC = motor vehicle collision, NA = not applicable; NEXUS = National X-radiography Utilization Study low risk criteria, NR = not reported.
The item “delayed onset of neck pain” was excluded because paramedics would assess patients before such delay.
Residents received a 5-min explanation as to using a standardized data collection form.
The quality, percentage agreement and κ statistic for the QUADAS items are shown in Table 2. Inter-rater reliability was slight to poor for most items, with one item having moderate reliability. No disagreement persisted between reviewers after the consensus meeting. The included studies were of modest quality. Only 6 studies reported enrolment of consecutive patients, highlighting potential selection bias in the remaining 9 studies.
Table 2:
QUADAS16 assessment of the methodologic quality of included studies
| Study | Selection bias* | Reference test†‡ | Disease progression§ | Partial verification bias¶ | Differential verification bias** | Incorporation bias†† | Reference reviewer bias‡‡ | Index reviewer bias§§ | Clinical review bias¶¶ | Uninterpretable results*** | Withdrawals††† |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hoffman et al., 200010 | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Stiell et al., 20012 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No | Yes |
| Stiell et al., 200313 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Unclear |
| Dickinson et al., 200426 | Yes | Yes | Unclear | Yes | No | Yes | Yes | Unclear | Yes | Yes | NA |
| Miller et al., 200619 | Yes | Yes | Yes | No | No | Yes | Unclear | Yes | Yes | Yes | Yes |
| Rethnam et al., 200820 | No | Yes | Unclear | Yes | Yes | Yes | Yes | Unclear | Yes | No | NA |
| Mahler et al., 200927 | No | Yes | Yes | Yes | Yes | Unclear | Unclear | Unclear | Yes | Yes | Yes |
| Stiell et al., 200921 | Yes | No | No | No | No | Yes | Unclear | Yes | Yes | No | No |
| Vaillancourt et al., 20092 | No | Yes | Yes | No | No | Unclear | Unclear | Unclear | Yes | Yes | Yes |
| Coffey et al., 201023 | Yes | Yes | Yes | No | No | Unclear | Unclear | Unclear | Yes | Yes | Yes |
| Stiell et al., 201024 | Yes | No | No* | No | No | Yes | Unclear | Unclear | Yes | Yes | Yes |
| Duane et al., 201125 | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes |
| Duane et al., 201128 | Unclear | Yes | Unclear | Yes | Yes | Yes | Unclear | Unclear | Yes | Yes | Yes |
| Griffith et al., 20117 | No | Yes | Unclear | Yes | Yes | Yes | Unclear | Unclear | Yes | Yes | NA |
| Migliore et al., 201129 | No | Yes | Unclear | No | No | Unclear | Unclear | Yes | Yes | No | No |
| Inter-rater reliability, k | 0.54 | 0.00 | 0.15 | −0.13 | 0.21 | 0.47 | 0.39 | 0.17 | −0.03 | −0.02 | 0.00 |
| Percentage agreement, % | 73 | 87 | 53 | 47 | 53 | 80 | 67 | 53 | 87 | 53 | 33 |
Note: NA = not applicable.
Was the spectrum of patients representative of the patients who will receive the test in practice? Is it a selective sample of patients?
Is the reference standard likely to classify the target condition correctly?
The 14-day proxy method was deemed to be an adequate reference standard because the outcome for all patients could be accounted for by either by the 14-day proxy method or radiography. This mirrors clinical practice.34 However, the 21-day surveillance strategy was deemed to be an inadequate reference standard because it assumes that patients with fractures missed at the initial presentation would be subsequently captured in patient logs. We found no data about the accuracy of the 21-day surveillance strategy to support its use as a reference standard.
Is the time between the reference standard and the index test short enough to be reasonably sure that the target condition did not change between the 2 tests?
Did the whole sample, or a random selection of the sample, receive verification using a reference standard of diagnosis?
Did patients receive the same reference standard regardless of the index test result?
Was the reference standard independent of the index test (i.e., the index test did not form part of the reference standard)?
