Abstract
The clinical laboratory diagnosis of cutaneous anthrax is generally established by conventional microbiological methods, such as culture and directly straining smears of clinical specimens. However, these methods rely on recovery of viable Bacillus anthracis cells from swabs of cutaneous lesions and often yield negative results. This study developed a rapid protocol for detection of B. anthracis on clinical swabs. Three types of swabs, flocked-nylon, rayon, and polyester, were evaluated by 3 extraction methods, the swab extraction tube system (SETS), sonication, and vortex. Swabs were spiked with virulent B. anthracis cells, and the methods were compared for their efficiency over time by culture and real-time PCR. Viability testing indicated that the SETS yielded greater recovery of B. anthracis from 1-day-old swabs; however, reduced viability was consistent for the 3 extraction methods after 7 days and nonviability was consistent by 28 days. Real-time PCR analysis showed that the PCR amplification was not impacted by time for any swab extraction method and that the SETS method provided the lowest limit of detection. When evaluated using lesion swabs from cutaneous anthrax outbreaks, the SETS yielded culture-negative, PCR-positive results. This study demonstrated that swab extraction methods differ in their efficiency of recovery of viable B. anthracis cells. Furthermore, the results indicated that culture is not reliable for isolation of B. anthracis from swabs at ≥7 days. Thus, we recommend the use of the SETS method with subsequent testing by culture and real-time PCR for diagnosis of cutaneous anthrax from clinical swabs of cutaneous lesions.
INTRODUCTION
Bacillus anthracis is a Gram-positive, aerobic, spore-forming bacterium that can infect both animals and humans. The virulence of B. anthracis is attributed to two plasmids, pXO1 and pXO2, and strains lacking either plasmid are avirulent or attenuated (27, 36). The pXO1 plasmid contains the lef, pagA, and cya genes, which encode proteins that interact to produce the two B. anthracis exotoxins, lethal toxin and edema toxin (2, 30, 40). The pXO2 plasmid contains the cap genes (A, B, C, D, and E), which are associated with B. anthracis capsule production (25, 37). Many studies have shown a lack of genetic diversity within B. anthracis; however, advancements in molecular subtyping techniques have been a powerful tool for characterizing the epidemiology of disease with this organism (15, 20, 21, 26).
B. anthracis is the causative agent of anthrax, a zoonotic disease that is primarily associated with herbivores and domestic livestock. Animals become infected after ingesting pathogenic spores from the soil. Infection in humans is acquired from close contact with infected animals or contaminated animal products, such as meat and skin (17). There are three primary forms of the disease in humans, inhalation, gastrointestinal, and cutaneous. Naturally occurring inhalation anthrax is rare, and in the United States, these cases were primarily associated with occupational exposure or close contact with contaminated animal products (4, 26). Gastrointestinal anthrax is also rare, though outbreaks have been reported in parts of Africa and Asia due to ingestion of contaminated meat (17). Cutaneous anthrax is the most common form of the disease and accounts for 95% of cases worldwide (3). It is acquired when spores enter through a cut or abrasion in the skin. The most common areas of exposure are the hands, arms, face, and neck (33). Because of the ability of its spores to persist in the environment for long periods of time, as well as the potential for spores to be disseminated in a powdered form, B. anthracis is regarded as an effective biological weapon (17, 32).
The 2001 bioterrorism-associated anthrax outbreak highlighted the need for validated rapid diagnostics. This outbreak investigation established the use of real-time PCR for detection of B. anthracis directly from clinical specimens, a process which aided in identifying confirmed cases of cutaneous anthrax (16, 19). The clinical diagnosis of cutaneous anthrax is generally established by bacterial culture or direct staining of material from lesion swabs. However, these cultures often yield negative results due to activity of local microbiota within the lesion site (34). Furthermore, culture relies upon efficient recovery of viable cells from the swab material. A validated protocol has been established for testing environmental swabs for recovery of B. anthracis spores (13); however, there have been no studies to validate a protocol with clinical swabs for recovery of B. anthracis vegetative cells. Moreover, it has been reported that swab processing methodologies can impact pathogen detection by molecular diagnostics (39), a finding which suggests the need for an evaluation of swab protocols using B. anthracis vegetative cells.
The purpose of this study was to evaluate three methods for extracting cells from swabs for efficiency of B. anthracis recovery as measured by culture and real-time PCR and to establish a swab protocol for testing clinical specimens. The methods were selected based on their reported use for recovery of other pathogenic organisms from swabs (18, 31, 39) and were compared using swabs spiked with known concentrations of virulent B. anthracis vegetative cells. The evaluation criteria included (i) efficiency of B. anthracis recovery in time course experiments to assess the impact of delays in specimen collection and testing, (ii) limit of detection (LOD) studies with two real-time PCR assays and three DNA purification methods, and (iii) assessments of vegetative cell extraction from different swab materials. The results of these experiments were used to develop a clinical swab protocol for B. anthracis vegetative cell extraction and DNA isolation which was then validated using clinical specimens from cutaneous anthrax outbreaks.
MATERIALS AND METHODS
Scientific ethics.
This report meets the definition of research under 45 CFR 46.102(d), the U.S. Code of Federal Regulations regarding the protection of human subjects. Therefore, review by the Centers for Disease Control and Prevention (CDC) institutional review board (IRB) was required, and approval was granted for continuation of the CDC protocol in January 2012. The specimens used in this study were obtained during the course of outbreak investigations. All identifiable information that can potentially link the specimens to the patients was coded to deidentify patient information.
Clinical specimens.
The clinical specimens used in this study were collected as part of the epidemiological response to cutaneous anthrax outbreaks that occurred in Bangladesh from August to October 2009 (5). During the outbreak investigations, swabs of vesicles were obtained from patients who met the case definition of suspected cutaneous anthrax as described in the report by Boyer et al. (1). Up to two swabs per patient were collected in purple or red vacuum-capped tubes (BD Diagnostics, Sparks, MD), shipped to the CDC Bacterial Zoonoses and Select Agent Laboratory, and stored at 4°C. A total of 23 clinical specimens were used in this study. These specimens were not tested for B. anthracis prior to this study.
Biosafety procedures.
All work with clinical specimens and virulent B. anthracis was performed in biosafety level 3 (BSL3) laboratories. Culture and swab extraction procedures were conducted in class II, type A2 biological safety cabinets (BSC; NuAire, Plymouth, MN). Additional BSL3 precautions included the use of powered air-purifying respirators and protective laboratory clothing.
Bacillus anthracis culture.
