Abstract
Objective
To better understand associations between managed care penetration in healthcare markets and intensity-modulated radiotherapy (IMRT) adoption.
Methods
We used Surveillance, Epidemiology, and End Results (SEER)-Medicare data to identify men diagnosed with prostate cancer between 2001 and 2007 who were treated with radiation therapy (n=55,162). We categorized managed care penetration in Health Service Areas (HSAs) as low (<3%), intermediate (3–10%), and high (>10%); and assessed our main outcomes (i.e., probability of IMRT adoption, which is the ability of a healthcare market to deliver IMRT, and IMRT utilization in HSA markets) using a Cox proportional-hazards model and Poisson regression model, respectively.
Results
Compared to markets with low managed care penetration, populations in highly penetrated HSAs were more racially diverse (25% vs. 15% non-white, p<0.01), densely populated (2,110 vs. 145 people/square mile, p<0.01), and wealthier (median income $48,500 vs. $31,900, p<0.01). The probability of IMRT adoption was greatest in markets with the highest managed care penetration (e.g., 0.82 (high) vs. 0.72 (low) in 2007, p=0.05). Among adopting markets, the use of IMRT increased in all HSA categories. However, relative to markets with low managed care penetration, IMRT utilization was constrained in markets with the highest penetration (0.69 (high) vs. 0.76 (low) in 2007, p<0.01).
Conclusion
Markets with higher managed care penetration demonstrated a greater propensity for acquiring IMRT technology. However, after adopting IMRT, more highly penetrated markets had roughly 7% slower growth in utilization over the study period. These findings provide insight into the implications of delivery system reforms for cancer-related technologies.
Keywords: intensity-modulated radiotherapy, managed care, health service area
INTRODUCTION
Over the last decade, intensity-modulated radiotherapy (IMRT) has disseminated rapidly and is now the most common form of radiation used for the treatment of prostate cancer.1 Enthusiasm for IMRT stems from its ability to deliver higher doses of radiation to cancer sites, while limiting the exposure of surrounding tissues.2,3 Although IMRT may be associated with more erectile dysfunction compared with its immediate predecessor, 3-dimensional conformal therapy,4 its improved targeting capability offers potential patient benefits, including the reduction of bowel or urinary toxicity4,5 and improve cancer control.6
However, access to IMRT for prostate cancer and its associated benefits may be hindered in certain delivery environments that emphasize cost-containment strategies, such as managed care organizations. The cost of acquiring IMRT equipment can exceed $1.5 million,7 and treating patients with IMRT costs $15,000–$20,000 more per treatment course than surgical or other radiation options.2 Indeed, there are at least two reasons why healthcare markets with high penetrations of managed care might limit the spread of an expensive new technology such as IMRT. First, these organizations tend to empower primary care physicians as gatekeepers8,9 to specialty care in an attempt to reduce unnecessary use of medical specialists. Whether intentional or not, this arrangement has resulted in the preferential migration of specialists to healthcare markets with less managed care.10 Second, managed care organizations establish unique incentives for physicians, such as capitation,11 which may deter the implementation of an expensive technology.12 Because payments for IMRT are higher than for other types of radiation, markets with high penetrations of managed care might continue to favor the less expensive alternative, resulting in slower uptake, even after acquiring the ability to implement the technology.
How managed care penetration influences the adoption of new prostate cancer technologies is important for two reasons. First, the evolution of medical payment systems at the federal level, while still in flux, appears to be headed in the direction of value-based purchasing that links payment directly to the quality of care13 as opposed to traditional fee-for-service. Indeed, managed care’s mission to improve quality while limiting costs is largely shared by accountable care organizations, which are becoming an integral part of current healthcare reform. Second, newer cancer-related technologies in the development pipeline, some of which may be more expensive, will inevitably face similar hurdles to diffusion, although perhaps in an even more cost-conscious environment. For these reasons, we performed a study to better understand the association between the managed care penetration in a healthcare market and the dissemination of IMRT.
