Abstract
Background and Objectives:
A variety of surgical procedures of the penis can be performed under local anesthesia. We evaluated the efficacy and safety of EMLA cream anesthetic in such procedures.
Materials and Methods:
In total 330 adult patients were subjected to minor penile surgery including: Complete circumcision (73), short frenulum plasty (168), meatotomy (14), fulguration of penile warts (56) and fulguration of urethral (meatal) warts (19). The level of anesthesia obtained by EMLA cream application along with any adverse effects was recorded.
Results:
The use of EMLA on mucosal lesions provided excellent level of local anesthesia in almost all patients (245/246, 99.5%). Anesthesia of skin lesions was in part influenced by the site of application. Circumcision patients showed the lowest efficacy of the EMLA cream as the majority (~80%) required some form of further anesthesia until the completion of the procedure. No significant adverse effects were noted. A transient erythema was present in almost all mucosal applications.
Conclusions:
The topical anesthetic EMLA cream is a useful, efficient and safe tool for minor surgical procedures of the penis at the office setting, with the exception of circumcision, where an additional type of anesthesia is likely to be necessary. Side effects can be kept to a minimum when the suggested doses are respected (especially at mucosal application) and the time allowed for action is carefully tailored to the site of application and the type of procedure.
Keywords: EMLA, penis, surgery, topical anesthesia
INTRODUCTION
A wide range of minor surgical procedures of the penis are being performed nowadays under local anesthesia, usually at an office setting. These procedures usually deal with the prepuce (circumcision, dorsal slit or prepuce plasty, separation of preputial adhesions), the urethral meatus (meatotomy) and the frenulum (short frenulum plasty). Another common procedure involves the removal of genital warts (penile HPV lesions). All of these procedures require some form of anesthesia. The development of local anesthetics in the latter half of the 19th century has provided both surgeons and patients with an easy, relative safe and effective form of pain alleviation for such procedures. However, infiltration of local anesthetics still has several drawbacks: Injections of local anesthetics are painful by themselves, may worsen needle anxiety and increase pain perception Moreover they may cause bleeding and distort the surgical area by development of edema or hematoma. There is also the risk of inadvertent intravascular injection, especially when larger volume of anesthetic solution is used.[1]
On the other hand, topical cream anesthetics are a more “patient-friendly” approach to local anesthesia; it has been shown that by using a topical anesthetic cream the patient's anxiety and distress about the procedure itself are alleviated.[1] Many compounds have been developed since the original enthusiasm with cocaine's topical anesthetic ability demonstrated by Carl Koller in Vienna in 1884.[2] However, initial concerns on anesthetic absorption through the mucosa hampered their extensive use in the genital region.
The aim of this study was to evaluate the efficacy and safety of a topical anesthetic cream (EMLA, Eutectic Mixture of Local Anesthetics, 2.5% lidocaine and 2.5% prilocaine) as topical anesthetic in several office surgical procedures of the external genitalia in adult males.
MATERIALS AND METHODS
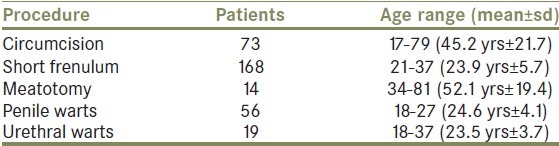
During a period of approximately 8 years (Sept. 2003-Aug. 2011) a total of 330 patients were subjected to minor penile surgery at an office setting under local anesthesia. The range of procedures included: Complete circumcision for phimosis, short frenulum plasty, meatotomy, fulguration of penile warts and fulguration of urethral (meatal) warts. The distribution of cases is described in Table 1.
Table 1.
