Abstract
The abrupt cessation of effective cardiac function due to an aberrant heart rhythm can cause sudden and unexpected death at any age, a syndrome called sudden cardiac death (SCD). Annually, more than 300,000 cases of SCD occur in the United States alone, making this a major public health concern. Our current understanding of the mechanisms responsible for SCD has emerged from decades of basic science investigation into the normal electrophysiology of the heart, the molecular physiology of cardiac ion channels, fundamental cellular and tissue events associated with cardiac arrhythmias, and the molecular genetics of monogenic disorders of heart rhythm. This knowledge has helped shape the current diagnosis and treatment of inherited arrhythmia susceptibility syndromes associated with SCD and has provided a pathophysiological framework for understanding more complex conditions predisposing to this tragic event. This Review presents an overview of the molecular basis of SCD, with a focus on monogenic arrhythmia syndromes.
Introduction
When a person dies suddenly and unexpectedly from a suspected cardiovascular cause, the term sudden cardiac death (SCD) is used to classify the mortal event. SCD is frequently caused by an abrupt change in heart rhythm (arrhythmia), most often ventricular tachycardia (VT) or ventricular fibrillation (VF), that impairs cardiac pumping, thereby depriving vital organs of oxygenated blood. A brief episode of VT or VF may cause only momentary loss of consciousness (syncope), but death is the inevitable result of sustained VF in the absence of emergent medical care. Estimates of the annual SCD incidence vary but are generally in the range of 50–100 per 100,000 persons in industrialized nations (1). In the United States, previous estimates have been as high as 450,000 deaths per year (2), representing a large fraction of total mortality due to heart disease and a substantial public health burden. These statistics largely reflect adult deaths in the setting of ischemic heart disease or heart failure, but children can also be susceptible to SCD in the context of certain genetic disorders.
Understanding the root causes of SCD has been an important research endeavor for several decades, and much progress has been made in defining the cellular, molecular, and genetic basis for ventricular arrhythmogenesis, the main pathophysiological provocateur of SCD (3). Mendelian (i.e., monogenic) syndromes predisposing to life-threatening ventricular arrhythmias in young adults and children are genetically heterogeneous, with more than 25 genes identified so far (Table 1). Molecular mechanisms related to these conditions involve membrane ion channels important for cardiomyocyte electrogenesis or regulation of intracellular Ca2+ homeostasis. By contrast, the genetic risk for SCD in older adults is more complex, with few if any unifying hypotheses about molecular mechanisms, although some overlap is observed with susceptibility to monogenic arrhythmia. Furthermore, the respective contributions of genetic and acquired factors to pathogenesis vary along the spectrum of age, with inborn errors having the greatest impact on SCD risk in younger subjects and acquired factors dominating risk in older subjects.
Table 1.
Genes involved in monogenic causes of SCD

This Review presents an overview of the molecular basis of SCD, with a focus on monogenic arrhythmia syndromes. The emerging picture of SCD risk as a complex genetic trait in older subjects has been reviewed elsewhere (4, 5). An initial brief summary of basic arrhythmia mechanisms at the cellular and tissue levels will provide a framework for presenting the molecular underpinnings.
Ventricular arrhythmia mechanisms
The normal initiation and orderly propagation of the cardiac impulse through the heart requires a tightly orchestrated sequence of changes in ionic currents that sum to produce the dynamic and phasic change in membrane potential referred to as the cardiac action potential (Figure 1). Abnormal properties of ionic currents can cause electrical disorder and lead to aberrant impulse generation or propagation. Consequently, rapid and sometimes chaotic electrical activity in the ventricles ensues, manifesting as either VT or VF that can lead to SCD. In a simplistic model, there are two major prerequisites for arrhythmic events: a vulnerable myocardial substrate and a trigger.
Figure 1. ECG and the cardiac action potential.

Approximate temporal relationships between surface ECG (A) and typical ventricular action potential (B). Individual ionic currents responsible for different phases of the action potential are labeled and represented schematically in (B). In the ECG (A), the P wave indicates atrial depolarization, whereas the QRS complex indicates ventricular depolarization. The T wave indicates ventricular repolarization, and the Q-T interval indicates the time for the entire ventricular depolarization and repolarization sequence to occur. The ionic events underlying a cardiac action potential are illustrated in (C) and include the depolarizing inward Na+ (INa) and calcium (ICa)currents, and the repolarizing transient outward current (ITO), and three outward potassium currents (IKr, IKs, IK1).
Myocardial conditions that increase risk for arrhythmias include structural (anatomical) and functional causes of heterogeneous conduction velocity that disrupt the normal orderly propagation of action potential waves through the ventricles (6). Heterogeneous conduction can predispose to the emergence of spiral waves, impulses that travel in a circular pattern around an anatomic barrier, as in ischemic or scarred myocardium, or around a point of reentry known as a rotor in non-ischemic and structurally normal myocardium (7). If uninterrupted, rhythmic spiral wave propagation in the ventricles will be associated with VT, but degeneration or fragmentation into smaller wavelets creates the more chaotic impulse movement associated with VF. Transmural dispersion of repolarization can also predispose to reentry. Normally, there is heterogeneity of action potential duration across the wall of the ventricles, with shorter action potentials occurring in the epicardial layer. This phenomenon arises from a more prominent epicardial transient outward current (Ito). Exaggeration of this transmural heterogeneity can create circumstances in which the fully repolarized epicardium can be reexcited by depolarized mid-myocardial and endocardial layers (8, 9).
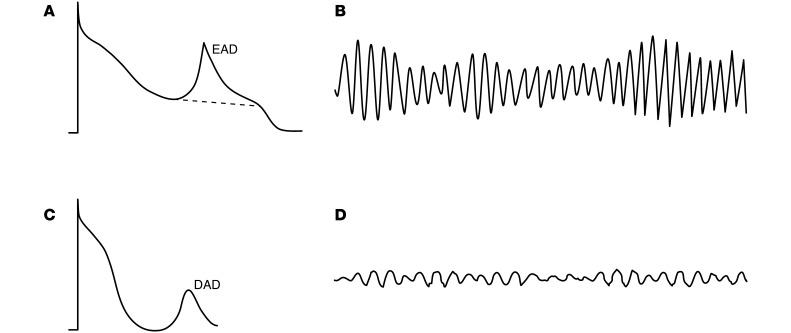
A focal ectopic impulse generated in the ventricles can trigger the initiation of spiral waves and cause reentrant arrhythmias. At the cellular level, early afterdepolarizations (EADs) or delayed afterdepolarizations (DADs) provide the most common mechanisms for ectopic excitation. EADs arise during the plateau phase of the cardiac action potential, whereas DADs emerge after completion of an action potential (Figure 2 and refs. 10, 11). Both events occur because of aberrant depolarizing ionic currents. In the case of EADs, increased activation of voltage-gated (L-type) Ca2+ channels or persistent activation of voltage-gated Na+ channels are the usual mechanisms. By contrast, DADs arise from spontaneous intracellular Ca2+ release and efflux of Ca2+ through the electrogenic Na+/Ca2+ exchanger (NCX; stoichiometry 3Na+:1Ca2+), evoking a transient inward Na+ (INa) current (12). Prolonged action potential duration increases the propensity of myocardial cells to exhibit EADs, whereas increased Ca2+ loading of the sarcoplasmic reticulum (SR) predisposes to DADs.
Figure 2. Afterdepolarizations and ventricular arrhythmias.
EADs and DADs occur due to dysregulation of depolarizing ionic currents. (A) EAD illustrated in the context of prolonged action potential duration. EADs typically result from increased activation of voltage-gated (L-type) Ca2+ channels or persistent activation of voltage-gated Na+ channels. (B) ECG from a typical polymorphic VT (also known as torsades de pointes), which is associated with EADs. (C) Illustration of a DAD arising after completion of action potential repolarization. DADs are commonly due to spontaneous intracellular Ca2+ release and efflux of Ca2+ through the electrogenic NCX (stoichiometry 3Na+:1Ca2+), which generates a a transient INa. (D) ECG of VF, which is associated with DADs.
