Abstract
It has been reported that borderline personality related characteristics can be observed in children, and that these characteristics are associated with increased risk for the development of borderline personality disorder. It is not clear whether borderline personality related characteristics in children share etiological features with adult borderline personality disorder. We investigated the etiology of borderline personality related characteristics in a longitudinal cohort study of 1,116 pairs of same-sex twins followed from birth through age 12 years. Borderline personality related characteristics measured at age 12 years were highly heritable, were more common in children who had exhibited poor cognitive function, impulsivity, and more behavioral and emotional problems at age 5 years, and co-occurred with symptoms of conduct disorder, depression, anxiety, and psychosis. Exposure to harsh treatment in the family environment through age 10 years predicted borderline personality related characteristics at age 12 years. This association showed evidence of environmental mediation and was stronger among children with a family history of psychiatric illness, consistent with diathesis–stress models of borderline etiology. Results indicate that borderline personality related characteristics in children share etiological features with borderline personality disorder in adults and suggest that inherited and environmental risk factors make independent and interactive contributions to borderline etiology.
Borderline personality disorder (BPD) is characterized by interpersonal dysfunction, behavioral impulsivity, affective dysregulation, and identity disturbance. It is prevalent in an estimated 1% to 6% of the general adult population (Grant et al., 2008; Lenzenweger, 2008; Torgersen, Kringlen, & Cramer, 2001). Clinically diagnosed BPD is costly economically (Bender et al., 2001; Zanarini, Jacoby, Frankenburg, Reich, & Fitzmaurice, 2009) and entails intense inner pain and self-harming behavior that compromises patients’ mental and physical well-being (Zanarini et al., 2008; Zanarini, Frankenburg, Hennen, Reich, & Silk, 2005). Recent research suggests that effective prevention and early intervention for BPD are possible, but improved means to identify children at risk are needed (Chanen, Jovev, McCutcheon, Jackson, & McGorry, 2008). A growing body of evidence indicates that borderline personality related characteristics (BPRCs) are present in children and that children who exhibit these characteristics are at elevated risk to develop BPD as adults (Bernstein et al., 1993; Bornovalova, Hicks, Iacono, & McGue, 2009; Chabrol, Montovany, Chouicha, Callahan, & Mullet, 2001; Chanen, Jovev, & Jackson, 2007; Crick, Murray-Close, & Woods, 2005; Gratz et al., 2009; Johnson et al., 2000; Lewinsohn, Rohde, Seeley, & Klein, 1997; Macfie & Swan, 2009; Winograd, Cohen, & Chen, 2008). However, diagnosis of BPD for persons younger than age 18 years remains controversial and the clinical and theoretical significance of BPRCs in children is unclear. From a clinical perspective, it is important to know whether children who exhibit BPRCs share risk contexts or clinical features that could provide points of entry for risk assessment and preventative intervention or treatment. From a theoretical perspective, it is important to know how the phenomenon of BPRCs in childhood fits into current understandings of the developmental psychopathology of BPD and whether children who exhibit these characteristics should be a focus for etiological research.
The currently ascendant theories of BPD etiology are diathesis–stress theories that posit interaction between a child’s genetic vulnerability and harsh treatment in the family environment (Crowell, Beauchaine, & Linehan, 2009; Fonagy, Target, & Gergely, 2000; Gunderson & Lyons-Ruth, 2008; Linehan, 1993; Paris, 2005; Zanarini & Frankenburg, 2007). There is evidence that inherited and environmental factors each influence BPD etiology. Studies of psychiatric patients show BPD is familial (Zanarini, Barison, Frankenburg, Reich, & Hudson, 2009) and studies of twin samples show it is heritable (Distel et al., 2008; Kendler et al., 2008; Torgersen et al., 2000, 2008). Correspondingly, retrospective and prospective studies link BPD in adulthood with harsh treatment early in life (Battle et al., 2004; Bradley, Jenei, & Westen, 2005; Carlson, Egeland, & Sroufe, 2009; Crawford, Cohen, Chen, Anglin, & Ehrensaft, 2009; Johnson, Cohen, Chen, Kasen, & Brook, 2006; Reich & Zanarini, 2001; Zanarini et al., 1997). Parallel findings are beginning to emerge from studies of BPRCs in samples of children (Bornovalova et al., 2009; Crawford et al., 2009). Research that extends these findings to test diathesis–stress theories of borderline etiology is needed.
A gap in the scientific literature is research that (a) establishes environmental mediation of the pathway from harsh childhood treatment to BPRCs and (b) directly evaluates the diathesis–stress model of borderline etiology by testing for interaction between inherited risk and harsh treatment. A strong test of the diathesis–stress model requires a prospective longitudinal design with measures of familial liability, measures of harsh treatment during childhood, and measures of early-emerging BPRCs soon thereafter.
In this study, we investigate whether the etiology of BPRCs in children is consistent with the dominant theoretical models of the etiology of BPD in adults. We describe antecedents and comorbidities of BPRCs in a cohort of twin children followed prospectively from age 5 to age 12 years and we test the independent and interactive contributions of inherited and environmental risk factors identified in theoretical models and empirical studies of borderline etiology. First, we describe the heritability, cognitive, behavioral, and affective antecedents, and psychiatric comorbidities of BPRCs to evaluate their correspondence with findings from adult samples. Specifically, we address three questions:
-
Aim 1.1
Are BPRCs in childhood heritable? We exploited the twin design of our sample to estimate the genetic contribution to children’s BPRCs.
-
Aim 1.2
Are BPRCs in childhood preceded by poor cognitive function and behavioral and affective dysregulation earlier in life? We exploited the prospective design of our sample to test relationships between children’s IQ, executive function, theory of mind, temperament, impulsivity, externalizing problems and internalizing problems measured at age 5 years and their BPRCs measured at age 12 years.
-
Aim 1.3
Are BPRCs in childhood accompanied by other psychiatric symptoms? We asked if symptoms of conduct disorder, depression, anxiety, and psychosis were more common among 12-year-olds who exhibited BPRCs.
Second, we test hypotheses that address diathesis–stress interaction in the etiology of BPRCs.
-
Aim 2.1
To test the hypothesis that harsh treatment during childhood contributes to the etiology of BPRCs, we tested associations between a child’s experience of physical maltreatment and maternal negative expressed emotion before age 10 years and his/her BPRCs at age 12 years. We used comparisons of twins within families to rule out the confounding effects of family background factors (e.g., social class) and children’s genotypes.
-
Aim 2.2
To test the hypothesis that an inherited diathesis interacts with harsh treatment during childhood in the etiology of BPRCs, we tested for interaction between a child’s family history of psychiatric disorder and his/her exposure to harsh treatment in a series of models predicting the child’s BPRCs at age 12 years. If the diathesis–stress model of BPD etiology applies to BPRCs in children, those who experience harsh treatment will be especially likely to exhibit BPRCs if they also have a positive family psychiatric history.
Methods
Sample
Participants were members of the Environmental Risk (E-Risk) Longitudinal Twin Study, which tracks the development of a nationally representative birth cohort of 2,232 British children. The sample was selected from a larger birth register of twins born in England and Wales in 1994–1995 (Trouton, Spinath, & Plomin, 2002). Details about the sample have been reported previously (Moffitt & E-Risk Team, 2002). Briefly, the E-Risk sample was constructed in 1999–2000, when 1,116 families with same-sex 5-year-old twins participated in home-visit assessments (93% of eligible families; 54% of twin pairs were monozygotic and 51% were female). Families were recruited to represent the UK population of families with newborns in the 1990s, based on residential location throughout England and Wales and mother’s age (i.e., older mothers having twins via assisted reproduction were underselected and teenaged mothers with twins were overselected). We used this sampling to replace high-risk families who were selectively lost to the register via nonresponse and to ensure sufficient numbers of children growing up in high-risk environments. Follow-ups were conducted when the children were aged 7 years (98% participation), 10 years (96% participation) and, most recently, 12 years (96% participation). Parents gave informed consent and children gave assent. Ethical approval was granted by the Joint South London and Maudsley and the Institute of Psychiatry Research Ethics Committee.
Measures
BPRCs at age 12 years were assessed during interviews with mothers when the children were age 12 years. Mothers responded to questions from a dimensional assessment of BPRCs derived from the Shedler–Westen Assessment Procedure 200-item Q-Sort for Adolescents (SWAP-200-A; Westen, Shedler, Durrett, Glass, & Martens, 2003). Items in the SWAP-200-A borderline assessment were selected from the set of SWAP-200-A items most commonly used by a sample of 294 doctoral-level clinicians to describe adolescent patients meeting DSM-IV diagnostic criteria for adult BPD (Bradley, Zittel Conklin, & Westen, 2005). The items reflect the three core features of adult BPD: affective instability/dysregulation, impulsivity/behavioral dysregulation, and disturbed relatedness/interpersonal dysfunction (Gunderson, 2009; Lieb, Zanarini, Schmahl, Linehan, & Bohus, 2004; Sanislow et al., 2009). We selected items that did not overlap with scales in the Achenbach System of Empirically Based Assessment (Achenbach, 2009) or symptom criteria for other childhood disorders. Table 1 shows the 15 items and their response frequencies. Sex differences were observed in 4 of 15 items.
Table 1.
