Abstract
Objective
This paper explored pharmacy staff perceptions of the strengths and weaknesses of electronic prescribing (e-prescribing) design in retail pharmacies using the sociotechnical systems framework. This study examined how adoption of e-prescribing technology is affecting clinical practice and patient care.
Materials and methods
Direct observations and think aloud protocols were used to collect data from seven retail pharmacies.
Results
Pharmacists and pharmacy technicians reported strengths of e-prescribing design that facilitated pharmacy work which included: legibility, ease of archiving, quick access to prescriptions and consistency in the format of electronic prescriptions (e-prescriptions). Design weaknesses and potential hazards to patient care associated with e-prescribing systems were due to differences between pharmacy and prescriber computer systems which resulted in the selection of wrong patient or drug (name, directions, dose, strength, formulation, package sizes). There were unique strengths and weaknesses in the design of e-prescriptions peculiar to the three pharmacy computer systems examined in this study.
Discussion
Findings from this study can help inform policy on creating e-prescribing design standards for pharmacy. e-Prescribing system developers can use the results of this study to identify and apply the most usable features of the three main pharmacy computer systems to design systems that support dispensing efficiency and safety.
Conclusions
This is the first study to highlight design flaws with e-prescribing in retail pharmacies. The sociotechnical systems framework was useful in providing an indepth understanding of the pharmacist and pharmacy technician's interface with e-prescribing technology. This information can be used by policy makers to create e-prescribing standards for pharmacies.
Keywords: Electronic prescribing, pharmacy, health information technology, medication safety, sociotechnical systems
Introduction
Electronic prescribing (e-prescribing) is defined as the direct computer-to-computer transmission of prescriptions from prescriber offices to retail pharmacies.1 Electronic prescriptions (e-prescriptions) are generated within Computerized Physician Order Entry systems and are electronically transmitted to pharmacies via a secure electronic network between prescribers and pharmacies.2 e-Prescribing was initially intended to allow for medication orders to be received and processed electronically thereby completely eliminating the use of paper in the processing of prescriptions in pharmacies. The ultimate goal of implementing e-prescribing was to achieve the following: reduce medical errors, decrease pharmacy costs, improve both prescriber and pharmacy efficiency, eliminate handwriting interpretation errors, reduce phone calls between pharmacists and physicians, reduce data entry, and expedite prescription refill requests.3
Prior to the adoption of e-prescriptions, handwritten prescriptions were the primary means of communicating drug choice and therapy of a patient between prescribers and pharmacists. The hazards associated with poor handwritten prescriptions such as difficulties with readability, risk of misinterpretation and falsification of handwritten prescriptions prompted the adoption of e-prescriptions.4 Of all commonly used health information technology (HIT), e-prescribing has received the most attention for its potential to improve safety.5 e-Prescribing use is now being promoted as an integral component of HIT and has been mandated for use by all prescribers by federal government regulations on meaningful use of HIT. e-Prescribing use by prescribers and pharmacists is expected to improve the safety, quality and efficiency of patient care. It has also been speculated that e-prescribing use can improve patient satisfaction with care by reducing waiting time at the pharmacy.6 Since this mode of transmitting prescriptions has been mandated by the federal government, approximately 91% of retail pharmacies are now receiving e-prescriptions.7
The number of e-prescriptions received nationwide in retail pharmacies, such as Walgreens and Medicine Shoppe pharmacies, has rapidly increased. In 2010, over 320 million e-prescriptions were transmitted to pharmacies nationwide, while only 191 million prescriptions were received electronically in 2009, a 72% increase.8 Studies conducted with physicians who generate and transmit e-prescriptions to pharmacies have indicated that problems exist with e-prescribing systems due to poor implementation and usability of these systems.9 However, little is known about e-prescription processing in retail pharmacies.
