Abstract
The induction of persistent intraepithelial CD8+ T cell responses may be key to the development of vaccines against mucosally transmitted pathogens, particularly for sexually transmitted diseases. Here we investigated CD8+ T cell responses in the female mouse cervicovaginal mucosa after intravaginal immunization with human papillomavirus vectors (HPV pseudoviruses) that transiently expressed a model antigen, respiratory syncytial virus (RSV) M/M2, in cervicovaginal keratinocytes. An HPV intravaginal prime/boost with different HPV serotypes induced 10-fold more cervicovaginal antigen-specific CD8+ T cells than priming alone. Antigen-specific T cell numbers decreased only 2-fold after 6 months. Most genital antigen-specific CD8+ T cells were intra- or subepithelial, expressed αE-integrin CD103, produced IFN-γ and TNF-α, and displayed in vivo cytotoxicity. Using a sphingosine-1-phosphate analog (FTY720), we found that the primed CD8+ T cells proliferated in the cervicovaginal mucosa upon HPV intravaginal boost. Intravaginal HPV prime/boost reduced cervicovaginal viral titers 1,000-fold after intravaginal challenge with vaccinia virus expressing the CD8 epitope M2. In contrast, intramuscular prime/boost with an adenovirus type 5 vector induced a higher level of systemic CD8+ T cells but failed to induce intraepithelial CD103+CD8+ T cells or protect against recombinant vaccinia vaginal challenge. Thus, HPV vectors are attractive gene-delivery platforms for inducing durable intraepithelial cervicovaginal CD8+ T cell responses by promoting local proliferation and retention of primed antigen-specific CD8+ T cells.
Introduction
An important role of CD8+ T cells is to clear intracellular pathogens through the interaction between their T cell receptor and pathogen-derived peptides presented in the groove of the MHC I at the surface of infected cells (1, 2). Because CD8+ T cells are activated by cell-to-cell interactions, it is assumed that memory CD8+ T cells present at the site of infection are advantageous for early control of infections. The ability to direct vaccine-induced CD8+ T cell responses to the female cervicovaginal mucosa may be critical to the successful development of prophylactic vaccines against some sexually transmitted viral infections, such as HIV and herpes simplex virus (HSV), as well as the development of therapeutic vaccines against human papillomaviruses (HPV) and the intraepithelial neoplasia that they induce. However, the female cervicovaginal mucosa is generally considered a difficult site in which to induce an immune response (3), and, with the exception of replication-competent microbial vectors (which raise safety concerns; refs. 4, 5), there is little evidence for effective vaccination via the female cervicovaginal mucosa (6, 7). Efforts to induce genital CD8+ T cell responses have therefore focused on either systemic immunization or mucosal immunization at distant sites, particularly the upper respiratory tract.
Studies have shown that after systemic immunization or viral infection, CD8+ T cells spread to virtually all peripheral tissues, where they can subsequently differentiate into effector memory cells with increased survival potential and distinct phenotypes influenced by their microenvironment (8–10). Furthermore, several systemic immunization strategies using live viruses, replication-defective viral vectors, or protein antigens and adjuvant have been shown to induce CD8+ T cell responses in the cervicovaginal mucosa in addition to systemic CD8+ T cell responses (11–13). Nevertheless, T cell trafficking is clearly regulated at the site of induction through the expression of an array of homing molecules such as integrins, addressins, and chemokine receptors (14). For instance, the acquisition of a gut-homing phenotype, characterized by the expression of CCR9 and integrin α4β7 by T cells after infection or immunization, is driven by the local environment, notably by local DCs, which may account for the preferential localization of effector CD8+ T cells at the site of viral infection or immunization (15–19). On the other hand, cervicovaginal T cells induced after vaginal Chlamydia infection display a different set of homing molecules compared with their intestinal counterpart and more closely resemble systemic T cells, as they express integrin β1, CCR5, and CXCR3 (20, 21). Other studies have shown that local immunization preferentially induces CD8+ T cell responses at the site of immunization, including the cervicovaginal mucosa, supporting the concept of anatomical compartmentalization of CD8+ T cell responses (22–25). In addition, the integrin αE(CD103)β7, a marker for intraepithelial lymphocytes, was shown to be upregulated by tissue-resident memory CD8+ T cells upon in situ antigen expression (26) and expressed by mucosal CD8+ T cells after viral infection (27, 28).
Together, these data suggest that local immunization may be better suited for the induction of local CD8+ T cells than a remote immunization regimen. However, to our knowledge there is no study that directly compares distant versus local mucosal immunization to determine whether the induced T cells reside in the epithelium, lamina propria, and/or the vasculature of the target mucosa. The generation of effector or effector memory T cells that home to the genital tract epithelium may be particularly advantageous for combating infections that are initiated and/or maintained in cervicovaginal keratinocytes, such as HSV and HPV (29, 30).
Most replication-defective viral vectors for genetic vaccination have been administered systemically and have successfully induced CD8+ T cell responses, but few of these vectors have been used for mucosal vaccination (31, 32). HPV pseudoviruses (PsV), composed of the viral L1 and L2 proteins and a double-stranded DNA pseudogenome, have several attractive features as vectors for genetic immunization of the female genital mucosa, which is the natural target tissue for many HPV types. They can encapsidate virtually any 6- to 8-kb circular target plasmid, and the target antigen(s) can be the only gene product(s) expressed (33). Titers of up to 1011 can easily be generated in tissue culture. Previous studies have shown that de novo expression of a reporter gene after intravaginal (Ivag) instillation of HPV PsV in mice (34) and non-human primates (35, 36) requires mild disruption of the epithelium and can be routinely accomplished by pretreatment with an over-the-counter spermicide containing nonoxynol-9 (N-9), a non-ionic detergent. Expression of the transduced gene is transient and restricted to cervicovaginal keratinocytes. Thus, the vectors can be used to test the specific hypothesis that transient expression limited to “wounded” keratinocytes can effectively induce mucosal immune responses.
In an initial study, we showed that Ivag vaccination with HPV PsV primed broad-based systemic and respiratory T and B cell responses against the M/M2 antigen from respiratory syncytial virus (RSV) (37). In the current study, we evaluated genital CD8+ T cell responses in mice after Ivag HPV PsV prime/boost immunization with M/M2-expressing vectors, using different HPV types in the prime and boost to overcome antibody-mediated neutralization of the vectors. The local versus distal mucosal and systemic responses were compared with those induced after delivery of the same vectors to the upper respiratory mucosa or induced by i.m. vaccination with standard adenovirus type 5 (Ad5) vectors, respectively. In addition, we investigated the phenotype and activity of the induced mucosal T cells, their localization within the cervicovaginal tissue, the site of their proliferation after primary or booster immunization, and the duration of the cervicovaginal CD8+ T cell response. Finally, the protection conferred by Ivag HPV PsV vaccination was assessed in an Ivag challenge with recombinant vaccinia virus (VV).
Results
Heterotypic HPV PsV prime/boost Ivag immunization overcomes type-specific antibody neutralization and enhances the frequency of CD8+ T cells in the cervicovaginal mucosa.
HPV PsV immunization can induce high-titer type-specific neutralizing antibodies, which could compromise a strategy that uses the same HPV PsV for prime and boost immunization. To determine whether a prime/boost strategy that uses heterotypic PsV could overcome this problem, we inoculated groups of 5 mice Ivag with 1 × 107 infectious units (IU) of HPV16 or HPV45 PsV encapsidating a plasmid encoding luciferase. Luciferase expression was monitored daily by measuring luciferase activity after Ivag luciferin instillation (expressed in photons/second [p/s]) in the genital area using a Xenogen IVIS imager. Following Ivag delivery of HPV16 or HPV45 luciferase PsV, luciferase expression peaked between days 2 and 3 and returned to baseline by day 5 for both serotypes (Supplemental Figure 1A; supplemental material available online with this article; doi: 10.1172/JCI63287DS1). Inoculation with 1 μg HPV16 PsV elicited type-specific serum neutralizing antibodies (geometric mean titer [GMT] range, 150–1350) (Supplemental Figure 1B and Supplemental Methods). Ivag delivery of 5 × 107 IU HPV16 luciferase PsV conferred complete protection against a subsequent secondary challenge with 5 × 107 IU HPV16 luciferase PsV but did not affect secondary challenge with 5 × 107 IU HPV45 luciferase PsV (Figure 1A).
Figure 1. Ivag heterologous prime/boost immunization regimen overcomes type-specific antibody neutralization and enhances CD8+ T cell response in the genital tract.
(A) Depo-Provera–treated BALB/c mice (n = 5/group) were inoculated Ivag with 5 × 107 IU HPV16 PsV expressing luciferase (16Luc) or sham treated. One month after initial 16Luc PsV inoculation, mice were challenged Ivag with 5 × 107 IU 16Luc or HPV45 PsV expressing luciferase (45Luc). In vivo luciferase expression was measured 2 days after Ivag challenge and is expressed as mean luminescence in photons per second + SD (**P < 0.01, Mann Whitney U test). (B) Depo-Provera–treated mice were immunized Ivag with 5 × 107 IU HPV PsV expressing the RSV fusion protein M/M2. For the single immunization regimen, mice were immunized with 5 × 107 IU HPV16MM2 PsV, and for the prime/boost regimen, they were immunized with 5 × 107 IU HPV16MM2; 1 month later the primed animals were immunized with 5 × 107 IU HPV45MM2. Two weeks after the final immunization, vaginal cell suspensions were analyzed by flow cytometry for the presence of KdM282-tetramer+CD8+ T lymphocytes. Data are expressed as the mean of the total number of cells per organ + SD (*P < 0.05, **P < 0.01, Kruskal-Wallis/Dunn’s test).
In other experiments, mice were immunized Ivag with 5 × 107 IU of an HPV16 PsV encapsidating a plasmid encoding M/M2 (a fusion protein of the RSV M and M2 protein) as a model antigen. Dominant CD8+ T cell responses directed against the Kd-restricted peptide (SYIGSINNI) from the M2 protein were measured by flow cytometry using allophycocyanin-conjugated (APC-conjugated) KdM282–90 tetramer (KdM282-tetramer). Two weeks after a single Ivag immunization with HPV16-MM2 PsV, KdM282-tetramer+CD8+ T cells were readily detected in the cervicovaginal mucosa. However, upon a secondary immunization with HPV45-MM2 PsV, the number of KdM282-tetramer+CD8+ T cells per cervicovaginal mucosa increased 10-fold compared with single immunization (Figure 1B). In other experiments, mice were primed with HPV16-MM2 PsV and boosted with either HPV16-MM2 PsV or HPV45-MM2 PsV. Homologous prime/boost immunization did not result in an enhanced number of KdM282-tetramer+CD8+ T cells compared with N-9, suggesting that de novo antigen expression is required for the enhancement of genital CD8+ T cell responses (Supplemental Figure 2). These results underscore the advantage of heterotypic prime/boost immunization regimen to increase genital CD8+ T cell responses after HPV PsV Ivag immunization.
Prime/boost Ivag immunization regimen with HPV PsV induces intraepithelial CD8+ T cells in the cervicovaginal mucosa.
To evaluate in more detail the CD8+ T cell response induced by the HPV PsV immunization, groups of 5–7 mice were primed Ivag with HPV16-MM2 PsV (5 × 107 IU) and 1 month later were boosted Ivag with HPV45-MM2 PsV (5 × 107 IU). Two weeks after the second immunization, the presence of KdM282-tetramer+CD8+ T cells was measured by flow cytometry. Prime/boost Ivag immunization with HPV-MM2 PsV induced a 10-fold increase in the percentage of total CD8+ T cells (15.5%) of a cervicovaginal cell suspension compared with HPV-control PsV (1.57%), whereas the percentage of CD4+ T cells (11% in HPV-control vs. 9.6% in HPV-MM2) remained unchanged (Figure 2A). Remarkably, the majority of the cervicovaginal CD8+ T cells induced after Ivag immunization were specific for the immunodominant M282–90 epitope (Figure 2A). Thus, most of the increase in cervicovaginal CD8+ T cells observed after HPV-MM2 PsV immunization was attributable to the CD8+ T cell response against the Kd-restricted M282–90 epitope. This was confirmed by the analysis of the absolute number of cervicovaginal CD8+ T cells and KdM282-tetramer+CD8+ T cells (Figure 2B).
Figure 2. HPV Ivag prime/boost immunization induces high numbers of cervicovaginal CD8+ T cells.