Caregiver ratings of borderline personality related characteristics scale items for boys and girls
| Statement is “Very True or Often True” of Child
|
pa | N | |||
|---|---|---|---|---|---|
| Boys | Girls | Full Sample | |||
| Easily jealous | 11.1% | 6.9% | 9.0% | .003 | 2,139 |
| Falls for new friends intensely, expects too much too quickly | 5.5% | 5.7% | 5.6% | .808 | 2,139 |
| Changes friends constantly, loves them one day and hates the next | 4.7% | 3.8% | 4.3% | .389 | 2,140 |
| Fears they will be rejected or abandoned | 3.2% | 2.8% | 3.0% | .668 | 2,140 |
| Feels others are out to get him/her | 2.7% | 1.5% | 2.1% | .086 | 2,141 |
| Acts overly seductive or sexy, flirts a lot | 2.6% | 0.9% | 1.7% | .005 | 2,139 |
| Attracted to unsuitable romantic partners | 0.7% | 0.6% | 0.7% | .927 | 2,136 |
| Emotions spiral out of control, has extremes of rage, despair, excitement | 10.5% | 7.7% | 9.1% | .035 | 2,140 |
| Cannot think when upset, becomes irrational | 7.5% | 5.8% | 6.6% | .157 | 2,139 |
| Unable to soothe or comfort self | 4.0% | 3.4% | 3.7% | .471 | 2,141 |
| Lacks stable image of self, changes goals/values | 3.8% | 3.1% | 3.5% | .393 | 2,139 |
| Expresses emotions in an exaggerated dramatic way | 10.8% | 12.2% | 11.5% | .376 | 2,140 |
| Irritable, touchy, or quick to “fly off the handle” | 8.9% | 5.7% | 7.3% | .011 | 2,139 |
| Angry and hostile | 2.2% | 1.3% | 1.7% | .141 | 2,140 |
| Engages in self-harm behavior | 2.9% | 2.9% | 2.9% | .961 | 2,141 |
Note: Items were selected that did not overlap with Achenbach System of Empirically Based Assessment scales or symptom criteria for other childhood disorders. Self-harm was coded as present/absent on the basis of interviews with mothers during home visits. Self-harm was excluded from the scale for the analysis predicting self-harm and was included in the scale in all other anlayses. Differences in response patterns by child sex were evaluated using logistic regression. Standard errors were adjusted to account for nonindependence of twin data.
The value for test of sex difference.
We constructed a dimensional scale of BPRCs by summing positive responses to the 15 questions; internal consistency reliability (Cronbach α) was 0.86. We also generated a dichotomous measure identifying the group of children at the extreme end of the borderline dimension (the extreme borderline group) by identifying children at or above the 95th percentile of the quantitative symptom scale (N = 122, 5.7% of the sample). The 5% (or 2 SD) cutoff is consistent with previous approaches to identifying “clinically significant” borderline pathology using a dimensional measure (Winograd et al., 2008), falls within the range of prevalence estimates reported for clinically significant borderline pathology in adolescents (Bernstein et al., 1993; Chabrol et al., 2001; Lewinsohn et al., 1997), and is consistent with the most recent estimates of the prevalence of BPD in adults in the community (Grant et al., 2008). The dimensional and dichotomous measures were characterized by modest sex differences. Compared to girls, boys exhibited more BPRCs (boys, mean = 4.50, SD = 4.77; girls, mean = 4.00, SD = 4.29; t = 2.09, p = .037) and were more likely to be in the extreme borderline group (6.8% of boys vs. 4.6% of girls, p = .052). Although BPD is thought to be more prevalent in women compared to men, studies of borderline personality in community-based samples of children and adults often find no difference between the sexes (Bernstein et al., 1993; Chabrol et al., 2004; Gratz et al., 2009; Lenzenweger, Lane, Loranger, & Kessler, 2007; Torgersen et al., 2001). Differences in BPRCs between boys and girls in our sample are small, in keeping with this literature.
To establish the incremental predictive validity of our measure of BPRCs, we tested the relationship between children’s BPRCs and their self-harm behavior. Self-harm is especially characteristic of BPD (Skodol, Gunderson, et al., 2002), but is also associated with more general emotional and behavioral problems (Lewinsohn, Rohde, & Seeley, 1993). Our analysis tested whether children’s BPRCs predicted self-harm that was not explained by their emotional and behavioral problems at the same age: we regressed self-harm on BPRCs while statistically controlling for mothers’ Achenbach System of Empirically Based Assessment (Achenbach, 2009) ratings of their children’s internalizing and externalizing problems. For these analyses only, the borderline phenotype was measured without self-harm as part of the scale. Children in the extreme borderline group and those with more BPRCs (excluding self-harm) more often engaged in self-harm, net of risk attributable to their emotional and behavioral problems (odds ratio [OR] = 6.84, 95% confidence interval [CI] = 2.39–19.61, p < .001 for borderline group membership; OR = 1.13, 95% CI = 1.02–1.25, p = .022 for BPRCs). This result supports the validity of our measure of BPRCs.
Children’s cognitive function and behavioral and affective problems at age 5 years were assessed through direct testing of children, mothers’ reports to home visitors, and by teachers’ reports to postal questionnaires. Detailed descriptions of these measures are included in Table 2.
Table 2.
Measures of children’s cognitive function and behavioral and affective problems at age 5 years and comorbid psychiatric problems at age 12 years
| Description | Respondent | Mean (SD) % | N | |
|---|---|---|---|---|
| Cognitive Function at Age 5 Years | ||||
|
| ||||
| IQ | Wechsler Preschool and Primary Scale of Intelligence (WPPSI) Revised. (Wechsler, 1989) Children were administered two subtests: vocabulary and block design. IQ scores were prorated, following procedures described by Sattler (1992). | Child | 100 (15.0) | 2,210 |
| Executive function | Children were administered three executive functions tests: mazes (Grodzinsky & Diamond, 1992) is a WPPSI subtest; day night (Gerstadt et al., 1994) is a nonverbal analogue of the Stroop task; sentence working memory, based on the Baddeley model of working memory (Baddely, 1986: Hughes et al., 2000) requires the child to hold one (or more) item in active working memory while processing necessary information for the generation of the second (etc.,) item. Children’s scores on the three tests were averaged and standardized. | Child | 100 (15.0) | 2,212 |
| Theory of mind | Battery of theory of mind tasks (Hughes et al., 2000, 2005) administered in a set order of increasing difficulty. The test questions tapped children’s ability to attribute a first-order false belief to a story character, to make inferences from an attributed false belief, and to attribute a second-order false belief to a story character. Children’s responses were summed and standardized. | Child | 100 (15.0) | 2,223 |
|
| ||||
| Behavioral and Affective Problems at Age 5 Years | ||||
|
| ||||
| Child temperament Lack of control Approach Inhibition | After the age 5 home visit, examiners rated each child on 25 different behavioral characteristics that assess children’s style of approach and response to the testing session and to the home visit more generally. Each behavioral characteristic was defined in explicit terms and the examiner evaluated whether each characteristic was (0) not at all, (1) somewhat, or (2) definitely characteristic of the child. As described by Caspi et al. (1995), these ratings form three temperament scales: “lack of control” indexes emotional lability, restlessness, short attention span, and negativism; “approach” indexes quick adjustment to new situations, friendliness, self-confidence, and self-reliance; “inhibition” indexes flat affect, passivity, shyness, and fear. | Interviewer | 0 (1) 0 (1) 0 (1) |
2,225 2,224 2,225 |
| Impulsivity | Caregivers and teachers each reported on symptoms of impulsivity from DSM IV attention-deficit/hyperactivity disorder (American Psychiatric Association, 1994). | Mother Teacher |
0 (1) 0 (1) |
2,230 2,084 |
| Externalizing problems | Children’s internalizing and externalizing problems were evaluated by caregivers and teachers using the Achenbach System of Empirically Based Assessment (Achenbach, 2008; Achenbach & Rescorla, 2001). | Mother Teacher Mother |
0 (1) 0 (1) 0 (1) |
2,230 2,089 2,230 |
| Internalizing problems | Teacher | 0 (1) | 2,090 | |
|
| ||||
| Children’s Comorbid Psychiatric Problems at Age 12 Years | ||||
|
| ||||
| Conduct disorder | DSM-IV conduct disorder Items (American Psychiatric Association, 1994) | Child | 0 (1) | 2,120 |
| Depression symptoms | Children’s Depression Inventory (Kovacs, 1992) | Child | 0 (1) | 2,130 |
| Anxiety symptoms | Multidimensional Anxiety Scale for Children (March et al., 1997) | Child | 0 (1) | 2,130 |
| Psychosis symptoms | Psychosis Symptoms Scale (Polanczyk et al., 2010) | Child | 0 (1) | 2,127 |
|
| ||||
| Harsh Treatment | ||||
|
| ||||
| Physical maltreatment | History of physical maltreatment was determined from mother reports in interviews when children were age 5, 7, and 10 years using the reliable standardized clinical protocol from the Multi-Site Child Development Project, a protocol designed to enhance mothers’ comfort with reporting valid child maltreatmen information while also meeting researchers’ legal and ethical responsibilities for reporting (Dodge et al., 1990). Under the UK Children Act our responsibility was to secure intervention if maltreatment was current and ongoing. Such intervention on behalf of E-Risk families was carried out I with parental cooperation in all but one case. Five percent of E-Risk children had a positive history of physical maltreatment. Of this group, 11% were sexually abused by an adult and 89% were physically harmed (including punished by being burned with matches, injured from neglectful or abusive care, formally registered with a child protection team for physical abuse). The abuser was the child’s mother in 21% of cases, another adult family member (biological father, stepfather, grandparents, uncles, adult siblings) in 52% of cases, or an adult nonfamily member (mothers’ boyfriend, neighbor, family friend, baby sitter) in 27% of cases. | Mother | 5% | 2,232 |
| Maternal negative expressed emotion | Maternal negative expressed emotion was assessed using 5-min speech samples eliciting expressed emotion from the mother collected at the age 5 and 10 home visits. Speech samples were audiotaped and audiotapes were coded by two independent blind raters. Scores were averaged across years. Maternal negative expressed emotion (coded on a 0–5 scale) is a global measure of the whole speech sample, indexing negativism expressed in the interview about the child (Caspi et al., 2004). | Mother (coded by trained raters) | 1.46 (0.81) | 2,220 |
Children’s comorbid psychiatric problems at age 12 years were assessed through children’s reports of their own symptoms of conduct disorder, depression, anxiety, and psychosis. Detailed descriptions of these measures are included in Table 2.
Measures of harsh treatment included (a) the child’s history of physical maltreatment through age 10 years obtained in interviews with mothers when children were ages 5, 7, and 10 years and (b) measurements of maternal negative expressed emotion, assessed from speech samples of children’s mothers collected during home visits when children were ages 5 and 10 years. Detailed descriptions of these 2 measures are included in Table 2.
