Abstract
The aims of this study were to optimize the experimental conditions for labeling extracellularly oriented, solvent-exposed cysteine residues of γ-aminobutyric acid transporter 1 (GAT1) with the membrane-impermeant sulfhydryl reagent [2-(trimethylammonium)ethyl]methanethiosulfonate (MTSET) and to characterize the functional and pharmacological consequences of labeling on transporter steady-state and presteady-state kinetic properties. We expressed human GAT1 in Xenopus laevis oocytes and used radiotracer and electrophysiological methods to assay transporter function before and after sulfhydryl modification with MTSET. In the presence of NaCl, transporter exposure to MTSET (1–2.5 mM for 5–20 min) led to partial inhibition of GAT1-mediated transport, and this loss of function was completely reversed by the reducing reagent dithiothreitol. MTSET treatment had no functional effect on the mutant GAT1 C74A, whereas the membrane-permeant reagents N-ethylmaleimide and tetramethylrhodamine-6-maleimide inhibited GABA transport mediated by GAT1 C74A. Ion replacement experiments indicated that MTSET labeling of GAT1 could be driven to completion when valproate replaced chloride in the labeling buffer, suggesting that valproate induces a GAT1 conformation that significantly increases C74 accessibility to the extracellular fluid. Following partial inhibition by MTSET, there was a proportional reduction in both the presteady-state and steady-state macroscopic signals, and the functional and pharmacological properties of the remaining signals were indistinguishable from those of unlabeled GAT1. Therefore, covalent modification of GAT1 at C74 results in completely nonfunctional as well as electrically silent transporters.
Keywords: Neurotransmitter:sodium symporter, SLC6, GABA transporter, SLC6A1, Sulfhydryl modification, Cysteine 74
Introduction
In the nervous system, removal of the inhibitory neurotransmitter γ-aminobutyric acid (GABA) from the extracellular space of neurons and glia is accomplished by electrogenic Na+- and Cl−-coupled GABA transporters (GATs) (Borden 1996; Nelson 1998; Dalby 2003; Richerson and Wu 2003; Conti et al. 2004). Four GAT isoforms exist in mammalian tissues and belong to the large neurotransmitter/Na+ symporter family (NSS; 2.A.22 according to the transporter classification system; SLC6 according to the Human Genome Organization classification) (Nelson 1998; Busch and Saier 2002; Chen et al. 2004; Saier et al. 2006). Two sets of nomenclature systems are used to refer to the GATs: rat/human GAT-1, BGT-1, GAT-2 and GAT-3 correspond to mouse GAT1, GAT2, GAT3 and GAT4, respectively. GAT1 was the first family member to be cloned (Guastella et al. 1990; Nelson et al. 1990) and paved the way for the cloning and characterization of the related serotonin, dopamine, norepinephrine and glycine transporters (Blakely et al. 1991; Hoffman et al. 1991; Kilty et al. 1991; Pacholczyk et al. 1991; Shimada et al. 1991; Usdin et al. 1991; Guastella et al. 1992; Liu et al. 1992). GAT1 is the most abundant isoform within the nervous system and is expressed in both neurons and glia (Conti et al. 2004; Madsen et al. 2010). Tiagabine, a specific inhibitor of GAT1, is used clinically as an anticonvulsant drug and highlights the importance of GAT1 in maintaining GABA homeostasis in the brain extracellular fluid (Dalby 2003; Schousboe et al. 2011).
Chemical modification of endogenous or engineered cysteine residues has served as an important tool for structure–function studies of membrane proteins (Frillingos et al. 1998; Rudnick 2006; Guan and Kaback 2007; see also Anderson et al. 2010); and, in particular, when coupled with high-resolution information from crystal structures, sulfhydryl modification has served as a powerful tool to address specific questions regarding the functional role of targeted residues. Ideally, individual cysteine residues are engineered in the primary protein sequence against a cysteine-less background. Covalent modification of the introduced cysteine with thiol-specific probes, many of which differ in chemical properties, would then provide insight regarding the role that the residue in question plays in protein function. In practice, however, cysteine-less membrane proteins are difficult to study as they may not be properly trafficked to the plasma membrane or may be nonfunctional. Therefore, many investigators have relied on labeling endogenous cysteines in order to glean insight about protein function. This happens to be the case with GAT1. The extracellularly exposed, endogenous cysteine residue of GAT1, cysteine 74 (C74), has been used to gain insight into the nature and functional consequences of sulfhydryl modification at this residue (Bennett and Kanner 1997; Yu et al. 1998; Golovanevsky and Kanner 1999; Li et al. 2000; Kanner 2003; Zomot and Kanner 2003; Zhou et al. 2004, 2006; Zhou and Kanner 2005; Zomot et al. 2005; Mari et al. 2006; Rosenberg and Kanner 2008; Ben-Yona and Kanner 2009; Meinild et al. 2009). While it has been shown that sulfhydryl modification at C74 renders the transporter nonfunctional, the mechanism of this effect is not known. In previous studies, rather harsh labeling conditions were required to achieve any significant degree of GAT1 C74 labeling, which made it difficult to carry out a thorough biophysical characterization of the labeled transporter.
With the long-term goal of utilizing endogenous, extracellularly oriented, solvent-exposed cysteine residues of GAT1 for specific and targeted transporter labeling in the Xenopus laevis oocyte plasma membrane, we set out to fully characterize the functional consequences of sulfhydryl modification of GAT1 with the membrane-impermeant sulfhydryl reagent [2-(trimethylammonium)ethyl]methanethiosulfonate (MTSET). Our data suggest that C74 is very likely the only functionally sensitive residue labeled by MTSET and that such labeling renders the transporter nonfunctional as well as electrically silent with respect to all known electrophysiological assays of transporter function (steady-state and presteady-state measurements). Labeling in the presence of valproate, an anion that specifically interacts with GAT1 and increases the rate of Na+/Cl−/GABA cotransport (Whitlow et al. 2003), significantly increases the accessibility of C74 to the extracellular fluid and, hence, allows for rapid and complete labeling of all transporter copies at the cell surface. Our findings have established the optimal conditions for labeling GAT1 in the plasma membrane and set the stage for future structure–function studies.
Experimental Procedures
Expression of Wild-type (WT) and Mutant GAT1 in X. laevis Oocytes
Stage V–VI X. laevis oocytes were injected with 50 ng of complementary RNA (cRNA) for human GAT1 (SLC6A1) (Nelson et al. 1990; Chen et al. 2004) or the mutant GAT1 C74A. The GAT1 C74A mutant was generated by polymerase chain reaction site-directed mutagenesis using the QuikChange Lightning Site-Directed Mutagenesis Kit (Agilent Technologies, La Jolla, CA). The sense (5′ GG TTC CCC TAT CTC GCC GGG AAA AAT GGT GGG 3′) and antisense (3′ CC AAG GGG ATA GAG CGG CCC TTT TTA CCA CCC 5′) mutagenic primers were synthesized by Retrogen (San Diego, CA); underlined bases denote the mutated codon. Following site-directed mutagenesis, the entire coding region of the plasmid containing GAT1 C74A was sequenced (Retrogen) to confirm the proper introduction of the mutation. cRNA for (WT) GAT1, or GAT1 C74A, was synthesized in vitro using T7 RNA polymerase (mMessage mMachine T7 Kit; Applied Biosystems/Ambion, Austin, TX). After cRNA injection, oocytes were maintained in Barth’s medium (in mM: 88 NaCl, 1 KCl, 0.33 Ca(NO3)2, 0.41 CaCl2, 0.82 MgSO4, 2.4 NaHCO3 and 10 HEPES [pH 7.4] as well as 50 μg/ml gentamicin, 100 μg/ml streptomycin and 100 U/ml penicillin) at 18 °C for up to 14 days until used in experiments. Unless otherwise indicated, all experiments were performed at 21 ± 2 °C.
Experimental Solutions and Reagents
Unless otherwise indicated, experiments were performed in NaCl buffer containing (in mM) 100 NaCl, 2 KCl, 1 CaCl2, 1 MgCl2 and 10 HEPES (pH 7.4). In experiments which required Na+-free conditions, NaCl was isosmotically replaced, depending on the experimental protocol, with choline-Cl, LiCl, KCl, CsCl or tetraethylammonium-chloride. In experiments which required Cl−-free conditions, NaCl was isosmotically replaced with Na-[2-(N-morpholino) ethanesulfonic acid], Na-gluconate or Na-(2-propylpentanoic acid) (Na-valproate). In chloride-free buffers, KCl, CaCl2 and MgCl2 were replaced with their corresponding gluconate salts. The buffers used for solutions at pH 5.0 and 9.0 were MES and N-tris(hydroxymethyl)methyl-3-aminopropanesulfonic acid, respectively. GABA, 1-(4,4-diphenyl-3-butenyl)-3-piperidinecarboxylic acid (SKF-89976A), 1-[2-[[(diphenylmethylene)imino]oxy]ethyl]-1,2,5,6-tetrahydro-3-pyridinecarboxylic acid (NO-711), MTSET, 2-[(methylsulfonyl)thio]ethanesulfonic acid (MTSES, sodium salt), N-ethylmaleimide (NEM), tetramethylrhodamine-6-maleimide (TMR6M) and/or dithiothreitol (DTT) was added to the experimental solution as indicated. Stock solutions of sulfhydryl reagents (MTSET, MTSES, NEM and TMR6M) were stored in nanopure water (MTSET, MTSES), absolute ethanol (NEM) or dimethyl sulfoxide (TMR6M) at −20 °C and diluted in the experimental solution immediately before use. DTT was prepared from the solid material immediately before use. MTSET and MTSES were purchased from Toronto Research Chemicals (Toronto, ON, Canada) or Anatrace (Maumee, OH). TMR6M was purchased from Invitrogen (Carlsbad, CA). [3H]-GABA was obtained from GE Healthcare (Piscataway, NJ). All other reagents were purchased from Fisher Scientific (Pittsburgh, PA) or Sigma (St. Louis, MO).