Distribution of patients according to surgical procedure and age
All patients were offered to choose between infiltration with a local anesthetic and application of a topical cream as a form of local analgesia. After detailed information was given, all patients (100%) opted for the topical cream application. Informed consent was obtained by those patients whose genitals were photographed for archival and scientific purposes. In all cases the topical cream used was EMLA 5 gr (2.5% lidocaine and 2.5% prilocaine), Astra Zeneca, Inc. The amount of cream used varied among individuals and procedures (see below). For the fulguration of genital warts, frenulum plasty and haemostasis during circumcision we used the Birtcher Hyfercator Plus™ (Birtcher Medical Systems Inc, Utica, NY), a high frequency device used for monoterminal fulguration at low power settings (7-10 Watts). When additional anesthesia was required, local infiltration with lignocaine (Xylocaine 2%, AstraZeneca Inc) was performed.
Application method and surgical procedure
Circumcision
A total of 73 patients were subjected to circumcision due to phimosis. Topical anesthesia was initially achieved by spreading EMLA cream (approx. 2-5 gr) in the preputial sac with the aid of a 5 ml syringe. A plain cling film dressing was used for preventing the cream to spread out and the level of analgesia was evaluated first at 20 minutes and again at 30 minutes by pinching the prepuce with a toothed forceps. If the patient still reported pain or discomfort, further anesthesia was achieved initially by local infiltration with lignocaine at the ventral preputial surface (the frenular area). If this measure was inadequate, dorsal penile block with approximately 20 ml 1% Xylocaine was performed. After completion of the procedure the traumatic surface was smeared with povidone iodine cream and a circular gauge dressing was applied. No antibiotics or analgesics were prescribed.
Short frenulum plasty
Short frenulum plasty was performed in 168 young males. The method used for short frenulum correction was the “pull and burn method” described previously.[3] Briefly, a small amount of EMLA cream (max 2 gr) was applied at the frenulum area and an occlusive dressing (Tegaderm®, 3M Inc.) was used to prevent the cream from leaking [Figure 1]. After 20 minutes the adhesive dressing was gently removed and the procedure started if the patient reported no pain at all at pinprick. A small horizontal cut was made using the Hyfercator and the superficial layer of the frenulum was gradually separated by applying gentle and stable traction to the glans and the shaft of the penis. Minor bleeders were sealed by the Hyfercator at low power, taking care not to severe the frenular artery. Patients were instructed to start personal hygiene on the following day, with emphasis on keeping the trauma as dry as possible.
Figure 1.
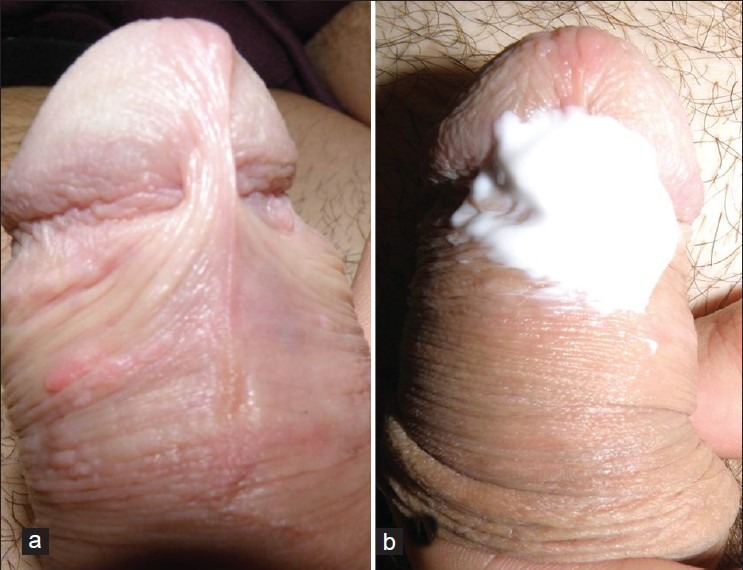
(a) A short frenulum case in a young patient. (b) Note limited amount of EMLA cream applied just before placement of the dressing
Meatotomy
A total of 14 patients were subjected to meatotomy due to meatal stenosis. In five cases the patients presented Balanitis Xerotica Obliterans (BXO) affecting the glans and the meatus. A small quantity of EMLA cream (~1 gr) was applied using a small 1-ml syringe and an occlusive dressing was applied. After 20 minutes the adhesive dressing was gently removed, the glans was squeezed to remove excess cream and a small haemostatic clip was used to spread the urethral meatus. The incision was made to the ventral surface of the meatus and was extended ventrally (6 o’clock position) until a sufficient opening of the meatus was achieved (calibrated with a 18 Fr Tiemann catheter). In four patients the urethral mucosa was sutured at the meatal lips at the 3 and 9 o’clock position using fine absorbable sutures (5-0 polyglycolic acid, Safil Quick™, B. Braun Melsungen AG).