B. anthracis strain K1694 (Ames) was used throughout this study. Cultures were initiated from frozen glycerol stocks and streaked for isolated colonies on Trypticase soy agar plates with 5% (vol/vol) sheep blood (TSAB; BD Diagnostic Systems), and the plates were incubated overnight at 37°C. A single colony was transferred to 1 ml of sterile physiological saline (0.85% sodium chloride) using a sterile inoculating loop, and a smooth suspension of cells was prepared by vortexing at low speed for 30 s.
To ensure that only vegetative cells were used, a spore-free culture procedure was adapted from the method described by King et al. (22) and was used throughout this study. The cultures were streaked for isolated colonies on triplicate TSAB plates and incubated for up to 24 h at 37°C. Using 1-μl disposable loops, cells from the outer edges of isolated colonies were harvested and transferred to 5-ml culture tubes, with each containing 4 ml of heart infusion broth plus 0.1% glucose, supplemented with heat-inactivated horse serum (Oxoid, Ltd., Basingstoke, Hampshire United Kingdom) and sodium bicarbonate (Sigma-Aldrich, St. Louis, MO) to final concentrations of 50% and 0.8%, respectively, to induce B. anthracis capsule production (29). These cultures were incubated for up to 4 h at 37°C under ambient conditions without shaking as described previously (22). Following incubation, the cultures were pooled and harvested by centrifugation for 20 min at 10,000 × g and at 4°C. The cell pellets were resuspended in 5 ml of sterile phosphate-buffered saline (PBS; 0.01 M, pH 7.4), and the total culture volume was divided into two equal aliquots designated harvest A and harvest B. Harvest A was immediately used as an inoculum to spike the swabs, numbers of CFU/ml were quantified on TSAB plates using standard procedures (9), and the cells were examined by staining and light microscopy (see below). Harvest B underwent a heat-shock treatment (30 min at 65°C) to verify that the inoculum was spore free. Following heat shock, 200-μl aliquots were spread on TSAB plates until the entire volume was depleted. The plates were incubated at 37°C and observed for growth for up to 48 h. When growth from spores was observed, the cultures and associated spiked swabs were discarded and the procedure was repeated.
Staining and microscopy.
A 5-μl drop of harvest A was transferred to a microscope slide, and the cells were stained with India ink (Remel, Inc., Lenexa, KS) for identification of capsule formation. Harvest A was also stained with Malachite green (Sigma-Aldrich) and counterstained with Safranin (BD Diagnostics Systems) to visually verify that cultures were spore free. Multiple fields of each slide were viewed at ×5,000 magnification using a model VHX-600 digital light microscope (Keyence Corp., Woodcliff Lake, NJ) and examined for the presence of clear zones around cells (indicative of capsule production for the India ink-stained slides) and for the absence of spherically shaped, green-stained structures (indicative of spores for the Malachite green-stained slides). In subsequent experiments, Gram staining of suspect colonies was performed using procedures that are provided with the Gram stain kit (BD Diagnostics), and the slides were observed by light microscopy as described above.
Spiking of swabs.
A total of 12 flocked-nylon swabs each (Copan Diagnostics Inc., Murrieta, CA) were used for the initial spiking experiments. Each swab was inoculated with 10 μl of B. anthracis cells at a concentration of 107 CFU/ml. To simulate clinical specimens, the swabs were coinoculated with 10 μl of normal human sera (Millipore Corporation, Billerica, MA). The swabs were stored at room temperature inside a BSC for time course recovery experiments at 1, 7, and 28 days postinoculation. Flocked-nylon swabs were also used in experiments to determine the LOD in real-time PCR. For these experiments, 10-fold serial dilutions of B. anthracis cells were prepared in PBS at concentrations ranging from 107 to 103 CFU/ml and the swabs were spiked in triplicate with 10-μl aliquots at each dilution and with normal human serum as described above. Two additional swab materials, polyester and rayon (Fisher Scientific), were selected to assess their relative impact on B. anthracis recovery. For these experiments, a total of 12 swabs each were spiked with 10 μl of B. anthracis cells at a concentration of 107 CFU/ml and with normal human serum as described above.
Swab extraction methods.
Three methods of extracting cells from swabs were compared: swab extraction tube system (SETS), sonication, and vortex. The swabs were rehydrated in 500 μl of PBS. The SETS (Roche Applied Science, Indianapolis, IN) is a disposable centrifugal system comprised of an inner tube and an outer collection tube, and its use for recovery of pathogenic microorganisms has been described in previous reports (18, 39). The inoculated swabs were rehydrated in the outer SETS tubes and were then transferred to the inner SETS tubes using disposable forceps. The tubes containing the swabs were centrifuged for 1 min at 8,000 × g, and the eluted swab suspensions were recovered in the outer tubes.
The sonication method has been described previously (39). Spiked swabs were rehydrated in 2-ml screw-cap tubes and were then incubated for 15 min at sweeping frequencies between 50 and 60 kHz in the model T50 ultrasonic bath (VWR, West Chester, PA). Following sonication, residual liquid was expressed from the swabs by pressing against the sides of the tubes, and the eluted swab suspensions were centrifuged briefly at 8,000 × g to remove residual liquid from the cap and sides of the tubes.
The vortex method was adapted from a method described for the recovery of B. anthracis spores from environmental swabs (31). Following rehydration, the spiked swabs were vortexed at high speed for 2 min. Residual liquid was expressed from the swabs by pressing against the sides of the tubes, and the samples were centrifuged briefly at 8,000 × g as described above.
Interlaboratory evaluation of the three swab extraction methods.
To compare the three swab extraction methods for recovery of B. anthracis, viability testing was performed independently and on separate dates between two Clinical Laboratory Improvement Amendments-certified BSL3 laboratories at the CDC, the Bioterrorism Rapid Response and Advanced Technology Laboratory (lab A) and the Zoonoses and Select Agent Laboratory (lab B). For each method, a total of 12 swabs each were tested for isolation of B. anthracis by culture at 1, 7, and 28 days postspiking. The eluted swab suspensions described above were split into equal volumes, and one half was used for bacterial culture while the other half underwent DNA purification for subsequent testing by real-time PCR. For culture testing, the suspensions were diluted 10-fold in physiological saline, and 100 μl each of the undiluted and diluted suspensions was spread onto duplicate TSAB plates. The plates were incubated for 24 h at 37°C, examined for colonies, and quantified in numbers of CFU/ml using standard plate counting procedures. For each swab extraction method, the percent recovery of B. anthracis cells was calculated using the cell spiking concentration and the mean CFU/ml recovery concentrations for the duplicate cultures (n = 24) at each time point.
DNA purification.
