Abstract
Background
Exercise training reduces adiposity and risk of cardiovascular disease. However, the combined effects of habitual free-living physical activity and aerobic training on waist circumference, weight, fitness, and blood pressure in postmenopausal women are unknown.
Purpose
To evaluate the effects of habitual physical activity levels during aerobic training on weight, waist circumference, fitness, and blood pressure.
Design
Secondary analysis of an RCT. Original data collected April 2001 to June 2005 and analyzed in 2012.
Setting/participants
Postmenopausal women in a supervised exercise trial.
Intervention
Women (n=325) were randomized to 4, 8, or 12 kcal per kg per week of aerobic training or a control group for 6 months. All outcome measures were collected at baseline and follow-up. Changes in dependent variables within each training group were evaluated across tertiles of pedometer-determined habitual physical activity outside exercise training sessions.
Main outcome measures
Changes in waist circumference and weight.
Results
Reductions in waist circumference were significantly greater with higher steps/day accumulated outside exercise training compared to lower levels in the 4 (high: −4.8 cm vs low: −1.4 cm, p=0.03); 8 (high: −4.2 cm vs low: −0.4 cm, p=0.03), and 12 kcal per kg per week groups (high: −4.1 cm vs low: −0.7 cm, p=0.05). For all groups, p-trend < 0.03). A trend was observed for greater weight reduction with higher steps/day in the 4 kcal per kg per week group (p-trend= 0.04), but not for the other exercise doses. No effects were observed for blood pressure or fitness measures (all p>0.05).
Conclusions
In postmenopausal women, higher habitual physical activity while participating in aerobic training was associated with greater reductions in central adiposity, and was supportive of weight loss compared to lower levels.
Introduction
Public health guidelines recommend that adults obtain 150 minutes of moderate-to-vigorous physical activity per week to reduce risk of cardiovascular disease (CVD) and type 2 diabetes.1,2 Adopting aerobic training3-5 or increasing free-living habitual physical activity6-9 has the potential to improve health. However, whether habitual physical activity levels can augment the effects of aerobic training has not been evaluated or quantified.
High habitual physical activity combined with aerobic training could increase total daily energy expenditure and further promote a negative energy balance,10 which could enhance the cardio-metabolic benefits of aerobic training. This relationship has public health implications as it is important to understand the extent to which leading an inactive lifestyle while doing exercise training limits these adaptations, or conversely, if a more active lifestyle while training promotes greater improvements. Further, the clinical implications may be particularly important for postmenopausal women who have lower energy expenditure,11 and higher risk for developing CVD12 compared to premenopausal women.
The Dose Response to Exercise in Women (DREW) trial evaluated the effects of aerobic training at 50% below, 50% above, and at a dose congruent with public health guidelines.13 Habitual physical activity (steps/day) in DREW was measured by pedometers, which were removed during aerobic training. The purpose of this analysis was to determine the effect of habitual physical activity level in combination with aerobic training on adiposity, fitness, and blood pressure.
Methods
Design and Participants
The methodology13 and primary outcomes3 of DREW are published. DREW was an RCT evaluating the dose-response of aerobic training with increasingly higher doses of energy expenditure on cardiorespiratory fitness in sedentary postmenopausal women. The research protocol was reviewed and approved annually by the Cooper Institute IRB and subsequently approved by Pennington Biomedical Research Center for continued analysis. Written informed consent was obtained from all participants prior to screening. Data were collected from April 2001 to June 2005, and this secondary analysis was conducted in 2012. Participants were overweight or obese, sedentary women, and with elevated systolic blood pressure. Important exclusion criteria included CVD, conditions contraindicated for exercise training, elevated low-density lipoprotein (>3.36 mmol/L), or substantial weight loss in the previous year.13 There was no racial bias in the selection of participants.