Children’s family histories of psychiatric disorder were ascertained at the age-12 assessment from reports by biological parents following a standardized and valid protocol (Milne, Caspi, Crump, et al., 2009; Milne et al., 2008). Family history of psychiatric disorder (hereafter “positive family history”) was defined as a report of hospitalization for psychiatric disorder or substance-use problem, or attempted or completed suicide for any of the child’s biological mother, father, grandparents, or aunts and uncles. Thirty-one percent of the 2140 children for whom a biological parent reported family information had a positive family history.
Statistical analyses
Descriptive analyses
To describe antecedents and comorbidities of BPRCs in childhood, we began by using biometric modeling in MPlus (Muthén & Muthén, 1998–2009) to test the heritability of children’s BPRCs (Aim 1.1). Next, using regression analyses, we tested whether children with BPRCs at age 12 years differed from comparison children in their cognitive functioning and behavioral and affective problems at age 5 years (Aim 1.2). Finally, using regression analyses, we tested whether children with BPRCs had more co-occurring psychiatric symptoms than comparison children (Aim 1.3).
Testing for association between harsh treatment and BPRCs (Aim 2.1)
We tested whether children’s history of harsh treatment (i.e., physical maltreatment, maternal negative expressed emotion) through age 10 years predicted their BPRCs at age 12 years. Because associations between harsh treatment and BPRCs could be confounded by features of the family environment (e.g., social class, family structure) that caused children to experience harsh treatment and to exhibit BPRCs, we subjected these longitudinal associations to the acid test of a twin-difference analysis. This analysis compared the twins in a family to determine whether the twin who received harsher treatment exhibited more BPRCs relative to his/her age and sex-matched co-twin. Because comparisons were made within families, associations could not be confounded by common causes in the family environment. In a further attempt to rule out confounding that could arise from gene–environment correlations in which the same inherited factor caused parents to treat children harshly and children to develop BPRCs, we repeated the the twin-difference analysis restricting our sample to only the monozygotic (MZ) twin pairs. Because MZ twins share nearly all of their genomes, the MZ twin difference design rules out genetic and family-level confounds.
Testing for interaction between family psychiatric history and harsh treatment in the etiology of BPRCs (Aim 2.2)
We tested whether children’s experiences of harsh treatment placed them at especially increased risk to develop BPRCs if they had a positive family psychiatric history. Analyses that considered the dimensional BPRCs scale score used a linear regression model including main-effect terms for family history and harsh treatment and a product term representing the interaction between these two main effects.
We repeated our twin difference acid test for the interaction analyses. In tests of interaction, the twin difference analysis asks: are differences between twins in harsh treatment stronger predictors of differences between twins in BPRCs if the family has a positive psychiatric history? A twin difference interaction analysis rules out the possibility that a spurious interaction could arise because families with positive psychiatric history differed from those with no psychiatric history in ways that caused parents to treat children harshly and caused children to develop BPRCs. To rule out the possibility that a spurious interaction could arise from skewed distributions of the variables in a model, we replicated analyses using log transformations of continuous measures.
To ensure results were robust to measurement scale, we also tested for interaction predicting the dichotomous outcome of extreme borderline group membership. We defined interaction as the epidemiological construct of biological synergy (Berenbaum, 1989; Rothman, Greenland, & Walker, 1980), in which the effect of two risk factors present together is greater than the sum of their independent effects. We tested diathesis–stress interaction using the 2 × 4 table method to compare relative risks (RR) among children with different combinations of exposures to positive family psychiatric history and exposures to harsh treatment. This method is recommended for investigations of diathesis–stress interaction with dichotomous outcomes (Botto & Khoury, 2001; Schwartz, 2006). In the 2 × 4 table method, interaction was tested as “departure from additivity” (here, if the risk ratio for children with both risk factors was greater than the sum of risk ratios for children with either risk factor independently). We estimated confidence intervals for departures from additivity calculated from the 2 × 4 table by bootstrapping. Because the 2 × 4 table method requires dichotomization of continuous treatment measures, we dichotomized maternal negative expressed emotion at the 80th percentile value (scale score = 2.5). Results were verified using the original (continuous) measure of negative expressed emotion using the BINREG procedure in STATA. BINREG fits a generalized linear model adapted to the binomial family to estimate risk differences and has been used to test interaction in the etiology of categorical psychiatric phenotypes (van Os, Hanssen, Bak, Bijl, & Vollebergh, 2003).
Analyses were conducted using STATA 10.0 (StataCorp, 2009). Twin-difference analyses were implemented using a family-level fixed-effects regression model (Madsen & Osler, 2009). Standard errors were adjusted to account for nonindependence of twin data in models that did not explicitly incorporate the data set’s twin design (Williams, 2000).
Results
Descriptive analyses
Aim 1.1: Are BPRCs in childhood heritable? The correlation between twins on the BPRCs scale was 0.66 among MZ twins and 0.29 among dizotic (DZ) twins. Biometric modeling estimated that genetic factors accounted for 66% (95% CI = 62%–70%) of the variance in BPRCs. The probandwise concordance rate (McGue, 1992) for extreme borderline group membership, that is, the probability that a twin would be in the extreme group conditional on their co-twin being in that group, was 52% for MZ twins and 7% for DZ twins. The greater concordance rate for MZ compared to DZ twin pairs indicates that genetic factors contributed to twins’ BPRCs.
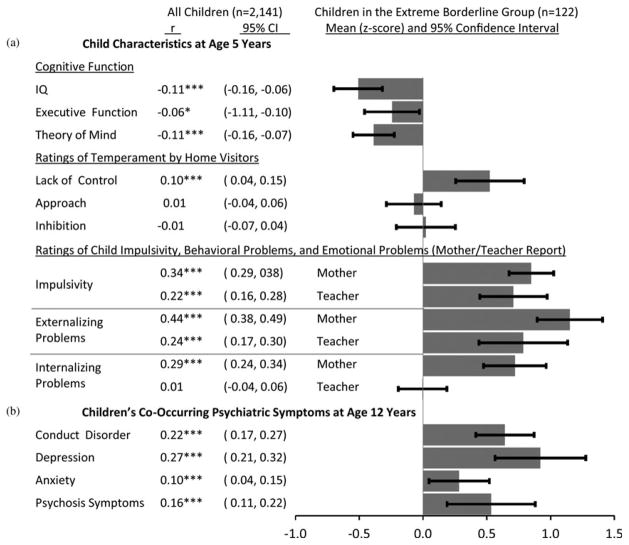
Aim 1.2: Are BPRCs in childhood preceded by poor cognitive function and behavioral and affective dysregulation earlier in life? Consistent with research showing impaired cognitive function, heightened impulsivity, and behavioral and affective dysregulation among adults meeting diagnostic criteria for BPD (Grant et al., 2008; Judd, 2005), children in the extreme borderline group and who exhibited more BPRCs at age 12 years had lower IQs and less well developed theory of mind, lacked self-control, and had high levels of impulsivity and externalizing and internalizing problems at age 5 years (Figure 1a).
Figure 1.
Psychiatric antecedents and comorbidities of borderline personality related characteristics in 12-year-old children: correlations with the Dimensional Borderline Scale and deviations from sample means (z scores) for children in the extreme borderline group. (Left) Correlations were estimated as standardized coefficients from regressions of the continuous scales measuring psychiatric antecedents and comorbidities on the dimensional measure of borderline personality related characteristics. *p <.05, ***p <.001. (Right) The graphs depict means (z scores) and 95% confidence intervals for the psychiatric antecedents and comorbidities among children in the extreme borderline group. The sample mean is represented by zero. The y axis measures standard deviations from the mean. All estimates were adjusted for the nonindependence of twin data.
Aim 1.3: Are BPRCs in childhood accompanied by other psychiatric symptoms? Children in the extreme borderline group and who exhibited more BPRCs at age 12 years reported more symptoms of other psychiatric problems, particularly depression, but also conduct disorder, psychosis, and anxiety (Figure 1b).
Hypothesis tests
Aim 2.1: Harsh treatment during childhood contributes to the etiology of BPRCs. Children’s exposure to harsh treatment before age 10 years predicted their BPRCs at age 12 years. Parallel findings were observed for both measures of harsh treatment: physical maltreatment and maternal negative expressed emotion (Table 3).
Table 3.
Tests of children’s harsh treatment prior to age 10 years and family history of psychiatric disorder as risk factors for borderline personality related characteristics at age 12 years
| Borderline Personality Related Characteristics Scale Score
|
Extreme-Borderline Group Membership
|
||||||
|---|---|---|---|---|---|---|---|
| r | p | 95% CI | Discordant Twin Pairs | OR | p | 95% CI | |
| Children’s Harsh Treatment | |||||||
|
| |||||||
| Physical maltreatment | .20 | .000 | (0.12, 0.28) | 7.22 | .000 | (4.13, 12.63) | |
| Twin-difference design | .06 | .023 | (0.00, 0.12) | 32 | — | — | — |
| MZ-twin difference design | .07 | .063 | (−0.02, 0.16) | 9 | — | — | — |
| Maternal negative expressed emotion | .39 | .000 | (0.34, 0.44) | 3.25 | .000 | (2.60, 4.07) | |
| Twin-difference design | .31 | .000 | (0.26, 0.37) | 825 | — | — | — |
| MZ-twin difference design | .22 | .000 | (0.15, 0.29) | 425 | — | — | — |
|
| |||||||
| Children’s Family History of Psychiatric Disorder | |||||||
|
| |||||||
| Family history | .17 | .000 | (0.12, 0.23) | 3.47 | .000 | (2.27, 5.29) | |
Note: Odds ratios (OR) were estimated with logistic regression models. Effect size correlations (Pearson r) were estimated as standardized regression coefficients from ordinary least squares and, in the case of twin-difference analyses, fixed effects regression models. Twin difference analyses could not be conducted for extreme borderline group membership because most twins were in the same group on that outcome. Standard errors in logistic and ordinary least squares regression models were adjusted for nonindependence of twin data. CI, confidence interval; MZ, monozygotic.