Depo-Provera–treated mice (n = 5/group) were immunized with 5 × 107 IU HPV16MM2 or HPV16 control (HPV-CTL) Ivag, and 1 month later, primed mice were immunized with 5 × 107 IU HPV45MM2 or HPV45 control, respectively. Two weeks after the second immunization, cervicovaginal cell suspensions were analyzed by flow cytometry for the presence of KdM282-tetramer+CD8+ T lymphocytes in HPVMM2-immunized and sham-treated animals. (A) CD8 and CD4 expression on gated vaginal cells with a lymphocyte morphology (contour plot) and KdM282-tetramer binding on gated CD8+ T cells (histogram plot); the percentage of each gate and marker of the parent population is indicated in each plot. (B) Total CD8+ T lymphocytes and KdM282-tetramer+CD8+ T lymphocytes per cervicovaginal mucosa. Data are representative of more than 3 experiments (*P < 0.05, **P < 0.01, Mann-Whitney U test).
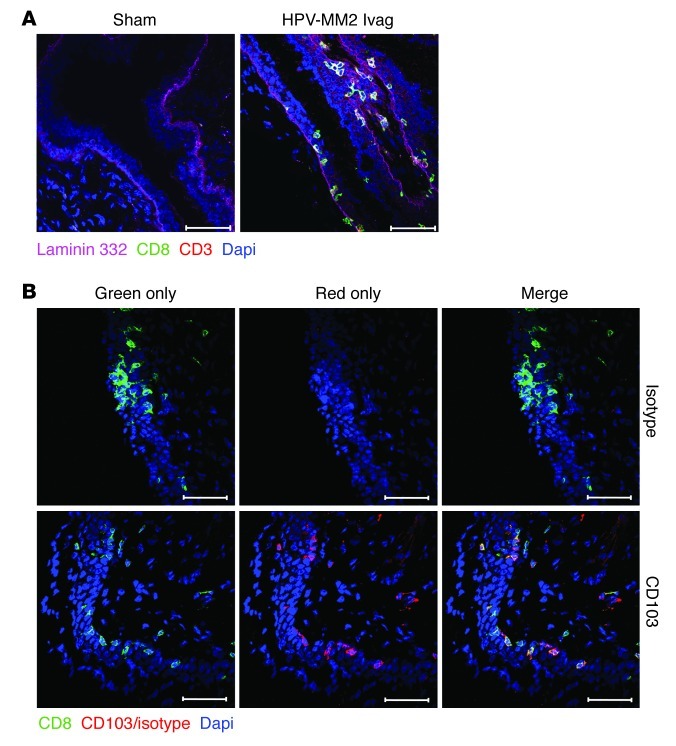
Next we used confocal microscopy to determine the localization in the cervicovaginal mucosa of the CD8+ T cells induced after HPV PsV Ivag immunization. Tissue sections were stained with laminin 332 antibody to delineate the basement membrane and with CD8 and CD3 antibodies to detect CD8+ T cells. To our surprise, the cervicovaginal mucosa of the control animals was essentially devoid of CD8+ T cells associated with the epithelium (Figure 3A). By contrast, the cervicovaginal mucosa of immunized animals displayed high numbers of CD8+ T cells lining, within, or beneath the epithelium (Figure 3A). Further staining of cervicovaginal tissue sections revealed that most intraepithelial CD8+ T cells expressed αE-integrin (CD103), a cell surface marker often associated with bona fide intraepithelial T cells (Figure 3B).
Figure 3. HPV Ivag prime/boost immunization induces CD103+ cervicovaginal intraepithelial CD8+ T cells.
Depo-Provera–treated mice (n = 5/group) were immunized with 5 × 107 IU HPV16MM2 or HPV16 control Ivag, and 1 month later, primed mice were immunized with 5 × 107 IU HPV45MM2 or HPV45 control, respectively. Two weeks after the second immunization, the distribution of CD8+ T cells was analyzed in cervicovaginal tissue section from HPVMM2-immunized and sham-treated animals. (A) Cervicovaginal tissue section stained with CD8 (green), CD3 (red), laminin 332 (magenta), and DAPI (blue). (B) Cervicovaginal tissue sections from HPVMM2-immunized mice were stained with CD8 (green), isotype control (upper images), or CD103 (lower images; red) antibodies and DAPI (blue). Single channel for CD8 staining (green only) and CD103/isotype control (red only) and merge. Scale bars: 50 μm. Images are representative of 5 animals tested for each condition examined.
Prime/boost Ivag immunization regimen with HPV PsV induces systemic CD8+ T cell responses.
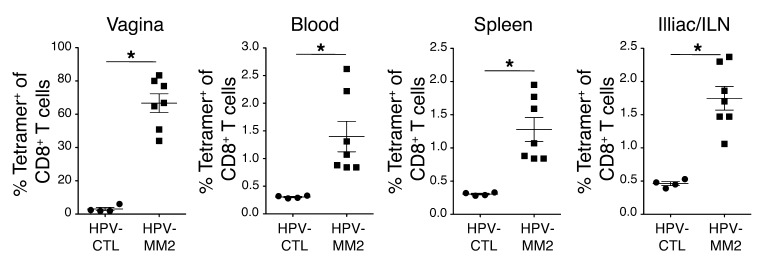
We further analyzed the tissue distribution of CD8+ T cell responses 2 weeks after HPV-MM2 PsV Ivag prime/boost immunization in the cervicovaginal mucosa, blood, spleen, and draining lymph nodes (Figure 4). In the cervicovaginal mucosa, 61% of CD8+ T cells were KdM282-tetramer+, whereas the average frequency of KdM282-tetramer+CD8+ T cells was much lower in blood (1.4%), spleen (1.3%), and ilio-sacral/inguinal lymph nodes (ILNs) (1.7%). These results indicate that HPV PsV prime/boost Ivag immunization can induce systemic CD8+ T cell responses but it preferentially induces cervicovaginal CD8+ T cells responses.
Figure 4. HPV Ivag prime/boost immunization induces local and systemic CD8+ T cell responses.
Depo-Provera–treated mice were immunized with 5 × 107 IU HPV16MM2 or HPV16 control Ivag, and 1 month later, primed mice were immunized with 5 × 107 IU HPV45MM2 or HPV45 control, respectively. Two weeks after the final immunization, cervicovaginal, blood, spleen, and ILN cell suspensions were analyzed by flow cytometry for the presence of KdM282-tetramer+CD8+ T cells. Data are representative of more than 3 experiments (*P < 0.05, Mann-Whitney U test).
Ivag immunization with HPV pseudovirions induces durable effector-memory CD8+ T cell responses in the cervicovaginal mucosa and in lymphoid tissues.
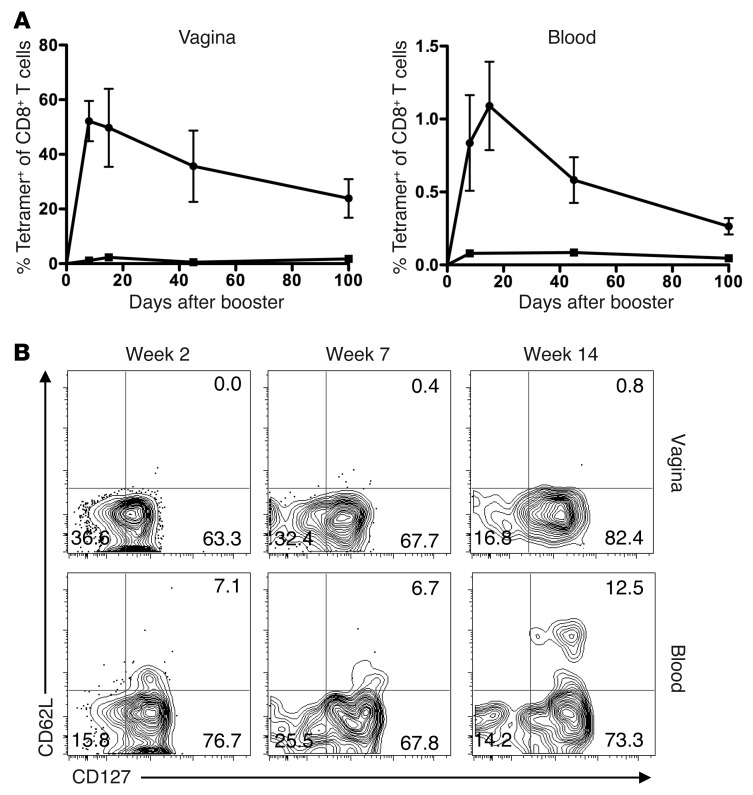
Durability of CD8+ T cell responses, especially in the cervicovaginal mucosa, is a critical parameter for many applications of vaccines against sexually transmitted infection. After prime/boost Ivag immunization with 5 × 107 IU of HPV-MM2 PsV, we monitored the KdM282-specific CD8+ T cell response in blood, spleen, ILN, and cervicovaginal mucosa from week 1 to week 14 after boost. In all organs tested, the KdM282-specific CD8+ T cell responses peaked between weeks 1 and 2 (Figure 5A). At week 7, the KdM282-specific CD8+ T cell response in the cervicovaginal mucosa had declined by only 15%, compared with week 1, whereas the response in blood had undergone a 2-fold decline (Figure 5A). At week 14, KdM282-tetramer+CD8+ T cells in the genital tract had declined approximately 2-fold and still accounted for 24% of total CD8+ T cells in the cervicovaginal mucosa, whereas the frequency in blood was less than 0.5%. These results indicate that HPV PsV Ivag prime/boost immunization induces long-lasting CD8+ T cell responses in the cervicovaginal mucosa.
Figure 5. HPV PsV Ivag prime/boost immunization induces durable CD8+ T cell responses with an effector memory phenotype after HPV PsV Ivag immunization.
Depo-Provera–treated mice were immunized with 5 × 107 IU HPV16MM2 or HPV16 control Ivag, and 1 month later mice were immunized with 5 × 107 IU HPV45MM2 or HPV45 control, respectively. (A) Cervicovaginal and blood cell suspensions were obtained from week 1 to week 14 and analyzed by flow cytometry for the presence of KdM282-tetramer+CD8+ T lymphocytes in HPVMM2 (squares) and HPV control (circles). Data are expressed as the mean percentage of KdM282-tetramer+CD8+ T lymphocytes in total CD8+ T lymphocytes + SD. (B) Representative plots of CD62L and CD127 expression of KdM282-tetramer+CD8+ T lymphocytes in cervicovaginal and blood cells suspensions collected at weeks 2, 7, and 14. The percentage of CD8+ T cells in each quadrant is indicated in each plot. Data are representative of 3 experiments.
Next, we assessed the T cell memory phenotype induced after HPV PsV Ivag immunization. Previous studies have shown that effector, effector-memory, and central memory T cell populations can be distinguished based on their expression of IL-7 receptor (CD127) and L-selectin (CD62L), which reflects their differential migratory, survival, and protective potential (38–40). We used multi-parametric flow cytometry to analyze the expression of CD62L and CD127 by KdM282-tetramer+CD8+ T cells in the cervicovaginal mucosa and blood from animals at week 2 to week 14 after booster immunization. In the cervicovaginal mucosa at the peak of the secondary response, KdM282-specific CD8+ T cells were distributed between CD62L–CD127+ (effector-memory) and CD62L–CD127– (effector) cells (Figure 5B). By week 14, the proportion of effector-memory KdM282-specific CD8+ T cells had increased, consistent with the known properties of short-lived effector T cells relative to effector-memory T cells (Figure 5B). At no time point were significant numbers of central memory KdM282-specific CD8+ T cells detected in the cervicovaginal mucosa, consistent with their propensity to localize in lymph nodes. In the blood, 2 weeks after booster immunization, the majority (70%) of KdM282-specific CD8+ T cells were effector-memory cells, whereas central memory and effector cells accounted for 7% and 15% of KdM282-specific CD8+ T cells, respectively (Figure 5B). These results indicate that Ivag immunization with HPV PsV induces predominantly long-lived effector-memory CD8+ T cells and that many of these cells reside at the side of inoculation in the cervicovaginal mucosa.
Ivag immunization with HPV pseudovirions induces CD8+ T cells able to produce multiple cytokines and have cytotoxic activity.
