This study concludes that a modified single-incision procedure for cholecystectomy using 2 regular ports inserted through the umbilicus can be performed at lower cost than a conventional 4-port procedure.
Keywords: Single-incision, Single-site, Cost, Laparoscopic cholecystectomy
Abstract
Background and Objectives:
Specially designed surgical instruments have been developed for single-incision laparoscopic surgery, but high instrument costs may impede the implementation of these procedures. The aim of this study was to compare the cost of operative implements used for elective cholecystectomy performed as conventional laparoscopic 4-port cholecystectomy or as single-incision laparoscopic cholecystectomy.
Methods:
Two consecutive series of patients undergoing single-incision laparoscopic cholecystectomy were assessed: (1) single-incision cholecystectomy using a commercially available multichannel port (n=80) and (2) a modified single-incision cholecystectomy using 2 regular trocars inserted through the umbilicus (n=20) with transabdominal sutures for gallbladder mobilization (puppeteering technique). Patients who underwent conventional 4-port cholecystectomy during the same time period (n=100) were selected as controls.
Results:
The instrumental cost of the single-incision cholecystectomy using a commercial port was significantly higher (median, $1123) than the cost for conventional 4-port (median $441, P < .0005) and modified single-incision cholecystectomy (median $342, P < .0005). The cost of the modified single-incision procedure was significantly lower than that for the 4-port cholecystectomy (P < .0005).
Conclusion:
The modified single-incision procedure using 2 regular ports inserted through the umbilicus can be performed at lower cost than conventional 4-port cholecystectomy.
INTRODUCTION
Single-incision laparoscopic cholecystectomy (SILC) has recently emerged as a less invasive alternative to conventional 4-port laparoscopic cholecystectomy. Despite the fact that SILC defies basic laparoscopic concepts including triangulation and external spacing to limit clashing of instruments,1 numerous series2–6 have described elective SILC as a safe and feasible technique with great patient satisfaction related to the potential of improved cosmesis, because the incision is concealed in the umbilicus. Specially designed equipment has been developed for single-incision procedures including purpose-built optics and disposable instruments, such as ports, roticulating devices, and fixation instruments.7,8 A recognized issue related to these new instruments is cost. The use of single-use instruments generally increases instrumental costs of conventional 4-port laparoscopic cholecystectomy (CLC) using reusable equipment with a factor 6.4,9 and the same may be the case for single-site laparoscopic surgery. Expenses of disposable instruments for CLC are relevant, because they account for approximately 28% and 17% of operative and hospital costs, respectively.10
The aim of this study was to compare the cost of operative instruments used for elective gallbladder removal performed as either a conventional laparoscopic 4-port procedure or a SILC procedure. The analysis was based on our initial experience with SILC. Furthermore, we wanted to assess how the implementation of a modified SILC procedure using conventional laparoscopic ports through the umbilicus and a suture (puppeteering technique) of the infundibulum for exposure of Calot's triangle and the liver–gallbladder interface11,12 impacted instrument costs.
MATERIALS AND METHODS
SILC was introduced at our department in April 2009, and until September 2010 all the operations were registered consecutively in a prospective database including data on patient age, sex, BMI, ASA score, operative time, length of hospitalization, and surgical instruments used. The first 100 SILC procedures were performed by 2 experienced surgeons. During the same time period, CLC was undertaken in 435 patients. From this group, 100 patients were selected according to birth date (year and day of month1–31) to serve as matching controls to the patients who underwent SILC. Data on the control group were obtained from the Danish Cholecystectomy Database13 and the patients’ medical files.
For all 3 different surgical techniques, we used reusable 5-mm laparoscopic graspers and scissors, a single-use dissection hook, and a specimen retrieval bag. Only those instruments that were unique for each of the 3 procedures were considered for the cost calculation. Thus, we only assessed the direct variable instrumental costs specific for the different procedures. The following direct costs were excluded on the assumption that these were similar to the different surgical scenarios in the analysis: professional costs, other surgical services (i.e., drapes, standard reusable surgical instruments, and anesthesia), pharmacy services, radiology and laboratory charges. The instrument cost was calculated by the number of used total units multiplied by the local unit purchasing price that was negotiated between the hospital administration and the manufacturer. Three surgical scenarios were assessed:
CLC (n=100)
The same equipment was used for every procedure (Figure 1). Pneumoperitoneum was established with a Veress needle. Four trocars (2 Versaport Plus 12mm and 2 Versaport 5mm, Covidien) were placed under direct visualization. A smoke filter was used. The cystic artery and duct were closed with clips (Ligaclip 10-M/L, Ethicon).
