Abstract
Introduction
Cell-based therapies for regeneration of the degenerated intervertebral disc (IVD) are an alternative to current surgical intervention. Mesenchymal stem cells (MSCs), in combination with a scaffold, might be ideal candidates for regenerating nucleus pulposus (NP), the pressure-distributing part of the IVD. While the use of growth factors for MSCs differentiation currently receives major attention, in this study we compare the performance of sponge-like matrixes in supporting cell differentiation into NP-like cells.
Materials and methods
Four types matrixes approved as medical devices for other applications were tested as scaffolds for MSCs: two made of equine or porcine collagen, one of gelatin and one of chitosan. Bone marrow-derived human MSCs were seeded in these scaffolds or embedded in alginate, as a three-dimensional control. After five weeks in culture, NP-like differentiation of the cell-scaffold constructs was analyzed by qRT-PCR, histology, total DNA quantification, proteoglycan accumulation and immunohistochemistry.
Results
MSCs in collagen matrixes and gelatin produced more mRNA and proteins of the chondrogenic markers collagen type I, collagen type II (COL2) and aggrecan (ACAN), when compared with cells embedded in alginate or chitosan. Proteoglycan accumulation and cell survival were also higher in collagen and gelatin matrixes. Gene expression results were also confirmed by histological and immunohistochemical staining. In contrast to alginate control, the gene expression of the undesired bone marker osteopontin was lower in all tested groups. In porcine collagen supports, MSC expression ratio between COL2/ACAN closely resembled the expression of nucleus pulposus cells, but gene expression of recently described NP markers keratin19, PAX1 and FOXF1 was lower.
Conclusions
Collagen supports provide a readily available, medically approved and effective scaffold for chondrogenic differentiation in vitro, but the phenotype of differentiated MSCs is not yet completely equivalent to that of NP cells.
Keywords: Mesenchymal stem cells, Chondrogenesis, Intervertebral disc, Nucleus pulposus and three-dimensional cultures
Introduction
Regenerative medicine is a rapidly expanding field and some potential treatments are already in clinical trial stages, but still there are no available cures for intervertebral disc (IVD) degeneration. IVDs are considered as the major “joints” of the spine and structurally they comprise of a gelatinous nucleus pulposus (NP) in the center, surrounded by the collagen-rich annulus fibrosus (AF), and they are connected on the upper and lower faces to the vertebral body by cartilage the end-plates [1]. The main components of the NP are an amorphous mix of proteoglycans, in particular aggrecan (ACAN), which by absorbing water provide stiffness, compression resistance and viscoelasticity, and collagen type II (COL2), which is responsible for NP tensile strength [2]. This particular matrix composition is qualitatively very similar to that of the articular cartilage tissue, but it differs in the ratio between proteoglycans and COL2; in cartilage it is 2:1, whereas in the NP is 27:1 [3]. While multifactoral causes for disc degeneration are proposed, such as genetics (polymorphisms in the genes of SOX9 and Collagen type IX [4]), age, lifestyle and extended mechanical loads on the spine column [5], there is no consensus on what leads to disc degeneration, which is characterized by decreased extracellular matrix synthesis and cell death. Therefore, cell-based therapies should have a potential, in terms of recovery and healing of degenerated IVDs. Unlike gene and molecular therapies, which have problems such as the risks associated with viral gene transfer and growth factor production issues (intellectual property ownership and heavy clinical regulatory requirements) [6], autologous cell-based therapies have the advantages of improved safety and easier regulatory approval. Cell therapies have been tested in animal models with some success for degenerative disc disease [7], and some human clinical trials show an increase in the height of the degenerated disc and a reduction of pain in patients treated with disc-chondrocyte cells [8]. IVD tissue engineering with cells derived from the same tissue is characterized by some important limitations, such as the low cell availability in the degenerated tissue [9], and the great risk of damaging an intact IVD if cells were to be explanted from a healthy disc. Considering these problems, a better strategy to repair a degenerated disc might be to search for a different, more abundant cell type. The principal candidates for such therapies are the mesenchymal stem cells (MSCs), which are present in a number of tissues and can be extracted from bone marrow, adipose tissue, synovial membrane and umbilical cord tissue [10]. MSCs have a high proliferative capacity [11] and have the ability to differentiate into several cell types [12], including adipocytes [13], osteocytes [14] and chondrocytes [15], although their differentiation potential diminishes with passages in vitro [16]. As NP cells have a similar morphology and gene expression profile to articular chondrocytes, one can presume that MSCs might be able to differentiate into NP cells. In the disc, though, MSCs will face the challenges of a difficult environment, being the largest avascular organ of the human body, under constant load and hypoxic conditions [1]. In the case of implantation of a substantial number of stem cells, such conditions can lead to cell death rather than cell differentiation and matrix production. Additionally, after the removal of degenerated disc tissue, the implanted cells may need too much time to differentiate and generate new disc tissue and a more probable scenario might be that undesired scar tissue is formed instead [17]. To address these problems, the goal is to improve the viability of the cells and to accelerate the process of matrix production, which could be achieved by pre-differentiation of MSCs with the use of three-dimensional (3D) extracellular scaffolds. The use of scaffolds is a key step in the culturing of MSC for our understanding of cell fate and cell based therapies. Scaffolds facilitate cellular attachment, provide mechanical advantages for cell growth and an implantable scaffold should be suited to help infiltration, proliferation, and differentiation of MSC, thus mimicking the in vivo environment. A good scaffold should aid the introduction of chemical stimuli by appropriate composition of the matrix, which can immobilize growth factors and keep them at a higher local concentration than in the liquid phase of the culture. To induce MSC chondrogenesis growth factors such as transforming growth factor (TGF)-β1, 2 or 3 [18], bone morphogenetic protein-2 [19], -4 [20], -7 [21] or -14 (GDF-5) [22], have been described to facilitate MSCs differentiation, however the aim of this project was to focus on the differences caused by variety of matrixes. In particular, many studies already described culture of MSCs embedded in several types of scaffolds, such as agarose gels [23], alginate beads [24–26], synthetic polymers [27, 28] and other biomaterials [29–32]. These studies provide clear evidence that there is a need of a cell support for enhancing cell–cell and cell–matrix interactions and creating a 3D environment. In vitro differentiation of MSCs would require materials that were non-immunogenic, biodegradable and can withstand the mechanically loaded environment into the IVD. These scaffolds would have to degrade slowly (or not at all) to allow the seeded cells to differentiate and produce new matrix. The scaffolds tested in this work are sponge-like medical devices, of different composition, stiffness and porosity, which are normally used in surgical intervention as a support in wound management, as a haemostat or in wound healing.
We hypothesized that approved medical devices can be used as scaffolds for chondrogenic differentiation of MSCs in 3D cultures and analyzed in vitro differentiation of bone marrow-derived MSCs towards NP-like phenotype in four such matrixes, made of equine and porcine collagen, gelatin and chitosan. We investigated the grade of MSCs differentiation into a NP-like phenotype analyzing the expression and production of extracellular matrix proteins, and we compared the results with NP cells and fragments.
Materials and methods
Scanning electron microscopy and stiffness measurements of matrixes
For electron microscopy, a Philips XL 30 FEG ESEM was used. Secondary electron images were recorded using an acceleration voltage of 10 kV.