Electrophysiological Measurements and Data Analysis
The two-microelectrode voltage-clamp technique was used for the recording of whole-cell transporter-mediated currents. Oocytes were voltage-clamped at the indicated membrane potential (V
m) using the Warner oocyte clamp (OC-725C; Warner Instrument; Hamden, CT). In the experimental recording chamber, oocytes were initially stabilized in NaCl buffer, and the composition of the bath was changed as indicated. In all experiments, reference electrodes were connected to the experimental oocyte chamber via agar bridges (3 % agar in 3 M KCl). For continuous holding current measurements, currents were low pass-filtered at 1 Hz (LPF 8, Warner Instrument) and sampled at 10 Hz (pCLAMP 8.1; Axon Instruments, Union City, CA). The GABA-evoked current was obtained as the difference in steady-state current in the absence and presence of GABA and/or inhibitor. As the GAT1-mediated, GABA-evoked current is Na+- and Cl−-coupled (Loo et al. 2000), it is referred to as
The effects of substrate concentration ([GABA]o, [Na+]o and [Cl−]o) on the steady-state kinetics were determined by nonlinear curve fitting of the induced currents (I) with Eq. 1:
| 1 |
where S is the substrate (GABA, Na+ or Cl−),
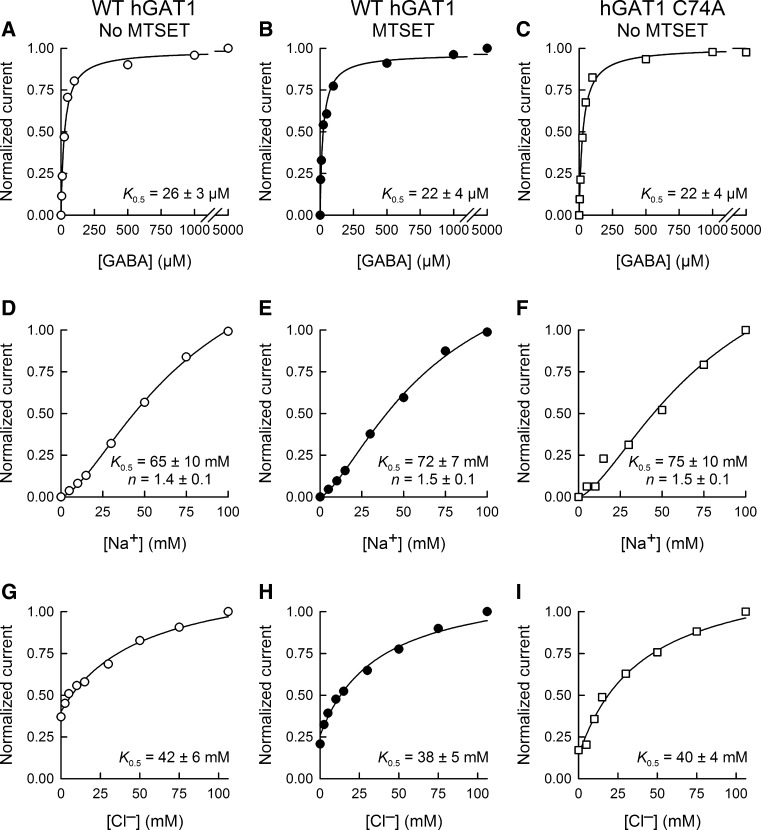
Fig. 6.
Steady-state kinetic parameters of WT GAT1 before and after sulfhydryl modification with MTSET. Representative GABA (a–c), Na+ (d–f) and Cl− (g–i) steady-state kinetic curves are shown for WT GAT1 before (left panels) and after (middle panels) treatment with MTSET (1 mM for 5 min at −50 mV) as well as for GAT1 C74A without MTSET treatment (right panels). The half-maximal concentration values (K 0.5) for GABA, Na+ and Cl− were similar for WT GAT1 and GAT1 C74A. The Hill coefficient values for Na+ and Cl− activation of the inward currents were also similar for WT GAT1 and GAT1 C74A. Moreover, MTSET exposure had no effect on WT GAT1 steady-state kinetic parameters. V m = −50 mV. For GABA kinetic experiments (a–c), [Na+]0 was 100 mM and [Cl−] was 106 mM. For sodium kinetic experiments (d–f), [Cl−] was 106 mM and [GABA]0 was 5 mM. For chloride kinetic experiments (g–i), [Na+]0 was 100 mM and [GABA]0 was 5 mM. The smooth lines represent fits of the experimental data with Eq. 1 (see “Experimental Procedures” Section). Reported values represent the mean ± SE from three or more oocytes
To examine the carrier-mediated presteady-state current transients, the pulse protocol consisted of voltage jumps (400 ms) from the holding voltage (−50 mV) to test voltages ranging from +80 to −130 mV in 15-mV steps. Unless otherwise indicated, voltage pulses were separated by an interval of at least 3 s in order to allow for complete relaxation of the OFF transients (see Sacher et al. 2002; Karakossian et al. 2005). Currents were low pass-filtered at 1 kHz and sampled at 12.5 kHz without averaging. To obtain the transporter presteady-state currents, at each V m, the total current for the ON transients, I(t), was fitted with Eq. 2:
| 2 |
where t is time,
| 3 |
where Q NaCl = Q dep − Q hyp (Q dep and Q hyp are Q at depolarizing and hyperpolarizing limits, respectively) and represents the maximum charge moved (i.e., Q max), z is the apparent valence of movable charge, δ is the fraction of the membrane electric field traversed by the charge, V 0.5 is the V m for 50 % charge movement, F is Faraday’s constant, R is the gas constant and T is the absolute temperature.
The inhibition experiments involved GAT1-specific competitive inhibitors of GABA transport (SKF-89976A and NO-711). Data for the inhibition experiments were fitted with Eq. 4 (Krause and Schwarz 2005; Matthews et al. 2009):
| 4 |
where I
max is the maximum current evoked by a saturating concentration of GABA in the absence of the blocker (B, here SKF-89976A or NO-711), I is the evoked current in the presence of the indicated concentrations of GABA and blocker (B),
To determine the effect of sulfhydryl modification on the ratio of GAT1-mediated charge flux to GABA flux across the plasma membrane, uptake experiments were performed under voltage clamp in individual control oocytes and oocytes expressing WT GAT1 (Eskandari et al. 1997; Forster et al. 1999; Loo et al. 2000; Sacher et al. 2002; Whitlow et al. 2003; Karakossian et al. 2005; Gonzales et al. 2007; Matthews et al. 2009). The membrane potential was held at the indicated value (−50 mV), and the holding current was continuously monitored. Oocytes were initially incubated in NaCl buffer until a baseline was established. GABA (500 μM) and [3H]-GABA (20 nM) were added to the perfusion solution for 5–10 min. At the end of the incubation period, GABA and the isotope were removed from the perfusion solution until the holding current returned to baseline. Oocytes were removed from the experimental chamber, washed in ice-cold choline-Cl buffer and solubilized in 10 % sodium dodecyl sulfate (SDS). Oocyte [3H]-GABA content was determined in a liquid scintillation counter (LS 6500; Beckman, Fullerton, CA). Net inward charge was obtained from the time integral of the GABA-evoked inward current and correlated with GABA influx in the same cell. GABA uptake under voltage clamp was also performed in oocytes expressing WT GAT1 after a 5-min exposure to 1 mM MTSET in NaCl buffer. This treatment reduces the GAT1-mediated, GABA-evoked current by approximately 50 % (see Figs. 1, 2, 3, 4, 7). In all experiments, the GAT1-mediated GABA uptake was obtained by subtracting endogenous GABA uptake in control cells from the same batch that were subjected to the same experimental condition as GAT1-expressing cells. Depending on the level of GAT1 expression in the plasma membrane as well as the duration of GABA exposure (5–10 min), the magnitude of endogenous GABA uptake was 0.5–5 % of the total GABA uptake (endogenous plus GAT1-mediated uptake).
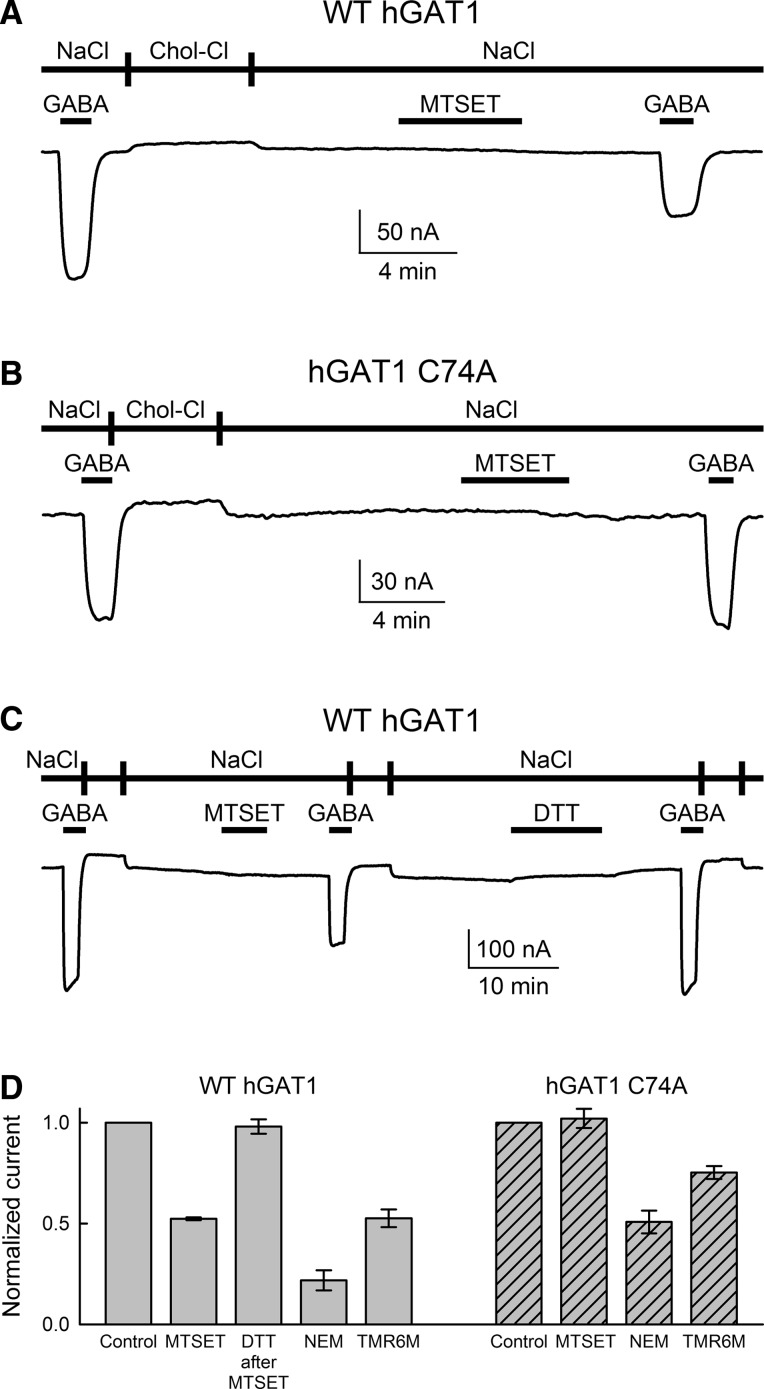
Fig. 1.
