Abstract
We assessed the influence of intimate partner violence (IPV), depression and post-traumatic stress disorder (PTSD) on disordered eating patterns (DE) among women of African descent through a comparative case-control study (N=790) in Baltimore, MD and St. Thomas and St. Croix, US Virgin Islands from 2009–2011. IPV, depression and PTSD were independent risk factors in the full sample. The relationship between IPV and DE was partially mediated by depression. The influence of risk for lethality from violence was fully mediated by depression. IPV should be considered in research and treatment of DE and both IPV and DE assessed when the other or depression is detected.
Eating disorders and disordered eating (DE) patterns affect more than estimated 8 million Americans, 7 million of whom are women. (South Carolina Department of Mental Health, 2006) In a nationally representative survey of US households (2001–2003), prevalence rates of eating disturbances for women ranged from 1%–4%. (Hudson, Hiripi, Pope Jr., & Kessler, 2007; Meltzer-Brody et al., 2011) Understanding of risk factors associated with DE and eating disorder symptomatology is critical as eating disorders have the highest mortality rate of any mental health related problem. (South Carolina Department of Mental Health, 2006)
Both disordered eating and eating disorders are DSM-I-TR classifications. Different eating disorders, such as anorexia nervosa and bulimia, have specific criteria that must be met for diagnosis per the DSM-IV-TR. On the other hand, DE encompasses a broader range of irregular eating patterns and behaviors that do fall under a specific eating disorder diagnosis. People with disordered eating patterns may exhibit symptoms of several different eating disorders, but the patterns are usually erratic (American Psychiatric Association, 2000).
DE and eating disorders are acute and chronic adverse health outcomes of intimate partner violence (IPV) (J. C. Campbell et al., 2002), yet this link is seldom mentioned in the DE and eating disorder literature. IPV, consisting of physical, sexual, and psychological abuse by an intimate partner, remains a pervasive epidemic in the United States, where between nearly one in three women has experienced violence from a partner in their lifetime (Black et al., 2011). IPV occurs in both opposite- and same-sex relationships, with 11% of women in same-sex relationships reporting IPV perpetrated by their female partner (Tjaden & Thoennes, 2000). In population-based studies, nearly 29% of the women reporting abuse are African-American (Tjaden & Thoennes, 2000), a prevalence disproportionate to their proportion in the population. In addition, a study conducted in 16 U.S. states and two territories found that 22.5 % of women of African descent in the U.S. Virgin Islands (USVI) have been victims of IPV (Breiding, Black, & Ryan, 2008).
When abuse is considered in conjunction with DE, young women experiencing dating violence and partner rape are up to 5 times more likely to have DE behaviors (Ackard & Neumark-Sztainer, 2002). Adult women experiencing IPV are also at increased risk for various eating disorders, when compared to their non-abused counterparts (Danielson, Moffitt, Caspi, & Silva, 1998; Vos et al., 2006). No published literature to date has examined DE behaviors and IPV specifically among women of African descent nor has there been examination of the influence of type of IPV or risk for lethality of IPV on a woman’s risk for DE.
Other research has examined the relationship between depression, PTSD and DE, most often without regard to violence experiences. Both depression and PTSD are widely prevalent among women with eating disorders (Brewerton, 2007; Dansky, Brewerton, Kilpatrick, & O’Neil, 1997). In a meta-analysis of 232 studies on the factors associated with disordered eating, women with eating disorders showed higher levels of depression than women without eating disorders. (Vince & Walker, 2008) Research also shows an association between PTSD and eating disorders. The prevalence rates of lifetime PTSD are significantly higher among women with eating disorders (36.9%) as compared with women without eating disorders (11.8%) (Brewerton, 2007; Dansky et al., 1997).
Women experiencing abuse are more likely to experience depression and post-traumatic stress disorder (PTSD) than women reporting no abuse. (Cascardi, O’Leary, & Schlee, 1999; Kelly, 2010) In a meta-analysis of 18 studies of depression, the weighted average prevalence of depression among abused women was 47.6% (Golding, 1999), and the Stith and colleagues meta-analysis found an medium effect size with depression (d= 0.59 CI = 0.45/0.72 r= .28*** Qw = 20.44**) (Stith, Smith, Penn, Ward, & Tritt, 2004). In terms of PTSD, the Golding (1999) meta-analysis of 11 studies on IPV as a risk factor for mental illness reported that 31–84% of abused women suffered from PTSD, while other community based studies in the U.S. have reported PTSD prevalence rates in IPV victims ranging from 6–34% (J. C. Campbell, 2002; Seedat, Stein, & Forde, 2005; Sullivan & Holt, 2008). Basile and colleagues (2004) found that all forms of IPV (including physical and sexual) were significantly associated with women’s presentation of PTSD symptoms (Basile, Arias, Desai, & Thompson, 2004). In addition, a study of 7,700 women drawn from the Survey of Violence and Threats of Violence Against Women and Men in the United States (1994–1996) found that severity of physical abuse and severity of sexual abuse were significantly related to elevated symptoms of depression among women (Demaris & Kaukinen, 2005).
