Abstract
Fibromyalgia is a chronic widespread pain disorder commonly associated with comorbid symptoms, including fatigue and nonrestorative sleep. As in the management of other chronic medical disorders, the approach for fibromyalgia management follows core principles of comprehensive assessment, education, goal setting, multimodal treatment including pharmacological (eg, pregabalin, duloxetine, milnacipran) and nonpharmacological therapies (eg, physical activity, behavioral therapy, sleep hygiene, education), and regular education and monitoring of treatment response and progress. Based on these core management principles, this review presents a framework for primary care providers through which they can develop a patient-centered treatment program for patients with fibromyalgia. This proactive and systematic treatment approach encourages ongoing education and patient self-management and is designed for use in the primary care setting.
Abbreviations and Acronyms: CBT, cognitive behavioral therapy; FIQ, Fibromyalgia Impact Questionnaire; PCP, primary care provider
Fibromyalgia is a chronic widespread pain disorder estimated to affect 2% to 5% of the US adult population and 0.5% to 5% of other Western populations. 1-4 In addition to widespread pain present for more than 3 months, patients with fibromyalgia often report fatigue, nonrestorative sleep, cognitive dysfunction, stiffness, and mood disturbance. 5-7 With growing recognition of fibromyalgia by patients and health care professionals, more people are seeking medical help for chronic pain conditions and making frequent visits to their health care practitioner. 8 This has resulted in fibromyalgia becoming a clinical problem commonly seen in primary care and an economic burden on health care resources. 9,10
The management of patients with fibromyalgia in the primary care setting may be challenging for several reasons. Although there is increasing evidence about the underlying pathophysiologic mechanisms involved in fibromyalgia, 11,12 clinicians may find it difficult to communicate this emerging information to their patients. Also, many clinicians report difficulty in identifying and diagnosing fibromyalgia. 7,13 Finally, patients with fibromyalgia are sometimes perceived as difficult to treat, 14 especially in the primary care office where time and resources may be limited for complex presenting problems. This review is the third and final installment of a series of concise reviews that addresses challenges in fibromyalgia diagnosis, treatment, and management. The series was developed by the FibroCollaborative, an initiative organized and funded by Pfizer in which a diverse group of experts on fibromyalgia provided state-of-the-art information on the understanding, assessment, and treatment of fibromyalgia. Clauw et al 12 presented an update on pathophysiologic mechanisms in fibromyalgia. Arnold et al 7 described an approach to the differential diagnosis of fibromyalgia in primary care. This final review provides a framework for primary care providers (PCPs) to treat patients with fibromyalgia effectively as part of a multidisciplinary approach with the goal of improving patient education, symptom management, health status, and outcomes. The framework is similar to the integrated approach taken in the long-term care of other chronic health conditions, such as diabetes, asthma, and hypertension.
A Framework for the Management of Patients With Fibromyalgia
Educate Patients and Explain Fibromyalgia
As in other chronic conditions requiring ongoing management, education plays an essential role in fibromyalgia management 15-17 and can be integrated into a treatment plan after diagnosis and continued throughout follow-up. Confirming the diagnosis and describing its clinical picture can itself have a positive impact on patients with fibromyalgia, in particular giving them validation and reassurance. 18 For some patients, this alone may improve satisfaction with health status. 19 Furthermore, when the PCP explains fibromyalgia, patients may feel reassured that their symptoms have a cause. 18 When a diagnosis is given, an overview of fibromyalgia's pathophysiology, symptoms, treatment, and prognosis should be provided to aid understanding, acceptance, and self-management. The following examples of common patient questions and possible responses use terms that are understandable to the patient.
What is fibromyalgia?
-
•
Evidence suggests that fibromyalgia is a medical condition in which there are changes in how the central nervous system processes pain. Research shows that changes in the central nervous system cause the brain to process pain signals abnormally in fibromyalgia, leading to pain becoming amplified. It is as if the “volume control setting” for pain is abnormally high. In other words, a person with fibromyalgia has a low pain threshold and may experience pain with a lower stimulus.
-
•
Many of these central nervous system changes also influence sleep, mood, and energy. This helps explain some of the other common symptoms.
What causes fibromyalgia?
-
•
The exact causes of fibromyalgia are not fully understood.
-
•
Evidence suggests that genetic and environmental factors may predispose individuals to development of fibromyalgia.
Can fibromyalgia be cured?
-
•
Fibromyalgia is similar to other chronic conditions in that it cannot be cured, but symptoms can be controlled.
-
•
New treatments are available, and much can be done to improve symptoms and function to enable individuals to get back to doing more of the things that they enjoy and that are important to them.
How is fibromyalgia treated?