This secondary analysis was based on a subset (n=325) of the DREW study, as women were excluded who: did not complete the trial (n=40); had ≤75% adherence to the exercise training program (n=10); did not have step-counter data for at least 5 of the 6 months of the exercise intervention (n=74); or displayed extreme (i.e., outlying) change in habitual steps/day over the course of the study (more than ±4,000 steps from baseline; n=15). There were no differences in relevant baseline factors between excluded and retained participants. In this secondary analysis, data were available for 72 participants from the control group, and for 106, 72, and 75 participants from the 4, 8, and 12 kcal per kg per week groups, respectively. The larger sample size in the 4 kcal per kg per week group reflects a design feature of DREW to increase the statistical power due to smaller anticipated changes compared to the 8 and 12 kcal per kg per week groups following exercise training
Fitness Testing
Testing was performed using a Lode Excalibur Sport electronically-braked cycle ergometer. Participants cycled at 30 watts (W) for 2 minutes, then 50 W for 4 minutes, followed by increases of 20 W every 2 minutes until they could no longer maintain a pedal cadence of 50 revolutions per minute. Respiratory gases were measured using a Parvomedics Truemax 2400 Metabolic Measurement Cart. Details have been previously published.13
Resting Blood Pressure
Resting blood pressure was evaluated with the participant in the supine position. Four blood pressure measurements were taken 2 minutes apart using a Colin STBP-780 automated BP unit.
Anthropometric Measures
Height was measured with a standard stadiometer. Weight was measured on an electronic scale. Waist circumference was measured following the guidelines of the Airlie Conference.14 BMI was determined by standard calculation.
Exercise Training
The exercise groups participated in three to four sessions each week for 6 months at a heart rate associated with 50% of each woman’s peak VO2. All participants were asked to maintain habitual physical activity levels during the study. During the first week, all groups expended 4 kcal perkg body weight per week. Participants assigned to the 4 kcal per kg per week group remained at that dose for the entire 6 months. All the other groups increased their energy expenditure by 1 kcal per kg body weight per week until they reached their assigned exercise dose.
Participants were weighed each week and their weight was multiplied by their assigned exercise dose to determine the number of calories to be expended for the week. Women in the exercise groups alternated training sessions on semi-recumbent cycle ergometers and treadmills. The exercise groups in DREW had an adherence of 99.5% of the target 6-month caloric expenditure.
Step Counter Data
Baseline average steps/day were measured with an Accusplit Eagle AE1620 pedometer over the course of 1 week prior to randomization.13 All participants, regardless of group assignment, wore pedometers during the entire intervention. Participants were instructed to wear pedometers during waking hours except while sleeping and bathing. The average steps/day represented their non-exercise habitual physical activity throughout the intervention. Change in steps from baseline was calculated as the average steps/day performed during the intervention (Month 1 through Month 6) subtracted from baseline.
Pedometers were removed during aerobic training sessions. Pedometer data were obtained from participants in the exercise groups at training sessions. Women in the control group mailed pedometer logs to study personnel. As mentioned previously, only participants with complete step counter data for at least 5 of 6 months of the exercise intervention were included in this analysis.
Statistical Procedure
Analyses were performed using SAS 9.3. Descriptive data were summarized as M (SD) or frequencies and percentages as appropriate. A one-way ANOVA was performed to evaluate baseline differences across randomization groups for continuous variables. A chi-squared test was used to test for baseline differences in categoric variables.
The total study sample was divided into tertiles based on average steps/day accumulated outside of aerobic training (baseline through follow-up Month 6). The control group was coded as a single group since these women did not receive any aerobic training intervention. An ANCOVA was performed to evaluate changes in adiposity and CVD risk factors across tertiles of steps/day with baseline value, age, and change in steps/day from baseline included as covariates. Results for each group are summarized as adjusted least-square means with 95% CIs. Multiple linear regression models were used to evaluate the association between habitual physical activity and anthropometric/CVD risk factors at a given dose of exercise. Trend analysis did not include the non-exercise control group as the goal of this particular analysis was to determine the effect of exercise training at various levels of habitual physical activity.
