Abstract
Mechanisms linked to actin filaments have long been thought to cooperate in smooth muscle contraction, although key molecules were unclear. We show evidence that cardiac troponin T (cTnT) substantially contributes to Ca2+-mediated contraction in a physiological range of cytosolic Ca2+ concentration ([Ca2+]i). cTnT was detected in various smooth muscles of the aorta, trachea, gut and urinary bladder, including in humans. Also, cTnT was distributed along with tropomyosin in smooth muscle cells, suggesting that these proteins are ready to cause smooth muscle contraction. In chemically permeabilised smooth muscle of cTnT+/− mice in which cTnT reduced to ~50%, the Ca2+-force relationship was shifted toward greater [Ca2+]i, indicating a sizeable contribution of cTnT to smooth muscle contraction at [Ca2+]i < 1 μM. Furthermore, addition of supplemental TnI and TnC reconstructed a troponin system to enhance contraction. The results indicated that a Tn/Tn-like system on actin-filaments cooperates together with the thick-filament pathway.
Increases in cytosolic Ca2+ concentration ([Ca2+]i) cause contraction in any muscle. It is, however, believed that regulatory mechanisms underlying the Ca2+-mediated actin-myosin interaction differ fundamentally between muscle types. Namely, in striated skeletal and cardiac muscles, Ca2+ bound to troponin (Tn) on actin filaments removes the inhibitory effect of Tn on the actin-myosin interaction1,2. In contrast, smooth muscles employ the Ca2+/calmodulin complex to activate myosin light chain kinase (MLCK), in turn resulting in an actin-myosin interaction through phosphorylation of the myosin light chain (MLC)3,4,5.
Although a major contribution of myosin thick-filaments to smooth muscle contraction is widely accepted, there is considerable evidence that thin filament-linked mechanisms are operating in parallel (e.g. contribution of caldesmon and calponin)6,7,8,9,10. In addition, a number of chemicals, e.g. activators for protein-kinase C and PI3-kinase11,12,13,14, are known to cause contraction independent of MLC phosphorylation. Despite this, to date, the functional contribution of a troponin-regulatory system is ambiguous.
In the present study, we show evidence that cardiac troponin T (cTnT) exists in smooth muscle, including humans, and substantially contributes to Ca2+-mediated contraction in a physiological range of [Ca2+]i especially below 1 μM. The results indicate that a Tn-like system on actin-filaments cooperates together with the myosin regulatory pathway in smooth muscle, as the phosphorylation of myosin light chain modulates contractions in striated muscles15. The present findings on TnT suggest new insight into medical treatments to overcome numerous diseases related to the malfunction of smooth muscle distributed over the body: The Tn-like system in smooth muscle is a possible target in pharmacological and genetic therapies. In addition, mutations on TnT and associated proteins are likely to also alter smooth muscle contractility through the Tn-like system, as observed in familial myopathies of cardiac and skeletal muscles2,16.
Results
Expression of troponins in smooth muscle
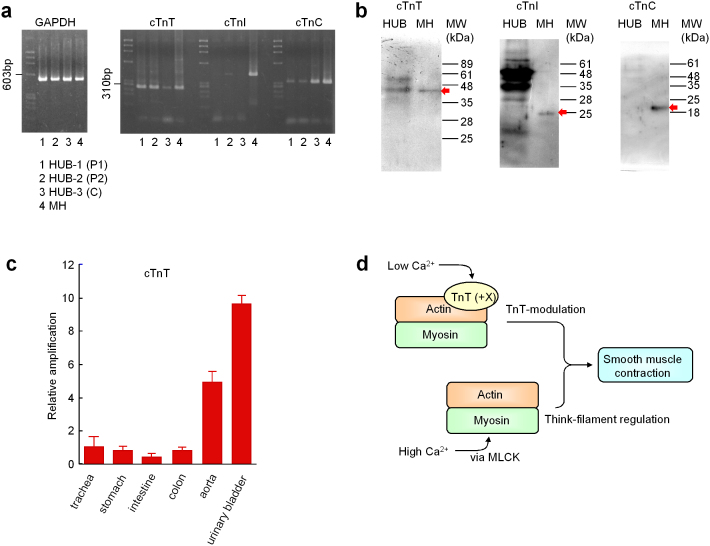
In striated muscle, a complex of three troponins, namely TnT/TnC/TnI, acts as a molecular switch of the actin-myosin interaction2. Thus, we first explored the expression of cardiac troponins (cTn) in detrusor smooth muscle isolated from the urinary bladder of humans. RT-PCR detected all three components of cTn (Fig. 1a). Although amplicons were faint in some of cTnI and cTnT examinations, the sequences of the amplicons were exactly the same as known sequences of cDNAs of cTnT, cTnI and cTnC in human detrusor, respectively (Fig. S1). Whilst immunoblotting clearly detected only cTnT (Fig. 1b). Positive controls were obtained from mouse heart (MH).
Figure 1. Expression of cardiac troponins in smooth muscle.
(a) RT-PCR detection of cardiac troponins (cTnT/cTnI/cTnC) in detrusor smooth muscle. Specimens used were from human urinary bladder (HUB) detrusor smooth muscle (cystectomy patients: P-1 and P-2), commercial tRNA of human urinary bladder smooth muscle (C), and mouse cardiac ventricular muscle (MH). (b) Western blot examination of cardiac troponins in human detrusor smooth muscle and mouse heart (MH). Red arrow indicates the expected molecular weight (MW) of each cardiac troponin. (c) Real-time PCR quantification of cTnT in commercial tRNA of various human smooth muscle tissues. cTnT expression is plotted relative to that in trachea. (d) Schematic diagram. cTnT may contribute to smooth muscle contraction by modulating actin filaments.