Retail pharmacies have been the forerunners in the adoption of HIT, having adopted computer systems to manage patients' prescription profiles and electronic billing for prescriptions for over 3 decades.10 There is clear evidence that the usability of HIT is an important factor for meaningful use by all healthcare professionals affected by its adoption.11 Compared with hospitals, the usability of e-prescribing systems is rarely studied in retail pharmacies, the recipients of e-prescriptions. Studies have reported inconsistent results in explaining how e-prescribing affects the quality of patient care. One study reported that pharmacists perceived key weaknesses in how e-prescribing had been implemented in their organizations.12 Another study found that e-prescribing presented certain threats to safe dispensing of medications.13 These two studies examined e-prescribing technology when it was in its infancy and their evaluation was based on national chain pharmacies (such as Walgreens and CVS) and excluded independent pharmacies. Little is known about the extent to which the design of e-prescribing technology facilitates or hinders processing of prescriptions in pharmacies. To our knowledge, this is the first study to examine the design of e-prescribing in retail pharmacies.
Objective
The purpose of this study was to explore pharmacy staff perceptions of the positive and negative aspects of e-prescribing in retail pharmacies and to understand how e-prescribing design facilitates or hinders efficient and safe processing of prescriptions.
Materials and methods
Conceptual framework
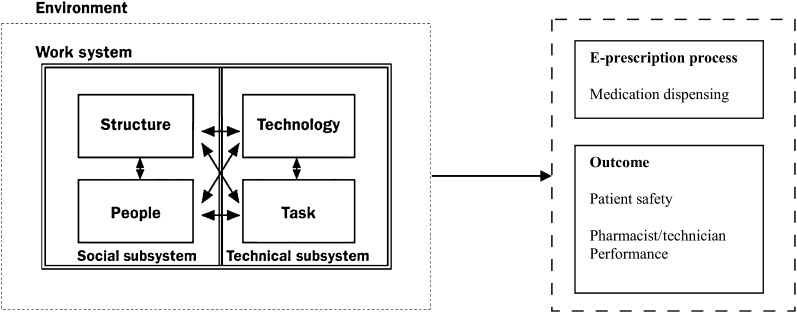
Adoption of technology in healthcare settings affects both the technical and social aspects of the work system. We applied the sociotechnical system (STS) theory developed in the 1940s and 1950s by Trist to describe the cause of problems arising from the adoption of technology in mining organizations.14 STS theory was used as a guiding framework to understand how the strengths and weaknesses of current e-prescription design is affecting pharmacy practice. This approach has been used extensively by human factors engineers to characterize, evaluate and improve the design of human–computer interfaces.15 16 STS theory assumes a systems perspective which takes into consideration the social, technical and environmental work elements of a user's interface with technology. This systematic approach was used to investigate the different design and functional capabilities of e-prescribing technology and to identify the potential design weaknesses. Figure 1 shows how this framework was applied to pharmacy. Experts in human factors engineering have found that qualitative (observational) methods provide direct information about the human–technology interaction. These methods tend to have strong face validity.16 17 We used a qualitative approach to characterize the design strengths and weaknesses of pharmacy e-prescribing technology design interface, and compare the e-prescribing design features among three major pharmacy computer systems.
Figure 1.
Application of sociotechnical systems framework.
Design and setting
We examined e-prescription processing in retail pharmacies using PDX (Forth Worth, Texas, USA), QS/1 (Spartanburg, South Carolina, USA), and McKesson PharmaServ (San Francisco, California, USA) computer software. These computer systems are used by pharmacy staff for various aspects of handling prescriptions such as receiving prescriptions from prescribers, managing patients' medical information and prescription profile, online real-time insurance adjudication, and inventory control. Pharmacies had to meet the following criteria to participate in this study: (1) be a retail pharmacy and not a hospital pharmacy (only one pharmacy recruited per corporation); (2) process a minimum of 10 e-prescriptions daily; and (3) process e-prescriptions from the electronic order (vs immediately printing the e-prescription to paper and handling the prescription as a paper prescription). These strict inclusion criteria were developed to ensure that only pharmacies that frequently used e-prescribing as originally designed were selected.