Figure 1.

Equipment used for the conventional 4-port laparoscopic cholecystectomy.
SILC Procedure Using a Commercially Available Port (n=80)
For umbilical access, we used different commercially available multichannel ports (Table 1). A 2-0 nylon suture mounted on a 60-mm straight cutting needle (Ethilon, Ethicon) was used for transcutaneous retraction of the gallbladder fundus. In 75% of the cases, a disposable instrument was used for mobilization of the gallbladder (Figure 2).
Table 1.
Disposable Instruments Used for Conventional Laparoscopic Cholecystectomy and Single Incision Cholecystectomy (SILC)
| Conventional Laparoscopic Cholecystectomy (n=100) | Single Incision Laparoscopic Cholecystectomy with a Commercially Available Port n=80 (%) | Modified Single Incisionq Laparoscopic Cholecystectomy n=20 (%) | |
|---|---|---|---|
| Veress needle | 100 | 0 | 0 |
| Trocars | |||
| One 12-mm Versaport (Covidien) | 0 | 0 | 20 (100) |
| One 5-mm Versaport (Covidien) | 0 | 12 (15) | 16 (80) |
| Two 12-mm Versaport (Covidien) | 100 | 0 | 0 |
| Two 5-mm Versaport (Covidien) | 100 | 4 (5) | 4 (20) |
| Commercial SILC port | |||
| SILS port (Covidien) | 0 | 73 (91) | 0 |
| LESS triport (Olympus) | 0 | 4 (5) | 0 |
| LESS quadport (Olympus) | 0 | 1 (1) | 0 |
| Air seal (SurgiQuest) | 0 | 1 (1) | 0 |
| Unoport (Ethicon) | 0 | 1 (1) | 0 |
| Fixating instruments | |||
| Roticulator Endo Grasp (Covidien) | 0 | 45 (56) | 0 |
| Endograb (Virtual Ports, Israel) | 0 | 6 (8) | 2 (10) |
| MiniLap (Stryker) | 0 | 9 (11) | 2 (10) |
| Nylon sutures, straight needle | |||
| One Ethilon 2-0 (Ethicon) | 0 | 51 (64) | 5 (25) |
| Two Ethilon 2-0 (Ethicon) | 0 | 18 (23) | 13 (65) |
| Three Ethilon 2-0 (Ethicon) | 0 | 4 (5) | 1 (5) |
| Clip applier | |||
| Ligaclip 10-M/L (Ethicon) | 100 | 0 | 0 |
| Ligamax 5 (Ethicon) | 0 | 80 (100) | 20 (100) |
Figure 2.

Equipment used for single-incision laparoscopic cholecystectomy using a commercially available port and in most cases a disposable instrument for fixation of the gallbladder.
The Modified SILC Procedure (n=20)
We inserted 2 trocars (Versaport Plus 12mm and Versaport system 5mm, Covidien) (Figure 3) through the umbilicus without using a commercially available port and attached a suture to the gallbladder fundus for retraction as described above. The abdominal wall was penetrated with a similar suture caudally to the xiphoid process. The suture was stitched twice through the infundibulum of the gallbladder and brought out close to the right anterior iliac spine. This suture allowed a puppeteering technique for mobilization of the infundibulum from suture traction for visualization of Calot's triangle. Most often, this method obviated the need for a disposable fixation device for this procedure.12
Figure 3.

Equipment used for the modified single-incision laparoscopic cholecystectomy.
For both SILC procedures, we used a 5-mm Endoclip device (Ligamax 5, Ethicon). If retraction of the gallbladder was insufficient, we placed an additional suture for mobilization, used a roticulating grasper (Roticulator Endo Grasp, Covidien), mounted an Endograb fixation device (Virtual Ports, Israel), or used a 2.3-mm combined trocar/grasper instrument (MiniLap, Stryker, MI). A SILC procedure was considered converted if at least 2 additional extraumbilical instruments were placed, but these operations were still considered as SILC in the cost analyses according to an intention-to-treat principle.