Last, an evaluation was made of the effect of habitual physical activity independent of the amount of exercise training on anthropometric, fitness and blood pressure variables. An ANCOVA was used with exercise dose, change in habitual steps/day and age in the model as covariates in exercisers only (n=253). Multiple linear regression analysis was performed to determine the trend across tertiles of habitual steps/day for the change in anthropometric and CVD risk factors following the 6-month intervention. For all analyses, a p-value <0.05 was used to reject the null hypothesis.
Results
Baseline characteristics are shown in Table 1. The women were approximately 66% Caucasian, and had M (SD) age of 57.3 years (6.2); and mean (SD) BMI of 32.1 (5.5). Study participants averaged 4943.8 (1751.4) steps/day at baseline, and 5456.1 (1751.4) steps/day during the 6-month intervention. No baseline differences were observed in subject characteristics among randomization groups.
Table 1.
Baseline characteristics and habitual physical activity (steps/day) during the intervention
| Control (n=72) |
4 kcal/kg (n=106) |
8 kcal/kg (n=72) |
12 kcal/kg (n=75) |
|
|---|---|---|---|---|
| Age (years) | 57.4 (5.8) | 57.9 (6.3) | 56.7 (6.6) | 56.9 (6.3) |
| African American (%, n) | 23.6 (17) | 34.0 (36) | 29.2 (21) | 22.7 (17) |
| Hormone replacement therapy (%, n) | 52.8 (38) | 39.6 (42) | 43.1 (31) | 46.7 (35) |
| Weight (Kg) | 86.7 (11.7) | 82.4 (11.9) | 85.3 (12.7) | 83.5 (11.3) |
| BMI | 32.5 (3.8) | 32.3 (7.8) | 32.3 (4.2) | 31.2 (3.5) |
| Waist Circumference(cm) | 102.0 (11.5) | 98.9 (10.6) | 102.5 (12.1) | 99.9 (12.0) |
| Peak VO2, mL per kg per minute | 15.4 (3) | 15.6 (2.9) | 14.9 (2.5) | 15.8 (2.7) |
| Peak VO2 (L/minute) | 1.3 (0.3) | 1.3 (0.2) | 1.3 (0.2) | 1.3 (0.2) |
| Baseline daily steps (steps per day) | 5195.9 (1655.5) | 4917.1 (1830.2) | 4806.2 (1668.4) | 4871.7 (1813.9) |
| Habitual physical activity (steps/day) | 5838.7 (1871.0) | 5316.2 (1699.2) | 5339.1 (1602.5) | 5398.8 (1593.2) |
| Change in average daily steps (steps/day) | 642.8 (1477.2) | 399.1 (1386.6) | 532.9 (1378.2) | 527.1 (1504.6) |
Note: Continuous variables are expressed as M (SD); categoric variables are expressed as (%, n). kcal/kg=kilocalories per kilogram of body weight per week (energy expenditure in the exercise training group).
Peak VO2: Maximal oxygen consumption
Baseline Characteristics Within Tertiles of Habitual Steps/Day
Mean baseline characteristics across tertiles of habitual steps/day accumulated outside of aerobic training are shown in Table 2. Trends were observed for higher baseline steps/day and greater change in steps/day across tertiles of habitual steps/day (p-trend <0.001). Participants in the highest tertile were younger, more fit, and had a lower BMI compared to women in the lowest tertile (p-trend<0.05).
Table 2.