-
•
No single treatment works for every symptom.
-
•
Fibromyalgia is usually treated using a combination of approaches, including medications, physical activity/exercise, sleep hygiene, and cognitive behavioral therapy (CBT).
-
•
Treatment requires patients to be active participants in their care.
Time for patient education is often restricted in busy practices, making it important to plan and make optimal use of existing resources. Examples of educational sources in books, on the Internet, and in the community include Managing Pain Before It Manages You by Caudill (third edition, 2009); The Fibromyalgia Help Book by Fransen and Russell (1996); The Pain Survival Guide by Turk and Winter (2006); industry-sponsored websites (eg, www.knowfibro.com, www.fibrocenter.com, www.fibrotogether.com); and patient advocacy organizations (www.painfoundation.org, www.healthywomen.org, www.fmcpaware.org).
Organizing small group lectures for individuals with fibromyalgia and their family members and using clinical support staff to provide supplemental education are also efficient ways to provide fibromyalgia information. 16,17 Education should include management of expectations early in the course of therapy. Setting basic expectations for how the clinician and patient will work together can help to establish a productive and efficient partnership and minimize frustration. 20 It can be helpful to discuss the following:
-
•
How frequent office visits will be. Early in treatment, it may be useful to see patients with fibromyalgia more often and to initiate nonpharmacological therapies in addition to medications to emphasize the important role of multimodal treatment. More frequent visits help clinicians manage early adverse effects of treatment and may improve patients' engagement in all therapies.
-
•
How much time is available at each visit.
-
•
How to prioritize treatment goals. It is important to discuss the need to take a step-by-step approach rather than trying to solve everything at once.
-
•
The expected outcomes from treatment and the long-term prognosis of fibromyalgia. It can be helpful to inform patients of the limitations of treatments as well as potential benefits. For example, medications will help to reduce symptoms but may not eliminate them altogether. However, a reduction in symptoms may allow the patient to engage in nonpharmacological treatments, such as exercise.
Set Treatment Goals
Fibromyalgia, like other chronic conditions, significantly affects multiple domains of a patient's life, including the ability to engage in everyday activities and work. 5,6 It is therefore important to assess the impact of fibromyalgia across multiple domains at diagnosis and then to work collaboratively in a patient-centered approach during follow-up sessions to develop and prioritize treatment goals with a focus on the domains most affected. A number of questionnaires and assessment tools have been developed and validated to assess pain, patient function (physical, emotional, cognitive, social), and health-related quality of life associated with fibromyalgia. 21-26 Using assessment tools in goal setting at diagnosis gives a “baseline” health status from which progress can be tracked.
Tools made specifically for fibromyalgia include the Fibromyalgia Impact Questionnaire (FIQ) 21 and the more recently revised version (FIQR). 24 The FIQR assesses 3 domains (function, overall impact, symptoms) using 21 check-box questions, and it can be completed in less than 2 minutes. 24 Also based on the FIQ, the mVASFIQ assesses 5 symptom domains using 7 scale questions designed for symptom quantification and pharmacological management, combining visual analog scale scores based on FIQ domains. 25
Although yet to be validated to track fibromyalgia progress over time, the 2010 American College of Rheumatology diagnostic criteria 26 use symptom severity scores and the widespread pain index to provide numerical scores that can be tracked over time. Individual clinicians can develop other scales based on numerical rating scales or visual analog scale (0-10 cm or 0-100 mm) 22,23 to provide simple and quick means of assessing symptoms. These scales are adaptable to different domains (eg, pain, sleep quality, mood) and can provide a distinct, comparable score to track symptoms. It is also important for patients to focus on achievable goals related to improved function, in addition to change in individual symptoms, such as pain.
The key to effective patient management is for PCPs to research, select, and use the most appropriate tools for each patient and to provide a clear overview of what the results mean for the patient and his or her long-term fibromyalgia management. A patient-centered management plan with prioritized treatment goals should be developed on the basis of these assessments. Importantly, goals should be specific, realistic, and measurable and should reflect patients' priorities. 27 Establishing these treatment goals early will help to give structure for follow-up visits, enabling goals to be achieved and progress to be tracked.
Apply a Multimodal Treatment Approach
Because widespread pain and tenderness, along with associated symptoms such as fatigue, sleep disturbance, cognitive difficulties, and mood disturbances, are characteristics of fibromyalgia, 26,28 no single treatment targets all symptoms. Accordingly, a comprehensive multimodal treatment plan is recommended, integrating (1) ongoing patient education, (2) pharmacotherapy, and (3) nonpharmacological therapies ( Figure). Using these principles, the PCP must consider carefully the most appropriate treatment regimen, starting at diagnosis but continuing as the patient's health state changes. Consistent with the treatment approach in other chronic diseases, a number of health care specialists may be required to collaborate on the patient's care, including the patient taking responsibility for self-management and adherence to all aspects of the treatment plan. As for any chronic condition, effective management of fibromyalgia should be viewed through a proactive, patient-centric approach. To achieve this, physicians should know their patients, know their community, and know their team ( Figure).
