Abstract
It is increasingly perceived that gut host–microbial interactions are important elements in the pathogenesis of functional gastrointestinal disorders (FGID). The most convincing evidence to date is the finding that functional dyspepsia and irritable bowel syndrome (IBS) may develop in predisposed individuals following a bout of infectious gastroenteritis. There has been a great deal of interest in the potential clinical and therapeutic implications of small intestinal bacterial overgrowth in IBS. However, this theory has generated much debate because the evidence is largely based on breath tests which have not been validated. The introduction of culture-independent molecular techniques provides a major advancement in our understanding of the microbial community in FGID. Results from 16S rRNA-based microbiota profiling approaches demonstrate both quantitative and qualitative changes of mucosal and faecal gut microbiota, particularly in IBS. Investigators are also starting to measure host–microbial interactions in IBS. The current working hypothesis is that abnormal microbiota activate mucosal innate immune responses which increase epithelial permeability, activate nociceptive sensory pathways and dysregulate the enteric nervous system. While we await important insights in this field, the microbiota is already a therapeutic target. Existing controlled trials of dietary manipulation, prebiotics, probiotics, synbiotics and non-absorbable antibiotics are promising, although most are limited by suboptimal design and small sample size. In this article, the authors provide a critical review of current hypotheses regarding the pathogenetic involvement of microbiota in FGID and evaluate the results of microbiota-directed interventions. The authors also provide clinical guidance on modulation of gut microbiota in IBS.
Keywords: Functional gastrointestinal disorders, microbiota, irritable bowel syndrome, small intestinal bacterial overgrowth, breath tests, probiotics, prebiotics, synbiotics, antibiotics
Introduction
Functional gastrointestinal disorders (FGIDs) are defined by symptom-based diagnostic criteria that combine chronic or recurrent symptoms attributable to the GI tract in the absence of other pathologically-based disorders.1 The FGIDs are classified into six major categories for adults: oesophageal, gastroduodenal, bowel, functional abdominal pain syndrome, biliary and anorectal. Of these, the functional bowel disorders (FBD) constitute one of the most common reasons for seeking healthcare,2 and they are associated with poor health-related quality of life3–5 and substantial costs to society.6–9 The pathophysiological mechanisms underlying these disorders are incompletely known, but abnormal gastrointestinal (GI) motility, visceral hypersensitivity, altered brain–gut function, low-grade inflammation, psychosocial disturbance and intestinal microbes may contribute.10–12
The human body is inhabited by a complex community of microbes, collectively referred to as microbiota.13 It is estimated that the human microbiota contains 1014 cells, which outnumber the human cells in our bodies by a factor of ten.14 A vast majority of these are found in the GI tract, with a continuum from 101–103 bacteria per gram of content in the stomach and duodenum to 1011–1012 cells per gram in the colon.15 Moreover, the microbial composition differs between these sites,16 and there are also significant differences between the microbiota present in the gut lumen and the microbiota attached to and embedded in the mucus layer of the GI tract.17 The microbiota is taxonomically classified via the traditional biological nomenclature (phylum—class—order—family—genus—species) and currently more than 50 bacterial phyla have been described, of which 10 inhabit the colon and three predominate: the Firmicutes, Bacteroidetes and the Actinobacteria; other sites display a different microbial composition.18 19 A challenge for researchers and clinicians is that most of the microbial diversity in the human GI tract is not currently represented by available cultured species,20 but during recent years, the use of culture-independent techniques to study the gut microbiota has increased the understanding of the role of gut microbiota in health and disease.14
Several lines of evidence indicate that bacteria may be involved in the pathogenesis and pathophysiology of FBD, through the metabolic capacity of the luminal microbiota, and the potential of the mucosa-associated microbiota to influence the host via immune–microbial interactions.21 For instance, many subjects with irritable bowel syndrome (IBS) report symptom onset following an enteric infection.22 There are also studies reporting positive effects of treatments directed at gut microbiota in patients with FBD.23 24 Moreover, small intestinal bacterial overgrowth (SIBO)25 and altered intestinal microbiota26 are implicated in subgroups of FBD patients. However, the clinical relevance of these findings remains unclear and, therefore, we sought to critically review the existing literature on the role of intestinal microbiota in FBD, focusing predominantly on IBS, and to provide recommendations for how to implement the current knowledge into clinical practice and to guide future research.
This manuscript is a synthesis of the endeavour of the Rome Foundation Committee Report. More indepth description of the work produced by this team is provided as online supplementary material.
Current knowledge of the microbiota
A relationship, often termed symbiosis, has developed between the host and the intestinal microbiota over millions of years. Host genetic and immune as well as environmental factors influence intestinal microbiota composition which in turn shape host immunity and physiology within and beyond the gut (figure 1). Recent human studies demonstrate a hitherto unimagined complexity of the human gut microbiota with hundreds of phylotypes, of which 80% remain uncultured.19 Of the 10 bacterial phyla detected in the gut the Firmicutes, Bacteroidetes and Actinobacteria predominate, of which the Firmicutes is the most dominant and diverse phylum in the GI tract. Facultative anaerobes account for <0.1% of the total bacteria detected in faecal samples. A recent paper suggested that the human GI tract microbiota can be divided into three robust clusters called enterotypes formed by groups of species that jointly contribute to their respective preferred community composition.27 Remarkably, these enterotypes do not vary by patient characteristics, such as nation, gender, age or body mass index, although these findings are based on relatively small numbers of subjects. While most studies used faecal material, this does differ somewhat from the bacteria adherent to the mucosa, which are likely to interact most strongly with the host.28
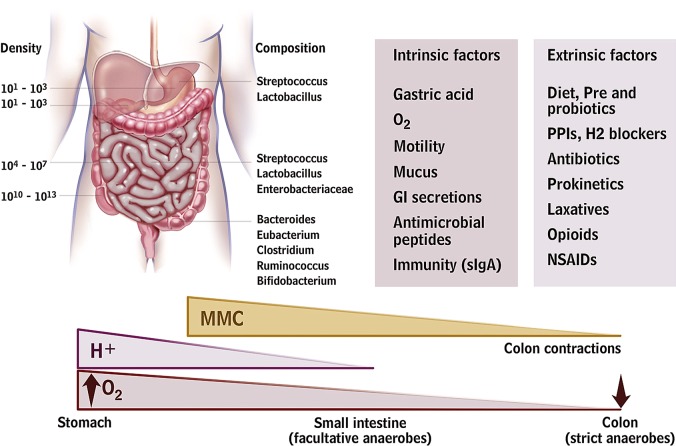
Figure 1.
Gut microbiota and the intrinsic and extrinsic factors that can affect its distribution and composition. A number of host mechanisms participate in gut microbiota modulation, including gastric acid secretion, fluid, anticommensal sIgA and antimicrobial peptide production, and gastrointestinal (GI) motility. Drugs that block acid secretion and affect GI motility can indirectly alter the microbiota. Antibiotics, depending on spectrum and dosage, will directly affect microbiota composition. Dietary modifications, including probiotic and fibre supplements, will also affect microbiota composition. MMC, migrating motor complexes; H+ hydrogen ions; O2, partial oxygen tension; sIgA, secretory immunoglobulin A; PPI, proton pump inhibitor; NSAID, non-steroidal anti-inflammatory drug.
Babies are born with sterile intestines but are rapidly colonised by bacteria from their immediate environment, most importantly their mother's vagina and gut.29 Early colonisers of the neonatal gut are mainly aerobes (such as staphylococci, streptococci and enterobacteria), while late colonisers are strict anaerobes (such as eubacteria and clostridia) as the total microbiota become more complex, more stable and converge to a common pattern.30 31 The microbiota continue to evolve until adulthood with a gradual increase in Bacteroides spp., a decline in Lactobacillus spp. after the age of five and a decline in Bifidobacterium spp. in late teenage.32 Changes also occur in extreme old age when Bacteroides spp. decrease while Enterococcus spp. and Escherichia coli increase.33 34 Industrialisation has changed both our diet and microbiota as evidenced by comparing the faecal microbiota of African rural children with a polysaccharide-rich diet with Italian city children on a high fat, high protein diet. African children have a significant enrichment in Bacteroidetes, especially Prevotella and Xylanibacter genera known to contain genes for xylan hydrolysis35 (figure 2). Whole grain cereals,36 resistant starch37 38 and low residue diets profoundly alter the microbiota.39 Although there is evidence indicating that obese individuals have an increase in Firmicutes and a decrease in Bacteroidetes (a difference likely related in part to different diets40), other studies failed to support these observations.41 42 Many dietary prebiotics including oligofructose,43 lactulose,44 45 lupin kernel,46 inulin-containing juices47 and arabinoxylan-oligosaccharides48 significantly alter human faecal microbiota. The concept of poorly absorbed but fermentable oligo-, di- and mono-saccharides and polyols (FODMAPs) includes many substances which are substrates for bacterial metabolism and may therefore alter the microbiota but this has as yet not been studied.
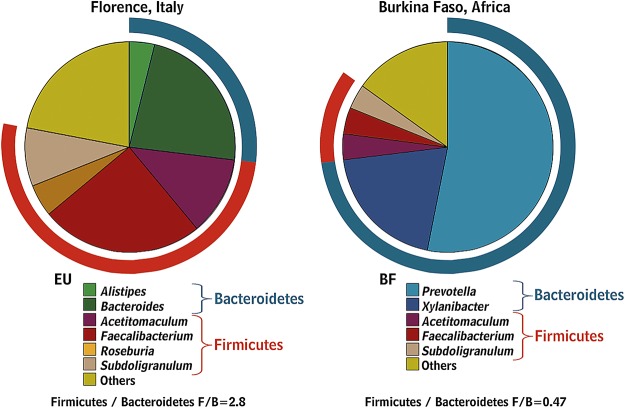
Figure 2.
Gut microbiota composition in African children living in rural areas with a polysaccharide-rich diet when compared with Italian city children.35 (Reprinted with permission from Proc Natl Acad Sci USA).
Most high fibre diets alter the microbiota and accelerate transit. Accelerating transit using senna increased the production of short chain fatty acids (SCFAs) but reduced faecal methanogens, the opposite to the effect of loperamide.49 Accelerating transit with cisapride also increases production of SCFAs, particularly propionic and butyric acids.50 Acetate, which predominates in the colonic contents, is largely inhibitory. In contrast, propionate and butyrate stimulate motility, activate propulsive ileal motor patterns in humans51 and ensure that bacteria are propelled from the ileum to the colon. The normal microbiota also strongly influence the mucosal immune system52 53 which is underdeveloped in germ-free animals, who have reduced T cells, immunoglobulin A producing B cells and intraepithelial T cells.52 54–56 Twin studies suggest that the host genotype influences the gut microbiota, although results remain conflicting because of the inability to control for shared environmental factors.40 57 One of the most important genetic effects is mediated via the innate immune response. Thus, mice lacking the bacterial sensing receptor nucleotide-binding oligomerisation domain-containing protein-2 showed significantly more Bacteroidetes as well as Firmicutes compared with wild-type mice.58
Modulation of the microbiota induces visceral hypersensitivity in mice, which is reduced by Lactobacillus paracasei NCC2461 secreted products.59 Lactobacillus acidophilus NCFM and Lactobacillus paracasei NCC2461 also modulate visceral pain perception in rodents.60 61 Transient perturbation of the microbiota with antimicrobials alters brain-derived neurotrophic factor expression, exploratory behaviour and colonisation of germ-free mice suggesting that intestinal microbiota impact is not limited to the gut and the immune system, but may involve the central nervous system.62 (Note: this last sentence appears run-on but I can't quite decipher how to fix it.)