WT GAT1, but not GAT1 C74A, is sensitive to membrane-impermeant sulfhydryl reagents. a A representative GABA-evoked (500 μM) current trace is shown for WT GAT1 before and after labeling with the membrane-impermeant sulfhydryl reagent MTSET. Labeling of GAT1 with MTSET led to ~50 % reduction in the GABA-evoked current. The membrane potential (V m) was −50 mV throughout the experiment. Labeling was carried out at 1 mM MTSET for 5 min in NaCl buffer bathing the oocyte (at 21 ± 2 °C, pH 7.4). b Similar to WT GAT1, GAT1 C74A mediates Na+-dependent and Cl−-facilitated GABA transport (see Fig. 6). Exposure of GAT1 C74A to MTSET (1 mM for 5 min) had no effect on the magnitude of the GABA-evoked (500 μM) current. c Sulfhydryl modification of WT GAT1 with MTSET was completely reversed with DTT. Labeling with MTSET was carried out as in (a), and DTT was applied at 12 mM for 10 min in NaCl buffer. d Summary of data collected from four or more oocytes expressing WT GAT1 or GAT1 C74A. For each experimental condition, the GABA-evoked current obtained after labeling with MTSET, NEM or TMR6M (all at 1 mM for 5 min at −50 mV) was normalized to that prior to sulfhydryl modification in the same cell. Reported values represent the mean ± SE from four or more oocytes. Note that GAT1 C74A is insensitive to the membrane-impermeant MTSET but sensitive to the membrane-permeant NEM. GAT1 C74A was also sensitive to TMR6M
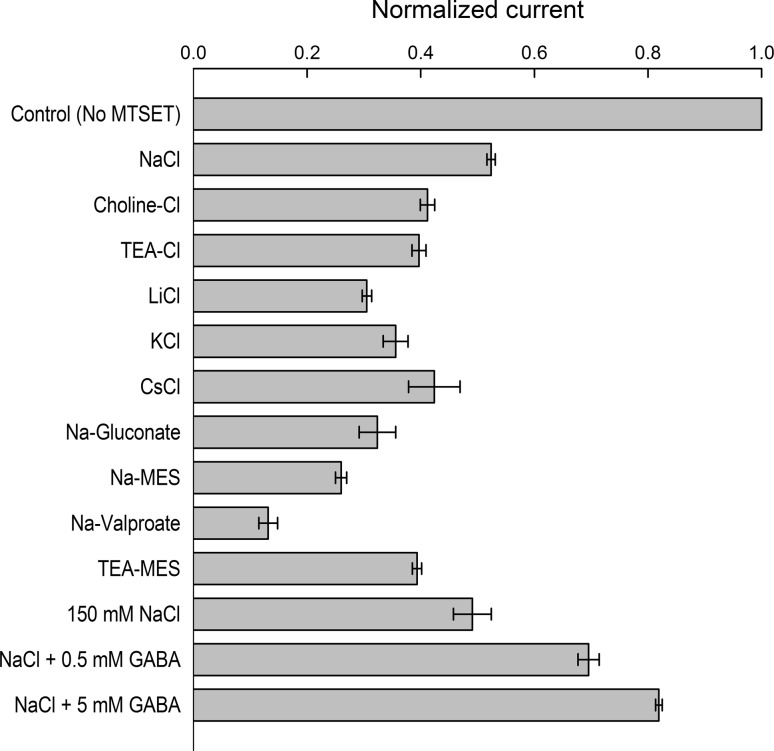
Fig. 2.
Effect of buffer composition on MTSET labeling of WT GAT1. WT GAT1 was labeled with MTSET in the indicated extracellular bathing solution, in which Na+ and/or Cl− of the NaCl buffer had been isosmotically replaced by another cation or anion, respectively. The experimental protocol was similar to that shown in Fig. 1 (5-min exposure to 1 mM MTSET at −50 mV, 21 ± 2 °C, pH 7.4) with the exception that sulfhydryl modification was carried out in the indicated buffer. The GABA-evoked (500 μM in NaCl buffer) current after MTSET modification was normalized to that obtained in the same cell before exposure to MTSET. Reported values represent the mean ± SE from three or more oocytes
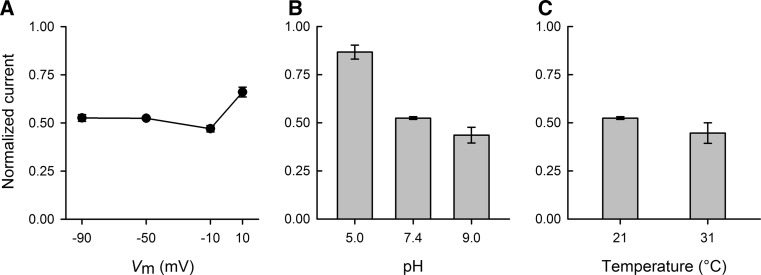
Fig. 3.
Effect of membrane potential, pH and temperature on MTSET labeling of WT GAT1. The GABA-evoked (500 μM at −50 mV) current mediated by WT GAT1 was measured before and after MTSET labeling (1 mM for 5 min) at different membrane potential values (a), extracellular pH values (b) and experimental temperatures (c). In all experiments, labeling was carried out in NaCl buffer. Labeling was performed at the indicated membrane potential values for the experiments of a and at −50 mV for the experiments of (b) and (c). Labeling was performed at pH 7.4 for the experiments of (a) and (c) and at the indicated values for the experiments of (b). Labeling was performed at 21 °C for the experiments of (a) and (b) and at the indicated values for the experiments of (c). The GABA-evoked current after MTSET modification was normalized to that obtained in the same cell before exposure to MTSET. Reported values represent the mean ± SE from three or more oocytes
Fig. 4.
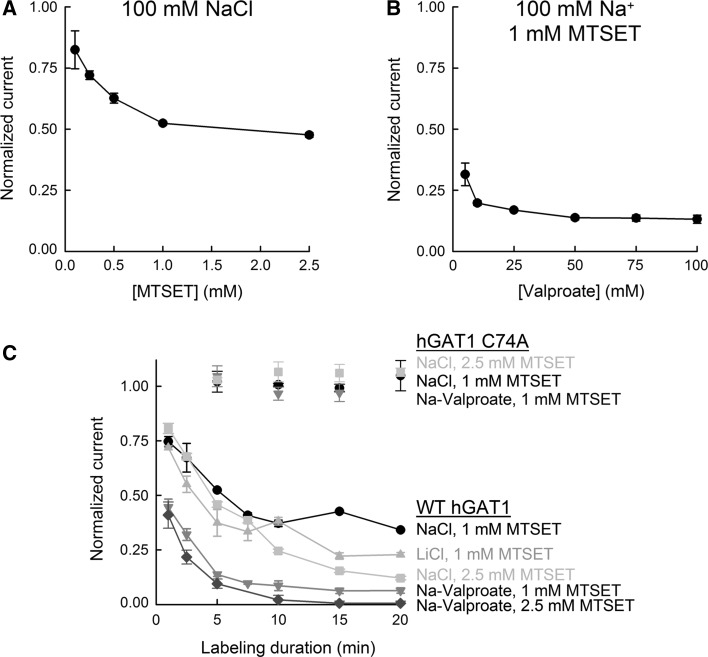
Effect of MTSET concentration and labeling duration on sulfhydryl modification of WT GAT1. a Sulfhydryl modification of WT GAT1 was carried out for 5 min in NaCl buffer in the presence of the indicated concentration of MTSET. b Sulfhydryl modification of WT GAT1 was carried out at 1 mM MTSET for 5 min in the presence of the indicated concentration of valproate. [Na+] = 100 mM. c Duration of labeling with 1 or 2.5 mM MTSET was varied (up to 20 min) in NaCl, LiCl or Na-valproate buffer for WT GAT1 or GAT1 C74A. Note that under all conditions GAT1 C74A was functionally insensitive to MTSET exposure. See text for the second-order rate constants for MTSET labeling of WT GAT1 under different conditions. In all experiments, labeling was carried out at −50 mV. In all experiments, the GABA-evoked (500 μM in NaCl buffer at −50 mV) current after MTSET modification was normalized to that obtained in the same cell before exposure to MTSET. Reported values represent the mean ± SE from three or more oocytes
Fig. 7.
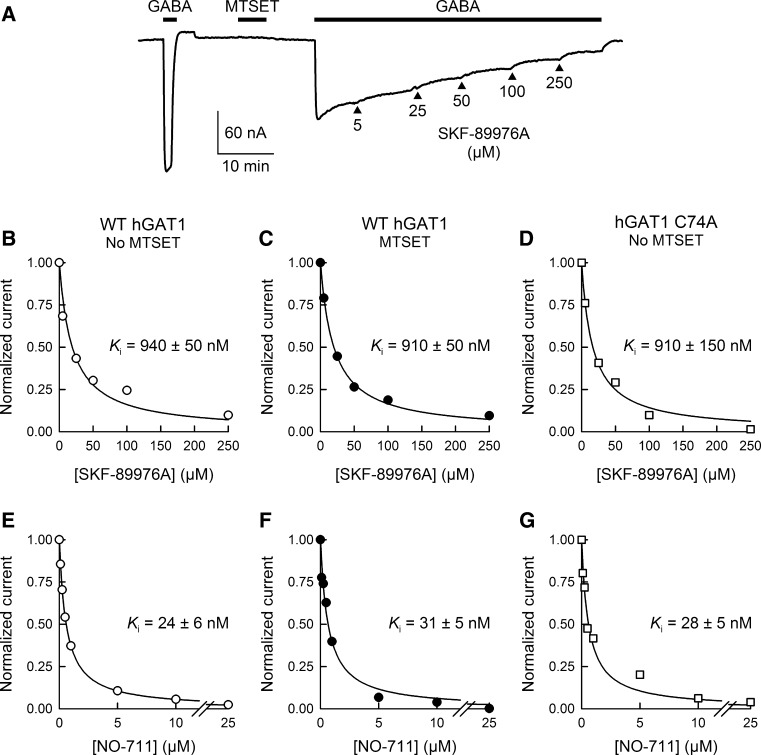
Sulfhydryl modification with MTSET has no effect on WT GAT1 sensitivity to transport inhibitors. a A representative WT GAT1 current trace is shown for inhibition of the GABA-evoked (500 μM at −50 mV) current with SKF-89976A (a specific inhibitor of GAT1) following sulfhydryl modification with MTSET (1 mM for 5 min at −50 mV). Similar to that shown in this panel, inhibition kinetics experiments were performed with SKF-89976A or NO-711 for WT GAT1 without (b, e) or with (c, f) prior exposure to MTSET (1 mM for 5 min at −50 mV) as well as for GAT1 C74A without MTSET treatment (d, g). Sulfhydryl modification of WT GAT1 had no effect on the K i values for SKF-89976A or NO-711. Moreover, the K i values for SKF-89976A (d) and NO-711 (g) inhibition of GAT1 C74A GABA-evoked currents were not different from those of WT GAT1. The smooth lines in (b–g) represent fits of the experimental data with an equation for competitive inhibition at a single binding site (Eq. 4, see “Experimental Procedures” section). Reported K i values represent the mean ± SE from three or more oocytes
Where sample sizes are indicated (n), they refer to the number of oocytes in which the experiments were repeated. Reported errors represent the standard error of the mean obtained from data from several oocytes.