FIGURE.
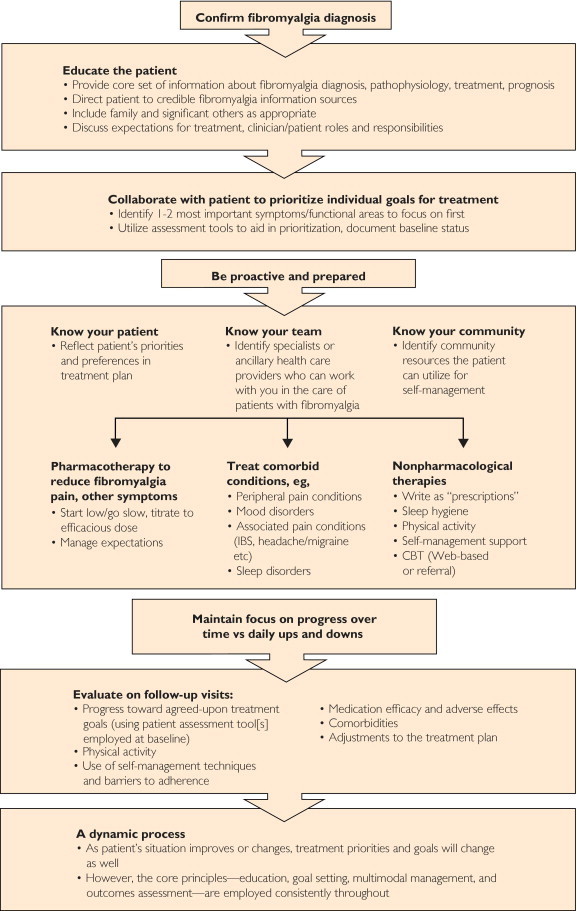
Core principles for an integrated approach for fibromyalgia management. CBT = cognitive behavioral therapy; IBS = irritable bowel syndrome.
Knowing the patient involves monitoring individuals over the long term for their risk of becoming overwhelmed or unable to engage in the recommended treatment plan. Much of fibromyalgia management depends on what patients do, or do not do, and what resources are available to help them outside of the PCP's office. Health plan barriers may limit access to nonpharmacological treatments, therapists, or fitness facilities. However, by knowing their community, clinicians can highlight alternative options. For example, community resources, such as the YMCA or similar health clubs, may be available for exercise, and Web-based CBT may be an alternative to face-to-face therapist counseling. 29 Through knowing their team, PCPs are ideally positioned to coordinate care across specialties and to encourage and reinforce the importance of ongoing self-management.
Ongoing Education
Continued education after diagnosis is a key objective of this management framework. As part of this ongoing education, the importance of adherence to all aspects of the treatment program should be highlighted, and nonadherence with pharmacological or nonpharmacological therapies should be addressed, particularly for medications that do not produce an instant, noticeable effect on symptoms. We advise a “start low, go slow” strategy for both pharmacotherapy and any physical exercise program, which should limit adverse events and better assure adherence to any treatment regimen.
Pharmacological Therapies
The US Food and Drug Administration (FDA) has approved 3 medications for fibromyalgia (pregabalin, duloxetine, and milnacipran), which act differently to influence transmission of sensory signals via central nociceptive pathways. 30 Approval of these medications contributed to the acceptance of fibromyalgia as a legitimate, treatable condition. As noted earlier in this article, patients and their families should have their expectations managed on initiation of any therapy, with PCPs reiterating that although medications cannot cure the underlying disease, medications can improve symptoms and function. 31-34
Pregabalin is an alpha2delta calcium channel ligand; duloxetine and milnacipran are serotonin and norepinephrine reuptake inhibitors ( Table). Alpha2delta calcium channel ligands are thought to act in part by reducing the activity of excitatory neurotransmitters (eg, glutamate), whereas serotonin and norepinephrine reuptake inhibitors act largely by increasing norepinephrine and serotonin and thereby increasing activity in the descending inhibitory pain pathways. 30,35 Efficacy for providing symptomatic benefit to patients with fibromyalgia has been demonstrated in specifically designed studies. Other medications, such as tricyclic medications (eg, amitriptyline, cyclobenzaprine), gabapentin, tramadol, fluoxetine, and sodium oxybate, are also used for symptomatic management and have demonstrated efficacy in randomized controlled trials for fibromyalgia (see article by Arnold 36 and references therein). Although none are specifically indicated by the FDA for the management of fibromyalgia, the lower cost of generic products may lead some physicians to prescribe them if patients cannot afford the FDA-approved medications. Patients with fibromyalgia may also use other analgesics, such as nonsteroidal anti-inflammatory agents and opioids, for pain management; however, their efficacy has not been demonstrated in trials of patients with fibromyalgia. 36 As part of knowing their patients, PCPs should recommend the most appropriate treatments for each individual patient, according to his or her clinical history and presentation. Further detail regarding a stepwise approach to selecting medications that could be integrated into the fibromyalgia management framework has been published elsewhere. 36
TABLE.