While the physical and mental health outcomes of IPV have been well-documented and the influence of depression and PTSD on DE has been examined, the interplay between the abuse, depression, PTSD, and DE has not been well investigated. Evidence suggests that depression and PTSD may influence the extent to which victimization is associated with eating disorder problems (Brady, 2008; Kong & Bernstein, 2009; Mazzeo, Mitchell, & Williams, 2008), thereby positioning PTSD and depression as potential mediators between IPV and disordered eating among women.
The purpose of the present study among African-American and African-Caribbean women was to examine whether a) IPV experiences, depression, and PTSD were associated with disordered eating problems, and b) severity and risk for lethality from partner abuse connotes additional risk on those women experiencing abuse from their partners, and c) depression and PTSD mediate the relationship between IPV and disordered eating after controlling for socio-demographic variables. The extent to which IPV and other factors influence the risk for DE among adult African-American and African-Caribbean adult women is unknown, particularly because there remains a dearth of eating disorder literature that extends to populations beyond college-aged samples and report findings by race and ethnicity or other demographics. The findings can assist practitioners in their assessment, prevention and interventions for minority women with DE patterns.
Methods
Study Population
The study population was composed of African-American and African-Caribbean women in Baltimore, MD and St. Croix and St. Thomas, U.S. Virgin Islands (USVI). Participants in the multi-site case–control study were recruited from primary care, prenatal or family planning clinics. Participation was restricted to women aged 18–55 with an intimate relationship within the past 2 years and who identified as being of racial or ethnic heritage that included African descent. Women who only reported history of child abuse or abuse by someone other than an intimate partner were deemed ineligible for participation.
After the informed consent process, eligible women completed a survey via an audio computer-assisted self-interview (ACASI). Women took the survey, which averaged about 30 minutes, in private offices in the clinics, and most participants completed it during the wait time for their appointments. Remuneration of a $20 gift card per participant was provided for their time. Of the 1184 eligible women, 394 were non-selected controls and 790 women participated in the study. A total of 781 participants responded regarding DE, with 499 reporting experiencing IPV. IRB approval was obtained from the Johns Hopkins Hospital and the University of the Virgin Islands.
Measures
The outcome measure of disordered eating (DE) was the response to “How often have you had an eating disorder (overeating/under-eating) in the past year?” Those responding “many times” and “everyday/almost every day” were considered positive for DE. The survey question used the term “eating disorder” as a mechanism to prompt women to think about their eating habits rather than to capture only those who had an eating disorder diagnosis. We use the term “disordered eating” when presenting results as acknowledgment that the women responding may not have had full DSM-IV Axis I diagnoses of specific eating disorders, but rather that they noted irregularities in their eating patterns.
The primary exposure variable of interest was the women’s experiences of IPV. IPV included experiences of physical, sexual and/or psychological abuse by an intimate partner. The Abuse Assessment Screen (AAS; (McFarlane, Parker, Soeken, & Bullock, 1992)) and the Women’s Experiences of Abuse (WEB; (Hall Smith, Earp, & DeVellis, 1995)) were used to identify cases. A case was defined as a woman who answered “yes” to any AAS question concerning a current or former intimate partner or who scored above the threshold of abuse (>19) on the WEB. Women in the control group were randomly selected never abused women. We further classified women who were cases into those reporting emotional abuse only, those reporting physical abuse, and those reporting physical and sexual abuse.
We measured the presence of depressive symptoms by responses to the Clinical Epidemiologic Services for Depression (CES-D 10; (Andresen, Malmgren, Carter, & Patrick, 1994)). We totaled participants’ scores and then categorized them into either not having (score <10) or having (score =10+) symptoms indicative of depressive symptomatology, a cutpoint previously established in the literature (Andresen et al., 1994). The presence of PTSD symptoms was also considered a key exposure variable. PTSD was assessed using the 4-question Primary Care Post Traumatic Stress Disorder Screening (range 0–4) (PC-PTSD; (Prins et al., 2003)). We used the recommended cut-off point of 3, by which participants scoring 3 or more were classified as positive for PTSD.
Potential confounders for the entire sample included demographics including site location, race, age, marital status, education level, employment status, insurance status, annual income, and children under 18 living at home.
For the subset of women experiencing abuse, we assessed severity of violence using the Severity of Violence Against Women instrument (SVAWS (Marshall, 1992)). Respondents answered a series of questions pertaining to abuse experiences in the last 12 months. Each response was weighted according to the non-student weights (Marshall, 1992). Total scores were derived for physical violence (range 0–54) and for sexual abuse (range 0–11.5). Risk for lethality from abuse was determined through the Danger Assessment (DA) (J. C. Campbell, Webster, & Glass, 2008)). Weights were assigned per recommended protocol, and total scores (range 0–36) were divided into three categories: variable (0), increased (1–13), and severe/extreme danger (14–36).