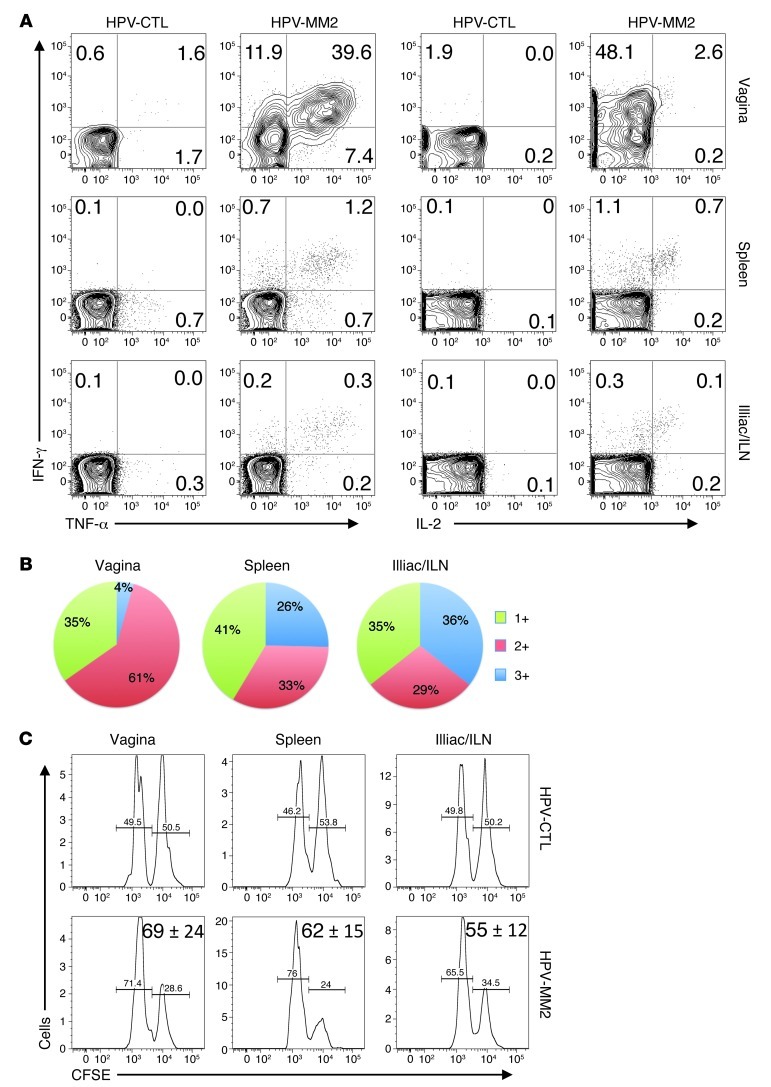
Multiple functions (e.g., cytokine production and cytotoxicity) displayed by CD8+ T cells are usually associated with a response of better quality in the settings of viral infections, and such functions simultaneously displayed are considered as predictive markers of protective CD8+ T cells induced by vaccination (41). We evaluated the ability of KdM282-specific CD8+ T cells induced after HPV PsV Ivag immunization to produce IFN-γ, TNF-α, and IL-2 using intracellular cytokine staining after in vitro restimulation with M282–90 peptide. Two weeks after booster HPV PsV immunization, cell suspensions of cervicovaginal mucosa, spleen, and ILN were stimulated for 5 hours in vitro with 5 μM M282–90 or without peptide. After surface staining with CD3, CD4, and CD8 antibodies, we performed intracellular cytokine staining with IFN-γ, TNF-α, and IL-2 antibodies or isotype control antibodies. In the cervicovaginal mucosa, an average of 58% of CD8+ T cells produced at least 1 cytokine after M282–90 in vitro stimulation, which is concordant with the high percentage of KdM282-tetramer+CD8+ T cells detected in the cervicovaginal tissue (Figure 6). In the ILN and spleen, the average percentages of cytokine-producing CD8+ T cells were 0.5% and 1%, respectively, which correlates with the percentage of KdM282-tetramer+CD8+ T cells in each organ (Figure 6). In the cervicovaginal mucosa, 51% of CD8+ T cells produced IFN-γ, 47% produced TNF-α, and less than 3% of CD8+ T cells produced IL-2 (Figure 6A and Supplemental Figure 3). The percentage of peptide-stimulated CD8+ T cells producing 1, 2, or 3 cytokines from the cervicovaginal mucosa, spleen, and ILN was further analyzed and is represented in Figure 6B. In the genital tract, the majority of the cytokine-producing CD8+ T cells (61%) produced 2 cytokines, predominantly IFN-γ and TNF-α (Supplemental Figure 3). Single-cytokine-producing cells represented 35% of the total cytokine-producing cells; they produced IFN-γ or TNF-α but not IL-2 (Supplemental Figure 3). Only 4% of cervicovaginal CD8+ T cells simultaneously produced all 3 cytokines. In contrast, ILN and spleen cytokine-producing CD8+ T cells were more evenly distributed among triple-, double-, and single-cytokine-producing profiles (Figure 6B). In the ILN and spleen, most double-cytokine-producing CD8+ T cells produced IFN-γ and TNF-α (Supplemental Figure 3), and most of the IL-2 was produced by triple-producing CD8+ T cells (Figure 6B and Supplemental Figure 3). The difference in cytokine production by the cervicovaginal CD8+ T cells versus secondary lymphoid organ CD8+ T cells may be due to the preferential induction of effector-memory CD8+ T cells in the cervicovaginal mucosa and the selective induction of central memory CD8+ T cells in secondary lymphoid organs after HPV PsV Ivag immunization.
Figure 6. HPV Ivag prime/boost immunization induces polyfunctional CD8+ T cells with cytotoxic activity.
Depo-Provera–treated mice were immunized with 5 × 107 IU HPV16MM2 or HPV16 control Ivag, and 1 month later, mice were immunized with 5 × 107 IU HPV45MM2 or HPV45 control, respectively. (A) Two weeks after the last immunization, the production of IFN-γ, TNF-α, and IL-2 by CD8+ T cells was measured after in vitro stimulation with M282–90 peptide in cervicovaginal, spleen, and ILN cell suspensions. The percentage of CD8+ T cells in each quadrant is indicated in each plot. (B) Relative proportion of single-, double-, and triple-cytokine-producing CD8+ T cells restimulated with M282–90 peptide after subtraction of background cytokine production of unstimulated CD8+ T cells. (C) In vivo cytotoxic activity was assessed 2 weeks after the last immunization. Target cells consisting of an equal mixture of two splenocyte populations labeled with a high and a low concentration of CFSE were pulsed with M282–90 peptide or remained unpulsed, respectively, were injected Ivag and i.v. Twenty-four hours later, cervicovaginal, spleen, and ILN cell suspensions were analyzed by flow cytometry. Representative histograms gated on CFSE-positive cells. Mean percentage ± SD of M282–90 specific lysis is indicated.
In addition to cytokine production, we assessed the cytotoxic activity of the CD8+ T cells induced after HPV PsV immunization and measured in vivo the presence of bona fide CTLs against the M282–90 epitope. Cytotoxic activity was measured in vivo by injection of target cells, which consisted of a mixture of spleen cells that had been either pulsed with M282–90 peptide or mock treated and had been labeled, respectively, with high or low concentrations of CFSE. Target cells were injected simultaneously i.v. and subdermally in the vaginal wall, and 18 hours after injection KdM282-specific in vivo cytotoxicity was assessed by flow cytometry in cervicovaginal mucosa, ILN, and spleen cell suspensions. Two weeks after the booster immunization, immune mice displayed 74% specific lysis in the cells from the cervicovaginal mucosa, 65% in those from the spleen, and 69% in the ILN cells (Figure 6C). Together, these results indicate that HPV PsV Ivag prime/boost immunization induces polyfunctional CD8+ T cells and bona fide CTL in the cervicovaginal mucosa and in the systemic compartment.
Naive CD8+ T cells are primed in the genital draining lymph nodes after HPV PsV Ivag immunization.
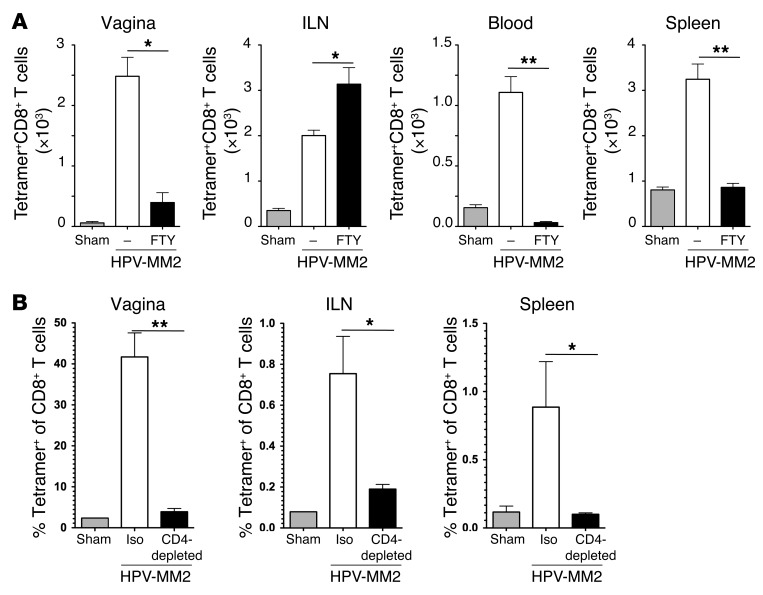
Because, the Ivag prime/boost immunization regimen with HPV PsV is so potent at inducing genital CD8+ T cell responses, we first sought to determine whether CD8+ T cells were primed in the cervicovaginal mucosa or in the genital draining lymph node (Figure 7A). FTY720 promotes the retention of naive lymphocytes in the lymph nodes leading to severe lymphopenia in blood and has been a useful tool for analyzing the dynamics of T cell responses during infection or vaccination (42–44). Therefore, mice were treated with FTY720 in drinking water from day 1 after immunization until the end of the experiment on day 14. As expected, FTY720 treatment abrogated the KdM282-tetramer+CD8+ T cell responses in the blood and spleen after a single HPV PsV Ivag immunization (Figure 7A). FTY720 treatment induced a 5-fold decrease in the number of KdM282-tetramer+CD8+ T cells compared with mock-treated mice in the cervicovaginal mucosa but did not completely abrogate the CD8+ T cell response (Figure 7A). Interestingly, analysis of the phenotype of KdM282-tetramer+CD8+ T cells in the cervicovaginal mucosa showed that in FTY720-treated animals, 81% of genital KdM282-tetramer+CD8+ T cells were effector cells, whereas in mock-treated animals, 61% of KdM282-tetramer+CD8+ T cells were effector memory cells (Supplemental Figure 4). In the draining lymph nodes, the expected increase in the number of KdM282-tetramer+CD8+ T cells in FTY720-treated animals compared with mock-treated mice was observed (Figure 7A). The phenotype of the KdM282-tetramer+CD8+ T cells in FTY720-treated as well as mock-treated animals was predominantly effector-memory (Supplemental Figure 4). These data suggest that ILNs are the primary site of priming of CD8+ T cell responses during HPV PsV immunization and that the CD8+ T cell response in spleen and in the cervicovaginal mucosa requires systemic circulation through the bloodstream after priming.
Figure 7. Primary CD8+ T cell responses are induced in the ILN and are abrogated in the absence of CD4+ T cell help.
Mice (n = 5/group) were treated with FTY720 in drinking water from day 1 to day 14 after single or booster immunization (A). On day 14, vagina, ILN, spleen, and blood cell suspensions were analyzed by flow cytometry for the presence KdM282-tetramer+CD8+ T lymphocytes. Data are expressed as mean + SD of the total number of KdM282-tetramer+CD8+ T lymphocytes per organ or per milliliter of blood. (B) To evaluate the role of CD4+ T cell help in the induction of CD8+ T cell responses, mice were injected i.p. every second day with rat anti-mouse CD4 or isotype control (iso) antibody from day –3 to day 9 relative to the day of immunization. Two weeks after immunization, vagina, ILN, and spleen were analyzed by flow cytometry for the presence KdM282-tetramer+CD8+ T cells. Data are expressed as the mean + SD percentage of KdM282-tetramer+CD8+ T cells in CD8+ T cells. Data are representative of 3 experiments (*P < 0.05, **P < 0.01, Kruskal-Wallis/Dunn’s test).
Primary CD8+ T cell responses are abrogated in the absence of CD4+ cells after a single HPV Ivag immunization.