Three commercial methods, including two automated methods and one manual method, were used to purify DNA from the eluted swab cell suspensions. Automated DNA purifications were performed using the MagNA Pure Compact and MagNA Pure LC instruments with the MagNA Pure Compact nucleic acid isolation kit I and MagNA Pure LC DNA isolation kit I (Roche), respectively. Both instruments utilize magnetic bead technology for DNA purification, and the procedures for their use have been described previously (8). Manual DNA purifications were performed with the QIAamp DNA blood minikit (Qiagen, Inc., Valencia, CA), which utilizes silica spin-filter technology for DNA purification. The procedures were carried out according to the manufacturer's instructions (8). The isolated DNA samples were filtered through 0.1-μm centrifugal filter units (Millipore Corporation) as described previously (7) and stored at −20°C throughout this study.
DNA yield.
For each swab extraction method, DNA isolated by the use of the MagNA Pure Compact, MagNA Pure LC, and QIAamp kit was quantified using a NanoDrop 2000 spectrophotometer (Thermo Scientific, Wilmington, DE). The absorbance at 260 nm (A260) was measured and used to calculate the average concentration for triplicate DNA samples from B. anthracis LOD studies (derived from swabs spiked in triplicate with each concentration of the B. anthracis cell suspensions, ranging from 107 to 103 CFU/ml). The average DNA concentrations were used to calculate genome equivalents at the LOD for B. anthracis DNA in subsequent real-time PCR experiments.
Preparation of positive controls for real-time PCR assays.
B. anthracis Ames strain DNA was used as a positive control in real-time PCR assays. Cell lysates from the Ames strain were prepared by harvesting isolated colonies into 500 μl of sterile deionized water, vortexing for 30 s, and boiling for 5 min, followed by centrifugation for 30 s at 10,000 × g. The supernatants were filtered using 0.1-μm centrifugal filter units (Millipore Corporation) as described previously (7), and the filtrates were diluted in Tris-EDTA buffer to dilutions that produced real-time PCR cross-threshold (cycle threshold [CT]) values between 25 and 30. The positive-control DNA samples were stored at −20°C throughout the study.
Real-time PCR assays.
Two different types of real-time PCR assays were used in this study. To evaluate the swab protocols for routine use in diagnostic laboratories, the multitarget 5′ nuclease (TaqMan) real-time PCR assay described by Hoffmaster et al. (16) was used. This is a highly sensitive and specific assay that was validated for detection of B. anthracis and was successfully used to test hundreds of samples during the 2001 bioterrorism-associated anthrax outbreak. The assay includes three primer and probe sets which target the B. anthracis chromosome and the pXO1 and pXO2 plasmids and has been described in previous reports (9, 16). PCR was carried out in triplicate 25-μl volumes. Each contained 1× PCR master mix (Roche Molecular Biochemicals, Indianapolis, IN), 500 nM each PCR primer, 100 nM each TaqMan probe, 5 mM total MgCl2, and 5 μl of either a sample, positive-control DNA, or water (no-template controls).
The molecular beacon-based real-time PCR assay described by Hadjinicolaou et al. (12) was also used in this study. This assay was developed for the rapid and specific detection of virulent B. anthracis in routine diagnostic tests. The molecular beacons were synthesized at the CDC Biotechnology Core Facility as described previously (12) with 5′ 6-carboxyfluorescein (FAM) fluorophore and 3′ Dabcyl quencher. The MBpag probe, with corresponding forward and reverse primers, targets the pagA allele on the pXO1 plasmid of B. anthracis, whereas the MBcapB probe, with corresponding primers, targets the capB allele located on the pXO2 plasmid. PCRs were performed in a 25-μl final volume, each of which contained 1× LightCycler FastStart DNA Master HybProbes PCR master mix (Roche Molecular Biochemicals), 1 μl of either the MBcapB molecular beacon (8 pmol/μl) or the MBpag molecular beacon (5 pmol/μl), 1.0 μl (20 pmol/μl) each of the forward and reverse primers, and 5 μl of either a sample, positive-control DNA, or water.
All real-time PCRs were performed using the 7500 Fast real-time PCR system (Applied Biosystems, Foster City, CA). For the TaqMan assay, the Fast 7500 operational setting was used with a thermocycling profile consisting of a hot-start Taq activation step of 95°C for 8 min, followed by 40 cycles of 95°C for 10 s and 60°C for 30 s (data collection). For the molecular beacon-based assay, the standard 7500 operational setting was used with a thermocycling profile consisting of a hot-start Taq activation step of 94°C for 10 min, followed by 40 cycles of 94°C for 15 s, 50°C for 30 s (data collection), and 72°C for 30 s. For both real-time PCR assays, data collection and analysis were performed using the 7500 Fast system sequence detection software version 1.4, including the 21 CFR part 11 electronic records module for Food and Drug Administration compliance.
To evaluate the three swab extraction methods for recovery of B. anthracis over time, real-time PCR was performed in triplicate using DNA isolated from spiked swabs at 1, 7, and 28 days postinoculation, and the PCR run was repeated (n = 24). To compare the real-time PCR LOD for each swab extraction method, B. anthracis DNA isolated with each of the three commercial DNA purification methods was tested in triplicate, and PCR runs with both real-time PCR assays were repeated. The LOD for each swab extraction method was the lowest concentration for which three out of three replicates produced a positive result (CT ≤ 40) for all of the real-time PCR targets. To assess the impact of swab materials on the recovery and subsequent detection of B. anthracis DNA, real-time PCR was performed in triplicate using DNA isolated from each swab material and the PCR runs for each swab material were repeated (n = 24).
Statistical analysis.
To determine whether the differences in CT values for the three swab extraction methods were significant, the mean values were compared using one-way analysis of variance (ANOVA). For experiments that used 12 swabs each, the mean value for triplicate PCRs was calculated for each swab so that an n value of 12 was used for each PCR run. The PCR runs were repeated so that a total n value of 24 was used for statistical analyses. When significant differences were identified, Tukey's multiple-comparison test was used to perform nonparametric pairwise analyses of the CT values.
Validation with outbreak specimens.
The results of the time course experiments, LOD studies, and assessments of the three swab extraction methods using different swab materials were used to develop and validate a swab protocol using clinical specimens from cutaneous anthrax outbreaks. Twenty-three lesion swabs were processed by the use of the SETS, and the eluted swab suspensions were tested by bacterial culture and diagnostic real-time PCR. Briefly, 200 μl of each suspension underwent automated DNA purification using the MagNA Pure Compact (Roche) followed by real-time PCR, while 100 μl of each suspension was also streaked for isolated colonies onto duplicate TSAB plates, which were incubated overnight at 37°C. Specimens were considered positive for B. anthracis DNA when all targets in the real-time PCR assay were positive. The criteria for positive identification of B. anthracis by culture were nonhemolytic growth on TSAB plates at 24 h with colony morphology consistent with that of B. anthracis and the presence of Gram-positive bacilli with capsule production by microscopic analysis. Real-time PCR was repeated in triplicate for all positive specimens.