Approaches to the study of microbiota
Approaches to the study of microbiota and relative advantages/pitfalls are reported in box 1. Culture-based studies reveal that the gut microbiota is a highly complex community (box 1).63 Although culturing remains valuable for identifying functional groups and for selective enumeration (eg, of pathogens), new culture-independent approaches provide more powerful and convenient methodologies for monitoring changes in the GI tract community (table 1). Information on the diversity of microbes that colonise the gut has expanded rapidly over the past 15 years, based largely on the analysis of the small subunit ribosomal RNA (16S rRNA for Bacteria and Archaea, 18S rRNA for Eukaryotes) gene sequences that can be obtained by direct amplification from nucleic acids extracted from gut or stool samples.64 This information provides the basis for a range of complimentary techniques for enumerating gut bacteria, including fingerprinting methods such as denaturing gradient gel electrophoresis65 and targeted methods such as fluorescent in situ hybridisation and quantitative PCR. The arrival of new high-throughput sequencing approaches and 16S rRNA-based microarraying has further accelerated the supply of data by allowing amplified 16S rRNA sequences to be analysed indepth without the need for ‘classical’ cloning and sequencing methods.66 67 Although culturing may bias against bacteria that are hard to grow in the laboratory, PCR amplification biases against certain groups of gut bacteria. For example, bifidobacterial 16S rRNA sequences are often under-represented among amplified products, although more reliably enumerated by 16S rRNA-targeted fluorescent in situ hybridisation detection or quantitative PCR.37 While most molecular enumeration methods target 16S rRNA, some are based on more functionally relevant genes, for example, involved in methanogenesis or butyrate synthesis.
Box 1 Approaches to the study of intestinal microbiota.
Breath tests are not validated to accurately detect small intestinal bacterial overgrowth.
Rapid molecular approaches have largely replaced cultural approaches for enumeration of the dominant gastrointestinal (GI) tract microbiota.
Cultural microbiology remains crucial for investigating microbial diversity and for the selective isolation of representatives of key functional groups, including pathogens.
- Culture-independent approaches to study the GI tract microbiota can answer the questions:
- Which microbes are present in the GI tract? (16S rRNA gene-based approaches)
- What microbial genes are present in the GI tract? (metagenomics)
- What are GI tract microbes doing? (metatranscriptomics, metaproteomics, metabonomics/metabolomics).
The possibilities of using high-throughput approaches and their depth of analysis are increasing rapidly, but it is important they are applied with careful reference to well-defined scientific questions.
Table 1.
Main features of culture-independent detection methods of gut microbiota
| Question | Target | Approach | Data generated | Can microbes be identified directly? | Main benefit | Main limitation |
| Which microbes are present in the GI tract? | Isolates | Cultivation | Phenotypic characterisation | Yes | Accurate species identification | Not representative |
| 16S rRNA gene | Cloning and sanger sequencing | Phylogenetic identification | Yes | Complete 16S rRNA gene sequence data | Cloning bias | |
| 16S rRNA gene | High-throughput sequencing | Phylogenetic identification | Yes | High-throughput data generation | Short reads | |
| 16S rRNA gene | Fingerpinting | Community profile | No | Fast comparison between communities | No direct link with phylogeny | |
| 16S rRNA | FISH | Cell numbers | Yes | Accurate enumeration | Dependent on 16S rRNA databases | |
| 16S rRNA gene | qPCR | 16S rRNA gene abundances | Yes | Wide dynamic range | Dependent on 16S rRNA databases | |
| 16S rRNA gene | Phylogenetic microarray | Phylogenetic identification | Yes | High-throughput phylogenetic profiling | Dependent on 16S rRNA databases | |
| What microbial genes are present in the GI tract? | Community DNA | Sequence-based metagenomics | Gene sequences | Not always | High-throughput data generation | Function mainly based on predictions |
| Community DNA | Function-based metagenomics | Functional properties encoded on DNA fragment | Not always | Functional properties linked to DNA sequences | Suitable cloning host/system and screening assays needed | |
| What are GI tract microbes doing? | mRNA | Metatranscriptomics | Community gene expression | Not always | Direct information about microbial activity | Community RNA extraction challenging |
| Proteins | Metaproteomics | Community protein production | Not always | Direct information about microbial activity | No uniform protocol for all cell fractions | |
| Metabonomics | Metabonomics/metabolomics | Community metabolity profiles | No | Microbiota activity representation | No link with microbes or its function | |
| Lactulose hydrogen breath test | Measuring GI tract gas production | Hydrogen and methane breath content | No | Unclear, simple test but not validated for diagnosing SIBO | May simply measure small intestinal transit time to caecum | |
| Glucose hydrogen breath test | Measuring GI tract gas production | Hydrogen breath content | No | Same as above | Poor sensitivity; misses distal SIBO |
FISH, fluorescent in situ hybridisation; GI, gastrointestinal; qPCR, quantitative PCR; SIBO, small intestinal bacterial overgrowth.
High-throughput DNA sequencing provides completely new possibilities for ‘-omics’-based analyses of the gut microbiota.19 Draft genomes of cultured gut bacteria can now be produced rapidly and at little cost.68 In addition, these methods can be applied to DNA recovered from gut or stool samples, and the analysis of the resulting complex mixture of sequences is referred to as metagenomics.69 70 The ability to analyse multiple gene sequences from large numbers of samples, complemented with functional screening and characterisation of randomly cloned DNA fragments from the GI tract, is currently being exploited to uncover changes in disease states including in inflammatory bowel disease (IBD). A related technology, metatranscriptomics, uses high-throughput sequencing or microarray analysis to examine RNA expressed in GI tract samples, thus focusing on bacteria that are transcriptionally active. Another potentially powerful tool, metaproteomics, employs protein separation and sequencing techniques to describe the major proteins present in gut or stool samples.71 72 These ‘meta-omics’ approaches rely in primary sequencing and annotation data.73 74 Thus, they rely heavily on the availability of genome sequences and functional information from cultured reference bacteria, which means there are considerable benefits from combining different approaches to gut microbiota analysis. A final ‘omics’ approach, metabonomics, is not linked directly to genetic information of the microbes, but examines the metabolite profiles resulting from total microbial activity in the gut. Since many of these metabolites exert biological effects (some positive, some negative) on the host, such analysis can provide a direct measure of the consequences of microbial activity in the gut, although excluding cell-mediated effects and direct identification to a target microbial species.
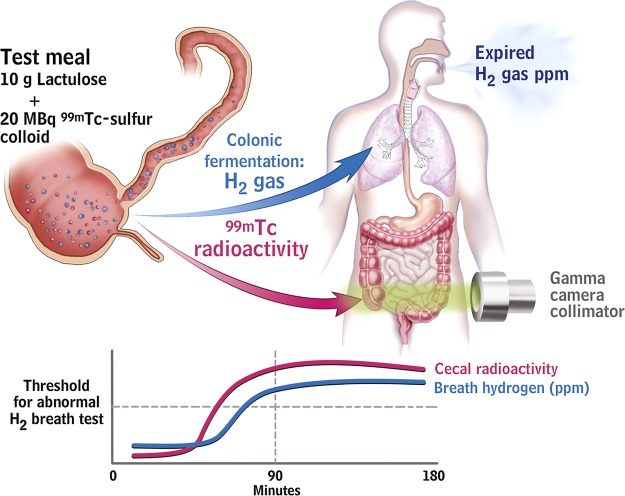
Breath testing has been used to detect SIBO in IBS patients by non-invasively detecting hydrogen producing bacteria or methane producing archaea within the gut lumen. The breath test is based on the concept that hydrogen gases are produced by colonic bacterial fermentation in response to ingestion of a test sugar. They rapidly diffuse into the blood, are excreted by breath, and can be collected and quantified.75 If SIBO exists, the timing of this fermentation would be altered but the criteria for abnormal tests lack validity (figure 3).
Figure 3.
The lactulose hydrogen breath test (LHBT) predominantly measures small intestinal transit rather than small intestinal bacterial overgrowth (SIBO) in irritable bowel syndrome (IBS) patients. Upper schematic shows ingestion of test meal with subsequent serial measurement of both H2 gas, resulting from fermentation of the lactulose by intestinal bacteria, and Tc99 scanning in the caecum. This latter measurement detects when the test meal has reached the caecum. The stylised drawing below shows a representative result from an IBS patient with serial measurements over time. The Tc99 had already reached the caecum in large quantities before the H2 PPM level has reached the threshold for an abnormal test. This demonstrates that the increased H2 production results from fermentation by colonic bacteria, not by abnormal bacteria small intestine (ie, SIBO).94
Differences in the microbiota in FBD and the link to pathophysiology
There is little known about the small intestinal microbiota as the small intestine is relatively inaccessible (summarised in table 2; box 2).75–85 Culture studies show considerably fewer bacteria compared with the colon with a marked gradient from duodenum to distal ileum. The bacteria are typically Gram-positive aerobes proximally and Gram-negative and Gram-positive anaerobes and facultative anaerobes in the terminal ileum. Culture-independent studies of the small intestinal microbiota are in their infancy but suggest complexity not appreciated by standard culture techniques, including marked individual differences, fluctuations over time (even within the same day), age-related differences and several phylotypes not previously identified.86–88 Moreover, a recent paper indicated that the small intestinal microbiota are driven by a rapid uptake and conversion of available simple carbohydrates in which Streptococcus spp. play an important role.89
Table 2.
Summary of studies culturing small bowel microbiome
| Study | Number of patients | Sample type | Microbiology results | Comments |
| Drasar and Shiner76 | 13 Diarrhoea, all investigations negative | Jejunal capsule | No difference from controls; no increased numbers of pathogens or non-pathogens | Possible IBS but not defined as IBS |
| Rumessen et al 77 | 60 Patients suspected of SIBO | Proximal jejunal aspirate | 15 With no predisposing cause had no evidence of SIBO; of 23 with SIBO, 4 had no predisposing cause | Groups poorly defined, 8 IBS identified and all negative for SIBO; 22 cases considered inconclusive |
| Corazza et al 78 | 31 Chronic diarrhoea, no predisposing cause | Proximal jejunal aspirate | 10 Had SIBO (≥106 cfu/ml or colonic bacteria), 2 IBS, 8 other multiple other diagnoses | IBS not defined, and total IBS not clear |
| Bardhan et al 79 | 10 Controls; 4 irritable colon; 22 other | Endoscopic aspirates from proximal jejunum | No positive cultures in irritable colon | Positive cultures in 11 cases, many postsurgical |
| Lewis et al 80 | 23 With functional bowel disorders | Duodenal endoscopic aspirate | Mean control count 3.2×102 cfu/ml, no anaerobes, no sterile samples | No specific IBS, defined as functional bowel disorders |
| Sullivan et al 81 | 7 IBS; 20 controls | Proximal jejunal biopsy using Watson capsule | No differences, flora similar to normal oropharyngeal flora | Colonic pathogen in 2 healthy subjects |
| Posserud et al 82 | 162 IBS; 42 controls | Proximal jejunal aspirate | 4%≥105 cfu, same as controls. Subanalysis using ≥5×103, 43% IBS vs 12% controls | No correlation with motor pattern in IBS group |
| Kerckhoffs et al 83 | 8 IBS; 9 controls | Proximal jejunal aspirate | No different number diagnosed with SIBO using multiple definitions | No differences also using molecular-based counts |
| Choung et al 84 | 148 IBS; 542 ‘other indications to test for SIBO’ | Duodenal endoscopic aspirate | 2% IBS >105 cfu/ml 10% in ‘other’ indications | Retrospective study 18% IBS >0<105 cfu/ml |
| Pyleris et al 85 | 85 IBS 150 non-IBS | Duodenal endoscopic aspirate | 37% IBS >103 cfu/ml 15.11% non-IBS | All investigated because of UGI bleed |
IBS, irritable bowel syndrome; SIBO, small intestinal bacterial overgrowth; UGI, upper gastrointestinal.