We also assessed the role of CD4+ T cells in the induction of primary CD8+ T cell response after a single HPV Ivag immunization. Mice received CD4-depleting antibody by i.p. injection every other day from 3 days prior to immunization until 9 days after the day of immunization. In preliminary experiments, we evaluated the efficacy of CD4+ T cell depletion, which was >90% in the genital tract and >95% in the lymph node (Supplemental Figure 5 and unpublished observations). In addition, neither plasmacytoid DCs nor conventional DCs were depleted by the CD4 antibody treatment, even though they have been shown to express CD4 in mice (ref. 45, Supplemental Figure 5, and unpublished observations). CD4 depletion did not affect the efficacy of HPV-mediated gene delivery in vivo (Supplemental Figure 5), but it completely abrogated the IgG response against the major protein (L1) of the HPV capsid (Supplemental Figure 6A). KdM282-specific CD8+ T cell responses were assessed in the vagina, ILN, and spleen on day 14 (Figure 7B). In vivo CD4 depletion completely abrogated KdM282-specific CD8+ T cell responses in the cervicovaginal tract and spleen (Figure 6B). However, residual KdM282-tetramer+CD8+ T cells were detected in the ILN (Figure 6B), and these cells exhibited predominantly a central memory phenotype (Supplemental Figure 6C). These data indicate that CD4+ T cells play a critical role in the induction of effector and effector-memory CD8+ T cell responses after HPV PsV immunization but that their role is at least partially dispensable for the induction of central memory CD8+ T cells in the ILN.
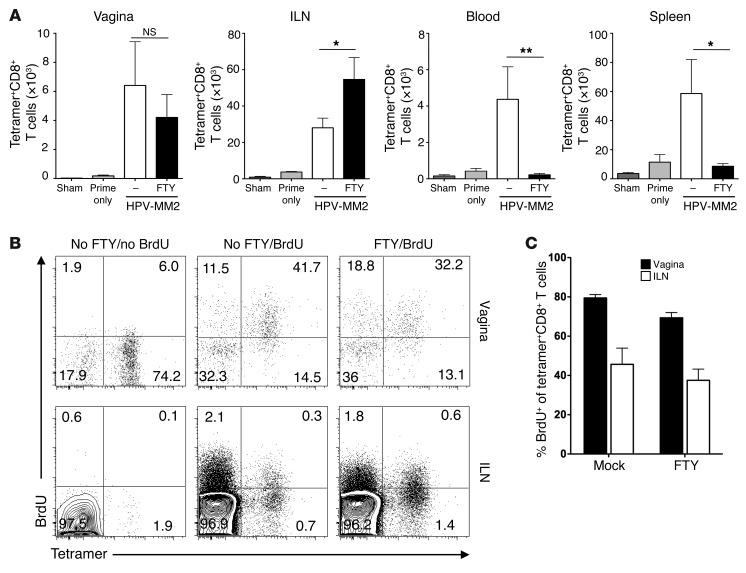
Secondary CD8+ T cell responses expand locally in the cervicovaginal mucosa and in the ILN upon secondary HPV PsV Ivag immunization.
Because a single HPV PsV Ivag immunization induced a strong CD8+ T cell response in the cervicovaginal mucosa, we sought to analyze the behavior of resident effector-memory CD8+ T cells upon a secondary Ivag immunization with HPV PsV (Figure 8). We used FTY720 treatment to evaluate whether the dynamics of the secondary CD8+ T cell response would differ from the dynamics of the primary CD8+ T cell response after Ivag HPV PsV booster immunization (44). Mice were primed with HPV16 PsV Ivag in the absence of FTY720 and 1 month later received an Ivag HPV45 PsV booster immunization with or without FTY720 treatment from day 1 to day 14 after booster immunization. While CD8+ T cell responses were still detected in the cervicovaginal mucosa, blood, ILN, and spleen 1 month after priming, CD8+ T cell responses were, as expected, further enhanced after a booster immunization in mice not treated with FTY720 (Figure 8A). In spleen and blood, boosted animals that were FTY720 treated had CD8+ T cell responses that were similar to those in primed-only animals, indicating that FTY720 treatment abrogated secondary CD8+ T cell responses in these organs (Figure 8A). In the ILN of FTY720-treated animals, CD8+ T cell responses were increased compared with mock-treated animals, indicating that memory CD8+ T cells present in the lymph node could further expand locally upon secondary Ivag HPV PsV immunization (Figure 8A). In the cervicovaginal mucosa, FTY720 treatment during booster immunization only modestly reduced the secondary CD8+ T cell response by a non-significant 25% (Figure 8A), in marked contrast to the large reduction in cervicovaginal CD8+ T cells when FTY720 treatment was given during priming (Figure 7A). Remarkably, in FTY720-treated animals, secondary genital KdM282-specific CD8+ T cells were predominantly effector-memory cells, as was the case with mock-treated animals (Supplemental Figure 4), which suggest that FTY720 treatment did not alter the acquisition of this memory phenotype.
Figure 8. Memory CD8+ T lymphocytes can expand locally in the vagina upon booster Ivag immunization with HPV.
Depo-Provera–treated mice (n = 5/group) were immunized Ivag with 5 × 107 IU HPV16MM2, followed 1 month later by a second immunization with 5 × 107 IU. On day 14, vagina, ILN, spleen, and blood cell suspensions were analyzed by flow cytometry for the presence KdM282-tetramer+CD8+ T lymphocytes (A). Data are expressed as mean + SD of the total number of KdM282-tetramer+CD8+ T lymphocytes per organ or per ml of blood. FTY, FTY720. (B and C) Mice received BrdU per os after the boost to measure in vivo proliferation of KdM282-tetramer+CD8+ T cells in FTY720- or mock-treated mice upon secondary immunization. Two weeks after boost, incorporation of BrdU by KdM282-tetramer+CD8+ T cells was measured by intracellular staining of cervicovaginal and ILN cell suspensions and further analyzed by flow cytometry. (B) Representative plot of BrdU and KdM282-tetramer staining of CD8+ T cells (percentage of CD8+ T cells in each quadrant is indicated). (C) Mean + SD percentage of BrdU+ relative to KdM282-tetramer+CD8+ T cells. Data are representative of 2 (A) and 3 (B) experiments (*P < 0.05, **P < 0.01, Kruskal-Wallis/Dunn’s test).
In some experiments, mice received both FTY720 and BrdU in drinking water from day 1 to day 14 after booster immunization to evaluate the proliferation in vivo of KdM282-specific CD8+ T cells. ILN, spleen, and cervicovaginal mucosa cell suspensions were obtained on day 14 after boosting, and surface staining was performed for detection of KdM282-tetramer+CD8+ T cells, followed by intracellular staining for BrdU incorporation (Figure 8B). In the ILN of FTY720-treated animals, BrdU incorporation by KdM282-tetramer+CD8+ T cells (40%) was similar to BrdU incorporation in mock-treated animals, which indicates that FTY720 treatment had no effect on cell proliferation in the draining lymph nodes (Figure 8C). Thus, the non-significant increase in the number of KdM282-tetramer+CD8+T cells in the ILN of FTY720-treated animals compared with mock-treated animals likely resulted from the impaired migratory properties of KdM282-tetramer+CD8+ T cells.
Remarkably, in mock-treated mice, up to 80% of cervicovaginal KdM282-tetramer+CD8+ T cells had incorporated BrdU within 2 weeks after the booster immunization, whereas BrdU incorporation in nonspecific CD8+ T cells was modest (20%) and probably accounted for by homeostatic proliferation (Figure 8B). In the cervicovaginal mucosa of FTY720-treated mice, 80% of KdM282-tetramer+CD8+ T cells also incorporated BrdU (Figure 8B), indicating recent proliferation upon booster immunization. Because FTY720 treatment abrogated the circulation of KdM282-specific CD8+ T cells in blood, these data suggest that upon booster Ivag immunization, secondary CD8+ T cell responses can proliferate in the cervicovaginal mucosa in response to de novo antigen expression by genital keratinocytes.
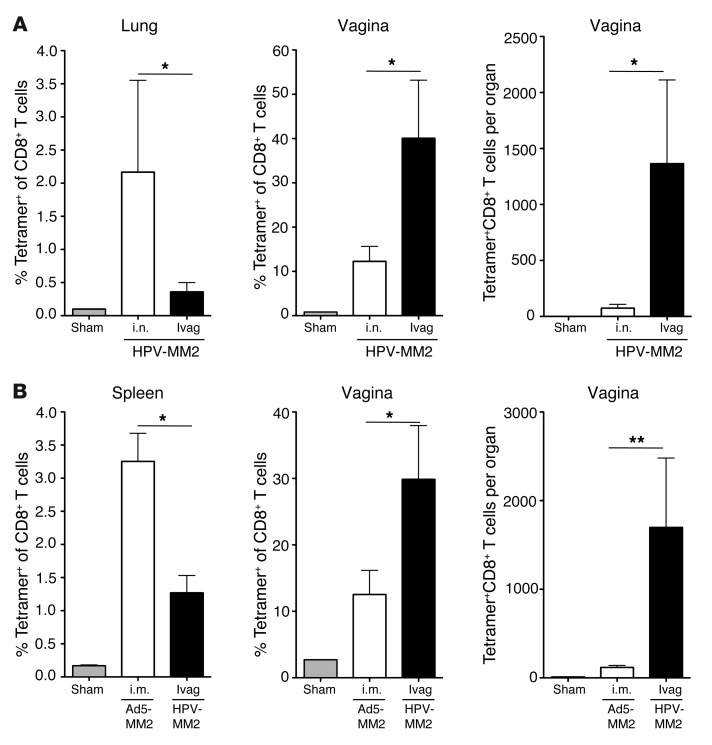
HPV PsV prime/boost Ivag immunization induces more potent CD8+ T cell responses in the cervicovaginal mucosa than does prime/boost immunization at remote sites.
We next compared genital CD8+ T cell responses in the cervicovaginal mucosa induced by HPV Ivag immunization versus other well-characterized routes of immunization. Intranasal immunization has been shown to induce CD8+ T cell responses in the upper respiratory tract as well as remote CD8+ T cell responses in the cervicovaginal mucosa (24). Efficient i.n. gene delivery of HPV PsV required mild disruption of the nasal epithelium using a lower dose of N-9 (0.2%). After i.n. prime/boost immunization with 5 × 107 IU HPV-MM2 PsV, 12% of cervicovaginal CD8+ T cells were KdM282-tetramer+, which was much lower than the frequency of KdM282-tetramer+CD8+ T cells (40%) after HPV PsV Ivag immunization (Figure 9A). The difference was even more striking when analyzed in terms of absolute numbers of cells, as Ivag prime/boost immunization induced 10 times more cervicovaginal KdM282-tetramer +CD8+ T cells than i.n. immunization. Conversely, i.n. prime/boost immunization induced a higher frequency of KdM282-tetramer +CD8+ T cells (2.1%) in the lungs than Ivag immunization (0.3% of CD8+ T cells) (Figure 9A).
Figure 9. HPV Ivag prime/boost immunization preferentially induces genital CD8+ T lymphocyte responses compared with HPV IN and Ad5 IM immunization.
Depo-Provera–treated mice were immunized Ivag or i.n. with 5 × 107 IU HPV16MM2 and 1 month later received a second immunization of 5 × 107 IU HPV45MM2, or mice were immunized i.m. twice, 1 month apart, with 5 × 106 PFU Ad5-MM2. Two weeks after the last immunization, lung, spleen, and cervicovaginal cell suspensions were analyzed by flow cytometry for the presence of KdM282-tetramer+CD8+ T lymphocytes. Data are expressed as the mean ± SD percentage or total number per organ of KdM282-tetramer+ of CD8+ T lymphocytes. Data are representative of 2 (A) and 3 (B) experiments (*P < 0.05, **P <0.01, Kruskal-Wallis/Dunn’s test).
Intramuscular immunization with adenoviral vectors has been reported to induce potent CD8+ T cell responses in the cervicovaginal mucosa (13, 46). Consistent with these data, i.m. prime/boost immunization with 5 × 106 PFU of Ad5-MM2 induced a strong CD8+ T cell response in the spleen and cervicovaginal mucosa, with 3.3% and 12.9% of KdM282-tetramer +CD8+T cells, respectively (Figure 9B). After HPV PsV Ivag immunization, the frequency of KdM282-tetramer + in CD8+ T cells (30%) was 2.5 times higher than after Ad5 intramuscular immunization in the cervicovaginal mucosa (Figure 9B). More strikingly, the absolute number of KdM282-tetramer+CD8+ T cells in the cervicovaginal mucosa after HPV PsV immunization was 10 times higher than after Ad5 intramuscular immunization (Figure 9B). In contrast, the M282–90–specific CD8+ T cell response in the spleen after HPV PsV Ivag immunization was less than half that induced by Ad5 intramuscular immunization (Figure 9B). Taken together, these data indicate that HPV PsV Ivag immunization is more effective than remote immunization regimens for the preferential induction of CD8+ T cell responses in the cervicovaginal mucosa.
HPV PsV Ivag, but not Ad5 i.m., prime/boost immunization induces high numbers of intraepithelial KdM282-tetramer+CD8+ T cells with restricted CD103 expression in the cervicovaginal epithelium.