Statistical Analysis
We assessed internal consistency of the CESD-10 and PC-PTSD scales (Cronbach’s alpha 0.84 and 0.79, respectively). Chi-square tests and independent sample T-tests were used to describe the associations between variables of demographics, IPV, depressive symptoms, and PTSD and the outcome variable of DE for the entire sample. The same were used among abused women to assess the associations between severity and risk of lethality from abuse and the outcome variable of DE. A series of generalized linear mixed models were conducted for the dependent variable of DE, which included random effects for site-to-site variability. Variables with p-values of less than 0.15 in bivariate analyses or theoretically relevant were considered for the final mixed effects models. Two sets of multivariate logistic regression models were performed with a random effect for site included. The first was for the entire sample to determine the effects of IPV, depressive symptoms, and PTSD on DE. The second set examined only women experiencing IPV to ascertain the influence of severity and risk for lethality on DE. Mediation was tested for both groups using the recommended approach for dichotomous outcome variables, using bootstrapping with biased-corrected confidence intervals. (Mackinnon & Dwyer, 1993) Estimates of adjusted odds ratios (AORs) and 95% confidence intervals (CI) were obtained with the mixed effects logistic regressions. Final models were selected based on their AIC values. All statistical analyses were performed using Stata 12 (StataCorp, 2011).
Results
Characteristics of Participants
Of the 781 women included in this analysis, 327 (42%) women were from Baltimore, MD, 234 (30%) were from St. Thomas, USVI and 220 (28%) were from St. Croix, USVI. The majority of the women (n=727, 93%) identified as being black African American or African Caribbean, while 43 (6%) identified as being Spanish or Hispanic African American and another 11 (1%) considered themselves other mixed race. The average age was 29.4 years old (9.0 SD, range 18–55). Nearly three-fourths (74%) had at least one child, and 44% were either partnered or married. Approximately 80% of the participants had at least a high school diploma or equivalent, nearly half of the sample (48%) was employed, and 69% had some form of health insurance including 42% on Medicaid or government subsidized programs. The vast majority (93%) reported an individual annual income of less than 24,000USD. None of the socio-demographic variables showed statistically significant associations with disordered eating (see Table 1).
Table 1.
Associations Between Sociodemographic Variables and Disordered Eating in a sample of African-American and African-Caribbean Women in Baltimore, MD and St. Thomas and St. Croix, USVI
| Disordered Eating | |||||
|---|---|---|---|---|---|
|
| |||||
| Sample Total (n=781) | No DE (n=733) | DE (n=48) | Test Statistic | p-value | |
| Site, n (%) | |||||
| Baltimore | 327 (42) | 309 (42) | 18 (38) | χ2=0.45 | 0.80 |
| St. Thomas | 234 (30) | 218 (30) | 16 (33) | ||
| St. Croix | 220 (28) | 206 (28) | 14 (29) | ||
|
| |||||
| Race, n (%) | |||||
| Black AA or CA | 727 (93) | 685 (94) | 42 (88) | Fischer’s Exact | 0.17 |
| Hispanic AA or CA | 43 (6) | 38 (5) | 5 (10) | ||
| Other mixed race | 11 (1) | 10 (1) | 1 (2)) | ||
|
| |||||
| Age, mean years (SD) | 29.4 (9.0) | 29.4 (9.0) | 30.1 (8.6) | t=−0.52 | 0.60 |
|
| |||||
| Marital Status, n (%) | |||||
| Single | 390 (50) | 368 (50) | 22 (45) | χ2=3.72 | 0.29 |
| Partnered | 227 (29) | 213 (29) | 14 (29) | ||
| Married | 116 (15) | 110 (15) | 6 (13) | ||
| Other | 48 (6) | 42 (6) | 6 (13) | ||
|
| |||||
| Education Level, n (%) | |||||
| No HS Grad | 157 (20) | 142 (19) | 15 (31) | χ2=4.87 | 0.18 |
| HS Grad/GED | 331 (42) | 315 (43) | 16 (33) | ||
| Some College | 183 (23) | 174 (24) | 9 (19) | ||
| College Grad | 110 (14) | 102 (14) | 8 (17) | ||
|
| |||||
| Employed, n (%) | 375 (48) | 355 (48) | 20 (41) | χ2=0.83 | 0.36 |
|
| |||||
| Insured (Health), % | 536 (69) | 507 (69) | 29 (60) | χ2=1.60 | 0.21 |
|
| |||||
| Yearly Income, % | |||||
| Less than $4800 | 248 (34) | 231 (33) | 17 (37) | Fischer’s Exact | 0.98 |
| $4800 – 14,400 | 318 (43) | 299 (43) | 19 (41) | ||
| $14,401 – 24,000 | 118 (16) | 111 (16) | 7 (15) | ||
| >$24,000 | 54 (7) | 51 (7) | 3 (7) | ||
Associations between DE and IPV, depressive symptomatology, and PTSD
Overall prevalence of DE among participants was 6%. No significant difference was present in prevalence between St. Thomas, St. Croix, and Baltimore. Over one-third (37%) of the participants reported symptoms indicative of depression, and 12% reported PTSD. Of the abused women, 75 (15%) reported emotional abuse only, 263 (53%) reported physical abuse, and 161 (32%) reported both physical and sexual abuse. The prevalence of same sex victimization was 8% among women reporting IPV. However, 33% of these women reported also experiencing abuse from a male partner or ex-partner, and therefore we had insufficient power to assess differences by sex of perpetrator.