Cardiac action potential
The generation and propagation of action potentials in heart muscle as well as excitation-contraction coupling are physiological events dependent upon a symphony of ion channels acting in concert with many associated regulatory or interacting proteins. Ion channels are ubiquitous proteins that confer selective ionic permeability to cell membranes. Voltage-gated ion channels are opened and closed by changes in membrane potential, whereas ligand-gated ion channels require binding of intracellular or extracellular molecules to open an ionic pore. Voltage-gated ion channels with selective permeability for Na+, K+, and Ca2+ ions feature prominently in normal cardiac electrophysiology and in the molecular pathogenesis of monogenic disorders predisposing to SCD (Table 1).
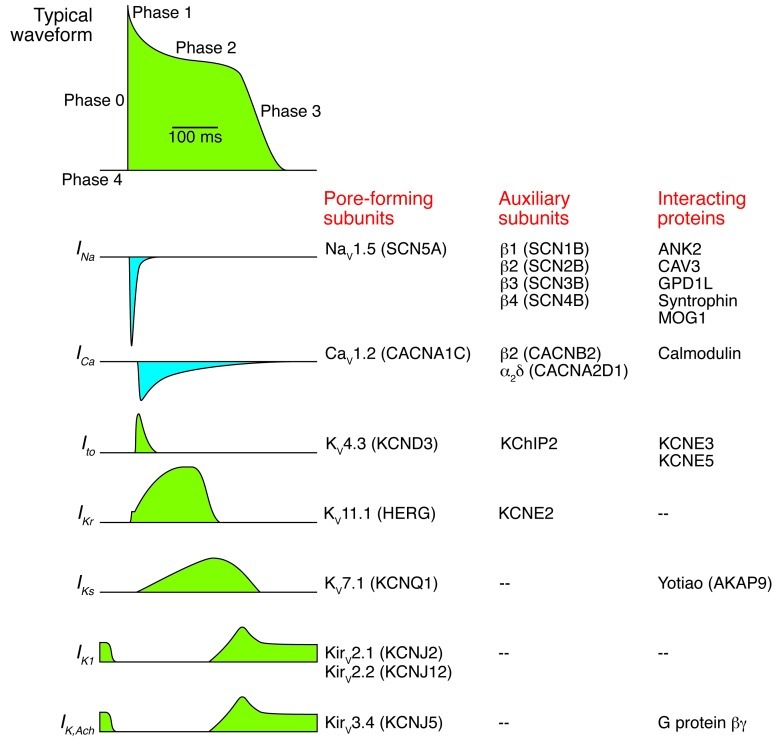
Action potentials are initiated by a localized change in membrane potential that activates voltage-gated Na+ channels, allowing rapid but transient INa and producing the typical upstroke known as phase 0 depolarization (Figure 3). In some myocytes, a rapid and transient phase 1 repolarization follows due to activation of the Ito conducted in part by fast-gating K+ channels. During phases 0 and 1, Na+ channels rapidly inactivate, while voltage-gated (L-type) Ca2+ channels activate and contribute to a long plateau of membrane depolarization. This plateau phase (phase 2) reflects a delicate balance between inward current, largely through L-type Ca2+ channels (ICa) with a small amount of residual INa, and emerging outward currents carried by K+ channels. Activation of two types of K+ currents (IKr, IKs) in concert with inactivation of Ca2+ channels tips the balance in favor of the outward current, thereby promoting phase 3 repolarization. Finally, the inward rectifying K+ current (IK1) finishes the job of repolarizing myocyte membranes. Other electrogenic transporters (NCX, Na+/K+ ATPase) are involved in maintaining intracellular ionic homeostasis in the face of large ion fluxes accompanying each action potential.
Figure 3. Ionic and molecular basis for cardiac action potential.
Left: A typical ventricular action potential waveform labeled to show different phases, and representative inward (blue) or outward (green) currents aligned temporally below. Right: Molecular components of each ionic current are listed. IK,Ach, acetylcholine-activated K+ current.
Many ion channels involved with the generation and propagation of cardiac action potentials are regulated by several factors, most notably β-adrenergic stimulation. In particular, during exercise or stress in which the sympathetic nervous system is activated (fight or flight response), heart rate acceleration requires shortening of the action potential duration, and this is accomplished in part by activating IKs through a cAMP-dependent mechanism. Sympathetic stimulation also enhances contractility of the heart, mainly through augmentation of Ca2+ influx (activation of ICa) and increased loading of the SR so that more Ca2+ can be released intracellularly during systole.
Monogenic causes of SCD
Two categories of monogenic heart disease predispose to SCD. These are genetic disorders of heart rhythm and familial cardiomyopathy. Cardiomyopathy is discussed in depth elsewhere in this Review series (13), and therefore the focus here will be on genetic arrhythmia susceptibility. Although rare, these syndromes have been tractable at the molecular level, and nearly two decades of research have uncovered molecular mechanisms that may be shared with more common acquired conditions. The genes responsible for congenital arrhythmia syndromes for the most part encode either ion channel subunits or proteins that interact with ion channels (Table 1).
Rare genetic conditions known to predispose to SCD in children and young adults include the congenital long QT syndrome (LQTS), short QT syndrome (SQTS), Brugada syndrome (BrS), idiopathic VF, and catecholaminergic polymorphic VT (CPVT). Three general mechanisms responsible for arrhythmia susceptibility have been elucidated in these disorders: abnormal repolarization (LQTS, SQTS, BrS), slow ventricular conduction (BrS), and aberrant intracellular Ca2+ homeostasis (CPVT).
Congenital LQTS.
The QT interval measured by standard surface ECG provides a surrogate measurement of the average ventricular action potential duration. Both a prolonged or shortened QT interval indicates an increased risk of life-threatening cardiac arrhythmia (14, 15). Congenital LQTS is characterized clinically by an increased risk of potentially fatal ventricular arrhythmias, especially torsades de pointes (16), manifesting as syncope, cardiac arrest, and SCD in otherwise healthy young adults and children. The syndrome is most often transmitted in families as an autosomal dominant trait (Romano-Ward syndrome) and less commonly as an autosomal recessive disease combined with deafness (Jervell and Lange-Nielsen syndrome). Autosomal dominant LQTS occurs in approximately 1 in 2,500 live births (17). LQTS is genetically heterogeneous and can be caused by mutations in several genes encoding voltage-gated K+ channel subunits (KCNQ1, KCNH2, KCNE1, KCNE2) (18–23), voltage-gated Na+ channel subunits (SCN5A, SCN4B) (24, 25), an L-type Ca2+ channel (CACNA1C) (26), inwardly rectifying K+ channels (KCNJ2, KCNJ5) (27, 28), and various channel-interacting proteins (ANK2, CAV3, AKAP9, SNTA1) (29–32).
The most common genetic subtype of LQTS, LQT1, is caused by mutations in KCNQ1, a gene encoding the pore-forming subunit of the voltage-gated K+ channel (KV7.1) responsible for IKs (20). Mutations in KCNH2, which encodes HERG (KV11.1), the voltage-gated K+ channel responsible for IKr, cause the LQT2 variant and account for the second largest proportion of LQTS cases (19, 33). Heterozygous mutations in either KCNQ1 or KCNH2 lead to loss of function and can exert dominant-negative effects on the wild-type (non-mutant) allele. Loss of function of either KV7.1 or HERG channels will reduce IKs or IKr, respectively, causing delayed repolarization and prolonged ventricular action potential duration. During sympathetic activation, failure to augment IKs during heart rate acceleration further exposes impaired repolarization and explains why LQT1 patients are most prone to arrhythmic events during exercise and emotional stress. Mutations in KCNE1 and AKAP9 (encoding the A-kinase anchor protein also known as yotiao) exert similar functional effects on IKs but are much less common (31, 33). Similarly, KCNE2 mutations associated with LQTS may disrupt HERG function and reduce IKr but sometimes only during pharmacological suppression of this current (22, 34).
In autosomal-dominant LQTS, mutations in KCNQ1 and KCNH2 may exert dominant-negative effects on the respective wild-type allele. Dominant-negative effects are best explained by the formation of dysfunctional tetrameric channel complexes with mixtures of wild-type and mutant subunits. Recessive KCNQ1 and KCNE1 mutations are responsible for Jervell and Lange-Nielsen syndrome (21, 23, 35) but do not exhibit dominant-negative effects, most likely because mutant proteins are not stable or do not form heteromultimers with wild-type subunits.