MATERIALS and METHODS
Data Sources and Study Population
We used the Surveillance, Epidemiology, and End Results (SEER)-Medicare linked data to identify men aged 66 years or older diagnosed with prostate cancer between 2001 and 2007. This nationally representative population-based registry consists of all incident cancers occurring in these areas, which collectively comprise approximately 26% of the U.S. population.14 Next, we identified men undergoing radiation therapy within the first 12 months of diagnosis using Healthcare Common Procedure Coding System (HCPCS) codes in the outpatient and carrier files.2 Only fee-for-service beneficiaries eligible for both Medicare Parts A and B from 12 months prior to diagnosis until 12 months after diagnosis were included in the study. Men aged 65 years were excluded to ensure accurate comorbidity estimation using Medicare claims for the 12-month period prior to diagnosis.15 Using these criteria, our study population consisted of 55,162 patients treated with radiation therapy for localized prostate cancer.
Identifying Health Care Markets
We divided the SEER registries into healthcare markets using 164 Health Service Area (HSA) boundaries specified by the Area Resource File. Briefly, HSAs were originally defined by the National Center for Health Statistics as a single county or cluster of contiguous counties that are relatively self-contained with respect to hospital care.16 We chose HSAs as opposed to a larger unit of population because radiation treatment for prostate cancer is elective, discretionary, requires daily visits, and hence, is generally delivered locally. We excluded one HSA because no patients from that market received radiation for prostate cancer during the study period.
For each HSA, we characterized its managed care penetration using explicit data in the Area Resource File. As the Area Resource File defines managed care penetration, the numerator is the number of Medicare enrollees in managed care plans and the denominator is the number of eligible Medicare beneficiaries. HSAs were sorted into roughly equal-sized groups with varying levels of managed care penetration: low (<3%), intermediate (3–10%) and high (>10%).
Outcomes
To assess the association of managed care penetration and IMRT dissemination, we first characterized the probability of adopting IMRT (i.e., a healthcare market that acquires the ability to deliver IMRT). To reduce measurement error, a market was considered an adopter if it contained 5 or more patients treated with IMRT within a 12-month period. The time of adoption was backdated to the first claim for IMRT. Because managed care penetration might influence the diffusion of IMRT within an HSA even after it acquires this capability, we next measured utilization among the adopting HSAs (n=128). For this ratio, the numerator was the number of men treated with IMRT and the denominator was the number of men treated with radiation. For both outcomes, the HSA was the unit of analysis.
Statistical Analysis
We first contrasted aggregate patient and HSA population characteristics according to managed care penetration using a chi-square test for categorical variables and a Student’s t-test for continuous variables. Next, we fit a Cox proportional-hazards model to assess the probability of IMRT adoption across the managed care penetration exposure. This model met the proportional-hazards assumptions. Time-to-event was calculated from the beginning of the study period (January 1, 2001) until the first date of an IMRT claim or the end of the observation window (December 31, 2008). Among HSAs that adopted IMRT, we fit a Poisson regression model to measure a market’s utilization of IMRT within a year of adoption. This model was back-transformed to generate the predicted probability of IMRT utilization according to managed care penetration. For both outcomes, models were adjusted for patient characteristics (age, tumor grade and stage, and comorbidity). Comorbidity was measured using established methods for claims data as described by Klabunde.15 In addition, due to potential confounding from HSA-level characteristics, we adjusted for several market characteristics (racial composition, population density, education, income, percent speaking English as a secondary language, number of hospital beds and radiation oncologists in a market, and SEER region). All analyses were performed using SAS v9.2 (Cary, NC). The probability of a type I error was set at 0.05 and all testing was two-sided. The Institutional Review Board of the University of Michigan approved the study protocol.