Fulguration of urethral warts
A total of 19 male patients were treated for warts (HPV lesions, condylomata acuminata) at the external urethral meatus. The lesions were limited to the meatus or fossa navicularis [Figure 2]. Application of EMLA was similar as described above. The warts were fulgurated using the Hyfercator at low power settings (approximately 5 Watts).
Figure 2.
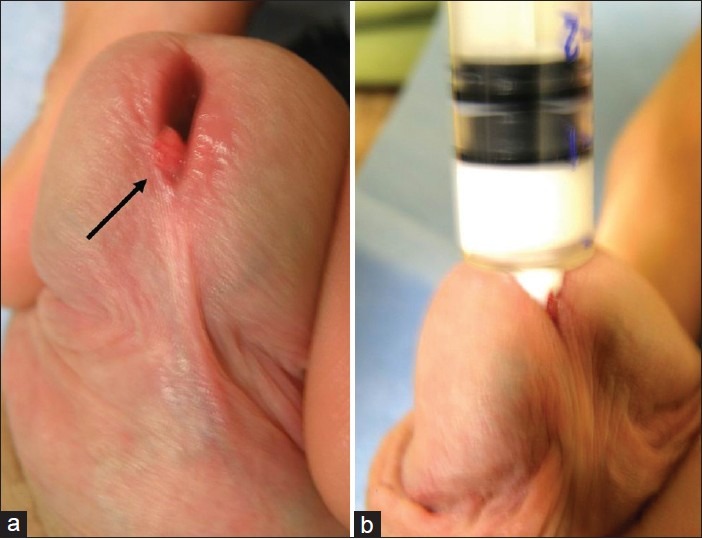
(arrow, a) A urethral wart protruding from the external urethral meatus. (b) Infusion of anesthetic through the meatus
Fulguration of penile warts
Penile warts (HPV lesions, condylomata acuminata) were treated with fulguration in 56 young patients. The location of the warts varied: In most cases they involved the penile shaft skin and the preputial ridge, the inner layer of the prepuce, the frenular region and the glans penis [Figures 3 and 4]. In cases of mucosal lesions topical anesthesia was achieved using a small quantity of EMLA cream (approximately 1-3 gr, depending on the extent of the lesions) and an occlusive dressing to keep the cream from being dislodged. In the cases of penile skin lesions the dressing was left in place for 1 hour. The procedure was completed by fulguration at low power settings (approx. 5 Watts).
Figure 3.

(arrows, a) Multiple penile warts at the dorsal surface of the preputial ridge. (b) Application of the occlusive dressing
Figure 4.