Box 2 Relevance of studies showing changes in microbiota in irritable bowel syndrome.
The relevance of small intestinal bacterial overgrowth in irritable bowel syndrome (IBS) remains unclear due to methodological problems, influence of confounding factors and large differences between studies.
Heterogeneity of IBS and variation in methods used to study the faecal microbiota have resulted in conflicting reports of differences from healthy controls.
The microbiome may contribute to IBS symptoms by altering gut neuromotor-sensory function, barrier function and/or the brain–gut axis.
The role of SIBO in the pathogenesis of IBS is very controversial because the breath tests employed to establish this role have not been validated.90 91 Even the validity of the ‘gold standard’, jejunal cultures >105 cfu/ml with colonic-type bacteria, has been challenged, largely because this cut-off was established from samples following surgical diversion.91 Studies in IBS patients showed relatively few bacteria in the duodenum and proximal jejunum and no obvious differences from controls (table 2). Preliminary studies suggest that more IBS patients have SIBO when a lower cut-off of >103 cfu/ml is used but well-designed studies are needed.82 85 Available molecular studies are not adequately designed to establish whether SIBO is involved in IBS but have significant potential.
Several confounding factors, including acid suppression by proton pump inhibitors (PPIs) and altered motility, have been implicated in the studies of SIBO and IBS.92–94 Some studies suggest that PPI use might lead to symptomatic SIBO or at least increased numbers of bacteria and that following antibiotics they accelerate recurrence, but this depends on the tests employed and criteria applied.95 Although the link between SIBO and IBS is largely based on breath testing, most positive lactulose breath tests reflect rapid transit to the caecum rather than true SIBO94 (figure 4). Other factors such as antibiotics, probiotics and prebiotics, and other dietary items such as FODMAPs could also influence microbiota in IBS patients and result in a potentially spurious association.
Figure 4.
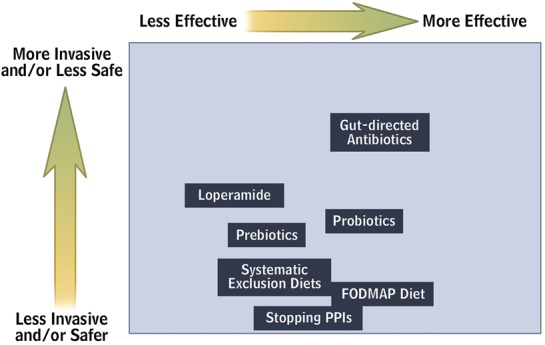
Plot chart of currently available strategies for modifying gut microbiota aiming to demonstrate the relationship between the effectiveness and invasiveness/safety of the proposed approach. FODMAP, fermentable oligo-, di- and mono-saccharides and polyols; PPI, proton pump inhibitor.
Earlier culture-based assessment of faecal microbiota obtained from patients with IBS demonstrated decreased faecal lactobacilli and bifidobacteria, and increased facultative bacteria dominated by streptococci and Escherichia coli as well as higher counts of anaerobic organisms such as Clostridium. 96 97 Studies using molecular-based techniques reveal changes in faecal microbiota composition in IBS versus controls (table 3). Interestingly, a recent study demonstrated that faecal microbiota of IBS patients could be grouped in a cluster which was completely different from that of healthy controls.114 Nonetheless, results to date are inconsistent and sometimes contradictory (table 3). This may reflect differences in molecular techniques employed, the use of single samples that are not linked to fluctuating symptoms (especially as studies suggest IBS faecal microbiomes are less stable), and probably other factors such as diet and phenotypic characterisation of patients. In addition, it should be realised that faecal samples do not necessarily reflect other parts of the GI tract.
Table 3.
Summary of culture and molecular studies of colonic microbiome
| Study | Subject | Sample | Method | Patient group | Main finding | Country of study |
| Balsari et al 96 |
|
Faeces | Culture | IBS |
|
Italy |
| Si et al 98 |
|
Faeces | Culture | IBS |
|
China |
| Malinen et al 99 |
|
Faeces | qPCR | IBS |
|
Finland |
| IBS-D |
|
|||||
| IBS-C |
|
|||||
| Mättö et al 100 |
|
Faeces | CulturePCR-DGGE | IBS |
|
Finland |
| Maukonen et al 101 |
|
Faeces |
|
IBS |
|
Finland |
| IBS-C |
|
|||||
| Kassinen et al 102 |
|
Faeces |
|
IBS |
|
Finland |
| Rajilić-Stojanović103 |
|
Faeces | Microarray | IBS |
|
Finland |
| Kerckhoffs et al 104 |
|
|
|
IBS |
|
The Netherlands |
| Krogius-Kurikka et al 105 |
|
Faeces | GC-profiling + sequencing of 16S rRNA genes | IBS-D |
|
Finland |
| Lyra et al 106 |
|
Faeces | qPCR | IBS-D |
|
Finland |
| IBS-C |
|
|||||
| IBS-A |
|
|||||
| Tana et al 107 |
|
Faeces |
|
IBS |
|
Japan |
| Codling et al 108 |
|
|
PCR-DGGE | IBS |
|
Ireland |
| Carroll et al 28 |
|
|
|
IBS-D |
|
USA |
| Noor et al 109 |
|
Faeces | PCR-DGGE + sequencing of 16S rRNA genes | IBS |
|
UK |
| Malinen et al 110 |
|
Faeces | qPCR |
|
Finland | |
| Ponnusamy et al 111 |
|
Faeces | DGGE + qPCR of 16sRNA genes |
|
Korea | |
| Rinttila et al 112 |
|
Faeces | qPCR | IBS |
|
Finland |
| Saulnier et al 113 |
|
Faeces | 16s Metagenomic sequencing and DNA microarray | IBS |
|
USA |
| Rajilic-Stojanovic et al 114 |
|
Faeces | Phylogenetic 16S rRNA microarray and qPCR | IBS |
|
Finland |
| Carroll et al 115 |
|
FaecesColonic mucosa | T-RFLP fingerprinting of 16S rRNA - PCR | IBS-D | Diminished microbial biodiversity in faecal samples | USA |
| Parkes et al 116 |
|
Colonic mucosa |
|
IBS | Expansion of mucosa-associated microbiota; mainly bacteroides and clostridia; association with IBS subgroups and symptoms | UK |
| Jeffery et al 117 |
|
Faeces | Pyrosequencing 16SrRNA | Clustering of IBS patients—normal-like versus abnormal microbiota composition (increased ratio of Firmicutes to Bacteroidetes); association with symptom profile | Sweden |
n, number of randomised subjects.
B, Bifidobacterium; C, constipation; C, Clostridium; Cl, Clostridium; ctrls, controls; D, diarrhoea; DGGE, denaturing gradient gel electrophoresis; FISH, fluorescent in situ hybridisation; IBS, irritable bowel syndrome; L, Lactobacillus; qPCR, quantitative PCR;R, Ruminococcus; S, Staphylococcus; T-RFLP, terminal restriction fragment length polymorphism.
The finding that IBS can develop following infective gastroenteritis prompted studies evaluating the role of inflammation in IBS, but there are fewer studies that focus on the associated changes in gut microbiota, which might be just as significant. Infective gastroenteritis produces a profound depletion of the commensal microbiota,118 whose production of metabolites such as SCFAs and antibiotics normally inhibits pathogen colonisation, as can be seen from the loss of colonisation resistance after antibiotics.119 It is unclear just how completely and over what time span recovery occurs.
Infective gastroenteritis is common, with an incidence of 19/100 person years in the UK.120 A third of episodes are viral (Norovirus/Rotavirus being the commonest). The commonest bacterial infections, Campylobacter and Salmonella, account for 10% and 3%, respectively. Onset of new IBS symptoms after a bout of infective gastroenteritis is relatively common, reported by 6%–17% of IBS patients,121 while a recent internet survey reported 18%,122 with around 40% beginning while travelling. The clinical features of post-infectious-IBS are predominantly those of IBS-diarrhoea (IBS-D).123 124 A recent meta-analysis pooling 18 studies indicated a relative increased risk of developing IBS 1 year after bacterial gastroenteritis (mostly Shigella, Campylobacter and Salmonella), RR=6.5 CI (2.6–15.4), an effect still apparent at 36 months, RR=3.9 (3.0–5.0).125 Viral gastroenteritis, in keeping with the lesser tissue injury, shows a reduced incidence of post-infectious-IBScompared with bacterial infections126 127 in which the strongest risk factors are bacterial toxicity,128 prolonged duration of diarrhoea,124 rectal bleeding129 and fever.125 Acute enteritis is associated with a prolonged increase in mucosal cytotoxic T lymphocytes and increase in enteroendocrine cells.123 Other studies have shown the importance of increased 5HT containing cells in IBS-D130 and increased sensitivity in IBS-D with increased EC cell counts,131 accelerated gut transit and visceral hypersensitivity.132 These effects on gut physiology will impact on the gut microbiota environment. An early study of children with acute gastroenteritis demonstrated alkalinisation of stool pH, likely due to the decrease in bacterial metabolites (SCFAs) and a fall in numbers of Bacteroides, Bifidobacterium, Lactobacillus and Eubacterium.133 Conventional enumeration of faecal bacteria showed a 10-fold fall in anaerobes (Bacteroidaceae and Eubacterium), little change in aerobes, but 109 cfu/g of pathogens. Another study using conventional culture methods showed a reversal of the normal anaerobe/aerobe dominance during acute infection.134 More recent human studies using modern culture-independent methods tended to confirm these findings.135 136 PCR-denaturing gradient gel electrophoresis profiling of 16S rRNA genes showed a reduced diversity, often associated with a dominant band suggesting overgrowth of one subtype, which may not always be the original pathogen. A recent clinical trial of an oral rehydration solution containing a prebiotic, amylase resistant starch in acute diarrhoea in India, including children aged 3 months to 5 years, used PCR primers directed at selected bacteria, for example, Eubacterium spp. and Faecalibacterium prausnitzii, key bacteria involved in starch fermentation. These studies showed a decline in some anaerobes (Bacteroides spp., Eubacterium spp. and Faecalibacterium prausnitzii) while other genera including Bifidobacterium spp. were unchanged.135 This depletion of anaerobes could be due to acceleration of transit, which could lead to a loss of the anaerobic niche. Since these are the key bacteria involved in colonic salvage of unabsorbed carbohydrate,137 this may also contribute to the diarrhoea phenotype by preventing fermentation to SCFAs, which are known to stimulate colonic salt and water absorption, both directly and by inducing increased expression of transporters.138–140 Previous earlier studies in IBS-D suggest impaired SCFA concentrations and production rates in ex vivo incubation, which may also reflect reduced anaerobes.141
Another cause of depletion of anaerobes is broad-spectrum antibiotics. There are no RCTs, but epidemiological studies show an association between antibiotic use and an increased risk of PI-IBS.142 A study of children showed that 3 months after Salmonella infection, vomiting, abdominal pain and diarrhoea were reported by 9.5% of those treated with antibiotics but only 2.9% of those who received no antibiotics.142
Changes in the interaction between intestinal microbiota and host factors (eg, age, diet, transit, host genetic factors, antibiotics) could be important for IBS pathophysiology. These factors, in turn, could be related to changes in homeostatic pathways including barrier function, neuromotor sensory function and the brain–gut axis.143 144 For example, bidirectional signalling between the microbiota and the epithelium regulates epithelial secretion of mucus as well as other defence factors involved in regulating the microbiota. Changes in these factors (eg, changes in mucus layer and increased β-defensin-2 peptide) have been detected in patients with IBS and functional diarrhoea and suggest a microbiota–host immune system engagement.145 146 In line with this concept, there is also recent demonstration that IBS patients have increased colonic mucosal expression of receptors recognising specific microbiota-related substances (such as Toll-like receptor-4 which recognises bacterial lipopolysaccharides)147 or increased titres of circulating antibodies against components of the indigenous microbiota (ie, antiflagellin antibodies).148 Several studies demonstrated low-grade activation of innate and adaptive mucosal immune response in large subgroups of patients with IBS.12 149 Increased activated mast cells, CD3+ve, CD4+ve and CD8+ve T cells have been detected in both postinfectious IBS and non-specific IBS.12 149 The relative importance of mast cells in this setting is demonstrated by the abundance of this immune cell type over other immunocytes and by increased release from mucosal biopsies of histamine, tryptase and prostaglandins.150 151 Mast cells were located in closer vicinity to mucosal innervation and correlated with the severity and frequency of abdominal pain in patients with IBS.152 There are potential implications of mucosal immune activation for sensorimotor dysfunction of patients with IBS. Histamine and tryptase released from mucosal biopsies of patients with IBS evoked increased mesenteric sensory afferent activation and induced visceral hyspersensitivity via histamine-1 receptors and proteinase activated-2 receptors when applied to recipient rats.150 151 Intestinal microbiota may well be an active participant in this scenario through stimulation of the immune system,153 likely in the subgroup of subjects showing increased epithelial permeability which could154 expose the immune system to an abnormal microbial antigenic load. Overall, the results suggest that bacterial–host interactions may be initiated by components of the microbiota that can cross the mucus and adhere to epithelial cells, inducing activation of the mucosal innate defence system even in the absence of mucosal destruction.