To examine the tissue-dependent expression of cTn among smooth muscles, real-time PCR was carried out using commercial standard mRNA samples obtained from the human trachea, stomach, small intestine, colon, aorta and urinary bladder. The amount of cTnT varied among smooth muscles. Urinary bladder (detrusor) contained 9.5 times more than trachea, while gastrointestinal smooth muscles contained only 35–77% (Fig. 1c). The amounts of cTnC and cTnI also varied among tissues (Fig. S2). These results imply that a part of contraction is mediated via the Tn complex and/or a Tn-like complex, including replaceable proteins on actin filaments along with a major control of myosin filament activation (Fig. 1d), and that detrusor smooth muscle is a suitable tissue to demonstrate cTnT-related contraction (Fig. 1c).
Colocalisation of TnT with tropomyosin
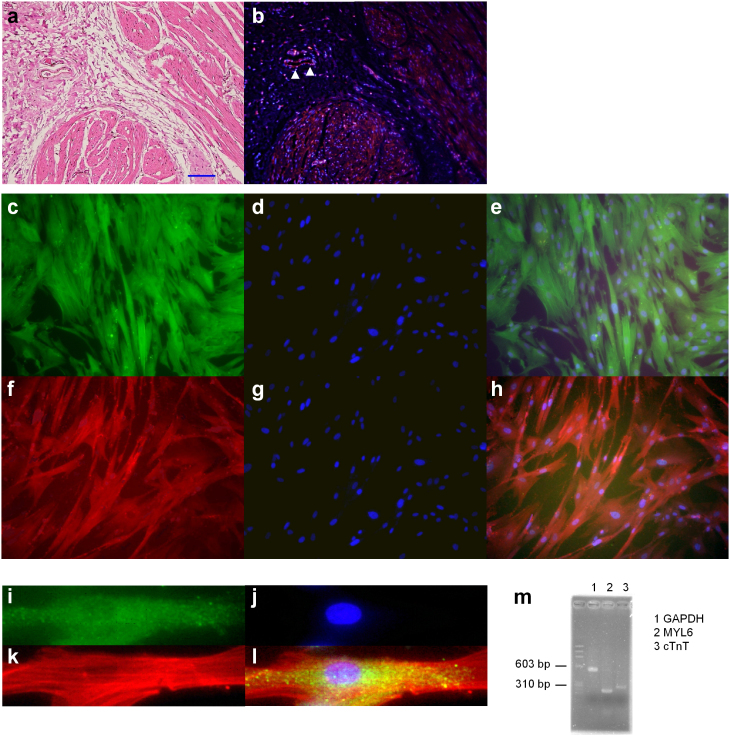
The Tn complex promotes an actin-myosin interaction by shifting tropomyosin, which covers myosin-binding sites on actin filaments in striated muscle. On the other hand, smooth muscle is known to contain tropomyosin in the cytosplasm, although its physiological function is not well understood so far17,18. Thus, we assessed if TnT and tropomyosin colocalize in the cytoplasm of smooth muscle cells. In a pair of thin sections prepared from human detrusor, cTnT fluorescence was observed in smooth muscle bundles, but not in the connective tissue region except for the wall of veins (Fig. 2a, 2b).
Figure 2. Histological analysis.
(a and b) A pair of thin sections of human urinary bladder detrusor smooth muscle were used. Hematoxylin-eosin (HE) staining in (a), and fluorescence of cTnT (red) and nuclear (blue) in (b). The scale bar indicates 150 μm (a), (c–l) Cultured smooth muscle cells of human detrusor smooth muscle were used in fluorescence photomicrographs. (c–e) Double staining of cTnT (green, c) and nuclear (blue, d); merge (e). (f–h) Double staining of tropomyosin (TM) (red, f) and nuclear (blue, g); merge (h). (i–l) Triple staining of cTnT (green, i), nuclear (blue, j) and tropomyosin (TM) (red, k) are shown expanded; merge (l). (m) The expression of GAPDH, MYL6 (smooth muscle marker) and cTnT in the same cultured smooth muscle cells was examined using RT-PCR.
To rule out background fluorescence from cells other than smooth muscle, cultured detrusor smooth muscle cells were next used. These cells were clearly stained with anti-cTnT (Fig. 2c, 2e) or anti-tropomyosin antibodies (Fig. 2f, 2h): double staining with cellular nuclei (Fig. 2d, 2e and Fig. 2g, 2h). Also, the overlap of cTnT and tropomyosin fluorescence is shown expanded: triple staining (Fig. 2i–2l). Furthermore, RT-PCR detected both cTnT and MYL6 (smooth muscle indicator) in the same cultured cells prepared from the human detrusor (Fig. 2m). These results suggest that cTnT and tropomyosin are fixed together and are ready to cause smooth muscle contraction if any signal targets thin filaments to be activated.