All three exposure variables were significantly associated with reports of disordered eating in bivariate analyses (see Table 2). Abused women were significantly more likely to report DE, although their risk was lowered when controlling for demographics, PTSD, and depressive symptomatology. Depressive symptoms and PTSD independently conferred increased odds for DE among the participants (see Table 3).
Table 2.
Associations Between Disordered Eating (DE) and Intimate Partner Violence (IPV), Depressive symptomatology, and PTSD in a sample of African-American and African-Caribbean Women in Baltimore, MD and St. Thomas and St. Croix, USVI
| Disordered Eating | |||||
|---|---|---|---|---|---|
|
| |||||
| Sample Total (n=784) | No DE (n=737) | DE (n=47) | Test Statistic | p value | |
| IPV, % | |||||
| Controls | 282 (36) | 279 (38) | 3 (6) | Fischer’s Exact | <0.001 |
| Cases | 499 (64) | 454 (62) | 45 (94) | ||
|
| |||||
| Depressive Symptoms, n (%) | |||||
| No | 470 (63) | 461 (66) | 9 (20) | χ2=38.76 | <0.001 |
| Yes | 272 (37) | 236 (34) | 36 (80) | ||
|
| |||||
| PTSD | |||||
| No | 687 (88) | 657 (90) | 30 (63) | χ2=31.3 | <0.001 |
| Yes | 94 (12) | 76 (10) | 18 (37) | ||
|
| |||||
| IPV Type | |||||
| Emotional only | 75 (15) | 72 (16) | 3 (7) | Fischer’s Exact | >0.01 |
| Physical only | 263 (53) | 245 (54) | 18 (40) | ||
| Physical/Sexual | 161 (32) | 137 (30) | 24 (53) | ||
|
| |||||
| IPV Severity,* Mean score (SD) | |||||
|
| |||||
| Physical (range 0–53.9) | 12.2 (15.8) | 4.7 (8.3) | 12.2 (15.8) | t=5.16 | <0.001 |
| Sexual (range 0–11.5) | 0.53 (1.7) | 0.42 (1.4) | 1.7 (3.3) | t=4.77 | <0.001 |
|
| |||||
| Lethality from IPV* | |||||
| No risk | 99 (20) | 97 (21) | 2 (4) | Fischer’s Exact | 0.001 |
| Variable/increased risk | 272 (55) | 249 (55) | 23 (51) | ||
| Severe/Extreme risk | 128 (25) | 108 (24) | 20 (45) | ||
Table 3.
Odds Ratios (ORs) Between Intimate Partner Violence (IPV), Depressive symptomatology and Post-Traumatic Stress Disorder (PTSD) and Disordered Eating in a sample of African-American and African-Caribbean Women
| Disordered Eating (Entire Sample, n=790) | Disordered Eating (IPV cases only, n=499) | ||||
|---|---|---|---|---|---|
|
| |||||
| Unadjusted OR† (95% CI) | Adjusted OR†* (95% CI) | Unadjusted OR† (95% CI) | Adjusted OR†* (95% CI) | ||
| IPV | 9.22 (2.83, 29.94) | 3.85 (1.12, 13.32) | NA | NA | |
|
| |||||
| Depressive Symptoms | 7.81 (3.70, 16.49) | 4.85 (2.21, 10.67) | 6.20 (2.69, 14.26) | 4.28 (1.78, 10.34) | |
|
| |||||
| PTSD | 5.19 (2.76, 9.75) | 2.34 (1.17, 4.70) | 3.37 (1.77, 6.42) | 1.59 (0.73, 3.45) | |
|
| |||||
| Type of IPV | |||||
| Emotional | NA | NA | 1.00 | 1.00 | |
| Physical | NA | NA | 1.76 (0.51, 6.16) | 1.14 (0.30, 4.31) | |
| Physical + sexual | NA | NA | 4.20 (1.22, 14.44) | 1.11 (0.27, 4.51) | |
|
| |||||
| Severity of Violence | |||||
| Physical Scale | NA | NA | 1.05 (1.03, 1.08) | 1.02 (0.99, 1.05) | |
| Sexual Scale | NA | NA | 1.27 (1.13, 1.44) | 1.14 (0.97, 1.34) | |
|
| |||||
| Lethality from IPV* | |||||
| No risk | NA | NA | 1.00 | 1.00 | |
| Variable/increased risk | NA | NA | 4.48 (1.03, 19.36) | 2.73 (0.60, 12.35) | |
| Severe/Extreme risk | NA | NA | 8.98 (2.04, 39.42) | 2.68 (0.53, 13.48) | |
The Role of Severity of Violence and Risk for Lethality of Violence for Abused Women
Among women who experienced physical and sexual partner abuse (n=499; Table 2), depressive symptomatology, PTSD, severity of physical and sexual violence and risk for lethality differences were associated with DE. In unadjusted models (Table 3), depressive symptomatology, PTSD, and both physical and sexual abuse elevated a woman’s risk for DE. Additionally, increasing severity of physical and sexual violence both conferred additional risk for DE. Those women with moderate and severe risk for lethality from IPV were nearly 4.5 and 9 times more likely to report DE in the past year, respectively, compared to women at no risk for lethality in unadjusted analysis (OR 4.48, 95% CI 1.03, 19.36; OR 8.98, 95% CI 2.04, 39.42). When controlling for socio-demographic variables and other covariates, however, only depressive symptoms remained an independent predictor (Table 3).