RESULTS
Comparison of swab extraction methods for isolation of B. anthracis in culture.
Table 1 shows the time course results for viability testing of spiked swabs in two independent laboratories. Overall, the results were consistent between the two laboratories, with a reduction in the number of viable cells recovered for each swab extraction method at each consecutive time point. The SETS yielded greater viability of B. anthracis than the other two methods after 1 day, with a mean percent recovery of 0.2% compared to 0.07% and 0.09% for the sonication and vortex methods, respectively. In both laboratories, the number of viable cells recovered was reduced after 7 days and the three swab extraction methods resulted in comparable yields. By 28 days postinoculation, isolation of viable B. anthracis in culture was not reproducible for any of the three swab extraction methods based on the following results: in lab A, the SETS yielded culture-negative results for all 12 swabs, and only 1 out of 12 swabs was positive with the sonication and vortex methods. In lab B, only 1 out of 12 swabs was positive with the SETS and sonication methods, whereas the vortex method yielded culture-negative results for all 12 swabs.
TABLE 1.
Interlaboratory evaluation of three methods for recovery and viability of Bacillus anthracis from spiked swabs over time
| Recovery methoda | Percent recovery (no. positive/no. tested) at each time pointb |
|||||
|---|---|---|---|---|---|---|
| 1 day |
7 days |
28 days |
||||
| Lab A | Lab B | Lab A | Lab B | Lab A | Lab B | |
| SETS | 0.2 (12/12) | 0.1 (12/12) | 0.0006 (10/12) | 0.0001 (11/12) | 0 (0/12) | 0 (1/12) |
| Sonication | 0.07 (12/12) | 0.05 (12/12) | 0.0004 (9/12) | 0.0001 (8/12) | 0 (1/12) | 0 (1/12) |
| Vortex | 0.09 (12/12) | 0.06 (12/12) | 0.0005 (7/12) | 0.0001 (9/12) | 0 (1/12) | 0 (0/12) |
A total of 12 nylon-flocked swabs each were spiked with 10 μl of virulent B. anthracis cells at a concentration of 107 CFU/ml, and the three methods were compared at 1, 7, and 28 days postspiking. The procedures were repeated on different days in two independent CDC laboratories (labs A and B) except on day 1, when they were repeated in the same laboratory.
The mean percent recovery for each method was calculated by dividing the spiking concentration by the average concentration of viable cells recovered (CFU/ml) at each time point. When <3 out of 12 swabs were negative in culture, the percent recovery was determined to be zero due to nonreproducibility. Values in parentheses show the number of swabs that were positive for isolation of B. anthracis in culture out of the total number of swabs tested.
Comparison of swab extraction methods by real-time PCR.
Table 2 shows time course results for real-time PCR analysis of DNA from extracted cells on spiked swabs with the B. anthracis TaqMan real-time PCR assay. On the whole, the results were equivalent for all three methods, with comparable CT values for each target at each time point. At day 1, the average CT values ranged from 23.3 to 23.6 with the chromosomal target, 22.5 to 22.8 with the pXO1 target, and 22.3 to 22.5 with the pXO2 target. Similarly, at day 7, the average CT values ranged from 22.9 to 23.6, 21.3 to 21.9, and 21.2 to 22.4 with the chromosomal, pXO1, and pXO2 targets, respectively. Also, at day 28, the ranges for the chromosomal, pXO1, and pXO2 targets were 22.9 to 23.2, 21.2 to 21.7, and 21.7 to 22.0, respectively. For each time point, there were no significant differences between the mean CT values obtained with the three swab extraction methods, as determined by one-way ANOVA (P > 0.05; n = 24 for each real-time PCR target).
TABLE 2.
Comparison of three recovery methods for detection of Bacillus anthracis from spiked swabs by real-time PCR
| Recovery methoda | Average CT (mean ± SD)b at each time point for each PCR target |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 day |
7 days |
28 days |
|||||||
| Chromosome | pXO1 | pXO2 | Chromosome | pXO1 | pXO2 | Chromosome | pXO1 | pXO2 | |
| SETS | 23.3 ± 0.07 | 22.8 ± 0.14 | 22.5 ± 0.14 | 22.9 ± 0.08 | 21.3 ± 0.13 | 21.6 ± 0.14 | 22.9 ± 0.20 | 21.6 ± 0.17 | 21.9 ± 0.33 |
| Sonication | 23.6 ± 0.09 | 22.5 ± 0.09 | 22.3 ± 0.08 | 23.3 ± 0.09 | 21.9 ± 0.14 | 21.2 ± 0.09 | 23.0 ± 0.12 | 21.2 ± 0.14 | 21.7 ± 0.31 |
| Vortex | 23.5 ± 0.05 | 22.5 ± 0.10 | 22.5 ± 0.09 | 23.6 ± 0.08 | 21.9 ± 0.21 | 22.4 ± 0.09 | 23.2 ± 0.15 | 21.7 ± 0.02 | 22.0 ± 0.31 |
A total of 12 nylon-flocked swabs each were spiked with 10 μl virulent B. anthracis cells at a concentration of 107 CFU/ml, and the three recovery methods were compared at 1, 7, and 28 days postspiking.
The eluted cell suspensions from each swab underwent automated DNA purification with the MagNA Pure Compact, followed by real-time PCR analysis. The average CT values (mean ± standard deviation) are shown for DNA tested in triplicate using the real-time PCR assay described by Hoffmaster et al. (16).
Evaluation of swab extraction methods with different swab materials.