Were the reference standard results interpreted without knowledge of the results of the index test?
Were the index test results interpreted without knowledge of the results of the reference standard?
Were the same clinical data available when the index test results were interpreted as would be available when the test is used in practice?
Were uninterpretable and/or intermediate test results reported?
Were withdrawals from the study explained?
Six studies used a “gold standard” reference test for all patients;7,10,25,27,28 the remaining 9 studies were influenced by differential verification bias because not all patients underwent imaging or patients underwent different reference tests at the discretion of the treating physician. In the 8 studies that used different reference tests, patients who did not undergo imaging were followed up with either the 14-day proxy2,13,19,22,23,26 or the 21-day surveillance strategy.19,21,24 With the 14-day proxy method, patients are contacted by a registered nurse 14 days after discharge and asked 8 questions about pain and return to function. A positive response to these questions resulted in patients being asked to return to hospital for imaging investigations. With the 21-day surveillance strategy, patient logs at major hospitals and neurosurgical centres were monitored for readmission.
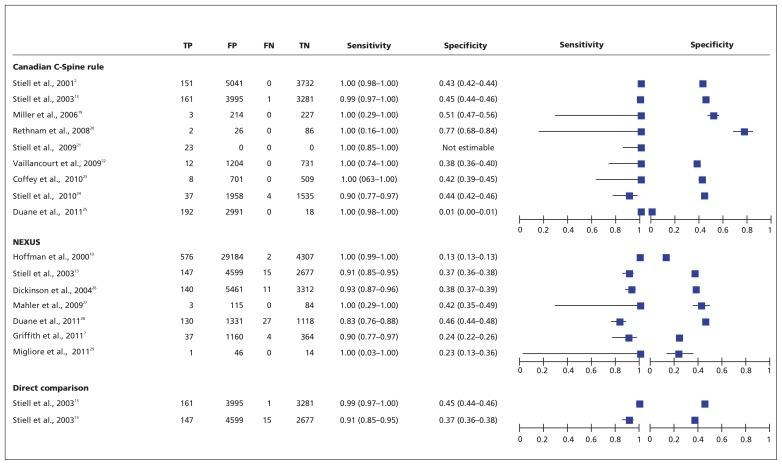
Canadian C-spine rule
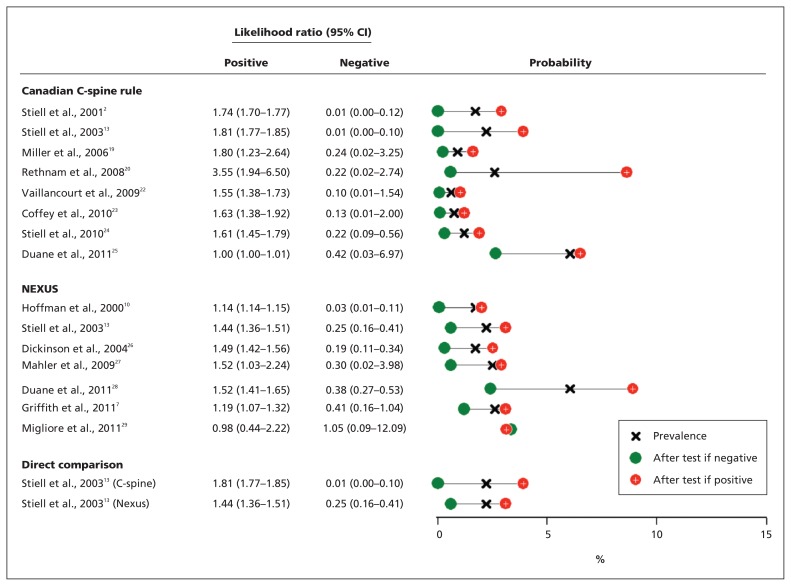
Of the 9 studies that assessed the Canadian C-spine rule, 4 were prospective studies2,13,21,23 that aimed to assess the rule in its entirety; 4 prospectively applied a modified version of the rule;19,22,24,25 and 1 was a retrospective study.20 The sensitivity of the Canadian C-spine rule ranged from 0.90 to 1.0, while the specificity ranged from 0.01 to 0.77 (Figure 2). The Canadian C-spine rule had a low rate of false negative results (0%–0.11%),24 and imaging rates would have been reduced by an average of 42.0% (0.6%–75.4%) without missing a clinically important cervical spine injury. Figure 3 shows the prevalence of clinically important injury reported in each study, positive and negative likelihood ratios and the post-test probability given a positive and negative test result. The median negative likelihood ratios of 0.18 (IQR 0.03–0.24) were more informative than the median positive likelihood ratios of 1.69 (IQR 1.57–1.81). Given the low prevalence of clinically important spinal injury (median 1.95%), a positive response to the Canadian C-spine rule only increased the post-probability to 2.4% (IQR 1.30%–5.85%), while a negative test result was more informative because it reduced the post-probability to 0.16% (IQR 0.38%–3.08%).