For the determination of the matrix stiffness, cylindrical specimens (6 mm diameter) were prepared with a biopsy punch and mounted between two parallel metal platens. Specimens were compressed in a ramp-and-hold sequence and the reaction force recorded by a load cell (10 N, ELPF, Measurement Specialties, Hampton, VA, USA). Scaffold specimens were compressed in steps of Δl = 1 mm (0.2 mm/s) and the displacement held for 20 s before applying the subsequent compression step. From the initial force peak of each step (ΔF), the equivalent elastic modulus (E) was calculated as E = ΔFlo/AΔl, where A is the cross-sectional area and lo the nominal height of the specimen.
MSCs isolation and culture
Fresh bone marrow (BM) samples were obtained from the iliac crest or the vertebral body of the donors during surgery after informed consent and approval by the ethics committee of canton Lucerne. MSCs were isolated from BM of ten patients (average age: 35 ± 14 years). The BM aspirates were diluted twofold in 3.8% sodium citrate and 1 × phosphate buffered saline (PBS) and filtered through a 100 μm cell strainer (Falcon, BD Bioscience). Mononuclear cells were separated by Ficoll gradient centrifugation (density 1.077 g/mL; GE Healthcare) in a Leucosep tube (Greiner) at 800g for 20 min, washed with PBS, centrifuged again at 250g for 10 min, re-suspended in 10 mL PBS and counted using trypan blue dye in a single use Neubauer chamber (C-Chip Typ Neubauer, Zeiss). Cells were placed in a T150 tissue culture flask (TPP) in Non-hematopoietic (NH) stem cell media (Miltenyi) at 37°C in a humid atmosphere containing 5% CO2. After 2 days, non-adherent cells were discarded, whereas adherent cells were cultured in DMEM/F12 + GlutaMAX, supplemented with 10% foetal bovine serum (FBS), (100 units/mL) penicillin/(100 mg/mL) streptomycin, 2.5 ng/mL amphotericin B (all GIBCO) and 5 ng/mL recombinant basic Fibroblast Growth Factor (bFGF, Peprotech) with medium changed 3 times a week. At 80% confluence, cells were harvested by dissociation with 0.05% trypsin, used for seeding scaffolds, or expanded to another passage, or cryopreserved at −150°C in a medium containing 45% DMEM/F12, 45% FBS and 10% dimethyl sulfoxide (DMSO). Cells used in this project were expanded for no more than 4 passages in culture.
NP Cells isolation and culture
Human NP cells were isolated from patients with disc trauma who underwent full or partial discectomy (Table 1) after approval of local ethics committee. NP fragments were digested with 0.05% collagenase (Sigma-Aldrich), 10% FBS, (100 units/mL) penicillin/(100 mg/mL) streptomycin in DMEM/F12 + GlutaMAX for 5 h at 37°C. After incubation, cell suspension was filtered through a 100 μm cell strainer and centrifuged for 5 min, and the pellet was washed with PBS. NP cells were expanded in culture for 20 days (two passages) as a monolayer in identical conditions as the ones used for expanding MSCs.
Table 1.
Demographic details of annulus fibrosus and nucleus pulposus donors
| Sample | Sex | Donor’s age (years) | Thompson grading scale | Type of operation |
|---|---|---|---|---|
| 1 | F | 44 | IV | Trauma Discectomy L2/3 |
| 2 | M | 29 | III | Trauma Discectomy L1/2 |
| 3 | M | 17 | IV | Trauma Discectomy L1/2 |
Average age = 30 ± 12 years old, (L lumbar vertebrae)
Scaffold constructs
The four sponge-shaped medical devices were made of collagen derived from different species, gelatin and chitosan. Collagen matrixes were composed of: lyophilized collagen extracted from horse flexor tendon (Biopad) or collagen from porcine corium (inner dermis layer) (ABE collagen, Beese) and gelatin––a partially hydrolyzed collagen (Spongostan, Ferrosan). The last matrix, chitosan (Beese medical), was produced by de-acetylation of chitin.
From these materials, cubes with 3 mm side length were cut and used as a support for cellular growth. The cell suspension was pipetted on the construct and completely absorbed by it. MSCs construct were kept at RT for 30 min to allow cells to anchor to the matrix, before the careful addition of media to the 6-well plate. The resulting MSC-matrix constructs were used in further experiments. A pilot experiment comparing different cell densities revealed an optimal cell suspension concentration of 4 × 106 cells/mL, which was used for all experiments.
MSC chondrogenic differentiation
To induce chondrogenesis, MSC constructs were maintained for 35 days in chondrogenic medium and compared to control. Chondrogenic medium consisted of DMEM/F12 + GlutaMAX, supplemented with 2.5% FBS, 40 ng/mL dexamethasone (Applichem), 50 μg/mL ascorbate-2-phosphate (Sigma), 50 μg/mL l-proline (Sigma), 100 U/mL penicillin–100 mg/mL streptomycin, 2.5 ng/mL amphotericin B, 1X insulin (10 μg/mL), transferrin (5.5 μg/mL), selenium (0.67 ng/mL), X supplement (ITS, Gibco), and 10 ng/mL transforming growth factor-β1 (TGF-β1) (Peprotech). Controls were maintained in DMEM/F12 + GlutaMAX, supplemented with penicillin–streptomycin, amphotericin B, FBS and ITS. The media was replaced three times per week.
RNA isolation, cDNA synthesis and real time PCR
Total RNA isolation from MSC constructs was performed at days 7 and 35 and RNA stored at −80°C as follows; constructs were homogenized using a Dispomix device (Axonlab). RNA was isolated from control NP fragments (n = 3; Thompson grading scale II) by hammering of the dry ice frozen samples and further using Aurum Total Mini Kit (Bio Rad), adding 2 μl polyacryl carrier to the lysis buffer and following the manufacturer’s instructions. Five hundred nanograms of total RNA were used for synthesis of cDNA (iScript cDNA Synthesis Kit, BioRad), which was diluted 1:10 with ultrapure water and the resulting cDNA template (5 μl) was mixed with the PCR reaction solution (IQ SYBR Green Supermix, BioRad) containing 0.25 μM specific primers as described in Table 2. Specific products (GAPDH, aggrecan, CD45, CD73, CD90, CD105, collagen type I, collagen type II, FOXF1, Keratin 19, PAX1 and osteopontin) were amplified by a quantitative PCR system (CFX96™ Real Time System, BioRad). qPCR was carried out in triplicates in a final volume of 25 μl in 96-well plates (Bio Rad), with the following settings: denaturation at 95°C for 3 min (1 cycle), at 95°C for 15 s, at 64°C for 20 s and at 72°C for 20 s (40 amplification cycles), followed by a melting curve analysis. The results were normalized to the expression of GAPDH.
Table 2.