Impaired trafficking of mutant subunits is a common in vitro observation for KCNH2 mutations (36, 37). For some KCNH2 mutations, impaired trafficking can be corrected pharmacologically in heterologous cells (38), thus stimulating interest in this approach for therapy of LQT2. Modeling the effects of human KCNQ1 and KCNH2 mutations in vivo (e.g., genetically modified mice) have been challenging because of substantial differences in repolarizing currents in mouse heart. However, recent progress has been made in generating transgenic rabbits expressing dominant-negative KCNQ1 or KCNH2 mutations that reproduce important features of human LQTS (39). Interestingly, loss-of-function mutations in the zebrafish homolog of KCNH2 (zERG) cause bradycardia, AV block, and prolonged action potential duration, and this has led some investigators to propose zebrafish as a model system for testing certain functional consequences of LQT2 mutations (40).
Approximately 10% of LQTS cases are caused by SCN5A mutations (LQT3) (33, 41). Most commonly, LQTS-associated SCN5A mutations confer a gain of function on the encoded cardiac Na+ channel (NaV1.5), characterized by impaired inactivation and increased persistent INa (42). A similar functional phenotype has been observed for mutations in other genes associated with LQTS including CAV3, SCN4B, and SNTA1 that encode proteins that interact directly or indirectly with NaV1.5 (25, 30, 43). Increased persistent INa disrupts the normal physiological balance of inward and outward currents flowing during the plateau phase of the cardiac action potential, causing delayed repolarization, prolonged action potential duration, and predisposition to reentrant arrhythmia triggered primarily by EADs. Genetically engineered mice carrying the first identified SCN5A mutation, an in-frame three-amino-acid deletion within the inactivation gate domain (delKPQ), recapitulated the cellular and molecular features of LQT3 including a propensity for ventricular arrhythmia, prolonged action potential duration with EADs, and increased persistent INa (44). Selective block of persistent INa by certain anti-arrhythmic agents (e.g., mexiletine) or the anti-angina drug ranolazine may offer targeted therapy for LQT3 mutations (45–48).
Acquired LQTS is more common than congenital LQTS but shares similar pathophysiological mechanisms. Drug-induced LQTS (diLQTS), the most common form of acquired LQTS, occurs when cardiac or non-cardiac drugs block HERG channels, suppress IKr, and cause delayed repolarization (49). A genetic predisposition to diLQTS has been hypothesized, and this notion has received support from genetic association studies (50, 51). A common KCNE1 variant (D85N) carried by 1%–2% of the general population is overrepresented among diLQTS cases (52). The variant confers a partial loss-of-function upon IKs and causes a condition referred to as reduced repolarization reserve that predisposes to overt LQTS upon collateral inhibition of IKr (53). Anecdotal evidence also suggests that latent congenital LQTS may be unmasked by HERG-blocking drugs (54, 55) or other physiological provocations such as acute myocardial infarction (56).
Syndromic LQTS: Andersen and Timothy syndromes.
In addition to Jervell and Lange-Nielsen syndrome, two other LQTS subtypes have prominent extracardiac manifestations. Andersen syndrome is an autosomal dominant disorder characterized by ventricular arrhythmias, periodic paralysis, and dysmorphic facial and skeletal features (27, 57). Considerable phenotypic variability exists among people diagnosed with Andersen syndrome, with many subjects exhibiting only one or two clinical features (58, 59). Although ventricular arrhythmia can be a prominent feature, this only rarely precipitates SCD (60).
Andersen syndrome is associated with mutations in KCNJ2 encoding the Kir2.1 inward rectifier K+ channel (27, 61, 62) that is responsible for the main component of IK1, an important current driving phase 3 repolarization (63). Dominant-negative, loss-of-function KCNJ2 mutations reduce IK1 and cause prolongation of the action potential duration, with increased propensity for re-entrant arrhythmias (62, 64, 65). Some identified KCNJ2 mutations are predicted to affect residues important for the regulation of Kir2.1 channel activity by phosphatidylinositol 4,5-bisphosphate (66). Other alleles impair trafficking of the channel to the plasma membrane (67, 68). Previous investigation of mice with homozygous deletion of Kcnj2 demonstrated premature death secondary to cleft palate but no overt ventricular arrhythmias despite lack of measurable IK1 in cardiac myocytes (64, 69). By contrast, in vitro suppression of IK1 in isolated canine left ventricle caused delayed action potential repolarization, increased transmural dispersion of repolarization, and polymorphic VT resembling cardiac features of Andersen syndrome (70, 71).
In Timothy syndrome, mutations in CACNA1C, which encodes the voltage-gated Ca2+ channel pore-forming subunit (CaV1.2), cause a complex phenotype including cardiac arrhythmia, syndactyly, and autism spectrum disorder (26). The syndrome exhibits sporadic occurrence as opposed to Mendelian inheritance, but a candidate gene survey demonstrated a common heterozygous mutation (G406R) in CACNA1C consistent with either de novo mutagenesis or parental mosaicism (26). A second mutation (G402S) was subsequently discovered (72). Both mutations occur within one of two mutually exclusive exons (exons 8 or 8A) present in alternatively spliced CACNA1C transcripts. Functionally, both mutations cause substantial impairment of channel inactivation, predicting an increased Ca2+ current during the plateau phase of the action potential (26, 72). Selective impairment of voltage-dependent inactivation rather than Ca2+-dependent inactivation may be the main functional disturbance (73). This gain-of-function defect leads to increased Ca2+ entry and activation of calmodulin-dependent kinase II, stimulating a proarrhythmic cascade in isolated rabbit ventricular myocytes (74). Mice with heterozygous or homozygous expression of a Timothy syndrome mutation are not viable.
SQTS.
Another disorder of repolarization, the SQTS, was described more recently and appears to be much rarer than LQTS (75). As in LQTS, subjects with SQTS can be stricken with life-threatening ventricular arrhythmias and SCD, often during childhood. Mutations in six different genes encoding either K+ channel (KCNQ1, KCNH2, KCNJ2) (76–78) or Ca2+ channel (CACNA1C, CACNB2, CACNA2D1) (79, 80) subunits have been associated with this phenotype. Many of these SQTS genes are the same as those implicated in LQTS, but the functional consequence of mutations is opposite. Mutations in K+ channels encoded by KCNH2 and KCNQ1 that cause SQTS exhibit gain-of-function effects predicted to enhance repolarizing power and shorten action potential duration (76, 77), effects that are modeled in zebrafish carrying mutant zERG channels with altered gating properties (81). By contrast, mutations in genes encoding Ca2+ channel subunits exhibit loss of function (79, 80). Mutations in KCNJ2 also confer a gain of function that for some alleles stems from unique biophysical behaviors, such as loss of inward rectification (82).
BrS.
Individuals with BrS have an increased risk for potentially lethal ventricular arrhythmias usually occurring during sleep, but in the absence of myocardial ischemia, electrolyte abnormalities or structural heart disease (83). Individuals with the disease may exhibit a characteristic baseline ECG pattern consisting of ST elevation in the right precordial leads, apparent right bundle branch block, but normal QT intervals. Administration of Na+ channel blocking agents (e.g., procainamide, flecainide, ajmaline) (84) and fever (85) may unmask this ECG pattern in latent cases. A family history of unexplained sudden death is typical. The sudden unexplained death syndrome is clinically similar to BrS and causes sudden death, typically during sleep, in young and middle-aged males, with a higher prevalence in individuals from Southeast Asian countries (86–88). Inheritance is autosomal dominant with incomplete and often low penetrance and a substantial male predominance. One attractive hypothesis to explain incomplete penetrance in BrS is the existence of genetic modifiers that may be common variants in SCN5A or other genes (89–91).
Mutations in SCN5A account for less than 30% of BrS cases with known genotypes. Reduced INa is the primary pathophysiological mechanism due to loss-of-function mutations including frameshifts, splice site defects, or premature stop codons (92, 93) that are predicted to encode nonfunctional Na+ channels. Also, some missense mutations have been demonstrated to be nonfunctional either because of impaired protein trafficking to the cell membrane or presumed disruption of ion conductance (94–96). Other missense mutations are dysfunctional, with biophysical defects predicted to reduce channel availability such as altered voltage dependence of activation, more rapid fast inactivation, and enhanced slow inactivation (97–99). Reduced INa may also be the consequence of mutations in other genes that less frequently cause BrS, including those encoding Na+ channel β subunits (SCN1B, SCN3B) (100, 101) or glycerol-3-phosphate dehydrogenase 1-like (GPD1L) (102). The latter gene defect has been suggested to cause suppression of the Na+ current by a PKC-dependent mechanism that is linked with the redox state of the cell (103, 104). Specifically, reduced enzymatic activity of mutant GPD1L is associated with an NADH/NAD+ imbalance that can activate protein kinase C and lead to phosphorylation of a specific serine residue (Ser1503) on NaV1.5, causing reduced channel activity. Mutations in other genes have been identified in BrS that cause loss of Ca2+ channel function (105), increased Ito (106), or increased ATP-sensitive K+ current (IK,ATP) (107).