Results
Labeling with the Membrane-Impermeant Sulfhydryl Reagent MTSET Leads to Functional Modification of WT GAT1 but not the Mutant GAT1 C74A
Figure 1 shows the basic experimental approach used to assess the effect of sulfhydryl modification on the GABA-evoked current mediated by GAT1 (
Similar to WT GAT1, GAT1 C74A mediates Na+-dependent and Cl−-facilitated GABA transport (see Fig. 6). Exposure of GAT1 C74A to MTSET (1 mM for 5 min) had no effect on the magnitude of the GABA-evoked current (Fig. 1b, d). This result suggests that C74 is very likely the only functionally significant cysteine residue that is exposed to the extracellular fluid (and hence accessible to the membrane-impermeant MTSET).
The reduction in WT GAT1
The above results suggest that any functional consequence of sulfhydryl modification of WT GAT1 by MTSET very likely occurred at position C74. NEM, a membrane-permeant thiol modification reagent, led to a significant reduction in
As the long-term objective of this project is to utilize extracellularly exposed cysteine residues to label and quantify the number of transporter copies in the plasma membrane, we carried out a complete characterization of labeling WT GAT1 with MTSET with the goal of identifying experimental conditions that drive the labeling reaction to completion (i.e., 100 % labeling of transporter copies in the plasma membrane). Understanding these conditions would then allow us to pursue future labeling and quantification studies.
The Inhibitory Effect of MTSET is Dependent on the Composition of the Labeling Buffer
GABA transport by the GATs is Na+- and Cl−-coupled, and indeed, Na+ and Cl− interaction with the transporter leads to conformational changes (Golovanevsky and Kanner 1999; Lu and Hilgemann 1999b; Li et al. 2000; Zomot and Kanner 2003; Meinild et al. 2009). Therefore, we explored the possibility that the ionic composition of the buffer in which the MTSET exposure takes place can potentially enhance the solvent accessibility of C74, thus increasing the degree of labeling. To accomplish this, we investigated the degree of MTSET labeling when Na+ and/or Cl− was isosmotically replaced with various cations/anions in the labeling buffer, keeping all other labeling conditions constant (1 mM MTSET for 5 min at 21 ± 2 °C, V m = –50 mV, pH 7.4).
Labeling with MTSET in the standard NaCl conditions reduced
Changes in Membrane Potential, pH and Temperature Do Not Alter the Effect of MTSET
GAT activity is also known to be altered by changes in membrane potential (Mager et al. 1993, 1996; Lu and Hilgemann 1999a, b; Gonzales et al. 2007), pH (Grossman and Nelson 2002, 2003) and temperature (Lu and Hilgemann 1999a; Binda et al. 2002; Gonzales et al. 2007; Matthews et al. 2009). Therefore, we examined the influence of these factors on the degree of MTSET labeling of GAT1. In the experiments of Fig. 3, membrane potential (V m), pH and temperature were independently perturbed during the MTSET labeling period, while all other parameters were held constant according to our standard labeling conditions: 1 mM MTSET for 5 min at 21 ± 2 °C, V m = −50 mV and pH 7.4. Interestingly, changes in the membrane potential or pH of the labeling buffer or in temperature had little to no effect on the efficacy of MTSET labeling (Fig. 3). The apparent reduction in MTSET labeling at lower pH values (Fig. 3b) is unlikely to be a direct conformational effect on the transporter (see “Discussion” Section).
MTSET Labeling Conditions for Complete Elimination of GAT1-Mediated GABA Transport
In further pursuit of the optimal experimental conditions under which MTSET labeling of WT GAT1 would approach completion, we examined the effect of MTSET concentration (Fig. 4a) and labeling duration (Fig. 4c) on GAT1-mediated, GABA-evoked current. The concentration dependence of MTSET labeling in NaCl buffer is shown in Fig. 4a. Keeping all other labeling conditions constant, increasing the concentration of MTSET from 1 to 2.5 mM slightly decreased the normalized
Increasing the MTSET incubation time in NaCl buffer to 20 min decreased the GAT1-mediated, GABA-evoked current to 34 ± 1 % at 1 mM MTSET (n = 3) and 12 ± 1 % at 2.5 mM MTSET (n = 3) (Fig. 4c). Similarly, MTSET incubation in LiCl buffer for up to 20 min failed to lead to 100 % elimination of
Importantly,
Thus far, the results demonstrate that sulfhydryl modification of GAT1 at C74 leads to a reduction in the GABA-evoked current (
Fig. 5.
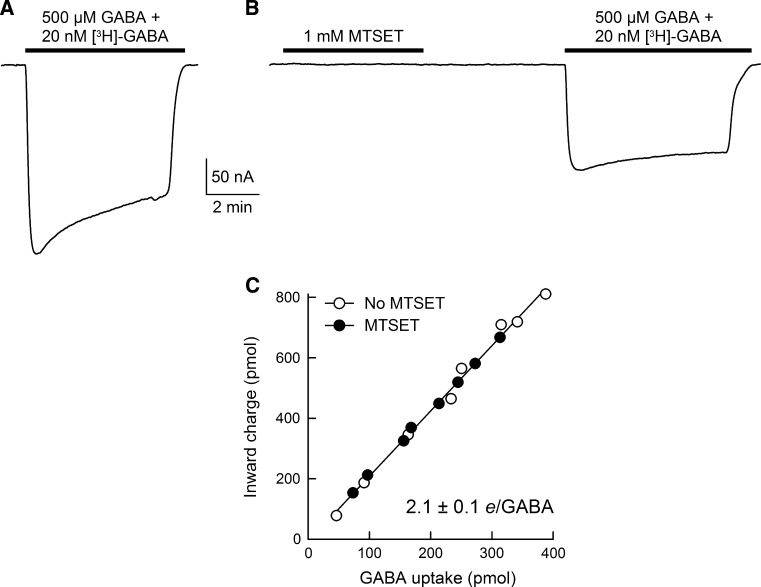
Sulfhydryl modification of WT GAT1 with MTSET does not alter the ion/GABA transport coupling ratio. GABA-uptake experiments were performed under voltage clamp without MTSET treatment (a) or after labeling with 1 mM MTSET for 5 min (b). V m = −50 mV. c Cells expressing GAT1 were exposed to 500 μM GABA and 20 nM [3H]-GABA for 5–10 min. After washout of GABA and isotope, cells were solubilized in 10 % SDS and intracellular GABA content was determined using a liquid scintillation counter. In the same cell, the net inward charge flux was obtained from the time integral of the GABA-evoked current trace. The ratio of charge flux to GABA flux (i.e., net positive charges per GABA, e/GABA) was 2.1 ± 0.1 whether or not the cell was exposed to MTSET (n = 8 and 8). The smooth line in (c) is a linear regression through all data points
Fig. 8.
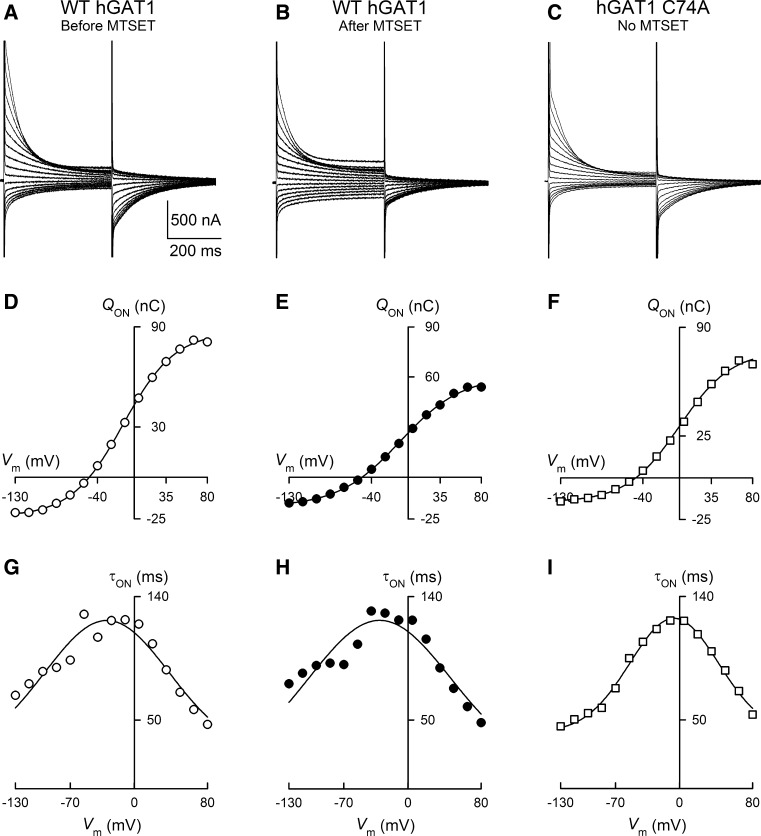
Presteady-state charge movements of WT GAT1 before and after sulfhydryl modification with MTSET. a–c Representative current relaxations are shown in response to 400-ms voltage pulses from +80 to −130 mV for WT GAT1 before (a) and after (b) treatment with MTSET (1 mM for 5 min) as well as for GAT1 C74A without MTSET treatment (c). Holding potential was −50 mV. d–f For each evoked current trace, time integration of the ON presteady-state currents yielded the total charge moved (Q ON) and, when plotted as a function of the test voltage, the Q–V relationship for WT GAT1 before (d) and after (e) labeling with MTSET as well as for GAT1 C74A (f). The smooth lines in (d–f) represent the fit of the data with a Boltzmann function (Eq. 3, see “Experimental Procedures” section). g–i Presteady-state currents monoexponentially decay to the zero level. The time constant plotted as a function of the test voltage yielded the τ–V relationship. The smooth lines in (g–i) represent the fit of the data with a gaussian function (Sacher et al. 2002). While MTSET treatment led to a reduction in the total charge moved (compare d and e), it had no effect on the midpoint of the Q–V relationship (V 0.5) and no effect on the relaxation time constants (compare g and h). The presteady-state parameters of GAT1 C74A were not different from those of WT GAT1. See text for additional details
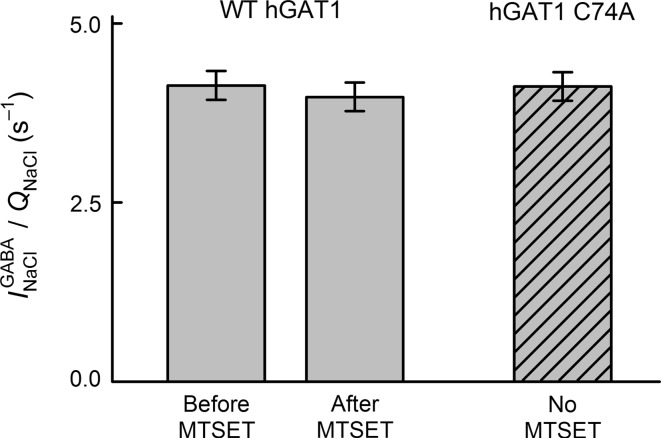
Fig. 9.