Human marker genes used in quantitative RT-PCR
| Gene | Primer nucleotide sequence (5′–3′) | Product size (bp) |
|---|---|---|
| GAPDH | F-TGGACTCCACGACGTACTCA | 102 |
| R-GGAAGCTTGTCATCAATGGAA | ||
| Aggrecan | F-AGGCTATGAGCAGTGTGAACG | 125 |
| R-GCACGCCATAGGTCCTGA | ||
| CD45 | F-CAGTTTCCCCATTGACAACC | 120 |
| R-CAGAGGCATTAAGGTAGGCATC | ||
| CD73 | F-CCAGTCCACTGGAGAGTTCC | 111 |
| R-CGACACTTGGTGCAAAGAAC | ||
| CD90 | F-AGGACGAGGGCACCTACAC | 107 |
| R-GCCCTCACACTTGACCAGTT | ||
| CD105 | F-GCTTGTTGCGCATTTGAA | 95 |
| R-GGCTCGATGGTGTTGGAG | ||
| Collagen type I | F-CCTCCTGGCTCTCCTGGT | 106 |
| R-AGGGAGACCGTTGAGTCCAT | ||
| Collagen Type II | F-GAAGTGCTGGTGCTCGTG | 125 |
| R-GGCCTCTCCTTGCTCACC | ||
| FOXF1 | F-CAGCCTCTCCACGCACTC | 122 |
| R-CCTTTCGGTCACACATGCT | ||
| PAX1 | F-GCAATGACCTTCAAGCATCC | 91 |
| R-GGCAGTCCGTGTAAGCTACTG | ||
| Keratin 19 | F-GCCACTACTACACGACCATCC | 126 |
| R-CAAACTTGGTTCGGAAGTCAT | ||
| Osteopontin | F-GAGGGCTTGGTTGTCAGC | 129 |
| R-CAATTCTCATGGTAGTGAGTTTTCC |
F Forward, R reverse
Immunohistological analysis
Immunohistochemical analysis was used to detect aggrecan, collagen type I and type II accumulations. Constructs were harvested at 35 days of culture in chondrogenic medium, embedded in Neg-50 compound for 30 min, frozen at −80°C and subsequently sectioned at 20 μm using a cryostat (CM 1850, Leica).
Endogenous peroxidase was quenched by 3% H2O2 in PBS at room temperature for 10 min, and washed with PBS. Before incubation with anti-collagen type II antibody, sections were pre-treated for 40 min with 2,500 U/mL hyaluronidase (Sigma-Aldrich) in PBS at 37°C, while sections for immunodetection with anti-aggrecan antibody were pre-treated with chondroitinase ABC (0.25 U/mL, Sigma-Aldrich) in 0.1 M Tris 0.03 M acetate buffer pH 6.5 for 3 h at 37°C. Non-specific background was blocked with PBS containing 1 mg/mL BSA, 10% FBS and 0.1% Triton (Applichem) for 30 min followed by overnight incubation at 4°C with monoclonal mouse antibodies against collagen type I (1:20; M-38, Development Studies Hybridoma Bank), collagen type II (1:20; II-II6B3, Development Studies Hybridoma Bank) and aggrecan (1:10,000; AHP0022, Biosource) in blocking solution. After washing with PBS, sections were incubated with a secondary biotinylated goat anti-mouse antibody (1:200; B0529, Sigma), and then with streptavidin-horseradish peroxidase (1:200; S2438, Sigma) for 45 min at room temperature. Aggrecan, and collagen types I and II were visualized by reaction with 0.075% solution of 3-amino-9-ethylcarbazole (AEC, Applichem) in 0.01% H2O2. Sections were mounted with 70% glycerol (Applichem) and examined by light microscopy.
Histological detection of sulfated glycosaminoglycan (GAG) accumulation was carried out by alcian blue staining. Sections were stained overnight with 0.4% alcian blue (Fluka) dissolved in 0.01% H2SO4 and 0.5 M guanidine hydrochloride (Fluka). Next, sections were washed for 30 min in 40% DMSO and 0.05 M MgCl2. Finally, sections were mounted with 70% glycerol and examined by light microscopy.
Glycosaminoglycans (GAG) accumulation and DNA assays
Proteoglycan accumulation was quantified with alcian blue binding assay after 6 h digestion of three constructs per sample at 60°C with 125 μg/mL papain (Sigma-Aldrich) in 5 mM l-cysteine-HCl (Sigma-Aldrich), 5 mM Na-citrate, 150 mM NaCl, 5 mM EDTA (all AppliChem). GAG accumulation was determined by binding to alcian blue (Fluka), absorption was measured at 595 nm and quantified against chondroitin sulfate (Sigma-Aldrich) reference standards [33].
Total double stranded DNA was measured for each sample after papain digestion, as previously described. The amount of DNA was determined using SYBR green (Invitrogen) fluorescent assay (absorption measured at 535 nm), quantified by referring to calf thymus DNA (Sigma-Aldrich) standards. All test groups were analyzed in triplicates.
Statistical analysis
Data were collected from triplicate samples and expressed as the mean ± SD. Non-parametric Mann–Whitney–Wilcoxon U test for dependent variables was used to compare gene expression, DNA quantification and GAG accumulation, because ANOVA would assume normal distribution of the data, which cannot be guaranteed in this data set. For all tests, p < 0.05 was considered significant. Data analysis was performed with SPSS 14.0 for Windows (SPSS Inc.).
Results
Matrix and cell characterization and cell-construct behavior
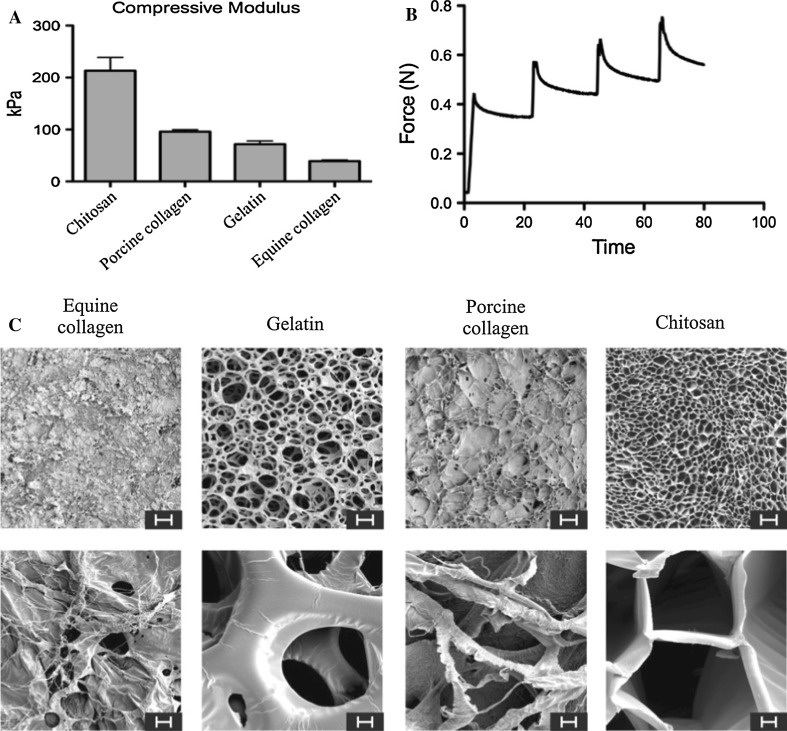
The stiffness of dry scaffolds was tested and represented as average modulus (Fig. 1a). Chitosan was up to twofold stiffer than equine collagen and gelatin. Equine collagen was the softest matrix, with an average modulus 20% that of chitosan. All matrixes possessed the typical response of a viscoelastic material (Fig. 1b): first, an immediate force peak is followed by relaxation; second, the force increment with each displacement step increased as the material was compressed. The chitosan matrix needed to be compressed over 10% before it showed any response and it also possessed the peculiar characteristic to permanently deform easily, although its stiffness was higher than other matrixes. The other matrixes were characterized by a softer structure, but they rebounded elastically when the force was released, although the gelatin was also fragile.
Fig. 1.