Children with a history of physical maltreatment exhibited more BPRCs (r = .20, p < .001). This association remained statistically significant in a twin difference design, which controlled for unmeasured family-level confounds. Compared to his/her nonmaltreated co-twin, the maltreated twin exhibited more BPRCs, although the effect size was small (r = .06, p = .023). A similar effect size was observed using an MZ twin difference design, which controlled genetic and family-level confounds, although too few twin pairs were discordant for maltreatment for the effect to reach statistical significance (r = .07, p = .063). Children with a history of physical maltreatment were also more likely to be in the extreme borderline group (OR = 7.22, 95% CI = 1.13, 12.63). Twin difference analyses could not be conducted for extreme borderline group membership because most co-twins were in the same group on that outcome.
Children exposed to greater maternal negative expressed emotion exhibited more BPRCs (r = .39, p < .001). This association remained statistically significant in twin difference and MZ twin difference analyses (r = .31 and r = .22, respectively, p < .001 for both tests). Children exposed to greater maternal negative expressed emotion were also more likely to be in the extreme borderline group (OR = 3.25, 95% CI = 2.60, 4.07).
Aim 2.2: Family history interacts with harsh treatment in the etiology of BPRCs. Family history of psychiatric disorder constituted a significant diathesis for the development of BPRCs; children with positive family histories exhibited more BPRCs (r = .17, p < .001) and were more likely to be in the extreme borderline group (OR = 3.47, 95% CI = 2.27, 5.29; Table 3). Family history can establish familiality, but it cannot distinguish the source of this effect, that is, whether it is genetic or environmental. Modified Sobel–Goodman tests of mediation (Preacher & Hayes, 2008) estimated that physical maltreatment mediated 9% of the family history–BPRCs association, maternal negative expressed emotion mediated 16% of the family history–BPRCs association. This suggests that family psychiatric history communicates risk for BPRCs even in the absence of harsh treatment.
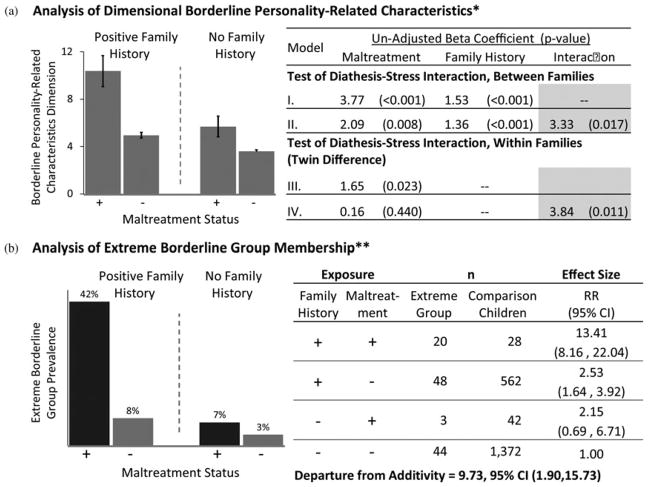
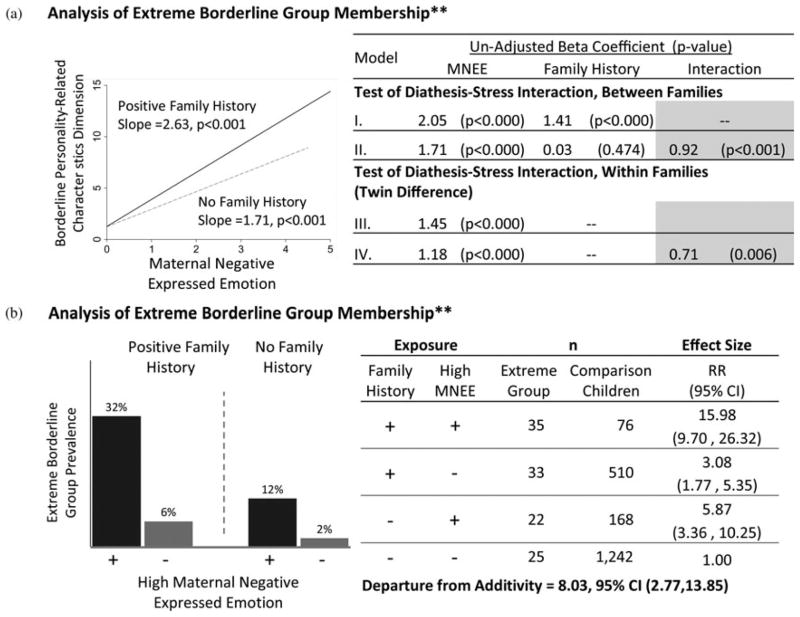
We observed evidence of diathesis–stress interaction in borderline etiology between family psychiatric history and harsh treatment. Children who experienced harsh treatment were at greater risk of developing BPRCs if they had a positive family psychiatric history. Parallel findings were observed for physical maltreatment (Figure 2) and for maternal negative expressed emotion (Figure 3). Findings were consistent across analyses of dimensional BPRCs (Figures 2a and 3a) and dichotomous extreme borderline group membership (Figures 2b and 3b), as described next.
Figure 2.
Diathesis–stress interaction between family history of psychiatric disorder and physical maltreatment. The figure shows (a) the diathesis–stress interaction in the analyses of the dimensional outcome of borderline personality related characteristics and (b) the dichotomous outcome of extreme borderline group. The convergence between these analyses indicates the interaction is not an artifact of measurement scale. (a) *Error bars in the graph represent standard errors of means, adjusted for nonindependence of twin data. Model I is an ordinary least-squares regression of borderline personality related characteristics on physical maltreatment and family history. Model II adds an interaction between family history and maltreatment. Model III is a twin-difference analysis. A family history coefficient cannot be estimated in a twin-difference analysis, which controls for this and all other family-level factors, child sex, and child age. Model IV is a twin difference analysis including the interaction between family history and maltreatment. The interaction term from this model indexes the degree to which a difference between twins in maltreatment status is a stronger predictor of the difference between those twins in borderline symptoms in families with positive psychiatric history. Standard errors in models I and II were adjusted to account for nonindependence of twin data. Twelve of the 32 twin pairs discordant for maltreatment had positive family history of psychiatric disorder. (b) The analysis of the extreme borderline group membership. (** ++) Children with both risk factors, (+ −) children with positive family history only, (− +) children with maltreatment only, (− −) children with neither risk factor; risk ratios calculated relative to children with neither risk factor. Departure from additivity = relative risk (RR)[++ ] − (RR[+ −] + RR[− +] − 1). Ninety-five percent confidence intervals were adjusted for nonindependence of twin data. Confidence interval for departure from additivity estimated from 1000 bootstrap repetitions.
Figure 3.
Diathesis–stress interaction between family history of psychiatric disorder and maternal negative expressed emotion. The figure shows (a) the diathesis–stress interaction in analyses of the dimensional outcome of borderline personality related characteristics and (b) the dichotomous outcome of extreme borderline group. The convergence between these analyses indicates the interaction is not an artifact of measurement scale. (a) *Slopes reflect coefficients estimated from ordinary least-squares regression. Model I is an ordinary least-squares regression of borderline personality related characteristics on maternal negative expressed emotion and family history. Model II adds an interaction between family history and maternal negative expressed emotion to the model. Model III is a twin difference analysis. A family history coefficient cannot be estimated in a twin-difference analysis, which controls for this and all other family-level factors, child sex, and child age. Model IV is a twin difference analysis including the interaction between family history and maternal negative expressed emotion. The interaction term from this model indexes the degree to which a difference between twins in maternal negative expressed emotion is a stronger predictor of the difference between those twins in borderline symptoms in families with positive psychiatric history. Standard errors in Models I and II were adjusted to account for nonindependence of twin data. A total of 252 of 825 twin pairs discordant for maternal negative expressed emotion had positive family history of psychiatric disorder. (b) (** ++ ) Children with both risk factors, (+ −) children with positive family history only, (− +) children exposed to high negative expressed emotion only, (− −) children with neither risk factor; risk ratios calculated relative to children with neither risk factor. Departure from additivity = relative risk (RR)[++ ] − (RR[+ −] + RR[− +] − 1). Ninety-five percent confidence intervals were adjusted for nonindependence of twin data. The confidence interval for the departure from additivity was estimated from 100 bootstrap repetitions.
Figure 2 depicts diathesis–stress interaction between family history and physical maltreatment. Figure 2a presents analyses of the dimensional BPRCs. The left side of Figure 2a shows mean BPRCs scale scores as a function of maltreatment among children with positive family history and among children with no family history. The right side of Figure 2a presents results of regression analyses of diathesis–stress interaction. We observed a significant interaction between family history and maltreatment ( p = .017, Model II). We replicated this analysis using a twin difference design. The twin who was maltreated exhibited more BPRCs relative to their age- and sex-matched co-twin, and this sibling difference was wider in families with a positive psychiatric history ( p = .011, Model IV). We obtained comparable results when these models were tested using a log-transformation of the BPRC scale score as the dependent variable (not shown). Figure 2b presents analyses of the dichotomous outcome of extreme borderline group membership. The left side of Figure 2b shows extreme borderline group prevalence as a function of maltreatment among children with positive family history and among children with no family history. The right side of Figure 2b shows the 2 × 4 analysis of diathesis–stress interaction. This analysis presents the number of extreme borderline group and comparison children in four groups of children defined by family history (positive/negative) and physical maltreatment (positive/negative). Children with both risk factors were 13.41 (95% CI = 8.61, 22.04) times more likely to be in the extreme borderline group than were children with neither risk factor. In contrast, children with only positive family history were only 2.53 (95% CI = 1.64, 3.92) times more likely and children with only maltreatment were only 2.15 (95% CI = 0.69, 6.71) times more likely to be in the extreme borderline group relative to children with neither risk factor. Analysis of diathesis–stress interaction showed a significant departure from additivity of 9.73 (95% CI = 1.90, 15.73), indicating that there is a significant interaction between diathesis and stress. We obtained comparable results from a test of interaction using the BINREG procedure in STATA (not shown).