Two mechanisms are proposed to explain the cellular basis of BrS (108). In one mechanism, a reduction in myocardial Na+ current is predicted to exaggerate differences in action potential duration between the inner (endocardium) and outer (epicardium) layers of ventricular muscle (8, 9). These differences occur because of an unequal distribution of Ito, which is more prominent in the epicardial layer and contributes to the characteristic spike and dome shape of the cardiac action potential. Reduced INa causes disproportionate shortening of epicardial action potentials because of unopposed Ito, leading to an exaggerated transmural dispersion of repolarization, a substrate promoting reentrant arrhythmias. This mechanism is supported by elegant work using the canine ventricular wedge model (8, 9). The second hypothesis posits that the main effect of reduced myocardial INa is slowing of impulse conduction in the right ventricle and delayed activation of the right ventricular outflow tract (RVOT) (108–111). This mechanism has gained support primarily from clinical observations including electroanatomic mapping studies (112, 113) and the observed therapeutic benefit of epicardial ablation over the RVOT (114). Heterozygous Scn5a knockout mice (Scn5a+/–) have provided an animal model of BrS (115–117). Whether these two hypotheses are mutually exclusive or whether all cases of BrS originate by the same pathophysiological mechanism remains unclear.
CPVT.
Alternations in intracellular Ca2+ homeostasis can also promote life-threatening ventricular arrhythmias and precipitate SCD. In the monogenic disorder CPVT, abnormal control or regulation of Ca2+ release from the SR can trigger DADs and cause ventricular arrhythmias (118). The condition is usually diagnosed during childhood and typically presents with syncope or SCD in the setting of exercise, emotional stress, or other circumstances associated with a surge in catecholamine release (119).
Mutations in RYR2 encoding the cardiac ryanodine receptor/Ca2+ release channel are associated with autosomal dominant CPVT (120). Autosomal recessive forms of the disorder are associated with mutations in either CASQ2, encoding the SR Ca2+-binding protein calsequestrin (121), or TRDN, encoding triadin, which links RYR2 with calsequestrin (122). These three proteins reside together within the terminal cisternae of the SR, where intracellular membranes lie adjacent to the transverse tubule (T tubule) region of the plasma membrane. Normally, electrical impulses conducted into the T tubules activate voltage-gated L-type Ca2+ channels and evoke a wave of Ca2+ influx sufficient to promote Ca2+-induced Ca2+ release through RYR2. Release of Ca2+ from the SR promotes myocyte contraction (excitation-contraction coupling), which is then terminated by removal of cytosolic Ca2+ mostly by reuptake into SR by a Ca2+-ATPase pump (SERCA) and through exchange for extracellular Na+ by an electrogenic NCX on the plasma membrane (Figure 4). Spontaneous SR Ca2+ release during diastole can be evoked by β-adrenergic stimulation by several proposed mechanisms (123, 124).
Figure 4. Molecular basis for intracellular Ca2+ homeostasis.
Illustration of T tubule with adjacent junctional SR containing the ryanodine receptor (RYR2) Ca2+ release channel, calsequestrin Ca2+ binding protein, and Ca2+ pump (SERCA) with regulatory protein phospholamban (PLN). The electrogenic NCX is represented on the surface plasma membrane. Electrical impulses conducted into the T tubules trigger a wave of Ca2+ influx via the voltage-dependent, L-type Ca2+ channel (LTCC) that promotes Ca2+ release through RYR2. This release of Ca2+ from the SR promotes myocyte contraction. The subsequent removal of cytosolic Ca2+, mostly by reuptake into the SR by SERCA and by pumping out of the cell by the plasma membrane Ca2+ ATPase (PMCA), and the exchange for extracellular Na+ by an electrogenic NCX on the plasma membrane, terminates the contraction.
CPVT-associated RYR2 mutations sensitize the channel to luminal Ca2+, leading to exaggerated spontaneous SR Ca2+ release (125). The effects of CASQ mutations are more complex and include a loss of SR Ca2+ buffering, loss of RYR2 regulation by calsequestrin, and remodeling of SR ultrastructure (126–128). Loss of triadin, as in some cases of recessive CPVT (122), may also predispose to unregulated SR Ca2+ release by disrupting normal regulation of intracellular Ca2+ homeostasis. In Trdn knockout mice, attenuated Ca2+-dependent inactivation of L-type Ca2+ channels appears to promote SR Ca2+ overload and the predisposition to aberrant SR Ca2+ release (129).
Summary and future directions
Fundamental molecular and genetic mechanisms of SCD have been elucidated by investigations of rare monogenic disorders of heart rhythm. Despite the identification of more than 25 causal genes, there remain many subjects with inherited arrhythmia susceptibility who do not have mutations, which suggests that other, unidentified genes exist. Newer strategies such as exome and whole genome sequencing may be valuable to uncover additional molecular etiologies. Efforts to understand mechanisms responsible for incomplete penetrance, including identification of modifier genes, will also contribute to deciphering the complex relationships between genotype and phenotype. Finally, better disease models such as cardiomyocytes derived from human-induced pluripotent stem cells created from patients with monogenic disorders predisposing to SCD, as described elsewhere in this Review series (130), may also help advance our understanding of SCD pathophysiology and inspire new therapeutic approaches.
Acknowledgments
The author is supported by grants from the NIH (HL083374 and HL068880).
Footnotes
Conflict of interest: The author has declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2013;123(1):75–83. doi:10.1172/JCI62928.
References
- 1.Fishman GI, et al. Sudden cardiac death prediction and prevention: report from a National Heart, Lung, and Blood Institute and Heart Rhythm Society Workshop. Circulation. 2010;122(22):2335–2348. doi: 10.1161/CIRCULATIONAHA.110.976092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104(18):2158–2163. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 3.Lehnart SE, et al. Inherited arrhythmias: a National Heart, Lung, and Blood Institute and Office of Rare Diseases workshop consensus report about the diagnosis, phenotyping, molecular mechanisms, and therapeutic approaches for primary cardiomyopathies of gene mutations affecting ion channel function. Circulation. 2007;116(20):2325–2345. doi: 10.1161/CIRCULATIONAHA.107.711689. [DOI] [PubMed] [Google Scholar]
- 4.George AL., Jr Common genetic variants in sudden cardiac death. Heart Rhythm. 2009;6(11 suppl):S3–S9. doi: 10.1016/j.hrthm.2009.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deo R, Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation. 2012;125(4):620–637. doi: 10.1161/CIRCULATIONAHA.111.023838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Auerbach DS, Grzda KR, Furspan PB, Sato PY, Mironov S, Jalife J. Structural heterogeneity promotes triggered activity, reflection and arrhythmogenesis in cardiomyocyte monolayers. J Physiol. 2011;589(pt 9):2363–2381. doi: 10.1113/jphysiol.2010.200576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaquero M, Calvo D, Jalife J. Cardiac fibrillation: from ion channels to rotors in the human heart. Heart Rhythm. 2008;5(6):872–879. doi: 10.1016/j.hrthm.2008.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Antzelevitch C, Yan GX, Shimizu W. Transmural dispersion of repolarization and arrhythmogenicity: the Brugada syndrome versus the long QT syndrome. J Electrocardiol. 1999;32(suppl):158–165. doi: 10.1016/S0022-0736(99)90074-2. [DOI] [PubMed] [Google Scholar]