Sulfhydryl modification with MTSET has no effect on WT GAT1 turnover rate. The ratio of
Sulfhydryl Modification of GAT1 C74 Does Not Alter GAT1-Mediated Charge/GABA Flux Ratio
Translocation of GABA by GAT1 across the plasma membrane is coupled to cotranslocation of Na+ and Cl− (Radian and Kanner 1983; Keynan and Kanner 1988; Loo et al. 2000), and recent studies suggest that Na+/Cl−/GABA cotransport is a tightly coupled process (Gonzales et al. 2007; Matthews et al. 2009). To examine the possibility that MTSET modification of C74 leads to a change in the ion/GABA coupling ratio of GAT1, we performed GABA uptake under voltage-clamp experiments (Fig. 5). In these experiments, [3H]-GABA uptake was measured under voltage clamp in individual GAT1-expressing cells in the absence of MTSET labeling (Fig. 5a, c) or after labeling with 1 mM MTSET for 5 min (at 21 ± 2 °C, V m = –50 mV and pH 7.4) (Fig. 5b, c). This experimental protocol yielded two measured parameters for each cell: (1) net GABA-evoked inward charge translocation during the recording period (charge flux) and (2) GABA uptake in the same cell (GABA flux) (Fig. 5c). The ratio of charge flux to GABA flux was 2.1 ± 0.1 whether or not the cell was exposed to MTSET (Fig. 5c).
Sulfhydryl Modification of GAT1 C74 Does Not Alter Transporter Steady-State or Presteady-State Kinetic Parameters
To determine if MTSET modification of GAT1 C74 alters the transporter steady-state kinetic properties, we performed steady-state kinetic experiments for GABA, Na+ and Cl− in WT GAT1 before and after labeling with MTSET (1 mM for 5 min in NaCl buffer) (Fig. 6). The results of these experiments show that the apparent affinity constants for GABA (26 ± 3 vs. 22 ± 4 μM, Fig. 6a, b), Na+ (66 ± 10 vs. 72 ± 7 mM, Fig. 6d, e) and Cl− (42 ± 6 vs. 38 ± 5 mM, Fig. 6g, h) were not significantly different before and after partial labeling with 1 mM MTSET for 5 min. Moreover, the Hill coefficient for Na+ activation of the currents was the same before and after sulfhydryl modification of C74 (Fig. 6d, e). The apparent affinity constants of the mutant GAT1 C74A for GABA (22 ± 4 μM, Fig. 6c), Na+ (75 ± 10 mM, Fig. 6f) and Cl− (40 ± 4 mM, Fig. 6i) were not significantly different from those of WT GAT1.
To further characterize the behavior of WT GAT1 after partial labeling with 1 mM MTSET for 5 min, we investigated the sensitivity of WT GAT1 to known transporter inhibitors before and after sulfhydryl modification (Fig. 7). The apparent half-inhibition constant values for SKF-89976A (940 ± 50 vs. 910 ± 50 nM, Fig. 7b, c) and NO-711 (24 ± 6 vs. 31 ± 5 nM, Fig. 7e, f) were not significantly different before and after sulfhydryl labeling with MTSET. Moreover, the apparent half-inhibition constant values of GAT1 C74A for SKF-89976A (910 ± 150 nM, Fig. 7d) and NO-711 (28 ± 5 nM, Fig. 7g) were similar to those of WT GAT1.
To examine the effect of MTSET labeling on WT GAT1 voltage-evoked presteady-state currents, 400-ms voltage pulses were applied, from a holding voltage of −50 mV to test voltages ranging from +80 to −130 mV in 15-mV steps, before (Fig. 8a) and after (Fig. 8b) labeling with 1 mM MTSET for 5 min. At each voltage, the evoked current transient was analyzed to obtain the GAT1-mediated charge moved (see “Experimental Procedures” Section), and the resulting presteady-state charge was plotted as a function of the test voltage to obtain the Q–V relationships (Fig. 8d, e). After labeling WT GAT1 with 1 mM MTSET for 5 min, Q
NaCl was reduced to 60 ± 8 % (n = 4) of that prior to MTSET treatment (compare Fig. 8d, e), suggesting a similar degree of loss of function as that seen with steady-state GABA-evoked current (
Sulfhydryl Modification of GAT1 C74 Does Not Alter Transporter Turnover Rate
Turnover rate is the rate at which ion/GABA molecules are cotranslocated across the plasma membrane per unit time. In a comprehensive characterization, the GAT1 turnover rate was determined to be 15 GABA molecules per second at 21 °C, −50 mV and physiological ion concentrations (Gonzales et al. 2007). When extrapolated to the physiological temperature of 37 °C, the turnover rate was estimated to be 79 s−1 (Gonzales et al. 2007). An important prerequisite to characterizing the turnover rate is the ratio of the maximum GABA-evoked current (
The ratio of
Discussion
In anticipation of utilizing extracellularly oriented, solvent-exposed cysteine residues of GAT1 for labeling and quantifying the transporter in the plasma membrane, the primary objective of this study was to characterize the functional consequences of sulfhydryl modification of GAT1 with the membrane-impermeant sulfhydryl reagent MTSET. Our results show that exposure of the extracellular surface of WT GAT1 to MTSET resulted in a significant and proportional, yet reversible, decrease in both the steady-state GABA-evoked current as well as the presteady-state charge movements. Labeling proved to be insensitive to changes in membrane potential, temperature and pH. Labeling was relatively insensitive to changes in Na+ and/or Cl− concentration when Na+ was replaced with cations such as choline or tetraethylammonium or when Cl− was replaced with anions such as gluconate or MES. However, substitution of Cl− with valproate significantly increased the rate of labeling with MTSET, driving it to completion and leading to a complete loss of transporter function.
GAT1 contains 14 cysteine residues, of which only three (C74, C164, C173) are predicted to be exposed to the extracellular fluid. C74 is in the first transmembrane domain near the membrane/extracellular fluid interface. C164 and C173 are located in the extracellular loop connecting transmembrane domains 3 and 4, and there is evidence that these as well as homologous residues of the related serotonin and dopamine transporters form a disulfide bridge under most conditions (Chen et al. 1997, 2007). Site-directed mutagenesis revealed that the site of covalent sulfhydryl modification of GAT1 is most likely the cysteine at position 74. Our data cannot rule out the possibility that the functional consequence of labeling is due to modification of a cysteine residue other than C74, whose accessibility is altered in the mutant C74A. However, considering the totality of our data set (insensitivity of C74A to MTSET and virtually identical steady-state state and presteady-state kinetic properties of WT and GAT1 C74A), it is plausible to conclude that C74 is very likely the only functionally sensitive cysteine residue that is labeled by MTSET. Extensive functional characterization suggested that GAT1 C74 is only partially accessible from the extracellular fluid. However, once covalently modified with MTSET, GAT1 is incapable of undergoing the conformational changes necessary for presteady-state transients or Na+/Cl−/GABA cotranslocation across the plasma membrane.
Our first goal was to optimize the experimental conditions under which all GAT1 copies in the plasma membrane could be rapidly labeled with MTSET, while maintaining cellular and plasma membrane integrity such that accurate biophysical measurements could be carried out. Initial time and concentration dependence of MTSET labeling of GAT1 demonstrated that, under most labeling conditions, very long incubation times at high MTSET concentrations are required to approach complete labeling of all transporter copies in the plasma membrane. This observation is not consistent with the very high intrinsic reactivity of methanethiosulfonate reagents toward free thiol groups (Karlin and Akabas 1998) and suggests that C74 is only partially exposed to the extracellular fluid, such that accessibility of this site to MTSET is restricted (Yu et al. 1998). Indeed, sequence alignments of GAT1 with the related bacterial leucine transporter (LeuTAa) and other members of the SLC6A family of transporters, as well as homology models of GAT1 built using the high-resolution structure of LeuTAa as a template, strongly suggest that C74 is in the first transmembrane domain near the membrane–extracellular fluid interface and is partially buried in the membrane (Yamashita et al. 2005; Beuming et al. 2006; Livesay et al. 2007). As a practical matter, the relatively short half-life of MTSET in physiological buffers (~10 min) also necessitates the use of experimental conditions that can achieve faster labeling of GAT1.