RESULTS
Patient and HSA-level characteristics according to managed care penetration are shown in Table 1. Clinical characteristics (i.e., age, tumor grade and stage, and comorbidities) were similar across HSAs. Compared to markets with low managed care penetration, markets in highly penetrated HSAs were more racially diverse, more densely populated, more educated, wealthier, and more likely to use English as a secondary language. In addition, highly penetrated markets had fewer hospital beds and more radiation oncologists per capita.
Table 1.
Population characteristics of Health Service Areas according to managed care penetration
| Health Service Area | Managed care penetration | P Value | ||
|---|---|---|---|---|
| Low | Intermediate | High | ||
| No. Health Service Areas | 49 | 69 | 45 | -- |
| No. patients treated with radiation, % | 5,025 | 25,048 | 25,089 | -- |
| Patient Characteristics | ||||
| Mean patient age, years | 73.4 | 73.4 | 73.8 | 0.05 |
| Well/moderately differentiated tumor grade, % | 55 | 55 | 55 | 0.97 |
| Tumor stage T1, % | 40 | 45 | 42 | 0.15 |
| Charlson Score 2 or higher, % | 11 | 13 | 10 | 0.05 |
| Market Characteristics | ||||
| Non-white population, % | 15 | 16 | 25 | <0.01 |
| Population density, (people per square mile) | 145 | 710 | 2,110 | <0.01 |
| At least college education, % | 15 | 18 | 27 | <0.01 |
| Median income, $ | 31,900 | 38,200 | 48,500 | <0.01 |
| English secondary language, % | 1 | 2 | 4 | <0.01 |
| No. hospital beds per 1,000,000 residents | 3820 | 3390 | 2810 | 0.03 |
| No. radiation oncologists per 1,000,000 residents | 4 | 8 | 12 | <0.01 |
| No. Health Service Areas by SEER region | <0.01 | |||
| Northeast | 1 | 9 | 3 | |
| South | 21 | 27 | 7 | |
| Midwest | 17 | 15 | 3 | |
| West | 10 | 18 | 32 | |
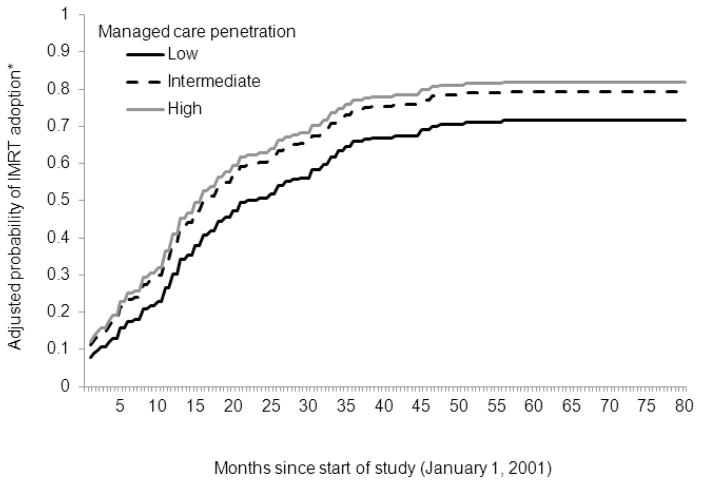
A total of 128 of the 163 HSAs (79%) adopted IMRT over the course of the study. Of the 45 HSAs with the highest managed care penetration, 43 (96%) adopted IMRT. In contrast, of the 69 and 49 HSAs with intermediate and low managed care penetration, only 53 (77%) and 32 (65%) adopted IMRT, respectively. After adjusting for patient- and market-level differences, the adoption trends differed across the three categories of HSAs, with high managed care markets showing the greatest propensity for IMRT adoption (p=0.05) (Figure 1). By 2007, intermediate and highly penetrated markets were roughly 7% to 10% more likely to adopt IMRT compared to those with low managed care penetration. That is, the probability of IMRT adoption in 2007 was 0.82, 0.79, and 0.72 in markets with high, intermediate, and low managed care penetration, respectively.