As shown above, HPV PsV Ivag immunization induced high numbers of intraepithelial CD8+ T cells (Figure 3), and Ad5 i.m. immunization induced KdM282-tetramer+CD8+ T cell responses in the cervicovaginal mucosa (Figure 9B). We therefore analyzed the distribution of CD8+ T cells in the cervicovaginal mucosa by immunofluorescence staining of tissue sections from mice prime/boost immunized Ivag or i.m. with HPV PsV or Ad5 vectors, respectively (Figure 10A). As previously noted, the cervicovaginal epithelium of sham-treated mice was devoid of CD8+ T cells, whereas HPV PsV Ivag prime/boost immunization induced numerous CD8+ T cells within or beneath the epithelium (Figure 10A). Strikingly, the cervicovaginal epithelium of mice prime/boost immunized i.m. with 5 × 107 PFU of Ad5-MM2 vector was devoid of CD8+ T cells (Figure 10A), despite the fact that KdM282-tetramer+CD8+ T cells could be readily detected by flow cytometry. This surprising result suggests that i.m. immunization fails to induce intraepithelial T cells. The induced T cells detected by flow cytometry may instead be associated with the vasculature or remain deeper in the cervicovaginal tissue, and so are either lost during processing or not seen in the stained sections. We also compared expression of the CD103 integrin on KdM282-tetramer+CD8+ T cells in the cervicovaginal mucosa, blood, and ILN 4 weeks after the booster doses (Figure 10B). After Ivag immunization, most KdM282-tetramer+CD8+ T cells were CD103+ in the genital tract (80%), few were positive in the ILN (17%), and a negligible number were positive in blood (Figure 10B). Importantly, i.m. prime/boost induced a very different pattern of CD103 expression; it was detected on only 14% of the KdM282-tetramer+CD8+ T cells in the cervicovaginal mucosa and was nearly absent in blood and ILN (Figure 10B). Together, these data suggest that CD103 is differentially upregulated on CD8+ T cells exposed to antigens expressed transiently in the genital tract and may account for the preferential intraepithelial localization of CD8+ T cells after Ivag but not after i.m. immunization.
Figure 10. HPV Ivag, but not Ad5 i.m., prime/boost immunization induces intraepithelial CD8+ T cells in the cervicovaginal epithelium.
Depo-Provera–treated mice were immunized with 5 × 107 IU HPV16MM2 Ivag or with 5 × 107 PFU Ad5-MM2 i.m., and 1 month later mice were immunized with 5 × 107 IU HPV45MM2 or Ad5-MM2 i.m., respectively. (A) Two weeks after the last immunization, cervicovaginal tissue sections were co-stained for CD8 (green), CD3 (red), laminin 332 (magenta), and nuclei (blue). Scale bars: 50 μm. Images are representative of 5 animals tested for each condition examined. (B) In separate experiments, CD103 expression by KdM282-tetramer+CD8+ T lymphocytes was analyzed by flow cytometry in cervicovaginal, ILN, and blood cell suspensions from HPV Ivag and Ad5 i.m. immunized animals. Control isotype (red lines) and CD103 antibody (blue lines) staining is shown in B, and the percentage of CD103+ cells is indicated in the histogram plots. Data are representative of 3 experiments.
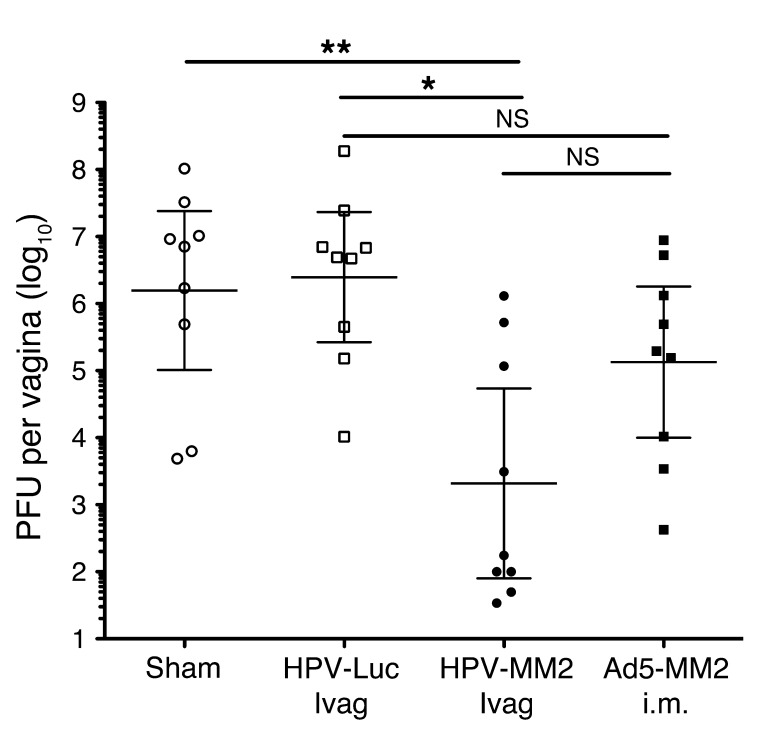
HPV Ivag prime/boost immunization confers protection against recombinant vaccinia vaginal challenge.
We further analyzed the potential of HPV Ivag prime/boost immunization to confer protection to a model infectious agent for genital infection, recombinant VV. VV typically infects stratified squamous epithelium and has been used previously to infect the vaginal mucosa (7, 22). We used a recombinant VV expressing the M282–90 epitope (rVV-M282–90) (47) to assess the protective potential of cervicovaginal M282–90–specific CD8+ T cells induced after HPV Ivag or Ad5 i.m. prime/boost immunization (Figure 11). Two months after the last immunization, mice received 107 PFU of rVV-M282–90 Ivag, and on day 3 after challenge, cervicovaginal mucosa was collected and homogenates assessed for rVV-M282–90 content by plaque assay. Recombinant VV-M282–90 titer did not differ significantly between sham-treated and HPV-Luc–treated mice, with rVV-M282–90 geometric mean titers of 1.6 × 106 and 2.5 × 106 PFU per organ, respectively (Figure 11). In contrast, HPV-MM2–immunized mice showed a statistically significant 1,000-fold-lower VV titer in cervicovaginal homogenate (2.1 × 103 PFU per organ) compared with control groups, implying that M282–90–specific CD8+ T cells played a key role in controlling VV replication in the vagina. Importantly, the Ad5-MM2 i.m. immunized mice displayed an average recombinant VV titer in the cervicovaginal mucosa of 1.3 × 105 PFU, a level that was 100-fold higher than that in the HPV-MM2–immunized mice and non-significantly lower than in the sham-immunized mice.
Figure 11. HPV Ivag, but not Ad5 i.m., prime/boost immunization reduces viral titers in the cervicovaginal mucosa after vaginal challenge with recombinant M282–90–VV.
Depo-Provera–treated mice were immunized with 5 × 107 IU HPV16MM2 Ivag or with 5 × 107 PFU Ad5-MM2 i.m., and 1 month later mice were immunized with 5 × 107 IU HPV45MM2 or Ad5-MM2 i.m., respectively. Two months after the last immunization, mice were challenged Ivag with 1 × 107 PFU of recombinant M282–90–VV. Three days after challenge, vaginal tissue was collected, and recombinant VV titers were determined by plaque assays. Results are expressed as PFU per vagina for individual mice (symbols) and geometric mean (horizontal bars). Data are representative of 3 experiments (*P < 0.05, **P < 0.01, Kruskal-Wallis/Dunn’s test).
In separate experiments, we evaluated whether recognition of the M282–90 epitope by CD8+ T cells was required for protection. Sham-treated, HPV-Luc–, or HPV-MM2–immunized mice were challenged Ivag with either a recombinant VV expressing the irrelevant NP147–155 epitope of influenza virus A/PR/8/34 (rVV-NP147–155) or rVV-M282–90. Average viral titers in the cervicovaginal mucosa were similar in all groups challenged with the control rVV-NP147–155 (Supplemental Figure 7A). Consistent with the results shown in Figure 11, the HPV-MM2–immunized group challenged with rVV-M282–90 displayed significantly lower average viral titers in the vagina compared with control groups (Supplemental Figure 7B). These data indicate that intraepithelial CD8+ T cells can participate in the control of viral replication in the cervicovaginal mucosa.
Discussion
This study provides evidence that the female cervicovaginal mucosa can be an effective site for induction and boosting of effector memory CD8+ T cell responses using a non-replicating viral vector. Previous studies involving live viruses or attenuated replicating vectors left open the possibility that the presence of these cells in the cervicovaginal mucosa might have resulted from their immune induction at remote sites. Trafficking of the virus/vector and expression of the antigen in other tissues could lead to subsequent recruitment of immunocytes to the cervicovaginal mucosa. We have focused our studies on the induction of effector T cell responses, rather than antibodies, because the efficient induction of cervicovaginal mucosa T cells by a non-replicating vaccine had not previously been demonstrated. In contrast, it is now recognized, thanks to the remarkable efficacy of the commercial HPV prophylactic vaccines, that systemic immunization with a protein antigen, in this case a virus-like particle, can induce protective levels of antibodies in the female cervicovaginal mucosa (48–50).
Antigen expression by the HPV PsV, which is transient because the infected keratinocytes are sloughed during the normal squamous differentiation process, is limited to “wounded” cervicovaginal keratinocytes because infection occurs in conjunction with epithelial disruption, which allows binding of the virus particle to the basement membrane before they infect the keratinocytes (34, 51). Therefore, the genetically delivered antigen is expressed in the proinflammatory and potentially immunogenic setting of disrupted epithelium rather than in an undisturbed tissue that is more likely to be tolerogenic (3). Other characteristics of HPV PsV, such as the ability of the capsid to trigger an innate immune response, may also contribute to making them exceptionally potent inducers of genital CD8+ T cell responses (52, 53).
This is the first study to our knowledge to demonstrate the preferential induction of large numbers of intraepithelial CD103+CD8+ T cells (IELs) in the cervicovaginal mucosa after Ivag immunization with a non-replicating vector. Unfortunately, because of technical limitations inherent in the available KdM282-tetramers, we were unable to monitor in situ antigen-specific CD8+ T cells by M2-tetramer staining on tissue sections of the cervicovaginal mucosa. However, the paucity of preexisting CD8+ T cells in the cervicovaginal epithelium of young mice that have not been bred, and the fact that the exceptional increase in genital CD8+ T cells was attributable entirely to the expansion of KdM282-tetramer–positive CD8+ T cells as shown by flow cytometry, strongly imply that the intraepithelial CD8+ T cells induced after HPV PsV Ivag immunization are specific for the immunodominant epitope M282–90. The low number of cervicovaginal T cells prior to vaccination led us to focus on absolute numbers of T cells induced rather than on their relative percentage in the tissue, since the latter calculation can produce an overestimate of the response in tissues with low preexisting numbers of T cells.
Based on the large number of CD3+CD8+ T cells detected histologically in most tissue sections from vaccinated mice, it is our impression that the flow cytometry analysis substantially underestimates the true number of T cells induced in the cervicovaginal mucosa, which might result from the incomplete liberation of T cells from the tissue by our extraction procedures. In future studies, it will be important to determine whether higher numbers of preexisting IELs in the cervicovaginal epithelium inhibit induction of antigen-specific CD8+ T cells after Ivag HPV PsV vaccination and whether the pool of memory IEL CD8+ T cells can expand further, as previously reported for the pool of memory CD8+ T cells in PBMCs (54).
Some vaccination strategies have sought to increase the strength and durability of effector memory CD8+ T cell responses by inducing persistent antigen expression with live virus vectors (12). Our results demonstrate that even transient antigen expression can induce strong, durable responses. It is noteworthy that we did not observe an acute contraction phase in genital CD8+ T cells after Ivag vaccination. Our findings support accumulating evidence that intraepithelial T cells, especially effector memory cells, may in general be longer lived than systemic effector T cells, as befits their putative role as guardians of epithelial surfaces. It is unclear whether the marked acquisition of an effector memory phenotype observed in the genital CD8+ T cells over time is due to the evolution of the phenotype of individual cells or gradual replacement of effector with effector memory cells, for instance, by preferential survival or homeostatic proliferation.