Ca2+-mediated contraction
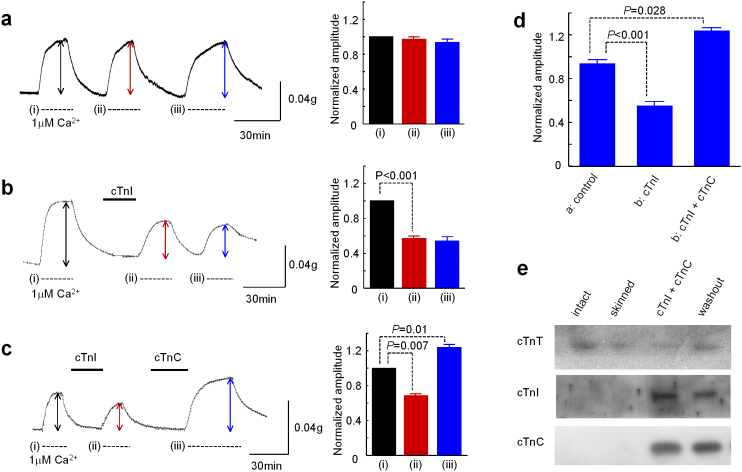
In order to assess whether [Ca2+]i-dependent force development employs endogenous TnT on tropomyosin to induce contraction, we permeabilized human detrusor strips with β-escin to control [Ca2+]i. After chemical permeabilization at least three subsequent applications of 1 μM Ca2+ caused stable contractions of similar amplitude (i, ii and iii in Fig. 3a): 0.97±0.04 and 0.94±0.06 in the second and third contraction, respectively relative to the first one (n = 5).
Figure 3. Potentiation of Ca2+-dependent force development by constituting Tn complex.
Three contractions (i, ii and iii) were successively induced by applying a bathing solution containing 1 μM [Ca2+] in chemically permeabilised strips prepared from human detrusor smooth muscle. (a) Left panel, an example trace showing a measurement of forcedevelopment; right panel, summary graph for the three successive contractions. cTnI was added to the bathing solution before the second contraction in b, and cTnC was additionally applied before the third contraction in c. The amplitude of the third contraction relative to the first one is plotted in d. The application of cTnI reduced, and the application of both cTnI and cTnC potentiated the third contraction statistically significantly (* P<0.05 and ** P<0.01, respectively, unpaired t-test). (e) Western blot examinations of Tn proteins. Lane 1 and lane 2 show before and after permeabilisation, respectively. Lane 3 and 4 correspond to the force measurement c before and after washout with relaxing solution for 30 min, respectively.
cTnT appears to be fixed on tropomyosin in the cytoplasm (Fig. 2c–2f), while cTnI and cTnC are less than cTnT (Fig. 1c), and the peameabilization procedure is likely to release these troponin proteins along with replaceable proteins, if any, toward the extracellular space. We thus examined the effects of exogenous cTnI and cTnC. The application of cTnI after first contraction decreased the amplitude of the third contraction to 0.55±0.04 (n = 6; Fig. 3b), whereas the application of cTnC restored it to 1.23±0.03 (n = 6; Fig. 3c). The amplitude of the third contraction is summarized in Fig. 3d (see also Fig. S3 showing consistent effects of cTnI and cTnC irrespective of exposure time). An immunoblot shows the existence of cTnT after the permeabilization procedure (Fig. 3e: lane 1 in control; lane 2 after permeabilization). Also, after the application of exogenous cTnI and cTnC, all three troponin proteins were detected even after washout for 30 min (Fig. 3e lane 3), corresponding to the force measurement shown in Fig. 3c. Taken together, these results indicate that the potentiation of contraction (~23% increase), seen after the application of exogenous cTnI and cTnC, is due to construction of a Tn-complex-mediated contractile pathway, also reinforcing the working hypothesis that thin and thick filament-related pathways co-contribute to Ca2+-mediated smooth muscle contraction.
cTnT-deficient mice
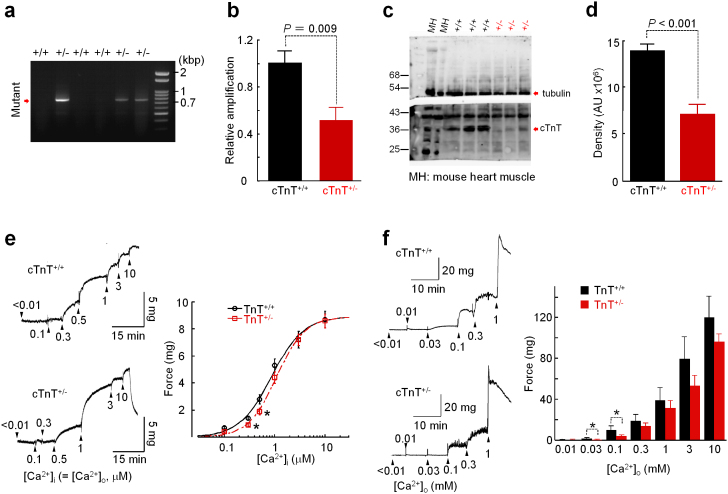
To further confirm the role of cTnT in smooth muscle contraction, we next used cTnT+/− mice. The expression of cTnT in mRNA and protein was significantly reduced in urinary bladder detrusor smooth muscle of cTnT+/− mice (cTnT mRNA: 100±10.1% in WT mice, n = 5 vs 51.4±10.1% in cTnT+/− mice, n = 5 in; cTnT protein: 13.5±1.46 × 106, n = 6 vs 7.0±0.24 × 106 n = 6) (Fig. 4a–4d). [Ca2+]i-dependence of force development was examined in chemically permeabilized detrusor strips. [Ca2+] of bathing solution increased cumulatively. The force development caused by Ca2+ < 1 μM was significantly smaller in cTnT+/− mice (at 0.3 μM [Ca2+]i, 1.41±0.16 mg vs 0.91±0.13 mg, P = 0.033; at 0.5 μM [Ca2+]i, 2.84±0.33 mg vs 1.94±0.14 mg, P = 0.0017, respectively; n = 29 in WT vs 34 in cTnT+/− mice), and it reached nearly the same level in both muscle strips at [Ca2+]i > 3 μM (Fig. 4e).