The Mann-Whitney and χ2 tests were used for comparisons between groups, and P < .05 was considered statistically significant. Statistical software used was SPSS for Windows version 13.0.
RESULTS
Patients who were selected for SILC did not differ significantly from those undergoing CLC regarding age, sex, and BMI, whereas ASA classification was significantly lower in patients operated on by the SILC technique (Table 2). Operation time was comparable between the groups, but length of hospitalization was significantly shorter for patients operated on by SILC (Table 2).
Table 2.
Patient Demographics and Perioperative Data [Median (Range)]
| Conventional Laparoscopic Cholecystectomy (n=100) | Single Incision Laparoscopic Cholecystectomy (n=100) | P Value | |
|---|---|---|---|
| Patient age, yrs | 49.5 (16–84) | 44.5 (16–85) | .15 |
| Male/female ratio | 34/66 | 22/78 | .06 |
| BMI kg/m2 | 27.6 (19.0–48.5) | 27.1 (18.8–44.3) | .37 |
| ASA classification | |||
| I | 43 | 66 | |
| II | 56 | 32 | .003 |
| III | 1 | 2 | |
| Operative time, min | 80.5 (37–234) | 82.5 (43–192) | .77 |
| Length of hospitalization, hrs | 22.5 (3.6–101.4) | 19.6 (2.6–144.9) | .03 |
The instruments used for each procedure are listed in Table 1. The SILS port (Covidien) was used in 91% of the SILC procedures with commercially available ports, and a roticulating grasper was utilized in half of the cases. In around 20% of both types of SILC procedures, an Endograb or MiniLap fixation device was applied.
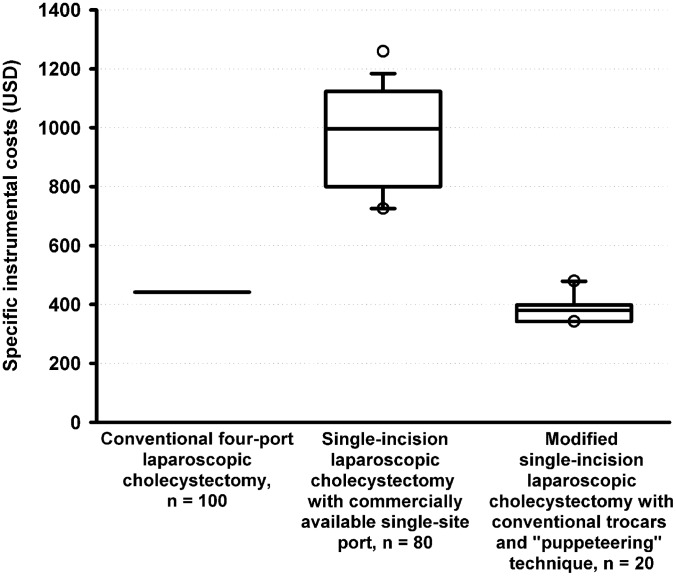
The prices of the instruments are listed in Table 3. The median cost increase of specific procedure-related instruments used for a SILC procedure with a commercially available port compared to CLC was $682. The cost associated with a modified SILC procedure was a median $781 lower than for the SILC procedure with a commercially available port and $99 lower than for the CLC procedure (Figure 4). These price differences were statistically significant (P < .0005).
Table 3.
Costs of Instruments
| Instruments | Price (USD) |
|---|---|
| Veress needle | 8.57 |
| Smoke filter | 17.71 |
| 12-mm Versaport (Covidien) | 70.48 |
| 5-mm Versaport (Covidien) | 56.19 |
| SILS port (Covidien) | 510.10 |
| LESS triport (Olympus) | 571.43 |
| LESS quadport (Olympus) | 730.10 |
| Air seal (SurgiQuest) | 457.14 |
| Unoport (Ethicon) | 761.90 |
| Roticulator Endo Grasp (Covidien) | 402.86 |
| Endograb (Virtual Ports, Israel) | 142.86 |
| MiniLap (Stryker) | 133.33 |
| Nylon suture straight needle Ethilon 2-0 (Ethicon) | 12.89 |
| Ligaclip 10-M/L (Ethicon) | 161.90 |
| Ligamax 5 (Ethicon) | 204.76 |
Figure 4.