Figure 2:
Sensitivity and specificity of the Canadian C-spine rule (CCR) and National Emergency X-radiography Utilization Study (NEXUS) criteria. For Stiell and colleagues,21 we were only able to calculate sensitivity, because we were unable to acquire additional information from the authors. Note: FN = false negative, FP = false positive, TN = true negative, TP = true positive.
Figure 3:
Probability of clinically important cervical spinal injury and likelihood ratios for the Canadian C-spine rule and National Emergency X-Radiography Utilization Study (NEXUS) criteria. For Stiell and colleagues,21 we were only able to calculate sensitivity, because we were unable to acquire additional information from the authors.
Four studies2,13,21,23 were included in the sensitivity analysis. This analysis reaffirmed that the Canadian C-spine rule is highly sensitive (range 0.99–1.00) and significantly reduced the range over which specificity spanned (range 0.42–0.45).
NEXUS
Seven studies assessed the NEXUS rule. Of the 5 prospective studies, 4 assessed the rule in its entirety10,13,28,29 and 1 assessed a modified version (adding 7 questions from the Clinical sobriety assessment tool).27 Two were retrospective studies.7,26 The sensitivity of NEXUS ranged from 0.83 to 1.0, while the specificity ranged from 0.13 to 0.46 (Figure 2). Similar to the Canadian C-spine rule, the negative likelihood ratio (median 0.30, IQR 0.19–0.41) was more informative than the positive likelihood ratio (median 1.44, IQR 1.14–1.52) (Figure 3). In contrast, most of the NEXUS studies did not report large shifts in the post-test probability of clinically important injury from the prevalence (median 1.95%) with a positive test result (median post-test probability 3.10%, IQR 2.50%–3.10%) or negative test result (median post-test probability 0.60%, IQR 0.30%–2.40%). False negatives for NEXUS ranged from 0% to 1.0%,7 and imaging rates would have been reduced by an average of 30.9% (range 12.6%10 to 42.9%28) without missing a clinically important cervical spine injury. The findings by Migliore and colleagues29 should be interpreted with caution because this small study was of low methodologic quality and the data yield counterintuitive likelihood ratios (positive liklihood ratio < 1.0, negative liklihood ratio > 1.0). Only data for the residents, and not emergency physicians, were reported because these 2 groups are not statistically independent and the results for the emergency physicians appeared unreliable because all study participants were sent for imaging. Four studies10,13,28,29 were included in the sensitivity analysis, and these results were consistent with the primary analysis.
Direct comparison of the Canadian C-spine rule and NEXUS
The only direct comparison of the 2 rules indicates that the Canadian C-spine rule has better diagnostic accuracy, as shown by nonoverlapping 95% confidence intervals for sensitivity, specificity and the likelihood ratios (Figures 2 and 3).13 The Canadian C-Spine rule would have reduced imaging rates by 44%, while NEXUS would have reduced the rates by 36%.