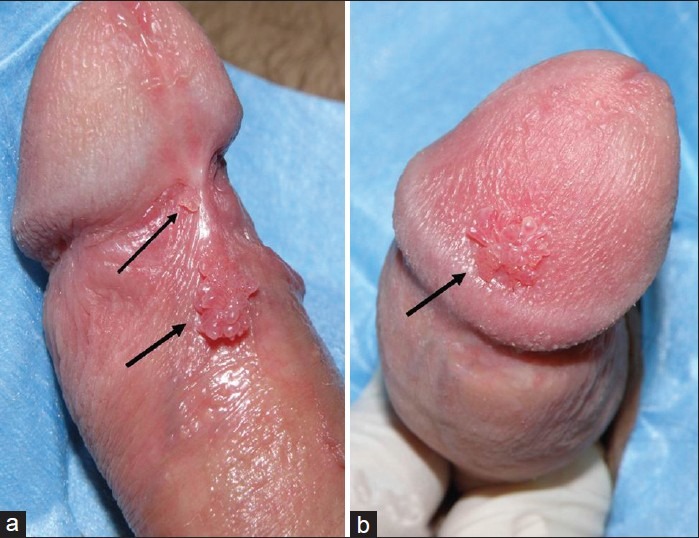
(a) Multiple HPV lesions (penile warts) at the frenular area and (b) the glans penis
RESULTS
A total of 330 patients were subjected to minor surgery of the external genitalia under topical anesthesia with EMLA cream. With the exception of circumcision patients, in whom efficacy of EMLA anesthesia was limited, only one case in the short frenulum group and four cases in the penile warts group required further infiltration with local anesthetic. The overall satisfaction rate was evaluated asking the global assessment question: “Are you fully satisfied with the result of the topical anesthetic cream? - Yes/No.” A total of 267/330 patients (80.9%) were satisfied and stated that they would opt again for this type of local anesthesia for a similar procedure in the future. Detailed results for each type of procedure are presented below.
Circumcision
Efficacy of EMLA application was quite limited, as in only 15/73 cases (20.5%) with phimosis the use of topical cream alone was sufficient for anesthesia until completion of the procedure. In the rest of the 58 patients (79.5%) further local infiltration with 2% lignocaine was required in 24 cases (41.4%) while dorsal penile nerve block with 1% lignocaine was required in 34 cases (58.6%). The use of EMLA cream in most of these cases would alleviate to some extent the painful stimuli (e.g., clamping with forceps); however, this was not adequate for completion of the procedure and the patients requested further analgesia.
Short frenulum plasty
The level of local anesthesia obtained by EMLA cream in 20 minutes was sufficient in all 168 cases but one patient with a notably thick frenulum, who required further local anesthesia with lignocaine infiltration (~0.5 ml Xylocaine 2%). No sutures were generally used; in only three patients (1.8%) with a thick and wide frenulum, fine absorbable sutures (5-0 polyglycolic acid, Safil Quick™, B. Braun Melsungen AG) were used to approximate the lateral edges of the tear in order to achieve faster wound healing and better cosmetic result.
Meatotomy
The use of EMLA cream was in all cases sufficient to obtain a satisfactory level of local anesthesia until completion of the procedure. Even when sutures were used to anchor the urethral mucosa at the meatal lips, no pain was reported by the patients.
Fulguration of urethral warts
Topical EMLA application achieved a complete level of local anesthesia in all patients. Even when meatotomy was performed in order to gain deeper access to the fossa navicularis, no further anesthesia was necessary.
Fulguration of penile warts
Generally, warts present on the mucosal surface were removed under topical cream anesthesia. However, in 4/11 (36.4%) cases of penile skin warts, further infiltration with 2% lignocaine was required. However, in three of these cases with condylomata located at the penile shaft skin near the pubis, the occlusive dressing had been dislocated during the waiting time of 1 hour, as pubic hair did not allow for air-tight adhesion of the Tegaderm® dressing. In the rest of 52 patients no further local anesthetic was required and fulguration was completed uneventfully.
The application of EMLA was generally well tolerated. A sensation of “mint freshness” or minor itching was reported by most patients when the cream was applied on mucosal surface. Local erythema was present in almost all cases with mucosal application; however, this did not affect the course of the procedures. No significant skin reaction or allergic reaction, cyanosis or methemoglobinemia were recorded.