As GAT1-mediated GABA transport is Na+- and Cl−-coupled, we investigated the degree of MTSET labeling when Na+ or Cl− was isosmotically replaced with various cations/anions in the labeling buffer. It is well established that Na+ and/or Cl− binding events to GAT1 cause transporter conformational changes (Mager et al. 1993, 1996; Golovanevsky and Kanner 1999; Lu and Hilgemann 1999b; Li et al. 2000; Bicho and Grewer 2005; Karakossian et al. 2005; Meinild et al. 2009). We reasoned that conformational changes induced by Na+ and/or Cl− binding may alter the accessibility of C74 to the extracellular space and that, therefore, it was plausible to examine the degree of labeling in buffers that lacked either one or both of these cosubstrates. For most ion replacement conditions tested, only a modest enhancement was observed in the ability of MTSET to label GAT1, as judged by the reduction in the GABA-evoked current (see Fig. 2). Two notable exceptions were replacement of Na+ with Li+ and replacement of Cl− with valproate.
Consistent with previous reports on GAT1 and the serotonin transporter (SERT), we observed a substantial reduction in transport activity following MTSET labeling when Li+ replaced Na+ in the labeling buffer (Figs. 2, 4) (Ni et al. 2001; Meinild et al. 2009). In SERT, the increased accessibility of C109 (homologous with GAT1 C74) is due to Li+ binding rather than the absence of Na+ (Ni et al. 2001), and this is consistent with our findings in GAT1 (Fig. 2). In GAT1, Li+ by itself is not capable of driving Li+/Cl−/GABA cotransport as the Li+-bound transporter conformation is distinct from the Na+-bound conformation (Meinild et al. 2009). However, in the presence of low concentrations of Na+, Li+ can substitute for Na+ at one of the cation-binding sites, allowing for Li+/Na+/Cl−/GABA cotransport (MacAulay et al. 2002; Meinild and Forster 2012). Thus, in the presence of Li+ (Na+ absent) GAT1 assumes a distinct conformation with increased accessibility of C74 to the extracellular fluid.
Remarkably, the most significant environmental condition which favored GAT1 labeling by MTSET was when Cl− was replaced with valproate (Figs. 2, 4). Valproate increases the turnover rate of the GATs via an allosteric mechanism that involves increasing the rate of Na+ binding to the transporter, the transition that is thought to be the rate-limiting step in the transport cycle (Whitlow et al. 2003; Soragna et al. 2005). Our data show that in the presence of valproate complete MTSET labeling of GAT1 can be accomplished within 10 min (Fig. 4c) and suggest that any future attempts to utilize C74 to label GAT1 in the plasma membrane should use valproate as the major anion in the labeling buffer.
Interestingly, the presence of GABA protected GAT1 from MTSET labeling (Fig. 2) (Zhou et al. 2004). This suggests that during the normal translocation cycle (i.e., Na+/Cl−/GABA cotranslocation) there is a reduction in the probability (i.e., time) that C74 is exposed to the extracellular fluid and, hence, accessible to covalent modification by MTSET.
We found it surprising that the accessibility of GAT1 C74 to the extracellular fluid and, hence, MTSET was not altered by changes in experimental conditions such as membrane potential, temperature or pH. GAT1 function is highly voltage-dependent, and indeed, voltage-clamp fluorometric measurements have provided strong evidence for conformational changes evoked by voltage jumps (Li et al. 2000; Meinild et al. 2009). Moreover, the rates of both GAT1 steady-state and presteady-state kinetic properties are very temperature-dependent (Binda et al. 2002; Gonzales et al. 2007). Finally, changes in the extracellular pH have been reported to alter GAT1 function (Grossman and Nelson 2002, 2003). Nonetheless, none of these conditions appeared to play a significant role in the ability of MTSET to label GAT1, suggesting that the global conformational changes caused by these factors do not lead to a change in the accessibility of C74 to the extracellular fluid. When labeling was performed at pH 5.0, there appeared to be a decrease in the efficacy of MTSET; however, this was very likely due to the significantly decreased fraction of GAT1 C74 in the deprotonated thiol form—the form that can nucleophilically attack and, thus, react with MTSET. With a pK a of ~8.37, only 0.04 % of C74 thiol groups are predicted to be in the deprotonated form at pH 5.0 (vs. 9.7 and 19.0 % at pH 7.4 and 9.0, respectively). Indeed, there appeared to be a correlation between the fraction of C74 in the deprotonated form and loss of transporter function following MTSET treatment (13, 47 and 56 % at pH 5.0, 7.4 and 9.0, respectively) (see Fig. 3 for raw data).
Having found improved experimental conditions for sulfhydryl modification of GAT1 C74 with MTSET (i.e., labeling in the presence of valproate), we wished to understand the mechanism by which MTSET labeling of GAT1 C74 leads to a reduction in the GABA-evoked current (
The results of uptake under voltage-clamp experiments suggest that the current that remains after MTSET sulfhydryl modification of GAT1 has the same ion/GABA flux coupling ratio as that mediated by untreated GAT1: two net positive charges for every GABA molecule translocated across the plasma membrane (Fig. 5). GAT1 exhibits tight coupling of charge flux and GABA flux under a variety of experimental conditions, which suggests a fixed ion/substrate transport stoichiometry (Gonzales et al. 2007; Matthews et al. 2009). Therefore, if labeling with MTSET alters the transport stoichiometry, the ratio of charge flux to GABA flux should shift from the known value of 2. Our results do not support this possibility. Thus, after MTSET treatment, the GABA-evoked current is mediated by transporters that operate with a normal Na+/Cl−/GABA coupling stoichiometry.
After MTSET treatment, the remaining GABA-evoked current had the same steady-state and presteady-state kinetic parameters, as well as pharmacological properties, as those of untreated GAT1 (Figs. 6, 7, 8). Thus, a reduction in the apparent affinity of the cosubstrates cannot account for the observed reduction in
After MTSET treatment, the GATs that contribute to the observed macroscopic signal have the same turnover rate as that of untreated GAT1 (Fig. 9). While the exact turnover rate of the GATs and, in fact, most electrogenic Na+-coupled transporters has been elusive due to technical limitations (Gonzales et al. 2007), we have at our disposal a simple measurement that provides an index of the transporter turnover rate. The ratio of the maximum steady-state GABA-evoked current (I max) to the maximum presteady-state charge moved in response to voltage pulses (Q NaCl or Q max) correlates with the transporter turnover rate (Loo et al. 1993; Mager et al. 1993; Eskandari et al. 1997; Sacher et al. 2002; Whitlow et al. 2003; Karakossian et al. 2005; Gonzales et al. 2007). These two parameters are independently measured in individual GAT1-expressing cells, and each is directly related to the total number of functional transporters in the plasma membrane (Zampighi et al. 1995; Eskandari et al. 1997, 1998; Gonzales et al. 2007). Our results demonstrated that, while both I max and Q max are reduced after labeling (see Figs. 1 and 8), the ratio of I max to Q max was not altered following MTSET labeling (Fig. 9), suggesting that both parameters were reduced proportionally and that the transporter population that gives rise to these measurements operates with the same turnover rate.
All in all, our data suggest that the observed current following partial labeling with MTSET is mediated by an unlabeled transporter population that operates normally. Transmembrane domain 1 is thought to play a prominent role in GAT1 function by lining the permeation pathway and containing determinants for substrate specificity (Mager et al. 1996; Zhou et al. 2004; Yamashita et al. 2005). It is highly unlikely that the bulky, positively charged MTSET, covalently bonded to C74 at the extracellular end of transmembrane domain 1, does not alter the transport stoichiometry or any of the relevant steady-state, presteady-state or inhibition kinetic parameters of GAT1. It is more likely that the observed GABA-evoked current following MTSET exposure is mediated by transporters that were simply never labeled. We conclude that MTSET labels GAT1 at C74 and that such covalent sulfhydryl modification renders that transporter completely nonfunctional and electrically silent.
At this time, it is difficult to reconcile our data with those reported previously using the voltage-clamp fluorometry method (Li et al. 2000; Meinild et al. 2009). The totality of our data suggests that labeling C74 with MTSET renders the transporter nonfunctional as all known electrical signals of GAT1 are abolished after labeling. These signals include the GABA-evoked steady-state current as well as voltage-evoked presteady-state charge movements. Thus, at first glance, it appears that a fluorophore-conjugated C74 is not a suitable experimental model by which to examine transporter conformational changes that are relevant to those operating during the normal transport cycle. However, previous measurements obtained with the voltage-clamp fluorometry method suggest that GAT1 conjugated (reportedly at C74) with TMR6M exhibits voltage-induced changes in fluorescence intensity and that the time course of these transitions corresponds well to the relaxation time constants of the presteady-state charge movements. Our data show that TMR6M is capable of labeling both WT GAT1 and the mutant GAT1 C74A (see Fig. 1d), suggesting that, in addition to C74, this agent labels other cysteine residues, possibly those buried in the membrane or even exposed to the cytoplasmic space. Clearly, additional studies are needed to better understand the electrophysiological and fluorescence signals following GAT1 labeling with TMR6M. A challenge with selecting suitable fluorescent probes is that their lipid solubility coefficients are generally not known or cannot be estimated (for proprietary molecules). We propose that the simple assay shown here on GAT1 C74A may be performed in order to assess the ability of the fluorophore to cross the plasma membrane and, hence, gain access to internally exposed cysteine residues.
A sequence alignment for members of the neurotransmitter/Na+ symporter family (NSS) reveals that the cysteine at position 74 of GAT1 is conserved in most of the mammalian members of the family. However, each family member is predicted to have different numbers of extracellularly oriented cysteine residues, making it difficult to utilize a single residue for labeling purposes without engineering cysteine mutants against a cysteine-less background. Moreover, very different observations have been reported regarding the functional consequence of labeling with the membrane-impermeant MTSET. For example, WT dopamine and norepinephrine transporters appear to be insensitive to functional modification by extracellularly applied MTSET (Sucic and Bryan-Lluka 2005). The SERT exhibits significant functional sensitivity to MTSET only when Li+ is the major extracellular cation, and this effect is abolished in the C109A mutant, where SERT C109 is homologous to GAT1 C74 (Chen et al. 1997; Ni et al. 2001; Sucic and Bryan-Lluka 2005). In the glycine transporter (GlyT1b), MTSET leads to a reduction in both steady-state and voltage-evoked presteady-state currents, and this effect is eliminated in the corresponding cysteine-to-alanine mutant (Roux et al. 2001). The basic observations presented here on sulfhydryl modification of GAT1 with MTSET are similar to those reported for the glycine transporter GlyT1b (Roux et al. 2001).