Depressive symptomatology and PTSD as Mediators
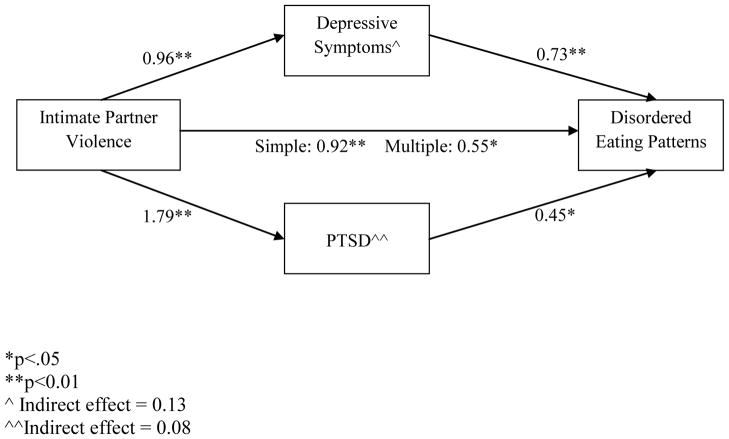
Depressive symptoms and PTSD mediated the relationship between IPV and disordered eating in the full sample (see Figure 1). For the entire sample, 48% of the total effect of IPV on DE was mediated, and depressive symptoms accounted for 62% of the indirect effect. Both the total indirect and direct effects were significant, thereby suggesting partial mediation.
Figure 1.
Visual display of coefficients from mediation analysis of the effects of depressive symptomatology and PTSD on the relationship between IPV and binary outcome of disordered eating in a sample of African-American and African-Caribbean women
*p<.05
**p<0.01
^ Indirect effect = 0.13
^^Indirect effect = 0.08
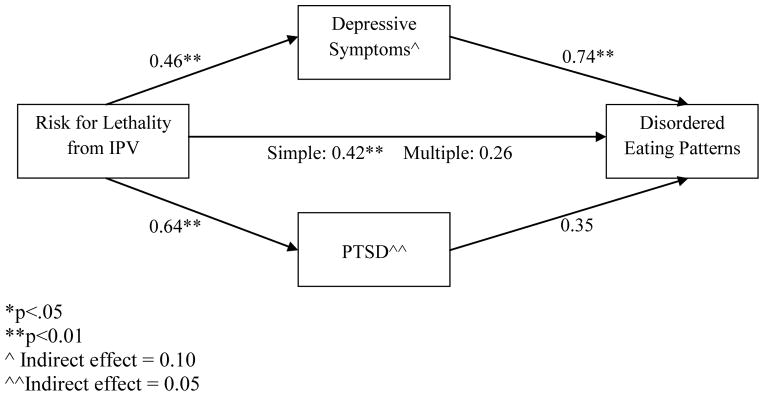
Among the women reporting abuse, depressive symptomatology mediated the relationship between the risk for lethality and disordered eating (see Figure 2). For this group, the indirect effect of depressive symptoms was significant, although that of PTSD was not. Depressive symptoms accounted for 67% of indirect effect. The total indirect effect was significant, while direct effects were non-significant, suggesting complete mediation of the relationship between risk for lethality and disordered eating through depressive symptoms.
Figure 2.
Visual display of coefficients from mediation analysis of the effects of depressive symptomatology and PTSD on the relationship between risk for lethality from IPV and binary outcome of disordered eating in a sample of African-American and African-Caribbean women
*p<.05
**p<0.01
^ Indirect effect = 0.10
^^Indirect effect = 0.05
Discussion
While our study measured the broader construct of disordered eating rather than diagnosed eating disorders, prevalence was relatively high among this population. Although the preponderance of DE literature has utilized college-aged, Caucasian women, our results support research that suggests race is not a protective factor against DE (Franko, Becker, Thomas, & Herzog, 2007; Taylor, Caldwell, Baser, Faison, & Jackson, 2007). We also found that younger age or lower levels of education conferred no additional risk for DE. Our prevalence of DE, depressive symptoms and PTSD among this help-seeking sample were all similar to those of other studies of African American women. Few studies of these disorders among African Caribbean women have been conducted.