DISCUSSION
We evaluated the efficacy and safety of the use of the topical cream anesthetic EMLA in several outpatient procedures on the penis. In the past such procedures would require infiltration with a local anesthetic such as lignocaine and at least some form of sedation. The use of topical acting anesthetics is patient-friendly as it eliminates needle fear, anxiety and injection pain at the beginning of the procedure. In contrast, infiltrative anesthetics often produce bleeding, hematomas or edema that may distort the surgical site, an important factor in delicate procedures with a desirable good aesthetic result. One should also bear in mind the always present risk of accidental systemic intravascular injection of injectables, especially in procedures where higher doses are needed.[4]
EMLA cream is an oil-in-water emulsion of 2.5% lignocaine and 2.5% prilocaine. The eutectic mixture contains a thickener, an emulsifier and distilled water adjusted to a pH level of 9.4.[5] This formulation enhances absorption through intact skin. For our group of patients EMLA appeared as the best choice, due to its commercial availability, low cost and easiness in application. It should be noted however that other topical anesthetics give comparable results as they all share common action mechanisms.[6]
The overall efficacy of EMLA application in our series was excellent, especially when the cream was applied on mucosal surfaces. In all but one of the 246 mucosal applications (0.4%) the topical cream provided adequate anesthesia for completion of the procedure. Similar results have been demonstrated with EMLA use in procedures such as frenuloplasty or meatotomy, although most studies would also include some additional forms of analgesia or sedation (e.g., nitrous oxide).[7–9] Skin application on the other hand requires an extended period of application time (approx. 1 hr) and care must be taken to ensure that the dressing stays in place to prevent cream leak. In four of our cases with penile skin warts the dressing was not air-tight enough, due to the presence of pubic and penile shaft hair in the region. This could probably be avoided by shaving pubic hair when lesions are on or near hairy skin.
In contrast, the circumcision cases showed limited efficacy of the EMLA application as a sole anesthetic agent: Only in 15/73 cases (20.5%) was EMLA adequately effective. The reasons behind this finding may be explained by the complex nature of the penile and foreskin innervation.[10] In the case of a proper circumcision, three parts of the penis have to be anesthetized: The penile shaft skin, the inner layer of the prepuce and especially the ridged band and the mostly sensitive frenular area. This may explain why application of EMLA on the inner part of the preputial sac was firstly incomplete (due to concomitant phimosis) and secondly inadequate to provide anesthesia to the penile shaft skin. Interestingly, those patients to whom EMLA cream provided sufficient analgesia featured a thin, soft prepuce (although this has not been properly measured). It is possible that penetration of the anesthetic was easier through a thinner mucosal epithelium and lamina propria of the prepuce. Nevertheless, it should be noted that although EMLA was insufficient for initiation or completion of the procedure it did, however, partly alleviated the pain from further local infiltration. This finding suggests that EMLA might be used as an agent for pain reduction associated with local infiltration or dorsal penile nerve block during circumcision.
Application of the EMLA cream as a local anesthetic is simple and straightforward. According to the product datasheet, the recommended time is 1 hr for skin application and 5-10 minutes for mucosal surfaces; in our series, however, we generally allowed 20 mins for the anesthetic to act, especially for procedures such as frenulum plasty or large condylomata, in which deeper levels of the preputial mucosa had to be fulgurated. Other studies have suggested that the quality of analgesia actually decreases with application times longer than 10-15 minutes.[4] The decreasing efficacy associated with longer periods of application time is attributed to lidocaine-induced vasodilatation and subsequent increased systemic absorption.[5] However, this negative time effect has not been verified in our series.
Safety issues have always been a concern with topical anesthetics. In our series no significant adverse effects were recorded. A minor local transient erythema was present in almost all cases of mucosal application; this is attributed to initial peripheral vasoconstriction followed by vasodilatation.[11] It appears that EMLA use is safe when the recommended doses are respected and the application time is not being exceeded significantly. Every effort should be made to limit the skin or mucosal area covered to the smaller extent necessary. Moreover, special precautions should be used in specific cases. A history of congenital or idiopathic methemoglobinemia is an absolute contraindication; patients with glucose-6-phosphate dehydrogenase (G-6-P-D) deficiency and those who require treatment with methemoglobin-inducing drugs are more susceptible to acquired methemoglobinemia.[12]
CONCLUSIONS
The topical anesthetic EMLA cream is a useful, efficient and safe tool for minor surgical procedures of the penis at the office setting. It is a patient-friendly method of local anesthesia, providing excellent results in mucosal applications, with the exception of proper circumcision, where an additional type of anesthesia is likely to be necessary. Side effects can be kept to a minimum when the suggested doses are respected (especially at mucosal application) and the time allowed for action is carefully tailored to the site of application and the type of procedure.