Acknowledgements
We thank Jessica Martinez for technical assistance. This work was supported by a U.S. National Institute of General Medical Sciences grant awarded to S. E. (SC1GM086344).
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
References
- Anderson CM, Kidd PD, Eskandari S. GATMD: γ-aminobutyric acid transporter mutagenesis database. Database (Oxford) 2010;2010:baq028. doi: 10.1093/database/baq028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Yona A, Kanner BI. Transmembrane domain 8 of the γ-aminobutyric acid transporter GAT-1 lines a cytoplasmic accessibility pathway into its binding pocket. J Biol Chem. 2009;284:9727–9732. doi: 10.1074/jbc.M809423200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett ER, Kanner BI. The membrane topology of GAT-1, a (Na+ + Cl−)-coupled γ-aminobutyric acid transporter from rat brain. J Biol Chem. 1997;272:1203–1210. doi: 10.1074/jbc.272.2.1203. [DOI] [PubMed] [Google Scholar]
- Beuming T, Shi L, Javitch JA, Weinstein H. A comprehensive structure-based alignment of prokaryotic and eukaryotic neurotransmitter/Na+ symporters (NSS) aids in the use of the LeuT structure to probe NSS structure and function. Mol Pharmacol. 2006;70:1630–1642. doi: 10.1124/mol.106.026120. [DOI] [PubMed] [Google Scholar]
- Bicho A, Grewer C. Rapid substrate-induced charge movements of the GABA transporter GAT1. Biophys J. 2005;89:211–231. doi: 10.1529/biophysj.105.061002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binda F, Bossi E, Giovannardi S, Forlani G, Peres A. Temperature effects on the presteady-state and transport-associated currents of GABA cotransporter rGAT1. FEBS Lett. 2002;512:303–307. doi: 10.1016/S0014-5793(02)02271-8. [DOI] [PubMed] [Google Scholar]
- Blakely RD, Berson HE, Fremeau RT, Jr, Caron MG, Peek MM, Prince HK, Bradley CC. Cloning and expression of a functional serotonin transporter from rat brain. Nature. 1991;354:66–70. doi: 10.1038/354066a0. [DOI] [PubMed] [Google Scholar]
- Borden LA. GABA transporter heterogeneity: pharmacology and cellular localization. Neurochem Int. 1996;29:335–356. doi: 10.1016/0197-0186(95)00158-1. [DOI] [PubMed] [Google Scholar]
- Busch W, Saier MH., Jr The transporter classification (TC) system, 2002. Crit Rev Biochem Mol Biol. 2002;37:287–337. doi: 10.1080/10409230290771528. [DOI] [PubMed] [Google Scholar]
- Chen JG, Liu-Chen S, Rudnick G. External cysteine residues in the serotonin transporter. Biochemistry. 1997;36:1479–1486. doi: 10.1021/bi962256g. [DOI] [PubMed] [Google Scholar]
- Chen NH, Reith ME, Quick MW. Synaptic uptake and beyond: the sodium- and chloride-dependent neurotransmitter transporter family SLC6. Pflugers Arch. 2004;447:519–531. doi: 10.1007/s00424-003-1064-5. [DOI] [PubMed] [Google Scholar]
- Chen R, Wei H, Hill ER, Chen L, Jiang L, Han DD, Gu HH. Direct evidence that two cysteines in the dopamine transporter form a disulfide bond. Mol Cell Biochem. 2007;298:41–48. doi: 10.1007/s11010-006-9348-7. [DOI] [PubMed] [Google Scholar]
- Conti F, Minelli A, Melone M. GABA transporters in the mammalian cerebral cortex: localization, development and pathological implications. Brain Res Brain Res Rev. 2004;45:196–212. doi: 10.1016/j.brainresrev.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Dalby NO. Inhibition of γ-aminobutyric acid uptake: anatomy, physiology and effects against epileptic seizures. Eur J Pharmacol. 2003;479:127–137. doi: 10.1016/j.ejphar.2003.08.063. [DOI] [PubMed] [Google Scholar]
- Eskandari S, Loo DD, Dai G, Levy O, Wright EM, Carrasco N. Thyroid Na+/I− symporter. Mechanism, stoichiometry, and specificity. J Biol Chem. 1997;272:27230–27238. doi: 10.1074/jbc.272.43.27230. [DOI] [PubMed] [Google Scholar]
- Eskandari S, Wright EM, Kreman M, Starace DM, Zampighi GA. Structural analysis of cloned plasma membrane proteins by freeze-fracture electron microscopy. Proc Natl Acad Sci USA. 1998;95:11235–11240. doi: 10.1073/pnas.95.19.11235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forster IC, Loo DD, Eskandari S. Stoichiometry and Na+ binding cooperativity of rat and flounder renal type II Na+-Pi cotransporters. Am J Physiol Renal Physiol. 1999;276:F644–F649. doi: 10.1152/ajprenal.1999.276.4.F644. [DOI] [PubMed] [Google Scholar]
- Frillingos S, Sahin-Tóth M, Wu J, Kaback HR. Cys-scanning mutagenesis: a novel approach to structure function relationships in polytopic membrane proteins. FASEB J. 1998;12:1281–1299. doi: 10.1096/fasebj.12.13.1281. [DOI] [PubMed] [Google Scholar]
- Golovanevsky V, Kanner BI. The reactivity of the γ-aminobutyric acid transporter GAT-1 toward sulfhydryl reagents is conformationally sensitive. Identification of a major target residue. J Biol Chem. 1999;274:23020–23026. doi: 10.1074/jbc.274.33.23020. [DOI] [PubMed] [Google Scholar]
- Gonzales AL, Lee W, Spencer SR, Oropeza RA, Chapman JV, Ku JY, Eskandari S. Turnover rate of the γ-aminobutyric acid transporter GAT1. J Membr Biol. 2007;220:33–51. doi: 10.1007/s00232-007-9073-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman TR, Nelson N. Differential effect of pH on sodium binding by the various GABA transporters expressed in Xenopus oocytes. FEBS Lett. 2002;527:125–132. doi: 10.1016/S0014-5793(02)03194-0. [DOI] [PubMed] [Google Scholar]
- Grossman TR, Nelson N. Effect of sodium lithium and proton concentrations on the electrophysiological properties of the four mouse GABA transporters expressed in Xenopus oocytes. Neurochem Int. 2003;43:431–443. doi: 10.1016/S0197-0186(03)00032-9. [DOI] [PubMed] [Google Scholar]
- Guan L, Kaback HR. Site-directed alkylation of cysteine to test solvent accessibility of membrane proteins. Nat Protoc. 2007;2:2012–2017. doi: 10.1038/nprot.2007.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guastella J, Nelson N, Nelson H, Czyzyk L, Keynan S, Miedel MC, Davidson N, Lester HA, Kanner BI. Cloning and expression of a rat brain GABA transporter. Science. 1990;249:1303–1306. doi: 10.1126/science.1975955. [DOI] [PubMed] [Google Scholar]
- Guastella J, Brecha N, Weigmann C, Lester HA, Davidson N. Cloning, expression, and localization of a rat brain high-affinity glycine transporter. Proc Natl Acad Sci USA. 1992;89:7189–7193. doi: 10.1073/pnas.89.15.7189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazama A, Loo DD, Wright EM. Presteady-state currents of the rabbit Na+/glucose cotransporter (SGLT1) J Membr Biol. 1997;155:175–186. doi: 10.1007/s002329900169. [DOI] [PubMed] [Google Scholar]
- Hoffman BJ, Mezey E, Brownstein MJ. Cloning of a serotonin transporter affected by antidepressants. Science. 1991;254:579–580. doi: 10.1126/science.1948036. [DOI] [PubMed] [Google Scholar]
- Kanner BI. Transmembrane domain I of the γ-aminobutyric acid transporter GAT-1 plays a crucial role in the transition between cation leak and transport modes. J Biol Chem. 2003;278:3705–3712. doi: 10.1074/jbc.M210525200. [DOI] [PubMed] [Google Scholar]
- Karakossian MH, Spencer SR, Gomez AQ, Padilla OR, Sacher A, Loo DD, Nelson N, Eskandari S. Novel properties of a mouse γ-aminobutyric acid transporter (GAT4) J Membr Biol. 2005;203:65–82. doi: 10.1007/s00232-004-0732-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlin A, Akabas MH. Substituted-cysteine accessibility method. Meth Enzymol. 1998;293:123–145. doi: 10.1016/S0076-6879(98)93011-7. [DOI] [PubMed] [Google Scholar]
- Keynan S, Kanner BI. γ-Aminobutyric acid transport in reconstituted preparations from rat brain: coupled sodium and chloride fluxes. Biochemistry. 1988;27:12–17. doi: 10.1021/bi00401a003. [DOI] [PubMed] [Google Scholar]
- Kilty JE, Lorang D, Amara SG. Cloning and expression of a cocaine-sensitive rat dopamine transporter. Science. 1991;254:578–579. doi: 10.1126/science.1948035. [DOI] [PubMed] [Google Scholar]
- Krause S, Schwarz W. Identification and selective inhibition of the channel mode of the neuronal GABA transporter 1. Mol Pharmacol. 2005;68:1728–1735. doi: 10.1124/mol.105.013870. [DOI] [PubMed] [Google Scholar]
- Li M, Farley RA, Lester HA. An intermediate state of the γ-aminobutyric acid transporter GAT1 revealed by simultaneous voltage clamp and fluorescence. J Gen Physiol. 2000;115:491–508. doi: 10.1085/jgp.115.4.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu QR, Nelson H, Mandiyan S, López-Corcuera B, Nelson N. Cloning and expression of a glycine transporter from mouse brain. FEBS Lett. 1992;305:110–114. doi: 10.1016/0014-5793(92)80875-H. [DOI] [PubMed] [Google Scholar]
- Livesay DR, Kidd PD, Eskandari S, Roshan U. Assessing the ability of sequence-based methods to provide functional insight within membrane integral proteins: a case study analyzing the neurotransmitter/Na+ symporter family. BMC Bioinformatics. 2007;8:397. doi: 10.1186/1471-2105-8-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loo DD, Hazama A, Supplisson S, Turk E, Wright EM. Relaxation kinetics of the Na+/glucose cotransporter. Proc Natl Acad Sci USA. 1993;90:5767–5771. doi: 10.1073/pnas.90.12.5767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loo DD, Eskandari S, Boorer KJ, Sarkar HK, Wright EM. Role of Cl− in electrogenic Na+-coupled cotransporters GAT1 and SGLT1. J Biol Chem. 2000;275:37414–37422. doi: 10.1074/jbc.M007241200. [DOI] [PubMed] [Google Scholar]