Summary of Treatment Regimens for Pharmacological and Nonpharmacological Therapies Used in Multimodal Management of Patients With Fibromyalgia a
| Therapy | Representative treatment regimen | Outcomes b |
|---|---|---|
| Pharmacotherapy | ||
| Pregabalin (alpha2delta ligand) | Start at 75 mg BID and up-titrate to 300-450 mg/d (150-225 mg twice a day) c |
|
| Duloxetine (SNRI) | Start at 30 mg/d and up-titrate to 60 mg once daily d |
|
| Milnacipran (SNRI) | Start at 12.5 mg/d and up-titrate to 50 mg twice a day e |
|
| Nonpharmacological | ||
| Education | Provide core information about fibromyalgia diagnosis, physiology, treatment, prognosis, importance of exercise, sleep. Manage expectations |
|
| Physical activity | Start low, go slow; eg, walk 10 min/d, build to 30-60 min of low or moderate activity up to 2-3 times/wk |
|
| CBT/Web-based CBT | CFIDS and Fibromyalgia Self-Help (www.cfidsselfhelp.org; www.treatcfsfm.org) Arthritis Foundation's Fibromyalgia Self-Help Course Online self-help courses, tools, books, and CDs Face-to-face CBT counseling |
|
| Sleep hygiene | Make sleep routine a priority. Optimize relaxing sleep environment. Provide advice on diet and exercise: avoid nighttime stimulants (eg, coffee); exercise during the day; hide clock |
|
AE = adverse event; BPI = Brief Pain Inventory; CBT = cognitive behavioral therapy; CFIDS = chronic fatigue and immune dysfunction syndrome; FIQ = Fibromyalgia Impact Questionnaire; HRQoL = health-related quality of life; NRS = numerical rating scale; PGIC = Patient Global Impression of Change; SF = short form; SNRI = serotonin and norepinephrine reuptake inhibitor; VAS = visual analog scale.
Safety is based on the most frequently occurring adverse reactions (≥5% and twice placebo for pregabalinc and duloxetined or ≥5% and greater than placebo for milnaciprane).
For further detail, see prescribing information: http://labeling.pfizer.com/ShowLabeling.aspx?id=561.
For further detail, see prescribing information: http://pi.lilly.com/us/cymbalta-pi.pdf.
For further detail, see prescribing information: http://www.frx.com/pi/Savella_pi.pdf.
Nonpharmacological Therapies
Several nonpharmacological approaches are beneficial to patients with fibromyalgia, reducing pain and improving function ( Table). We recommend incorporating appropriate nonpharmacological approaches into the overall treatment plan as written “prescriptions” to highlight their equal importance to medications. Among the nonpharmacological approaches that have demonstrated efficacy in clinical trials are exercise; sleep hygiene; some forms of CBT, including Web-based CBT; and ongoing patient education. 15,17,29,37-41 Furthermore, other nonpharmacological approaches, such as yoga, massage, and other types of physical therapy, may also be considered, 42 although more study is needed to assess their efficacy in fibromyalgia. An integrated approach is key, and the importance of self-management should be highlighted. For example, the benefits of exercise were enhanced in one study when exercise was combined with a targeted self-management program (the Arthritis Foundation's Fibromyalgia Self-Help Course). 17 Providing materials that promote basic self-management techniques to accomplish daily activities and manage symptoms, in addition to suggesting ways to incorporate wellness activities into daily life, should form the foundation of guided self-management. Family members and significant others should be actively involved from the outset, particularly when symptoms of fibromyalgia have placed a strain on these relationships. In fact, integrating family members into the treatment program may aid effectiveness. 43 It is also important for PCPs themselves to ensure that they are sufficiently knowledgeable about these nonpharmacological practices to give their patients succinct advice and recommendations for self-management. This is particularly needed for treatments such as CBT, a term often used in the lay press to encompass a wide range of disparate approaches to therapy. The key ingredients in CBT are problem solving, stress management, and self-control.