Figure 3 depicts diathesis–stress interaction between family history and maternal negative expressed emotion. Figure 3a presents analyses of the dimensional BPRCs. The left side of Figure 3a shows a graph of predicted slopes for BPRCs as a function of negative expressed emotion among children with positive family history and among children with no family history. The right side of Figure 3a presents regression analyses of diathesis-stress interaction. We observed a significant interaction between family history and negative expressed emotion ( p = .001, Model II). This finding was replicated in the twin difference analysis ( p = .006, Model IV). We obtained comparable results when these models were tested using a log-transformation of the BPRCs scale score as the dependent variable and when our measure of maternal negative expressed emotion was also log-transformed (not shown). Figure 3b shows analyses of the dichotomous outcome of extreme borderline group membership. The 2×4 analysis of diathesis–stress interaction in Figure 3b shows a significant departure from additivity of 8.03 (95% CI = 2.77, 13.85), indicating a significant interaction between diathesis and stress. We obtained comparable results from a test of interaction using the BINREG procedure in STATA (not shown).
Discussion
We investigated the etiology of BPRCs in a birth cohort of twins ascertained from the general population and studied from age 5 to 12 years. Results are consistent with previous prospective studies of adult BPD and support previously untested theoretical models of diathesis–stress interaction in borderline etiology. Our clinical description of BPRCs overlaps with characterizations of childhood BPD by earlier theorists (Bemporad, Smith, Hanson, & Cicchetti, 1982), including heterogeneous cognitive deficits, intermittent losses of reality testing, poor functioning in response to stress, inability to contain or manage anxiety, and episodic behavioral dyscontrol. Our clinical description of BPRCs is also consistent with findings from previous empirical studies of BPRCs in children (Carlson et al., 2009; Chanen et al., 2007; Crick et al., 2005).
BPRCs at age 12 years were heritable within the range of estimates reported for adult BPD (Distel et al., 2008; Torgersen et al., 2000) and were preceded by poor cognitive function and behavioral and affective dysregulation at age 5 years. This profile is consistent with findings from retrospective studies of adults with BPD (Grant et al., 2008; Judd, 2005), studies of BPRCs in adolescent clinical and community samples (Chanen et al., 2007; Crick et al., 2005; Gratz et al., 2009; Paris, Zelkowitz, Guzder, Joseph, & Feldman, 1999), and prospective studies that include observations of children’s psychological functioning and their borderline outcomes in adulthood (Bornovalova et al., 2009; Carlson et al., 2009; Crawford et al., 2009). Consistent also with etiological research on child and adult borderline personality (Battle et al., 2004; Carlson et al., 2009; Crawford et al., 2009; Guzder, Paris, Zelkowitz, & Feldman, 1999; Guzder, Paris, Zelkowitz, & Marchessault, 1996; Johnson et al., 2006; Zanarini, 2000), children in our study who were exposed to harsh treatment earlier in life exhibited more BPRCs at age 12 years. This finding survived our “acid-test” of twin difference and MZ twin difference analyses, indicating that the association was specific to children’s personal experiences of harsh treatment (i.e., not attributable to features of their families that were shared with their co-twins) and was environmentally mediated (i.e., not attributable to gene–environment correlation): children who were physically maltreated or exposed to greater maternal negative expressed emotion developed more BPRCs compared to peers, co-twins, and genetically identical co-twins who were treated less harshly. Moreover, children were especially vulnerable to developing BPRCs following experiences of harsh treatment if they carried a positive family history of psychiatric disorder. In analyses of dimensional and dichotomous measures of BPRCs and using comparisons of peers and of co-twins, risk from a history of physical maltreatment and from exposure to maternal negative expressed emotion was greater for children with positive family psychiatric history. Consistent with diathesis–stress theories of borderline etiology (Crowell et al., 2005; Fonagy et al., 2000; Gunderson & Lyons-Ruth, 2008; Linehan, 1993; Paris, 2005; Zanarini & Frankenburg, 2007), inherited liability and harsh treatment both contributed to BPRCs, and each acted as a more virulent risk factor in the presence of the other.
Our findings have implications for theory, research, and clinical practice, and provide support for developmental theories of borderline etiology (Crowell et al., 2005; Fonagy & Bateman, 2008; Gunderson & Lyons-Ruth, 2008). With respect to theory, two interesting findings emerge. First, consistent with the assumption of an attachment-specific dysfunction in BPD, BPRCs were associated with physical maltreatment as well as maternal negative expressed emotion. Other prospective longitudinal studies (Carlson et al., 2009; Crawford et al., 2009; Johnson et al., 2006) have also reported that both maltreatment and maternal negativity directed at the child are potent predictors of borderline symptomatology. A unique contribution of our study is that we were able to demonstrate environmental mediation of this pathway. Second, the effects of harsh treatment were most potent in children with a family history of psychiatric disorder. Family history of psychiatric disorder may be an indicator of a vulnerability for more intense emotional response to parental malevolence leading to an increased likelihood of disrupting the neurobehavioral system subserving attachment (Coan, 2008; Fox & Hane, 2008) also implicated in borderline etiology (Gunderson & Lyons-Ruth, 2008; Stanley & Siever, 2010). A full understanding of the nature of the interaction between familial vulnerability and childhood adversity will require research to disentangle relationships among the multiple biological systems (Siever & Davis, 1991; Siever, Torgersen, Gunderson, Livesley, & Kendler, 2002; Skodol, Siever, et al., 2002; Stanley & Siever, 2010) and multiple genes (Joyce et al., 2006; Lyons-Ruth et al., 2007; Nemoda et al., 2005, 2010) implicated in borderline etiology. More generally, future etiological research on BPRCs in children should proceed within a diathesis–stress framework. Studies of risk and protective environments may benefit from considering populations with positive family psychiatric history, which can serve as a proxy measure of diathesis. Studies seeking to identify genes for borderline personality may increase their power to detect genotype–phenotype associations by considering samples with positive family histories of psychiatric disorder or with histories of harsh childhood treatment. In the first case, risk genotypes may be more common in samples with positive family psychiatric history. In the second case, the associations between risk genotypes and borderline phenotypes may be larger in magnitude in populations with a history of harsh treatment (Caspi, Hariri, Holmes, Uher, & Moffitt, 2010).
Our findings also have implications for prevention. At the level of psychological processes, the diathesis–stress model underscores the importance of early family-based interventions in preventing the progression from childhood BPRCs to adult BPD. Prevention and treatment should be person centered, with interventions aiming to ensure that the family resumes its role in facilitating the child’s self-regulation. Such evidence-based intervention protocols are available for infancy (Donelan-McCall, Eckenrode, & Olds, 2009; Olds, Sadler, & Kitzman, 2007) and preschool (Campbell, Pungello, Miller-Johnson, Burchinal, & Ramey, 2001; Gottlieb & Blair, 2004). Prioritizing children with positive family history may help target prevention.
Diagnostic assessment tools and treatments derived from diathesis–stress theories of borderline etiology, including dialectical behavioral therapy (Linehan, Armstrong, Suarez, Allmon, & Heard, 1991) and mentalization-based therapy (Fonagy & Luyten, 2009), also receive support from findings in this study. These treatment approaches have shown success in clinical trials (Bateman & Fonagy, 2008; Bateman, Ryle, Fonagy, & Kerr, 2007; Chiesa, Fonagy, & Holmes, 2006; Linehan et al., 2002, 2006), but direct tests of their diathesis–stress theoretical models can refine clinical practice. To further inform treatment, research is needed that links interaction between inherited liability and harsh treatment to the cognitive, behavioral, and emotional underpinnings of borderline personality.
These implications should be considered in light of several limitations. First, measurement of BPRCs in children is relatively new and replication of findings using alternate measures of borderline personality is necessary. Nevertheless, our measure of borderline personality showed good construct validity and expected patterns of psychiatric comorbidity (Skodol, Gunderson, et al., 2002; Zanarini et al., 1998). Although there are competing approaches to measurement of juvenile BPD traits, the content of the Shedler–Westen system used in our study overlaps with these other instruments (Crick et al., 2005; Rogosch & Cicchetti, 2005; Tellegen & Waller, 2008; Zanarini, Frankenburg, Sickel, & Yong, 1996) and with the proposed revisions of DSM-V (American Psychiatric Association, 2010), attesting to its construct validity. Nevertheless, the BPRCs measured in our study may be tapping a general risk syndrome, rather than a developmental precursor specific to adult BPD. We will need to follow-up with this sample in adulthood to determine how well childhood BPRCs predict adult BPD compared to other forms of psychopathology. Second, children’s BPRCs were assessed in interviews with mothers. Mothers were also the source of information on family history, maltreatment and, by providing speech samples, our ratings of expressed emotion. Consequently, correlations among these measures may be inflated due to a shared reporter. However, this potential limitation may be mitigated by the time lapse between measurements; the most proximate measurements of maltreatment and expressed emotion were collected 2 years before measurements of BPRCs and family history. More importantly, shared-reporter bias cannot account for the consistent pattern of associations we observed in twin difference analyses. Third, we did not have access to a specific risk genotype or family history of BPD per se. We measured diathesis using family history of serious psychiatric disorder because BPD is a complex disorder that likely involves many genes (Beauchaine, Klein, Crowell, Derbidge, & Gatzke-Kopp, 2009; Gunderson & Lyons-Ruth, 2008; Stanley & Siever, 2010), and because relatives of borderline probands exhibit a range of affective and impulse spectrum disorders (Zanarini et al., 2004). In addition, it is important to acknowledge that family history reflects not only genetic vulnerability, but also environmental inputs. Nevertheless, environmental inputs comprised in family history did not substantively overlap with the environmental inputs we studied, physical maltreatment and maternal negative expressed emotion; consistent with the diathesis–stress model, our measures of harsh treatment were principally moderators and not mediators of the association between family history and BPRCs. Fourth, the risk factors included in this study are not specific to BPD, but predict many other psychiatric disorders (Cannon et al., 2002; Caspi, Moffitt, Newman, & Silva, 1996; Kim-Cohen et al., 2005; Koenen et al., 2009; Milne, Caspi, Harrington, et al., 2009; Moffitt et al., 2007; Polanczyk et al., 2009). This raises the question of how specific disorders emerge from a common early risk profile. Finally, we studied a cohort of twins and our results may not generalize to singletons. However, there is no evidence to suggest that twins and singleton differ in their family psychiatric history, experiences of harsh treatment, or in behavior problems (Johnson, Krueger, Bouchard, & McGue, 2002).