Box-Whisker plot of instrumental costs specific for each of the 3 surgical techniques assessed. Horizontal lines, boxes, bars, and circles indicate median, 25 to 75 percentile range, 5 to 95 percentile range and outlier values, respectively. All groups were mutually significantly different: P < .0005.
The placement of 2 extra 5-mm trocars was necessary in 5 of the SILC procedures with the commercially available port, resulting in a 6% conversion rate from SILC to CLC. The median procedure-specific costs for a converted and a nonconverted procedure were $1235 (range, $771 to $1378) and $1123 (range, $726 to $1338), respectively (P = .10). None of the modified SILC surgeries were converted, although the placement of 1 extra 5-mm trocar was necessary in 4 cases.
DISCUSSION
We evaluated the intraoperative cost of elective cholecystectomies in our department. The price of a SILC varied with the kind of instruments used for the procedure. Interestingly, the modified SILC with the use of 2 regular ports and sutures attached to the gallbladder is the procedure with the lowest cost, also lower than the conventional laparoscopic 4-port technique.
Recently, laparoscopic surgery has trended toward increasingly minimally invasive approaches to minimize pain and improve cosmesis. The ultimate benefit over conventional multiport laparoscopic surgery remains to be determined, because of a limited number of available randomized trials.14
The choice of a certain surgical method for a standard procedure depends on several factors, such as operative time, invasiveness, level of difficulty, safety, postoperative complications, patient satisfaction, and cost. A recent study found that the cost of the SILC procedure without the use of a commercially available port did not differ significantly from the cost of CLC.15 In that study, the total price of the operating room and hospital charges was calculated, but the cost of the surgical equipment was not specified separately. Therefore, the cost calculation is not comparable to our cost calculation. However, we agree on the fact that the cost of the modified SILC procedure should not be the factor rendering the technique unsustainable.
There are recent reports on other modalities to reduce costs from the use of commercially available disposable ports and instruments specifically designed for single-site laparoscopic surgery. A homemade port consisting of existing instrumentation and materials (a disposable wound retractor and a surgical glove) was found more cost effective than existing port systems yielding an expense of only approximately $150.16 In a porcine model, single-site laparoscopic procedures were performed using a reusable multiport access device (X-CONE, Karl Storz, Tuttlingen, Germany) and reusable prebent surgical instruments representing a low-cost alternative for single-site laparoscopic surgery.17 In a similar model, needlescopic-assisted laparoscopic surgery using standard laparoscopic instruments through trocars in the umbilicus and a single 2-mm extraumbilical port for a reusable grasper restored triangulation without jeopardizing safety or cosmesis. Instrumental costs were reduced by approximately 79%.18 In a series with 1000 patients, needlescopic laparoscopic cholecystectomy with reusable instruments also was cost reducing and resulted in improved esthetic outcome compared to CLC.19 Moreover, it is a fact that surgeons who conduct single-site procedures also use traditional reusable straight instruments for various surgical procedures and find them feasible and safe.20
The present study was conducted during the early era of SILC procedures in our center for which reason we tested various types of commercially available single-site ports. A review reported that the specially designed ports for single site laparoscopic surgery not only reduce air leakage but are also ergonomically easier to use.8 However, we experienced that a SILC performed by insertion of multiple umbilical ports is a feasible procedure to perform. Another study has hypothesized that there might be an increased risk of incisional hernia formation with the use of 2 or 3 ports instead of one commercially available port in the umbilicus,7 although there are no data in the literature to support this.
Another advantage of the modified SILC procedure without the commercially available port is the possibility of performing the procedure without an assistant. The surgeon can hold the scope in one hand and the instrument in the other hand, while the scrub nurse can provide tension on the gallbladder by retracting the suture, or the suture can be secured by a clamp. Not surprisingly, conversion of SILC to CLC increases total costs.15 We found a similar trend only considering procedure-specific surgical instruments. The few conversions in the present study may have caused a lack of a statistically significant difference due to a type 2 error.
Numerous series have described SILC in select patients as a safe, feasible procedure with good cosmetic results.14,21 However, one recent study22 has compared postoperative pain in patients undergoing SILC and conventional laparoscopic cholecystectomy and found no significant differences. Unfortunately, the patients in that study were neither randomized nor blinded. Randomized controlled trials with relevant end points, such as postoperative pain and complications, are still necessary to evaluate whether SILC is more favorable to the patient than the CLC procedure.