The ability to preferentially induce large numbers of antigen-specific IELs by vaccination should facilitate future studies of this unique class of lymphocytes. Our characterization indicates that primary CD8+ T cells depend on CD4+ T cell help, which is consistent with their priming occurring in lymph nodes. However, the role of CD4+ T cells during at the booster immunization step remains to be assessed. The recruitment of circulating T cells to the genital mucosa has been previously described and requires CD4+ T cells as well as expression of CXCR3 by circulating memory CD8+ T cells (55). Our FTY720 and BrdU experiments strongly implicate local mucosal proliferation during the secondary response to keratinocyte-expressed antigen, but it does not address the role of CD4+ T cells or whether inflammation-driven recruitment from the circulation was required. While this is, to our knowledge, the first evidence of this phenomenon in a mucosal tissue after vaccination, several recent studies have presented evidence that peripheral proliferation of primed CD8+ T cells in response to antigen can occur in other settings, for instance, in tumors or neuronal tissues (26, 56). In future studies, it will be important to determine whether the “wounded” keratinocytes, which can express costimulatory and MHC I molecules, can directly present antigen for in situ proliferation of CD8+ T cells or whether cross-presentation by professional APCs or membrane transfer from keratinocytes to DCs, referred to as cross-dressing, are involved in the recall of memory T cells in the cervicovaginal mucosa (57). In addition, the trafficking patterns of IELs within the epithelium and between the epithelium and other tissues are poorly understood, and this system might allow for their study.
There are numerous reports of the induction of CD8+ T cell responses in the cervicovaginal mucosa after systemic vaccination with non-replicating vectors (7, 11, 13, 46), and we confirmed these observations using our Ad5-MM2 vector in an intramuscular prime/boost regimen. However, this regimen was qualitatively and quantitatively inferior to the Ivag prime/boost immunization regimen. In spite of the relatively high numbers of cervicovaginal KdM282-tetramer+CD8+ T cells measured by flow cytometry, there was no increase in IEL number after systemic prime/boost immunization, which raises the possibility that the T cells extracted from the cervicovaginal tissues after the systemic immunization procedures may have largely been retained within the mucosal vasculature or were loosely associated with the submucosa. The unique ability of HPV PsV Ivag vaccination, compared with Ad5 i.m. vaccination, to confer enhanced protection against a local viral challenge is associated with the unique induction of CD8 IELs and their upregulation of CD103. Intraepithelial memory CD8+ T cells would be able to respond to infection more promptly than their circulating counterparts, but one could also speculate that the expression of CD103 at the surface of cervicovaginal IEL CD8+ T cells would contribute to enhancing protection, as this integrin has been shown to participate in the cytotoxic activity of human tumor-infiltrating CD8+ T cells (58). Also, the fact that CD103 expression was restricted to KdM282-tetramer+CD8+ T cells from the cervicovaginal mucosa and expressed up to 6 months after boost (our unpublished observations) suggests a role for the cervicovaginal microenvironment in CD103 induction. This conjecture is consistent with recent reports indicating that persistent tissue-resident memory T cells upregulate CD103 in peripheral tissues but not in other lymphoid organs (27, 59). Furthermore, the limited CD103 expression in the cervicovaginal CD8+ T cells induced after i.m. immunization may explain the absence of intraepithelial CD8+ T cells in i.m. immunized mice and suggests that de novo antigen expression in wounded keratinocytes is driving the upregulation of CD103.
The phenotypic and functional characterization of the genital CD8+ T cells induced after genital HPV PsV vaccination is consistent with their being functional effector memory cells with potential antiviral activity. First, most cells were polyfunctional, as they simultaneously secreted IFN-γ and TNF-α. Second, they exhibited in vivo cytotoxic activity against autologous cells pulsed with the immunodominant M282–90 peptide. Third, they were associated with a 1,000-fold reduction in the mean cervicovaginal mucosa viral load of recombinant VV expressing the M282–90 peptide after vaginal inoculation. It is noteworthy that this viral challenge model is rather stringent, since protection is entirely mediated by CD8+ T cells.
The ability to preferentially induce long-lived antigen-specific intraepithelial CD8+ T cells may be an attractive feature for a vaccine designed to prevent a viral infection that is initiated in the cervicovaginal mucosa such as HIV or HSV. Having sentinel T cells at the initial site of infection has been shown to lead to a more rapid response in the skin during HSV-1 infection and thereby control infection before it can spread systemically (57). Indeed, recruitment of systemic T cells may take too long to effectively control the initial phase of infection, which is an important determinant of clinical outcome. Having local T cells can increase the local ratio of virus-specific CD8+ T cells to virus-infected cells and provide enhanced protection (29, 60). For application to HIV vaccines, it is noteworthy that our Ivag vaccination protocol did not increase the number of cervicovaginal mucosa CD4+ T helper cells, so it would not be expected to increase the pool of infection targets, which could thereby potentiate infection.
Transudated systemic antibodies and effector IELs ideally could act synergistically to prevent or control infection of the genital mucosa, and vaccines inducing both major limbs of the adaptive immune response should be considered. If the absence of genital IELs after systemic immunization of mice is predictive for humans, then the role of IELs should be critically evaluated in future HIV or HSV clinical trials of candidate vaccines (61, 62). Using HPV-encapsidated DNA or other viral vectors to locally induce effector CD8+ IELs should be a high-priority approach to evaluate difficult vaccine targets, such as HSV or HIV.
Vaccines that induce cervicovaginal mucosa IELs might also be considered for therapeutic vaccines, particularly against HSV herpetic lesions and HPV-induced intraepithelial neoplasia. Abatement of recurrent genital herpes lesions was recently correlated with the appearance of CD8+ T cells located between the nerve endings and the adjacent epithelial cells at the site of previous herpetic lesions (63). Generation of HSV-specific effector memory T cells at these sites by vaccination might have a similar effect. A marked recruitment of CD8+ T cells into the epithelium of HPV-induced cervical intraepithelial neoplasia was observed in lesions that subsequently regressed (30). In contrast, a T cell infiltrate in the submucosa, along with its exclusion from the overlying dysplastic epithelium, was observed in lesions that persisted. Induction of HPV-specific IELs by vaccination might overcome this apparent barrier to clearance.
Finally, the feasibility of translating our vaccination strategy to women should be considered. We have recently shown that our HPV PsV–based vaccination strategy is not restricted to mice, with studies in non-human primates demonstrating efficient gene delivery and immunogenicity against SIV antigens in Depo-Provera–treated monkeys (35). The mice in this study were similarly progesterone treated to ensure that they had uniformly thin cervicovaginal epithelium and so relatively consistent vector infection. However, this treatment might be more critical in mouse studies than in human applications for two reasons. First, the thickness of the cervicovaginal epithelium appears to be more hormonally dependent in mice, with estrogen-dominated mice exhibiting highly keratinized squamous epithelium. The thickness of the squamous epithelium varies less across the menstrual cycle in women. Second, the simple columnar epithelium of the endocervix begins rather high up the endocervical channel in mice and is not readily exposed to N-9 and PsV unless the cervix is cannulated (34). In contrast, the endocervical epithelium is exposed in women, particularly in young women. It might be predicted that the simple columnar epithelium of the endocervix would be exceptionally susceptible to N-9 disruption and PsV infection, and this susceptibility to infection would not be expected to vary substantially across the menstrual cycle. It will be important to further determine in non-human primate models whether IELs can similarly be induced in the simple columnar epithelium of the endocervix throughout the menstrual cycle, particularly since the endocervix and/or the transformation zone between endo- and ectocervix may be especially susceptible to viral transmission.
The requirement for epithelial permeabilization or disruption in conjunction with vaccination might also raise safety concerns. For this reason, we purposely chose to use a disrupting agent that is an over-the-counter product containing N-9 (Conceptrol) that is approved for unregulated Ivag application in women. While N-9–containing spermicides used repeatedly may increase susceptibility to some sexually transmitted infections, these agents could be acceptable for a limited number of applications as part of a vaccination protocol. Although the use of N-9–containing products was associated with an increased risk of HIV transmission (64), the epithelial disruption they induce is transient, and refraining from unprotected sexual activity for several days after their use as part of a vaccination regimen would likely mitigate this risk. Finally, the experience from clinical trials of topical microbicides against STDs provides a rational basis for developing a relatively simple gel-based vaccine for topical application.
Methods
Mice.
Six- to 8-week-old female BALB/cAnNCr and CB6F1/Cr mice were purchased from the Animal Production Program (NCI-Frederick) and housed and handled under specific pathogen–free conditions in the animal care facilities at the National Cancer Institute.
Viral vectors and viruses.
HPV16 and HPV45 pseudovirions (PsV) containing a plasmid that encodes a fusion protein of the M and M2 protein of RSV-2 (pCMMf, NCBI AAB86677 and AAB86660) or firefly luciferase (pCLucf, NCBI AY738225) were generated as described previously (37, 65, 66).
Briefly, 293TT cells were co-transfected with a plasmid encoding the M/M2 fusion protein or luciferase and a plasmid too large to self-package encoding the L1 and L2 protein of HPV type 16 (L1 and L2, EMBL 16L1h L2 AJ313179 AJ313180) or 45 (L1 and L2, NCBI DQ080002) (67). After maturation, HPV PsV were purified over an OptiPrep gradient; fractions containing the encapsidated plasmid were pooled; and infectious titer was determined on the 293TT cells by measuring a coexpressed green fluorescent protein gene by flow cytometry and expressed as IU/ml.
A non-replicating adenoviral type 5 vector (Ad5) encoding the MM2 fusion protein was generated and produced by GenVec. The number of infectious particles (PFU) of Ad5 was measured by plaque assay using a helper cell line, and MM2 protein expression was measured by Western blot analysis in 293T cells infected with Ad5-MM2 (37).
Respiratory syncytial virus M282–90 and influenza NP147–155 recombinant vaccinia viruses were a gift from Brian Murphy (NIAID) and were generated, produced, and characterized essentially as previously described (47, 68). The titer of the recombinant VV was analyzed by plaque assay on BSC-1 cells and expressed as PFU/ml.
Immunization procedures and recombinant vaccinia challenge.
For all immunization procedures, mice received 3 mg of medroxy-progesterone acetate (Depo-Provera, Pfizer) subcutaneously in a volume of 100 μl PBS 5 days prior to vaccination. Mice were immunized with HPV PsV Ivag as previously described (34, 37). Briefly, 5 hours before immunization, the vaginal epithelium was disrupted by instillation of a gel containing 4% N-9 (Conceptrol, Ortho Options) in a 50-μl volume. Mice were immunized with 20 μl of HPV PsV diluted in 2% carboxymethyl cellulose gel (medium viscosity, 400–800 cP at 25°C; Sigma-Aldrich).
For intranasal immunization, mice were pretreated in each nostril with 10 μl of 0.2% N-9 (Spectrum) diluted in PBS and 5 hours later received a volume of 5 μl HPV PsV (5 × 107 IU) in each nostril. For i.m. immunization, the Ad5 vector (1 × 107 or 5 × 107 PFU) was diluted in 50 μl PBS and injected in the quadriceps muscle.
For prime/boost mucosal immunization, mice were primed with 5 × 107 IU of HPV16 PsV and boosted 4 weeks later with 5 × 107 IU of HPV45 PsV in order to overcome type-specific antibody-mediated neutralization. For the single immunization regimen, mice were immunized with 1 × 108 IU of HPV16 PsV.
For Ivag recombinant vaccinia challenge, mice were given Ivag 1 × 107 PFU of recombinant VV diluted in 20 μl of 2% carboxymethylcellulose, and 3 days after challenge the viral load was assessed in a vaginal homogenate by plaque assay and expressed as PFU per organ.
Preparation of cell suspensions.
Mice were euthanized and organs were removed by dissection. Vaginal and lung cell suspensions were obtained by enzymatic dispersion in RPMI containing 2% FBS, collagenase (0.5 mg/ml; Roche Diagnostics), and DNase I (0.1 mg/ml; Roche Diagnostics) for 1 hour at 37°C while shaking. Vaginal cells were passed through a 70-μM cell strainer (BD). Lymph node and spleen cell suspensions were obtained after 20 minutes enzymatic dispersion at 37°C and were mechanically dispersed by teasing the organs on a 70-μm cell strainer (BD). Vaginal, spleen, and lymph node cell suspensions were washed in RPMI/FBS 2% and were freed from erythrocytes by treatment with ammonium chloride solution (ACK, Lonza).
Antibodies and tetramers.
The following anti-mouse antibodies were used for cell surface staining for flow cytometry analysis: anti-NKp46 (29A1.4), anti-IA/IE (M5/114), anti-CD3 (clone 145-2C11), anti-PDCA1 (clone 927), anti-CD8 (clone 53-6.7), anti-CD103 (2E7), and anti-CD4 (RM4-5 and RM4-4) from BioLegend, anti-CD127 (SB/199, eBioscience), and anti-CD11c (HL3, BD Biosciences). APC-conjugated M282–90/H2-Kd-tetramer (KdM282-tetramer) was obtained from the NIH Tetramer Core Facility (Emory University).