The use of probiotics, particularly in animal models, also demonstrates that their secreted products or metabolites can modulate contractility of intestinal smooth muscle and visceral sensitivity.59–61 Moreover, application of probiotics can recover neuromotor-sensory dysfunction in IBS-like models.
Modulation of the brain–gut axis is particularly relevant in IBS because psychological comorbidity is common. Some forms of psychological stress in animal studies can induce shifts in the bacterial composition of the gut that is accompanied by systemic cytokine response and increased intestinal permeability.155 The interplay may be bidirectional as suggested by animal studies showing that the microbiota can affect brain chemistry and behaviour.156 Nonetheless, for the time, the potential relevance of brain–microbiota interactions have yet to be shown in humans in general and in FBD in particular.
GI disorders mimicking and overlapping with FBDs
Although celiac disease, IBD or diverticulitis can coexist with IBS, an ‘IBS’ diagnosis in the presence of an organic disease may be challenging.
Gluten causes coeliac disease in genetically susceptible people and causes gut dysfunction in mice and can generate IBS symptoms in the absence of coeliac disease.157 Some patients with IBS lack tissue transglutaminase antibodies or histological markers of coeliac disease yet still respond symptomatically to a gluten-free diet. This entity is termed ‘non-coeliac gluten sensitivity’ or ‘gluten sensitive IBS’.157–159 The underlying mechanisms in humans remain unclear. Mouse models indicate that gluten can induce activation of innate immunity, increased small intestinal permeability,160 neuro-muscular dysfunction159 and dysbiosis161 in the absence of autoimmunity.
IBS-like symptoms are common in IBD patients in long-standing remission, or are frequently reported in patients before the diagnosis of IBD.162 163 It is possible that IBS and IBD coexist with a higher than expected frequency, or may exist on a continuum, with IBS and IBD at different ends of the inflammatory spectrum. A study investigating IBS symptoms in IBD patients who were thought to be in clinical remission demonstrated high levels of calprotectin levels; this suggests that in most cases IBS symptoms are the result of undetected ongoing inflammation.164 Underlying mechanistic links are lacking but it is tempting to raise the hypothesis that the intestinal microbiota may be a common factor in both diseases.165 In fact, as with IBS (tables 2 and 3), faecal166–171 and mucosal-associated dysbiosis167 172–178 has been described IBD.
A high proportion of patients hospitalised with acute diverticulitis continue to have persistent symptoms that mimic IBS179 despite the absence of complications.180 Some uncontrolled studies claim benefit from antibiotics and/or mesalazine suggesting a role for the microbiota in this syndrome.181
Treatment implications: antibiotics, probiotics, prebiotics and synbiotics
As the microbiota may be disturbed in functional GI disorders, a potential treatment approach is to try to correct dysbiosis either by the administration of an antibiotic or a preparation of ‘beneficial’ bacteria (box 3).
Box 3 Modulation of intestinal microbiota in functional bowel disorders.
A short course of a non-absorbable antibiotic such as rifaximin has been shown to moderately improve the symptoms of irritable bowel syndrome (IBS), particularly bloating and flatulence. Improvement persists after the cessation of treatment but the exact duration of this effect remains uncertain.
The majority of trials of probiotics in IBS show some degree of efficacy although some of the early studies were of very poor quality.
Prebiotics and synbiotics should theoretically have the potential in treating functional gastrointestinal disorders but there are as yet no reliable data to support this view.
Antibiotics
Despite evidence that previous antibiotic use may be related to the development of IBS,182 183 and the fact that antibiotic treatment may increase the development of long-term digestive symptoms after bacterial gastroenteritis,142 poorly absorbable antibiotics might still have therapeutic potential in this condition.184 Neomycin was the original choice184 185 although interest is now focused on a non-absorbed derivative of rifampicin called rifaximin.186
There are three fully-published, double blind, placebo controlled trials of rifaximin in FBD187–189 and the data suggest an improvement in symptoms, especially bloating and flatulence for approximately 10 weeks following treatment187 189 with a therapeutic advantage over placebo around 10%. The doses used in these and other studies vary between 600 and 2400 mg daily for 7–14 days190–195 but there remain concerns about antibiotic resistance and possible Clostridium difficile infection although so far these issues have not appeared to be a problem.196–200
Thus, a short course of gut-specific antibiotics may have utility in some patients with IBS but we need to know more about predictors of treatment responsiveness, antibiotic resistance, the efficacy and safety of re-treatment schedules as well as the optimal dosing regimen.201 202
Probiotics
Probiotics are live microorganisms which when administered in adequate amounts confer a health benefit on the host203 with the most commonly used being the lactobacilli and bifidobacteria. Probiotics can be packaged in many formulations containing just one organism or a mixture and have a wide range of activities with evidence supporting an effect on at least some of the putative pathophysiological mechanisms implicated in IBS, such as visceral hypersensitivity,59 60 204 205 GI dysmotility,206–210 intestinal permeability,204 211 212 the intestinal microbiota213 214 and immune function215 although these effects can differ considerably between one organism and another. Thus, just because one organism is beneficial, this does not mean that related organisms will behave similarly. For use in gastroenterology, it is important that a preparation contains sufficient quantities of microbes which need to be acid and enzyme resistant with good mucosal adherence also being an advantage.
Table 4 lists the results of the fully published placebo controlled probiotic trials to date.208–210 212 214–240 Unfortunately, their designs vary considerably;241–244 some of the older studies are of poor quality, and few attempt to define the mechanism of action or assess whether symptomatic improvement is accompanied by a change in the microbiota. A recent systematic review reported that studies of poorer quality tended to show larger effects and published data indicate a publication bias, with non-reporting of negative effects in small trials.244 Around three-quarters of these studies were positive, of which four were in children, although different symptoms improved and the therapeutic gain over placebo was generally modest. Furthermore, it remains unclear which organisms are most effective as, for instance, some mainly reduce bloating and flatulence,209 210 218 whereas others improve bowel frequency,222 and some have a positive effect on global symptom scores.214 215 224 226 229 230 233 In some of the better quality trials bifidobacteria, such as Bifidobacterium infantis 35624,215 224 241 Bifidobacterium lactis DN 173010208 225 and Bifidobacterium bifidum MIMBb75,226 seem to be advantageous and in others probiotic mixtures appear to be useful.214 229 233 In only one study was there symptom deterioration221 although some large, high quality trials have been negative.221 231 234 235
Table 4.
Placebo controlled clinical trials of single or mixed probiotic preparations in IBS
| Organism | n | Outcome | Reference |
| Studies in adult patients | |||
| S faecium | 54 | ↓ Global score | Gade et al 216 |
| Lactobacillus acidophilus | 18 | ↓ Global score | Halpern et al 217 |
| Lactobacillus plantarum 299V | 60 | ↓ Flatulence | Nobaek et al 218 |
| L plantarum 299V | 20 | ↓ Pain, ‘all IBS symptoms’ | Niedzielin et al 219 |
| L plantarum 299V | 12 | Negative | Sen et al 220 |
| L plantarum MF1298 | 16 | Deterioration of symptoms | Ligaarden et al 221 |
| L ramnosus GG | 25 | Negative | O'Sullivan et al 240 |
| L reuterii ATCC 55730 | 54 | Negative | Niv et al 223 |
| L salivarius UCC4331 | 75 | Negative | O'Mahony et al 215 |
| Bifidobacterium infantis 35624 | 75 | ↓ Pain and composite score | O'Mahony et al 215 |
| B infantis 35624 | 362 | ↓ Pain and composite score | Whorwell et al 224 |
| B ifidobacterium lactis DN-173-010 | 274 | ↓ Digestive discomfort | Guyonnet et al 225 |
| B lactis DN-173-010 | 34 | ↓ Maximum distension & pain | Agrawal et al 208 |
| B ifidobacterium bifidum MIMBb75 | 122 | ↓ Global score | Guglielmetti et al 226 |
| Bacillus coagulans GBI-30, 6086 | 52 | ↓ Bowel movements | Dolin222 |
| Escherichia coli Nissle 1917 | 120 | ↑ Treatment satisfaction | Kruis et al 227 |
| VSL#3® (x8)* | 25 | ↓ Bloating | Kim et al 209 |
| VSL#3® (x8)* | 48 | ↓ Flatulence | Kim et al 210 |
| Medilac DS® (x2)* | 40 | ↓ Pain | Kim et al 228 |
| Mixture (x4)* | 103 | ↓ Global score | Kajander et al 229 |
| Mixture (x4)* | 86 | ↓ Global score | Kajander et al 214 |
| LAB4 (x4)* | 52 | ↓ Global score | Williams et al 230 |
| Mixture (x4)* | 106 | Negative | Drouault-Holowacz et al 231 |
| Mixture (x2)* | 40 | ↓ Pain | Sinn et al 232 |
| ProSymbioFlor® (x2)* | 297 | ↓ Global score | Enck et al 233 |
| Cultura® (x3)* | 74 | Negative | Simrén et al 234 |
| Cultura® (x3)* | 52 | Negative | Sondergaard et al 235 |
| Mixture (x4)* | 70 | ↓ Pain | Hong et al 236 |
| Studies in paediatric patients | |||
| L ramnosus GG | 50 | ↓ Abdominal distension | Bausserman and Michail237 |
| L ramnosus GG | 104 | ↓ Pain | Gawronska et al 238 |
| L ramnosus GG | 141 | ↓ Pain | Francavilla et al 212 |
| VSL#3® (x8)* | 59 | ↓ Global score | Guandalini et al 239 |
*Number of organisms in a mixture.
n, number of randomised subjects.
