Abstract
BACKGROUND
In a prior study, we found changing tobacco use was more complex than previously thought, with users often transitioning between intending to quit and not intending to quit, and among typical use, abstinence, and reduction, on multiple occasions. The current study attempted to replicate those results.
METHODS
A convenience sample of 40 tobacco smokers who intended to quit within the next 3 months called in nightly for 28 days to an Interactive Voice Response system to report cigs/day and daily intentions to smoke or not for the next day. We provided no treatment.
RESULTS
Within the month of the study, 32% of smokers had multiple episodes of intentions to not smoke, and 64% transitioned among smoking as usual, abstinence, and reduction status on multiple occasions. When participants reported they intended to not smoke the next day, 56% of the time they did not make a quit attempt the next day. Just under half (44%) of quit attempts occurred on days with no intentions to quit the night before. Most quit attempts (69%) lasted less than a day. Reduction in cigs/day was as common as abstinence.
CONCLUSIONS
Our prospective results replicated retrospective findings that most attempts to stop smoking result in a complex pattern of changes in smoking. These results suggest future research on treatments that can accommodate a) multiple quit attempts over a short period, b) reduction episodes, c) unplanned quit attempts, and d) immediate relapse.
Keywords: smoking cessation, tobacco, relapse, harm reduction
1. INTRODUCTION
Prior studies suggest that when tobacco smokers try to quit on their own, many smokers change their intentions about quitting daily (Hughes et al., 2005), and often rapidly vacillate among short periods of use, reduction and abstinence (Peters and Hughes, 2009). The current study extends these findings by adding information on the incidence of a) quit attempts lasting less than a day, b) aborted quit attempts, and c) reduction specifically associated with a quit attempt. Our major interest was whether, among daily tobacco smokers who intend to quit in the near future, a) most will transition between intentions to quit and no such intentions, and among smoking as usual, reduction or abstinence status, on multiple occasions, b) many daily intentions to quit will not result in abstinence, c) many quit attempts will be unplanned, d) many quit attempts will not last a full day, and e) reduction will be as common as abstinence.
2. METHODS
2.1. Recruitment
Notices on Craigslist (www.craigslist.org), newspaper ads, and internet banner ads invited “daily cigarette smokers who plan to quit”. To enrich the sample to observe smoking changes, smokers had to state they probably or definitely intended to quit in the next 3 months. Also, in order to observe significant reductions in cigs/day, smokers had to smoke ≥ 10 cigs/day.
Among the 309 smokers screened, 269 were ineligible (mostly due to low motivation to quit). Among the 40 participants, the mean age was 40 (sd = 10); most were women (65%) and high school graduates (98%). Most participants were Non-Hispanic Whites (70%) with fewer African Americans (25%), Asians (2%), and Hispanics (2%). Most were neither married (78%), nor employed full-time (62%). They smoked an average of 16.2 cigs/day (5.0), and had a mean Fagerstrom Test for Nicotine Dependence score of 4.4 (2.4; Piper et al., 2006). The sample appeared comparable to the average US daily smoker on age, race, cigs/day and dependence, but were more likely to be women, unmarried and unemployed (Hughes and Callas, 2010a; Piper et al., 2006).
2.2. Interactive Voice Response (IVR)
Participants were instructed to call to an Interactive Response (IVR) system near bedtime. The IVR asked number of cigarettes smoked that day and “Do you think you will smoke cigarettes tomorrow? (Yes/No)”. We used this wording because we believed it would be less reactive than asking about quit attempts every night.
If the IVR detected a day of abstinence, it asked if this was due to a quit attempt. Few (8%) days of abstinence were not due to a quit attempt. To detect quit attempts that may not have lasted a full day, once each week the IVR asked whether participants made a quit attempt that lasted less than a day in the past week. Participants were reimbursed $2/daily for IVR completion plus a $10 bonus if they completed all IVR calls in a week. We provided no treatment. The study was approved by the University of Vermont Committee on the Use of Human Subjects and was registered at www.clinicaltrials.gov (NCT00995644).
2.3. Data Analysis
In analyses, we assumed missed data represented smoking except in the 5% of calls when the missing period was ≤2 days, when we imputed outcomes based on the day prior and the day after the missing days. Also, to prevent counting rapid transitions of abstinence/lapse/abstinence during a quit attempt as two different quit attempts, we required 7 days of consecutive smoking between quit attempts (Hughes et al., 2003).