Participant characteristics across tertiles of habitual physical activity accumulated during the exercise intervention (n=325)
| Habitual physical activity tertiles | ||||
|---|---|---|---|---|
| Tertile 1 (n=107) |
Tertile 2 (n=108) |
Tertile 3 (n=110) |
p-value | |
| Age (years) | 59.2 (6.7) | 57.5 (6.3) | 55.2 (5.0) | <0.001 |
| Weight (kg) | 86.4 (12.3) | 84.0 (12.3) | 82.4 (11.0) | 0.016 |
| BMI | 33.0 (6.0) | 32.2 (6.2) | 31.0 (3.8) | 0.008 |
| Waist Circumference (cm) | 102.6 (10.9) | 100.0 (11.9) | 98.8 (11.5) | 0.020 |
| Peak VO2 (mL per kilogram per minute) | 14.6 (2.6) | 15.4 (3.0) | 16.3 (2.6) | <0.001 |
| Peak VO2 (L/min) | 1.3 (0.2) | 1.3 (0.2) | 1.3 (0.3) | 0.008 |
| Baseline daily steps (steps/day) | 3543.6 (1253.1) | 4954.7 (1431.2) | 6295.1 (1346.3) | <0.001 |
| Daily steps during intervention (steps/day) | 3609.3 (630.3) | 5348.7 (438.7) | 7357.9 (999.8) | <0.001 |
| Change in average daily steps (steps/day) | 65.7 (1253.8) | 394.0 (1393.1) | 1062.8 (1456.8) | <0.001 |
Note: Shown are the baseline characteristics of participants in the DREW study stratified by tertiles of daily physical activity outside the exercise intervention. Values are expressed as M (SD). Tertiles are calculated based on the average daily step count obtained through pedometry. Significant trends across tertiles for continuous variables were analyzed using multiple linear regression.
Steps per day were 1687–4467 for Tertile 1; 4485-6203 for Tertile 2; 6209–10,571 for Tertile 3.
Peak VO2: Maximal oxygen consumption
Changes in Anthropometric, Fitness, and Blood Pressure Measures Following Intervention Across Tertiles of Habitual Steps/Day Accumulated Outside of Exercise Training
Changes in waist circumference, weight, relative fitness, and systolic blood pressure following structured exercise training across tertiles of habitual steps/day are shown in Appendix A (available online at www.ajpmonline.org). In the 4 kcal per kg per week group, waist circumference was reduced in the highest tertile of habitual steps/day compared to the lowest tertile (−4.8 cm [95% CI=−7.0, −2.6] vs. −1.5 cm [95% CI= −3.4, 0.4), p =0.03). In the 8 kcal per kg per week group, waist circumference was reduced in the highest tertile compared to the lowest tertile (−4.2 cm, [95% CI= −6.7, −1.8] vs. −0.4 cm [95% CI= −2.8, 2.0], p= 0.03). In the 12 kcal per kg per week group, waist circumference was reduced in the highest tertile and in the lowest tertile (−4.1 cm [95% CI= −6.4. −1.8] vs. −0.7 cm [95% CI= −3.2, 1.8], p= 0.05).
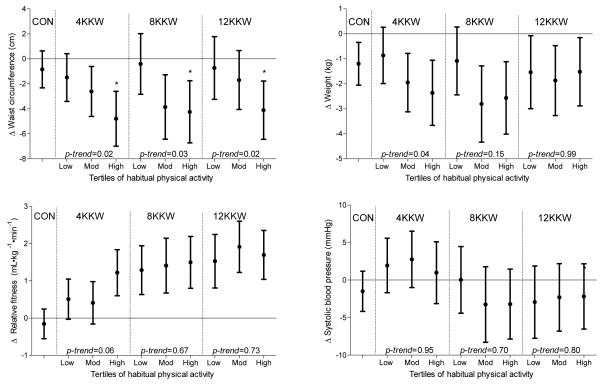
Figure 1.
Change in anthropometric, fitness and blood pressure across tertiles of habitual physical activity following training CON, control; KKW, kcal per kg per week
A main effect was observed for the change in waist circumference with tertile of habitual steps/day (p=0.002). However, there was no interaction between exercise training dose and habitual steps/day tertile (p=0.83). Analysis for trend revealed a greater reduction in waist circumference with higher amounts of habitual steps/day in the 4 (p-trend= 0.02); 8, (p-trend=0.03); and 12 kcal per kg per week (p-trend=0.03) groups, respectively (Figure 1). Weight was not significantly reduced in the highest tertile compared to the lowest tertile of habitual steps/day in the 8 (p=0.15) and 12 kcal per kg per week groups (p=0.99), but weight reduction approached significance in the 4 kcal per kg per week group (p=0.09). Weight change across tertiles of habitual steps/day was only significant (p-trend=0.04) in the 4 kcal per kg per week group (Figure 1).