IBS, irritable bowel syndrome; L ramnosus, Lactobacillus ramnosus; L reuterii, Lactobacillus reuterii; L salivarius, Lactobacillus salivarius; S faecium, Streptococcus faecium.
Diet, fibre, prebiotics and synbiotics
There are few proper randomised, placebo controlled trials of diet modification because of the difficulty in controlling for the placebo effect. One randomised controlled trial showed bran aggravated symptoms;245 excluding bran should help, and many patients believe this is true.246 A prebiotic is a product that, on ingestion, stimulates the growth of beneficial bacteria already present in the host, which promotes the health of the individual.247 248 A variety of oligosaccharides serve this function and a synbiotic is a combined prebiotic and probiotic. One of the earliest prebiotics was lactulose, an unabsorbable disaccharide laxative that increases the faecal concentrations of Bifidobacterium spp.45 249 as does inulin which, like lactulose, increases flatulence47 and thus makes it unlikely it will help IBS patients.
To date, there has only been one double blind, placebo controlled trial of a prebiotic in IBS which used a trans-galactooligosaccharide mixture.250 Compared with placebo this prebiotic reduced symptoms and stimulated the growth of bifidobacteria but clearly more research is required on dosing and the relative merits of other compounds. With regard to synbiotics, there are some studies but their design is not sufficiently robust to draw any firm conclusions251–255 although the concept of combining a prebiotic and probiotic is theoretically attractive. Thus, attempting to modify the microbiota in patients with functional GI disorders shows some promise. However, we need to know how symptomatic improvement is achieved: is it mirrored by a change in gut microbiota or is some other mechanism involved?
Clinical guidance regarding modulation of intestinal microbiota in IBS
While the science regarding the role of microbiota in FGIDs remains in its infancy, patients are exposed to conflicting claims concerning the symptomatic benefit from modulating gut microbiota. This section aims to help clinicians give the best advice, despite limited evidence (box 4).
Box 4 Diagnostic and therapeutic general recommendations.
There is currently no clinically useful way of identifying whether the microbiota are disturbed in particular patients with irritable bowel syndrome (IBS).
Dietary evaluation and exclusion of possible sources of unabsorbable carbohydrates including fermentable oligo-, di- and mono-saccharides and polyols and excessive fibre could be beneficial in select patients.
Probiotics have a reasonable evidence base and should be tried, for a period of at least 1 month, at adequate doses before a judgement is made about the response to treatment.
The utility of testing for small intestinal bacterial overgrowth (SIBO) in the setting of IBS remains an area of uncertainty.
If SIBO is strongly suspected based on clinical presentation and testing is being considered, using stringent criteria for the glucose breath test or jejunal aspirate appear to be the best tests.
Consideration should be given to discontinuing proton pump inhibitors in those with SIBO.
There is emerging evidence that non-absorbable antibiotics may have the potential to reduce symptoms in some patients with IBS.
Diet profoundly alters the microbiota. Reducing intake of fibre256 or FODMAPs257 is one of the simplest and safest ways of altering gut microbiota, which can lead to improvement in bloating and diarrhoea, an effect which may last for years.258 However, so far the evidence to support widespread use of FODMAP reduction in patients with IBS is limited and comes mainly from one research group. Systematic exclusion diets may also help258 but are laborious; targeted exclusion of regularly consumed suspects, such as dairy, wheat, fruit and vegetables, may be more practical.
The safety of probiotics in IBS is acceptable but some aggravate symptoms221 and so patients should be warned of this possibility. At present, the strongest evidence is for Bifidobacterium infantis 35624 at a dose of 1×108 cfu/day taken for at least 4 weeks.224 It remains unclear who benefits from which variety of probiotic since there are many incompletely answered questions surrounding this therapeutic approach, including:
Are single organisms better than mixtures or vice versa?
Do some mixtures of organisms contain strains that are competitive or antagonistic without additive effects?
Can probiotic foods and drinks be administered simultaneously?
What are the best delivery systems—liquids or capsules?
How can viability and bioavailability be ensured?
What are the optimal dosing regimens and their duration?
What is the frequency of host colonisation?
Probiotics are not potent pharmacological agents: what patient group should be targeted?
Are there any groups of patients where probiotics might be contraindicated such as newborns, immunocompromised or seriously ill individuals?
Are there any safety issues about some strains of probiotics, for example, those of Escherichia coli?
Should different probiotics be given to specific subgroups of IBS patients?
Which symptoms of IBS should be the main target for therapy?
What are the possible mechanisms behind symptom improvement?
How should doctors and patients be advised about their administration?
The considerable acid suppression induced by PPIs may alter upper gut microbiota and can potentially induce IBS symptoms.92 Thus, it is worth considering PPI discontinuation in selected IBS patients on PPIs for unclear reasons, especially if their symptoms started with PPI therapy.
The most direct way of altering gut microbiota is to use broad-spectrum antibiotics. However, rapid development of antibiotic resistance leads to concerns about using antibiotics in such a ubiquitous and chronic condition. Moreover, it is likely that patients may require repeated courses of therapy, as trial evidence suggests the benefit diminishes by 12 weeks.189 The best evidence is for rifaximin 550 mg, thrice daily for 2 weeks.189 The number-needed-to-treat was 11 which should be compared with 4 for ‘placebo without deception,259 7 for alosetron,260 8 for linaclotide261 and 14 for tegaserod.262
Although rifaximin appears to be well tolerated and safe, given its relatively low potency its use should be restricted to difficult cases since its widespread use could promote resistance, such as rifampin-resistant strains of stapyholococci.196 Figure 4 provides a plot chart of currently available strategies for modifying gut microbiota according to the effectiveness and invasiveness of the proposed approach, and general recommendations appear in box 4.
Conclusions and recommendations for future research and development
Although there is good evidence supporting the concept that the intestinal microbiota is perturbed in patients with FBD, we still lack data on the mechanisms through which host–microbiota interactions underlie pathophysiology and generate symptoms; we need to overcome several boundaries that hold back our knowledge in this field.
The SIBO hypothesis in IBS remains a matter of debate because the breath tests and the small bowel culture techniques have not been validated. In addition, confounding factors, including the use of antibiotics or PPIs, have not been taken into account in many studies. The wide heterogeneity of FBD and the inter-individual variability of microbiota profiles suggest that larger sample size studies (both in the pathophysiology and therapeutic settings) are of key importance in the future. Attention should be directed to the assessment of correlations between microbiota changes with patient's symptoms. Whenever possible, studies should be stratified by factors known or assumed to affect intestinal microbiota (eg, age, diet, enterotype) and designed to reduce potential confounding factors (eg, antibiotics, probiotics, laxatives, prokinetcs, PPI and mesalazine). Although faecal samples are relatively easy to obtain, future work should better characterise microbial populations at the luminal and mucosal level which may differ substantially from faecal microbiota. Host–microbiota interactions are dynamic events and likely influenced by several factors. This suggests that there is a need for longitudinal studies assessing gut microbiota during remission, and symptom flare-ups, stress, infection or following dietary manipulation and the use of probiotics, prebiotics and antibiotics. The effect of bowel transit on microbiota profiles and correlation with symptoms should also be assessed.
One important limitation of available studies is their descriptive rather than mechanistic nature. Accordingly, studies should be directed at clarifying cause–effect relationships between microbiota changes and bowel dysfunction. In this way, microbiota signatures can be developed to help identify IBS biomarkers which might, in turn, offer therapeutic targets. For example, the theory that luminal bacteria may drive low-grade intestinal immune activation should now be substantiated by mechanistic and interventional studies. Data in rodents suggest the existence of a bidirectional interplay between the brain and gut microbiota.144 In addition, the existence of systemic immune responses to microbial luminal antigens (antiflagellin antibodies)148 provides initial evidence that microbial homeostasis may be perturbed beyond the GI tract. These aspects need to be further explored to open new avenues of research in FBD.
Currently, there are promising results suggesting that a subgroup of patients with FBD may respond favourably to a short course of gut-specific antibiotics. However, most probiotic and antibiotic trials are underpowered and suffer suboptimal design. Bloating and flatulence appear to be especially responsive to non-absorbable antibiotics. In order to safely direct these treatment options to the appropriate patients, we need to know more about predictors of treatment responsiveness, the risk of development of antibiotic resistance, the efficacy and safety of re-treatment schedules, and the optimal dosing regimen.201 202 Further studies should also investigate the mechanism and site of action of non-absorbable antibiotics since amelioration of gas-related symptoms in patients occurred also in patients with no evidence of SIBO.188 Probiotics seem to have a positive, albeit modest, effect in both children and adults with FBD, especially IBS. However, head-to-head comparisons between different probiotic products would be useful and future trials need to be large scale, high-quality and use valid end points. Trials should also explore the mechanisms behind symptom improvement.
Faecal transplantation is efficacious in 145⁄166 (87%) patients with fulminant and refractory C difficile infection. This procedure has also been proposed for the treatment of IBS but further research is needed.263
In conclusion, a better definition of the role of intestinal microbiota in the pathogenesis and pathophysiology of FBD represents a challenge for the future. Although promising, therapeutic implications will need to be better defined in well-conducted, large clinical trials. A strict cooperation of experienced clinical researchers with microbial ecologists should be considered an important factor for the success of these future studies.
Supplementary Material
Acknowledgments
The authors would like to thank Professor Willem de Vos, Professor Eamonn Quigley, Professor Patrizia Brigidi and the Rome Foundation board members for critical revision of the manuscript. We also acknowledge the valuable help of Cesare Cremon in manuscript editing and the expert secretarial support from Emma Bradley.
Footnotes
Contributors: The Working Team was led by MS and GB. All working team members contributed equally to the manuscript.
Funding: This work is supported by Rome Foundation, USA. In addition, the authors would like to acknowledge the following funding sources: Italian Ministry of Education, University and Research (PRIN 2009); Fondazione Cassa di Risparmio and IMA, Bologna, Italy (GB); Scottish government RESAS support (HJF); The Swedish Medical Research Council (grants 13409, 21691 and 21692), the Marianne and Marcus Wallenberg Foundation, and the University of Gothenburg, Centre for Person-Centred Care (GPCC), Sahlgrenska Academy, University of Gothenburg and by the Faculty of Medicine, University of Gothenburg (MS); Shire/Movetis, Amgen, Ironwood (BS); Canadian Institute of Health Research (CIHR) and Crohn's and Colitis Foundation of Canada (CCFC) (SV); Lesaffre International, Norgine, National Institute for Health Research Biomedical Research Unit Grant (RS); CAG/CIHR, CCA (Canadian Celiac Association), CCFC and Nestec (EFV); EFV holds a Career Award from the Department of Medicine, McMaster University.