3. RESULTS
3.1. Individual Data
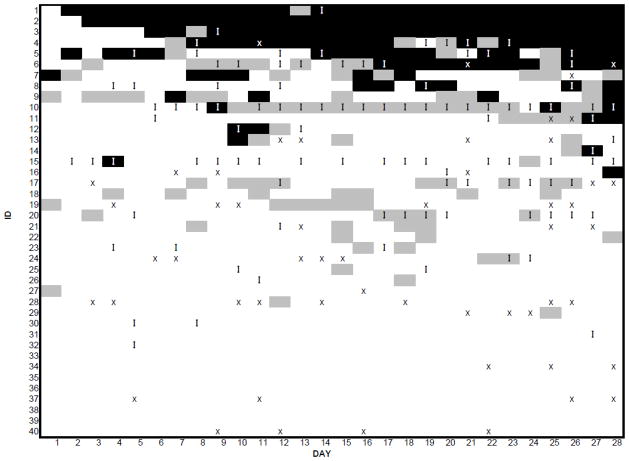
A pixel graph (Figure 1) illustrates transitions for individual participants. This graph examines smoking status only and thus, does not include retrospective reports of quit attempts of less than a day. Three participants (8%; the first three rows of Figure 1) made a quit attempt that resulted in multiple consecutive days of abstinence. In contrast, 10 participants (25%; the bottom 10 rows) never reported either a day of abstinence or reduction. Most smokers (26, 64%) transitioned among smoking as usual, reduction, and abstinence on multiple occasions. For example, Participant 5 smoked near his/her usual cigs/day for 1 day, abstained for 1 day, smoked for 1 day, abstained for 3 days, reduced > 50% for 1 day, smoked for 6 days, abstained for 6 days, reduced for 1 day, smoked for 1 day, abstained for 2 days, smoked for 1 day, reduced for 1 day, and abstained for 3 days.
FIGURE 1.
Outcomes for individual participants (rows) across the 28 days of the study. Black pixels indicate abstinence; grey pixels indicate reduction ≥ 50%, white pixels indicate smoking near their usual cigs/day, and “x” represents missing data. An “I” indicates that, the night before, the participant stated they intended to not smoke on the next day.
3.2. Daily intentions to Quit
During the month, 55% of participants stated they intended to not smoke the next day on one or more days. Among the 104 days in which smokers stated they intended not to smoke the next day, on 56% of these days, participants later stated they did not make a quit attempt on that day.
3.3. Quit Attempts
Fifteen participants (38%) reported 17 quit attempts that were associated with a day of abstinence and 22 participants (55%) reported 37 attempts not associated with a day of abstinence. Combining these two, 30 participants (75%) reported 54 attempts. Overall, there were 140 days of abstinence. Among the attempts associated with abstinence, 8 (44%) were not preceded by an intention to not smoke the next day; i.e., were unplanned. Abstinence was more likely when participants said they would not smoke the night before than when they said they would smoke (Multilevel logistic regression, t = 6.1, p< .001). Very few participants achieved long periods of abstinence: 69% of attempts lasted less than a day, 9% lasted only one day, 7% lasted 2–6 days, and 15% lasted 7+ days.
3.4. Reduction
If reduction is defined as a ≥ 50% decrease in cigs/day (omitting abstinent days) (Hughes and Carpenter, 2005), 27 smokers (68%) had a total of 116 days of smoking reduction. The number of days of reduction is similar to the number of days of abstinence (Goodness-of-fit test x2= 2.25 p=.13). Few reduction episodes were associated with an intention to quit on the prior day (9%; i.e., due to a failed quit attempt), immediately preceded abstinence (11%; i.e., due to gradual cessation), or immediately followed abstinence (23%; i.e., due to a relapse process). Thus, most reduction (58%) was not associated with quit attempts.
3.5. Comparison with Prior Study
Our prior study recruited daily smokers who planned to quit abruptly, quit gradually, reduce but not quit, or not change their smoking over the next one month (Peters and Hughes, 2009). In contrast, the current study was of those who planned to quit in the next three months. Other methods of the two studies were almost identical. We compared the results of the current study with the outcomes from the quit abruptly and quit gradually groups in our prior study. The results were very similar between the two studies (Table 1).