Interpretation
We found 15 studies of modest methodologic quality that evaluated the diagnostic accuracy of the Canadian C-spine rule and NEXUS. We found that both rules had consistently high sensitivity, indicating that a negative test result is highly informative in excluding a clinically important cervical spine injury and, therefore, the need for radiographic examination. The value of a negative test result is further shown by the low negative likelihood ratio and post-test probability. In the only direct comparison, the Canadian C-spine rule had higher sensitivity, and thus gives fewer false negative results. Because both rules are based on imaging all patients with positive results, the low specificity and high false positive rate means that many people without injury will undergo unnecessary imaging. The results of the sensitivity analysis reinforced the primary findings. However, for the Canadian C-spine rule, the range over which specificity spanned was significantly reduced. This suggests that the diagnostic accuracy of the Canadian C-spine rule is superior when the rule is used in its entirety.
The findings of this review are consistent with a previous meta-analysis14 and 2 literature reviews.30,31 However, our review used a larger and more sensitive search strategy, which resulted in a larger number of primary studies identified for inclusion. In addition, we considered the methodologic quality of the included studies when interpreting the diagnostic accuracy. As a result, we have outlined an optimal diagnostic study design for future studies in this area (Appendix 2, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.120675/-/DC1) in order to reduce potential biases.
Clinically, our review highlights the effectiveness of the Canadian C-spine rule and NEXUS in clearing the cervical spine without the need for imaging, while maintaining patient safety. Although most of the studies included in this review are validation studies, only the Canadian C-Spine rule has been evaluated in an impact analysis study, which further supports its use in practice.21 Despite these findings, there is a more liberal use of imaging in current clinical practice, which may reflect patient preference, physicians’ fear of litigation or missing a fracture, or uncertainty of the application or accuracy of the screening tools. Improved education of physicians may facilitate greater use of these rules. In particular, educational content should focus on the subjective components of the Canadian C-spine rule (e.g., dangerous mechanism of injury,21 range of motion assessment) and NEXUS (e.g., distracting injuries, intoxication)32 because these components were most frequently misinterpreted.
Educating patients may also improve the utilization of these screening tools. In the absence of any clinical indication of a clinically important cervical spinal injury, routine imaging is not associated with psychological benefits or improved outcomes.33 Patients knowledge of this, together with knowledge about the accuracy of these screening tools weighed against the potential harms of unnecessary radiation exposure, would allow for more informed decisions to be made. To ease the concerns of patients discharged without imaging, further evaluation of alternate follow-up strategies, such as the 14-day proxy, would be beneficial for both clinical practice and research. Currently there is only limited data to support the use of the 14-day proxy as a reference standard,34 and there is no data on the accuracy of the 21-day surveillance strategy.
Limitations
Limitations of this review included the selected use of data sources, the moderate methodologic quality of the included studies and the heterogeneity, which prevented pooling. Although a sensitive search strategy including citation tracking was used to identify eligible studies, we did not search for grey literature (e.g., contacting key authors to identify unpublished data). The inability to pool results means that the findings of this review are based on individual studies and only one direct comparison. Factors contributing to the heterogeneity identified included between trial variations in methodologic quality, clinical characteristics (e.g., professions applying the rules, their experience and training) and within-trial variations in how rules were interpreted and applied.
Conclusion
Based on studies with modest methodologic quality, we found that both the Canadian C-spine rule and NEXUS were highly sensitive rules that have the potential to reduce imaging rates. However, the lower specificity and false-positive results indicate that many people will continue to undergo unnecessary imaging. In the only direct comparison, the Canadian C-spine rule appeared to have better diagnostic accuracy, and it should be used over NEXUS to assess the need for cervical spine imaging. Future studies of diagnostic test accuracy need to ensure that rigorous methodologic procedures are followed to reduce bias. Furthermore, the evaluation of these tools in settings outside of emergency departments, in pediatric and older populations and by primary care physicians, such as general practitioners and physiotherapists, is also required.