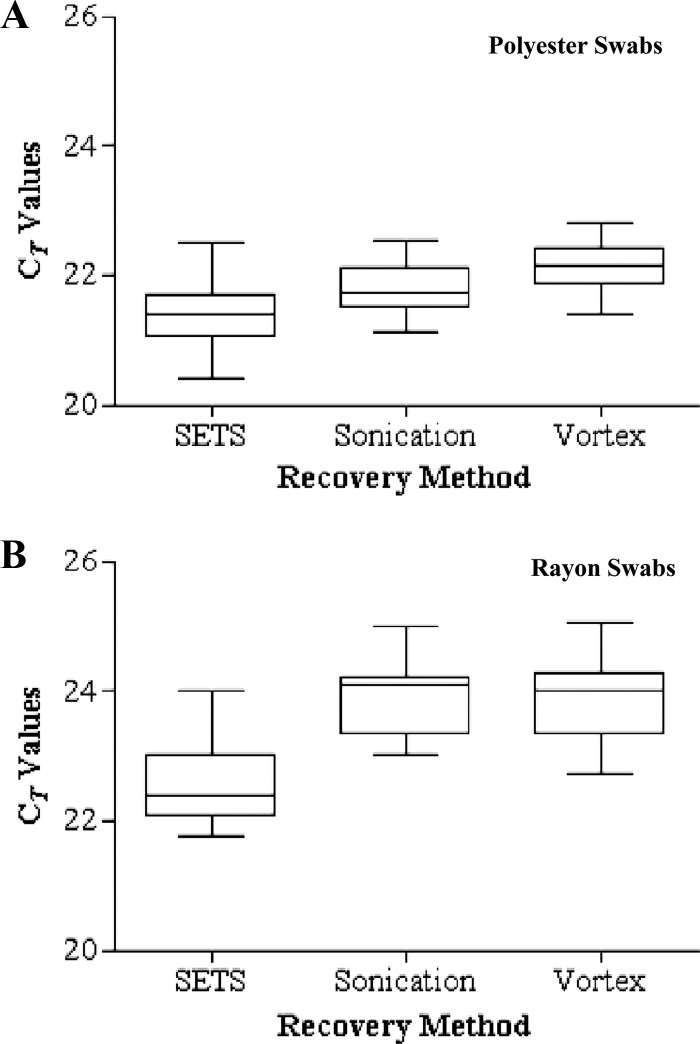
Figure 1 shows the real-time PCR results for the SETS, sonication, and vortex methods with polyester and rayon swabs using the chromosomal target of the B. anthracis TaqMan assay. Taken as a whole, B. anthracis detection was not impacted by the swab material for any of the three swab extraction methods. Figure 1A shows the distribution of CT values for polyester swabs. The SETS, sonication, and vortex methods yielded CT values with mean values (ranges) of 21.4 (20.4 to 22.5), 21.8 (21.1 to 22.5), and 22.2 (21.4 to 22.8), respectively. Figure 1B shows the distribution of CT values for the three swab extraction methods with rayon swabs, with mean values (ranges) of 22.4 (21.7 to 24.0) for the SETS, 23.8 (23.0 to 25.0) for sonication, and 23.9 (22.7 to 25.1) for the vortex method. For both swab materials, the differences in mean CT values between the three swab extraction methods were found to be significant by one-way ANOVA (P < 0.001; n = 24). For polyester swabs, pairwise comparisons of CT values using Tukey's multiple-comparison test indicated significant differences between all three methods (P < 0.001; n = 24). For rayon swabs, pairwise comparisons indicated significant differences between the SETS and the sonication method and between the SETS and the vortex method (P < 0.001; n = 24); however, there was no significant difference between the sonication and vortex methods (P = 0.09; n = 24).
Fig 1.
Box-and-whisker plots showing the distribution of CT values with the chromosomal target of the B. anthracis real-time PCR assay (16) for polyester (A) and rayon (B) swabs spiked with virulent B. anthracis Ames strain cells at a concentration of 107 CFU/ml and then processed by the use of the three swab recovery methods. The bottom, middle, and top lines of each box correspond to the 25, 50, and 75% cumulative frequencies of the observed values, respectively. The endpoints of the whiskers show the 2.5 and 97.5 percentiles. For both swab materials, the differences in mean CT values between the three methods were found to be significant by one-way ANOVA (P < 0.001; n = 24). For polyester swabs, Tukey's multiple-comparison test revealed significant differences between all three methods (P < 0.001; n = 24). For rayon swabs, significant differences were identified between the SETS and the sonication method and the SETS and the vortex method (P < 0.001; n = 24); however, there was no significant difference between the sonication and vortex methods (P = 0.09; n = 24).
Real-time PCR analysis using three DNA purification methods.
Table 3 shows the LOD with the TaqMan and molecular beacon-based real-time PCR assays using DNA isolated by three different DNA purification methods. By and large, the SETS method yielded the most consistent results with all three DNA purification methods, with a LOD of 500 CFU/swab and a detection range of 6.2 × 102 to 9.0 × 102 molecules (genome copy numbers [gc]) for the two real-time PCR assays. The real-time PCR results for swab extracts from sonication were comparable to those for swabs from the SETS method with all DNA purification methods except the MagNA Pure LC, which resulted in one-log-unit-less detection with the molecular beacon real-time PCR assay (5,000 CFU/swab [4.9 × 103 gc]). The vortex method yielded the least-consistent detection levels by real-time PCR, with a LOD of 5,000 CFU/swab with the QIAamp kit and the TaqMan assay (4.6 × 103 gc) as well as with the MagNA Pure LC instrument and both real-time PCR assays (5.0 × 103 gc).
TABLE 3.
Real-time PCR limits of detection for three recovery methods using DNA isolated from Bacillus anthracis-spiked swabs
| Recovery methoda | LOD (CFU/swab [genome copy numbers])b |
|||||
|---|---|---|---|---|---|---|
| QIAamp |
MagNA Pure Compact |
MagNA Pure LC |
||||
| PCR 1 | PCR 2 | PCR 1 | PCR 2 | PCR 1 | PCR 2 | |
| SETS | 500 (8.2 × 102) | 500 (8.2 × 102) | 500 (9.0 × 102) | 500 (9.0 × 102) | 500 (6.2 × 102) | 500 (6.2 × 102) |
| Sonication | 500 (5.1 × 102) | 500 (5.1 × 102) | 500 (7.0 × 102) | 500 (7.0 × 102) | 500 (4.9 × 102) | 5,000 (4.9 × 103) |
| Vortex | 5,000 (4.6 × 103) | 500 (4.6 × 102) | 500 (6.5 × 102) | 500 (6.5 × 102) | 5,000 (5.0 × 103) | 5,000 (5.0 × 103) |
Nylon-flocked swabs were spiked in triplicate with 10 μl of 10-fold dilutions of virulent B. anthracis Ames strain cells at a starting concentration of 107 CFU/ml and then underwent the three swab recovery methods. DNA was isolated by the use of three different DNA purification methods, the QIAamp manual method and the MagNA Pure Compact and MagNA Pure LC automated methods.
Real-time PCR was performed in triplicate using two different assays, the TaqMan assay described by Hoffmaster et al. (PCR 1) (16) and the molecular beacon assay described by Hadjinicolaou et al. (PCR 2) (12). The limit of detection (LOD) (in numbers of CFU/swab) was calculated based on numbers of CFU/ml of the spiking concentration, and genome equivalents (genome copy numbers) were calculated for the lowest concentration that resulted in three out of three replicates with positive results for all targets in each real-time PCR assay.
Validation of the SETS protocol with outbreak specimens.