Inadequate sleep is a common and problematic symptom of fibromyalgia, and sleep hygiene is an area of growing interest. Indeed, disrupting slow-wave sleep for consecutive nights is associated with decreased pain threshold, increased musculoskeletal pain, and fatigue, 44 suggesting an interrelationship between sleep and pain. Behavioral strategies aimed at improving sleep hygiene (some are outlined in the Table) can help individuals improve sleep quality and, if used regularly, may lead to additional benefits, such as improved mood and mental clarity, less fatigue, and less pain. 39 Primary care providers should also consider the possibility of a comorbid sleep disorder and referral to specialists in the evaluation of sleep problems. 7 Collaboration with other clinicians in the evaluation and treatment of patients with fibromyalgia is part of PCPs knowing their team.
Track Progress
The course of fibromyalgia is not straightforward, with pain and symptoms fluctuating over time. 45 Given the complexity and chronic nature of fibromyalgia, and the impact on patients' daily lives, there is a clear need to track progress. Tracking progress will help patients focus on self-management and encourage motivation, particularly after a flare-up or period of poor health. For some chronic diseases, protocols are provided that identify variables to track over time. Currently no such protocols exist for fibromyalgia. However, several questionnaires and assessment tools are available (discussed earlier in this article) that can and should be selectively employed to track patient progress.
Conclusion
Many complex chronic diseases are effectively managed in primary care, supported by collaboration with health care specialists in a patient-centered approach. Management of patients with fibromyalgia in the primary care setting should be approached in a similar manner, by implementation of a chronic care framework based on core principles of education, goal setting, multidisciplinary management, routine monitoring, and outcomes assessment (focusing on improvement in symptoms, physical and emotional functioning, and overall health-related quality of life). Follow-up should involve specific resources that help health care professionals educate patients and their families to engage in self-management and carry out ongoing assessment to track disease status over time. Because no single treatment approach for fibromyalgia targets all symptoms or will manage every patient, there is a clear need for a dynamic, multifaceted approach to management. Using these principles, PCPs, in association with other health care professionals and patients themselves, can form an active health care team to enhance well-being and reduce patient suffering.
Acknowledgments
Medical writing support was provided by Karen Burrows, MPhil, of UBC Scientific Solutions and was funded by Pfizer. The authors thank Andrew Clair, PhD, of Pfizer for his critical review and input during development of the manuscript.
Footnotes
See end of article for correct answers to questions.
A list of additional members of the FibroCollaborative is provided at the end of the article.
Additional Members of the FibroCollaborative: Kenneth Barrow, PA-C, MHS, Independence Back Institute, Wilmington, NC; Lucinda Bateman, MD, Fatigue Consultation Clinic Inc, Salt Lake City, UT; Larry Culpepper, MD, MPH, Boston University, Boston, MA; Cassandra Curtis, MD, American Health Network, Greenfield, IN; Yvonne D'Arcy, MS, CRNP, CNS, Suburban Hospital–Johns Hopkins Medicine, Bethesda, MD; Kevin B. Gebke, MD, Indiana University, Indianapolis; Robert Gerwin, MD, Pain and Rehabilitation Medicine, Bethesda, MD; Don L. Goldenberg, MD, Newton-Wellesley Hospital, Newton, MA; James I. Hudson, MD, ScD, McLean Hospital/Harvard Medical School, Belmont, MA; Rakesh Jain, MD, MPH, Clinical Research Center, Lake Jackson, TX, University of Texas Medical School, Houston; Texas Tech School of Medicine, Midland; Arnold L. Katz, MD, Overland Park Regional Medical Center, Overland Park, KS; Andrew G. Kowal, MD, Tufts University, Burlington, MA; Charles Lapp, MD, Duke University, Charlotte, NC; Michael McNett, MD, The Paragon Clinic for Fibromyalgia & Muscular Pain, Chicago, IL; Philip J. Mease, MD, Swedish Medical Center, Seattle, WA; Danielle Petersel, MD, Pfizer Inc, New York, NY; I. Jon Russell, MD, PhD, University of Texas, San Antonio; Stephen M. Stahl, MD, PhD, University of California, San Diego; Roland Staud, MD, UF Center for Musculoskeletal Pain Research, University of Florida, Gainesville; Alvin F. Wells, MD, PhD, Rheumatology & Immunotherapy Center, Oak Creek, WI.