In December 2010, pharmacists were initially recruited by a solicitation through the Pharmacy Society of Wisconsin (PSW) Fast Facts listserv, a weekly electronic newsletter distributed to all PSW members via email. A follow-up invitation was sent to pharmacists on the PSW listserv 1 month after the original invitation in order to recruit more pharmacists. Pharmacists representing 19 pharmacies responded to the PSW solicitation but 15 of these pharmacies did not meet the study criteria and were excluded from the study because they printed e-prescriptions and handled them as traditional paper prescriptions. A targeted snowball sampling was then used to recruit additional pharmacists. Pharmacists were identified and recruited based on the study criteria in order to have at least two pharmacies with the same computer system in the study. Once the pharmacist agreed to participate in the study, we received permission to recruit the other pharmacists and technicians that worked in the pharmacy. Letters of support were obtained from each pharmacy in order to receive ethical approval for the study. Approval was granted by the University of Wisconsin-Madison Institutional Review Board. Written informed consent forms were obtained from all participants: seven pharmacists and nine technicians from seven retail pharmacies.
Data collection
Qualitative data were collected using direct observations and think aloud protocols between January and February 2011. The researcher observed pharmacy workflow practices that pertained to e-prescriptions processing. The duration of observation ranged from 2 to 5 h depending on the frequency of receiving e-prescriptions. E-prescribing workflow included the time from when an e-prescription is received in the pharmacy to the time the patient received the medication. Each participant was observed processing at least five consecutive e-prescriptions.
Think aloud protocol is an observation method that provides empirical and procedural information about human–technology interaction.18–20 Think aloud protocol has been used in pharmacy research to evaluate the textual signals used by pharmacists for detection of adverse drug events as they process medication orders.21 The goal of using this method of data collection was to provide objective information on how pharmacy staff interact with e-prescribing technology. For example, how e-prescriptions were handled real-time in pharmacies, workflow challenges that emerged and information needs of the pharmacy staff when handling e-prescriptions.
During the think aloud protocols, participants were instructed to verbalize their thoughts as they processed each e-prescription and to highlight the signals that helped or hindered them from processing prescriptions accurately and efficiently. With every step in the dispensing process, participants were asked to verbally state what they were thinking about, what information they needed to fulfil each step, what questions they had and how they would proceed to the next step. The average duration for each think aloud protocol ranged from 3 to 7.5 min. The time that it took to complete each think aloud protocol was dependent on the type of prescription, interruptions in the environment and pharmacy workflow. Recording of each think aloud protocol began when the participant started processing the e-prescription on the computer and ended when the participant indicated that he or she was done with e-prescription processing. Additional information was also collected by the researcher using field notes to contribute to the responses that were audio-taped and digitally recorded. Sample questions that participants may be thinking about during the think aloud are provided in the online appendix.
Data analysis
Field notes and audio-recordings were transcribed resulting in a total of 108 pages of single-spaced pages of transcription. Transcripts were originally coded manually in a Microsoft Word 2007 document according to the five main elements (environment, people, technology, tasks and structure) of the STS framework. Key interactions were identified through by a detailed content analysis by (OO). Transcripts were subjected to qualitative thematic analysis by the two researchers (OO and MC). Thematic analysis is an analytical method in qualitative research which involves identifying themes or patterns within data.22 Both researchers met to deliberate and reach a consensus on the classification and interpretation of themes to ensure consistency. In addition to categorizing the data into themes inductively, data were also categorized to link the key interactions identified to examine their effect on e-prescribing processing, pharmacist performance and patient safety. In conducting the analysis, several themes and subthemes relevant to the sociotechnical aspects of e-prescribing in retail pharmacies were identified and annotated in the margin of the transcripts. Triangulation was done with two methods of data collection, direct observation and think aloud protocol. Triangulation involved the comparison of the data obtained from the two methods of data collection to ensure cross validity between the recurrent themes identified. Data obtained from the individual pharmacies were compared for accuracy and precision in describing the use of e-prescribing technology in pharmacies.
Results
Table 1 shows the characteristics of pharmacies that participated in this study. Table 2 contains selected verbatim quotes from participants about e-prescribing related to each theme so that readers can assess the correspondence between original data and the researchers' interpretation. Three major themes emerged from the data. Based on the themes identified, the primary STS interactions that were found were between three constructs: technology, people and tasks. The design of the e-prescribing in each pharmacy affected how the participants performed their tasks related to processing of prescriptions; it also influenced their performance and the likelihood of making an error. The themes described below were patterns that were seen across all pharmacies.