Table 4 shows the results for B. anthracis PCR-positive lesion swabs from cutaneous anthrax outbreaks, which were processed using the SETS protocol. None of the swabs were positive for isolation of B. anthracis in culture. In contrast, 15 of the 23 specimens tested were positive for B. anthracis DNA. Two specimens (BCA00020 and BCA00021) yielded positive results for the chromosomal and pXO1 targets but negative results for the pXO2 target and thus were not considered positive according to the diagnostic assay criteria (data not shown).
TABLE 4.
Results from the SETS swab extraction protocol by culture and real-time PCR using lesion swabs from cutaneous anthrax outbreaksa
| Specimen IDb | Culture result and growth characteristic | Average CT (mean ± SD)c |
||
|---|---|---|---|---|
| Chromosome | pXO1 | pXO2 | ||
| BCA00001 | −, no growth | 35.9 ± 0.52 | 34.9 ± 0.72 | 35.6 ± 0.63 |
| BCA00004 | −, no growth | 38.2 ± 0.49 | 37.8 ± 0.71 | 36.9 ± 1.37 |
| BCA00007 | −, non-B. anthracis | 37.3 ± 0.67 | 39.0 ± 0.55 | 39.0 ± 0.55 |
| BCA00009 | −, non-B. anthracis | 25.7 ± 0.17 | 24.4 ± 0.22 | 24.5 ± 0.02 |
| BCA00010 | −, non-B. anthracis | 37.4 ± 1.14 | 35.0 ± 0.45 | 29.5 ± 0.67 |
| BCA00011 | −, non-B. anthracis | 31.6 ± 0.37 | 34.6 ± 0.90 | 36.6 ± 0.48 |
| BCA00012 | −, non-B. anthracis | 34.9 ± 0.90 | 31.7 ± 0.77 | 31.5 ± 0.35 |
| BCA00014 | −, non-B. anthracis | 36.1 ± 1.01 | 33.8 ± 0.03 | 34.5 ± 0.49 |
| BCA00015 | −, non-B. anthracis | 31.7 ± 0.48 | 29.4 ± 0.29 | 30.1 ± 0.04 |
| BCA00016 | −, non-B. anthracis | 31.3 ± 0.23 | 29.2 ± 0.14 | 29.8 ± 0.35 |
| BCA00017 | −, non-B. anthracis | 32.4 ± 0.25 | 30.7 ± 0.34 | 31.2 ± 0.14 |
| BCA00018 | −, non-B. anthracis | 38.1 ± 0.09 | 37.2 ± 0.94 | 38.3 ± 0.55 |
| BCA00019 | −, no growth | 34.6 ± 0.34 | 33.0 ± 0.15 | 34.0 ± 0.20 |
| BCA00022 | −, no growth | 28.2 ± 0.14 | 26.5 ± 0.04 | 26.7 ± 0.14 |
| BCA00023 | −, non-B. anthracis | 30.6 ± 0.05 | 28.1 ± 0.10 | 29.0 ± 0.09 |
Outbreaks in Bangladesh in 2009.
Identification (ID) numbers were assigned to deidentify patient specimens. The specimens were processed using the SETS method and were tested for isolation of B. anthracis in culture as well as automated DNA purification with the MagNA Pure Compact, followed by real-time PCR analysis.
Average CT values (mean ± standard deviation) are shown only for triplicate DNA samples from specimens that were positive for all three targets in the B. anthracis real-time PCR assay described by Hoffmaster et al. (16). PCR-negative results from eight swabs are not shown.
DISCUSSION
This study describes a comparison of three methods for processing clinical swabs for detection of B. anthracis. Of the three swab extraction methods evaluated, the SETS yielded greater recovery of viable B. anthracis in culture with the lowest limit of detection and the most consistent results by real-time PCR. These findings were consistent with those in our previous report, which demonstrated that the use of the SETS was optimal for detection of Francisella tularensis from spiked swabs (39). There are established protocols for recovery of B. anthracis spores from environmental swabs (13, 14); however, this is the first report to evaluate procedures and develop a protocol for recovery of B. anthracis vegetative cells from clinical swabs. Further, this protocol was successfully employed for the identification of B. anthracis from cutaneous anthrax outbreak specimens.
The clinical laboratory diagnosis of cutaneous anthrax is commonly established by conventional microbiological methods, such as staining and microscopic analysis of lesion material and isolation of B. anthracis in culture. Unlike B. anthracis spores, vegetative bacteria have poor survival outside the host, and it has been reported that colony counts begin to decline within 24 h in some sample matrices, such as water (35). The results of this study demonstrated that successful culture is dependent on how soon the swabs can be processed after sample collection (Table 1). It is also known that the timing of collection in the course of disease and the use of antimicrobial agents prior to specimen collection can affect culture results (33). Results from this study were consistent with previous reports of culture-negative results for clinical specimens from cutaneous anthrax cases, such as during the 2001 bioterrorism-associated anthrax outbreak when only 2 of the 11 cutaneous anthrax cases were confirmed by isolation of B. anthracis in culture (19). More recently, a study by Doganay et al. (10) reviewed cutaneous anthrax cases over a 7-year time period in Turkey, and of the 22 cases evaluated, 19 yielded culture-negative results. In both of the aforementioned studies (10, 19), when culture yielded negative results, additional laboratory evidence of B. anthracis infection was used to support the diagnosis of cutaneous anthrax.
In contrast to culture, the results of this study showed that real-time PCR was not impacted by time postspiking of the swabs, as the PCR yields were comparable at 1, 7, and 28 days with all three swab extraction methods (Table 2). This finding is supported by results reported in an article on pathology in the 2001 anthrax investigation, when three confirmed cases of cutaneous anthrax were negative by culture yet positive by PCR (33). An interesting finding to note is that the SETS yielded greater recovery of viable B. anthracis by culture at 1 day postspiking; however, the differences between the three swab extraction methods were not significant and did not constitute significantly greater PCR yields (Tables 1 and 2). These results show that at 1 day postspiking, the SETS method was more efficient than the sonication and vortex methods for recovery of viable cells, not total cells.
Flocked-nylon swabs were used for most of the experiments in this study because they are frequently tested in clinical laboratories and they have been shown to be superior for recovery of pathogenic bacteria (6, 38). With regard to swab materials, all three swab extraction methods yielded detectable levels of B. anthracis DNA from polyester and rayon swabs as well (Fig. 1). Though significant differences between the three swab extraction methods were observed with both swab materials, this had no consequence on detection by real-time PCR when high concentrations of B. anthracis (107 CFU/ml [105 CFU/swab]) were used for spiking (Fig. 1A and B). These results suggest that any of the swab materials may be used with the three swab extraction methods used in this study for recovery of B. anthracis cells provided that there are sufficient numbers of cells on the swab.