Figure 4. Expression of cTnT and mechanical activity in WT (cTnT+/+) and cTnT+/− mice.
(a) Genotyping of WT (cTnT+/+) and cTnT+/− mice. Mutant bands at 0.76 kbp. (b) Real-time PCR quantification of cTnT. Expression of cTnT mRNA was normalized by the average value in cTnT+/+ mice. (c and d) Western blot detection of cTnT is shown with β-tubulin in c. To quantify, cTnT content was normalized by β-tubulin in d. MH: Mouse heart. (e) Force development measured in chemically permeabilised strips of detrusor smooth muscle (~0.3 × 0.3 × 2 mm) isolated from WT (cTnT+/+) and cTnT+/− mice (n = 28 versus 34, * P<0.05: left panel). Force development (F) is plotted against [Ca2+] (right panel). The curves were drawn by fitting all data to the following equation: F([Ca2+]) = Fmax/{1+(KM/[Ca2+])H}, where KM, and H are [Ca2+] for the half-maximal force development and Hill coefficient, respectively. The estimated KM was 0.76 μM in WT mice and 1.11 μM in cTnT+/− mice. (f) Force development measured in intact detrusor strips in the presence of CCh (right panel), and the Ca2+-force relationship (left panel) in WT and cTnT+/− mice (n = 25 vs 30, unpaired t-test).
Muscarinic agonists such as acetylcholine (ACh) and carbachol (CCh), activate non-selective cation channels (NSCC) permeable to Ca2+ in detrusor smooth muscle19. In intact detrusor strips (without chemical permeabilization) from WT and cTnT+/− mice, the extracellular Ca2+ concentration ([Ca2+]o) cumulatively increased in the presence of 1 μM CCh in order to alter [Ca2+]i via NSCC (Fig. 4f). The force development was again significantly smaller in cTnT+/− mice at lower extracellular Ca2+ concentrations (P = 0.024 at 0.03 mM [Ca2+]o and P = 0.041 at 0.1 mM [Ca2+]o; n = 25 in WT vs 30 in cTnT+/− mice). These results suggest that part of the contraction, especially medicated by a small rise in [Ca2+]i, utilizes the Tn complex and/or a Tn-like complex which includes replaceable proteins of Tn subunits (Fig. 1g).
Discussion
It is widely accepted that myosin thick-filaments make a major contribution to initiating smooth muscle contraction through phosphorylation of its light chain3,4,5, on one hand, there is considerable evidence that thin filament-linked mechanisms are operating in parallel5,6,7. The present study has elucidated that cTnT plays a crucial role in the latter mechanism. Firstly, we have observed that cTnT is expressed in various smooth muscles (Fig. 1a and also see Fig. S4), and is the most abundant in the urinary bladder (Fig. 1c). A previous paper reports the expression of fast-twitch skeletal-type TnT (fTnT) in the murine aorta20. In contrast, our immunoblotting examinations have detected only cTnT in human detrusor smooth muscle, suggesting a wide variation of Tn expression among tissues and species. Furthermore, we have observed cTnT is colocalized with tropomyosin in the cytoplasm, implying that smooth muscle does not contain these proteins coincidently, but utilizes them in contraction via a thin-filament-linked signalling pathway. This finding also prompts us to consider possible detection of TnT-like proteins, for example calponin, which is known to be colocalized with tropomyosin in smooth muscle21,22. We have thus examined the sequences of the RT-PCR products, and confirmed that they are identical to the known cDNA sequences of Tns (Fig. S1).
Secondly, we have provided lines of functional evidence for the involvement of cTnT in smooth muscle contraction. In chemically permeabilized detrusor strips of humans, in which cTnT alone is detected in immunoblotting, application of both cTnI and cTnC causes significant potentiation of Ca2+-mediated contraction. Also, when cTnT content is genetically reduced (in cTnT+/− mice), the Ca2+-force relationship is shifted toward greater [Ca2+]i. In line with this observation, i.e. attenuation of [Ca2+]i sensitivity, muscarinic agonists induced contractions of smaller amplitude in intact detrusor strips of cTnT+/− mice at low extracellular Ca2+ concentrations ([Ca2+]o). Together, these results indicate that the Tn complex and/or a Tn complex-like system involving TnT make a substantial contribution to smooth muscle contraction.
In smooth muscle, [Ca2+]i is thought to be ~100 nM in basal conditions, and rises to 300 nM-1.5 μM in response to physiological stimuli including neurotransmitters and membrane depolarizations23,24. In this [Ca2+]i range, the force development of chemically permeabilized smooth muscle preparations in cTnT+/− mice was ~17–43% smaller than in WT mice (Fig. 4). cTnT is partially reduced (to ~50%) in cTnT+/− mice (Fig. 4B). Also, it is known that the TnT subtypes, i.e. cTnT/sTnT/fTnT are replaceable to form a Tn complex in reconstitution studies25. Therefore, in smooth muscle preparations of cTnT+/− mice, skeletal muscle subtypes of TnT, if any exists as for human smooth muscle, are likely to play a role. The actual contribution of thin-filament regulation via TnT to smooth muscle contraction is, thus, expected to exceed twice the apparent difference of the [Ca2+]i-tension relationship between WT and cTnT+/− mice.
Using permeabilized smooth muscle preparations, we have also successfully constructed the Tn system itself. Namely, the addition of exogenous cTnI followed by cTnC26 significantly potentiated the Ca2+-mediated force development (Fig. 3c). This implies that among Tn subunits, cTnT is predominant compared to cTnI and cTnC in smooth muscle, and that cTnT is already assembled with thin-filaments ready to convert the tropomyosin conformation, i.e. to cause thin-filament-linked contraction, when it receives the two other components of Tn.