Stiffness measurements of dry matrixes (a) and representation of results obtained for chitosan, which possessed the typical response of a viscoelastic material (b) Scanning electron microphotographs of equine collagen, gelatin, porcine collagen and chitosan matrixes (c) (Scale bar is 100 μm in the upper row and 10 μm in the lower row)
Scanning electron micrographs showed different porosity and structure among matrixes (Fig. 1c). Equine and porcine collagen matrixes were characterized by a thick plot of fibers, more densely packed in the equine collagen. On the other hand, gelatin and chitosan presented with more homogeneous and ordered structures where gelatin was to be noted for the largest size of pores. Notably, in the chitosan matrix the pore structure assumed a tubular “honeycomb” shape, whereas in the other matrixes the structures were more reminiscent of a net.
MSCs grown in monolayer displayed the typical fibroblast-like morphology and MSCs phenotype was assessed by positive gene expression of the characteristic antigens CD73, CD90 and CD105 [34], and absence of expression of the leukocyte common marker CD45 (data not shown).
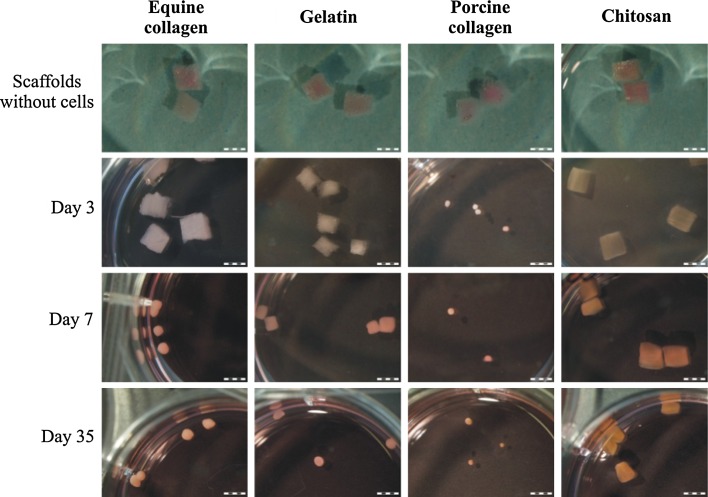
Depending on the time in culture, constructs undergoing chondrogenic differentiation conditions reduced their size compared to the initial size (Fig. 2). Porcine collagen constructs shrank drastically after 3 days, equine collagen constructs after 7 days. Gelatin constructs showed moderate condensation during chondrogenesis, while chitosan constructs remained almost unaltered and size throughout the whole period of differentiation.
Fig. 2.
Images of scaffolds at day 0 and constructs at days 3, 7 and 35 during chondrogenic differentiation. (Entire scale bar is 3 mm)
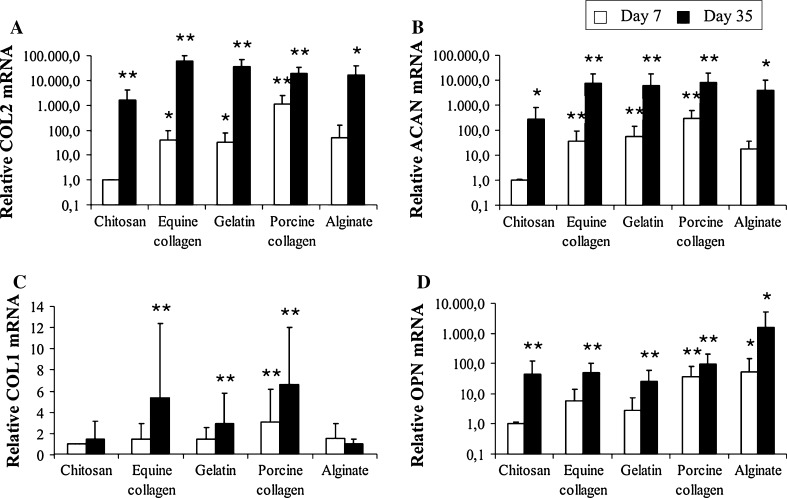
Quantification of gene expression levels of MSCs
To follow MSC differentiation, the gene expression of disc and bone markers were analyzed by real-time PCR on the 7th and 35th days in chondrogenic culture and normalized to the respective gene expression of MSCs in chitosan constructs at day 7 (Fig. 3). After 7 days in culture, porcine collagen constructs already had an up-regulated expression of chondrogenic markers. Compared to chitosan, MSCs seeded in the porcine collagen matrix expressed higher RNA levels of collagen type II (~1,100-fold, p < 0.01), aggrecan (300-fold, p < 0.01) and collagen type I (~threefold p < 0.01). Also compared to chitosan constructs, the osteogenic marker osteopontin was significantly up-regulated in alginate beads (50-fold, p < 0.05) and porcine collagen constructs (37-fold, p < 0.01), but not in equine collagen and gelatin samples. After 35 days in chondrogenic media, MSCs’ expression of collagen type II was significantly higher in MSCs in gelatin (30,000-fold, p < 0.01), equine collagen (60,000-fold, p < 0.01), porcine collagen and alginate beads (18,000-fold, p < 0.05) and chitosan (1,500-fold, p < 0.05) compared to chitosan constructs at day 7 (Fig. 3a). Similar pattern but not level of expression was observed for aggrecan (Fig. 3b). MSCs in gelatin and both collagen matrixes reached approximately ~7,000-fold increase (p < 0.01) compared to ~4,000-fold increase in alginate (p < 0.05), while in chitosan aggrecan gene expression increased only ~250-fold compared to day 7 (p < 0.05). The highest MSC levels of expression of collagen type II and aggrecan were achieved in equine collagen and porcine collagen scaffolds, respectively. Expression of collagen type I was significantly up-regulated in all collagen-derived matrixes by approximately fourfold (p < 0.01); while it remained low in alginate beads and chitosan constructs (Fig. 3c). Gene expression of osteopontin (Fig. 3d) was highest in alginate beads (1,500-fold, p < 0.05), followed by porcine collagen (90-fold, p < 0.01), and equal in chitosan, equine collagen and gelatin constructs (35-fold, p < 0.01).
Fig. 3.
Gene expression of collagen type II (a), aggrecan (b), collagen type I (c) and osteopontin (d) by MSCs in chitosan, equine collagen, gelatin, porcine collagen constructs and alginate beads after 7 and 35 days of chondrogenic culture. Data are normalized to MSCs expression in chitosan constructs at day 7. (Gene expression was normalized to GAPDH, and represented as a mean ± SD, *p < 0.05 and **p < 0.01 compared to MSCs expression in chitosan constructs at day 7)
We also grouped MSCs data by donor’s age, creating two groups––with average age of 25 and 55 years. Gene expression analysis revealed that cells in the older group significantly up-regulated the expression of collagen type I, while collagen type II, aggrecan and osteopontin levels were comparable between the two groups (data not shown).