We observed a positive relationship between all of the key exposure variables and DE among women in the full sample. Women reporting a history of abuse by their partner experienced significantly higher risk for DE than non-abused women, and women with physical abuse or sexual and physical abuse were more likely to experience DE than those with emotional abuse alone. Previous research demonstrated a similar role for sexual violence experiences on disordered eating (Jacobi, Hayward, de Zwaan, Kraemer, & Agras, 2004; Wonderlich et al., 2001), but our study was unique in its inclusion of physical, sexual, and emotional partner violence. DE has often been associated with a desire to exert personal control; this need may be enhanced in an abusive relationship in which personal control may be impeded. DE may also be used to deal with chronic and acute stress (Pecoraro, Reyes, Gomez, Bhargava, & Dallman, 2004; Timmerman, 2001), clearly present in abusive relationships (J. C. Campbell et al., 2002; J. C. Campbell, 2002). Recent studies of African American women also reported associations between trauma, stress and (binge) eating disorder (Harrington, Crowther, Payne Henrickson, & Mickelson, 2006; Harrington, Crowther, & Shipherd, 2010).
Women with depressive symptoms and PTSD were at elevated risk for DE in our study. These women may be using DE to cope with their depression (Adams, Katz, Beauchamp, Cohen, & Zavis, 1993), but a further analysis involving more measures of coping strategies would be required. PTSD symptoms conferred elevated risk for DE, and these findings corroborate previous research showing PTSD to co-occur with eating disorders. PTSD does not co-occur as often as other anxiety disorders (Godart, Flament, Perdereau, & Jeammet, 2002), but this may be attributed, in part, to the lack of routine assessment for PTSD in these studies (Godart et al., 2002). Additional research with better measures of DE and full rather than screening measures of PTSD are needed to further examine these relationships.
Considering depressive symptoms, PTSD, severity of physical and sexual violence, and severe risk for lethality from violence among women experiencing abuse, only depressive symptoms remained an independent risk factor DE. The relationship between risk for lethality and DE was fully mediated by the presence of depressive symptoms. It stands to reason that depression is the most important driver of DE, given that women in serious danger in an IPV relationship often become depressed and this in turn influences DE. Even so, given the direct association of IPV with DE in the full sample analysis, a relationship of IPV and DE remains that is not explained by increased depressive symptomatology from potential lethality. Again, additional research especially prospective studies with more precise measures of DE are needed, particularly measures of anorexia nervosa, binge eating and bulimia and analyses by ethnicity of patterns of disordered eating.
A noteworthy strength of this study is its focus on African American and African-Caribbean women of varying ages and educational backgrounds. Most studies on DE have focused on predominantly Caucasian and college samples of women. Our study contributes to the literature on factors associated with ED and DE in a non-college sample and within an understudied minority group.
This study also employed the ACASI method to collect data. Computerized methods have been shown to increase the likelihood of reporting of sensitive topics such as abuse over disclosing to an interviewer (Trautman, McCarthy, Miller, Campbell, & Kelen, 2007). It also automated the screening of participants and the random selection of controls, maximized participant confidentiality, facilitated administration for low-literacy participants, and enabled immediate identification and follow-up with participants who disclosed possible suicidality or who were at severe risk on the Danger Assessment.
The study, however, has limitations as well. First, the measure of DE used in the study relies on a single item and thus may not capture the range of behaviors associated with DE. Another limitation is related to the wide confidence intervals noted for some of the variables. This may be attributed to low prevalence of DE in a sample of this size, particularly among the non-abused control group. Unfortunately, statistical methods to correct for wide confidence intervals are not available for multilevel modeling at this time. Because the sample was recruited through medical settings, the findings may not reflect the experiences of general and diverse populations of women. In addition, the etiology of DE is complex and may stem from several aspects of a woman’s life, including cultural influences and past experiences. Some of these factors may have been present among the women in our study, but because these potentially causative factors were not included in the parent study, they could not be controlled for in this analysis. Finally, the cross-sectional design prevents us from making causal inferences of the study findings. However, our measures were such that women reported DE in the past year, while abuse measures encompassed past two-year and lifetime partner abuse. Despite these limitations, however, this study’s findings add to the relatively small empirical research base on the effect of IPV, depressive symptomatology and PTSD on disordered eating behavior.
Conclusions
This study strengthens the support for the IOM Committee on Women’s Health (2011) that recommended routine screening and brief counseling for IPV in primary care settings where DE is often first detected (Committee on Preventive Services for Women & Institute of Medicine, 2011). These co-occurring disorders (PTSD, depression, IPV, DE) need to be considered with the development of protocols to identify and provide counseling for IPV and other women’s health problems. When DE is identified or female patients with DE are referred for further assessment and mental health interventions, IPV should also be assessed. Similarly, female patients being treated for depression and/or PTSD should also be assessed for IPV and DE. Clinicians also need to be alerted to the prevalence of DE in African American women, especially those with histories of IPV and/or depression.
Treatment for DE, PTSD and/or depression clearly also needs to address IPV from the onset, so that women can be helped to be safer as they obtain interventions for other co-occurring problems. Health care professionals functioning under the belief that eating disorders occur less frequently among women of African heritage than among women of other ethnic groups could be less likely to detect them in these women, contributing to disparities in care and treatment. African American and African Caribbean women are less likely to have access to and utilize mental health services designed to treat eating disorders, making it imperative that culturally competent practitioners with preparation and training to recognize and treat eating disorders in ethnically-diverse patient populations are available in primary care and public health settings. Appropriate training and health policy interventions could help achieve optimal and equitable care for eating disorders across all ethnic groups in the United States.