- 9.Yan GX, Antzelevitch C. Cellular basis for the Brugada syndrome and other mechanisms of arrhythmogenesis associated with ST-segment elevation. Circulation. 1999;100(15):1660–1666. doi: 10.1161/01.CIR.100.15.1660. [DOI] [PubMed] [Google Scholar]
- 10.January CT, Fozzard HA. Delayed afterdepolarizations in heart muscle: mechanisms and relevance. Pharmacol Rev. 1988;40(3):219–227. [PubMed] [Google Scholar]
- 11.January CT, Moscucci A. Cellular mechanisms of early afterdepolarizations. Ann N Y Acad Sci. 1992;644:23–32. doi: 10.1111/j.1749-6632.1992.tb30999.x. [DOI] [PubMed] [Google Scholar]
- 12.Wu Y, Roden DM, Anderson ME. Calmodulin kinase inhibition prevents development of the arrhythmogenic transient inward current. Circ Res. 1999;84(8):906–912. doi: 10.1161/01.RES.84.8.906. [DOI] [PubMed] [Google Scholar]
- 13.McNally EM, Golbus JR, Puckelwartz MJ. Genetic mutations and mechanisms in dilated cardiomyopathy. J Clin Invest. 2013;123(1):19–26. doi: 10.1172/JCI62862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwartz PJ, Wolf S. QT interval prolongation as predictor of sudden death in patients with myocardial infarction. Circulation. 1978;57(6):1074–1077. doi: 10.1161/01.CIR.57.6.1074. [DOI] [PubMed] [Google Scholar]
- 15.Chugh SS, et al. Determinants of prolonged QT interval and their contribution to sudden death risk in coronary artery disease: the Oregon Sudden Unexpected Death Study. Circulation. 2009;119(5):663–670. doi: 10.1161/CIRCULATIONAHA.108.797035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vincent GM. The molecular genetics of the long QT syndrome: Genes causing fainting and sudden death. Annu Rev Med. 1998;49:263–274. doi: 10.1146/annurev.med.49.1.263. [DOI] [PubMed] [Google Scholar]
- 17.Schwartz PJ, et al. Prevalence of the congenital long-QT syndrome. Circulation. 2009;120(18):1761–1767. doi: 10.1161/CIRCULATIONAHA.109.863209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Curran ME, et al. A molecular basis for cardiac arrhythmia: HERG mutations cause long QT syndrome. . Cell. 1995;80(5):795–803. doi: 10.1016/0092-8674(95)90358-5. [DOI] [PubMed] [Google Scholar]
- 19.Sanguinetti MC, Jiang C, Curran ME, Keating MT. A mechanistic link between an inherited and an acquired cardiac arrhythmia: HERG encodes the IKr potassium channel. . Cell. 1995;81(2):299–307. doi: 10.1016/0092-8674(95)90340-2. [DOI] [PubMed] [Google Scholar]
- 20.Wang Q, et al. Positional cloning of a novel potassium channel gene: KVLQT1 mutations cause cardiac arrhythmias. . Nat Genet. 1996;12(1):17–23. doi: 10.1038/ng0196-17. [DOI] [PubMed] [Google Scholar]
- 21.Splawski I, Tristani-Firouzi M, Lehmann MH, Sanguinetti MC, Keating MT. Mutations in the hminK gene cause long QT syndrome and suppress IKs function. . Nat Genet. 1997;17(3):338–340. doi: 10.1038/ng1197-338. [DOI] [PubMed] [Google Scholar]
- 22.Abbott GW, et al. MiRP1 forms IKr potassium channels with HERG and is associated with cardiac arrhythmia. . Cell. 1999;97(2):175–187. doi: 10.1016/S0092-8674(00)80728-X. [DOI] [PubMed] [Google Scholar]
- 23.Schulze-Bahr E, et al. KCNE1 mutations cause Jervell and Lange-Nielsen syndrome. Nat Genet. 1997;17(3):267–268. doi: 10.1038/ng1197-267. [DOI] [PubMed] [Google Scholar]
- 24.Wang Q, et al. SCN5A mutations associated with an inherited cardiac arrhythmia, long QT syndrome. . Cell. 1995;80(5):805–811. doi: 10.1016/0092-8674(95)90359-3. [DOI] [PubMed] [Google Scholar]
- 25.Medeiros-Domingo A, et al. SCN4B-encoded sodium channel β4 subunit in congenital long-QT syndrome. . Circulation. 2007;116(2):134–142. doi: 10.1161/CIRCULATIONAHA.106.659086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Splawski I, et al. CaV1.2 calcium channel dysfunction causes a multisystem disorder including arrhythmia and autism. . Cell. 2004;119(1):19–31. doi: 10.1016/j.cell.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 27.Plaster NM, et al. Mutations in Kir2.1 cause the developmental and episodic electrical phenotypes of Andersen’s syndrome. . Cell. 2001;105(4):511–519. doi: 10.1016/S0092-8674(01)00342-7. [DOI] [PubMed] [Google Scholar]
- 28.Yang Y, et al. Identification of a Kir3.4 mutation in congenital long QT syndrome. . Am J Hum Genet. 2010;86(6):872–880. doi: 10.1016/j.ajhg.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mohler PJ, et al. Ankyrin-B mutation causes type 4 long-QT cardiac arrhythmia and sudden cardiac death. Nature. 2003;421(6923):634–639. doi: 10.1038/nature01335. [DOI] [PubMed] [Google Scholar]
- 30.Vatta M, et al. Mutant caveolin-3 induces persistent late sodium current and is associated with long-QT syndrome. Circulation. 2006;114(20):2104–2112. doi: 10.1161/CIRCULATIONAHA.106.635268. [DOI] [PubMed] [Google Scholar]
- 31.Chen L, Marquardt ML, Tester DJ, Sampson KJ, Ackerman MJ, Kass RS. Mutation of an A-kinase-anchoring protein causes long-QT syndrome. Proc Natl Acad Sci U S A. 2007;104(52):20990–20995. doi: 10.1073/pnas.0710527105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheng J, et al. Alpha1-syntrophin mutations identified in sudden infant death syndrome cause an increase in late cardiac sodium current. Circ Arrhythm Electrophysiol. 2009;2(6):667–676. doi: 10.1161/CIRCEP.109.891440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Splawski I, et al. Spectrum of mutations in long-QT syndrome genes. KVLQT1, HERG, SCN5A, KCNE1, and KCNE2. Circulation. 2000;102(10):1178–1185. doi: 10.1161/01.CIR.102.10.1178. [DOI] [PubMed] [Google Scholar]
- 34.Sesti F, et al. A common polymorphism associated with antibiotic-induced cardiac arrhythmia. Proc Natl Acad Sci U S A. 2000;97(19):10613–10618. doi: 10.1073/pnas.180223197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neyroud N, et al. A novel mutation in the potassium channel gene KVLQT1 causes the Jervell and Lange-Nielsen cardioauditory syndrome. Nat Genet. 1997;15(2):186–189. doi: 10.1038/ng0297-186. [DOI] [PubMed] [Google Scholar]
- 36.Furutani M, et al. Novel mechanism associated with an inherited cardiac arrhythmia: defective protein trafficking by the mutant HERG (G601S) potassium channel. Circulation. 1999;99(17):2290–2294. doi: 10.1161/01.CIR.99.17.2290. [DOI] [PubMed] [Google Scholar]
- 37.Anderson CL, et al. Most LQT2 mutations reduce KV11.1 (hERG) current by a class 2 (trafficking-deficient) mechanism. . Circulation. 2006;113(3):365–373. doi: 10.1161/CIRCULATIONAHA.105.570200. [DOI] [PubMed] [Google Scholar]
- 38.Rajamani S, Anderson CL, Anson BD, January CT. Pharmacological rescue of human K+ channel long-QT2 mutations: human ether-a-go-go-related gene rescue without block. . Circulation. 2002;105(24):2830–2835. doi: 10.1161/01.CIR.0000019513.50928.74. [DOI] [PubMed] [Google Scholar]
- 39.Brunner M, et al. Mechanisms of cardiac arrhythmias and sudden death in transgenic rabbits with long QT syndrome. J Clin Invest. 2008;118(6):2246–2259. doi: 10.1172/JCI33578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arnaout R, et al. Zebrafish model for human long QT syndrome. Proc Natl Acad Sci U S A. 2007;104(27):11316–11321. doi: 10.1073/pnas.0702724104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kapplinger JD, et al. Spectrum and prevalence of mutations from the first 2,500 consecutive unrelated patients referred for the FAMILION long QT syndrome genetic test. Heart Rhythm. 2009;6(9):1297–1303. doi: 10.1016/j.hrthm.2009.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bennett PB, Yazawa K, Makita N, George AL., Jr Molecular mechanism for an inherited cardiac arrhythmia. Nature. 1995;376(6542):683–685. doi: 10.1038/376683a0. [DOI] [PubMed] [Google Scholar]