Footnotes
Source of Support: Nil,
Conflict of Interest: None
REFERENCES
- 1.Kaweski S. Plastic Surgery Educational Foundation Technology Assessment Committee. Topical anesthetic creams. Plast Reconstr Surg. 2008;121:2161–5. doi: 10.1097/PRS.0b013e318170a7a4. [DOI] [PubMed] [Google Scholar]
- 2.Gordetsky J, Bendana E, O’Brien J, Rabinowitz R. (Almost) painless surgery: A historical review of the evolution of intraurethral anesthesia in urology. Urology. 2011;77:12–6. doi: 10.1016/j.urology.2010.03.068. [DOI] [PubMed] [Google Scholar]
- 3.Gyftopoulos K. Male dyspareunia due to short frenulum: The suture-free, “pull and burn” method. J Sex Med. 2009;6:2611–4. doi: 10.1111/j.1743-6109.2009.01357.x. [DOI] [PubMed] [Google Scholar]
- 4.Zilbert A. Topical anesthesia for minor gynaecological procedures: A review. Obstet Gynecol Surv. 2002;57:171–8. doi: 10.1097/00006254-200203000-00022. [DOI] [PubMed] [Google Scholar]
- 5.Kundu S, Achar S. Principles of office anesthesia: Part II. Topical anesthesia. Am Fam Physician. 2002;66:99–102. [PubMed] [Google Scholar]
- 6.Smith DP, Gjellum M. The efficacy of LMX versus EMLA for pain relief in boys undergoing office meatotomy. J Urol. 2004;172:1760–1. doi: 10.1097/01.ju.0000139830.42599.a6. [DOI] [PubMed] [Google Scholar]
- 7.Laffon M, Gouchet A, Quenum M, Haillot O, Mercier C, Huguet M. Eutectic mixture of local anesthetics in adult urology patients: An observational trial. Reg Anesth Pain Med. 1998;23:502–5. doi: 10.1016/s1098-7339(98)90035-9. [DOI] [PubMed] [Google Scholar]
- 8.Buckley MM, Benfield P. Eutectic lidocaine/prilocaine cream: A review of the topical anaesthetic/analgesic efficacy of a eutectic mixture of local anaesthetics (EMLA) Drugs. 1993;46:126–51. doi: 10.2165/00003495-199346010-00008. [DOI] [PubMed] [Google Scholar]
- 9.Ben-Meir D, Livne PM, Feigin E, Djerassi R, Efrat R. Meatotomy using local anesthesia and sedation or general anesthesia with or without penile block in children: A prospective randomized study. J Urol. 2011;185:654–7. doi: 10.1016/j.juro.2010.09.119. [DOI] [PubMed] [Google Scholar]
- 10.Cold CJ, Taylor JR. The prepuce. BJU Int. 1999;83(Suppl 1):34–44. doi: 10.1046/j.1464-410x.1999.0830s1034.x. [DOI] [PubMed] [Google Scholar]
- 11.Lener EV, Bucalo BD, Kist DA, Moy RL. Topical anesthetic agents in dermatologic surgery.A review. Dermatol Surg. 1997;23:673–83. doi: 10.1111/j.1524-4725.1997.tb00388.x. [DOI] [PubMed] [Google Scholar]
- 12.Wright RO, Lewander WJ, Woolf AD. Methemoglobinemia: etiology, pharmacology, and clinical management. Ann Emerg Med. 1999;34:646–56. doi: 10.1016/s0196-0644(99)70167-8. [DOI] [PubMed] [Google Scholar]