Since the 2001 bioterrorism-associated anthrax outbreak, several different types of real-time PCR assays for the detection of B. anthracis have been developed (11, 12, 24, 28). The molecular beacon-based assay utilized in this study was selected to assess whether recovery of B. anthracis with the three swab extraction methods would be consistent irrespective of the type of real-time PCR assay used. Diagnostic laboratories may also choose between several commercially available methods for isolation of B. anthracis DNA; therefore, this study employed three different DNA purification methods. The results showed that the differences in recovery efficiency between the three swab extraction methods had an impact at lower inoculum concentrations of B. anthracis, as the SETS and sonication methods yielded a one-log-unit-greater level of detection than the vortex method using the TaqMan assay with the QIAamp kit and with the MagNA Pure LC instrument. Also, the SETS method yielded a one-log-unit-greater level of detection than the other two swab extraction methods with the molecular beacon assay and the MagNA Pure LC instrument (Table 3). Combined, these results indicate that the SETS method provided the best levels of detection for B. anthracis DNA and the most consistent results and, thus, that these results were independent of the real-time PCR assay or DNA purification method used.
During outbreaks or public health investigations, laboratories are likely to receive large numbers of specimens for testing (19, 23). Swabs are frequently submitted to diagnostic laboratories where time to results is important; thus, a need for rapid swab-processing protocols exists. One advantage of the SETS method is that it required the least amount of processing time, and it is reported to average 7 min total for 24 samples, compared to 22 min and 9 min for the sonication and vortex methods, respectively (39). In addition, the SETS protocol was successfully used in conjunction with real-time PCR when there was a long delay in specimen testing. The clinical specimens that were used in this study were collected in 2009, and 15 out of 23 were positive by PCR yet none were positive by culture (Table 4), as expected based on the results of negative cultures after 28 days in the time course experiments. Therefore, this protocol may be useful when there are delays in specimen testing, such as in cases of international shipments of specimens. When taking into consideration the need for rapid testing of specimens as well as factors that may contribute to culture-negative results, such as time period postinfection, the swab protocol described in this report offers advantages over the use of conventional microbiological methods alone for laboratory diagnosis of cutaneous anthrax.
One limitation of this study was the lack of clinical specimens from recent outbreaks of cutaneous anthrax. In addition, this study was limited to clinical specimens that were not tested by other diagnostic methods during the outbreak investigations (23 lesion swabs). Therefore, the initial experiments in this study were performed using spiked swabs. Culture testing of spiked swabs indicated significantly reduced recovery of viable B. anthracis after ≥7 days; however, it is unknown whether the time course results would be identical with clinical specimens, although human serum was added to the inoculated swabs to mimic a clinical sample as closely as possible. Future studies should evaluate different swab collection and transport methods to see if culture results can be improved and lessen the impact of any delays in processing the swabs.
The results of this study showed that the SETS method yielded greater recovery of viable B. anthracis in culture as well as consistent detection of B. anthracis DNA by real-time PCR with three DNA purification methods and with three different swab materials. The use of the SETS followed by automated nucleic acid purification and real-time PCR provided a rapid method for detection of B. anthracis in outbreak specimens. Thus, we recommend incorporating this swab protocol into laboratory testing procedures for diagnosis of cutaneous anthrax.
ACKNOWLEDGMENTS
We gratefully acknowledge Vladimir Loparev and Nicky Sulaiman for synthesis of the molecular beacon probes used in this study, Mindy Glass for facilitating intrafacility select agent transfers, and Wendy Carr for assistance with IRB compliance requirements. We thank John Bowzard, Julia Bugrysheva, Janetta Hakovirta, Samantha Prezioso, Bernard Quigley, and David Sue for assistance with data review. We thank Pierre Michel, Linda Weigel, Scott Santibanez, Toby Merlin, and Anthony Sanchez for their editorial reviews.
B. anthracis is a select agent, and the possession, use, and transfer are regulated by the U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, and the U.S. Department of Agriculture, Animal and Plant Health Inspection Service. The select agent regulations have mandatory reporting requirements for identification of select agents in diagnostic specimens.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry. Names of vendors or manufacturers are provided as examples of available product sources; inclusion does not imply endorsement of the vendors, manufacturers, or products by the Centers for Disease Control and Prevention or the U.S. Department of Health and Human Services.
Footnotes
Published ahead of print 3 October 2012
REFERENCES
- 1. Boyer AE, et al. 2011. Lethal factor toxemia and anti-protective antigen antibody activity in naturally acquired cutaneous anthrax. J. Infect. Dis. 204:1321–1327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bragg TS, Robertson DL. 1989. Nucleotide sequence and analysis of the lethal factor gene (lef) from Bacillus anthracis. Gene 81:45–54 [DOI] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention 2001. Human anthrax associated with an epizootic among livestock—North Dakota, 2000. MMWR Morb. Mortal. Wkly. Rep. 50:677–680 [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention 2006. Inhalation anthrax associated with dried animal hides—Pennsylvania and New York City, 2006. MMWR Morb. Mortal. Wkly. Rep. 55:280–282 [PubMed] [Google Scholar]
- 5. Chakraborty A, et al. 2012. Anthrax outbreaks in Bangladesh, 2009-2010. Am. J. Trop. Med. Hyg. 86:703–710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chernesky M, Castriciano S, Jang D, Smieja M. 2006. Use of flocked swabs and a universal transport medium to enhance molecular detection of Chlamydia trachomatis and Neisseria gonorrhoeae. J. Clin. Microbiol. 44:1084–1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dauphin LA, Bowen MD. 2009. A simple method for the rapid removal of Bacillus anthracis spores from DNA preparations. J. Microbiol. Methods 76:212–214 [DOI] [PubMed] [Google Scholar]