Potential Competing Interests: Dr Arnold has received grants/research support from Eli Lilly and Company, Pfizer, Cypress Biosciences, Boehringer Ingelheim, Forest Laboratories, and Novartis. She is a consultant for Eli Lilly and Company, Pfizer, Cypress Biosciences, Forest Laboratories, Takeda, AstraZeneca, sanofi, Grünenthal, Johnson & Johnson, and Daiichi Sankyo. Dr Clauw has received grants/research support from Pfizer, Forest Laboratories, Merck, and Nuvo. He is a consultant for Pfizer, Eli Lilly and Company, Forest Laboratories, Cypress Biosciences, Pierre Fabre Pharmaceuticals, UCB, Merck, Nuvo, Abbott, Johnson & Johnson, and AstraZeneca. Dr Clauw is a member of the advisory boards for Pfizer, Eli Lilly and Company, Forest Laboratories, Cypress Biosciences, Pierre Fabre Pharmaceuticals, UCB, and AstraZeneca. Dr Dunegan has received grants from and been a consultant to Purdue Pharma, Ortho-McNeil-Janssen, and Pfizer. Dr Turk has received grants from Ortho-McNeil-Janssen and Endo Pharmaceuticals. He is a consultant to Ironwood Pharmaceuticals, Johnson & Johnson, Nevro, Pfizer, and Phillips Respironics. The FibroCollaborative was organized and sponsored by Pfizer.
CORRECT ANSWERS: 1. b, 2. e, 3. e, 4. d, 5. c
Questions About Fibromyalgia
-
1A framework for managing patients with fibromyalgia consists of all of the following except
-
aEducate patients and explain fibromyalgia
-
bEmphasize that earlier diagnosis and treatment can lead to a cure
-
cSet treatment goals and expectations
-
dApply a multimodal treatment approach
-
eTrack progress and manage expectations
-
a
-
2Pharmacological agents approved by the Food and Drug Administration for the management of fibromyalgia include
-
aDuloxetine, pregabalin, amitriptyline
-
bGabapentin, milnacipran, duloxetine
-
cPregabalin, duloxetine, cyclobenzaprine
-
dVenlafaxine, gabapentin, duloxetine
-
ePregabalin, duloxetine, milnacipran
-
a
-
3Nonpharmacological approaches to fibromyalgia management include all of the following except
-
aEducation
-
bSleep hygiene
-
cCognitive behavioral therapy
-
dPhysical activity
-
eHigh-intensity aerobics
-
a
-
4Which assessment tool was specifically developed for use in patients with fibromyalgia?
-
aNumerical rating scale
-
bPatient Global Impression of Change
-
cVisual analog scale
-
dRevised Fibromyalgia Impact Questionnaire
-
eBrief Pain Index
-
a
-
5This framework approach to self-management of fibromyalgia is based on which clinician type as the care coordinator?
-
aRheumatologist
-
bPain specialist
-
cPrimary care provider
-
dPsychiatrist
-
eNeurologist
-
a
References
- 1.Wolfe F., Ross K., Anderson J., Russell I.J., Hebert L. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38(1):19–28. doi: 10.1002/art.1780380104. [DOI] [PubMed] [Google Scholar]
- 2.White K.P., Harth M. Classification, epidemiology, and natural history of fibromyalgia. Curr Pain Headache Rep. 2001;5(4):320–329. doi: 10.1007/s11916-001-0021-2. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence R.C., Felson D.T., Helmick C.G. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Branco J.C., Bannwarth B., Failde I. Prevalence of fibromyalgia: a survey in five European countries. Semin Arthritis Rheum. 2010;39(6):448–453. doi: 10.1016/j.semarthrit.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Arnold L.M., Crofford L.J., Mease P.J. Patient perspectives on the impact of fibromyalgia. Patient Educ Couns. 2008;73(1):114–120. doi: 10.1016/j.pec.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choy E.H., Mease P.J. Key symptom domains to be assessed in fibromyalgia (outcome measures in rheumatoid arthritis clinical trials) Rheum Dis Clin North Am. 2009;35(2):329–337. doi: 10.1016/j.rdc.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Arnold L.M., Clauw D.J., McCarberg B.H., FibroCollaborative Improving the recognition and diagnosis of fibromyalgia. Mayo Clin Proc. 2011;86(5):457–464. doi: 10.4065/mcp.2010.0738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hootman J.M., Helmick C.G., Schappert S.M. Magnitude and characteristics of arthritis and other rheumatic conditions on ambulatory medical care visits, United States, 1997. Arthritis Rheum. 2002;47(6):571–581. doi: 10.1002/art.10791. [DOI] [PubMed] [Google Scholar]