- 43.Ueda K, et al. Syntrophin mutation associated with long QT syndrome through activation of the nNOS-SCN5A macromolecular complex. Proc Natl Acad Sci U S A. 2008;105(27):9355–9360. doi: 10.1073/pnas.0801294105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nuyens D, et al. Abrupt rate accelerations or premature beats cause life-threatening arrhythmias in mice with long-QT3 syndrome. Nat Med. 2001;7(9):1021–1027. doi: 10.1038/nm0901-1021. [DOI] [PubMed] [Google Scholar]
- 45.Schwartz PJ, et al. Long QT syndrome patients with mutations of the SCN5A and HERG genes have differential responses to Na+ channel blockade and to increases in heart rate — Implications for gene-specific therapy. . Circulation. 1995;92(12):3381–3386. doi: 10.1161/01.CIR.92.12.3381. [DOI] [PubMed] [Google Scholar]
- 46.Wang DW, Yazawa K, Makita N, George AL, Jr, Bennett PB. Pharmacological targeting of long QT mutant sodium channels. J Clin Invest. 1997;99(7):1714–1720. doi: 10.1172/JCI119335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fredj S, Sampson KJ, Liu H, Kass RS. Molecular basis of ranolazine block of LQT-3 mutant sodium channels: evidence for site of action. Br J Pharmacol. 2006;148(1):16–24. doi: 10.1038/sj.bjp.0706709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moss AJ, Zareba W, Schwarz KQ, Rosero S, McNitt S, Robinson JL. Ranolazine shortens repolarization in patients with sustained inward sodium current due to type-3 long-QT syndrome. J Cardiovasc Electrophysiol. 2008;19(12):1289–1293. doi: 10.1111/j.1540-8167.2008.01246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kannankeril P, Roden DM, Darbar D. Drug-induced long QT syndrome. Pharmacol Rev. 2010;62(4):760–781. doi: 10.1124/pr.110.003723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Itoh H, et al. Latent genetic backgrounds and molecular pathogenesis in drug-induced long-QT syndrome. Circ Arrhythm Electrophysiol. 2009;2(5):511–523. doi: 10.1161/CIRCEP.109.862649. [DOI] [PubMed] [Google Scholar]
- 51.Ramire AH, et al. Pharmacogenomics J. Novel rare variants in congenital cardiac arrhythmia genes are frequent in drug-induced torsades de pointes [published online ahead of print May 15, 2012]. doi: 10.1038/tpj.2012.14 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kääb S, et al. A large candidate gene survey identifies the KCNE1 D85N polymorphism as a possible modulator of drug-induced torsades de pointes. . Circ Cardiovasc Genet. 2011;5(1):91–99. doi: 10.1161/CIRCGENETICS.111.960930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Roden DM. Long QT syndrome: reduced repolarization reserve and the genetic link. J Intern Med. 2006;259(1):59–69. doi: 10.1111/j.1365-2796.2005.01589.x. [DOI] [PubMed] [Google Scholar]
- 54.Yang P, et al. Allelic variants in long-QT disease genes in patients with drug-associated torsades de pointes. Circulation. 2002;105(16):1943–1948. doi: 10.1161/01.CIR.0000014448.19052.4C. [DOI] [PubMed] [Google Scholar]
- 55.Liu K, et al. New mechanism contributing to drug-induced arrhythmia: rescue of a misprocessed LQT3 mutant. Circulation. 2005;112(21):3239–3246. doi: 10.1161/CIRCULATIONAHA.105.564008. [DOI] [PubMed] [Google Scholar]
- 56.Crotti L, et al. Torsades de pointes following acute myocardial infarction: Evidence for a deadly link with a common genetic variant. Heart Rhythm. 2012;9(7):1104–1112. doi: 10.1016/j.hrthm.2012.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tawil R, et al. Andersen’s syndrome: potassium-sensitive periodic paralysis, ventricular ectopy, and dysmorphic features. Ann Neurol. 1994;35(3):326–330. doi: 10.1002/ana.410350313. [DOI] [PubMed] [Google Scholar]
- 58.Yoon G, et al. Andersen-Tawil syndrome: Prospective cohort analysis and expansion of the phenotype. Am J Med Genet A. 2006;140(4):312–321. doi: 10.1002/ajmg.a.31092. [DOI] [PubMed] [Google Scholar]
- 59.Andelfinger G, Tapper AR, Welch RC, Vanoye CG, George AL, Jr, Benson DW. KCNJ2 mutation results in Andersen syndrome with sex-specific cardiac and skeletal muscle phenotypes. Am J Hum Genet. 2002;71(3):663–668. doi: 10.1086/342360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang L, et al. Electrocardiographic features in Andersen-Tawil syndrome patients with KCNJ2 mutations: characteristic T-U-wave patterns predict the KCNJ2 genotype. Circulation. 2005;111(21):2720–2726. doi: 10.1161/CIRCULATIONAHA.104.472498. [DOI] [PubMed] [Google Scholar]
- 61.Hosaka Y, et al. Function, subcellular localization and assembly of a novel mutation of KCNJ2 in Andersen’s syndrome. J Mol Cell Cardiol. 2003;35(4):409–415. doi: 10.1016/S0022-2828(03)00046-4. [DOI] [PubMed] [Google Scholar]
- 62.Tristani-Firouzi M, et al. Functional and clinical characterization of KCNJ2 mutations associated with LQT7 (Andersen syndrome). . J Clin Invest. 2002;110(3):381–388. doi: 10.1172/JCI15183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zobel C, et al. Molecular dissection of the inward rectifier potassium current IK1 in rabbit cardiomyocytes: evidence for heteromeric co-assembly of Kir2.1 and Kir2.2. . J Physiol. 2003;550(pt 2):365–372. doi: 10.1113/jphysiol.2002.036400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zaritsky JJ, Redell JB, Tempel BL, Schwarz TL. The consequences of disrupting cardiac inwardly rectifying K+ current IK1 as revealed by the targeted deletion of the murine Kir2.1 and Kir2.2 genes. . J Physiol. 2001;533(pt 3):697–710. doi: 10.1111/j.1469-7793.2001.t01-1-00697.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Miake J, Marban E, Nuss HB. Functional role of inward rectifier current in heart probed by Kir2.1 overexpression and dominant-negative suppression. . J Clin Invest. 2003;111(10):1529–1536. doi: 10.1172/JCI17959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Donaldson MR, et al. PIP2 binding residues of Kir2.1 are common targets of mutations causing Andersen syndrome. . Neurology. 2003;60(11):1811–1816. doi: 10.1212/01.WNL.0000072261.14060.47. [DOI] [PubMed] [Google Scholar]
- 67.Bendahhou S, Donaldson MR, Plaster NM, Tristani-Firouzi M, Fu YH, Ptácek LJ. Defective potassium channel Kir2.1 trafficking underlies Andersen-Tawil syndrome. J Biol Chem. 2003;278(51):51779–51785. doi: 10.1074/jbc.M310278200. [DOI] [PubMed] [Google Scholar]
- 68.Ballester LY, et al. Trafficking-competent and trafficking-defective KCNJ2 mutations in Andersen syndrome. Hum Mutat. 2006;27(4):388. doi: 10.1002/humu.9418. [DOI] [PubMed] [Google Scholar]
- 69.Zaritsky JJ, Eckman DM, Wellman GC, Nelson MT, Schwarz TL. Targeted disruption of Kir2.1 and Kir2.2 genes reveals the essential role of the inwardly rectifying K+ current in K+-mediated vasodilation. . Circ Res. 2000;87(2):160–166. doi: 10.1161/01.RES.87.2.160. [DOI] [PubMed] [Google Scholar]
- 70.Tsuboi M, Antzelevitch C. Cellular basis for electrocardiographic and arrhythmic manifestations of Andersen-Tawil syndrome (LQT7). Heart Rhythm. 2006;3(3):328–335. doi: 10.1016/j.hrthm.2005.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Morita H, Zipes DP, Morita ST, Wu J. Mechanism of U wave and polymorphic ventricular tachycardia in a canine tissue model of Andersen-Tawil syndrome. Cardiovasc Res. 2007;75(3):510–518. doi: 10.1016/j.cardiores.2007.04.028. [DOI] [PubMed] [Google Scholar]