Cell surface staining.
All staining was performed in 96-well plates in a final volume of 100 μl PBS/2% FBS (FACS buffer) for 30 minutes at 4°C. To avoid nonspecific antibody binding through surface Fc receptor, all cells were preincubated with CD16/32 purified antibody (2.4G2, BioXcell). Samples were acquired directly from 96-well plates on a FACSCanto II flow cytometer with the HTS module (BD Biosciences). Data were analyzed with FlowJo software (TreeStar).
In vitro peptide stimulation and intracellular cytokine staining.
Spleen, lymph node, and vaginal cells were incubated in RPMI/FBS 10%, l-glutamine, sodium pyruvate, and β-mercaptoethanol supplemented with 1 μg/ml of Brefeldin A (GolgiPlug, BD Bioscience) for 5 hours at 37°C/5% CO2 in the presence of M282–90 peptide (GenScript) at 5 μg/ml, in medium only or with PMA (5 ng/ml; Sigma-Aldrich) and ionomycin (500 ng/ml; Sigma-Aldrich) as a positive control. Cells were washed and surface stained with anti-CD3, anti-CD4, and anti-CD8 antibodies, then fixed and permeabilized (Cytofix/Cytoperm, BD Biosciences) before staining for intracellular cytokine content using anti–TNF-α (MP6-XT22, BD Biosciences), anti–IL-2 (JES6-5H4, BioLegend), and anti–IFN-γ (XMG1.2, BD Biosciences) antibodies. Stained cells were analyzed by flow cytometry.
Immunofluorescence confocal microscopy analysis.
Cervicovaginal tracts were dissected, washed in PBS, and snap frozen in tissue freezing medium (Tissue-Tek OCT, Sakura). Six-micrometer tissue cryosections were transferred onto glass slides and fixed for 10 minutes in cold 100% ethanol. Fixed tissue sections were kept at 4°C for no longer than 2 weeks. Tissues sections were blocked with CD16/CD32 antibody (2.4G2, BioXcell) and normal donkey serum, then stained with purified rabbit laminin 332 antibody (Abcam), followed by a second-step incubation with donkey anti-rabbit IgG–Alexa Fluor 594 (51), anti-CD8–Alexa Fluor 488 (BioLegend), and anti-CD3–Alexa Fluor 647 (BioLegend) diluted in 0.1% Brij58. Alternatively, sections were stained with CD103 or Armenian hamster IgG isotype control antibodies (BioLegend), followed by a second-step incubation with CD8–Alexa Fluor 488 and anti-Armenian hamster IgG–Alexa Fluor 594 (BioLegend). Confocal images were acquired at the Confocal Microscopy Core Facility, Center for Cancer Research, National Cancer Institute, NIH, with Zeiss ZEN software on a Zeiss LSM 510 Confocal system with a Zeiss Observer Z1 inverted microscope and 50-mW argon UV laser tuned to 364 nm, a 25-mW argon visible laser tuned to 488 nm, a 1-mW HeNe laser tuned to 543 nm, and a 5-mW HeNe laser tuned to 633 nm. A ×40 Plan-Neofluar 1.3 NA oil immersion objective was used. Emission signals after sequential excitation of each fluorochrome were collected with a BP 385–470 filter, BP 505–530 filter, BP 560–615 filter, or LP 650 filter using individual photomultipliers. Images were analyzed using LSM image browser (Zeiss).
In vivo CD4+ T cell depletion.
Mice were depleted of CD4+ T cells by i.p. injection of 100 μg anti-CD4 mAb (GK1.5, BioXcell) on days –3, –1, 2, 4, and 6 with respect to day 0 of immunization. Control mice were injected with a rat IgG2b isotype control mAb (LTF-2, BioXcell).
In vivo FTY720 treatment.
Mice were treated with FTY720 (Cayman Chemical) in drinking water (4 μg/ml) from the day of immunization until the end of the experiment. In some experiments, FTY720 was administered during a single immunization regimen as described previously (42). For the prime/boost immunization regimen, FTY720 was administered at the time of boost only.
In vivo BrdU incorporation assay.
Mice were given BrdU (Sigma-Aldrich) in drinking water at a concentration of 0.8 mg/ml. Drinking water was changed daily to overcome BrdU degradation. Intracellular staining for BrdU was performed using a BrdU Flow Kit (BD Bioscience) after surface staining for KdM282-tetramer+CD8+ T cells.
In vivo CTL assay.
The in vivo CTL assay was performed as previously described (69, 70). Briefly, spleen cells from a naive BALB/c mouse were split into two fractions. The first fraction was labeled with 4 μM CFSE (CFSEhi) and pulsed with 1 μM RSV M282–90 peptide (GenScript), and the other fraction was labeled with 0.4 μM CFSE (CFSElo) and remained unpulsed. Equal numbers of cells from CFSEhi and CFSElo fractions were pooled and are referred to as target cells. A total of 1.5 × 107 or 2 × 106 target cells were injected intravenously or directly in the vaginal mucosa, respectively. One day after transfer of the target cells, specific CTL activity was measured by flow cytometry in cell suspensions from the spleen, ILN, and cervicovaginal mucosa. Specific lysis was calculated as follows: (1 – [ratio of CFSElo/CFSEhi cells in control mice divided by ratio of CFSElo/ CFSEhi cells in immunized mice] × 100).
Statistics.
The non-parametric Mann-Whitney U test was used for comparisons in experiment of 2 independent groups. For experiments involving more than 2 groups, ANOVA by Kruskal-Wallis followed by Dunn’s post-test was performed for selected pairwise comparisons. A P value less than or equal to 0.05 was considered significant.
Study approval.
All animal experiments and procedures were carried out in accordance with National Cancer Institute guidelines and under NCI Animal Care and Use Committee–approved protocols.
Supplementary Material
Acknowledgments
We acknowledge Amy Stout and Dale Long for outstanding support at the NIH Tetramer Core Facility (Emory University, Atlanta, Georgia, USA). We gratefully acknowledge Brian Murphy (NIAID, Bethesda, Maryland, USA) for providing the M2 recombinant VV. This work was supported by the Intramural Research Program of the NIH, National Cancer Institute, CCR.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2012;122(12):4606–4620. doi:10.1172/JCI63287.
Rhonda C. Kines’s present address is: Aura Biosciences Inc., Cambridge, Massachusetts, USA.
References
- 1.Zinkernagel RM, Doherty PC. Restriction of in vitro T cell-mediated cytotoxicity in lymphocytic choriomeningitis within a syngeneic or semiallogeneic system. Nature. 1974;248(450):701–702. doi: 10.1038/248701a0. [DOI] [PubMed] [Google Scholar]
- 2.Bjorkman PJ, Saper MA, Samraoui B, Bennett WS, Strominger JL, Wiley DC. The foreign antigen binding site and T cell recognition regions of class I histocompatibility antigens. Nature. 1987;329(6139):512–518. doi: 10.1038/329512a0. [DOI] [PubMed] [Google Scholar]
- 3.Black CA, et al. Vaginal mucosa serves as an inductive site for tolerance. J Immunol. 2000;165(9):5077–5083. doi: 10.4049/jimmunol.165.9.5077. [DOI] [PubMed] [Google Scholar]
- 4.Dudek T, Knipe DM. Replication-defective viruses as vaccines and vaccine vectors. Virology. 2006;344(1):230–239. doi: 10.1016/j.virol.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 5.Rollier CS, Reyes-Sandoval A, Cottingham MG, Ewer K, Hill AV. Viral vectors as vaccine platforms: deployment in sight. Curr Opin Immunol. 2011;23(3):377–382. doi: 10.1016/j.coi.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Li Z, Zhang M, Zhou C, Zhao X, Iijima N, Frankel FR. Novel vaccination protocol with two live mucosal vectors elicits strong cell-mediated immunity in the vagina and protects against vaginal virus challenge. J Immunol. 2008;180(4):2504–2513. doi: 10.4049/jimmunol.180.4.2504. [DOI] [PubMed] [Google Scholar]
- 7.Suvas PK, Dech HM, Sambira F, Zeng J, Onami TM. Systemic and mucosal infection program protective memory CD8 T cells in the vaginal mucosa. J Immunol. 2007;179(12):8122–8127. doi: 10.4049/jimmunol.179.12.8122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu L, Fuhlbrigge RC, Karibian K, Tian T, Kupper TS. Dynamic programming of CD8+ T cell trafficking after live viral immunization. Immunity. 2006;25(3):511–520. doi: 10.1016/j.immuni.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 9.Masopust D, Vezys V, Marzo AL, Lefrancois L. Preferential localization of effector memory cells in nonlymphoid tissue. Science. 2001;291(5512):2413–2417. doi: 10.1126/science.1058867. [DOI] [PubMed] [Google Scholar]
- 10.Masopust D, Vezys V, Wherry EJ, Barber DL, Ahmed R. Cutting edge: gut microenvironment promotes differentiation of a unique memory CD8 T cell population. J Immunol. 2006;176(4):2079–2083. doi: 10.4049/jimmunol.176.4.2079. [DOI] [PubMed] [Google Scholar]
- 11.Decrausaz L, et al. Parenteral is more efficient than mucosal immunization to induce regression of human papillomavirus-associated genital tumors. Int J Cancer. 2011;129(3):762–772. doi: 10.1002/ijc.25973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hansen SG, et al. Effector memory T cell responses are associated with protection of rhesus monkeys from mucosal simian immunodeficiency virus challenge. Nat Med. 2009;15(3):293–299. doi: 10.1038/ng0397-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaufman DR, et al. Trafficking of antigen-specific CD8+ T lymphocytes to mucosal surfaces following intramuscular vaccination. J Immunol. 2008;181(6):4188–4198. doi: 10.4049/jimmunol.181.6.4188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sigmundsdottir H, Butcher EC. Environmental cues, dendritic cells and the programming of tissue-selective lymphocyte trafficking. Nat Immunol. 2008;9(9):981–987. doi: 10.1038/ni.f.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iwata M, Hirakiyama A, Eshima Y, Kagechika H, Kato C, Song SY. Retinoic acid imprints gut-homing specificity on T cells. Immunity. 2004;21(4):527–538. doi: 10.1016/j.immuni.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 16.Koelle DM, et al. Expression of cutaneous lymphocyte-associated antigen by CD8(+) T cells specific for a skin-tropic virus. J Clin Invest. 2002;110(4):537–548. doi: 10.1172/JCI15537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johansson-Lindbom B, Svensson M, Wurbel MA, Malissen B, Marquez G, Agace W. Selective generation of gut tropic T cells in gut-associated lymphoid tissue (GALT): requirement for GALT dendritic cells and adjuvant. J Exp Med. 2003;198(6):963–969. doi: 10.1084/jem.20031244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mora JR, Cheng G, Picarella D, Briskin M, Buchanan N, von Andrian UH. Reciprocal and dynamic control of CD8 T cell homing by dendritic cells from skin- and gut-associated lymphoid tissues. J Exp Med. 2005;201(2):303–316. doi: 10.1084/jem.20041645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stagg AJ, Kamm MA, Knight SC. Intestinal dendritic cells increase T cell expression of alpha4beta7 integrin. Eur J Immunol. 2002;32(5):1445–1454. doi: 10.1002/1521-4141(200205)32:5<1445::AID-IMMU1445>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 20.Olive AJ, Gondek DC, Starnbach MN. CXCR3 and CCR5 are both required for T cell-mediated protection against C. trachomatis infection in the murine genital mucosa. Mucosal Immunol. 2011;4(2):208–216. doi: 10.1038/mi.2010.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perry LL, Feilzer K, Portis JL, Caldwell HD. Distinct homing pathways direct T lymphocytes to the genital and intestinal mucosae in Chlamydia-infected mice. J Immunol. 1998;160(6):2905–2914. [PubMed] [Google Scholar]
- 22.Belyakov IM, et al. Mucosal immunization with HIV-1 peptide vaccine induces mucosal and systemic cytotoxic T lymphocytes and protective immunity in mice against intrarectal recombinant HIV-vaccinia challenge. Proc Natl Acad Sci U S A. 1998;95(4):1709–1714. doi: 10.1073/pnas.95.4.1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Calzascia T, et al. Homing phenotypes of tumor-specific CD8 T cells are predetermined at the tumor site by crosspresenting APCs. Immunity. 2005;22(2):175–184. doi: 10.1016/j.immuni.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 24.Gallichan WS, Rosenthal KL. Long-lived cytotoxic T lymphocyte memory in mucosal tissues after mucosal but not systemic immunization. J Exp Med. 1996;184(5):1879–1890. doi: 10.1084/jem.184.5.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luci C, Hervouet C, Rousseau D, Holmgren J, Czerkinsky C, Anjuere F. Dendritic cell-mediated induction of mucosal cytotoxic responses following intravaginal immunization with the nontoxic B subunit of cholera toxin. J Immunol. 2006;176(5):2749–2757. doi: 10.4049/jimmunol.176.5.2749. [DOI] [PubMed] [Google Scholar]