Table 1.
Participating pharmacies
| Pharmacies | Dispensing system | eRx experience (in years) | Daily eRx volume | Daily Rx volume | Daily staffing | Practice setting |
| 1 | PDX | 2–3 | 33% | 150–200 |
|
Chain |
| 2 | PDX | 2–2.5 | 90% | 150 |
|
Chain |
| 3 | PDX | 5 | 50% | 130–180 |
|
Chain |
| 4 | QS/1 | 2 | 50% | 107–614 |
|
Independent |
| 5 | QS/1 NRx | 0.5 | 90% | 200 |
|
Independent |
| 6 | Pharmaserv | 1 | 50% | 200–450 |
|
Independent |
| 7 | Pharmaserv | 2 | 80% | 300–400 |
|
Independent |
eRx, electronic prescription; Rx, prescription.
Table 2.
Sample quotes from pharmacists and technicians about e-prescribing design
| Related subtheme | Sample quotes |
| Positive aspects of eRx design | |
| Legibility | ‘You don't have to worry about legibility. Legibility doesn't become an issue anymore because everything is all typed in.’ |
| Differences between eRx design | |
| PDX | ‘The way ours is presented it's split screen, so on the left is what you get from the doctor and on the right is what we're processing. It's nice to be able to compare it right away, without having to switch between screens.’ |
| QS1 |
|
| Drawbacks of eRx design | |
| Mismatch related to textbox sizes |
|
| Mismatch related to drug names | ‘It doesn't match the drug. It doesn't give me choices like this right away. You have to re-enter the drug. The problem there is that there could be an error. Because I could choose the wrong drug. You know there's no link between the drug that comes in over the e-scribe with the drug that we have in our stock. So I have to choose the drug every time. There's potential for error.’ |
| Mismatch related to patient/physician names | ‘If for example the patient's name is [Jonathan Doe], and the doctor puts the e-scribe in for Jon. It may say you don't have that person in the system because they are writing his short name versus his full name or whatever we have. So then it would tell you we don't have them in there. Or another thing too that is irritating is the doctor's name that e-scribes is just written different than what's in our McKesson system, it will create them again. So when we look into our list of doctors we have one Dr [Jeff] but there might be 7 in there. Each one might have a different fax, might not have a fax number or has a different fax number… That's one down thing about it is if the doctor that it's faxed from adds like even a middle initial or something like that, it would create them in there again.’ |
| Mismatch related to drug quantities |
|
| Inability to discontinue old e-prescriptions |
|
eRx, electronic prescription.
Theme 1: design strengths of e-prescriptions
Consistent sequence
Although there were slight differences in the physical presentation of each prescription in the pharmacy systems, each system always presented e-prescription information to pharmacy staff in the same order. This allowed for the pharmacy staff to develop a systematic method for processing prescriptions. The consistency in presentation of information was viewed as an advantage that allowed participants to adapt quickly to processing e-prescriptions irrespective of the computer system. Participants processed e-prescriptions on the computer in this sequence: Patient name→Date of birth→Drug name→Drug strength→Drug formulation/route→ Drug directions→Drug quantity/package size/days supply/duration→Physician name→Dispense as written code. This was not the case with conventional prescriptions, where pieces of information were rarely presented in the same location on the paper or faxed prescription.
Ease of legibility
Improved legibility was cited numerous times by participants as a key benefit of e-prescriptions. This was the case because e-prescriptions were generally easier to read and therefore faster to process when compared with other types of prescriptions whereby interpretation of prescriber handwriting was an issue. Unlike handwritten prescriptions, e-prescriptions did not require the pharmacist to interpret the prescriber's handwriting or make frequent calls to the prescriber to clarify illegible handwritten prescription information.