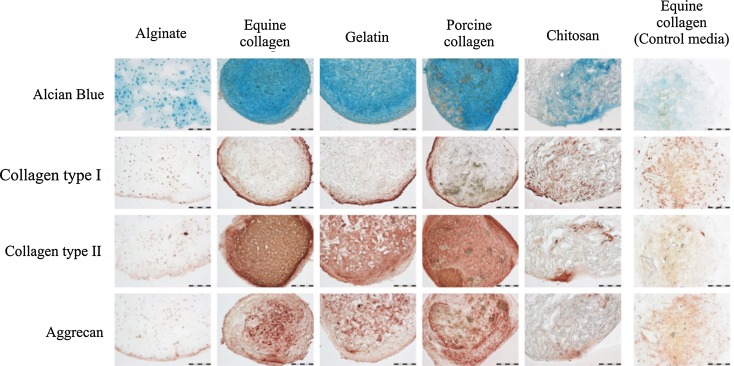
Protein accumulation and localization
Histological and immunohistochemical analysis showed that, depending on the scaffold used, the specific extracellular matrix components which characterize chondrogenic differentiation were produced to different extent (Fig. 4). Alcian blue staining was particularly intensive in collagen and gelatin constructs, indicating extracellular deposition of proteoglycans. Compared to these constructs, staining in alginate beads and in the chitosan matrix was considerably lower. Immunostaining of the alginate constructs showed that collagen type I accumulation was higher compared to collagen type II and aggrecan (almost undetectable). On the contrary, in the collagen and gelatin matrixes, immunostaining demonstrated a specific pattern of protein deposition: collagen type I formed a thin outer layer surrounding the constructs (with oriented collagen fibrils somewhat resembling AF), while the inner part was positive for collagen type II and to lower extent for aggrecan. In comparison, in the chitosan matrix, collagen type I production was also spread across the section, while collagen type II and aggrecan were deposed in much lower amounts.
Fig. 4.
Microphotographs of alginate beads, equine collagen, gelatin, porcine collagen and chitosan sections of constructs stained after 35 days of chondrogenic culture (On the right as a control, sections of equine collagen-construct in control media). The deposition of proteoglycan-rich extracellular matrix was defined by alcian blue staining (upper row). Immunohistochemical analysis of collagen type I (second row), collagen type II (third row) and aggrecan (bottom row), where positive staining is indicated by the presence of red-brown staining. (Entire scale bar is 200 μm)
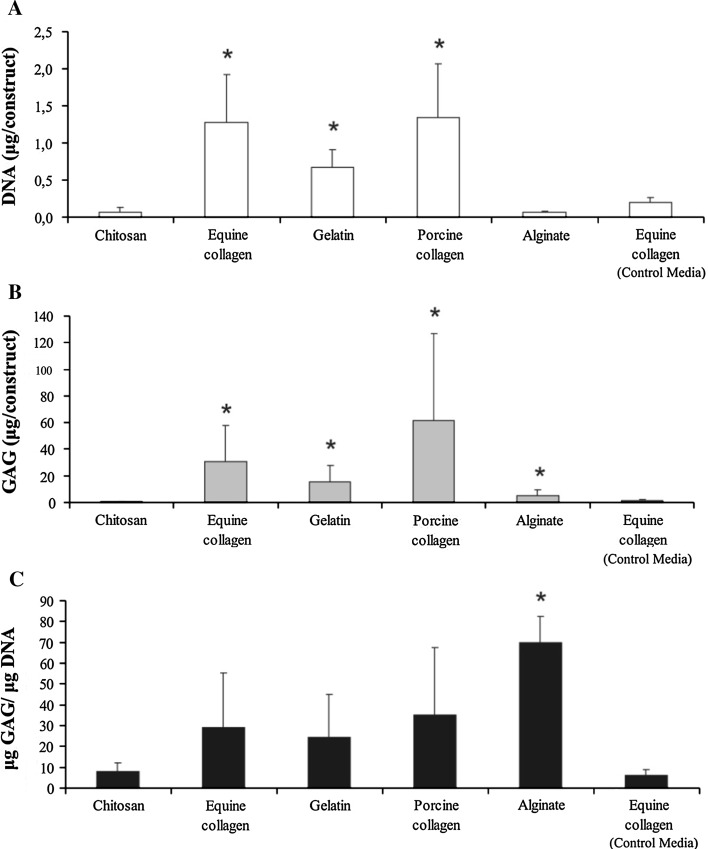
Cell number and GAG accumulation in MSC constructs
To estimate cell number, total dsDNA content was measured for all MSC constructs after 35 days in chondrogenic culture (Fig. 5a). Compared to alginate beads and chitosan, DNA amount was significantly higher in equine and porcine collagen constructs (~20-fold, p < 0.05) and in gelatin constructs (~tenfold, p < 0.05). Non significant DNA increase was measured for equine collagen constructs in control media culture.
Fig. 5.
DNA quantification in alginate beads, equine collagen, gelatin, porcine collagen and chitosan constructs after 35 days of chondrogenic culture, and in control media (equine collagen) (a), GAG accumulation per bead (b), and GAG/DNA ratio in the same samples (c) (Values represent the triplicate mean ± standard deviation; *p < 0.05 compared to chitosan construct values)
After 35 days, different scaffolds showed variable GAG accumulation (Fig. 5b). The overall accumulation of GAG was measured and normalized per construct. GAG showed a significant increase (p < 0.05) in every construct compared to chitosan: porcine collagen 120-fold, equine collagen 60-fold, gelatin 30-fold and alginate beads tenfold. GAG accumulation with control medium in the equine collagen construct remained at the level of the chitosan group. When GAG accumulation was normalized to DNA, the highest ratio between accumulated GAG and total DNA was in alginate beads (Fig. 5c), this ratio being twofold more than in gelatin, equine and porcine collagen constructs, and approximately tenfold more than chitosan constructs (p < 0.05).
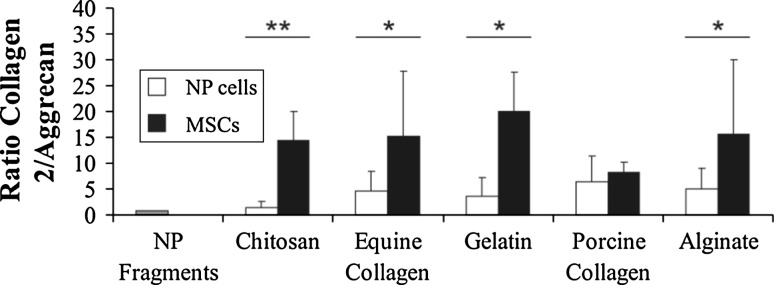
Chondrogenic markers expression ratio in MSC compared to NP cells
To analyze and compare the potential of MSCs to undergo NP-like chondrogenesis in different scaffolds, we calculated the ratio of collagen type II/aggrecan (COL2/ACAN), compared these to NP cells in the respective scaffolds as well as to ex vivo NP tissue fragments (Fig. 6). The COL2/ACAN ratio was significantly higher in alginate, equine collagen, gelatin (p < 0.05) and chitosan (p < 0.01) MSCs construct compared to NP cells, except in the porcine collagen matrix. In this particular scaffold, the ratios were comparable to NP cells because MSCs expressed higher levels of aggrecan compared to MSCs in other supports. NP fragments were characterized by COL2/ACAN gene expression ratio of approximately 1:1.
Fig. 6.