Figure 1. Probability of IMRT adoption according to managed care penetration.
Throughout the study, high managed care markets demonstrated a greater propensity for IMRT adoption compared to low managed care markets (p=0.05).
HSA, health service area; IMRT, intensity-modulated radiotherapy
*Adjusted for patient-level (i.e., age, tumor grade and stage, and comorbidity) and market-level characteristics (i.e., racial composition, population density, education, income, percent speaking English as a secondary language, number of hospital beds and radiation oncologists in a market, and SEER region).
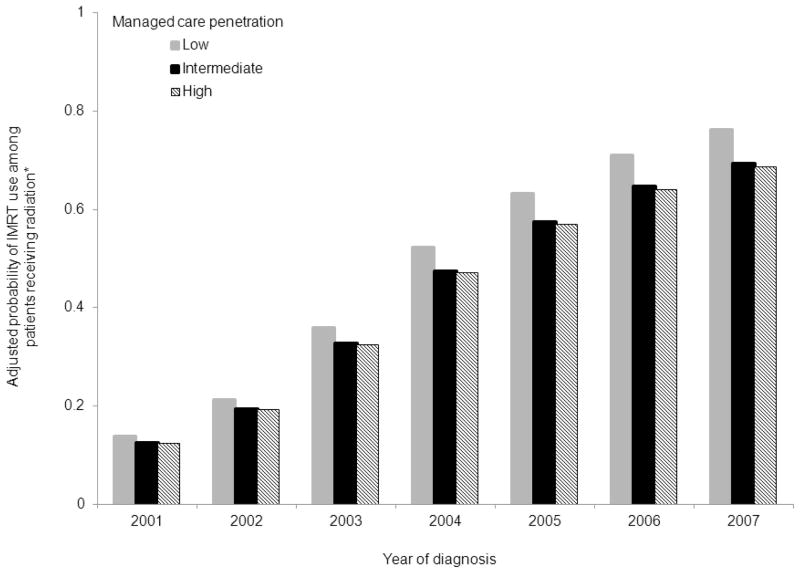
Among HSAs that adopted IMRT, patient and HSA-level characteristics are shown in Table 2. Although statistically significant, the differences in patient characteristics across HSAs were small. In these adopting markets, the use of IMRT among patients treated with radiation is demonstrated in Figure 2, adjusting for differences in patients and healthcare markets. In all three categories of HSAs, the probability of IMRT use increased over time (p<0.01 for trend). However, compared to low managed care markets, the use of IMRT was constrained in markets with the highest managed care penetration (p<0.01). The likelihood of IMRT utilization increased from 13% in 2001 to 69% in 2007 among markets with high managed care penetration. Conversely, in markets with low managed care penetration, IMRT utilization increased from 14% in 2001 to 76% in 2007. Markets with high and intermediate managed care penetration shared similar probabilities of IMRT utilization (p=0.67).
Table 2.
Population characteristics among Health Service Areas that have adopted intensity-modulated radiotherapy
| Health Service Area | Managed care penetration | P Value | ||
|---|---|---|---|---|
| Low | Intermediate | High | ||
| No. Health Service Areas | 32 | 53 | 43 | -- |
| No. patients treated with radiation, % | 4,710 | 24,659 | 24,964 | -- |
| Patient Characteristics | ||||
| Mean patient age, years | 73.6 | 73.5 | 73.8 | <0.01 |
| Well/moderately differentiated tumor grade, % | 57 | 57 | 55 | 0.02 |
| Tumor stage T1, % | 41 | 45 | 43 | <0.01 |
| Charlson Score 2 or higher, % | 11 | 12 | 10 | <0.01 |
| Market characteristics | ||||
| Non-white population, % | 16 | 17 | 27 | <0.01 |
| Population density, (people per square mile) | 228 | 1,070 | 2,380 | <0.01 |
| At least college education, % | 16 | 20 | 28 | <0.01 |
| Median income, $ | 32,800 | 40,900 | 50,200 | <0.01 |
| English secondary language, % | 1 | 2 | 5 | <0.01 |
| No. hospital beds per 1,000,000 residents | 3840 | 3370 | 2850 | <0.01 |
| No. radiation oncologists per 1,000,000 residents | 5 | 11 | 13 | <0.01 |
| No. Health Service Areas by SEER region | <0.01 | |||
| Northeast | 1 | 9 | 3 | |
| South | 16 | 21 | 7 | |
| Midwest | 10 | 10 | 3 | |
| West | 5 | 13 | 30 | |
Figure 2. The probability of IMRT use among men treated with radiation in markets that have adopted IMRT.