There are some limitations to this study. Patients were not randomized with regard to type of SILC procedure. However, we prospectively registered which surgical instruments we used for every SILC procedure. Moreover, all SILC procedures were conducted by the same 2 experienced surgeons, whereas the conventional laparoscopic procedures were performed by other surgeons in the department, some of whom were low-volume surgeons. Furthermore, the prices of instruments may vary according to local agreements between surgical equipment manufacturers and hospitals. There are trocars on the market with a lower price than the Versaport system, but the implementation of such instruments would hardly alter the conclusion of this study, because fewer trocars would still be applied in the group of patients that underwent the modified SILC procedure. Patients operated on by SILC had a significantly lower ASA classification–a perioperative factor known to be associated with lower hospital costs.23 Furthermore, some manufacturers offer a special price policy for implement kits. The prices used in our calculations were, however, the prices that were actually paid for the equipment.
In the present trial, costs were assessed exclusively considering the equipment differences between the 3 laparoscopic scenarios. Total cost calculations are complex and should include diagnostic workup, reoperations, intensive care, and extended hospitalization due to postoperative complications. It remains to be established from large-scale studies that SILC compared to CLC is not associated with an increased incidence of bile duct injury, port herniation, or wound infection. Moreover, it needs to be determined if SILC may actually reduce epigastric vessel injury, port-site bleeding, and visceral organ injury.24
CONCLUSION
The modified SILC procedure with the use of 2 regular trocars through the umbilicus and sutures attached to the gallbladder is a feasible technique. The modified SILC procedure has a lower cost than both the SILC procedure with a commercially available port and CLC. Therefore, the cost of the SILC procedure should not be the reason to reject the technique. However, large-scale randomized controlled trials are still required to clarify whether SILC is as safe as CLC without increased morbidity.
Acknowledgments
Nadia A. Henriksen and Haytham Al-Tayar have received educational grants from Covidien and Ethicon. Jacob Rosenberg has received grants for research from Covidien and coverage of travel expenses from Ethicon. Lars N. Jorgensen has received consultant fees from Covidien and an educational grant from Olympus.
Contributor Information
Nadia A. Henriksen, Department of Surgery K, Bispebjerg Hospital Copenhagen, Denmark..
Haytham Al-Tayar, Department of Surgery K, Bispebjerg Hospital Copenhagen, Denmark..
Jacob Rosenberg, Department of Gastrointestinal Surgery, Herlev Hospital, University of Copenhagen, Copenhagen, Denmark..
Lars Nannestad Jorgensen, Department of Surgery K, Bispebjerg Hospital Copenhagen, Denmark..
References:
- 1. Canes D, Desai MM, Aron M, et al. Transumbilical single-port surgery: evolution and current status. Eur Urol. 2008; 54: 1020–1029 [DOI] [PubMed] [Google Scholar]
- 2. Edwards C, Bradshaw A, Ahearne P, et al. Single-incision laparoscopic cholecystectomy is feasible: initial experience with 80 cases. Surg Endosc. 2010; 24: 2241–2247 [DOI] [PubMed] [Google Scholar]
- 3. Philipp SR, Miedema BW, Thaler K. Single-incision laparoscopic cholecystectomy using conventional instruments: early experience in comparison with the gold standard. J Am Coll Surg. 2009; 209: 632–637 [DOI] [PubMed] [Google Scholar]
- 4. Ersin S, Firat O, Sozbilen M. Single-incision laparoscopic cholecystectomy: is it more than a challenge? Surg Endosc. 2010; 24: 68–71 [DOI] [PubMed] [Google Scholar]
