In this issue of Diabetes, Chen et al. (1) used rodent models of type 1 diabetes and ischemia-induced retinal neovascularization to examine how the lipid-lowering drug fenofibrate may prevent progression of diabetic retinopathy. Diabetic retinopathy is the sight-threatening complication of diabetes that causes retinal microvascular dysfunction, which in turn leads to diabetic macular edema (DME), formation of exudate deposits, and microhemorrhages. In the advanced proliferative stage of diabetic retinopathy, neovascularization can result in retinal detachment and blindness. Therapeutic options for diabetic retinopathy have been limited. Until recently, intensive glycemic control, with its risks of hypoglycemic events and increased mortality, was the only known means of reducing the progression of diabetic retinopathy (2,3). Laser photocoagulation of the peripheral retinal tissue, intravitreal injection of steroids or vascular endothelial growth factor (VEGF) inhibitors, and vitrectomy can each stabilize or improve vision, but they are all invasive and are associated with various complications. Additional treatment options are needed. An orally available drug that reduces the risk of diabetic retinopathy progression without intensive glycemic control, retinal destruction, or repeated intravitreal injections would be ideal.
Type 2 diabetes is often associated with dyslipidemia characterized by elevated triglycerides, reduced HDL cholesterol, and variable LDL cholesterol. Although statins are clearly beneficial, a residual atherogenic dyslipidemia often remains (4). Fibric acid derivatives, such as fenofibrate, stimulate the peroxisome proliferator–activated receptor type α (PPARα) and lead to increased fatty acid β-oxidation, thus decreasing plasma triglyceride and LDL cholesterol levels and increasing HDL cholesterol levels (5). This makes fibrates, in combination with statins, a logical treatment for diabetic dyslipidemia. Recent large-scale clinical studies, including the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) and Action to Control Cardiovascular Risk in Diabetes (ACCORD) studies, examined the effects of fenofibrate on cardiovascular risk and diabetes complications in type 2 diabetes. Although fenofibrate failed to affect visual acuity measures, both studies showed that the drug reduced the risk of developing severe diabetic retinopathy by approximately one-third (6,7). These findings have resulted in recommendations that fenofibrate be used as an adjunct treatment for type 2 diabetic patients with nonproliferative diabetic retinopathy (8,9).
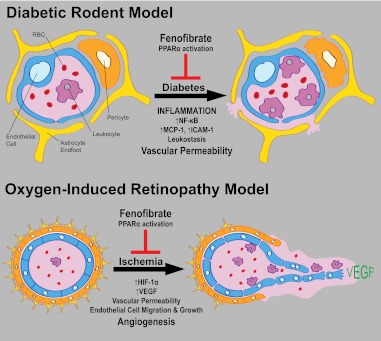
Further evaluation of fenofibrate’s impact on diabetic retinopathy progression and its mechanism of action are needed. Fenofibrate may affect diabetic retinopathy either indirectly by lowering plasma free fatty acid and triglyceride levels or directly by activating retinal PPARα (Fig. 1). PPARα agonists influence cellular physiology in many ways that might prove beneficial in diabetes complication–prone tissues (for a recent review, see ref. 10). In particular, fenofibrate provokes direct PPARα-dependent actions on inflammatory gene expression by inhibiting proinflammatory transcription factors, including nuclear factor-κB (NF-κB) (10). Relevant to the reduced risk of macular edema in diabetic retinopathy is the observation that fenofibrate inhibits endothelial cell layer permeability caused by oxygen-glucose deprivation in a PPARα-dependent manner (11). Chen et al. (1) examined the effects of fenofibrate on vascular leakiness in type 1 diabetic rat and mouse models. They found that orally administered fenofibrate abrogated diabetes-induced vascular permeability. Supplemental data suggest that the effect of fenofibrate was not accompanied by significant changes in plasma triglyceride levels. To determine whether fenofibrate acted directly on the retina, they administered the drug by intravitreal injection and found similar effects on vascular permeability. The ability to inhibit permeability coincided with the inhibition of diabetes-induced vascular adherence of leukocytes (leukostasis), as well as decreased expression of NF-κB, monocyte chemoattractant protein (MCP)-1, and intracellular adhesion molecule (ICAM)-1 in the diabetic retina. These results support earlier studies showing that fenofibrate inhibits cytokine-induced NF-κB activity, MCP-1, and ICAM-1 expression, as well as monocyte adhesion in endothelial cultures (12–15). Although there is no conclusive evidence for leukostasis as the direct cause of increased retinal vascular permeability in diabetic retinopathy, the results suggest that anti-inflammatory effects of fenofibrate diminish monocyte attraction and adherence to the retinal endothelium, thus preventing vascular damage and leakiness.
FIG. 1.