Table 1.
Outcomes in the current study and among the two quitter groups in our prior study (Peters and Hughes, 2009)a
| Outcome | Current Study | Prior Study | |
|---|---|---|---|
| Abrupt | Gradual | ||
| Median number of episodes of abstinence | 0.4 (0.6) | 0.5 (0.6) | 0.2 (0.4) |
| % With at least one episode of abstinence | 38 | 44 | 21 |
| % With at least one episode of reduction | 68 | 67 | 72 |
| % With multiple episodes of abstinence | 5 | 6 | 0 |
| % With multiple episodes of reduction | 38 | 42 | 44 |
| % With ≥7 days of consecutive abstinence | 15 | 16 | 12 |
| % With ≥7 days of consecutive reduction | 2 | 19 | 14 |
| Median (25th–75th percentiles) number of abstinent days | 0 (0–2) | 0 (0–7) | 0 (0–0) |
| Median (25th–75th percentiles) number of reduced days | 1 (0–5) | 3.5 (0–8) | 2 (0–7) |
See text for details of the prior study
4. DISCUSSION
4.1. Summary of Results
We replicated our prior results that a) most tobacco smokers transition between intentions to quit and no such intentions, and among smoking as usual, reduction or abstinence status, on multiple occasions, b) many daily intentions to quit will not result in abstinence on the next day, c) many quit attempts were not preceded by an intention to quit on the prior night, d) many quit attempts will not last a full day, and e) reduction is as common an outcome as abstinence.
4.2. Multiple transitions
Many smoking cessation studies classify smokers as cessation failures when they first lapse and do not follow them thereafter (Hughes et al., 2003). Our results suggest such studies may be missing important information.
4.3. Daily intentions to Quit
Daily intentions to not smoke changed frequently during the study period. These findings are consistent with those of our prior study of weekly changes in intentions (Hughes et al., 2005). In the current study, the majority of intentions to not smoke the next day did not result in a quit attempt. This prospective finding replicates the results observed in two recent retrospective surveys that found many quit attempts are aborted (Berg et al., 2010; Borland et al., 2012).
4.4. Unplanned quit attempts
The current prospective study found that almost half (44%) of quit attempts were “unplanned” according to our definition, i.e., not preceded by an intention to quit the night before; and, thus, replicates the results of retrospective studies that reported 37%–52% of quit attempts are unplanned (Cooper et al., 2010; Ferguson et al., 2009; Larabie, 2005; Sendzik et al., 2011; West and Sohal, 2006).
Our finding that intention on the day before often did not correspond with whether a quit attempt occurred on the next day should not be overinterpreted. We did not have a sufficient sample size nor study duration to test the plausible notion that quitting is a function of an accumulation of intentions to quit over time.
4.5. Quit attempt success
Our prospective finding that 69% of quit attempts lasted less than a day is similar to our prior prospective finding that 67% of quit attempts last less than 2 days (Hughes et al., 1992), but is discordant with three retrospective reports that only 13%–29% of self-quits lasted less than 1–2 days (Gilpin and Pierce, 1994; Marlatt et al., 1988). One possible reason for this discrepancy is that the later two studies asked about quit attempts several months previously and many smokers either forget short quit attempts or do not consider them as true quit attempts (Berg et al., 2010; Borland et al., 2012; Gilpin and Pierce, 1994). Also, our finding that many quit attempts last less than a day supports our prior finding that requiring 24 hours of abstinence to define a quit attempt excludes a large percent of quit attempts (Hughes and Callas, 2010b).
4.6. Reduction of cigs/day
Reduction was as common an outcome as abstinence. Most reduction did not appear to be due to a failed quit attempt, preparation for quitting, nor part of a relapse process.
4.7. Study strengths and limitations
Most reports of quit attempts are based on retrospective recall. Given that reports of recalls or quit attempts are often biased and underestimates (Berg et al., 2010; Gilpin and Pierce,1994; Herzog and Blagg, 2007), our prospectively daily recall of attempts to quit is an important asset. Also, our inclusion of reduction outcomes is a strength not typically found in studies. Other strengths include measures of daily intentions to smoke, inclusion of smokers who were not seeking treatment (most smokers quit without treatment; Shiffman et al., 2008), the low incidence of missing data (5%), and the consistency of results with prior studies.