Competing interests: This is a Rome Working Team Report. All authors are responsible for writing the study interpretation of data, and critical revision of the manuscript. The authors would like to disclose the following potential competing interests: Alfa-Wasserman, Prometheus, Shire/Movetis, Sofar (GB); Danone Research, Arla Foods, Novartis, Shire/Movetis, AstraZeneca (MS); Ironwood, Shire/Movetis, Prometheus (BS); Boeringer Ingelheim & Ironwood (RS); Ferring Canada and US (SV); Nestec grant support (EFV); Novartis Pharmaceuticals, GlaxoSmithKline, Solvay Pharmaceuticals, Pfizer Global Research and Development, Rotta Research, Proctor and Gamble, Danone Research, Astellas Pharma, Ironwood Pharmaceuticals, Sucampo Pharmaceuticals, Almirall Pharma, Movetis UK, Norgine, Chr Hansen, Boehringer-Ingelheim, and Heel GMBH (PW).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology 2006;130:1377–90 [DOI] [PubMed] [Google Scholar]
- 2. Koloski NA, Talley NJ, Boyce PM. Epidemiology and health care seeking in the functional GI disorders: a population-based study. Am J Gastroenterol 2002;97:2290–9 [DOI] [PubMed] [Google Scholar]
- 3. Belsey J, Greenfield S, Candy D, et al. Systematic review: impact of constipation on quality of life in adults and children. Aliment Pharmacol Ther 2010;31:938–49 [DOI] [PubMed] [Google Scholar]
- 4. Gralnek IM, Hays RD, Kilbourne A, et al. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology 2000;119:654–60 [DOI] [PubMed] [Google Scholar]
- 5. Simren M, Svedlund J, Posserud I, et al. Health-related quality of life in patients attending a gastroenterology outpatient clinic: functional disorders versus organic diseases. Clin Gastroenterol Hepatol 2006;4:187–95 [DOI] [PubMed] [Google Scholar]
- 6. Spiegel BM. The burden of IBS: looking at metrics. Curr Gastroenterol Rep 2009;11:265–9 [DOI] [PubMed] [Google Scholar]
- 7. Hillila MT, Farkkila NJ, Farkkila MA. Societal costs for irritable bowel syndrome–a population based study. Scand J Gastroenterol 2010;45:582–91 [DOI] [PubMed] [Google Scholar]
- 8. Jiang X, Locke GR, Zinsmeister AR, et al. Health care seeking for abdominal bloating and visible distention. Aliment Pharmacol Ther 2009;30:775–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Singh G, Lingala V, Wang H, et al. Use of health care resources and cost of care for adults with constipation. Clin Gastroenterol Hepatol 2007;5:1053–8 [DOI] [PubMed] [Google Scholar]
- 10. Gunnarsson J, Simren M. Peripheral factors in the pathophysiology of irritable bowel syndrome. Dig Liver Dis 2009;41:788–93 [DOI] [PubMed] [Google Scholar]
- 11. Ohman L, Simren M. New insights into the pathogenesis and pathophysiology of irritable bowel syndrome. Dig Liver Dis 2007;39:201–15 [DOI] [PubMed] [Google Scholar]
- 12. Ohman L, Simren M. Pathogenesis of IBS: role of inflammation, immunity and neuroimmune interactions. Nat Rev Gastroenterol Hepatol 2010;7:163–73 [DOI] [PubMed] [Google Scholar]
- 13. Young VB, Schmidt TM. Overview of the gastrointestinal microbiota. Adv Exp Med Biol 2008;635:29–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sekirov I, Russell SL, Antunes LC, et al. Gut microbiota in health and disease. Physiol Rev 2010;90:859–904 [DOI] [PubMed] [Google Scholar]
- 15. O'Hara AM, Shanahan F. The gut flora as a forgotten organ. EMBO Rep 2006;7:688–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Frank DN, St Amand AL, Feldman RA, et al. Molecular-phylogenetic characterisation of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci U S A 2007;104:13780–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Swidsinski A, Loening-Baucke V, Lochs H, et al. Spatial organization of bacterial flora in normal and inflamed intestine: a fluorescence in situ hybridization study in mice. World J Gastroenterol 2005;11:1131–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dethlefsen L, McFall-Ngai M, Relman DA. An ecological and evolutionary perspective on human-microbe mutualism and disease. Nature 2007;449:811–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zoetendal EG, Rajilic-Stojanovic M, de Vos WM. High-throughput diversity and functionality analysis of the gastrointestinal tract microbiota. Gut 2008;57:1605–15 [DOI] [PubMed] [Google Scholar]
- 20. Eckburg PB, Bik EM, Bernstein CN, et al. Diversity of the human intestinal microbial flora. Science 2005;308:1635–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Parkes GC, Brostoff J, Whelan K, et al. Gastrointestinal microbiota in irritable bowel syndrome: their role in its pathogenesis and treatment. Am J Gastroenterol 2008;103:1557–67 [DOI] [PubMed] [Google Scholar]
- 22. Spiller R, Garsed K. Postinfectious irritable bowel syndrome. Gastroenterology 2009;136:1979–88 [DOI] [PubMed] [Google Scholar]
- 23. Quigley EM. Therapies aimed at the gut microbiota and inflammation: antibiotics, prebiotics, probiotics, synbiotics, anti-inflammatory therapies. Gastroenterol Clin North Am 2011;40:207–22 [DOI] [PubMed] [Google Scholar]
- 24. Schmulson M, Chang L. Review article: the treatment of functional abdominal bloating and distension. Aliment Pharmacol Ther 2011;33:1071–86 [DOI] [PubMed] [Google Scholar]
- 25. Ford AC, Spiegel BM, Talley NJ, et al. Small intestinal bacterial overgrowth in irritable bowel syndrome: systematic review and meta-analysis. Clin Gastroenterol Hepatol 2009;7:1279–86 [DOI] [PubMed] [Google Scholar]
- 26. Salonen A, de Vos WM, Palva A. Gastrointestinal microbiota in irritable bowel syndrome: present state and perspectives. Microbiology 2010;156:3205–15 [DOI] [PubMed] [Google Scholar]
- 27. Arumugam M, Raes J, Pelletier E, et al. Enterotypes of the human gut microbiome. Nature 2011;473:174–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carroll IM, Chang YH, Park J, et al. Luminal and mucosal-associated intestinal microbiota in patients with diarrhoea-predominant irritable bowel syndrome. Gut Pathog 2010;2:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dominguez-Bello MG, Costello EK, Contreras M, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A 2010;107:11971–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stark PL, Lee A. The microbial ecology of the large bowel of breast-fed and formula-fed infants during the first year of life. J Med Microbiol 1982;15:189–203 [DOI] [PubMed] [Google Scholar]
- 31. Palmer C, Bik EM, DiGiulio DB, et al. Development of the human infant intestinal microbiota. PLoS Biol 2007;5:e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Balamurugan R, Janardhan HP, George S, et al. Bacterial succession in the colon during childhood and adolescence: molecular studies in a southern Indian village. Am J Clin Nutr 2008;88:1643–7 [DOI] [PubMed] [Google Scholar]
- 33. Enck P, Zimmermann K, Rusch K, et al. The effects of ageing on the colonic bacterial microflora in adults. Z Gastroenterol 2009;47:653–8 [DOI] [PubMed] [Google Scholar]
- 34. Biagi E, Nylund L, Candela M, et al. Through ageing, and beyond: gut microbiota and inflammatory status in seniors and centenarians. PLoS One 2010;5:e10667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. De Filippo C, Cavalieri D, Di Paola M, et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A 2010;107:14691–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Costabile A, Klinder A, Fava F, et al. Whole-grain wheat breakfast cereal has a prebiotic effect on the human gut microbiota: a double-blind, placebo-controlled, crossover study. Br J Nutr 2008;99:110–20 [DOI] [PubMed] [Google Scholar]
- 37. Walker AW, Ince J, Duncan SH, et al. Dominant and diet-responsive groups of bacteria within the human colonic microbiota. ISME J 2011;5:220–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Martinez I, Kim J, Duffy PR, et al. Resistant starches types 2 and 4 have differential effects on the composition of the fecal microbiota in human subjects. PLoS One 2010;5:e15046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Leach ST, Mitchell HM, Eng WR, et al. Sustained modulation of intestinal bacteria by exclusive enteral nutrition used to treat children with Crohn's disease. Aliment Pharmacol Ther 2008;28:724–33 [DOI] [PubMed] [Google Scholar]
- 40. Turnbaugh PJ, Hamady M, Yatsunenko T, et al. A core gut microbiome in obese and lean twins. Nature 2009;457:480–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Schwiertz A, Taras D, Schafer K, et al. Microbiota and SCFA in lean and overweight healthy subjects. Obes (Silver Spring) 2010;18:190–5 [DOI] [PubMed] [Google Scholar]
- 42. Duncan SH, Lobley GE, Holtrop G, et al. Human colonic microbiota associated with diet, obesity and weight loss. Int J Obes (Lond) 2008;32:1720–4 [DOI] [PubMed] [Google Scholar]
- 43. Lewis S, Burmeister S, Brazier J. Effect of the prebiotic oligofructose on relapse of Clostridium difficile-associated diarrhea: a randomised, controlled study. Clin Gastroenterol Hepatol 2005;3:442–8 [DOI] [PubMed] [Google Scholar]
- 44. Bouhnik Y, Attar A, Joly FA, et al. Lactulose ingestion increases faecal bifidobacterial counts: a randomised double-blind study in healthy humans. Eur J Clin Nutr 2004;58:462–6 [DOI] [PubMed] [Google Scholar]
- 45. Bouhnik Y, Neut C, Raskine L, et al. Prospective, randomised, parallel-group trial to evaluate the effects of lactulose and polyethylene glycol-4000 on colonic flora in chronic idiopathic constipation. Aliment Pharmacol Ther 2004;19:889–99 [DOI] [PubMed] [Google Scholar]
- 46. Smith SC, Choy R, Johnson SK, et al. Lupin kernel fiber consumption modifies fecal microbiota in healthy men as determined by rRNA gene fluorescent in situ hybridization. Eur J Nutr 2006;45:335–41 [DOI] [PubMed] [Google Scholar]
- 47. Ramnani P, Gaudier E, Bingham M, et al. Prebiotic effect of fruit and vegetable shots containing Jerusalem artichoke inulin: a human intervention study. Br J Nutr 2010;104:233–40 [DOI] [PubMed] [Google Scholar]
- 48. Cloetens L, Broekaert WF, Delaedt Y, et al. Tolerance of arabinoxylan-oligosaccharides and their prebiotic activity in healthy subjects: a randomised, placebo-controlled cross-over study. Br J Nutr 2010;103:703–13 [DOI] [PubMed] [Google Scholar]
- 49. Lewis S, Cochrane S. Alteration of sulfate and hydrogen metabolism in the human colon by changing intestinal transit rate. Am J Gastroenterol 2007;102:624–33 [DOI] [PubMed] [Google Scholar]
- 50. Oufir LE, Barry JL, Flourie B, et al. Relationships between transit time in man and in vitro fermentation of dietary fiber by fecal bacteria. Eur J Clin Nutr 2000;54:603–9 [DOI] [PubMed] [Google Scholar]
- 51. Kamath PS, Phillips SF, Zinsmeister AR. Short-chain fatty acids stimulate ileal motility in humans. Gastroenterology 1988;95:1496–502 [DOI] [PubMed] [Google Scholar]
- 52. Macpherson AJ, Uhr T. Induction of protective IgA by intestinal dendritic cells carrying commensal bacteria. Science 2004;303:1662–5 [DOI] [PubMed] [Google Scholar]
- 53. Tlaskalova-Hogenova H, Stepankova R, Hudcovic T, et al. Commensal bacteria (normal microflora), mucosal immunity and chronic inflammatory and autoimmune diseases. Immunol Lett 2004;93:97–108 [DOI] [PubMed] [Google Scholar]