Ease of archiving
An unanticipated positive consequence of e-prescribing use in retail pharmacies was time saved in retrieving old prescriptions. Prior to e-prescriptions, pharmacy staff either had to look through stacks of chronologically archived paper files or manually search for scanned prescriptions saved on their computer to retrieve old prescriptions. In contrast, e-prescriptions allowed for immediate storage and retrieval of hardcopies of electronically received prescriptions in the exact form in which they were sent. This enabled easy and quick access to e-prescriptions on the computer when needed.
Theme 2: design challenges with e-prescribing
Possible differences between pharmacy and prescriber computer systems were often suggested by participants to be a cause of design challenges that participants encountered while processing e-prescriptions. These resulted in difficulty in retrieving complete information sent electronically to the pharmacy.
Mismatch in textbox size
A mismatch between textbox sizes for prescription information in the prescriber and pharmacy system was observed numerous times. As a result, pharmacy staff were unable to see complete e-prescription information such as drug names or instructions. When the pharmacy textbox was not long enough to fit the length of the drug directions written by the prescriber, the screen cut off parts of the directions or appeared as ‘see long drug name’. The participants could only view the truncated drug directions in full when the e-prescription was printed on paper. In addition, when long drug names were sent from prescribers, the participants were not immediately aware of what the prescriber had ordered. This was common with drug combinations such as a fluticasone–salmeterol inhaler or ear/eye drops with common active ingredients but different routes of administration.
Mismatch in patient/physician names
Frequently, there was a mismatch between how names of patients or prescribers were saved in the pharmacy's and the prescriber's system especially when abbreviated names or initials were used in either system. This led to difficulty in finding the patient's or prescriber's names in the pharmacy system as e-prescriptions were being processed. Pharmacy staff sometimes selected the wrong patient or prescriber when there were many people bearing similar names (potentially because duplicate names were added in the past). In such cases, the pharmacy staff took extra steps to retrieve the patient's date of birth from a different screen to verify the correct patient. This problem also proved to be a challenge when pharmacists had to contact the prescriber for clarification on e-prescriptions. If participants could not find the right name of the prescriber they were unable to find the correct contact information. This required more steps to process the e-prescriptions. This distracted participants and prevented them from attending to more pressing issues in the pharmacy, and resulted in delays in patients receiving their medications.
Mismatch with drug quantities
When processing prescriptions, pharmacist and technicians typically have to calculate or infer the days' supply of the medication from the directions and quantity requested by the prescriber for purposes of insurance adjudication (ie, a direction of ‘take one tablet every 4–6 h’ with a quantity of 30 was calculated as a 7 days' supply). When prescribing traditional dosage forms such as tablets or liquid, prescribers are used to ordering a standard quantity such as 30 tablets or four ounces (of liquid). However, for more atypical dosage forms, such as inhalers, eye drops and insulin needles, prescribers typically order units (ie, one inhaler, one box of needles) on paper prescriptions.
Pharmacists knew that the actual quantity was the weight of the inhaler, for instance, ‘Combivent inhaler quantity #1’ is actually ‘15 gm’ and transcribed the correct quantity when they manually entered the paper prescription into the computer system. However, with e-prescriptions, the wrong quantity was auto-loaded into the pharmacy system and therefore more easily missed. This led to wrong days' supply entries, incorrect pharmacy billing, inventory problems and insurance rejections. Participants had to be extra vigilant in checking for the correct drug quantity and to recalculate when necessary.
Inability of the technology to discontinue old prescriptions
The technology design could not identify similar e-prescriptions for the same patient in the pharmacy computer system. As a result, for every new e-prescription that was received in the pharmacy, participants were required to review past e-prescriptions to verify that this was truly a new prescription and to keep patient profiles up-to-date and accurate. If old prescriptions were not discontinued by the participant, this led to inaccurate patient drug histories in the pharmacy system and inadequate drug utilization reviews by the pharmacist. Hence, when participants were processing an e-prescription they always had to backtrack into the patient's profile and inactivate a previous e-prescription similar to the new one received, taking several additional time-consuming steps in the prescription dispensing process.