- 72.Splawski I, et al. Severe arrhythmia disorder caused by cardiac L-type calcium channel mutations. Proc Natl Acad Sci U S A. 2005;102(23):8089–8096. doi: 10.1073/pnas.0502506102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Barrett CF, Tsien RW. The Timothy syndrome mutation differentially affects voltage- and calcium-dependent inactivation of CaV1.2 L-type calcium channels. . Proc Natl Acad Sci U S A. 2008;105(6):2157–2162. doi: 10.1073/pnas.0710501105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Thiel WH, et al. Proarrhythmic defects in Timothy syndrome require calmodulin kinase II. Circulation. 2008;118(22):2225–2234. doi: 10.1161/CIRCULATIONAHA.108.788067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gaita F, et al. Short QT Syndrome: a familial cause of sudden death. Circulation. 2003;108(8):965–970. doi: 10.1161/01.CIR.0000085071.28695.C4. [DOI] [PubMed] [Google Scholar]
- 76.Bellocq C, et al. Mutation in the KCNQ1 gene leading to the short QT-interval syndrome. Circulation. 2004;109(20):2394–2397. doi: 10.1161/01.CIR.0000130409.72142.FE. [DOI] [PubMed] [Google Scholar]
- 77.Brugada R, et al. Sudden death associated with short-QT syndrome linked to mutations in HERG. Circulation. 2004;109(1):30–35. doi: 10.1161/01.CIR.0000109482.92774.3A. [DOI] [PubMed] [Google Scholar]
- 78.Priori SG, et al. A novel form of short QT syndrome (SQT3) is caused by a mutation in the KCNJ2 gene. Circ Res. 2005;96(7):800–807. doi: 10.1161/01.RES.0000162101.76263.8c. [DOI] [PubMed] [Google Scholar]
- 79.Antzelevitch C, et al. Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST-segment elevation, short QT intervals, and sudden cardiac death. Circulation. 2007;115(4):442–449. doi: 10.1161/CIRCULATIONAHA.106.668392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Templin C, et al. Identification of a novel loss-of-function calcium channel gene mutation in short QT syndrome (SQTS6). Eur Heart J. 2011;32(9):1077–1088. doi: 10.1093/eurheartj/ehr076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hassel D, et al. Deficient zebrafish ether-a-go-go-related gene channel gating causes short-QT syndrome in zebrafish reggae mutants. . Circulation. 2008;117(7):866–875. doi: 10.1161/CIRCULATIONAHA.107.752220. [DOI] [PubMed] [Google Scholar]
- 82.Casini S, Postma AV. Decreased inward rectification of Kir2.1 channels is a novel mechanism underlying the short QT syndrome. . Cardiovasc Res. 2012;93(4):535–536. doi: 10.1093/cvr/cvs084. [DOI] [PubMed] [Google Scholar]
- 83.Brugada J, Brugada R, Brugada P. Right bundle-branch block and ST-segment elevation in leads V1 through V3: a marker for sudden death in patients without demonstrable structural heart disease. Circulation. 1998;97(5):457–460. doi: 10.1161/01.CIR.97.5.457. [DOI] [PubMed] [Google Scholar]
- 84.Brugada R, et al. Sodium channel blockers identify risk for sudden death in patients with ST-segment elevation and right bundle branch block but structurally normal hearts. Circulation. 2000;101(5):510–515. doi: 10.1161/01.CIR.101.5.510. [DOI] [PubMed] [Google Scholar]
- 85.Keller DI, et al. A novel SCN5A mutation, F1344S, identified in a patient with Brugada syndrome and fever-induced ventricular fibrillation. Cardiovasc Res. 2006;70(3):521–529. doi: 10.1016/j.cardiores.2006.02.030. [DOI] [PubMed] [Google Scholar]
- 86.Vatta M, et al. Genetic and biophysical basis of sudden unexplained nocturnal death syndrome (SUNDS), a disease allelic to Brugada syndrome. Hum Mol Genet. 2002;11(3):337–345. doi: 10.1093/hmg/11.3.337. [DOI] [PubMed] [Google Scholar]
- 87.Baron RC, Thacker SB, Gorelkin L, Vernon AA, Taylor WR, Choi K. Sudden death among Southeast Asian refugees. An unexplained nocturnal phenomenon. JAMA. 1983;250(21):2947–2951. doi: 10.1001/jama.1983.03340210045023. [DOI] [PubMed] [Google Scholar]
- 88.Nademanee K, et al. Arrhythmogenic marker for the sudden unexplained death syndrome in Thai men. Circulation. 1997;96(8):2595–2600. doi: 10.1161/01.CIR.96.8.2595. [DOI] [PubMed] [Google Scholar]
- 89.Poelzing S, et al. SCN5A polymorphism restores trafficking of a Brugada syndrome mutation on a separate gene. Circulation. 2006;114(5):368–376. doi: 10.1161/CIRCULATIONAHA.105.601294. [DOI] [PubMed] [Google Scholar]
- 90.Leoni AL, et al. Variable NaV1.5 protein expression from the wild-type allele correlates with the penetrance of cardiac conduction disease in the Scn5a+/– mouse model. . PLoS One. 2010;19(2):e9298. doi: 10.1371/journal.pone.0009298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ohno S, et al. KCNE5 (KCNE1L) Variants are novel modulators of Brugada syndrome and idiopathic ventricular fibrillation. Circ Arrhythm Electrophysiol. 2011;4(3):352–361. doi: 10.1161/CIRCEP.110.959619. [DOI] [PubMed] [Google Scholar]
- 92.Chen Q, et al. Genetic basis and molecular mechanism for idiopathic ventricular fibrillation. Nature. 1998;392(6673):293–296. doi: 10.1038/32675. [DOI] [PubMed] [Google Scholar]
- 93.Schulze-Bahr E, et al. Sodium channel gene (SCN5A) mutations in 44 index patients with Brugada syndrome: different incidences in familial and sporadic disease. . Hum Mutat. 2003;21(6):651–652. doi: 10.1002/humu.9144. [DOI] [PubMed] [Google Scholar]
- 94.Baroudi G, Acharfi S, Larouche C, Chahine M. Expression and intracellular localization of an SCN5A double mutant R1232W/T1620M implicated in Brugada syndrome. Circ Res. 2002;90(1):E11–E16. doi: 10.1161/hh0102.102977. [DOI] [PubMed] [Google Scholar]
- 95.Baroudi G, Pouliot V, Denjoy I, Guicheney P, Shrier A, Chahine M. Novel mechanism for Brugada syndrome: defective surface localization of an SCN5A mutant (R1432G). . Circ Res. 2001;88(12):E78–E83. doi: 10.1161/hh1201.093270. [DOI] [PubMed] [Google Scholar]
- 96.Valdivia CR, et al. A trafficking defective, Brugada syndrome-causing SCN5A mutation rescued by drugs. . Cardiovasc Res. 2004;62(1):53–62. doi: 10.1016/j.cardiores.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 97.Dumaine R, et al. Ionic mechanisms responsible for the electrocardiographic phenotype of the Brugada syndrome are temperature dependent. Circ Res. 1999;85(9):803–809. doi: 10.1161/01.RES.85.9.803. [DOI] [PubMed] [Google Scholar]
- 98.Wang DW, Makita N, Kitabatake A, Balser JR, George AL., Jr Enhanced Na+ channel intermediate inactivation in Brugada syndrome. . Circ Res. 2000;87(8):E37–E43. doi: 10.1161/01.RES.87.8.e37. [DOI] [PubMed] [Google Scholar]
- 99.Rook MB, et al. Human SCN5A gene mutations alter cardiac sodium channel kinetics and are associated with the Brugada syndrome. Cardiovasc Res. 1999;44(3):507–517. doi: 10.1016/S0008-6363(99)00350-8. [DOI] [PubMed] [Google Scholar]