- 54. Shroff KE, Meslin K, Cebra JJ. Commensal enteric bacteria engender a self-limiting humoral mucosal immune response while permanently colonizing the gut. Infect Immun 1995;63:3904–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Crabbe PA, Nash DR, Bazin H, et al. Immunohistochemical observations on lymphoid tissues from conventional and germ-free mice. Lab Invest 1970;22:448–57 [PubMed] [Google Scholar]
- 56. Helgeland L, Dissen E, Dai KZ, et al. Microbial colonization induces oligoclonal expansions of intraepithelial CD8 T cells in the gut. Eur J Immunol 2004;34:3389–400 [DOI] [PubMed] [Google Scholar]
- 57. Zoetendal EG, Akkermans AD, Akkermans-van Vliet WM, et al. The host genotype affects the bacterial community in the human gastrointestinal tract. Microb Ecol Health Dis 2001;13:129–34 [Google Scholar]
- 58. Petnicki-Ocwieja T, Hrncir T, Liu YJ, et al. Nod2 is required for the regulation of commensal microbiota in the intestine. Proc Natl Acad Sci U S A 2009;106:15813–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Verdu EF, Bercik P, Verma-Gandhu M, et al. Specific probiotic therapy attenuates antibiotic induced visceral hypersensitivity in mice. Gut 2006;55:182–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Rousseaux C, Thuru X, Gelot A, et al. Lactobacillus acidophilus modulates intestinal pain and induces opioid and cannabinoid receptors. Nat Med 2007;13:35–7 [DOI] [PubMed] [Google Scholar]
- 61. Eutamene H, Lamine F, Chabo C, et al. Synergy between Lactobacillus paracasei and its bacterial products to counteract stress-induced gut permeability and sensitivity increase in rats. J Nutr 2007;137:1901–7 [DOI] [PubMed] [Google Scholar]
- 62. Bercik P, Denou E, Collins J, et al. The intestinal microbiota affect central levels of brain-derived neurotropic factor and behavior in mice. Gastroenterology 2011;141:599–609, e1–3. [DOI] [PubMed] [Google Scholar]
- 63. Moore WE, Moore LH. Intestinal floras of populations that have a high risk of colon cancer. Appl Environ Microbiol 1995;61:3202–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Suau A, Bonnet R, Sutren M, et al. Direct analysis of genes encoding 16S rRNA from complex communities reveals many novel molecular species within the human gut. Appl Environ Microbiol 1999;65:4799–807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Zoetendal EG, Akkermans AD, De Vos WM. Temperature gradient gel electrophoresis analysis of 16S rRNA from human fecal samples reveals stable and host-specific communities of active bacteria. Appl Environ Microbiol 1998;64:3854–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Andersson AF, Lindberg M, Jakobsson H, et al. Comparative analysis of human gut microbiota by barcoded pyrosequencing. PLoS One 2008;3:e2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Rajilic-Stojanovic M, Heilig HG, Molenaar D, et al. Development and application of the human intestinal tract chip, a phylogenetic microarray: analysis of universally conserved phylotypes in the abundant microbiota of young and elderly adults. Environ Microbiol 2009;11:1736–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Nelson KE, Weinstock GM, Highlander SK, et al. ; Human Microbiome Jumpstart Reference Strains Consortium A catalog of reference genomes from the human microbiome. Science 2010;328:994–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kurokawa K, Itoh T, Kuwahara T, et al. Comparative metagenomics revealed commonly enriched gene sets in human gut microbiomes. DNA Res 2007;14:169–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Qin J, Li R, Raes J, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 2010;464:59–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Klaassens ES, de Vos WM, Vaughan EE. A metaproteomics approach to study the functionality of the microbiota in the human infant gastrointestinal tract. Appl Environ Microbiol 2007;73:1388–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Gosalbes MJ, Durbán A, Pignatelli M, et al. Metatranscriptomic approach to analyze the functional human gut microbiota. PLoS One 2011;6:e17447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Verberkmoes NC, Russell AL, Shah M, et al. Shotgun metaproteomics of the human distal gut microbiota. ISME J 2009;3:179–89 [DOI] [PubMed] [Google Scholar]
- 74. Rooijers K, Kolmeder C, Juste C, et al. An iterative workflow for mining the human intestinal metaproteome. BMC Genomics 2011;12:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Gasbarrini A, Corazza GR, Gasbarrini G, et al. Methodology and indications of H2-breath testing in gastrointestinal diseases: the Rome Consensus Conference. Aliment Pharmacol Ther 2009;29(Suppl 1):1–49 [DOI] [PubMed] [Google Scholar]
- 76. Drasar BS, Shiner M. Studies on the intestinal flora. II. Bacterial flora of the small intestine in patients with gastrointestinal disorders. Gut 1969;10:812–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Rumessen JJ, Gudmand-Hoyer E, Bachmann E, et al. Diagnosis of bacterial overgrowth of the small intestine. Comparison of the 14C-D-xylose breath test and jejunal cultures in 60 patients. Scand J Gastroenterol 1985;20:1267–75 [DOI] [PubMed] [Google Scholar]
- 78. Corazza GR, Menozzi MG, Strocchi A, et al. The diagnosis of small bowel bacterial overgrowth. Reliability of jejunal culture and inadequacy of breath hydrogen testing. Gastroenterology 1990;98:302–9 [DOI] [PubMed] [Google Scholar]
- 79. Bardhan PK, Gyr K, Beglinger C, et al. Diagnosis of bacterial overgrowth after culturing proximal small-bowel aspirate obtained during routine upper gastrointestinal endoscopy. Scand J Gastroenterol 1992;27:253–6 [DOI] [PubMed] [Google Scholar]
- 80. Lewis SJ, Young G, Mann M, et al. Improvement in specificity of [14C]d-xylose breath test for bacterial overgrowth. Dig Dis Sci 1997;42:1587–92 [DOI] [PubMed] [Google Scholar]
- 81. Sullivan A, Tornblom H, Lindberg G, et al. The micro-flora of the small bowel in health and disease. Anaerobe 2003;9:11–14 [DOI] [PubMed] [Google Scholar]
- 82. Posserud I, Stotzer PO, Bjornsson ES, et al. Small intestinal bacterial overgrowth in patients with irritable bowel syndrome. Gut 2007;56:802–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Kerckhoffs AP, Visser MR, Samsom M, et al. Critical evaluation of diagnosing bacterial overgrowth in the proximal small intestine. J Clin Gastroenterol 2008;42:1095–102 [DOI] [PubMed] [Google Scholar]
- 84. Choung RS, Ruff KC, Malhotra A, et al. Clinical predictors of small intestinal bacterial overgrowth by duodenal aspirate culture. Aliment Pharmacol Ther 2011;33:1059–67 [DOI] [PubMed] [Google Scholar]
- 85. Pyleris M, Giamarellos-Bourboulis EJ, Koussoulas B, et al. Small bowel culture confirms the presence of small intestinal bacterial overgrowth in a Subset of IBS subjects. Gastroenterology 2011;140:S-152. [Google Scholar]
- 86. Booijink CCGM, El-Aidy S, Rajilić-Stojanović M, et al. High temporal and inter-individual variation detected in the human ileal microbiota. Environ Microbiol 2010;12:3213–27 [DOI] [PubMed] [Google Scholar]
- 87. Guschin DY MB, Proudnikov D, Stahl DA, et al. Oligonucleotide microchips as genosensors for determinative and environmental studies in microbiology. Appl Environ Microbiol 1997;63:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Ahmed S, Macfarlane GT, Fite A, et al. Mucosa-associated bacterial diversity in relation to human terminal ileum and colonic biopsy samples. Appl Environ Microbiol 2007;73:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Zoetendal EG, Raes J, van den Bogert B, et al. The human small intestinal microbiota is driven by rapid uptake and conversion of simple carbohydrates. ISME J. Published Online First: 19 January 2012. doi:10.1038/ismej.2011.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Vanner S. The small intestinal bacterial overgrowth. Irritable bowel syndrome hypothesis: implications for treatment. Gut 2008;57:1315–21 [DOI] [PubMed] [Google Scholar]
- 91. Khoshini R, Dai SC, Lezcano S, et al. A systematic review of diagnostic tests for small intestinal bacterial overgrowth. Dig Dis Sci 2008;53:1443–54 [DOI] [PubMed] [Google Scholar]
- 92. Compare D, Pica L, Rocco A, et al. Effects of long-term PPI treatment on producing bowel symptoms and SIBO. Eur J Clin Invest 2011;41:380–6 [DOI] [PubMed] [Google Scholar]
- 93. Lombardo L, Foti M, Ruggia O, et al. Increased incidence of small intestinal bacterial overgrowth during proton pump inhibitor therapy. Clin Gastroenterol Hepatol 2010;8:504–8 [DOI] [PubMed] [Google Scholar]
- 94. Yu D, Cheeseman F, Vanner S. Combined oro-caecal scintigraphy and lactulose hydrogen breath testing demonstrate that breath testing detects oro-caecal transit, not small intestinal bacterial overgrowth in patients with IBS. Gut 2011;60:334–40 [DOI] [PubMed] [Google Scholar]
- 95. Law D, Pimentel M. Proton pump inhibitor therapy does not affect hydrogen production on lactulose breath test in subjects with IBS. Dig Dis Sci 2010;55:2302–8 [DOI] [PubMed] [Google Scholar]
- 96. Balsari A, Ceccarelli A, Dubini F, et al. The fecal microbial population in the irritable bowel syndrome. Microbiologica 1982;5:185–94 [PubMed] [Google Scholar]
- 97. Wyatt GM, Bayliss CE, Lakey AF, et al. The faecal flora of two patients with food-related irritable bowel syndrome during challenge with symptom-provoking foods. J Med Microbiol 1988;26:295–9 [DOI] [PubMed] [Google Scholar]
- 98. Si JM, Yu YC, Fan YJ, et al. Intestinal microecology and quality of life in irritable bowel syndrome patients. World J Gastroenterol 2004;10:1802–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Malinen E, Rinttila T, Kajander K, et al. Analysis of the fecal microbiota of irritable bowel syndrome patients and healthy controls with real-time PCR. Am J Gastroenterol 2005;100:373–82 [DOI] [PubMed] [Google Scholar]
- 100. Matto J, Maunuksela L, Kajander K, et al. Composition and temporal stability of gastrointestinal microbiota in irritable bowel syndrome–a longitudinal study in IBS and control subjects. FEMS Immunol Med Microbiol 2005;43:213–22 [DOI] [PubMed] [Google Scholar]
- 101. Maukonen J, Satokari R, Matto J, et al. Prevalence and temporal stability of selected clostridial groups in irritable bowel syndrome in relation to predominant faecal bacteria. J Med Microbiol 2006;55:625–33 [DOI] [PubMed] [Google Scholar]
- 102. Kassinen A, Krogius-Kurikka L, Makivuokko H, et al. The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects. Gastroenterology 2007;133:24–33 [DOI] [PubMed] [Google Scholar]
- 103. Rajilic-Stojanovic M. Diversity of the Human Gastrointestinal Microbiota: Novel Perspectives from High Throughput Analyses. Wageningen, The Netherlands: Wageningen University, 2007 [Google Scholar]
- 104. Kerckhoffs AP, Samsom M, van der Rest ME, et al. Lower Bifidobacteria counts in both duodenal mucosa-associated and fecal microbiota in irritable bowel syndrome patients. World J Gastroenterol 2009;15:2887–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Krogius-Kurikka L, Lyra A, Malinen E, et al. Microbial community analysis reveals high level phylogenetic alterations in the overall gastrointestinal microbiota of diarrhoea-predominant irritable bowel syndrome sufferers. BMC Gastroenterol 2009;9:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Lyra A, Rinttila T, Nikkila J, et al. Diarrhoea-predominant irritable bowel syndrome distinguishable by 16S rRNA gene phylotype quantification. World J Gastroenterol 2009;15:5936–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Tana C, Umesaki Y, Imaoka A, et al. Altered profiles of intestinal microbiota and organic acids may be the origin of symptoms in irritable bowel syndrome. Neurogastroenterol Motil 2010;22:512–19, e114–15. [DOI] [PubMed] [Google Scholar]