In striated muscles, the composition of Tn subunits and subtypes is known to alter during development and aging, and under pathological conditions27. Also, it is known that impaired RNA splicing and mutations of genes coding for Tns and related proteins such as tropomyosin, cause myopathies2,16. Such changes are likely to occur in numerous smooth muscles thereby altering contractility due to the Tn/Tn-like system. In addition, unidentified mutations of Tns, which mainly modulate smooth muscle contractility, may exist. Conversely, pharmacological and/or genetic treatments targeting the Tn/Tn-like system could be developed to overcome numerous diseases related to smooth muscle dysfunction, such as intractable hypertension, bronchial asthma, overactive bladder, intestinal hypomotility and so on. Furthermore, in the heart, some specific changes in the composition of Tn subtypes (expression of sTnI), affect the energetic cost of contraction and promote glycolysis28. Similar mechanisms might underlie characteristic features of smooth muscle contraction, such as the low energy cost, and the high rate of aerobic glycolysis29,30.
In conclusion, this study has elucidated the expression of Tns in smooth muscle and modulation of contractility via a Tn/Tn-like system, indicating that both thin and thick-filament-linked mechanisms are co-operating in Ca2+-mediated smooth muscle contraction (Fig. 1g). We assume that increases of [Ca2+]i in the physiological range (i.e. 300 nM~1.5 μM) preferably utilize the thin-filament-linked mechanism including cTnT. On the other hand, the thick-filament-linked mechanism appears to make a major contribution to pharmacomechanical coupling, such as contractions induced by neurotransmitters and hormones which activate MLCK at low [Ca2+]i, and pathological contractions which increase [Ca2+]i to extremely high concentrations. In order to develop new therapies, it merits exploring modulators of smooth muscle contractility via Tn/Tn-like systems.
Methods
Smooth muscle specimens
Detrusor smooth muscle specimens were obtained from humans and mice. Human detrusor was obtained from 7 males and 5 females with a mean age of 68.9±6.9 years undergoing cystectomy due to bladder cancer. Voiding functions were almost normal. All patients provided informed written consent approved by the Kyushu University Hospital Ethical Committee.
Mice were treated ethically. All procedures were approved by the Institutional Animal Care and Use Committee. Wild-type (WT = cTnT+/+) and cTnT+/− mice (~12 weeks after birth) were sacrificed by cervical dislocation after deeply anaesthetising with diethyl ether, and the urinary bladder was quickly dissected. Since the homozygous cTnT gene knockout (cTnT−/−) is lethal, heterozygous cTnT knockout (cTnT+/−) mice known to have a moderate decrease in cTnT expression despite having a normal life span31, were used in this study.
Genotyping was carried out 4 weeks after birth using total RNA (tRNA) extracted from the tail. PCR primers for the cTnT-deficient allele were: (+) 5′-GATTGCACGCAGGTTCTCCG; (–) 5′-CAAGAAGGCGATAGAAGGCG. In Fig. 4a, amplicons of 0.76-kbp indicate the mutant band to distinguish WT and cTnT+/− mice in genotyping after birth.
Biochemical, immunohistochemical and physiological examinations were carried out using detrusor in which the urothelial mucosa and connective tissue were carefully removed under a binocular microscope.
mRNA expression
Total RNA (tRNA) was extracted with Torizol reagent (Invitrogen) from detrusor smooth muscle in the human urinary bladder. Also, human tRNA samples of several smooth muscle tissues (the trachea, aorta, stomach small intestine, colon, urinary bladder) and the heart were purchased from Clontech.
The expression of cTnT, cTnI, cTnC and GAPDH mRNAs were examined by reverse transcription-polymerase chain reaction (RT-PCR)32. After treatment with RQ1 DNase (Promega), 1 μg of the tRNA was subjected to a RT reaction in a 10 μL reaction volume. RT was performed using random hexamer (12.5 pmol) and MMLV reverse transcriptase (100 U), according to the manufacturer's instructions (Promega). Then, 1 μl of RT product was used as a cDNA template for the PCR reaction. The resultant PCR amplicons were subcloned into pCR2.1 for TA cloning (Invitrogen) and DNA sequencing was carried out. The sequences of cTnT, cTnC and cTnI amplicons are shown in Fig. S2, together with the primers used.
In commercial tRNA samples, and tRNA from detrusor smooth muscle of WT and cTnT+/− mice, mRNAs of Tn subunits were quantified using real-time PCR. tRNA (2 μg) was subject to an RT reaction to produce 20 μl of cDNA template. Then, the template was diluted 1:50 (v/v), and 4.5 μl of the diluted sample was mixed with 0.5 μl TaqMan probe (in total 10 μl reaction mixture). The TaqMan probes used were (ABI catalogue number): Hs02758991_g1 for human and mouse GAPDH; Hs00165960_m1 (TNNT2) for human TnT type 2 (cardiac); Hs00165957_m1 (TNNI3) for human TnI type 3 (cardiac); Hs00268524_m1 (TNNC1) for human TnC type 1 (slow cardiac); Mm01290252_g1 (TNNT2) for mouse TnT type 2 (cardiac). The mRNA expression of cardiac troponins in each smooth muscle tissue was compensated by that of GAPDH.
Murine tRNA was also collected from several tissues, and the expression of cTnT was examined (Fig. S3).