Acknowledgments
The authors gratefully acknowledge the study participants and for contributions of the ACAAWS research study team We appreciate the contextual and cultural perspectives provided by Dr. Edith Ramsay-Johnson, Caribbean Exploratory Research Center and Lynn Spencer, Executive Director, Virgin Islands Domestic Violence And Sexual Assault Council, St Croix, VI. This research was supported by the Caribbean Exploratory Research Center, University of the Virgin Islands, NIMHD (P20MD002286). M.B. Lucea is supported by the NICHD (T32HD064428) and NIMHD (L60MD006272). B. Sabri is supported by the NICHD (T32HD064428). The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Ackard DM, Neumark-Sztainer D. Date violence and date rape among adolescents: Associations with disordered eating behaviors and psychological health. Child Abuse & Neglect. 2002;26(5):455–473. doi: 10.1016/S0145-2134(02)00322-8. [DOI] [PubMed] [Google Scholar]
- Adams PJ, Katz RC, Beauchamp K, Cohen E, Zavis D. Body dissatisfaction, eating disorders, and depression: A developmental perspective. Journal of Child and Family Studies. 1993;2(1):37–46. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. text revision. [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Basile K, Arias I, Desai S, Thompson MP. The differential association of intimate partner physical, sexual, psychological, and stalking violence and posttraumatic stress symptoms in a nationally representative sample of women. Journal of Traumatic Stress. 2004;17(5):413–421. doi: 10.1023/B:JOTS.0000048954.50232.d8. [DOI] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Stevens MR. The national intimate partner and sexual violence survey (NISVS): 2010 summary report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011. Retrieved from http://www.cdc.gov/ViolencePrevention/pdf/NISVS_Report2010-a.pdf. [Google Scholar]
- Brady SS. Lifetime family violence exposure is associated with current symptoms of eating disorders among both young men and women. Journal of Traumatic Stress. 2008;21(3):347–351. doi: 10.1002/jts.20335. [DOI] [PubMed] [Google Scholar]
- Breiding MJ, Black MC, Ryan GW. Prevalence and risk factors of intimate partner violence in eighteen U.S. States/Territories, 2005. American Journal of Preventive Medicine. 2008;34(2):112–118. doi: 10.1016/j.amepre.2007.10.001. [DOI] [PubMed] [Google Scholar]
- Brewerton TD. Eating disorders, trauma, and comorbidity: Focus on PTSD. Eating Disorders. 2007;15:285–304. doi: 10.1080/10640260701454311. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Snow Jones A, Dienemann J, Kub J, Schollenberger J, O’Campo P, Wynne C. Intimate partner violence and physical health consequences. Archive of Internal Medicine. 2002;162:1157–1163. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Webster D, Glass N. The danger assessment: Validation of a lethality risk assessment instrument for intimate partner femicide. Journal of Interpersonal Violence. 2008;000(00) doi: 10.1177/0886260508317180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359:1331–1336. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- Cascardi M, O’Leary KD, Schlee KA. Co-occurrence and correlates of post-traumatic stress disorder and major depression in physically abused women. Journal of Family Violence. 1999;3:227–247. [Google Scholar]
- Committee on Preventive Services for Women, & Institute of Medicine. Clinical preventive services for women: Closing the gaps. 1. Washington, DC: National Acadamies Press; 2011. [Google Scholar]
- Danielson KK, Moffitt TE, Caspi A, Silva PA. Comorbidity between abuse of an adult and DSM-III-R mental disorders: Evidence from an epidemiological study. American Journal of Psychiatry. 1998;155(1):131–133. doi: 10.1176/ajp.155.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dansky BS, Brewerton TD, Kilpatrick DG, O’Neil PM. The national women’s study: Relationship of victimization and posttraumatic stress disorder to bulimia nervosa. International Journal of Eating Disorders. 1997;21(3):213–228. doi: 10.1002/(SICI)1098-108X(199704)21:3<213::AID-EAT2>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- Demaris A, Kaukinen C. Violence victimization and women’s mental and physical health: Evidence from a national sample. Journal of Research in Crime and Delinquency. 2005;42(4):384–411. [Google Scholar]
- Franko DL, Becker AE, Thomas JJ, Herzog DB. Cross-ethnic differences in eating disorder symptoms and related distress. International Journal of Eating Disorders. 2007;40(2):156–164. doi: 10.1002/eat.20341. [DOI] [PubMed] [Google Scholar]
- Godart NT, Flament MF, Perdereau F, Jeammet P. Comorbidity between eating disorders and anxiety disorders: A review. International Journal of Eating Disorders. 2002;32(3):253–270. doi: 10.1002/eat.10096. [DOI] [PubMed] [Google Scholar]
- Golding J. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. Journal of Family Violence. 1999;14(2):99–132. [Google Scholar]
- Hall Smith P, Earp JA, DeVellis R. Measuring battering: Development of the women’s experience with battering (WEB) scale. Women’s Health: Research on Gender, Behavior, and Policy. 1995;1(4):273–288. [PubMed] [Google Scholar]