- Lu CC, Hilgemann DW. GAT1 (GABA:Na+:Cl−) cotransport function. Steady state studies in giant Xenopus oocyte membrane patches. J Gen Physiol. 1999;114:429–444. doi: 10.1085/jgp.114.3.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu CC, Hilgemann DW. GAT1 (GABA:Na+:Cl−) cotransport function. Kinetic studies in giant Xenopus oocyte membrane patches. J Gen Physiol. 1999;114:445–457. doi: 10.1085/jgp.114.3.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacAulay N, Zeuthen T, Gether U. Conformational basis for the Li+-induced leak current in the rat γ-aminobutyric acid (GABA) transporter-1. J Physiol. 2002;544:447–458. doi: 10.1113/jphysiol.2002.022897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madsen KK, White HS, Schousboe A. Neuronal and non-neuronal GABA transporters as targets for antiepileptic drugs. Pharmacol Ther. 2010;125:394–401. doi: 10.1016/j.pharmthera.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Mager S, Naeve J, Quick M, Labarca C, Davidson N, Lester HA. Steady states, charge movements, and rates for a cloned GABA transporter expressed in Xenopus oocytes. Neuron. 1993;10:177–188. doi: 10.1016/0896-6273(93)90309-F. [DOI] [PubMed] [Google Scholar]
- Mager S, Kleinberger-Doron N, Keshet GI, Davidson N, Kanner BI, Lester HA. Ion binding and permeation at the GABA transporter GAT1. J Neurosci. 1996;16:5405–5414. doi: 10.1523/JNEUROSCI.16-17-05405.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mari SA, Soragna A, Castagna M, Santacroce M, Perego C, Bossi E, Peres A, Sacchi VF. Role of the conserved glutamine 291 in the rat γ-aminobutyric acid transporter rGAT-1. Cell Mol Life Sci. 2006;63:100–111. doi: 10.1007/s00018-005-5512-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews E, Jr, Rahnama-Vaghef A, Eskandari S. Inhibitors of the γ-aminobutyric acid transporter 1 (GAT1) do not reveal a channel mode of conduction. Neurochem Int. 2009;55:732–740. doi: 10.1016/j.neuint.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinild AK, Forster IC. Using lithium to probe sequential cation interactions with GAT1. Am J Physiol Cell Physiol. 2012;302:C1661–C1675. doi: 10.1152/ajpcell.00446.2011. [DOI] [PubMed] [Google Scholar]
- Meinild AK, Loo DD, Skovstrup S, Gether U, Macaulay N. Elucidating conformational changes in the γ-aminobutyric acid transporter-1. J Biol Chem. 2009;284:16226–16235. doi: 10.1074/jbc.M109.003137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson H, Mandiyan S, Nelson N. Cloning of the human brain GABA transporter. FEBS Lett. 1990;269:181–184. doi: 10.1016/0014-5793(90)81149-I. [DOI] [PubMed] [Google Scholar]
- Nelson N. The family of Na+/Cl− neurotransmitter transporters. J Neurochem. 1998;71:1785–1803. doi: 10.1046/j.1471-4159.1998.71051785.x. [DOI] [PubMed] [Google Scholar]
- Ni YG, Chen JG, Androutsellis-Theotokis A, Huang CJ, Moczydlowski E, Rudnick G. A lithium-induced conformational change in serotonin transporter alters cocaine binding, ion conductance, and reactivity of Cys-109. J Biol Chem. 2001;276:30942–30947. doi: 10.1074/jbc.M104653200. [DOI] [PubMed] [Google Scholar]
- Pacholczyk T, Blakely RD, Amara SG. Expression cloning of a cocaine- and antidepressant-sensitive human noradrenaline transporter. Nature. 1991;350:350–354. doi: 10.1038/350350a0. [DOI] [PubMed] [Google Scholar]
- Radian R, Kanner BI. Stoichiometry of sodium- and chloride-coupled γ-aminobutyric acid transport by synaptic plasma membrane vesicles isolated from rat brain. Biochemistry. 1983;22:1236–1241. doi: 10.1021/bi00274a038. [DOI] [PubMed] [Google Scholar]
- Richerson GB, Wu Y. Dynamic equilibrium of neurotransmitter transporters: not just for reuptake anymore. J Neurophysiol. 2003;90:1363–1374. doi: 10.1152/jn.00317.2003. [DOI] [PubMed] [Google Scholar]
- Rosenberg A, Kanner BI. The substrates of the GABA transporter GAT-1 induce structural rearrangements around the interface of transmembrane domains 1 and 6. J Biol Chem. 2008;283:14376–14383. doi: 10.1074/jbc.M801093200. [DOI] [PubMed] [Google Scholar]
- Roux MJ, Martinez-Maza R, Le Goff A, Lopez-Corcuera B, Aragon C, Supplisson S. The glial and the neuronal glycine transporters differ in their reactivity to sulfhydryl reagents. J Biol Chem. 2001;276:17699–17705. doi: 10.1074/jbc.M009196200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudnick G. Serotonin transporters—structure and function. J Membr Biol. 2006;213:101–110. doi: 10.1007/s00232-006-0878-4. [DOI] [PubMed] [Google Scholar]
- Sacher A, Nelson N, Ogi JT, Wright EM, Loo DD, Eskandari S. Presteady-state and steady-state kinetics and turnover rate of the mouse γ-aminobutyric acid transporter (mGAT3) J Membr Biol. 2002;190:57–73. doi: 10.1007/s00232-002-1024-6. [DOI] [PubMed] [Google Scholar]
- Saier MH, Jr, Tran CV, Barabote RD. TCDB: the transporter classification database for membrane transport protein analyses and information. Nucleic Acids Res. 2006;34:D181–D186. doi: 10.1093/nar/gkj001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schousboe A, Madsen KK, White HS. GABA transport inhibitors and seizure protection: the past and future. Future Med Chem. 2011;3:183–187. doi: 10.4155/fmc.10.288. [DOI] [PubMed] [Google Scholar]
- Shimada S, Kitayama S, Lin CL, Patel A, Nanthakumar E, Gregor P, Kuhar M, Uhl G. Cloning and expression of a cocaine-sensitive dopamine transporter complementary DNA. Science. 1991;254:576–578. doi: 10.1126/science.1948034. [DOI] [PubMed] [Google Scholar]
- Soragna A, Bossi E, Giovannardi S, Pisani R, Peres A. Relations between substrate affinities and charge equilibration rates in the rat GABA cotransporter GAT1. J Physiol. 2005;562:333–345. doi: 10.1113/jphysiol.2004.076703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sucic S, Bryan-Lluka LJ. Roles of transmembrane domain 2 and the first intracellular loop in human noradrenaline transporter function: pharmacological and SCAM analysis. J Neurochem. 2005;94:1620–1630. doi: 10.1111/j.1471-4159.2005.03316.x. [DOI] [PubMed] [Google Scholar]
- Usdin TB, Mezey E, Chen C, Brownstein MJ, Hoffman BJ. Cloning of the cocaine-sensitive bovine dopamine transporter. Proc Natl Acad Sci USA. 1991;88:11168–11171. doi: 10.1073/pnas.88.24.11168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlow RD, Sacher A, Loo DD, Nelson N, Eskandari S. The anticonvulsant valproate increases the turnover rate of γ-aminobutyric acid transporters. J Biol Chem. 2003;278:17716–17726. doi: 10.1074/jbc.M207582200. [DOI] [PubMed] [Google Scholar]
- Yamashita A, Singh SK, Kawate T, Jin Y, Gouaux E. Crystal structure of a bacterial homologue of Na+/Cl−-dependent neurotransmitter transporters. Nature. 2005;437:215–223. doi: 10.1038/nature03978. [DOI] [PubMed] [Google Scholar]
- Yu N, Cao Y, Mager S, Lester HA. Topological localization of cysteine 74 in the GABA transporter, GAT1, and its importance in ion binding and permeation. FEBS Lett. 1998;426:174–178. doi: 10.1016/S0014-5793(98)00333-0. [DOI] [PubMed] [Google Scholar]
- Zampighi GA, Kreman M, Boorer KJ, Loo DD, Bezanilla F, Chandy G, Hall JE, Wright EM. A method for determining the unitary functional capacity of cloned channels and transporters expressed in Xenopus laevis oocytes. J Membr Biol. 1995;148:65–78. doi: 10.1007/BF00234157. [DOI] [PubMed] [Google Scholar]
- Zhang H, Karlin A. Identification of acetylcholine receptor channel-lining residues in the M1 segment of the β-subunit. Biochemistry. 1997;36:15856–15864. doi: 10.1021/bi972357u. [DOI] [PubMed] [Google Scholar]
- Zhou Y, Kanner BI. Transporter-associated currents in the γ-aminobutyric acid transporter GAT-1 are conditionally impaired by mutations of a conserved glycine residue. J Biol Chem. 2005;280:20316–20324. doi: 10.1074/jbc.M412937200. [DOI] [PubMed] [Google Scholar]
- Zhou Y, Bennett ER, Kanner BI. The aqueous accessibility in the external half of transmembrane domain I of the GABA transporter GAT-1 is modulated by its ligands. J Biol Chem. 2004;279:13800–13808. doi: 10.1074/jbc.M311579200. [DOI] [PubMed] [Google Scholar]
- Zhou Y, Zomot E, Kanner BI. Identification of a lithium interaction site in the γ-aminobutyric acid (GABA) transporter GAT-1. J Biol Chem. 2006;281:22092–22099. doi: 10.1074/jbc.M602319200. [DOI] [PubMed] [Google Scholar]
- Zomot E, Kanner BI. The interaction of the γ-aminobutyric acid transporter GAT-1 with the neurotransmitter is selectively impaired by sulfhydryl modification of a conformationally sensitive cysteine residue engineered into extracellular loop IV. J Biol Chem. 2003;278:42950–42958. doi: 10.1074/jbc.M209307200. [DOI] [PubMed] [Google Scholar]
- Zomot E, Zhou Y, Kanner BI. Proximity of transmembrane domains 1 and 3 of the γ-aminobutyric acid transporter GAT-1 inferred from paired cysteine mutagenesis. J Biol Chem. 2005;280:25512–25516. doi: 10.1074/jbc.M503864200. [DOI] [PubMed] [Google Scholar]