Despite these limitations, our study has important strengths. The validity of our findings is supported by five design features: (a) we assessed two different types of harsh treatment over the first decade of life; (b) we assessed harsh treatment prospectively, prior to our measurement of the borderline outcome; (c) we used twin pair comparisons to disentangle harsh treatment from influences of child genotype or other family environments; (d) we replicated our analyses using different outcome definitions and different estimation procedures, ensuring that the results were not statistical artifacts; and (e) we relied on a representative sample (of twins) from the general population, supporting generalization of findings.
Several studies have recently alerted the research and clinical communities to the emergence of borderline personality symptoms during childhood (Chanen, Jovev, McCutcheon, Jackson, & McGorry, 2008; Miller, Muehlenkamp, & Jacobson, 2008; Sharp & Romero, 2007). Results from our study and from other recent investigations in community samples of children (Crawford et al., 2009; Crick et al., 2005; Winograd et al., 2008) reveal that BPRCs are distributed quantitatively in children, consistent with the dimensional model of personality disturbance accepted for adults (Livesley, Jang, Jackson, & Vernon, 1993; Widiger & Trull, 2007), and that childhood BPRCs share key etiological features with adult BPD. Further, our study presents evidence that BPRCs early in life emerge from the interaction between an inherited diathesis and experiences of harsh treatment, consistent with theoretical models of adult borderline etiology (Crowell et al., 2005; Fonagy et al., 2000; Gunderson & Lyons-Ruth, 2008; Linehan, 1993; Paris, 2005; Zanarini & Frankenburg, 2007). Etiological studies and clinical trials of treatment modalities that do not assess inherited diathesis for borderline personality are likely to underestimate the influence of harsh treatment on the development of BPRCs.
Acknowledgments
The E-Risk Study is funded by the Medical Research Council (MRC Grant G9806489). Additional support was provided by NICHD Grant HD061298, NIMH Grant MH077874, NIDA Grant P30 DA023026, Economic, Social Research Council Grant RES-177-25-0013, the Lady Davis Fellowship of Hebrew University, and the Jacobs Foundation. We are grateful to the study’s mothers and fathers, the twins, and the twins’ teachers for their participation. Our thanks to Michael Rutter and Robert Plomin; Thomas Achenbach for kind permission to adapt the Child Behavior Checklist; Drew Westen for permission to adapt the Borderline Scale in the Shedler–Westen Assessment Procedure 200-item Q-sort for Adolescents; and members of the E-Risk team for their dedication, hard work, and insights.
References
- Achenbach T. The Achenbach System of Empirically Based Assessment (ASEBA): Development, findings, theory, and applications. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2009. [Google Scholar]
- Achenbach TM, Becker A, Dopfner M, Heiervang E, Roessner V, Steinhausen HC, et al. Multicultural assessment of child and adolescent psychopathology with ASEBA and SDQ instruments: Research findings, applications, and future directions. Journal of Child Psychology and Psychiatry. 2008;49:251–275. doi: 10.1111/j.1469-7610.2007.01867.x. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Proposed draft revisions to DSM disorders and criteria. 2010 Retrieved May 7, 2010, from http://www.dsm5.org/ProposedRevisions/Pages/PersonalityandPersonalityDisorders.asp.
- Baddeley AD. Working memory. Oxford: Oxford University Press; 1986. [Google Scholar]
- Bateman A, Fonagy P. Eight-year follow-up of patients treated for borderline personality disorder: Mentalization-based treatment versus treatment as usual. American Journal of Psychiatry. 2008;165:631–638. doi: 10.1176/appi.ajp.2007.07040636. [DOI] [PubMed] [Google Scholar]
- Bateman AW, Ryle A, Fonagy P, Kerr IB. Psychotherapy for borderline personality disorder: Mentalization based therapy and cognitive analytic therapy compared. International Review of Psychiatry. 2007;19:51–62. doi: 10.1080/09540260601109422. [DOI] [PubMed] [Google Scholar]
- Battle CL, Shea MT, Johnson DM, Yen S, Zlotnick C, Zanarini MC, et al. Childhood maltreatment associated with adult personality disorders: Findings from the collaborative longitudinal personality disorders study. Journal of Personality Disorders. 2004;18:193–211. doi: 10.1521/pedi.18.2.193.32777. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge C, Gatzke-Kopp L. Multifinality in the development of personality disorders: A Biology×Sex×Environment interaction model of antisocial and borderline traits. Development and Psychopathology. 2009;21:735–770. doi: 10.1017/S0954579409000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bemporad JR, Smith HF, Hanson G, Cicchetti D. Borderline syndromes in childhood: Criteria for diagnosis. American Journal of Psychiatry. 1982;139:596–602. doi: 10.1176/ajp.139.5.596. [DOI] [PubMed] [Google Scholar]
- Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlashan TH, et al. Treatment utilization by patients with personality disorders. American Journal of Psychiatry. 2001;158:295–302. doi: 10.1176/appi.ajp.158.2.295. [DOI] [PubMed] [Google Scholar]
- Berenbaum MC. What is synergy? Pharmacological Reviews. 1989;41:93–141. [PubMed] [Google Scholar]
- Bernstein DP, Cohen P, Velez CN, Schwabstone M, Siever LJ, Shinsato L. Prevalence and stability of the DSM-III-R personality-disorders in a community-based survey of adolescents. American Journal of Psychiatry. 1993;150:1237–1243. doi: 10.1176/ajp.150.8.1237. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Iacono WG, McGue M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: A longitudinal twin study. Development and Psychopathology. 2009;21:1335–1353. doi: 10.1017/S0954579409990186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botto LD, Khoury MJ. Commentary: Facing the challenge of gene–environment interaction: The two-by-four table and beyond. American Journal of Epidemiology. 2001;153:1016–1020. doi: 10.1093/aje/153.10.1016. [DOI] [PubMed] [Google Scholar]
- Bradley R, Jenei J, Westen D. Etiology of borderline personality disorder: Disentangling the contributions of intercorrelated antecedents. Journal of Nervous and Mental Disease. 2005;193:24–31. doi: 10.1097/01.nmd.0000149215.88020.7c. [DOI] [PubMed] [Google Scholar]
- Bradley R, Zittel Conklin C, Westen D. The borderline personality diagnosis in adolescents: Gender differences and subtypes. Journal of Child Psychology and Psychiatry. 2005;46:1006–1019. doi: 10.1111/j.1469-7610.2004.00401.x. [DOI] [PubMed] [Google Scholar]
- Campbell FA, Pungello E, Miller-Johnson S, Burchinal M, Ramey CT. The development of cognitive and academic abilities: Growth curves from an early childhood educational experiment. Developmental Psychology. 2001;37:231–242. doi: 10.1037/0012-1649.37.2.231. [DOI] [PubMed] [Google Scholar]
- Cannon M, Caspi A, Moffitt TE, Harrington H, Taylor A, Murray RM, et al. Evidence for early-childhood, pan-developmental impairment specific to schizophreniform disorder—Results from a longitudinal birth cohort. Archives of General Psychiatry. 2002;59:449–456. doi: 10.1001/archpsyc.59.5.449. [DOI] [PubMed] [Google Scholar]
- Carlson EA, Egeland B, Sroufe LA. A prospective investigation of the development of borderline personality symptoms. Development and Psychopathology. 2009;21:1311–1334. doi: 10.1017/S0954579409990174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Hariri AR, Holmes A, Uher R, Moffitt TE. Genetic sensitivity to the environment: The case of the serotonin transporter gene and its implications for studying complex diseases and traits. American Journal of Psychiatry. 2010;167:509–527. doi: 10.1176/appi.ajp.2010.09101452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Henry B, McGee RO, Moffitt TE, Silva PA. Temperamental origins of child and adolescent behavior problems: From age 3 to age 15. Child Development. 1995;66:55–68. doi: 10.1111/j.1467-8624.1995.tb00855.x. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Morgan J, Rutter M, Taylor A, Arseneault L, et al. Maternal expressed emotion predicts children’s antisocial behavior problems: Using monozygotic-twin differences to identify environmental effects on behavioral development. Developmental Psychology. 2004;40:149–161. doi: 10.1037/0012-1649.40.2.149. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders—Longitudinal evidence from a birth cohort. Archives of General Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- Chabrol H, Montovany A, Chouicha K, Callahan S, Mullet E. Frequency of borderline personality disorder in a sample of French high school students. Canadian Journal of Psychiatry. 2001;46:847–849. doi: 10.1177/070674370104600909. [DOI] [PubMed] [Google Scholar]
- Chabrol H, Montovany A, Duconge E, Kallmeyer A, Mullet E, Leichsenring F. Factor structure of the Borderline Personality Inventory in adolescents. European Journal of Psychological Assessment. 2004;20:59–65. [Google Scholar]
- Chanen AM, Jovev M, Jackson HJ. Adaptive functioning and psychiatric symptoms in adolescents with borderline personality disorder. Journal of Clinical Psychiatry. 2007;68:297–306. doi: 10.4088/jcp.v68n0217. [DOI] [PubMed] [Google Scholar]
- Chanen AM, Jovev M, McCutcheon LK, Jackson HJ, McGorry PD. Borderline personality disorder in young people and the prospects for prevention and early intervention. Current Psychiatry Reviews. 2008;4:48–57. [Google Scholar]
- Chiesa M, Fonagy P, Holmes J. Six-year follow-up of three treatment programs to personality disorder. Journal of Personality Disorders. 2006;20:493–509. doi: 10.1521/pedi.2006.20.5.493. [DOI] [PubMed] [Google Scholar]
- Coan JA. Toward a neuroscience of attachment. In: Cassidy J, Shaver PR, editors. Handbook of attachment theory and research. 2. New York: Guilford Press; 2008. pp. 666–697. [Google Scholar]
- Crawford TN, Cohen PR, Chen HNA, Anglin DM, Ehrensaft M. Early maternal separation and the trajectory of borderline personality disorder symptoms. Development and Psychopathology. 2009;21:1013–1030. doi: 10.1017/S0954579409000546. [DOI] [PubMed] [Google Scholar]