One limitation was that, in order to observe a modicum of quit attempts, we examined only the subset of smokers who intended to quit in the next 3 months. In comparison, 70% of smokers give serious thought to quitting at least once each year (Klesges et al., 2007). Our study may best be thought of a description of what happens after a smoker decides to attempt to quit in the near future. On the other hand, our study results may not generalize to smokers who currently have low intentions of quitting. Other study limitations include a small convenience sample, the short duration of the study, and the lack of biochemical verification of abstinence.
4.8. Significance
Many tobacco cessation studies label those who lapse or relapse as failures and fail to continue monitoring (Hughes et al., 2003). Our results suggest many lapsed/relapsed smokers continue to try to quit; thus, description of post-relapse outcomes in studies may provide important data to understand the quitting process. Our finding that intentions change on a day-to-day basis suggest more than a single day’s intention may be need to describe motivation to quit. Prior retrospective results indicated that half of quit attempts were unplanned. Our prospective replication that many attempts are unplanned suggests this finding is not due to biased recall. The current study replicated prior work that most relapse in self-quitters occurs in the first few days (Hughes et al., 2004); thus, further research into treatments that can be applied in the first few days after a quit attempt may be fruitful. Our finding that reduction is common suggests future studies should include this outcome to determine whether it predicts interest in future quit attempts or eventual abstinence.
Acknowledgments
Funding
This study was funded by grant 1R01 DA025089 from the US National Institute on Drug Abuse.
We thank Ginger Cloud, Miki Dash, Tonya Ferraro and Beth Walsh for help in conducting the study.
Footnotes
Conflict of Interests
Dr Hughes is currently employed by The University of Vermont and Fletcher Allen Health Care. Since 1/1/2008, he has received research grants from the National Institute on Health and Pfizer; the later develops and sells smoking cessation medications. During this time, he has accepted honoraria or consulting fees from several non-profit and for-profit organizations and companies that develop, sell or promote smoking cessation products or services or educate/advocate about smoking cessation: Alere; American Academy of Addiction Psychiatry; American Psychiatric Association; American Psychiatric Institute for Research and Education; Cambridge Hospital; Dartmouth College; Dartmouth-Hitchcock; DLA Piper; Embera; Embrex; Equinox; European Respiratory Society; Free and Clear; Glaxo-Smith Kline; Golin Harris; Healthwise; Integrated Communication; Maine Health; McGill University Medical School, McNeil Pharmaceuticals; Medical University of South Carolina; Novartis Pharmaceuticals; Ottawa Heart Institute, Pfizer Pharmaceuticals; Propagate Pharmaceuticals; Scientia; Selecta; University of Arkansas for Medical Sciences; University of California-San Francisco; University of Medicine and Dentistry of New Jersey; University of Wisconsin; US National Institutes of Health; Wolters Publishing. No other authors have conflicts.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
John R. Hughes, Departments of Psychiatry, Psychology and Family Practice, University of Vermont, Burlington; VT 05401
Laura J. Solomon, Department of Family Medicine, University of Vermont, Burlington, VT 05401
James R. Fingar, Department of Psychiatry, University of Vermont, Burlington, VT 05401; Shelly Naud, Dept of Medical Biostatistics, University of Vermont, Burlington, VT 05401
John E. Helzer, Department of Psychiatry, University of Vermont, Burlington, VT 05401
Peter W. Callas, Department of Biostatistics, University of Vermont, Burlington, VT 05401
References
- Berg C, An L, Kirch M, Guo H, Thomas J, Patten C, Ahluwalia J, West R. Failure to report attempts to quit smoking. Addict Behav. 2010;35:900–904. doi: 10.1016/j.addbeh.2010.06.009. [DOI] [PubMed] [Google Scholar]