- 100.Watanabe H, et al. Sodium channel β1 subunit mutations associated with Brugada syndrome and cardiac conduction disease in humans. . J Clin Invest. 2008;118(6):2260–2268. doi: 10.1172/JCI33891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hu D, et al. A mutation in the β3 subunit of the cardiac sodium channel associated with Brugada ECG phenotype. . Circ Cardiovasc Genet. 2009;2(3):270–278. doi: 10.1161/CIRCGENETICS.108.829192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.London B, et al. Mutation in glycerol-3-phosphate dehydrogenase 1 like gene (GPD1-L) decreases cardiac Na+ current and causes inherited arrhythmias. Circulation. 2007;116(20):2260–2268. doi: 10.1161/CIRCULATIONAHA.107.703330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Valdivia CR, Ueda K, Ackerman MJ, Makielski JC. GPD1L links redox state to cardiac excitability by PKC-dependent phosphorylation of the sodium channel SCN5A. Am J Physiol Heart Circ Physiol. 2009;297(4):H1446–H1452. doi: 10.1152/ajpheart.00513.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Liu M, et al. Cardiac Na+ current regulation by pyridine nucleotides. . Circ Res. 2009;105(8):737–745. doi: 10.1161/CIRCRESAHA.109.197277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cordeiro JM, Marieb M, Pfeiffer R, Calloe K, Burashnikov E, Antzelevitch C. Accelerated inactivation of the L-type calcium current due to a mutation in CACNB2b underlies Brugada syndrome. J Mol Cell Cardiol. 2009;46(5):695–703. doi: 10.1016/j.yjmcc.2009.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Giudicessi JR, et al. Transient outward current (Ito) gain-of-function mutations in the KCND3-encoded KV4.3 potassium channel and Brugada syndrome. . Heart Rhythm. 2011;8(7):1024–1032. doi: 10.1016/j.hrthm.2011.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Medeiros-Domingo A, et al. Gain-of-function mutation S422L in the KCNJ8-encoded cardiac KATP channel Kir6.1 as a pathogenic substrate for J-wave syndromes. . Heart Rhythm. 2010;7(10):1466–1471. doi: 10.1016/j.hrthm.2010.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Meregalli PG, Wilde AA, Tan HL. Pathophysiological mechanisms of Brugada syndrome: depolarization disorder, repolarization disorder, or more? Cardiovasc Res. 2005;67(3):367–378. doi: 10.1016/j.cardiores.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 109.Tukkie R, Sogaard P, Vleugels J, de Groot IK, Wilde AA, Tan HL. Delay in right ventricular activation contributes to Brugada syndrome. Circulation. 2004;109(10):1272–1277. doi: 10.1161/01.CIR.0000118467.53182.D1. [DOI] [PubMed] [Google Scholar]
- 110.Zhang ZS, Tranquillo J, Neplioueva V, Bursac N, Grant AO. Sodium channel kinetic changes that produce Brugada syndrome or progressive cardiac conduction system disease. Am J Physiol Heart Circ Physiol. 2007;292(1):H399–H407. doi: 10.1152/ajpheart.01025.2005. [DOI] [PubMed] [Google Scholar]
- 111.Coronel R, et al. Right ventricular fibrosis and conduction delay in a patient with clinical signs of Brugada syndrome: a combined electrophysiological, genetic, histopathologic, and computational study. Circulation. 2005;112(18):2769–2777. doi: 10.1161/CIRCULATIONAHA.105.532614. [DOI] [PubMed] [Google Scholar]
- 112.Postema PG, et al. Slow and discontinuous conduction conspire in Brugada syndrome: a right ventricular mapping and stimulation study. Circ Arrhythm Electrophysiol. 2008;1(5):379–386. doi: 10.1161/CIRCEP.108.790543. [DOI] [PubMed] [Google Scholar]
- 113.Postema PG, et al. Local depolarization abnormalities are the dominant pathophysiologic mechanism for type 1 electrocardiogram in brugada syndrome a study of electrocardiograms, vectorcardiograms, and body surface potential maps during ajmaline provocation. J Am Coll Cardiol. 2010;55(8):789–797. doi: 10.1016/j.jacc.2009.11.033. [DOI] [PubMed] [Google Scholar]
- 114.Nademanee K, et al. Prevention of ventricular fibrillation episodes in Brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation. 2011;123(12):1270–1279. doi: 10.1161/CIRCULATIONAHA.110.972612. [DOI] [PubMed] [Google Scholar]
- 115.Papadatos GA, et al. Slowed conduction and ventricular tachycardia after targeted disruption of the cardiac sodium channel gene Scn5a. Proc Natl Acad Sci U S A. 2002;99(9):6210–6215. doi: 10.1073/pnas.082121299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Martin CA, Zhang Y, Grace AA, Huang CL. In vivo studies of Scn5a+/– mice modeling Brugada syndrome demonstrate both conduction and repolarization abnormalities. . J Electrocardiol. 2010;43(5):433–439. doi: 10.1016/j.jelectrocard.2010.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Martin CA, Zhang Y, Grace AA, Huang CL. Increased right ventricular repolarization gradients promote arrhythmogenesis in a murine model of Brugada syndrome. J Cardiovasc Electrophysiol. 2010;21(10):1153–1159. doi: 10.1111/j.1540-8167.2010.01767.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Liu N, et al. Arrhythmogenesis in catecholaminergic polymorphic ventricular tachycardia: insights from a RyR2 R4496C knock-in mouse model. Circ Res. 2006;99(3):292–298. doi: 10.1161/01.RES.0000235869.50747.e1. [DOI] [PubMed] [Google Scholar]
- 119.Leenhardt A, Lucet V, Denjoy I, Grau F, Ngoc DD, Coumel P. Catecholaminergic polymorphic ventricular tachycardia in children. A 7-year follow-up of 21 patients. Circulation. 1995;91(5):1512–1519. doi: 10.1161/01.CIR.91.5.1512. [DOI] [PubMed] [Google Scholar]
- 120.Priori SG, et al. Mutations in the cardiac ryanodine receptor gene (hRyR2) underlie catecholaminergic polymorphic ventricular tachycardia. Circulation. 2001;103(2):196–200. doi: 10.1161/01.CIR.103.2.196. [DOI] [PubMed] [Google Scholar]
- 121.Lahat H, et al. A missense mutation in a highly conserved region of CASQ2 is associated with autosomal recessive catecholamine-induced polymorphic ventricular tachycardia in Bedouin families from Israel. Am J Hum Genet. 2001;69(6):1378–1384. doi: 10.1086/324565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Roux-Buisson N, et al. Absence of triadin, a protein of the calcium release complex, is responsible for cardiac arrhythmia with sudden death in human. Hum Mol Genet. 2012;21(12):2759–2767. doi: 10.1093/hmg/dds104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Curran J, Hinton MJ, Ríos E, Bers DM, Shannon TR. Beta-adrenergic enhancement of sarcoplasmic reticulum calcium leak in cardiac myocytes is mediated by calcium/calmodulin-dependent protein kinase. Circ Res. 2007;100(3):391–398. doi: 10.1161/01.RES.0000258172.74570.e6. [DOI] [PubMed] [Google Scholar]
- 124.Zhou P, et al. Beta-adrenergic signaling accelerates and synchronizes cardiac ryanodine receptor response to a single L-type Ca2+ channel. . Proc Natl Acad Sci U S A. 2009;106(42):18028–18033. doi: 10.1073/pnas.0906560106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Fernandez-Velasco M, et al. Increased Ca2+ sensitivity of the ryanodine receptor mutant RyR2 R4496C underlies catecholaminergic polymorphic ventricular tachycardia. . Circ Res. 2009;104(2):201–209. doi: 10.1161/CIRCRESAHA.108.177493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Knollmann BC, et al. Casq2 deletion causes sarcoplasmic reticulum volume increase, premature Ca2+ release, and catecholaminergic polymorphic ventricular tachycardia. . J Clin Invest. 2006;116(9):2510–2520. doi: 10.1172/JCI29128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Rizzi N, et al. Unexpected structural and functional consequences of the R33Q homozygous mutation in cardiac calsequestrin: a complex arrhythmogenic cascade in a knock in mouse model. Circ Res. 2008;103(3):298–306. doi: 10.1161/CIRCRESAHA.108.171660. [DOI] [PubMed] [Google Scholar]
- 128.Faggioni M, Knollmann BC. Calsequestrin 2 and arrhythmias. Am J Physiol Heart Circ Physiol. 2012;302(6):H1250–H1260. doi: 10.1152/ajpheart.00779.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chopra N, et al. Ablation of triadin causes loss of cardiac Ca2+ release units, impaired excitation-contraction coupling, and cardiac arrhythmias. . Proc Natl Acad Sci U S A. 2009;106(18):7636–7641. doi: 10.1073/pnas.0902919106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Priori SG, Napolitano C, Di Pasquale E, Condorelli G. Induced pluripotent stem cell–derived cardiomyocytes in studies of inherited arrhythmias. J Clin Invest. 2013;123(1):84–91. doi: 10.1172/JCI62838. [DOI] [PMC free article] [PubMed] [Google Scholar]