Comparison between gene expression levels of MSCs and NP cells. RNA from NP fragments is represented as reference. Results are reported as ratio of collagen type II to aggrecan RNA expression. (Relative expression normalized to GAPDH, and data are represented as a mean ± SD, *p < 0.05 and **p < 0.01)
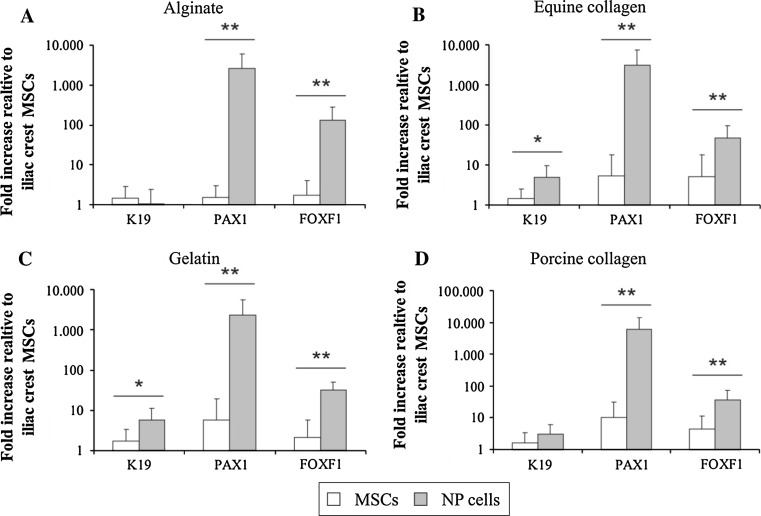
Gene expression of nucleus pulposus markers by differentiated MSCs
To improve the discrimination between cartilage-like and NP-like differentiation of MSCs in different scaffolds after 5 weeks in chondrogenic medium, we tested the expression of genes recently associated with NP phenotype [35, 36], namely KER19, PAX1 and FOXF1 (Fig. 7). Gene expression levels were normalized to MSCs in respective scaffolds and represented as fold increase. Chitosan is not shown because both MSC constructs with this scaffold were not expressing the analyzed genes. Independent of the scaffold used, gene expression levels of PAX1 and FOXF1 were significantly and substantially higher in NP cells when compared to MSCs (p < 0.01). The expression of KRT19 by MSCs and NP cells was not significantly different in alginate, but in contrast the expression of PAX1 and FOXF1 in NP cells was over 1000-fold and approximately 100-fold, respectively higher compared to MSCs expression. The average NP:MSCs expression ratio for PAX1 and FOXF1 of the collagen and gelatin constructs was approximately 550- and 10-fold, respectively. In all scaffolds, but alginate and porcine collagen scaffold, mRNA expression of KRT19 was higher in NP cells compared to MSCs (p < 0.05). Interestingly, in the porcine collagen construct the gene expression of PAX1 and FOXF1 by MSCs was the closest to NP cells, related to the other scaffolds.
Fig. 7.
Gene expression analysis of keratin 19 (KRT19), paired box 1 (PAX1) and forkhead box F1 (FOXF1) by MSCs and NP cells after 35 days of culture. Results are represented for each matrix: alginate (a), equine collagen (b), gelatin (c) and porcine collagen (d) and normalized to MSCs expression. Chitosan data are absent because of lack of expression of these genes. (Relative expression normalized to GAPDH, and data are represented as a mean ± SD, *p < 0.05 and **p < 0.01)
Discussion
In this study, we compared the effects of four different scaffolds to that of alginate for 3D cultures of MSCs derived from bone marrow extracts and differentiated in vitro to generate disc-like cells. Alginate is broadly used in in vitro experiments and provides an easy to control 3D cell culture environment. Previous studies have demonstrated differentiation of MSCs in alginate to NP-like cells [25, 26] but direct comparison with medically approved, although for different applications, materials was not done before. Since a range of these medical devices are made of biological extracellular matrix molecules, we hypothesized that they may support equally to or better than alginate chondrogenic differentiation. Indeed, our results clearly showed that scaffolds are a key component for MSCs undergoing differentiation characteristic for the NP of IVD [2], and we demonstrated that collagen and gelatin are more effective than alginate in enhancing the expression of relevant matrix genes such as collagen types I and II, aggrecan and accumulation of proteoglycans. On the contrary, as a scaffold, chitosan was characterized by a low gene expression and production of extracellular matrix, as well as low cell survival. The data indicates that MSCs can be stimulated by culture conditions to express collagen type II/aggrecan in a ratio similar to that of NP cells cultured in vitro, however gene expression analyses of recently identified NP markers [35], demonstrated that MSCs compared to NP cells express these markers in a different pattern.
The use of 3D cultures for tissue engineering is imperative, because only in such cultures chondrogenic differentiation of MSCs is possible. In vitro pre-differentiation of MSCs, or introduction of cell and scaffold together to the site of the IVD repair, could be a key step for the future implantation of MSCs, because already committed cells would be able to re-build immediately the needed extracellular matrix. Several materials have been studied in the form of hydrogels or porous scaffolds. Alginate gel is one of the most used supports for MSC chondrogenesis, but it was shown that in vivo implantation of the gel without cells was inhibiting the spontaneous repair of the tissue [37] and that cell-alginate constructs can induce in some cases severe immunological responses [38]. Further, alginate is mechanically unstable and therefore inappropriate for implant in vivo [39]. Also synthetic polymers, like poly-glycolic acid (PGA), poly0-L-lactic acid (PLA) and copolymer poly-lactic-co-glycolic acid (PLGA) were shown to promote some inflammation in vivo [40]. On the contrary, collagen is not only a natural molecule but also the main component of the extracellular matrix of IVD. Also natural materials, when not prepared properly, might be unsuitable as supports for in vivo transplantation because of fast degradation rates, possible transmission of pathogens and viruses from the derivation source of the material, and undesired breakdown products [29]. We might be able to overcome some of these problems by using bio-materials already approved for human use, such as wound healing or in surgery, which will have the advantages of being supplied sterile, validated to be non-toxic and biocompatible, thus simplifying lengthy and expensive procedures for translation of research into clinic. All materials used in this study were sponge-like, safe and easy to handle, permitting precise control over size and shape. Scanning electron microscopy imaging showed that the collagen scaffolds used contain highly interconnected pores with a rougher fibrous surface and the gelatin matrix had a smoother structure with more homogeneous pore size and more open space distribution. The chitosan matrix had the most ordered structure with “honeycomb” tubular geometrical, combined with highest stiffness of all tested materials but unfortunately was the most inept of all materials with regard to MSC differentiation into NP-like phenotype.
By the end of 5 weeks, collagen constructs were characterized by a strong shrinkage exerted by the MSCs, as shown by dramatic levels of condensation. The estimated shrinkage was more than a ninefold reduction, to reach only fraction of the initial volume. Collagen matrixes are softer than chitosan and this property allowed MSCs to condense the constructs in a process analogous to the first step of in vivo cartilage development [41]. Possibly, high modulus materials might be a better option for bone development, since bone often develops after a primary cartilage matrix already exists. This hypothesis is confirmed by alginate beads, which in supporting MSC chondrogenesis, performed in between chitosan and soft collagens and gelatin. In alginate beads, cells can communicate with each other within the soft gel, however they cannot pull and condense the whole bead, so histological analysis shows microsites of extracellular matrix deposition, without the additional effect of the condensation and the formation of a more homogenous tissue. Histological and immunohistochemical assays showed the deposition of extracellular matrix characterized by COL1, COL2, and ACAN and alcian blue staining-sulfated proteoglycan. Remarkably, extracellular matrix production from the MSCs was not evenly distributed throughout the collagen constructs. The inner part of the constructs showed accumulation of large amounts of COL2, proteoglycans and ACAN, while the outer perimeter was covered in parallel layers of COL1. These results may suggest that MSCs reacted diversely to different oxygen gradient established across the construct. GAG accumulation per bead was higher in the collagen and gelatin constructs compared to alginate beads, but lower when normalized to DNA. This has to be viewed with caution as the result is caused by the low long-term cell survival which characterizes alginate beads cultures.