Changes in relative fitness across tertiles of habitual steps/day approached significance in the 4 kcal per kg per week group (p=0.06), but was not significant in the 8 (p=0.67) or 12 kcal per kg per week groups (p=0.73). Similarly, test for trend for increasing relative fitness with higher amounts of habitual steps/day approached significance in the 4 kcal per kg per week group (p-trend= 0.06), but not the 8 (p=0.53) or 12 kcal per kg per week groups (p= 0.49; Figure 1). Absolute fitness, systolic (Figure 1), and diastolic blood pressure were not significantly different between the highest tertile compared to the lowest tertile of habitual steps/day (all p>0.05), and all tests for trends for these parameters were not significant.
Changes in the Effect of Habitual Steps/Day on Anthropometric, Fitness, and Blood Pressure Independent of Exercise Training Dose
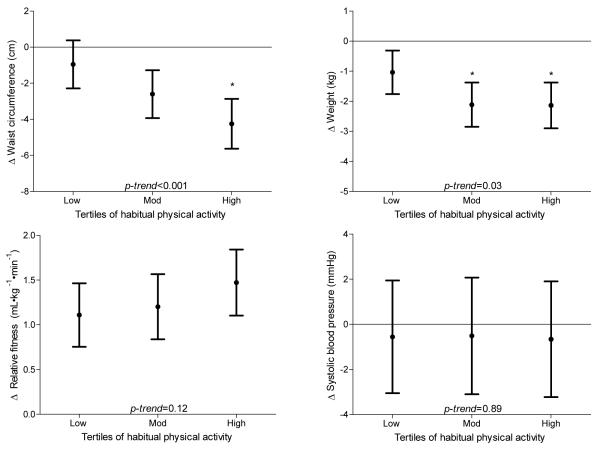
As shown in Figure 2, waist circumference (Figure 2) and weight (Figure 2) were reduced in the highest tertile of habitual steps/day compared to the lowest tertile (p<0.05). No effects were observed for absolute, relative fitness (Figure 2); systolic (Figure 2); or diastolic blood pressure.
Figure 2.
Change in anthropometric, fitness and blood pressure across tertiles of habitual physical activity following training with dose of exercise entered as a covariate (n=253)
Discussion
The primary finding of this secondary analysis of overweight and obese postmenopausal women participating in aerobic training was that those individuals with higher levels of habitual physical activity had greater reductions in waist circumference. This effect was found in women exercising at levels consistent with 50%, 100% and 150% of public health guidelines. In addition, higher levels of habitual physical activity were generally supportive of body weight reductions, especially in participants training below recommended levels of structured aerobic exercise. However, no additional benefits were observed for habitual physical activity level on fitness or blood pressure at any exercise training dose. These findings have public health implications for postmenopausal women, who as a group have elevated CVD risk12 and lower energy expenditure11 compared to premenopausal women. To our knowledge, this is the first study to examine and quantify the effect of habitual physical activity level on anthropometric and CVD risk factors in individuals participating in traditional structured exercise programs. Exercise training studies typically do not address how total physical activity levels (exercise training and habitual physical activity) affect body composition. Data from the present study show that women who had higher habitual activity levels had greater reductions in waist circumference compared to those with lower levels in the 4 (−4.8 cm vs −1.5 cm); 8 (−3.9 cm vs −0.4 cm) and 12 kcal per kg per week groups (−4.1 cm vs −0.7 cm). Similarly, when dose of exercise was held constant, the independent effect of higher habitual physical activity levels (>6209 steps/day) while exercise training was equivalent to a reduction in waist circumference of −4.2 cm. Based on epidemiologic data, this corresponds to approximately a 7% reduction in CVD risk above and beyond exercise training performed while maintaining lower physical activity habitual levels (<3652 steps/day, −1.0 cm).15 Similarly, higher levels of habitual physical activity with aerobic training may augment weight loss, although observed weight loss in general was modest.