- 9.Berger A., Dukes E., Martin S., Edelsberg J., Oster G. Characteristics and healthcare costs of patients with fibromyalgia syndrome. Int J Clin Pract. 2007;61(9):1498–1508. doi: 10.1111/j.1742-1241.2007.01480.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Silverman S., Dukes E.M., Johnston S.S., Brandenburg N.A., Sadosky A., Huse D.M. The economic burden of fibromyalgia: comparative analysis with rheumatoid arthritis. Curr Med Res Opin. 2009;25(4):829–840. doi: 10.1185/03007990902728456. [DOI] [PubMed] [Google Scholar]
- 11.Russell I.J., Larson A.A. Neurophysiopathogenesis of fibromyalgia syndrome: a unified hypothesis. Rheum Dis Clin North Am. 2009;35(2):421–435. doi: 10.1016/j.rdc.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 12.Clauw D.J., Arnold L.M., McCarberg B.H., FibroCollaborative The science of fibromyalgia. Mayo Clin Proc. 2011;86(9):907–911. doi: 10.4065/mcp.2011.0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choy E., Perrot S., Leon T. A patient survey of the impact of fibromyalgia and the journey to diagnosis. BMC Health Serv Res. 2010;10:102. doi: 10.1186/1472-6963-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asbring P., Närvänen A.L. Ideal versus reality: physicians perspectives on patients with chronic fatigue syndrome (CFS) and fibromyalgia. Soc Sci Med. 2003;57(4):711–720. doi: 10.1016/s0277-9536(02)00420-3. [DOI] [PubMed] [Google Scholar]
- 15.Burckhardt C.S., Mannerkorpi K., Hedenberg L., Bjelle A. A randomized, controlled clinical trial of education and physical training for women with fibromyalgia. J Rheumatol. 1994;21(4):714–720. [PubMed] [Google Scholar]
- 16.King S.J., Wessel J., Bhambhani Y., Sholter D., Maksymowych W. The effects of exercise and education, individually or combined, in women with fibromyalgia. J Rheumatol. 2002;29(12):2620–2627. [PubMed] [Google Scholar]
- 17.Rooks D.S., Gautam S., Romeling M. Group exercise, education, and combination self-management in women with fibromyalgia: a randomized trial. Arch Intern Med. 2007;167(20):2192–2200. doi: 10.1001/archinte.167.20.2192. [DOI] [PubMed] [Google Scholar]
- 18.Sim J., Madden S. Illness experience in fibromyalgia syndrome: a metasynthesis of qualitative studies. Soc Sci Med. 2008;67(1):57–67. doi: 10.1016/j.socscimed.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 19.White K.P., Nielson W.R., Harth M., Ostbye T., Speechley M. Does the label “fibromyalgia” alter health status, function, and health service utilization?: A prospective, within-group comparison in a community cohort of adults with chronic widespread pain. Arthritis Rheum. 2002;47(3):260–265. doi: 10.1002/art.10400. [DOI] [PubMed] [Google Scholar]
- 20.Paiva E.S., Jones K.D. Rational treatment of fibromyalgia for a solo practitioner. Best Pract Res Clin Rheumatol. 2010;24(3):341–352. doi: 10.1016/j.berh.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 21.Burckhardt C.S., Clark S.R., Bennett R.M. The fibromyalgia impact questionnaire: development and validation. J Rheumatol. 1991;18(5):728–733. [PubMed] [Google Scholar]
- 22.Farrar J.T., Young J.P., Jr, LaMoreaux L., Werth J.L., Poole R.M. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 23.Johnson C. Measuring pain: Visual analog scale versus numeric pain scale: what is the difference? J Chiropr Med. 2005;4(1):43–44. doi: 10.1016/S0899-3467(07)60112-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bennett R.M., Friend R., Jones K.D., Ward R., Han B.K., Ross R.L. The Revised Fibromyalgia Impact Questionnaire (FIQR): validation and psychometric properties. Arthritis Res Ther. 2009;11(4):R120. doi: 10.1186/ar2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boomershine C.S., Crofford L.J. A symptom-based approach to pharmacologic management of fibromyalgia. Nat Rev Rheumatol. 2009;5(4):191–199. doi: 10.1038/nrrheum.2009.25. [DOI] [PubMed] [Google Scholar]
- 26.Wolfe F., Clauw D.J., Fitzcharles M.A. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010;62(5):600–610. doi: 10.1002/acr.20140. [DOI] [PubMed] [Google Scholar]