The effects of fenofibrate treatment on experimental models of diabetic retinopathy. In type 1 diabetic rodent models, fenofibrate blocked vascular permeability in a PPARα-dependent fashion. This coincided with inhibition of the inflammatory processes including NF-κB activation, expression of MCP-1 and ICAM-1, and inhibition of leukostasis. Other studies have shown that the death of retinal pericytes contributes to vascular dysfunction in diabetic retinopathy. In the oxygen-induced retinopathy model, which mimics proliferative diabetic retinopathy changes, fenofibrate blocks angiogenesis in a PPARα-dependent fashion. This coincides with inhibition of HIF-1α upregulation and expression of VEGF. RBC, red blood cell.
There is precedent to suggest that fenofibrate could also inhibit neovascularization in proliferative diabetic retinopathy by acting directly on endothelial cells. In previous studies, fenofibrate reduced endothelial cell expression of VEGF receptor 2 and hindered the migration of endothelial cells toward VEGF (16,17). Since diabetic rodent models do not exhibit proliferative diabetic retinopathy, Chen et al. used a rat model of oxygen-induced retinopathy to test fenofibrate’s ability to influence retinal neovascularization. In this model, intravitreal injection of fenofibrate significantly reduced ischemia-induced angiogenesis. Rather than blocking the effects of VEGF on endothelial cells, fenofibrate attenuated expression of VEGF and hypoxia-inducible factor (HIF)-1α in the ischemic retina. Even so, the authors also showed that fenofibrate inhibited tube formation and basal migration of cultured retinal endothelial cells. Their results suggest that fenofibrate might reduce the risk of progression to proliferative diabetic retinopathy through inhibition of VEGF expression or by direct inhibition of the endothelial cell functions required for angiogenesis. The authors also demonstrated that a structurally unrelated PPARα agonist, GW590785, inhibited retinal permeability in diabetic rats to the same extent as fenofibrate. In addition, fenofibrate showed no ability to reduce retinal permeability or to inhibit retinal VEGF expression in PPARα knockout mice. Thus, these results establish the role of PPARα in mediating the blockade by fenofibrate of diabetes-associated endothelial activation, vascular leakiness, and ischemia-induced retinal VEGF expression.
The results of Chen et al. (1) are likely to heighten interest in fenofibrate as an adjunct therapy in diabetic patients. In particular, the direct mechanisms potentially explaining fenofibrate’s ability to prevent vascular dysfunction in diabetic retinopathy suggest a mode of action that is independent of systemic fatty acid oxidation. Fenofibrate might prove beneficial in the absence of hypertriglyceridemia or dyslipidemia, and its efficacy may not correlate with the normalization of these biomarkers. Their results also suggest that the drug may be efficacious in type 1 diabetes as well as type 2 diabetes patients. The data presented in this new report indicate that fenofibrate’s direct anti-inflammatory effects are key to vascular protection in diabetic retinopathy. Future studies will need to examine how fenofibrate blocks the expression or activation NF-κB and confirm that the expression of chemoattractants and cellular adhesion molecules in the diabetic retina are primarily directed by this transcription factor. Toward the former issue, fenofibrate was previously found to inhibit endothelial NF-κB activation through stimulation of AMP-activated protein kinase (AMPK) (13,18). Further studies will also need to determine the mechanism by which fenofibrate prevents ischemia-induced HIF-1α and VEGF expression. One previous study (19) included supplementary data showing that fenofibrate diminished the basal expression of VEGF by tumor cell lines. Incongruously, other studies found AMPK to be necessary for upregulation of HIF-1α in response to hypoxia and demonstrated that fenofibrate increased endothelial cell VEGF expression in an AMPK-dependent manner (20,21). These studies demonstrate the need to examine the effect of fenofibrate on vitreous levels of VEGF in diabetic retinopathy patients and to determine if fenofibrate influences the efficacy or required frequency of anti-VEGF treatments for diabetic retinopathy. Regardless of the precise mechanism of action, it was serendipitous that an oral therapeutic agent targeting systemic fatty acid metabolism was associated with the decreased risk of diabetic retinopathy progression, seemingly due to the direct actions of the drug within the diabetic retina. This development highlights the utility of complementary clinical and basic science research to facilitate advances in diabetic retinopathy treatment.
ACKNOWLEDGMENTS
This work was support by grants from the National Institutes of Health (R01-EY020582, R01-EY007739, P30-EY07003, DP3-DK094292) and from the JDRF (JDRFI-4-2007-231).
No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying original article, p. 261.