Interestingly, higher habitual physical activity did not influence absolute fitness or blood pressure above and beyond structured exercise training. Habitual physical activity may not have been performed at a high enough intensity to influence absolute or relative fitness parameters,16-18 but the additional energy expenditure likely promoted greater adiposity loss. Similarly, no changes in systolic or diastolic blood pressure were observed. Few published studies have investigated the effects of habitual physical activity level during exercise training on CVD risk factors. Di Blasio et al.19 reported no differences in fitness, heart rate, or blood pressure in postmenopausal women (n=34) who decreased spontaneous activity during exercise training compared to women who maintained or increased their physical activity outside of training.19 The present study supports and expands on these findings.
It is important to note that this study is descriptive in the sense that women self-selected their habitual physical activity levels while participating in aerobic training. Nevertheless, these data provide evidence that a dual approach of increasing both habitual physical activity and adopting aerobic training could optimize reductions in central adiposity and weight in women with low levels of habitual physical activity. Women in the lowest tertile for habitual physical activity were generally older, had lower relative fitness and were likely to be at the greatest risk of future weight gain.20,21 In addition, the current findings suggest that weight and waist circumference reductions are less likely to result from exercise training if habitual physical activity levels remain low. However, a prospective study is needed to evaluate the safety, feasibility and efficacy of this dual approach in sedentary individuals.
The present study has several strengths. DREW was a large randomized trial in which exercise dose was strictly monitored and supervised. Additionally, step-counter data were collected during the entire training intervention. Limitations of this analysis are that it is not possible to determine the intensity of habitual physical activity, dietary information was not measured during the training intervention, and our results may not be generalizable to other aerobic training intensities or modalities.
Conclusion
Habitual physical activity affects the effectiveness of structured aerobic training in reducing waist circumference in overweight and obese postmenopausal women. However, no additional effects were found for blood pressure or fitness. Future studies should investigate combining exercise training and increasing habitual physical activity prospectively in sedentary individuals, and evaluating their independent and combined effects on body composition and CVD risk factors.
Supplementary Material
Acknowledgements
This work was performed at The Cooper Institute, and the staff is especially commended for their efforts. The authors thank The Cooper Institute Scientific Advisory Board and the DREW participants. In addition, the authors thank the NIH T-32 postdoctoral fellowship (Obesity from Genes to man) which supports the salary and training of Dr. Damon Swift at Pennington Biomedical Research Center. This work was supported by NIH (grant number HL66262) and unrestricted research support from The Coca-Cola Company.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Haskell WL, Lee I-M, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: Updated recommendation for adults from the american college of sports medicine and the american heart association. Med. Sci. Sports Exerc. 2007;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 2.National Institute of Health Physical activity and cardiovascular health: Nih consensus development panel on physical activity and cardiovascular health. JAMA. 1996;276(3):241–246. [PubMed] [Google Scholar]
- 3.Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure. JAMA. 2007;297(19):2081–2091. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- 4.Church TS, Blair SN, Cocreham S, Johannsen N, Johnson W, Kramer K, et al. Effects of aerobic and resistance training on hemoglobin a1c levels in patients with type 2 diabetes. JAMA: The Journal of the American Medical Association. 2010;304(20):2253–2262. doi: 10.1001/jama.2010.1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kraus WE, Houmard JA, Duscha BD, Knetzger KJ, Wharton MB, McCartney JS, et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N. Engl. J. Med. 2002;347(19):1483–1492. doi: 10.1056/NEJMoa020194. [DOI] [PubMed] [Google Scholar]