In agreement with the histological data, MSCs in collagen constructs expressed higher levels of the IVD and cartilage markers COL1, COL2 and ACAN compared to alginate constructs. In contrast, the undesired bone marker OPN was significantly lower in gelatin and collagen as compared to alginate constructs, confirming lower level, or lack of osteogenesis. Altogether, these results suggest that the deposition of extracellular matrix in collagen constructs was similar to that in NP. In particular, in porcine collagen constructs, MSCs expression ratio for COL2/ACAN was the closest to that of NP cells seeded in the same scaffold. Despite these encouraging results, one of the major limitations we faced was that the MSC gene expression levels of the recently discovered NP markers PAX1 and FOXF1 [35] were approximately 500- and 10-fold lower, respectively, than NP cells seeded in the same supports, therefore far from ideal. Further studies, which will show what are the specific underlying biological functions of these genes in the IVD tissue, will enable better differentiation protocols.
At day 35, the cell number (based on DNA quantity) was significantly higher in gelatin, equine and porcine collagen constructs compared to alginate and chitosan constructs. Some of the performance difference between constructs might be also explained by the uneven number of cells attached to each scaffolds. Low percentage (2.5%) FBS was added to media to improve cell viability, since without it MSCs in the control group would not have survived the duration of the experiment.
Interestingly, when grouping donors by age, it became evident that MSCs chondrogenic potential could not be based only on donor’s age, a potentially important observation for future autologous cell therapies.
In conclusion, after 5 weeks of differentiation, we demonstrated that collagen and gelatin scaffolds are readily available and suitable matrixes for chondrogenic differentiation of MSCs in vitro, in comparison to alginate bead cultures and chitosan constructs. The possibility of use in future clinical IVD applications cannot be excluded and may take fewer resources than some alternative options. However, the expression of recently identified NP markers by MSCs was significantly lower compared to NP cells seeded in the same matrixes, which calls for additional in vitro and in vivo investigations on the biology of MSC differentiation and IVD development.
Acknowledgments
This work was supported by the Swiss Paraplegic Foundation. We thank Mr. Beat Haenni, from the Institute of Anatomy of Bern, for technical assistance with scanning electron microscopy.
Conflict of interest
None.
References
- 1.Richardson SM, Mobasheri A, Freemont AJ, Hoyland JA. Intervertebral disc biology, degeneration and novel tissue engineering and regenerative medicine therapies. Histol Histopathol. 2007;22:1033–1041. doi: 10.14670/HH-22.1033. [DOI] [PubMed] [Google Scholar]
- 2.Sive JI, Baird P, Jeziorsk M, Watkins A, Hoyland JA, Freemont AJ. Expression of chondrocyte markers by cells of normal and degenerate intervertebral discs. Mol Pathol. 2002;55:91–97. doi: 10.1136/mp.55.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mwale F, Roughley P, Antoniou J. Distinction between the extracellular matrix of the nucleus pulposus and hyaline cartilage: a requisite for tissue engineering of intervertebral disc. Eur Cell Mater. 2004;8:58–63. doi: 10.22203/ecm.v008a06. [DOI] [PubMed] [Google Scholar]
- 4.Zhang Y, Sun Z, Liu J, Guo X. Advances in susceptibility genetics of intervertebral degenerative disc disease. Int J Biol Sci. 2008;4:283–290. doi: 10.7150/ijbs.4.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pye SR, Reid DM, Adams JE, Silman AJ, O’Neill TW. Influence of weight, body mass index and lifestyle factors on radiographic features of lumbar disc degeneration. Ann Rheum Dis. 2007;66:426–427. doi: 10.1136/ard.2006.057166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sobajima S, Kim JS, Gilbertson LG, Kang JD. Gene therapy for degenerative disc disease. Gene Ther. 2004;11:390–401. doi: 10.1038/sj.gt.3302200. [DOI] [PubMed] [Google Scholar]
- 7.Sobajima S, Vadala G, Shimer A, Kim JS, Gilbertson LG, Kang JD. Feasibility of a stem cell therapy for intervertebral disc degeneration. Spine J. 2008;8:888–896. doi: 10.1016/j.spinee.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 8.Meisel HJ, Siodla V, Ganey T, Minkus Y, Hutton WC, Alasevic OJ. Clinical experience in cell-based therapeutics: disc chondrocyte transplantation A treatment for degenerated or damaged intervertebral disc. Biomol Eng. 2007;24:5–21. doi: 10.1016/j.bioeng.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Maroudas A, Stockwell RA, Nachemson A, Urban J. Factors involved in the nutrition of the human lumbar intervertebral disc: cellularity and diffusion of glucose in vitro. J Anat. 1975;120:113–130. [PMC free article] [PubMed] [Google Scholar]
- 10.Baksh D, Song L, Tuan RS. Adult mesenchymal stem cells: characterization, differentiation, and application in cell and gene therapy. J Cell Mol Med. 2004;8:301–316. doi: 10.1111/j.1582-4934.2004.tb00320.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Colter DC, Sekiya I, Prockop DJ. Identification of a subpopulation of rapidly self-renewing and multipotential adult stem cells in colonies of human marrow stromal cells. Proc Natl Acad Sci USA. 2001;98:7841–7845. doi: 10.1073/pnas.141221698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jiang Y, Jahagirdar BN, Reinhardt RL, Schwartz RE, Keene CD, Ortiz-Gonzalez XR, Reyes M, Lenvik T, Lund T, Blackstad M, Du J, Aldrich S, Lisberg A, Low WC, Largaespada DA, Verfaillie CM. Pluripotency of mesenchymal stem cells derived from adult marrow. Nature. 2002;418:41–49. doi: 10.1038/nature00870. [DOI] [PubMed] [Google Scholar]
- 13.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 14.Calvert JW, Marra KG, Cook L, Kumta PN, DiMilla PA, Weiss LE. Characterization of osteoblast-like behavior of cultured bone marrow stromal cells on various polymer surfaces. J Biomed Mater Res. 2000;52:279–284. doi: 10.1002/1097-4636(200011)52:2<279::AID-JBM6>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 15.Yoo JU, Barthel TS, Nishimura K, Solchaga L, Caplan AI, Goldberg VM, Johnstone B. The chondrogenic potential of human bone-marrow-derived mesenchymal progenitor cells. J Bone Joint Surg Am. 1998;80:1745–1757. doi: 10.2106/00004623-199812000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Bonab MM, Alimoghaddam K, Talebian F, Ghaffari SH, Ghavamzadeh A, Nikbin B. Aging of mesenchymal stem cell in vitro. BMC Cell Biol. 2006;7:14. doi: 10.1186/1471-2121-7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bogaerdt AJ, Veen VC, Zuijlen PP, Reijnen L, Verkerk M, Bank RA, Middelkoop E, Ulrich MM. Collagen cross-linking by adipose-derived mesenchymal stromal cells and scar-derived mesenchymal cells: Are mesenchymal stromal cells involved in scar formation? Wound Repair Regen. 2009;17:548–558. doi: 10.1111/j.1524-475X.2009.00501.x. [DOI] [PubMed] [Google Scholar]