REFERENCES
- 1.Chen Y, Hu Y, Lin M, et al. Therapeutic effects of PPARα agonists on diabetic retinopathy in type 1 diabetes models. Diabetes 2013;62:261–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lachin JM, Genuth S, Nathan DM, Zinman B, Rutledge BN. Effect of glycemic exposure on the risk of microvascular complications in the Diabetes Control and Complications Trial–revisited. Diabetes 2008;57:995–1001 [DOI] [PubMed] [Google Scholar]
- 3.Hemmingsen B, Lund SS, Gluud C, et al. Intensive glycaemic control for patients with type 2 diabetes: systematic review with meta-analysis and trial sequential analysis of randomised clinical trials. BMJ 2011;343:d6898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wanner C, Krane V. Recent advances in the treatment of atherogenic dyslipidemia in type 2 diabetes mellitus. Kidney Blood Press Res 2011;34:209–217 [DOI] [PubMed] [Google Scholar]
- 5.Kraja AT, Province MA, Straka RJ, Ordovas JM, Borecki IB, Arnett DK. Fenofibrate and metabolic syndrome. Endocr Metab Immune Disord Drug Targets 2010;10:138–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chew EY, Ambrosius WT, Davis MD, et al. Effects of medical therapies on retinopathy progression in type 2 diabetes. N Engl J Med 2010;363:233–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keech AC, Mitchell P, Summanen PA, et al. ; FIELD study investigators. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet 2007;370:1687–1697 [DOI] [PubMed] [Google Scholar]
- 8.Wong TY, Simó R, Mitchell P. Fenofibrate—a potential systemic treatment for diabetic retinopathy? Am J Ophthalmol 2012;154:6–12 [DOI] [PubMed] [Google Scholar]
- 9.Wright AD, Dodson PM. Medical management of diabetic retinopathy: fenofibrate and ACCORD eye studies. Eye (Lond) 2011;25:843–849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hiukka A, Maranghi M, Matikainen N, Taskinen MR. PPARalpha: an emerging therapeutic target in diabetic microvascular damage. Nat Rev Endocrinol 2010;6:454–463 [DOI] [PubMed] [Google Scholar]
- 11.Mysiorek C, Culot M, Dehouck L, et al. Peroxisome-proliferator-activated receptor-alpha activation protects brain capillary endothelial cells from oxygen-glucose deprivation-induced hyperpermeability in the blood-brain barrier. Curr Neurovasc Res 2009;6:181–193 [DOI] [PubMed] [Google Scholar]
- 12.Huang WP, Yin WH, Chen JW, Jen HL, Young MS, Lin SJ. Fenofibrate attenuates endothelial monocyte adhesion in chronic heart failure: an in vitro study. Eur J Clin Invest 2009;39:775–783 [DOI] [PubMed] [Google Scholar]
- 13.Okayasu T, Tomizawa A, Suzuki K, Manaka K, Hattori Y. PPARalpha activators upregulate eNOS activity and inhibit cytokine-induced NF-kappaB activation through AMP-activated protein kinase activation. Life Sci 2008;82:884–891 [DOI] [PubMed] [Google Scholar]
- 14.Rival Y, Benéteau N, Taillandier T, et al. PPARalpha and PPARdelta activators inhibit cytokine-induced nuclear translocation of NF-kappaB and expression of VCAM-1 in EAhy926 endothelial cells. Eur J Pharmacol 2002;435:143–151 [DOI] [PubMed] [Google Scholar]
- 15.Xu X, Otsuki M, Saito H, et al. PPARalpha and GR differentially down-regulate the expression of nuclear factor-kappaB-responsive genes in vascular endothelial cells. Endocrinology 2001;142:3332–3339 [DOI] [PubMed] [Google Scholar]
- 16.Goetze S, Eilers F, Bungenstock A, et al. PPAR activators inhibit endothelial cell migration by targeting Akt. Biochem Biophys Res Commun 2002;293:1431–1437 [DOI] [PubMed] [Google Scholar]
- 17.Meissner M, Stein M, Urbich C, et al. PPARalpha activators inhibit vascular endothelial growth factor receptor-2 expression by repressing Sp1-dependent DNA binding and transactivation. Circ Res 2004;94:324–332 [DOI] [PubMed] [Google Scholar]
- 18.Tomizawa A, Hattori Y, Inoue T, Hattori S, Kasai K. Fenofibrate suppresses microvascular inflammation and apoptosis through adenosine monophosphate-activated protein kinase activation. Metabolism 2011;60:513–522 [DOI] [PubMed] [Google Scholar]
- 19.Panigrahy D, Kaipainen A, Huang S, et al. PPARalpha agonist fenofibrate suppresses tumor growth through direct and indirect angiogenesis inhibition. Proc Natl Acad Sci USA 2008;105:985–990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim J, Ahn JH, Kim JH, et al. Fenofibrate regulates retinal endothelial cell survival through the AMPK signal transduction pathway. Exp Eye Res 2007;84:886–893 [DOI] [PubMed] [Google Scholar]
- 21.Lee M, Hwang JT, Lee HJ, et al. AMP-activated protein kinase activity is critical for hypoxia-inducible factor-1 transcriptional activity and its target gene expression under hypoxic conditions in DU145 cells. J Biol Chem 2003;278:39653–39661 [DOI] [PubMed] [Google Scholar]