Supplementary Material
Acknowledgements
Zoe Michaleff holds an Australian Postgraduate Award from the Australian Government. Chung-Wei Christine Lin holds a fellowship funded by the National Health and Medical Research Council of Australia. Chris Maher holds a fellowship funded by the Australian Research Council. Adrianne Verhagen is supported by the Department of General Practice, Erasmus University.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: All authors were involved and contributed to the design of the study, title screening, data extraction, interpretation and drafting of the manuscript. All authors approved the final version submitted for publication.
References
- 1.Stiell I, Lesiuk H, Vandemheen K, et al. Obtaining consensus for a definition of “clinically important cervical spine injury” in the CCC Study. Acad Emerg Med 1999;6:435 [Google Scholar]
- 2.Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA 2001;286:1841–8 [DOI] [PubMed] [Google Scholar]
- 3.Davis JW, Phreaner DL, Hoyt DB, et al. The etiology of missed cervical spine injuries. J Trauma 1993;34:342–6 [DOI] [PubMed] [Google Scholar]
- 4.Pimentel L, Diegelmann L. Evaluation and management of acute cervical spine trauma. Emerg Med Clin North Am 2010;28:719–38 [DOI] [PubMed] [Google Scholar]
- 5.Clinical guidelines for the best practice management of acute and chronic whiplash-associated disorders. Adelaide (South Australia): TRACsa; 2008 [Google Scholar]
- 6.Guidelines for the management of acute whiplash-associated disorders for health professionals. 2nd ed Sydney (Australia): Motor Vehicle Accidents Authority; 2007. Available: www.maa.nsw.gov.au/default.aspx?MenuID=115 (accessed 2012 Sept. 26). [Google Scholar]
- 7.Griffith B, Bolton C, Goyal N, et al. Screening cervical spine CT in a level I trauma center: Overutilization? AJR Am J Roentgenol 2011;197:463–7 [DOI] [PubMed] [Google Scholar]
- 8.Laupacis A, Sekar N. IG S. Clinical prediction rules: a review and suggested modifications of methodological standards. JAMA 1997;277:488–94 [PubMed] [Google Scholar]
- 9.Stiell IG, Bennett C. Implementation of clinical decision rules in the emergency department. Acad Emerg Med 2007;14:955–9 [DOI] [PubMed] [Google Scholar]
- 10.Hoffman JR, Mower WR, Wolfson AB, et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med 2000;343:94–9 [DOI] [PubMed] [Google Scholar]
- 11.National Health and Medical Research Council Evidence-based management of acute musculoskeletal pain. Canberra (AU): The Council; 2003 [DOI] [PubMed] [Google Scholar]
- 12.American College of Radiology ACR appropriateness criteria: suspected spinal trauma. Reston (VA): The College; 1999. Available: www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/SuspectedSpineTrauma.pdf (accessed 2012 Sept. 25). [Google Scholar]
- 13.Stiell IG, Clement CM, McKnight RD, et al. The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med 2003;349:2510–8 [DOI] [PubMed] [Google Scholar]
- 14.Anderson PA, Muchow RD, Munoz A, et al. Clearance of the asymptomatic cervical spine: a meta-analysis. J Orthop Trauma 2010;24:100–6 [DOI] [PubMed] [Google Scholar]
- 15.de Vet HCW, Eisinga A, Riphagen II, Aergeerts B, Pewser D. Chapter 7: Searching for studies. In: Cochrane handbook for systematic reviews of diagnostic test accuracy version 0.4 [updated September 2008]: The Cochrane Collaboration; 2008:60p. Available: http://srdta.cochrane.org/sites/srdta.cochrane.org/files/uploads/Chapter07-Searching-%28September-2008%29.pdf (accessed 2012 Sept. 27). [Google Scholar]
- 16.Whiting P, Rutjes AW, Reitsma JB, et al. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van der Windt D, Simons E, Riphagen I, et al. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Data Syst Rev 2010; (2):CD007431. [DOI] [PubMed] [Google Scholar]