- 18.Barry F, Boynton RE, Liu B, Murphy JM. Chondrogenic differentiation of mesenchymal stem cells from bone marrow: differentiation-dependent gene expression of matrix components. Exp Cell Res. 2001;268:189–200. doi: 10.1006/excr.2001.5278. [DOI] [PubMed] [Google Scholar]
- 19.Shen B, Wei A, Tao H, Diwan AD, Ma DD. BMP-2 enhances TGF-beta3-mediated chondrogenic differentiation of human bone marrow multipotent mesenchymal stromal cells in alginate bead culture. Tissue Eng Part A. 2009;15:1311–1320. doi: 10.1089/ten.tea.2008.0132. [DOI] [PubMed] [Google Scholar]
- 20.Miljkovic ND, Cooper GM, Marra KG. Chondrogenesis, bone morphogenetic protein-4 and mesenchymal stem cells. Osteoarthritis Cartilage. 2008;16:1121–1130. doi: 10.1016/j.joca.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 21.Cook SD, Patron LP, Salkeld SL, Rueger DC. Repair of articular cartilage defects with osteogenic protein-1 (BMP-7) in dogs. J Bone Joint Surg Am. 2003;85-A(Suppl 3):116–123. doi: 10.2106/00004623-200300003-00018. [DOI] [PubMed] [Google Scholar]
- 22.Feng G, Wan Y, Balian G, Laurencin CT, Li X. Adenovirus-mediated expression of growth and differentiation factor-5 promotes chondrogenesis of adipose stem cells. Growth Factors. 2008;26:132–142. doi: 10.1080/08977190802105917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang CY, Reuben PM, D’Ippolito G, Schiller PC, Cheung HS. Chondrogenesis of human bone marrow-derived mesenchymal stem cells in agarose culture. Anat Rec A Discov Mol Cell Evol Biol. 2004;278:428–436. doi: 10.1002/ar.a.20010. [DOI] [PubMed] [Google Scholar]
- 24.Diduch DR, Jordan LC, Mierisch CM, Balian G. Marrow stromal cells embedded in alginate for repair of osteochondral defects. Arthroscopy. 2000;16:571–577. doi: 10.1053/jars.2000.4827. [DOI] [PubMed] [Google Scholar]
- 25.Ma HL, Hung SC, Lin SY, Chen YL, Lo WH. Chondrogenesis of human mesenchymal stem cells encapsulated in alginate beads. J Biomed Mater Res A. 2003;64:273–281. doi: 10.1002/jbm.a.10370. [DOI] [PubMed] [Google Scholar]
- 26.Gaetani P, Torre ML, Klinger M, Faustini M, Crovato F, Bucco M, Marazzi M, Chlapanidas T, Levi D, Tancioni F, Vigo D, Rodriguez y Baena R. Adipose-derived stem cell therapy for intervertebral disc regeneration: an in vitro reconstructed tissue in alginate capsules. Tissue Eng Part A. 2008;14:1415–1423. doi: 10.1089/ten.tea.2007.0330. [DOI] [PubMed] [Google Scholar]
- 27.Seguin CA, Grynpas MD, Pilliar RM, Waldman SD, Kandel RA. Tissue engineered nucleus pulposus tissue formed on a porous calcium polyphosphate substrate. Spine (Phila Pa 1976) 2004;29:1299–1306. doi: 10.1097/01.BRS.0000127183.43765.AF. [DOI] [PubMed] [Google Scholar]
- 28.Martin I, Shastri VP, Padera RF, Yang J, Mackay AJ, Langer R, Vunjak-Novakovic G, Freed LE. Selective differentiation of mammalian bone marrow stromal cells cultured on three-dimensional polymer foams. J Biomed Mater Res. 2001;55:229–235. doi: 10.1002/1097-4636(200105)55:2<229::AID-JBM1009>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 29.Wang Y, Kim UJ, Blasioli DJ, Kim HJ, Kaplan DL. In vitro cartilage tissue engineering with 3D porous aqueous-derived silk scaffolds and mesenchymal stem cells. Biomaterials. 2005;26:7082–7094. doi: 10.1016/j.biomaterials.2005.05.022. [DOI] [PubMed] [Google Scholar]
- 30.Alini M, Li W, Markovic P, Aebi M, Spiro RC, Roughley PJ. The potential and limitations of a cell-seeded collagen/hyaluronan scaffold to engineer an intervertebral disc-like matrix. Spine (Phila Pa 1976) 2003;28:446–454. doi: 10.1097/01.BRS.0000048672.34459.31. [DOI] [PubMed] [Google Scholar]
- 31.Richardson SM, Hughes N, Hunt JA, Freemont AJ, Hoyland JA. Human mesenchymal stem cell differentiation to NP-like cells in chitosan-glycerophosphate hydrogels. Biomaterials. 2008;29:85–93. doi: 10.1016/j.biomaterials.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 32.Ponticiello MS, Schinagl RM, Kadiyala S, Barry FP. Gelatin-based resorbable sponge as a carrier matrix for human mesenchymal stem cells in cartilage regeneration therapy. J Biomed Mater Res. 2000;52:246–255. doi: 10.1002/1097-4636(200011)52:2<246::AID-JBM2>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 33.Bjornsson S. Simultaneous preparation and quantitation of proteoglycans by precipitation with alcian blue. Anal Biochem. 1993;210:282–291. doi: 10.1006/abio.1993.1197. [DOI] [PubMed] [Google Scholar]
- 34.Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop D, Horwitz E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8:315–317. doi: 10.1080/14653240600855905. [DOI] [PubMed] [Google Scholar]
- 35.Minogue BM, Richardson SM, Zeef LA, Freemont AJ, Hoyland JA. Characterisation of the human nucleus pulposus cell phenotype and evaluation of novel marker gene expression to define adult stem cell differentiation. Arthritis Rheum. 2010;62(12):3695–3705. doi: 10.1002/art.27710. [DOI] [PubMed] [Google Scholar]
- 36.Rutges J, Creemers LB, Dhert W, Milz S, Sakai D, Mochida J, Alini M, Grad S. Variations in gene and protein expression in human nucleus pulposus in comparison with annulus fibrosus and cartilage cells: potential associations with aging and degeneration. Osteoarthritis Cartilage. 2010;18:416–423. doi: 10.1016/j.joca.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 37.Fragonas E, Valente M, Pozzi-Mucelli M, Toffanin R, Rizzo R, Silvestri F, Vittur F. Articular cartilage repair in rabbits by using suspensions of allogenic chondrocytes in alginate. Biomaterials. 2000;21:795–801. doi: 10.1016/S0142-9612(99)00241-0. [DOI] [PubMed] [Google Scholar]
- 38.Hunziker EB. Articular cartilage repair: basic science and clinical progress A review of the current status and prospects. Osteoarthritis Cartilage. 2002;10:432–463. doi: 10.1053/joca.2002.0801. [DOI] [PubMed] [Google Scholar]
- 39.Richardson SM, Hoyland JA. Stem cell regeneration of degenerated intervertebral discs: current status. Curr Pain Headache Rep. 2008;12:83–88. doi: 10.1007/s11916-008-0016-3. [DOI] [PubMed] [Google Scholar]
- 40.Athanasiou KA, Niederauer GG, Agrawal CM. Sterilization, toxicity, biocompatibility and clinical applications of polylactic acid/polyglycolic acid copolymers. Biomaterials. 1996;17:93–102. doi: 10.1016/0142-9612(96)85754-1. [DOI] [PubMed] [Google Scholar]
- 41.Hall BK (1987) Earliest evidence of cartilage and bone development in embryonic life. Clin Orthop Relat Res 255–272 [PubMed]