In all three categories of HSAs, the probability of IMRT use increased over time (p<0.01 for trend). However, compared to low managed care markets, the use of IMRT was constrained in markets with the highest managed care penetration (p<0.01). Markets with high and intermediate managed care penetration shared similar probabilities of IMRT utilization (p=0.67).
HSA, health service area; IMRT, intensity-modulated radiotherapy
*Adjusted for patient-level (i.e., age, tumor grade and stage, and comorbidity) and market-level characteristics (i.e., racial composition, population density, education, income, percent speaking English as a secondary language, number of hospital beds and radiation oncologists in a market, and SEER region).
COMMENT
New technologies are thought to be responsible for much of the growth in healthcare spending.17,18 IMRT for prostate cancer is one example of a technology that has disseminated rapidly over the past decade. Compared with its predecessor, 3-dimensional conformal therapy, IMRT comes at a premium (~$31,000 vs. $20,000 per patient).2 Coupled with secular trends towards increasing treatment for prostate cancer in general, the dissemination of IMRT over the past decade has contributed, at least in part, to the spending growth of prostate cancer. However, because of its targeting capabilities, IMRT has the ability to deliver higher doses of radiation, which may yield similar or less toxicity4,5 and improve cancer control.6
Because of strong incentives to minimize cost, some worry that managed care organizations may slow the system-wide diffusion of new effective technologies.12,19 Managed care can have widespread effects on both managed care and non-managed care recipients.20 One reason a market’s managed care penetration may influence the overall dissemination of technology pertains to provider practice styles. Physicians have been shown to decrease their use of expensive technology in a managed care versus a fee-for-service setting.21 Moreover, physicians who treat mostly managed care patients offer equivalent treatment intensity among managed care and fee-for-service participants alike.22 This phenomenon, known as a spillover effect, helps explain why patients in similar markets receive similar care.23 As an example, managed care activity affects expenditures and utilization patterns in both the managed care and non-managed care sectors of a market.24 To the extent that a particular technology improves health, this may negatively impact patients residing in markets heavily influenced by managed care. As seen with some other expensive technologies as they are disseminated, healthcare markets with high penetrations of managed care can be sluggish in adopting them.19
Our study has mixed findings with regard to the impact of managed care on IMRT diffusion. On one hand, managed care penetration in a healthcare market did not appear to constrain the acquisition of IMRT for prostate cancer. In fact, markets with the highest managed care penetration obtained the capability to deliver IMRT more rapidly than those with lower penetration. Markets with low managed care penetration are oftentimes less populated and more rural, and thus, may lack the demand, physician expertise, or resources to support such an expensive new technology. However, even after adjusting for population density and several other market-level characteristics, markets with high managed care penetration markets had higher levels of adoption. Alternatively, physicians and hospitals, as opposed to managed care organizations, are the common purchasers of the infrastructure to deliver IMRT. Oftentimes these groups feel pressure to adopt new technologies to stay on the “cutting edge”, making it easier to attract new physicians and patients.25 Thus, these managed care organizations may have little to say about the upfront decision to acquire the technology. To some extent, this finding allays concerns surrounding the impact of evolving delivery systems (i.e., accountable care organizations), which emphasize efficiency, on the adoption of new and expensive healthcare technologies.