Theme 3: unique strengths and limitations of e-prescriptions in different pharmacy systems
Pharmacy prescription processing computer systems were used to support and document the work conducted in pharmacies such as prescription filling, prescription pricing, third party claim processing, refill authorizations, data reports, reconciliation and inventory management. All e-prescriptions contained similar information. However, e-prescriptions were presented differently in each of the three pharmacy systems and this influenced how they were processed. Participants identified aspects of the e-prescriptions design that resulted in delays in dispensing of medications.
PDX pharmacy system
When e-prescriptions were transmitted to pharmacies with the PDX systems, the computer screen was divided into a left and right section with similar text box information. On the left-hand side is the e-prescription transmitted from physician offices while on the right-hand side was the e-prescription that was to be input manually into the pharmacy system and dispensed to the patient. The pharmacy staff then entered information into each part of the prescription only on the right-hand side of the computer screen. Pharmacy staff simultaneously compared each text box on the left-hand side with what was being entered on the right hand side. Some aspects of the e-prescription on the left-hand side could be auto-loaded to the e-prescription on the right-hand. There were quick codes that pharmacy staff had memorized to search for relevant information on patients' profiles.
The primary advantage of this system design was that it allowed for immediate simultaneous comparison of information being input by the pharmacist or pharmacy technician and information sent by prescriber. The computer monitor was split into two. However, a primary design flaw with this system was that unlike other systems where information was auto-loaded from the e-prescription to the pharmacy system, participants had to manually re-enter more information. Participants stated that errors could easily occur when re-inputting information.
QS/1 pharmacy system
In order to fill an e-prescription using in the QS/1 system, e-prescription processing occurred in many steps because information on the original e-prescription sent from the prescriber was separated into different screens. For example, the initial screen showed only the prescriber and patient name, while the second screen showed only the drug name without the patient or prescriber's information.
Pharmacy staff had to constantly flip between at least three different screens to view and manually input all the information on each e-prescription (such as drug name or doctor's name). This forced participants to memorize parts of the e-prescription that were not always on display. This design flaw prevented participants from having a holistic view of the entire prescription and assessing if the totality of the prescription information fit together safely and effectively for the patient. For instance, participants might want to clarify that the prescribed dose was appropriate for a pediatric patient.
McKesson PharmaServ pharmacy system
Unlike the PDX or QS/1 systems, PharmaServ was a windows-based system. The monitor presentation contains clearly marked sections that have detailed information such as patient profile, medication order and drug cost information. However, some of the information provided is not necessarily for immediate processing of the e-prescription, such as driver's license ID and social security number. Such information overload was a distraction and prevented participants from focusing their attention on more important parts of the e-prescription. Another problem with this design was that it easily resulted in wrong selection of drug name and drug dose because it required frequent use of dropdown menus.
One unique characteristic of this system was the colored buttons at the bottom of the computer screen that indicate the status of e-prescriptions. These colored buttons provided quick access to real time numbers on e-prescriptions yet to be filled, successfully filled or rejected by insurance with the use of colored icons on the screen. It was more appealing in its presentation and ease of use for participants.
Discussion
The adoption of e-prescriptions is gradually reshaping the field of retail pharmacy.23 Many studies conducted in hospital settings have identified design flaws in HIT such as Computerized Physician Order Entry and Bar Code Assisted Medication Administration technology.24 25 These design flaws have been linked to poor clinical outcomes which can easily lead to patient harm.26 Consequently, poorly designed HIT can negatively affect clinical practice.
The relevant STS interactions noted were among the technology, the users (people) and the e-prescribing tasks performed; these interactions had the potential to affect pharmacists' performance and increased the likelihood of making errors when processing the prescriptions. Our findings show that some current design of e-prescribing systems have design flaws that may result in new kinds of unintended technology hazards in retail pharmacies that were previously not envisioned. These technology hazards may lead to medication errors and patient harm. Furthermore, poor design of e-prescribing technology may negatively affect pharmacy workflow and can hinder pharmacists' ability to efficiently and safely dispense medications to patients. The findings in this study are particularly important because they provide valuable information to HIT designers about changes that can be made to improve e-prescribing systems and the need for standardization of the design of e-prescriptions across healthcare settings.