- 18.Lijmer JG, Bossuyt PM, Heisterkamp SH. Exploring sources of heterogeneity in systematic reviews of diagnostic tests. Stat Med 2002;21:1525–37 [DOI] [PubMed] [Google Scholar]
- 19.Miller P, Coffey F, Reid AM, et al. Can emergency nurses use the Canadian cervical spine rule to reduce unnecessary patient immobilisation? Accid Emerg Nurs 2006;14:133–40 [DOI] [PubMed] [Google Scholar]
- 20.Rethnam U, Yesupalan R, Gandham G. Does applying the Canadian Cervical Spine rule reduce cervical spine radiography rates in alert patients with blunt trauma to the neck? A retrospective analysis. BMC Med Imaging 2008;8:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stiell IG, Clement CM, Grimshaw J, et al. Implementation of the Canadian C-Spine Rule: prospective 12 centre cluster randomised trial. BMJ 2009;339:b4146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vaillancourt C, Stiell IG, Beaudoin T, et al. The out-of-hospital validation of the Canadian C-Spine Rule by paramedics. Ann Emerg Med 2009;54:663–71 [DOI] [PubMed] [Google Scholar]
- 23.Coffey F, Hewitt S, Stiell I, et al. Validation of the Canadian c-spine rule in the UK emergency department setting. Emerg Med J 2011; 28:873–6 [DOI] [PubMed] [Google Scholar]
- 24.Stiell IG, Clement CM, O’Connor A, et al. Multicentre prospective validation of use of the Canadian C-Spine Rule by triage nurses in the emergency department. CMAJ 2010;182:1173–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duane TM, Wilson SP, Mayglothling J, et al. Canadian Cervical Spine rule compared with computed tomography: a prospective analysis. J Trauma 2011;71:352–5 [DOI] [PubMed] [Google Scholar]
- 26.Dickinson G, Stiell I, Schull M, et al. Retrospective application of the NEXUS low-risk criteria for cervical spine radiography in Canadian emergency departments. Ann Emerg Med 2004;43:507–14 [DOI] [PubMed] [Google Scholar]
- 27.Mahler S, Pattani S, Caldito G, et al. Use of a clinical sobriety assessment tool with the NEXUS low-risk cervical spine criteria to reduce cervical spine imaging in blunt trauma patients with acute alcohol or drug use: a pilot study. Ann Emerg Med 2009;54:S26–7 [Google Scholar]
- 28.Duane TM, Mayglothling J, Wilson SP, et al. National Emergency X-Radiography Utilization Study criteria is inadequate to rule out fracture after significant blunt trauma compared with computed tomography. J Trauma 2011;70:829–31 [DOI] [PubMed] [Google Scholar]
- 29.Migliore S, Strelkauskas A, Matteucci M. The NEXUS criteria: inter-rater reliability between residents versus attending physicians in the emergency department. Acad Emerg Med 2011;18: S139–40 [Google Scholar]
- 30.Blackmore CC. Evidence-based imaging evaluation of the cervical spine in trauma. Neuroimaging Clin N Am 2003;13:283–91 [DOI] [PubMed] [Google Scholar]
- 31.Cornelius RS. Imaging of acute cervical spine trauma. Semin Ultrasound CT MR 2001;22:108- 24-20 [DOI] [PubMed] [Google Scholar]
- 32.Vandemark RM. Radiology of the cervical spine in trauma patients: practice, pitfalls and recommendations for improving efficiency and communication. AJR Am J Roentgenol 1990;155:465–72 [DOI] [PubMed] [Google Scholar]
- 33.Flynn T, Smith B, Chiou R. Appropriate use of diagnostic imaging in low back pain: a reminder that unnecessary imaging may do as much harm as good. J Orthop Sports Phys Ther 2011;41:838–46 [DOI] [PubMed] [Google Scholar]
- 34.Vandemheen K, Stiell I, Brison R, et al. Validity Evaluation of the Cervical Spine Injury Proxy Outcome Assessment Tool in the CCC Study [abstract]. Acad Emerg Med 1999;6:434–5 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.