- 6.Tully MA, Cupples ME. Unistep (university students exercise and physical activity) study: A pilot study of the effects of accumulating 10,000 steps on health and fitness among university students. J. Phys. Act. Health. 2011;8(5):663–667. doi: 10.1123/jpah.8.5.663. [DOI] [PubMed] [Google Scholar]
- 7.David P, Buckworth J, Pennell ML, Katz ML, DeGraffinreid CR, Paskett ED. A walking intervention for postmenopausal women using mobile phones and interactive voice response. J. Telemed. Telecare. 2012;18(1):20–25. doi: 10.1258/jtt.2011.110311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Musto A, Jacobs K, Nash M, DelRossi G, Perry A. The effects of an incremental approach to 10,000 steps/day on metabolic syndrome components in sedentary overweight women. J. Phys. Act. Health. 2010;7(6):737–745. doi: 10.1123/jpah.7.6.737. [DOI] [PubMed] [Google Scholar]
- 9.Armit CM, Brown WJ, Marshall AL, Ritchie CB, Trost SG, Green A, et al. Randomized trial of three strategies to promote physical activity in general practice. Prev. Med. 2009;48(2):156–163. doi: 10.1016/j.ypmed.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med. Sci. Sports Exerc. 2009;41(2):459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 11.Lovejoy JC, Champagne CM, de Jonge L, Xie H, Smith SR. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int. J. Obes. 2008;32(6):949–958. doi: 10.1038/ijo.2008.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kannel WB, Hjortland MC, McNamara PM, Gordon T. Menopause and risk of cardiovascular disease. Ann. Intern. Med. 1976;85(4):447–452. doi: 10.7326/0003-4819-85-4-447. [DOI] [PubMed] [Google Scholar]
- 13.Morss GM, Jordan AN, Skinner JS, Dunn AL, Church TS, Earnest CP, et al. Dose-response to exercise in women aged 45-75 yr (drew): Design and rationale. Med. Sci. Sports Exerc. 2004;36(2):336–344. doi: 10.1249/01.MSS.0000113738.06267.E5. [DOI] [PubMed] [Google Scholar]
- 14.Lohman T. Antropometric standardization reference manual. Human Kinetics; Champaign: 1988. [Google Scholar]
- 15.de Koning L, Merchant AT, Pogue J, Anand SS. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: Meta-regression analysis of prospective studies. Eur. Heart J. 2007;28(7):850–856. doi: 10.1093/eurheartj/ehm026. [DOI] [PubMed] [Google Scholar]
- 16.O’Donovan G, Owen A, Bird SR, Kearney EM, Nevill AM, Jones DW, et al. Changes in cardiorespiratory fitness and coronary heart disease risk factors following 24 wk of moderate- or high-intensity exercise of equal energy cost. J. Appl. Physiol. 2005;98(5):1619–1625. doi: 10.1152/japplphysiol.01310.2004. [DOI] [PubMed] [Google Scholar]
- 17.Gormley SE, Swain DP, High R, Spina RJ, Dowling EA, Kotipalli US, et al. Effect of intensity of aerobic training on vo2max. Med. Sci. Sports Exerc. 2008;40(7):1336–1343. doi: 10.1249/MSS.0b013e31816c4839. [DOI] [PubMed] [Google Scholar]
- 18.Kemi OJ, Haram PM, Loennechen JP, Osnes J-B, Skomedal T, Wisløff U, et al. Moderate vs. High exercise intensity: Differential effects on aerobic fitness, cardiomyocyte contractility, and endothelial function. Cardiovasc. Res. 2005;67(1):161–172. doi: 10.1016/j.cardiores.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 19.Di Blasio A, Ripari P, Bucci I, Di Donato F, Izzicupo P, D’Angelo E, et al. Walking training in postmenopause: Effects on both spontaneous physical activity and training-induced body adaptations. Menopause. 2011 doi: 10.1097/gme.0b013e318223e6b3. In Press. [DOI] [PubMed] [Google Scholar]
- 20.Sternfeld B, Wang H, Quesenberry CP, Abrams B, Everson-Rose SA, Greendale GA, et al. Physical activity and changes in weight and waist circumference in midlife women: Findings from the study of women’s health across the nation. Am. J. Epidemiol. 2004;160(9):912–922. doi: 10.1093/aje/kwh299. [DOI] [PubMed] [Google Scholar]
- 21.Littman AJ, Kristal AR, White E. Effects of physical activity intensity, frequency, and activity type on 10-y weight change in middle-aged men and women. Int. J. Obes. Relat. Metab. Disord. 2005;29(5):524–533. doi: 10.1038/sj.ijo.0802886. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.