- Borland R, Partos T, Yong H, Cummings K, Hyland A. How much unsuccessful quitting activity is going on among adult smokers? Data from the International Tobacco Control 4-Country cohort survey. Addiction. 2012;107:673–682. doi: 10.1111/j.1360-0443.2011.03685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper J, Borland R, Yong H, McNeill A, Murray R, O’Connor R, Cummings K. To what extent do smokers make spontaneous quit attempts and what are the implications for smoking cessation maintenance? Findings from the International Tobacco Control Four country survey. Nicotine Tob Res. 2010;12:S51–S57. doi: 10.1093/ntr/ntq052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson S, Shiffman S, Gitchell J, Sembower M, West R. Unplanned quit attempts - results from a U.S. sample of smokers and ex-smokers. Nicotine Tob Res. 2009;11:827–832. doi: 10.1093/ntr/ntp072. [DOI] [PubMed] [Google Scholar]
- Gilpin E, Pierce JP. Measuring smoking cessation: problems with recall in the 1990 California Tobacco Survey. Cancer Epidemiol Biomark Prev. 1994;3:613–617. [PubMed] [Google Scholar]
- Herzog T, Blagg C. Are most precontemplators contemplating smoking cessation? Assessing the validity of the Stages of Change. Health Psychol. 2007;26:222–231. doi: 10.1037/0278-6133.26.2.222. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Carpenter MJ. The feasibility of reduced smoking: an update. Addiction. 2005;100:1074–1089. doi: 10.1111/j.1360-0443.2005.01174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99:29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Fagerstrom KO, Callas PW. Intentions to quit smoking change over short periods of time. Addict Behav. 2005;30:653–662. doi: 10.1016/j.addbeh.2004.08.011. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Gulliver SB, Fenwick JW, Valliere WA, Cruser K, Pepper SL, Shea PJ, Solomon LJ, Flynn BS. Smoking cessation among self-quitters. Health Psychol. 1992;11:331–334. doi: 10.1037//0278-6133.11.5.331. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely J, Niaura R, Ossip-Klein D, Richmond R, Swan G. Measures of abstinence from tobacco in clinical trials: issues and recommendations. Nicotine Tob Res. 2003;5:13–25. [PubMed] [Google Scholar]
- Hughes J, Callas P. Data to assess the generalizability of samples from studies of adult smokers. Nicotine Tob Res. 2010a;12:73–76. doi: 10.1093/ntr/ntp168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes J, Callas P. Definition of a quit attempt: a replication test. Nicotine Tob Res. 2010b;12:1176–1179. doi: 10.1093/ntr/ntq165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klesges R, Klesges L, Vander Weg M, DeBon M, Poston W, Ebbert J, Hays J, Haddock C. Characteristics of Air Force personnel who choose pharmacological aids for smoking cessation following an involuntary tobacco ban and tobacco control program. Health Psychol. 2007;26:588–597. doi: 10.1037/0278-6133.26.5.588. [DOI] [PubMed] [Google Scholar]
- Larabie LC. To what extent do smokers plan quit attempts? Tob Control. 2005;14:425–428. doi: 10.1136/tc.2005.013615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Curry S, Gordon JR. A longitudinal analysis of unaided smoking cessation. J Consult Clin Psychol. 1988;56:715–720. doi: 10.1037//0022-006x.56.5.715. [DOI] [PubMed] [Google Scholar]
- Peters E, Hughes J. The day-to-day process of stopping or reducing smoking: a prospective study of self-changers. Nicotine Tob Res. 2009;11:1083–1092. doi: 10.1093/ntr/ntp105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, McCarthy DE, Baker TB. Assessing tobacco dependence: a guide to measure evaluation and selection. Nicotine Tob Res. 2006;8:339–351. doi: 10.1080/14622200600672765. [DOI] [PubMed] [Google Scholar]
- Sendzik T, McDonald P, Brown KHD, Ferrence R. Planned quit attempts among Ontario smokers: impact on abstinence. Addiction. 2011;106:2005–2013. doi: 10.1111/j.1360-0443.2011.03498.x. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Use of smoking- cessation treatments in the United States. Am J Prev Med. 2008;34:102–111. doi: 10.1016/j.amepre.2007.09.033. [DOI] [PubMed] [Google Scholar]
- West R, Sohal T. Catastrophic pathways to smoking cessation: findings from a national survey. Br Med J. 2006;302:458–460. doi: 10.1136/bmj.38723.573866.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]