- 26.Wakim LM, Waithman J, van Rooijen N, Heath WR, Carbone FR. Dendritic cell-induced memory T cell activation in nonlymphoid tissues. Science. 2008;319(5860):198–202. doi: 10.1126/science.1151869. [DOI] [PubMed] [Google Scholar]
- 27.Piet B, et al. CD8 T cells with an intraepithelial phenotype upregulate cytotoxic function upon influenza infection in human lung. J Clin Invest. 2011;121(6):2254–2263. doi: 10.1172/JCI44675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang VA, Rosenthal KL. Intravaginal infection with herpes simplex virus type-2 (HSV-2) generates a functional effector memory T cell population that persists in the murine genital tract. J Reprod Immunol. 2010;87(1–2):39–44. doi: 10.1016/j.jri.2010.06.155. [DOI] [PubMed] [Google Scholar]
- 29.Schiffer JT, et al. Mucosal host immune response predicts the severity and duration of herpes simplex virus-2 genital tract shedding episodes. Proc Natl Acad Sci U S A. 2010;107(44):18973–18978. doi: 10.1073/pnas.1006614107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trimble CL, et al. Human papillomavirus 16-associated cervical intraepithelial neoplasia in humans excludes CD8 T cells from dysplastic epithelium. J Immunol. 2010;185(11):7107–7114. doi: 10.4049/jimmunol.1002756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gallichan WS, Johnson DC, Graham FL, Rosenthal KL. Mucosal immunity and protection after intranasal immunization with recombinant adenovirus expressing herpes simplex virus glycoprotein B. J Infect Dis. 1993;168(3):622–629. doi: 10.1093/infdis/168.3.622. [DOI] [PubMed] [Google Scholar]
- 32.Zhu Q, Thomson CW, Rosenthal KL, McDermott MR, Collins SM, Gauldie J. Immunization with adenovirus at the large intestinal mucosa as an effective vaccination strategy against sexually transmitted viral infection. Mucosal Immunol. 2008;1(1):78–88. doi: 10.1038/mi.2007.3. [DOI] [PubMed] [Google Scholar]
- 33.Buck CB, Pastrana DV, Lowy DR, Schiller JT. Efficient intracellular assembly of papillomaviral vectors. J Virol. 2004;78(2):751–757. doi: 10.1128/JVI.78.2.751-757.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roberts JN, et al. Genital transmission of HPV in a mouse model is potentiated by nonoxynol-9 and inhibited by carrageenan. Nat Med. 2007;13(7):857–861. doi: 10.1038/nm1598. [DOI] [PubMed] [Google Scholar]
- 35.Gordon SN, et al. Targeting the vaginal mucosa with human papillomavirus pseudovirion vaccines delivering simian immunodeficiency virus DNA. J Immunol. 2012;188(2):714–723. doi: 10.4049/jimmunol.1101404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roberts JN, Kines RC, Katki HA, Lowy DR, Schiller JT. Effect of Pap smear collection and carrageenan on cervicovaginal human papillomavirus-16 infection in a rhesus macaque model. J Natl Cancer Inst. 2011;103(9):737–743. doi: 10.1093/jnci/djr061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Graham BS, et al. Mucosal delivery of human papillomavirus pseudovirus-encapsidated plasmids improves the potency of DNA vaccination. Mucosal Immunol. 2010;3(5):475–486. doi: 10.1038/mi.2010.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bachmann MF, Wolint P, Schwarz K, Jager P, Oxenius A. Functional properties and lineage relationship of CD8+ T cell subsets identified by expression of IL-7 receptor alpha and CD62L. J Immunol. 2005;175(7):4686–4696. doi: 10.4049/jimmunol.175.7.4686. [DOI] [PubMed] [Google Scholar]
- 39.Kaech SM, Tan JT, Wherry EJ, Konieczny BT, Surh CD, Ahmed R. Selective expression of the interleukin 7 receptor identifies effector CD8 T cells that give rise to long-lived memory cells. Nat Immunol. 2003;4(12):1191–1198. doi: 10.1038/ni1009. [DOI] [PubMed] [Google Scholar]
- 40.Sallusto F, Lenig D, Forster R, Lipp M, Lanzavecchia A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature. 1999;401(6754):708–712. doi: 10.1038/44385. [DOI] [PubMed] [Google Scholar]
- 41.Seder RA, Darrah PA, Roederer M. T-cell quality in memory and protection: implications for vaccine design. Nat Rev Immunol. 2008;8(4):247–258. doi: 10.1038/nri2274. [DOI] [PubMed] [Google Scholar]
- 42.Masopust D, et al. Dynamic T cell migration program provides resident memory within intestinal epithelium. J Exp Med. 2010;207(3):553–564. doi: 10.1084/jem.20090858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matloubian M, et al. Lymphocyte egress from thymus and peripheral lymphoid organs is dependent on S1P receptor 1. Nature. 2004;427(6972):355–360. doi: 10.1038/nature02284. [DOI] [PubMed] [Google Scholar]
- 44.Pinschewer DD, Ochsenbein AF, Odermatt B, Brinkmann V, Hengartner H, Zinkernagel RM. FTY720 immunosuppression impairs effector T cell peripheral homing without affecting induction, expansion, and memory. J Immunol. 2000;164(11):5761–5770. doi: 10.4049/jimmunol.164.11.5761. [DOI] [PubMed] [Google Scholar]
- 45.Vremec D, Pooley J, Hochrein H, Wu L, Shortman K. CD4 and CD8 expression by dendritic cell subtypes in mouse thymus and spleen. J Immunol. 2000;164(6):2978–2986. doi: 10.4049/jimmunol.164.6.2978. [DOI] [PubMed] [Google Scholar]
- 46.Haut LH, et al. Robust genital gag-specific CD8+ T-cell responses in mice upon intramuscular immunization with simian adenoviral vectors expressing HIV-1-gag. Eur J Immunol. 2010;40(12):3426–3438. doi: 10.1002/eji.201040440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kulkarni AB, et al. Cytotoxic T cells specific for a single peptide on the M2 protein of respiratory syncytial virus are the sole mediators of resistance induced by immunization with M2 encoded by a recombinant vaccinia virus. J Virol. 1995;69(2):1261–1264. doi: 10.1128/jvi.69.2.1261-1264.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Day PM, et al. In vivo mechanisms of vaccine-induced protection against HPV infection. Cell Host Microbe. 2010;8(3):260–270. doi: 10.1016/j.chom.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lehtinen M, et al. Overall efficacy of HPV-16/18 AS04-adjuvanted vaccine against grade 3 or greater cervical intraepithelial neoplasia: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 2012;13(1):89–99. doi: 10.1016/S1470-2045(11)70286-8. [DOI] [PubMed] [Google Scholar]
- 50.Munoz N, et al. Impact of human papillomavirus (HPV)-6/11/16/18 vaccine on all HPV-associated genital diseases in young women. J Natl Cancer Inst. 2010;102(5):325–339. doi: 10.1093/jnci/djp534. [DOI] [PubMed] [Google Scholar]
- 51.Kines RC, Thompson CD, Lowy DR, Schiller JT, Day PM. The initial steps leading to papillomavirus infection occur on the basement membrane prior to cell surface binding. Proc Natl Acad Sci U S A. 2009;106(48):20458–20463. doi: 10.1073/pnas.0908502106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lenz P, et al. Papillomavirus-like particles induce acute activation of dendritic cells. J Immunol. 2001;166(9):5346–5355. doi: 10.4049/jimmunol.166.9.5346. [DOI] [PubMed] [Google Scholar]
- 53.Yang R, et al. B lymphocyte activation by human papillomavirus-like particles directly induces Ig class switch recombination via TLR4-MyD88. J Immunol. 2005;174(12):7912–7919. doi: 10.4049/jimmunol.174.12.7912. [DOI] [PubMed] [Google Scholar]
- 54.Vezys V, et al. Memory CD8 T-cell compartment grows in size with immunological experience. Nature. 2009;457(7226):196–199. doi: 10.1038/nature07486. [DOI] [PubMed] [Google Scholar]
- 55.Nakanishi Y, Lu B, Gerard C, Iwasaki A. CD8(+) T lymphocyte mobilization to virus-infected tissue requires CD4(+) T-cell help. Nature. 2009;462(7272):510–513. doi: 10.1038/nature08511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thompson ED, Enriquez HL, Fu YX, Engelhard VH. Tumor masses support naive T cell infiltration, activation, and differentiation into effectors. J Exp Med. 2010;207(8):1791–1804. doi: 10.1084/jem.20092454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gebhardt T, Wakim LM, Eidsmo L, Reading PC, Heath WR, Carbone FR. Memory T cells in nonlymphoid tissue that provide enhanced local immunity during infection with herpes simplex virus. Nat Immunol. 2009;10(5):524–530. doi: 10.1038/ni.1718. [DOI] [PubMed] [Google Scholar]
- 58.Le Floc’h A, et al. Alpha E beta 7 integrin interaction with E-cadherin promotes antitumor CTL activity by triggering lytic granule polarization and exocytosis. J Exp Med. 2007;204(3):559–570. doi: 10.1084/jem.20061524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wakim LM, Woodward-Davis A, Bevan MJ. Memory T cells persisting within the brain after local infection show functional adaptations to their tissue of residence. Proc Natl Acad Sci U S A. 2010;107(42):17872–17879. doi: 10.1073/pnas.1010201107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li Q, et al. Visualizing antigen-specific and infected cells in situ predicts outcomes in early viral infection. Science. 2009;323(5922):1726–1729. doi: 10.1126/science.1168676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Buchbinder SP, et al. Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet. 2008;372(9653):1881–1893. doi: 10.1016/S0140-6736(08)61591-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stanberry LR, et al. Glycoprotein-D-adjuvant vaccine to prevent genital herpes. N Engl J Med. 2002;347(21):1652–1661. doi: 10.1056/NEJMoa011915. [DOI] [PubMed] [Google Scholar]
- 63.Zhu J, et al. Virus-specific CD8+ T cells accumulate near sensory nerve endings in genital skin during subclinical HSV-2 reactivation. J Exp Med. 2007;204(3):595–603. doi: 10.1084/jem.20061792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Van Damme L, et al. Effectiveness of COL-1492, a nonoxynol-9 vaginal gel, on HIV-1 transmission in female sex workers: a randomised controlled trial. Lancet. 2002;360(9338):971–977. doi: 10.1016/S0140-6736(02)11079-8. [DOI] [PubMed] [Google Scholar]
- 65.Buck CB, Thompson CD. Production of papillomavirus-based gene transfer vectors. Curr Protoc Cell Biol Chapter. 2007;26:Unit 26 21. doi: 10.1002/0471143030.cb2601s37. [DOI] [PubMed] [Google Scholar]
- 66.Johnson KM, Kines RC, Roberts JN, Lowy DR, Schiller JT, Day PM. Role of heparan sulfate in attachment to and infection of the murine female genital tract by human papillomavirus. J Virol. 2009;83(5):2067–2074. doi: 10.1128/JVI.02190-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Buck CB, Thompson CD, Roberts JN, Muller M, Lowy DR, Schiller JT. Carrageenan is a potent inhibitor of papillomavirus infection. PLoS Pathog. 2006;2(7):e69. doi: 10.1371/journal.ppat.0020069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lawson CM, Bennink JR, Restifo NP, Yewdell JW, Murphy BR. Primary pulmonary cytotoxic T lymphocytes induced by immunization with a vaccinia virus recombinant expressing influenza A virus nucleoprotein peptide do not protect mice against challenge. J Virol. 1994;68(6):3505–3511. doi: 10.1128/jvi.68.6.3505-3511.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Coles RM, Mueller SN, Heath WR, Carbone FR, Brooks AG. Progression of armed CTL from draining lymph node to spleen shortly after localized infection with herpes simplex virus 1. J Immunol. 2002;168(2):834–838. doi: 10.4049/jimmunol.168.2.834. [DOI] [PubMed] [Google Scholar]
- 70.Cuburu N, et al. Sublingual immunization with nonreplicating antigens induces antibody-forming cells and cytotoxic T cells in the female genital tract mucosa and protects against genital papillomavirus infection. J Immunol. 2009;183(12):7851–7859. doi: 10.4049/jimmunol.0803740. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.