Immunoblotting
Samples were separated by 12% SDS-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to a polyvinylidene difluoride membrane using a semi-dry transfer system (1 hr, 15 V). After blocking with 5% skimmed milk for 1 hr, the membrane was probed with a first antibody. The membrane was washed three times and incubated with horseradish peroxidase-conjugated anti-mouse IgG (BioRad) for 1 hr. Immunoreactive proteins on the membrane were visualized by treatment with a detection reagent (LumiGLO, Cell Signaling Technology).
The monoclonal anti-cardiac TnT (cTnT) antibody was purchased from Hytest, the monoclonal anti-cardiac TnI (cTnI) antibody was from Fitzgerald, the monoclonal anti-slow muscle and-cardiac TnC (cTnC) antibody was from Abnova, while the monoclonal anti-tropomyosin antibody was from Sigma (St Louis, MO, USA).
Immunohistochemistry
Colocalization of TnT and tropomyosin was examined in thin sections (Fig. 2a, b). Formalin-fixed and paraffin-embedded detrusor smooth muscle was cut into small sections of ~3 μm thick. The sections were deparaffinized, dehydrated, and pretreated for heat-based antigen retrieval using 10 nM citrate buffer solution (pH 6.0) for 20 min in an autoclave. After blocking with 5% nonfat milk, the sections were incubated with monoclonal anti-cTnT antibody (1:100 in PBS containing 5% BSA and 0.1% Tween 20) overnight at 4°C. Inner peroxidase activity was blocked with methanol containing 1% H2O2, and the sections were incubated with an HRP-labeled anti-mouse secondary antibody, HistoFine (DAKO, Glostrup, Denmark) for 30 min. cTnT expression was visualized with the peroxidase stain DAB kit (Nacalai Tesque, Kyoto, Japan). Cell nuclei were counterstained with hematoxylin. Immunofluorescence staining was also performed. The sections treated with primary antibody were incubated with a biotinylated goat anti-mouse IgG secondary antibody (1:200; Vector Laboratories, Burlingame, CA). Thereafter, r-phycoerythrin (PE)-conjugated streptavidin (1:100; BD Biosciences, San Diego, CA) was applied, followed by 4,6-diamidino-2-phenylindole (DAPI) for counterstaining the nuclei. Immunofluorescence images were acquired using a fluorescence microscope (BZ-8000, Keyence, Osaka, Japan).
Co-localization of cTnT and tropomyosin was also examined in cultured detrusor cells (Fig. 2c–l). Detrusor tissues obtained from patients were minced into small pieces and incubated for 1 h in Dulbecco's modified Eagle's medium (DMEM) (Sigma) containing 1 mg/ml collagenase type I (Worthington, Lakewood, NJ) and 10 U/ml elastase (Wako, Osaka, Japan). After digestion, isolated cells were washed with DMEM containing 10% FBS, 100 μg/ml streptomycin, 100 units/ml penicillin, and 50 μg/ml ascorbic acid, and kept in a CO2 incubator at 37°C. Cultured cells of 6–10 passages were fixed in 4% formaldehyde and permeabilized in PBS containing 0.1% TritonX-100. Then cTnT and tropomyosin were labeled with their monoclonal antibodies (Hytest, Turku, Finland; Sigma St Louis, MO, USA) using a Zenon mouse IgG labeling kit (Invitrogen) according to the manufacturer's protocol. Cell nuclei were stained with DAPI. Negative controls of cTnT and tropomyosin were obtained from two types of human urinary bladder transitional cell carcinoma (UMUC3 and TCCSuP: left and right panels in Fig. S5, respectively). After permeabilization with Triton X-100, the same anti-cTnT and anti-tropomyosin antibodies were used to stain the cultured cells.
Force measurement
Small strips (~0.5 mm wide and 1.0 mm long) of detrusor were prepared for force measurement. Small strips were initially mounted between two tungsten wires, one of which was fixed and the other was attached to a force transducer (UL2; Minebea, Osaka, Japan), at the centre of a Perspex block in a 60 μl drop of physiological saline solution (PSS). The ‘normal’ physiological salt solution (PSS) had the following composition (mM): NaCl 138, KCl 6, CaCl2 2.4, glucose 12 and HEPES/Tris (pH 7.3). Incubating solutions were changed by moving the Perspex block.
After stable responses had been achieved by exposure to 100 mM K+ and/or 10 μM Carbachol (CCh), detrusor strips were moved into relaxing solutions for a few minutes. Then, the cell membrane was permeabilised with β-escin33 with some modifications. The composition of the relaxing solution was (mM): potassium methansulphonate 100, Na2ATP 2.2, MgCl2 3.38, ethyleneglycol-bis (β-aminoethylether)-N',N',N',N'-tetra acetic acid (EGTA) 10, creatine phosphate 10, Tris-maleate 20 (pH 7.2). The incubation time was 20–30 min for 20–40 μM β-escin. Activating solutions containing various ionized Ca2+ concentrations were made by adding appropriate amounts of CaCl2 to the relaxing solution, using the Ca2+-EGTA binding constant of 106/M 34. Ca2+-dependence of force development was examined at room temperature. The force became maximal at ~10 μM, as previously reported in chemically permeabilised smooth muscles33,35.
To examine the effect of exogenous troponins, human cTnI and cTnC were cloned and expressed in Escherichia coli BL21(DE3). Protein purification was carried out as described previously36.
In some experiments, Ca2+-dependence of tension development was examined in intact detrusor strips (without permeabilization) in the presence of CCh37. The application of exogenous cTnI and cTnC had little effect in intact muscle preparations (Fig. S6). On the other hand, in chemically permeabilized detrusor strips, the application of cTnI alone suppressed Ca2+-mediated tension development (Fig. 3b), as previously observed38.