- 27.Filoramo M.A. Improving goal setting and goal attainment in patients with chronic noncancer pain. Pain Manag Nurs. 2007;8(2):96–101. doi: 10.1016/j.pmn.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 28.Wolfe F., Smythe H.A., Yunus M.B. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia: Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33(2):160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 29.Williams D.A., Kuper D., Segar M., Mohan N., Sheth M., Clauw D.J. Internet-enhanced management of fibromyalgia: a randomized controlled trial. Pain. 2010;151(3):694–702. doi: 10.1016/j.pain.2010.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.D'Mello R., Dickenson A.H. Spinal cord mechanisms of pain. Br J Anaesth. 2008;101(1):8–16. doi: 10.1093/bja/aen088. [DOI] [PubMed] [Google Scholar]
- 31.Arnold L.M., Rosen A., Pritchett Y.L. A randomized, double-blind, placebo-controlled trial of duloxetine in the treatment of women with fibromyalgia with or without major depressive disorder. Pain. 2005;119(1-3):5–15. doi: 10.1016/j.pain.2005.06.031. [DOI] [PubMed] [Google Scholar]
- 32.Crofford L.J., Mease P.J., Simpson S.L. Fibromyalgia relapse evaluation and efficacy for durability of meaningful relief (FREEDOM): a 6-month, double-blind, placebo-controlled trial with pregabalin. Pain. 2008;136(3):419–431. doi: 10.1016/j.pain.2008.02.027. [DOI] [PubMed] [Google Scholar]
- 33.Clauw D.J., Mease P., Palmer R.H., Gendreau R.M., Wang Y. Milnacipran for the treatment of fibromyalgia in adults: a 15-week, multicenter, randomized, double-blind, placebo-controlled, multiple-dose clinical trial. Clin Ther. 2008;30(11):1988–2004. doi: 10.1016/j.clinthera.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 34.Arnold L.M., Russell I.J., Diri E.W. A 14-week, randomized, double-blinded, placebo-controlled monotherapy trial of pregabalin in patients with fibromyalgia. J Pain. 2008;9(9):792–805. doi: 10.1016/j.jpain.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 35.Schmidt-Wilcke T., Clauw D.J. Fibromyalgia: from pathophysiology to therapy. Nat Rev Rheumatol. 2011;7(9):518–527. doi: 10.1038/nrrheum.2011.98. [DOI] [PubMed] [Google Scholar]
- 36.Arnold L.M. Biology and therapy of fibromyalgia: new therapies in fibromyalgia. Arthritis Res Ther. 2006;8(4):212. doi: 10.1186/ar1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vlaeyen J.W., Teeken-Gruben N.J., Goossens M.E. Cognitive-educational treatment of fibromyalgia: a randomized clinical trial: I. Clinical effects. J Rheumatol. 1996;23(7):1237–1245. [PubMed] [Google Scholar]
- 38.Goldenberg D.L., Burckhardt C., Crofford L. Management of fibromyalgia syndrome. JAMA. 2004;292(19):2388–2395. doi: 10.1001/jama.292.19.2388. [DOI] [PubMed] [Google Scholar]
- 39.Edinger J.D., Wohlgemuth W.K., Krystal A.D., Rice J.R. Behavioral insomnia therapy for fibromyalgia patients: a randomized clinical trial. Arch Intern Med. 2005;165(21):2527–2535. doi: 10.1001/archinte.165.21.2527. [DOI] [PubMed] [Google Scholar]
- 40.Häuser W., Klose P., Langhorst J. Efficacy of different types of aerobic exercise in fibromyalgia syndrome: a systematic review and meta-analysis of randomised controlled trials. Arthritis Res Ther. 2010;12(3):R79. doi: 10.1186/ar3002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van Koulil S., van Lankveld W., Kraaimaat F.W. Tailored cognitive-behavioral therapy and exercise training for high-risk patients with fibromyalgia. Arthritis Care Res. 2010;62(10):1377–1385. doi: 10.1002/acr.20268. [DOI] [PubMed] [Google Scholar]
- 42.Busch A.J., Webber S.C., Brachaniec M. Exercise therapy for fibromyalgia. Curr Pain Headache Rep. 2011;15(5):358–367. doi: 10.1007/s11916-011-0214-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nicassio P.M., Radojevic V. Models of family functioning and their contribution to patient outcomes in chronic pain. Motiv Emot. 1993;17(3):295–316. [Google Scholar]
- 44.Lentz M.J., Landis C.A., Rothermel J., Shaver J.L. Effects of selective slow wave sleep disruption on musculoskeletal pain and fatigue in middle aged women. J Rheumatol. 1999;26(7):1586–1592. [PubMed] [Google Scholar]
- 45.Harris R.E., Williams D.A., McLean S.A. Characterization and consequences of pain variability in individuals with fibromyalgia. Arthritis Rheum. 2005;52(11):3670–3674. doi: 10.1002/art.21407. [DOI] [PubMed] [Google Scholar]