- Crick NR, Murray-Close D, Woods K. Borderline personality features in childhood: A short-term longitudinal study. Development and Psychopathology. 2005;17:1051–1070. [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin. 2009;135:495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, McCauley E, Smith CJ, Stevens AL, Sylvers P. Psychological, autonomic, and serotonergic correlates of parasuicide among adolescent girls. Development and Psychopathology. 2005;17:1105–1127. doi: 10.1017/s0954579405050522. [DOI] [PubMed] [Google Scholar]
- Distel MA, Trull TJ, Derom CA, Thiery EW, Grimmer MA, Martin NG, et al. Heritability of borderline personality disorder features is similar across three countries. Psychological Medicine. 2008;38:1219–1229. doi: 10.1017/S0033291707002024. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Bates JE, Pettit GS. Mechanisms in the cycle of violence. Science. 1990;250:1678–1683. doi: 10.1126/science.2270481. [DOI] [PubMed] [Google Scholar]
- Donelan-McCall N, Eckenrode J, Olds DL. Home visiting for the prevention of child maltreatment: Lessons learned during the past 20 years. Pediatric Clinics of North America. 2009;56:389. doi: 10.1016/j.pcl.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Bateman A. The development of borderline personality disorder—A mentalizing model. Journal of Personality Disorders. 2008;22:4–21. doi: 10.1521/pedi.2008.22.1.4. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Luyten P. A developmental, mentalization-based approach to the understanding and treatment of borderline personality disorder. Development and Psychopathology. 2009;21:1355–1381. doi: 10.1017/S0954579409990198. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Target M, Gergely G. Attachment and borderline personality disorder—A theory and some evidence. Psychiatric Clinics of North America. 2000;23:103. doi: 10.1016/s0193-953x(05)70146-5. [DOI] [PubMed] [Google Scholar]
- Fox NA, Hane AA. Studying the biology of human attachment. In: Cassidy J, Shaver PR, editors. Handbook of attachment theory and research. 2. New York: Guilford Press; 2008. pp. 666–697. [Google Scholar]
- Gerstadt CL, Hong YJ, Diamond A. The relationship between cognitition and action: perfornance of children 3 1/2–7 years old on a Stroop-like day-night test. Cognition. 1994;53:129–153. doi: 10.1016/0010-0277(94)90068-x. [DOI] [PubMed] [Google Scholar]
- Gottlieb G, Blair C. How early experience matters in intellectual development in the case of poverty. Prevention Science. 2004;5:245–252. doi: 10.1023/b:prev.0000045358.12782.6b. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69:533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Reynolds EK, Bagge CL, Latzman RD, Daughters SB, et al. Extending extant models of the pathogenesis of borderline personality disorder to childhood borderline personality symptoms: The roles of affective dysfunction, disinhibition, and self-and emotion-regulation deficits. Development and Psychopathology. 2009;21:1263–1291. doi: 10.1017/S0954579409990150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grodzinsky GM, Diamond R. Frontal lobe functioning in boys with attention-deficit hyperactivity disorder. Developmental Neuropsychology. 1992;8:427–445. [Google Scholar]
- Gunderson JG. Borderline personality disorder: Ontogeny of a diagnosis. American Journal of Psychiatry. 2009;166:530–539. doi: 10.1176/appi.ajp.2009.08121825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunderson JG, Lyons-Ruth K. BPD’s interpersonal hypersensitivity phenotype: A gene–environment–developmental model. Journal of Personality Disorders. 2008;22:22–41. doi: 10.1521/pedi.2008.22.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzder J, Paris J, Zelkowitz P, Feldman R. Psychological risk factors for borderline pathology in school-age children. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:206–212. doi: 10.1097/00004583-199902000-00021. [DOI] [PubMed] [Google Scholar]
- Guzder J, Paris J, Zelkowitz P, Marchessault K. Risk factors for borderline pathology in children. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:26–33. doi: 10.1097/00004583-199601000-00009. [DOI] [PubMed] [Google Scholar]
- Hughes C, Adlam A, Happe F, Jackson J, Taylor A, Caspi A. Good test–retest reliability for standard and advanced false-belief tasks across a wide range of abilities. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2000;41:483–490. [PubMed] [Google Scholar]
- Hughes C, Jaffee SR, Happe F, Taylor A, Caspi A, Moffitt TE. Origins of individual differences in theory of mind: From nature to nurture? Child Development. 2005;76:356–370. doi: 10.1111/j.1467-8624.2005.00850.x. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Chen HN, Kasen S, Brook JS. Parenting behaviors associated with risk for offspring personality disorder during adulthood. Archives of General Psychiatry. 2006;63:579–587. doi: 10.1001/archpsyc.63.5.579. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Skodol AE, Hamagami F, Brook JS. Age-related change in personality disorder trait levels between early adolescence and adulthood: A community-based longitudinal investigation. Acta Psychiatrica Scandinavica. 2000;102:265–275. doi: 10.1034/j.1600-0447.2000.102004265.x. [DOI] [PubMed] [Google Scholar]
- Johnson W, Krueger RF, Bouchard TJ, McGue M. The personalities of twins: Just ordinary folks. Twin Research. 2002;5:125–131. doi: 10.1375/1369052022992. [DOI] [PubMed] [Google Scholar]
- Joyce PR, McHugh PC, McKenzie JM, Sullivan PF, Mulder RT, Luty SE, et al. A dopamine transporter polymorphism is a risk factor for borderline personality disorder in depressed patients. Psychological Medicine. 2006;36:807–813. doi: 10.1017/S0033291706007288. [DOI] [PubMed] [Google Scholar]
- Judd PH. Neurocognitive impairment as a moderator in the development of borderline personality disorder. Development and Psychopathology. 2005;17:1173–1196. doi: 10.1017/s0954579405050558. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Czajkowski N, Roysamb E, Tambs K, Torgersen S, et al. The structure of genetic and environmental risk factors for DSM-IV personality disorders: A multivariate twin study. Archives of General Psychiatry. 2008;65:1438–1446. doi: 10.1001/archpsyc.65.12.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Arseneault L, Caspi A, Tomas MP, Taylor A, Moffitt TE. Validity of DSM-IV conduct disorder in 4 1/2 5-year-old children: A longitudinal epidemiological study. American Journal of Psychiatry. 2005;162:1108–1117. doi: 10.1176/appi.ajp.162.6.1108. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Moffitt TE, Roberts AL, Martin LT, Kubzansky L, Harrington H, et al. Childhood IQ and adult mental disorders: A test of the cognitive reserve hypothesis. American Journal of Psychiatry. 2009;166:50–57. doi: 10.1176/appi.ajp.2008.08030343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- Lenzenweger MF. Epidemiology of personality disorders. Psychiatric Clinics of North America. 2008;31:395–403. vi. doi: 10.1016/j.psc.2008.03.003. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;62:553–564. doi: 10.1016/j.biopsych.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Psychosocial characteristics of adolescents with a history of suicide attempt. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:60–68. doi: 10.1097/00004583-199301000-00009. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN. Axis II psychopathology as a function of Axis I disorders in childhood and adolescence. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:1752–1759. doi: 10.1097/00004583-199712000-00024. [DOI] [PubMed] [Google Scholar]
- Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M. Borderline personality disorder. Lancet. 2004;364:453–461. doi: 10.1016/S0140-6736(04)16770-6. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive–behavioral treatment for borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive–behavioral treatment of chronically parasuicidal borderline patients. Archives of General Psychiatry. 1991;48:1060–1064. doi: 10.1001/archpsyc.1991.01810360024003. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry. 2006;63:757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, et al. Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug and Alcohol Dependence. 2002;67:13–26. doi: 10.1016/s0376-8716(02)00011-x. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, Jang KL, Jackson DN, Vernon PA. Genetic and environmental contributions to dimensions of borderline personality disorder. American Journal of Psychiatry. 1993;150:1826–1831. doi: 10.1176/ajp.150.12.1826. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Holmesa BM, Sasvari-Szekely M, Ronai Z, Nemoda Z, Pauls D. Serotonin transporter polymorphism and borderline or antisocial traits among low-income young adults. Psychiatric Genetics. 2007;17:339–343. doi: 10.1097/YPG.0b013e3281ac237e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macfie J, Swan SA. Representations of the caregiver–child relationship and of the self, and emotion regulation in the narratives of young children whose mothers have borderline personality disorder. Development and Psychopathology. 2009;21:993–1011. doi: 10.1017/S0954579409000534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madsen M, Osler M. Commentary: Strengths and limitations of the discordant twin-pair design in social epidemiology. Where do we go from here? International Journal of Epidemiology. 2009;38:1322–1323. doi: 10.1093/ije/dyp264. [DOI] [PubMed] [Google Scholar]
- March JS, Parker JDA, Sullivan K, Stallings P, Conners CK. The multidimensional anxiety scale for children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- McGue M. When assessing twin concordance, use the probandwise not the pairwise rate. Schizophrenia Bulletin. 1992;18:171–176. doi: 10.1093/schbul/18.2.171. [DOI] [PubMed] [Google Scholar]