Statistics
Numerical data are expressed as mean ± s.e. Significant differences were evaluated by two-tail, paired and unpaired t-tests. Single and double asterisks represent the probability (P) < 0.05 and < 0.01, respectively.
Author Contributions
S.K., N.S., H.M., S.M., N.S. and T.S. performed experiments on force development, and analysed the data. F.T.-Y., M.M. and H.A. performed PCR and western blot. M.O. and Y.Y. contributed to immunohistochemistry. S.N. and S.K. designed experiments, prepared smooth muscle specimens and performed PCR. S.N., S.K., S.Naito and M.H. wrote the manuscript.
Supplementary Material
Supplemental Figures
Acknowledgments
The authors are grateful to Professor Joseph F. Clark (University of Cincinnati, USA) for stimulating discussion. This work was partly supported by Grant-in-Aid for Scientific Research from the Japan Society for the Promotion Science.
References
- Ebashi S. & Endo M. Calcium ion and muscle contraction. Prog. Biophys. Mol. Biol. 18, 123–183 (1968). [DOI] [PubMed] [Google Scholar]
- Ohtsuki I. & Morimoto S. Troponin: regulatory function and disorders. Biochem. Biophys. Res. Commun. 369, 62–73 (2008). [DOI] [PubMed] [Google Scholar]
- Dillon P. F., Aksoy M. O., Driska S. P. & Murphy R. A. Myosin phosphorylation and the cross-bridge cycle in arterial smooth muscle. Science 211, 495–497 (1981). [DOI] [PubMed] [Google Scholar]
- Ito M. & Hartshorne D. J. Phosphorylation of myosin as a regulatory mechanism in smooth muscle. Prog. Clin. Biol. Res. 327, 57–72 (1990). [PubMed] [Google Scholar]
- Kim H. R., Appel S., Vetterkind S., Gangopadhyay S. S. & Morgan K. G. Smooth muscle signalling pathways in health and disease. J. Cell. Mol. Med. 12, 2165–2180 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C. W., Pritchard K. & Marston S. B. The mechanism of Ca2+ regulation of vascular smooth muscle thin filaments by caldesmon and calmodulin. J. Biol. Chem. 262, 116–122 (1987). [PubMed] [Google Scholar]
- Kobayashi H., Inoue A., Mikawa T., Kuwayama H., Hotta Y., Masaki T. & Ebashi S. Isolation of cDNA for bovine stomach 155 kDa protein exhibiting myosin light chain kinase activity. J. Biochem. 112, 786–789 (1992). [DOI] [PubMed] [Google Scholar]
- Ansari S., Alahyan M., Marston S. B. & El-Mezgueldi M. Role of caldesmon in the Ca2+ regulation of smooth muscle thin filaments: evidence for a cooperative switching mechanism. J. Biol. Chem. 283, 47–56 (2008). [DOI] [PubMed] [Google Scholar]
- Jin J. P., Zhang Z. & Bautista J. A. Isoform diversity, regulation and functional adaptations of troponin and calponin. Crit. Rev. Eukar. Gene Expr. 18, 93–124 (2008). [DOI] [PubMed] [Google Scholar]
- Rozenblum G. T. & Gimona M. Calponins: adaptable modular regulators of the actin cytoskeleton. Int. J. Biochem. Cell Biol. 40, 1990–1995 (2008). [DOI] [PubMed] [Google Scholar]
- Chatterjee M. & Tejada M. Phorbol ester-induced contraction in chemically skinned vascular smooth muscle. Am. J. Physiol. 251, C356–361 (1986). [DOI] [PubMed] [Google Scholar]
- Fulginiti J. 3rd, Singer H. A. & Moreland R. S. Phorbol ester-induced contractions of swine carotid artery are supported by slowly cycling crossbridges which are not dependent on calcium or myosin light chain phosphorylation. J. Vasc. Res. 30, 315–322 (1993). [DOI] [PubMed] [Google Scholar]
- Walsh M. P., Andrea J. E., Allen B. G., Clément-Chomienne O., Collins E. M. & Morgan K. G. Smooth muscle protein kinase C. Can. J. Physiol. Pharmacol. 72, 1392–1399 (1994). [DOI] [PubMed] [Google Scholar]
- Su X., Smolock E. M., Marcel K. N. & Moreland R. S. Phosphatidylinositol 3-kinase modulates vascular smooth muscle contraction by calcium and myosin light chain phosphorylation-independent and -dependent pathways. Am. J. Physiol. Heart Circ. Physiol. 286, H657–666 (2004). [DOI] [PubMed] [Google Scholar]
- Scruggs S. B. & Solaro R. J. The significance of regulatory light chain phosphorylation in cardiac physiology. Arch. Biochem. Biophys. 510, 129–134 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochala J. Thin filament proteins mutations associated with skeletal myopathies: defective regulation of muscle contraction. J. Mol. Med. (Berl) 86, 1197–1204 (2008). [DOI] [PubMed] [Google Scholar]
- Ngai P. K., Scott-Woo G. C., Lim M. S., Sutherland C. & Walsh M. P. Activation of smooth muscle myosin Mg2+-ATPase by native thin filaments and actin/tropomyosin. J. Biol. Chem. 262, 5352–5359 (1987). [PubMed] [Google Scholar]
- Smillie L. B. Tropomyosin. In Biochemistry of smooth muscle contraction. M. Bárány, ed. (San Diego, California: Academic Press), pp. 63–75 (1996).