Study limitations
This study has several important limitations. First, only one observer collected the data which may present a measure of subjectivity in the data collected. However, two data collection methods were used and triangulation was done to compare information from both data sources. Second, only 2–4 h of observation was done in each pharmacy. However, this was sufficient in reaching data saturation. In addition, only seven pharmacies in Wisconsin participated in this study, and other pharmacies had to be excluded from this study because they did not process e-prescriptions as originally designed. Therefore, these results may not be generalizable to all pharmacies. However, the pharmacy computer systems studied are commonly used in many retail pharmacies.
Conclusions
As the number of e-prescriptions received in pharmacies continues to rise annually, there is a need for further research on the impact of the design of e-prescribing systems on safe and efficient delivery of patient care in retail pharmacies. This study motivates future large scale studies to determine whether reported e-prescribing hazards lead to a measurable increase in medication errors and patient harm in pharmacy settings. It is important to identify how problems with e-prescribing affect the pharmacists' ability to provide efficient and safe care to patients, and to empirically evaluate and compare the number and type of medication errors that may result from various pharmacy prescription processing systems. First, we need to assess how pharmacies are working around poorly designed e-prescription technology in order to prevent medication errors. Second, it is necessary to investigate how the current systems can be redesigned to address patient safety concerns of pharmacists by creating a new system that combines and highlights the design strengths of each system.
Finally, the STS framework was useful in providing an indepth understanding of the pharmacist and technician interface with e-prescribing technology. Results from this study can help inform policy on creating e-prescribing design standards for pharmacy. e-Prescribing system developers can use these study findings to identify and apply the most usable features of the three main pharmacy computer systems to design systems that support dispensing efficiency and safety.
Supplementary Material
Acknowledgments
The authors would like to thank the staff at the community pharmacies that supported and participated in this research. We would also like to thank Drs David Mott, Henry Young and John Lee for their feedback and comments during the research and manuscript preparation. Michelle Chui was supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR), grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Contributors: hipOO and MC had access to the raw data. Both authors take full responsibility for the accuracy of the data analysis and contributed to the writing of the manuscript, the interpretation of data and approved the final version.
Funding: The Community Pharmacy Foundation provided funding for this study, grant number: #70549. The Funder was not involved with the conceptualization, data collection, analysis, or write-up of this project.
Competing interests: None.
Ethics approval: Ethics approval for this study was provided by the University of Wisconsin-Madison Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: We also obtained additional unpublished data from this study on how electronic prescribing impacts pharmacy workflow and by conducting focus group interviews.
References
- 1. Lapane KL, Waring ME, Schneider KL, et al. A mixed method study of the merits of e-prescribing drug alerts in primary care. J Gen Intern Med 2008;23:442–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moniz TT, Seger AC, Keohane CA, et al. Addition of electronic prescription transmission to computerized prescriber order entry: effect on dispensing errors in community pharmacies. Am J Health Syst Pharm 2011;68:158–63 [DOI] [PubMed] [Google Scholar]
- 3. Webster L, Spiro RF. Health information technology: a new world for pharmacy. J Am Pharm Assoc (2003) 2010;50:e20–31, quiz e32–4. [DOI] [PubMed] [Google Scholar]