On the other hand, after acquiring the ability to deliver IMRT, markets with the highest managed care penetration limited the rate of growth in utilization of the new technology. Although the mechanism underlying this attenuation is uncertain, there are at least a couple of possibilities. First, managed care organizations typically empower primary care physicians as “gatekeepers”, who control the access to specialists and their interventions.11 Ultimately, this has led to some migration of specialists to markets with less managed care,10 and the pattern of IMRT use in this study possibly reflects this. Second, managed care organizations enter areas with hospital competition to leverage their bargaining power.26 While competitive markets may encourage the adoption of IMRT, growth in utilization in these areas might be slowed by the availability of other radiation treatments, which are less expensive but still effective.
Going forward, these findings have policy implications, particularly as accountable care organizations gain traction. Like managed care plans, these organizations strive to decrease costs while maintaining quality of care.27 However, with access to better patient information, more patient involvement in decision making,27 and more quality time with providers,28 it is hoped that physicians in accountable care organizations will deliver care in a more integrated and comprehensive manner. Indeed, although accountable care organizations are different from managed care organizations,28 many of their principles seem to stem from the managed care model.29 Thus, accountable care organizations may influence technology dissemination in similar ways.
Our findings should be interpreted in the context of some limitations. First, as with all observational data, our inference may be biased by unmeasured differences between markets. For instance, the growing presence of urology ownership of IMRT could influence adoption and utilization in certain markets.7 Although we cannot specifically account for unmeasured factors such as this, we adjusted for several measured market factors to minimize confounding. Further, the effects of unmeasured confounding are plausibly less significant in our analyses, which are not assessing differences in outcomes at the patient level. Second, managed care plans represent a variety of private health plans, including health maintenance organizations, preferred provider organizations, and private-fee-for-service plans, which all may have different effects on adoption and utilization. Nonetheless, these plans share the common goal of reducing healthcare costs while providing high-quality care. Further, our analysis involves fee-for-service beneficiaries (i.e., not managed care participants). However, the spillover effects of managed care penetration on Medicare fee-for-service beneficiaries are well-characterized,24 and thus, we feel our findings help tease out the general associations between the dissemination of IMRT and managed care penetration. Third, this study is limited to Medicare patients and may not be generalizable to young men with prostate cancer. However, Medicare managed care market share is highly correlated with overall managed care market share,24 which supports the notion that our findings pertain to younger patients as well.
These limitations notwithstanding, our study has two important findings. First, managed care penetration in a healthcare market was associated with the increased adoption of IMRT for prostate cancer. For IMRT, which is an expensive technology, other market forces (e.g., patient demands, aggressive advertising, and hospital competition) potentially have a greater influence on IMRT’s adoption. Second, after adopting IMRT, markets with the highest managed care penetration limited the rate of growth in its utilization. The decreased utilization of a promising new technology in markets with high managed care penetration may lessen incentives for the development of other technologies, thus conceding potential patient benefits in the future.30 As healthcare enters a period of reform, a deeper understanding of the interplay between healthcare organizations that promote cost-efficient care and market forces that fuel innovation is essential in improving the delivery of healthcare, while sustaining the development of new technologies.
Acknowledgments
SUPPORT
Bruce Jacobs is supported in part by the American Cancer Society Postdoctoral Fellowship Grant (121805-PF-12-008-01-CPHPS). Bruce Jacobs and Florian Schroeck are supported in part by the National Institutes of Health Training Grant NIH 5 T32 DK007782-12.
Brent Hollenbeck is supported in part by the American Cancer Society Pennsylvania Division—Dr. William and Rita Conrady Mentored Research Scholar Grant (MSRG-07-006-01-CPHPS), the American Urological Association Foundation, and Astellas Pharma US, Inc.