- 8. Dauphin LA, Hutchins RJ, Bost LA, Bowen MD. 2009. Evaluation of automated and manual commercial DNA extraction methods for recovery of Brucella DNA from suspensions and spiked swabs. J. Clin. Microbiol. 47:3920–3926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dauphin LA, Newton BR, Rasmussen MV, Meyer RF, Bowen MD. 2008. Gamma irradiation can be used to inactivate Bacillus anthracis spores without compromising the sensitivity of diagnostic assays. Appl. Environ. Microbiol. 74:4427–4433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Doganay M, Metan G, Alp E. 2010. A review of cutaneous anthrax and its outcome. J. Infect. Public Health 3:98–105 [DOI] [PubMed] [Google Scholar]
- 11. Ellerbrok H, et al. 2002. Rapid and sensitive identification of pathogenic and apathogenic Bacillus anthracis by real-time PCR. FEMS Microbiol. Lett. 214:51–59 [DOI] [PubMed] [Google Scholar]
- 12. Hadjinicolaou AV, et al. 2009. Use of molecular beacons and multi-allelic real-time PCR for detection of and discrimination between virulent Bacillus anthracis and other Bacillus isolates. J. Microbiol. Methods 78:45–53 [DOI] [PubMed] [Google Scholar]
- 13. Hodges LR, Rose LJ, O'Connell H, Arduino MJ. 2010. National validation study of a swab protocol for the recovery of Bacillus anthracis spores from surfaces. J. Microbiol. Methods 81:141–146 [DOI] [PubMed] [Google Scholar]
- 14. Hodges LR, Rose LJ, Peterson A, Noble-Wang J, Arduino MJ. 2006. Evaluation of a macrofoam swab protocol for the recovery of Bacillus anthracis spores from a steel surface. Appl. Environ. Microbiol. 72:4429–4430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hoffmaster AR, Fitzgerald CC, Ribot E, Mayer LW, Popovic T. 2002. Molecular subtyping of Bacillus anthracis and the 2001 bioterrorism-associated anthrax outbreak, United States. Emerg. Infect. Dis. 8:1111–1116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hoffmaster AR, et al. 2002. Evaluation and validation of a real-time polymerase chain reaction assay for rapid identification of Bacillus anthracis. Emerg. Infect. Dis. 8:1178–1182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Inglesby TV, et al. 2002. Anthrax as a biological weapon, 2002: updated recommendations for management. JAMA 287:2236–2252 [DOI] [PubMed] [Google Scholar]
- 18. Issa NC, et al. 2005. Comparison of specimen processing and nucleic acid extraction by the swab extraction tube system versus the MagNA Pure LC system for laboratory diagnosis of herpes simplex virus infections by LightCycler PCR. J. Clin. Microbiol. 43:1059–1063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jernigan DB, et al. 2002. Investigation of bioterrorism-related anthrax, United States, 2001: epidemiologic findings. Emerg. Infect. Dis. 8:1019–1028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Keim P, et al. 2000. Multiple-locus variable-number tandem repeat analysis reveals genetic relationships within Bacillus anthracis. J. Bacteriol. 182:2928–2936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Keim P, et al. 2004. Anthrax molecular epidemiology and forensics: using the appropriate marker for different evolutionary scales. Infect. Genet. Evol. 4:205–213 [DOI] [PubMed] [Google Scholar]
- 22. King DS, Luna VA, Cannons AC, Amuso PT. 2010. Procurement of spore-free Bacillus anthracis for molecular typing outside of BSL3 environment. J. Appl. Microbiol. 108:1817–1827 [DOI] [PubMed] [Google Scholar]
- 23. Kiratisin P, et al. 2002. Large-scale screening of nasal swabs for Bacillus anthracis: descriptive summary and discussion of the National Institutes of Health's experience. J. Clin. Microbiol. 40:3012–3016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Letant SE, et al. 2011. Rapid-viability PCR method for detection of live, virulent Bacillus anthracis in environmental samples. Appl. Environ. Microbiol. 77:6570–6578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Makino S, Uchida I, Terakado N, Sasakawa C, Yoshikawa M. 1989. Molecular characterization and protein analysis of the cap region, which is essential for encapsulation in Bacillus anthracis. J. Bacteriol. 171:722–730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Marston CK, et al. 2011. Molecular epidemiology of anthrax cases associated with recreational use of animal hides and yarn in the United States. PLoS One 6:e28274 doi:10.1371/journal.pone.0028274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mikesell P, Ivins BE, Ristroph JD, Dreier TM. 1983. Evidence for plasmid-mediated toxin production in Bacillus anthracis. Infect. Immun. 39:371–376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Moser MJ, Christensen DR, Norwood D, Prudent JR. 2006. Multiplexed detection of anthrax-related toxin genes. J. Mol. Diagn. 8:89–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Popovic T, et al. 2005. Validation of methods for confirmatory identification of presumptive isolates of Bacillus anthracis. J. AOAC Int. 88:175–177 [PubMed] [Google Scholar]
- 30. Robertson DL, Tippetts MT, Leppla SH. 1988. Nucleotide sequence of the Bacillus anthracis edema factor gene (cya): a calmodulin-dependent adenylate cyclase. Gene 73:363–371 [DOI] [PubMed] [Google Scholar]
- 31. Rose L, Jensen B, Peterson A, Banerjee SN, Srduino MJ. 2004. Swab materials and Bacillus anthracis spore recovery from nonporous surfaces. Emerg. Infect. Dis. 10:1023–1029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rotz LD, Khan AS, Lillibridge SR, Ostroff SM, Hughes JM. 2002. Public health assessment of potential biological terrorism agents. Emerg. Infect. Dis. 8:225–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shieh WJ, et al. 2003. The critical role of pathology in the investigation of bioterrorism-related cutaneous anthrax. Am. J. Pathol. 163:1901–1910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shlyakhov E, Rubinstein E. 1996. Evaluation of the anthraxin skin test for diagnosis of acute and past human anthrax. Eur. J. Clin. Microbiol. Infect. Dis. 15:242–245 [DOI] [PubMed] [Google Scholar]
- 35. Titball RW, Turnbull PC, Hutson RA. 1991. The monitoring and detection of Bacillus anthracis in the environment. Soc. Appl. Bacteriol. Symp. Ser. 20:9S–18S [PubMed] [Google Scholar]
- 36. Uchida I, Hashimoto K, Terakado N. 1986. Virulence and immunogenicity in experimental animals of Bacillus anthracis strains harbouring or lacking 110 MDa and 60 MDa plasmids. J. Gen. Microbiol. 132:557–559 [DOI] [PubMed] [Google Scholar]
- 37. Uchida I, Sekizaki T, Hashimoto K, Terakado N. 1985. Association of the encapsulation of Bacillus anthracis with a 60 megadalton plasmid. J. Gen. Microbiol. 131:363–367 [DOI] [PubMed] [Google Scholar]
- 38. Verhoeven P, Grattard F, Carricajo A, Pozzetto B, Berthelot P. 2010. Better detection of Staphylococcus aureus nasal carriage by use of nylon flocked swabs. J. Clin. Microbiol. 48:4242–4244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Walker RE, Petersen JM, Stephens KW, Dauphin LA. 2010. Optimal swab processing recovery method for detection of bioterrorism-related Francisella tularensis by real-time PCR. J. Microbiol. Methods 83:42–47 [DOI] [PubMed] [Google Scholar]
- 40. Welkos SL, et al. 1988. Sequence and analysis of the DNA encoding protective antigen of Bacillus anthracis. Gene 69:287–300 [DOI] [PubMed] [Google Scholar]