- 4. Astrand B, Montelius E, Petersson G, et al. Assessment of ePrescription quality: an observational study at three mail-order pharmacies. BMC Med Inform Decis Mak 2009;9:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kaushal R, Kern LM, Barron Y, et al. Electronic prescribing improves medication safety in community-based office practices. J Gen Intern Med 2010;25:530–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thomas CP, Kim M, McDonald A, et al. Prescribers' expectations and barriers to electronic prescribing of controlled substances. J Am Med Inform Assoc 2012;19:375–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lapane KL, Waring ME, Schneider KL, et al. E-prescribing and patient safety: results from a mixed method study. Am J Pharm Benefits 2011;3:24–33 [PMC free article] [PubMed] [Google Scholar]
- 8. Surescripts The National Progress Report on E-Prescribing and Interoperable Healthcare. About E-Prescribing Web Site. 2010. http://www.surescripts.com/about-e-prescribing/progress-reports/national-progress-reports.aspx (accessed 29 Sep 2011). [Google Scholar]
- 9. Chan J, Shojania KG, Easty AC, et al. Does user-centred design affect the efficiency, usability and safety of CPOE order sets? J Am Med Inform Assoc 2011;18:276–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Siska MH, Tribble DA. Opportunities and challenges related to technology in supporting optimal pharmacy practice models in hospitals and health systems. Am J Health Syst Pharm 2011;68:1116–26 [DOI] [PubMed] [Google Scholar]
- 11. Goldberg L, Lide B, Lowry S, et al. Usability and accessibility in consumer health informatics current trends and future challenges. Am J Prev Med 2011;40(5 Suppl 2):S187–97 [DOI] [PubMed] [Google Scholar]
- 12. Rupp MT, Warholak TL. Evaluation of e-prescribing in chain community pharmacy: best-practice recommendations. J Am Pharm Assoc (2003) 2008;48:364–70 [DOI] [PubMed] [Google Scholar]
- 13. Warholak TL, Rupp MT. Analysis of community chain pharmacists' interventions on electronic prescriptions. J Am Pharm Assoc (2003) 2009;49:59–64 [DOI] [PubMed] [Google Scholar]
- 14. Trist E. The Evolution of Socio-Technical Systems. Occasional Paper No. 2. In: Van de Ven A, Joyce W, eds. Perspectives on Organizational Design and Behavior. Ontario, Canada: Wiley Interscience, 1981. http://www.sociotech.net/wiki/images/9/94/Evolution_of_socio_technical_systems.pdf (accessed 22 Jun 2012). [Google Scholar]
- 15. Harrison MI, Koppel R, Bar-Lev S. Unintended consequences of information technologies in health care—an interactive sociotechnical analysis. J Am Med Inform Assoc 2007;14:542–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Holden RJ, Karsh BT. A theoretical model of health information technology usage behaviour with implications for patient safety. Behav & Ion Techngy 2009;28:21–38 [Google Scholar]
- 17. Carayon P, Wetterneck TB, Hundt AS, et al. Observing nurse interaction with infusion pump technologies. In: Henriksen K, Battles JB, Marks ES, et al., eds. Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology). Rockville, MD: Agency for Healthcare Research and Quality (AHRQ), 2005 [PubMed] [Google Scholar]
- 18. Lundgren-Laine H, Salantera S. Think-aloud technique and protocol analysis in clinical decision-making research. Qual Health Res 2010;20:565–75 [DOI] [PubMed] [Google Scholar]
- 19. Fairbanks RJ, Caplan SH, Bishop PA, et al. Usability study of two common defibrillators reveals hazards. Ann Emerg Med 2007;50:424–32 [DOI] [PubMed] [Google Scholar]
- 20. Wu RC, Orr MS, Chignell M, et al. Usability of a mobile electronic medical record prototype: a verbal protocol analysis. Inform Health Soc Care 2008;33:139–49 [DOI] [PubMed] [Google Scholar]
- 21. Phansalkar S, Hoffman JM, Hurdle JF, et al. Understanding pharmacist decision making for adverse drug event (ADE) detection. J Eval Clin Pract 2009;15:266–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pope C, May N. Qualitative Research in Healthcare. 3rd edn Oxford, UK: Blackwell Publishing Ltd, 2006 [Google Scholar]
- 23. Motulsky A, Winslade N, Tamblyn R, et al. The impact of electronic prescribing on the professionalization of community pharmacists: a qualitative study of pharmacists' perception. J Pharm Pharm Sci 2008;11:131–46 [DOI] [PubMed] [Google Scholar]
- 24. Koppel R, Wetterneck T, Telles JL, et al. Workarounds to barcode medication administration systems: their occurrences, causes, and threats to patient safety. J Am Med Inform Assoc 2008;15:408–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA 2005;293:1197–203 [DOI] [PubMed] [Google Scholar]
- 26. Karsh BT. Beyond usability: designing effective technology implementation systems to promote patient safety. Qual Saf Health Care 2004;13:388–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.