The views expressed in this article do not reflect the views of the federal government.
Footnotes
FINANCIAL DISCLOSURES
Bruce L. Jacobs: none
Yun Zhang: none
Ted A. Skolarus: none
John T. Wei: none
James E. Montie: none
Florian R. Schroeck: none
Brent K. Hollenbeck: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Bruce L. Jacobs, Email: brucejac@med.umich.edu.
Yun Zhang, Email: seanyz@med.umich.edu.
Ted A. Skolarus, Email: tskolar@med.umich.edu.
John T. Wei, Email: jtwei@med.umich.edu.
James E. Montie, Email: jmontie@med.umich.edu.
Florian R. Schroeck, Email: fschroec@med.umich.edu.
Brent K. Hollenbeck, Email: bhollen@med.umich.edu.
References
- 1.Jacobs BL, Zhang Y, Skolarus TA, et al. Growth of high-cost intensity-modulated radiotherapy for prostate cancer raises concerns about overuse. Health Aff (Millwood) 2012;31:750–759. doi: 10.1377/hlthaff.2011.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nguyen PL, Gu X, Lipsitz SR, et al. Cost implications of the rapid adoption of newer technologies for treating prostate cancer. J Clin Oncol. 2011;29:1517–1524. doi: 10.1200/JCO.2010.31.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Staffurth J. A review of the clinical evidence for intensity-modulated radiotherapy. Clin Oncol (R Coll Radiol) 2010;22:643–657. doi: 10.1016/j.clon.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 4.Sheets NC, Goldin GH, Meyer AM, et al. Intensity-modulated radiation therapy, proton therapy, or conformal radiation therapy and morbidity and disease control in localized prostate cancer. JAMA. 2012;307:1611–1620. doi: 10.1001/jama.2012.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jani AB, Su A, Milano MT. Intensity-modulated versus conventional pelvic radiotherapy for prostate cancer: analysis of acute toxicity. Urology. 2006;67:147–151. doi: 10.1016/j.urology.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 6.Vora SA, Wong WW, Schild SE, et al. Analysis of biochemical control and prognostic factors in patients treated with either low-dose three-dimensional conformal radiation therapy or high-dose intensity-modulated radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2007;68:1053–1058. doi: 10.1016/j.ijrobp.2007.01.043. [DOI] [PubMed] [Google Scholar]
- 7.Carreyrou J, Tamman M. A Device to Kill Cancer, Lift Revenue. Wall Street Journal. 2010 Dec 7; [Google Scholar]
- 8.Simon CJ, Dranove D, White WD. The impact of managed care on the physician marketplace. Public Health Rep. 1997;112:222–230. [PMC free article] [PubMed] [Google Scholar]
- 9.Franks P, Clancy CM, Nutting PA. Gatekeeping revisited--protecting patients from overtreatment. N Engl J Med. 1992;327:424–429. doi: 10.1056/NEJM199208063270613. [DOI] [PubMed] [Google Scholar]
- 10.Escarce JJ, Polsky D, Wozniak GD, et al. HMO growth and the geographical redistribution of generalist and specialist physicians, 1987–1997. Health Serv Res. 2000;35:825–848. [PMC free article] [PubMed] [Google Scholar]
- 11.Simon CJ, Dranove D, White WD. The effect of managed care on the incomes of primary care and specialty physicians. Health Serv Res. 1998;33:549–569. [PMC free article] [PubMed] [Google Scholar]
- 12.Baker LC, Phibbs CS. Managed care, technology adoption, and health care: the adoption of neonatal intensive care. Rand Journal of Economics. 2002;33:524–548. [PubMed] [Google Scholar]