- Kajioka S., Nakayama S., Asano H. & Brading A. F. Involvement of ryanodine receptors in muscarinic-receptor-mediated membrane current oscillation in urinary bladder smooth muscle. Am. J. Physiol. Cell Physiol. 288, C100–108 (2005). [DOI] [PubMed] [Google Scholar]
- Moran C. M., Garriock R. J., Miller M. K., Heimark R. L., Gregorio C. C. & Krieg P. A. Expression of the fast twitch troponin complex, fTnT, fTnI and fTnC, in vascular smooth muscle. Cell Motil. Cytoskeleton 65, 652–661 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi K., Hiwada K. & Kokubu T. Vascular smooth muscle calponin. A novel troponin T-like protein. Hypertension 11, 620–626 (1988). [DOI] [PubMed] [Google Scholar]
- Walsh M. P., Carmichael J. D. & Kargacin G. J. Characterization and confocal imaging of calponin in gastrointestinal smooth muscle. Am. J. Physiol. 265, C1371–1378 (1993). [DOI] [PubMed] [Google Scholar]
- Karaki H., Ozaki H., Hori M., Mitsui-Saito M., Amano K., Harada K., Miyamoto S., Nakazawa H., Won K. J. & Sato K. Calcium movements, distribution, and functions in smooth muscle. Pharmacol. Rev. 49, 157–230 (1997). [PubMed] [Google Scholar]
- Wray S., Burdyga T. & Noble K. Calcium signalling in smooth muscle. Cell Calcium 38, 397–407 (2005). [DOI] [PubMed] [Google Scholar]
- Liou Y. M. & Chang J. C. Differential pH effect on calcium-induced conformational changes of cardiac troponin C complexed with cardiac and fast skeletal isoforms of troponin I and troponin T. J. Biochem. 136, 683–692 (2004). [DOI] [PubMed] [Google Scholar]
- Rűegg J. C., Zeugner C., van Erk J., Kay C. M. & Hodges R. S. Inhibition of TnI-TnC interaction and contraction of skinned muscle fibres by the synthetic peptide TnI. Pflűgers Arch. 414, 430–436 (1989). [DOI] [PubMed] [Google Scholar]
- Anderson P. A., Greig A., Mark T. M., Malouf N. N., Oakeley A. E., Ungerleider R. M., Allen P. D. & Kay B. K. Molecular basis of human cardiac troponin T isoforms expressed in the developing, adult, and failing heart. Circ. Res. 76, 681–686 (1995). [DOI] [PubMed] [Google Scholar]
- Pound K. M., Arteaga G. M., Fasano M., Wilder T., Fischer S. K., Warren C. M., Wende A. R., Farjah M., Abel E. D., Solaro R. J. & Lewandowski E. D. Expression of slow skeletal TnI in adult mouse hearts confers metabolic protection to ischemia. J. Mol. Cell. Cardiol. 51, 236–243 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark J. F., Kemp G. J. & Radda G. K. The creatine kinase equilibrium, free [ADP] and myosin ATPase in vascular smooth muscle cross-bridges. J. Theor. Biol. 173, 207–211 (1995). [DOI] [PubMed] [Google Scholar]
- Lynch R. M. & Paul R. J. Compartmentation of carbohydrate metabolism in vascular smooth muscle. Am. J. Physiol. 252, C328–334 (1987). [DOI] [PubMed] [Google Scholar]
- Nishii K., Morimoto S., Minakami R., Miyano Y., Hashizume K., Ohta M., Zhan D. Y., Lu Q. W. & Shibata Y. Targeted disruption of the cardiac troponin T gene causes sarcomere disassembly and defects in heartbeat within the early mouse embryo. Dev. Biol. 322, 65–73 (2008). [DOI] [PubMed] [Google Scholar]
- Kajioka S., Nakayama S., Asano H., Seki N., Naito S. & Brading A. F. Levcromakalim and GDP activate small conductance KATP channels with the composition of Kir6.1/SUR2A in pig detrusor smooth muscle cells: Uncoupling of cAMP signal pathways. J. Pharmacol. Exp. Ther. 327, 114–123 (2008). [DOI] [PubMed] [Google Scholar]
- Durlu-Kandilci N. T. & Brading A. F. Involvement of Rho kinase and protein kinase C in carbachol-induced calcium sensitization in beta-escin skinned rat and guinea-pig bladders. Br. J. Pharmacol. 148, 376–384 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saida K. & Nonomura Y. Characteristics of Ca2+- and Mg2+-induced tension development in chemically skinned smooth muscle fibers. J. Gen. Physiol. 72, 1–14 (1978). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iino M. Tension responses of chemically skinned fibre bundles of the guinea-pig taenia caeci under varied ionic environments. J. Physiol. 320, 449–467 (1981). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanaga F., Morimoto S. & Ohtsuki I. Ca2+ sensitization and potentiation of the maximum level of myofibrillar ATPase activity caused by mutations of troponin T found in familial hypertrophic cardiomyopathy. J. Biol. Chem. 274, 8806–8812 (1999). [DOI] [PubMed] [Google Scholar]
- Baba K., Satake T., Takagi K. & Tomita T. Effects of verapamil on the response of the guinea-pig tracheal muscle to carbachol. Br. J. Pharmacol. 88, 441–449 (1986). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe M., Yoshino Y. & Morimoto S. Troponin I inhibitory peptide suppresses the force generation in smooth muscle by directly interfering with cross-bridge formation. Biochem. Biophys. Res. Commun. 307, 236–240 (2003). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figures