- Harrington EF, Crowther JH, Payne Henrickson HC, Mickelson KD. The relationships among trauma, stress, ethnicity, and binge eating. Cultural Diversity and Ethnic Minority Psychology. 2006;12(2):212–229. doi: 10.1037/1099-9809.12.2.212. [DOI] [PubMed] [Google Scholar]
- Harrington EF, Crowther JH, Shipherd JC. Trauma, binge eating, and the “strong black woman”. Journal of Consulting and Clinical Psychology. 2010;78(4):469–479. doi: 10.1037/a0019174. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biological Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin. 2004;130(1):19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- Kelly UA. Symptoms of PTSD and major depression in latinas who have experienced intimate partner violence. Issues in Mental Health Nursing. 2010;31:119–127. doi: 10.3109/01612840903312020. [DOI] [PubMed] [Google Scholar]
- Kong S, Bernstein K. Childhood trauma as a predictor of eating psychopathology and its mediating variables in patients with eating disorders. Journal of Clinical Nursing. 2009;18(13):1897–1907. doi: 10.1111/j.1365-2702.2008.02740.x. [DOI] [PubMed] [Google Scholar]
- Mackinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17(2):144–158. doi: 10.1177/0193841X9301700202. [DOI] [Google Scholar]
- Marshall LL. Development of the severity of violence against women scales. Journal of Family Violence. 1992;7(2):103. [Google Scholar]
- Mazzeo SE, Mitchell KS, Williams LJ. Anxiety, alexithymia, and depression as mediators of the association between childhood abuse and eating disordered behavior in african american and european american women. Psychology of Women Quarterly. 2008;32(3):267–280. doi: 10.1111/j.1471-6402.2008.00435.x. [DOI] [Google Scholar]
- McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy. JAMA. 1992;267:3176–3178. doi: 10.1001/jama.267.23.3176. [DOI] [PubMed] [Google Scholar]
- Meltzer-Brody S, Zerwas S, Leserman J, Holle AV, Regis T, Bulik C. Eating disorders and trauma history in women with perinatal depression. Journal of Women’s Health. 2011;20(6):863–870. doi: 10.1089/jwh.2010.2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pecoraro N, Reyes F, Gomez F, Bhargava A, Dallman MF. Chronic stress promotes palatable feeding, which reduces signs of stress: Feedforward and feedback effects of chronic stress. Endocrinology. 2004;145(8):3754–3762. doi: 10.1210/en.2004-0305. [DOI] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Sheikh JI. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry. 2003;9(1):9–14. [Google Scholar]
- Seedat S, Stein M, Forde D. Association between physical partner violence, posttraumatic stress, childhood trauma, and suicide attempts in a community sample of women. Violence and Victims. 2005;20(1):87–98. [PubMed] [Google Scholar]
- South Carolina Department of Mental Health. Eating disorder statistics. 2006 Retrieved 07/01, 2011, from http://www.state.sc.us/dmh/anorexia/statistics.htm.
- StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Stith SM, Smith DB, Penn CE, Ward DB, Tritt D. Intimate partner physical abuse perpetration and victimization risk factors: A meta-analytic review. Aggression and Violent Behavior. 2004;10(1):65–98. doi: 10.1016/j.avb.2003.09.001. [DOI] [Google Scholar]
- Sullivan TP, Holt LJ. PTSD symptom clusters are differentially related to substance use among community women exposed to intimate partner violence. Journal of Traumatic Stress. 2008;21(2):173–180. doi: 10.1002/jts.20318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JY, Caldwell CH, Baser RE, Faison N, Jackson JS. Prevalence of eating disorders among blacks in the National Survery of American Life. International Journal of Eating Disorders. 2007;40:s10–s14. doi: 10.1002/eat.20451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timmerman GM. The relationship between basic need satisfaction and emotional eating. Issues Ment Health Nurs. 2001;22(7):691–701. doi: 10.1080/01612840119628. [DOI] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. Research Report National Institute of Justice. 2000. Extent, nature, and consequences of intimate partner violence. [Google Scholar]
- Trautman DE, McCarthy ML, Miller N, Campbell JC, Kelen GD. Intimate partner violence and emergency department screening: Computerized screening versus usual care. Annals of Emergency Medicine. 2007;49(4):526–534. doi: 10.1016/j.annemergmed.2006.11.022. [DOI] [PubMed] [Google Scholar]
- Vince EP, Walker I. A set of meta-analytic studies on the factors associated with disordered eating. 2008. [Google Scholar]
- Vos T, Astbury J, Piers LS, Magnus A, Heenan M, Stanley L, Webster K. Measuring the impact of intimate partner violence on the health of women in Victoria, Australia. Bulletin of the World Health Organization. 2006;84:739–744. doi: 10.2471/blt.06.030411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wonderlich SA, Crosby RD, Mitchell JE, Thompson KM, Redlin J, Demuth G, Haseltine B. Eating disturbance and sexual trauma in childhood and adulthood. International Journal of Eating Disorders. 2001;30(4):401–412. doi: 10.1002/eat.1101. [DOI] [PubMed] [Google Scholar]