- 5. Roberts KE, Solomon D, Duffy AJ, Bell RL. Single-incision laparoscopic cholecystectomy: a surgeon's initial experience with 56 consecutive cases and a review of the literature. J Gastrointest Surg. 2010; 14: 506–510 [DOI] [PubMed] [Google Scholar]
- 6. Chow A, Purkayastha S, Aziz O, Paraskeva P. Single-incision laparoscopic surgery for cholecystectomy: an evolving technique. Surg Endosc. 2010; 24: 709–714 [DOI] [PubMed] [Google Scholar]
- 7. Romanelli JR, Earle DB. Single-port laparoscopic surgery: an overview. Surg Endosc. 2009; 23: 1419–1127 [DOI] [PubMed] [Google Scholar]
- 8. Froghi F, Sodergren MH, Darzi A, Paraskeva P. Single-incision laparoscopic surgery (SILS) in general surgery: a review of current practice. Surg Laparosc Endosc Percutan Tech. 2010; 20: 191–204 [DOI] [PubMed] [Google Scholar]
- 9. Slater M, Booth MI, Dehn TC. Cost-effective laparoscopic cholecystectomy. Ann R Coll Surg Engl. 2009; 91: 670–672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Traverso LW, Hargrave K. A prospective cost analysis of laparoscopic cholecystectomy. Am J Surg. 1995; 169: 503–506 [DOI] [PubMed] [Google Scholar]
- 11. Hodgett SE, Hernandez JM, Morton CA, Ross SB, Albrink M, Rosemurgy AS. Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg. 2009; 13: 188–192 [DOI] [PubMed] [Google Scholar]
- 12. Rivas H, Varela E, Scott D. Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc. 2010; 24: 1403–1412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harboe KM, Anthonsen K, Bardram L. Validation of data and indicators in the Danish cholecystectomy database. Int J Qual Health Care. 2009; 21: 160–168 [DOI] [PubMed] [Google Scholar]
- 14. Ahmed K, Wang TT, Patel VM, et al. The role of single-incision laparoscopic surgery in abdominal and pelvic surgery: a systematic review. Surg Endosc. 2011; 25: 378–396 [DOI] [PubMed] [Google Scholar]
- 15. Love KM, Durham CA, Meara MP, Mays AC, Bower CE. Single-incision laparoscopic cholecystectomy: a cost comparison. Surg Endosc. 2011; 25: 1553–1558 [DOI] [PubMed] [Google Scholar]
- 16. Tai HC, Lin CD, Wu CC, Tsai YC, Yang SS. Homemade transumbilical port: an alternative access for laparoendoscopic single-site surgery (LESS). Surg Endosc. 2010; 24: 705–708 [DOI] [PubMed] [Google Scholar]
- 17. Autorino R, Kim FJ, Rane A, et al. Low-cost reusable instrumentation for laparoendoscopic single-site nephrectomy: assessment in a porcine model. J Endourol. 2011; 25: 419–424 [DOI] [PubMed] [Google Scholar]
- 18. Nicolay LI, Bowman RJ, Heldt JP, et al. A prospective randomized comparison of traditional laparoendoscopic single-site surgery with needlescopic-assisted laparoscopic nephrectomy in the porcine model. J Endourol. 2011; 25: 1187–1191 [DOI] [PubMed] [Google Scholar]
- 19. Carvalho GL, Silva FW, Silva JS, et al. Needlescopic clipless cholecystectomy as an efficient, safe, and cost-effective alternative with diminutive scars: the first 1000 cases. Surg Laparosc Endosc Percutan Tech. 2009; 19: 368–372 [DOI] [PubMed] [Google Scholar]
- 20. Branco AW, Kondo W, Stunitz LC, Filho AJ, de George MA. Transumbilical laparoscopic urological surgery: are special devices strictly necessary? BJU Int. 2009; 104: 1136–1142 [DOI] [PubMed] [Google Scholar]
- 21. Antoniou SA, Pointner R, Granderath FA. Single-incision laparoscopic cholecystectomy: a systematic review. Surg Endosc. 2011; 25: 367–377 [DOI] [PubMed] [Google Scholar]
- 22. Prasad A, Mukherjee KA, Kaul S, Kaur M. Postoperative pain after cholecystectomy: Conventional laparoscopy versus single-incision laparoscopic surgery. J Minim Access Surg. 2011; 7: 24–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chung WC, Lee KT, Fan PL, Tzeng DS, Chiu HC. Operating room costs of laparoscopic cholecystectomy: does surgeon volume matter? Kaohsiung J Med Sci. 2006; 22: 126–134 [DOI] [PubMed] [Google Scholar]
- 24. Tugcu V, Ilbey YO, Mutlu B, Tasci AI. Laparoendoscopic single-site surgery versus standard laparoscopic simple nephrectomy: a prospective randomized study. J Endourol. 2010; 24: 1315–1320 [DOI] [PubMed] [Google Scholar]