- 13.Accountable Care Organizations. Centers for Medicare & Medicaid Services (CMS), HHS; Medicare Program; Medicare Shared Savings Program; pp. 67802–67990. [PubMed] [Google Scholar]
- 14.Altekruse SF, Kosary CL, Krapcho M, et al., editors. SEER Cancer Statistics Review, 1975–2007. National Cancer Institute; 2010. [Google Scholar]
- 15.Klabunde CN, Potosky AL, Legler JM, et al. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 16. [Accessed January 3, 2012.];National Center for Health Statistics. Available from URL: http://www.cdc.gov/nchs/
- 17.Newhouse JP. Medical care costs: how much welfare loss? J Econ Perspect. 1992;6:3–21. doi: 10.1257/jep.6.3.3. [DOI] [PubMed] [Google Scholar]
- 18.Maxwell S, Zuckerman S, Berenson RA. Use of physicians’ services under Medicare’s resource-based payments. N Engl J Med. 2007;356:1853–1861. doi: 10.1056/NEJMsa063258. [DOI] [PubMed] [Google Scholar]
- 19.Baker LC. Managed care and technology adoption in health care: evidence from magnetic resonance imaging. J Health Econ. 2001;20:395–421. doi: 10.1016/s0167-6296(01)00072-8. [DOI] [PubMed] [Google Scholar]
- 20.Baker LC. Association of managed care market share and health expenditures for fee-for-service Medicare patients. JAMA. 1999;281:432–437. doi: 10.1001/jama.281.5.432. [DOI] [PubMed] [Google Scholar]
- 21.Bennett CL, Bishop MR, Tallman MS, et al. The association between physician reimbursement in the US and use of hematopoietic colony stimulating factors as adjunct therapy for older patients with acute myeloid leukemia. Results from the 1997 American Society of Clinical Oncology survey. Annals of Oncology. 1999;10:1355–1359. doi: 10.1023/a:1008353130228. [DOI] [PubMed] [Google Scholar]
- 22.Glied S, Zivin JG. How do doctors behave when some (but not all) of their patients are in managed care? J Health Econ. 2002;21:337–353. doi: 10.1016/s0167-6296(01)00131-x. [DOI] [PubMed] [Google Scholar]
- 23.Bian J, Lipscomb J, Mello MM. Spillover effects of state mandated benefit laws: the case of outpatient breast cancer surgery. Inquiry. 2009;46:433–447. doi: 10.5034/inquiryjrnl_46.4.433. [DOI] [PubMed] [Google Scholar]
- 24.Baker LC. The effect of HMOs on fee-for-service health care expenditures: evidence from Medicare. J Health Econ. 1997;16:453–481. doi: 10.1016/s0167-6296(96)00535-8. [DOI] [PubMed] [Google Scholar]
- 25.Lotan Y, Bolenz C, Gupta A, et al. The effect of the approach to radical prostatectomy on the profitability of hospitals and surgeons. BJU Int. 2010;105:1531–1535. doi: 10.1111/j.1464-410X.2009.08996.x. [DOI] [PubMed] [Google Scholar]
- 26.Baker LC, Spetz JE. Managed Care and Medical Technology Growth. NBER Working Paper Series. 1999;w6894 Available at SSRN: http://ssrn.com/abstract=147169. [Google Scholar]
- 27.Correia EW. Accountable care organizations: the proposed regulations and the prospects for success. Am J Manag Care. 2011;17:560–568. [PubMed] [Google Scholar]
- 28.Berwick DM. Making good on ACOs’ promise--the final rule for the Medicare shared savings program. N Engl J Med. 2011;365:1753–1756. doi: 10.1056/NEJMp1111671. [DOI] [PubMed] [Google Scholar]
- 29.Weil TP. Accountable care organizations. HMOs by another name? J Fam Pract. 2012;61:10. [PubMed] [Google Scholar]
- 30.Baker LC, Atlas SW. Relationship between HMO market share and the diffusion and use of advanced MRI technologies. J Am Coll Radiol. 2004;1:478–487. doi: 10.1016/j.jacr.2004.02.009. [DOI] [PubMed] [Google Scholar]