- Miller AL, Muehlenkamp JJ, Jacobson CM. Fact or fiction: Diagnosing borderline personality disorder in adolescents. Clinical Psychology Review. 2008;28:969–981. doi: 10.1016/j.cpr.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Milne BJ, Caspi A, Crump R, Poulton R, Rutter M, Sears MR, et al. The validity of the family history screen for assessing family history of mental disorders. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 2009;150B:41–49. doi: 10.1002/ajmg.b.30764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milne BJ, Caspi A, Harrington H, Poulton R, Rutter M, Moffitt TE. Predictive value of family history on severity of illness the case for depression, anxiety, alcohol dependence, and drug dependence. Archives of General Psychiatry. 2009;66:738–747. doi: 10.1001/archgenpsychiatry.2009.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milne BJ, Moffitt TE, Crump R, Poulton R, Rutter M, Sears MR, et al. How should we construct psychiatric family history scores? A comparison of alternative approaches from the Dunedin Family Health History Study. Psychological Medicine. 2008;38:1793–1802. doi: 10.1017/S0033291708003115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Harrington H, Milne BJ, Melchior M, Gold-berg D, et al. Generalized anxiety disorder and depression: Childhood risk factors in a birth cohort followed to age 32. Psychological Medicine. 2007;37:441–452. doi: 10.1017/S0033291706009640. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, E-Risk Team. Teen-aged mothers in contemporary Britain. Journal of Child Psychology and Psychiatry. 2002;43:727–742. doi: 10.1111/1469-7610.00082. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. MPlus user’s guide. 5. Los Angeles: Author; 1998–2009. [Google Scholar]
- Nemoda Z, Lyons-Ruth K, Szekely A, Bertha E, Faludi G, Sasvari-Szekely M. Association between dopaminergic polymorphisms and borderline personality traits among at-risk young adults and psychiatric inpatients. Behavioral and Brain Functions. 2010;6:11. doi: 10.1186/1744-9081-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemoda Z, Ronai Z, Sasvari-Szekely M, Pauls D, Holmes BM, Lyons-Ruth K. Unpublished manuscript. 2005. Serotonin transporter polymorphism associated with borderline and antisocial features. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL, Sadler L, Kitzman H. Programs for parents of infants and toddlers: Recent evidence from randomized trials. Journal of Child Psychology and Psychiatry. 2007;48:355–391. doi: 10.1111/j.1469-7610.2006.01702.x. [DOI] [PubMed] [Google Scholar]
- Paris J. The development of impulsivity and suicidality in borderline personality disorder. Development and Psychopathology. 2005;17:1091–1104. doi: 10.1017/s0954579405050510. [DOI] [PubMed] [Google Scholar]
- Paris J, Zelkowitz P, Guzder J, Joseph S, Feldman R. Neuropsychological factors associated with borderline pathology in children. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:770–774. [PubMed] [Google Scholar]
- Polanczyk G, Caspi A, Williams B, Price TS, Danese A, Sugden K, et al. Protective effect of CRHR1 gene variants on the development of adult depression following childhood maltreatment replication and extension. Archives of General Psychiatry. 2009;66:978–985. doi: 10.1001/archgenpsychiatry.2009.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavioral Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Reich DB, Zanarini MC. Developmental aspects of borderline personality disorder. Harvard Review of Psychiatry. 2001;9:294–301. doi: 10.1080/10673220127909. [DOI] [PubMed] [Google Scholar]
- Rogosch FA, Cicchetti D. Child maltreatment, attention networks, and potential precursors to borderline personality disorder. Development and Psychopathology. 2005;17:1071–1089. doi: 10.1017/s0954579405050509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Walker AM. Concepts of interaction. American Journal of Epidemiology. 1980;112:467–470. doi: 10.1093/oxfordjournals.aje.a113015. [DOI] [PubMed] [Google Scholar]
- Sanislow CA, Little TD, Ansell EB, Grilo CM, Daversa M, Markowitz JC, et al. Ten-year stability and latent structure of the DSM-IV schizotypal, borderline, avoidant, and obsessive–compulsive personality disorders. Journal of Abnormal Psychology. 2009;118:507–519. doi: 10.1037/a0016478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattler JM. Unpublished manuscript. 1992. Assessment of children: WIOSC-III and WPPSI-R supplement. [Google Scholar]
- Schwartz S. Modern epidemiologic approaches to interaction: Applications to the study of genetic interaction. Washington DC: National Academies Press; 2006. [Google Scholar]
- Sharp C, Romero C. Borderline personality disorder: A comparison between children and adults. Bulletin of the Menninger Clinic. 2007;71:85–114. doi: 10.1521/bumc.2007.71.2.85. [DOI] [PubMed] [Google Scholar]
- Siever LJ, Davis KL. A psychobiological perspective on the personality disorders. American Journal of Psychiatry. 1991;148:1647–1658. doi: 10.1176/ajp.148.12.1647. [DOI] [PubMed] [Google Scholar]
- Siever LJ, Torgersen S, Gunderson JG, Livesley WJ, Kendler KS. The borderline diagnosis III: Identifying endophenotypes for genetic studies. Biological Psychiatry. 2002;51:964–968. doi: 10.1016/s0006-3223(02)01326-4. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ. The borderline diagnosis I: Psychopathology comorbidity, and personaltity structure. Biological Psychiatry. 2002;51:936–950. doi: 10.1016/s0006-3223(02)01324-0. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Siever LJ, Livesley WJ, Gunderson JG, Pfohl B, Widiger TA. The borderline diagnosis II: Biology, genetics, and clinical course. Biological Psychiatry. 2002;51:951–963. doi: 10.1016/s0006-3223(02)01325-2. [DOI] [PubMed] [Google Scholar]
- Stanley B, Siever LJ. The interpersonal dimension of borderline personality disorder: Toward a neuropeptide model. American Journal of Psychiatry. 2010;167:24–39. doi: 10.1176/appi.ajp.2009.09050744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata/SE for Windows (Version 10.1) College Station, TX: Author; 2009. [Google Scholar]
- Tellegen A, Waller NG. Exploring personality through test construction: development of the multidimensional personality questionnaire. In: Boyle GJ, Matthews G, Saklofske DH, editors. Handbook of personality theory and testing. Personality measurment and assesment. Vol. 2. London: Sage; 2008. pp. 261–292. [Google Scholar]
- Torgersen S, Czajkowski N, Jacobson K, Reichborn-Kjennerud T, Roysamb E, Neale MC, et al. Dimensional representations of DSM-IV cluster B personality disorders in a population-based sample of Norwegian twins: A multivariate study. Psychological Medicine. 2008;38:1617–1625. doi: 10.1017/S0033291708002924. [DOI] [PubMed] [Google Scholar]
- Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Archives of General Psychiatry. 2001;58:590–596. doi: 10.1001/archpsyc.58.6.590. [DOI] [PubMed] [Google Scholar]
- Torgersen S, Lygren S, Oien PA, Skre I, Onstad S, Edvardsen J, et al. A twin study of personality disorders. Comprehensive Psychiatry. 2000;41:416–425. doi: 10.1053/comp.2000.16560. [DOI] [PubMed] [Google Scholar]
- Trouton A, Spinath FM, Plomin R. Twins Early Development Study (TEDS): A multivariate, longitudinal genetic investigation of language, cognition and behavior problems in childhood. Twin Research. 2002;5:444–448. doi: 10.1375/136905202320906255. [DOI] [PubMed] [Google Scholar]
- van Os J, Hanssen M, Bak M, Bijl RV, Vollebergh W. Do urbanicity and familial liability coparticipate in causing psychosis? American Journal of Psychiatry. 2003;160:477–482. doi: 10.1176/appi.ajp.160.3.477. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children. 4. United Kingdom, San Antonio, TX: Harcourt Assessment; 2003. [Google Scholar]
- Westen D, Shedler J, Durrett C, Glass S, Martens A. Personality diagnoses in adolescence: DSM-IV axis II diagnoses and an empirically derived alternative. American Journal of Psychiatry. 2003;160:952–966. doi: 10.1176/appi.ajp.160.5.952. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Trull TJ. Plate tectonics in the classification of personality disorder—Shifting to a dimensional model. American Psychologist. 2007;62:71–83. doi: 10.1037/0003-066X.62.2.71. [DOI] [PubMed] [Google Scholar]
- Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56:645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- Winograd G, Cohen P, Chen HN. Adolescent borderline symptoms in the community: Prognosis for functioning over 20 years. Journal of Child Psychology and Psychiatry. 2008;49:933–941. doi: 10.1111/j.1469-7610.2008.01930.x. [DOI] [PubMed] [Google Scholar]
- Zanarini MC. Childhood experiences associated with the development of borderline personality disorder. Psychiatric Clinics of North America. 2000;23:89. doi: 10.1016/s0193-953x(05)70145-3. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Barison LK, Frankenburg FR, Reich DB, Hudson JI. Family history study of the familial coaggregation of borderline personality disorder with Axis I and non-borderline dramatic cluster Axis II disorders. Journal of Personality Disorders. 2009;23:357–369. doi: 10.1521/pedi.2009.23.4.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR. The essential nature of borderline psychopathology. Journal of Personality Disorders. 2007;21:518–535. doi: 10.1521/pedi.2007.21.5.518. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis I comorbidity of borderline personality disorder. American Journal of Psychiatry. 1998;155:1733–1739. doi: 10.1176/ajp.155.12.1733. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Psychosocial functioning of borderline patients and axis II comparison subjects followed prospectively for six years. Journal of Personality Disorders. 2005;19:19–29. doi: 10.1521/pedi.19.1.19.62178. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G, Weinberg I, Gunderson JG. The 10-year course of physically self-destructive acts reported by borderline patients and axis II comparison subjects. Acta Psychiatrica Scandinavica. 2008;117:177–184. doi: 10.1111/j.1600-0447.2008.01155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) Belmont, MA: McLean Hospital; 1996. [Google Scholar]
- Zanarini MC, Frankenburg FR, Yong L, Raviola G, Reich DB, Hennen J, et al. Borderline psychopathology in the first-degree relatives of borderline and Axis II comparison probands. Journal of Personality Disorders. 2004;18:439–447. doi: 10.1521/pedi.18.5.439.51327. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Jacoby RJ, Frankenburg FR, Reich DB, Fitzmaurice G. The 10-year course of social security disability income reported by patients with borderline personality disorder and Axis II comparison subjects. Journal of Personality Disorders. 2009;23:346–356. doi: 10.1521/pedi.2009.23.4.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Williams AA, Lewis RE, Reich RB, Vera SC, Marino MF, et al. Reported pathological childhood experiences associated with the development of borderline personality disorder. American Journal of Psychiatry. 1997;154:1101–1106. doi: 10.1176/ajp.154.8.1101. [DOI] [PubMed] [Google Scholar]