- 108. Codling C, O'Mahony L, Shanahan F, et al. A molecular analysis of fecal and mucosal bacterial communities in irritable bowel syndrome. Dig Dis Sci 2010;55:392–7 [DOI] [PubMed] [Google Scholar]
- 109. Noor SO, Ridgway K, Scovell L, et al. Ulcerative colitis and irritable bowel patients exhibit distinct abnormalities of the gut microbiota. BMC Gastroenterol 2010;10:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Malinen E, Krogius-Kurikka L, Lyra A, et al. Association of symptoms with gastrointestinal microbiota in irritable bowel syndrome. World J Gastroenterol 2010;16:4532–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Ponnusamy K, Choi JN, Kim J, et al. Microbial community and metabolomic comparison of irritable bowel syndrome faeces. J Med Microbiol 2011;60:817–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Rinttila T, Lyra A, Krogius-Kurikka L, et al. Real-time PCR analysis of enteric pathogens from fecal samples of irritable bowel syndrome subjects. Gut Pathog 2011;3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Saulnier DM, Riehle K, Mistretta TA, et al. Gastrointestinal microbiome signatures of Paediatric patients with irritable bowel syndrome. Gastroenterology 2011;141:1782–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Rajilic-Stojanovic M, Biagi E, Heilig HG, et al. Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome. Gastroenterology 2011;141:1792–801 [DOI] [PubMed] [Google Scholar]
- 115. Carroll IM, Ringel-Kulka T, Keku TO, et al. Molecular analysis of the luminal- and mucosal-associated intestinal microbiota in diarrhea-predominant irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol 2011;301:G799–807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Parkes GC, Rayment NB, Hudspith BN, et al. Distinct microbial populations exist in the mucosa-associated microbiota of sub-groups of irritable bowel syndrome. Neurogastroenterol Motil 2012;24:31–9 [DOI] [PubMed] [Google Scholar]
- 117. Jeffery IB, O'Toole PW, Ohman L, et al. An irritable bowel syndrome subtype defined by species-specific alterations in faecal microbiota. Gut 2012;61:997–1006 [DOI] [PubMed] [Google Scholar]
- 118. Lupp C, Robertson ML, Wickham ME, et al. Host-mediated inflammation disrupts the intestinal microbiota and promotes the overgrowth of enterobacteriaceae. Cell Host Microbe 2007;2:204. [DOI] [PubMed] [Google Scholar]
- 119. Barthel M, Hapfelmeier S, Quintanilla-Martinez L, et al. Pretreatment of mice with streptomycin provides a Salmonella enterica serovar Typhimurium colitis model that allows analysis of both pathogen and host. Infect Immun 2003;71:2839–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Wheeler JG, Sethi D, Cowden JM, et al. Study of infectious intestinal disease in England: rates in the community, presenting to general practice, and reported to national surveillance. The Infectious Intestinal Disease Study Executive. BMJ 1999;318:1046–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Longstreth GF, Hawkey CJ, Mayer EA, et al. Characteristics of patients with irritable bowel syndrome recruited from three sources: implications for clinical trials. Aliment Pharmacol Ther 2001;15:959–64 [DOI] [PubMed] [Google Scholar]
- 122. Spiller R, Card T, Mearin F, et al. Incidence and characteristics of postinfectious IBS (PI-IBS): a multinational internet survey. Gut 2010;59:A32 [Google Scholar]
- 123. Dunlop SP, Jenkins D, Neal KR, et al. Relative importance of enterochromaffin cell hyperplasia, anxiety, and depression in postinfectious IBS. Gastroenterology 2003;125:1651–9 [DOI] [PubMed] [Google Scholar]
- 124. Neal KR, Hebden J, Spiller R. Prevalence of gastrointestinal symptoms six months after bacterial gastroenteritis and risk factors for development of the irritable bowel syndrome: postal survey of patients. BMJ 1997;314:779–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Thabane M, Kottachchi DT, Marshall JK. Systematic review and meta-analysis: the incidence and prognosis of post-infectious irritable bowel syndrome. Aliment Pharmacol Ther 2007;26:535–44 [DOI] [PubMed] [Google Scholar]
- 126. Marshall JK, Thabane M, Borgaonkar MR, et al. Postinfectious irritable bowel syndrome after a food-borne outbreak of acute gastroenteritis attributed to a viral pathogen. Clin Gastroenterol Hepatol 2007;5:457–60 [DOI] [PubMed] [Google Scholar]
- 127. Porter CK, Gormley R, Tribble DR, et al. The incidence and gastrointestinal infectious risk of functional gastrointestinal disorders in a healthy US adult population. Am J Gastroenterol 2011;106:130–8 [DOI] [PubMed] [Google Scholar]
- 128. Thornley JP, Jenkins D, Neal K, et al. Relationship of Campylobacter toxigenicity in vitro to the development of postinfectious irritable bowel syndrome. J Infect Dis 2001;184:606–9 [DOI] [PubMed] [Google Scholar]
- 129. Marshall JK, Thabane M, Garg AX, et al. Incidence and epidemiology of irritable bowel syndrome after a large waterborne outbreak of bacterial dysentery. Gastroenterology 2006;131:445–50; quiz 660. [DOI] [PubMed] [Google Scholar]
- 130. Cremon C, Carini G, Wang B, et al. Intestinal serotonin release, sensory neuron activation, and abdominal pain in irritable bowel syndrome. Am J Gastroenterol 2011;106:1290–8 [DOI] [PubMed] [Google Scholar]
- 131. Park JH, Rhee PL, Kim G, et al. Enteroendocrine cell counts correlate with visceral hypersensitivity in patients with diarrhoea-predominant irritable bowel syndrome. Neurogastroenterol Motil 2006;18:539–46 [DOI] [PubMed] [Google Scholar]
- 132. Gwee KA, Leong YL, Graham C, et al. The role of psychological and biological factors in postinfective gut dysfunction. Gut 1999;44:400–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Fujita K, Kaku M, Yanagase Y, et al. Physicochemical characteristics and flora of diarrhoeal and recovery faeces in children with acute gastro-enteritis in Kenya. Ann Trop Paediatr 1990;10:339–45 [DOI] [PubMed] [Google Scholar]
- 134. Albert MJ, Bhat P, Rajan D, et al. Faecal flora of South Indian infants and young children in health and with acute gastroenteritis. J Med Microbiol 1978;11:137–43 [DOI] [PubMed] [Google Scholar]
- 135. Balamurugan R, Janardhan HP, George S, et al. Molecular studies of fecal anaerobic commensal bacteria in acute diarrhea in children. J Pediatr Gastroenterol Nutr 2008;46:514–19 [DOI] [PubMed] [Google Scholar]
- 136. Mai V, Braden CR, Heckendorf J, et al. Monitoring of stool microbiota in subjects with diarrhea indicates distortions in composition. J Clin Microbiol 2006;44:4550–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Rao SS, Edwards CA, Austen CJ, et al. Impaired colonic fermentation of carbohydrate after ampicillin. Gastroenterology 1988;94:928–32 [DOI] [PubMed] [Google Scholar]
- 138. Musch MW, Bookstein C, Xie Y, et al. SCFA increase intestinal Na absorption by induction of NHE3 in rat colon and human intestinal C2/bbe cells. Am J Physiol Gastrointest Liver Physiol 2001;280:G687–93 [DOI] [PubMed] [Google Scholar]
- 139. Ruppin H, Bar-Meir S, Soergel KH, et al. Absorption of short-chain fatty acids by the colon. Gastroenterology 1980;78:1500–7 [PubMed] [Google Scholar]
- 140. Zeissig S, Fromm A, Mankertz J, et al. Butyrate induces intestinal sodium absorption via Sp3-mediated transcriptional up-regulation of epithelial sodium channels. Gastroenterology 2007;132:236–48 [DOI] [PubMed] [Google Scholar]
- 141. Treem WR, Ahsan N, Kastoff G, et al. Fecal short-chain fatty acids in patients with diarrhea-predominant irritable bowel syndrome: in vitro studies of carbohydrate fermentation. J Pediatr Gastroenterol Nutr 1996;23:280–6 [DOI] [PubMed] [Google Scholar]
- 142. Barbara G, Stanghellini V, Berti-Ceroni C, et al. Role of antibiotic therapy on long-term germ excretion in faeces and digestive symptoms after Salmonella infection. Aliment Pharmacol Ther 2000;14:1127–31 [DOI] [PubMed] [Google Scholar]
- 143. Barbara G, Stanghellini V, Brandi G, et al. Interactions between commensal bacteria and gut sensorimotor function in health and disease. Am J Gastroenterol 2005;100:2560–8 [DOI] [PubMed] [Google Scholar]
- 144. Collins SM, Bercik P. The relationship between intestinal microbiota and the central nervous system in normal gastrointestinal function and disease. Gastroenterology 2009;136:2003–14 [DOI] [PubMed] [Google Scholar]
- 145. Swidsinski A, Loening-Baucke V, Verstraelen H, et al. Biostructure of fecal microbiota in healthy subjects and patients with chronic idiopathic diarrhea. Gastroenterology 2008;135:568–79 [DOI] [PubMed] [Google Scholar]
- 146. Langhorst J, Junge A, Rueffer A, et al. Elevated human beta-defensin-2 levels indicate an activation of the innate immune system in patients with irritable bowel syndrome. Am J Gastroenterol 2009;104:404–10 [DOI] [PubMed] [Google Scholar]
- 147. Brint EK, MacSharry J, Fanning A, et al. Differential expression of toll-like receptors in patients with irritable bowel syndrome. Am J Gastroenterol 2011;106:329–36 [DOI] [PubMed] [Google Scholar]
- 148. Schoepfer AM, Schaffer T, Seibold-Schmid B, et al. Antibodies to flagellin indicate reactivity to bacterial antigens in IBS patients. Neurogastroenterol Motil 2008;20:1110–18 [DOI] [PubMed] [Google Scholar]
- 149. Barbara G, Cremon C, Carini G, et al. The immune system in irritable bowel syndrome. J Neurogastroenterol Motil 2011;17:349–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Barbara G, Wang B, Stanghellini V, et al. Mast cell-dependent excitation of visceral-nociceptive sensory neurons in irritable bowel syndrome. Gastroenterology 2007;132:26–37 [DOI] [PubMed] [Google Scholar]
- 151. Cenac N, Andrews CN, Holzhausen M, et al. Role for protease activity in visceral pain in irritable bowel syndrome. J Clin Invest 2007;117:636–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Barbara G, Stanghellini V, De Giorgio R, et al. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology 2004;126:693–702 [DOI] [PubMed] [Google Scholar]
- 153. Round JL, Mazmanian SK. The gut microbiota shapes intestinal immune responses during health and disease. Nat Rev Immunol 2009;9:313–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Piche T, Barbara G, Aubert P, et al. Impaired intestinal barrier integrity in the colon of patients with irritable bowel syndrome: involvement of soluble mediators. Gut 2009;58:196–201 [DOI] [PubMed] [Google Scholar]
- 155. Gareau MG, Jury J, MacQueen G, et al. Probiotic treatment of rat pups normalises corticosterone release and ameliorates colonic dysfunction induced by maternal separation. Gut 2007;56:1522–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Bercik P, Verdu EF, Foster JA, et al. Chronic gastrointestinal inflammation induces anxiety-like behavior and alters central nervous system biochemistry in mice. Gastroenterology 2010;139:2102–12e1. [DOI] [PubMed] [Google Scholar]
- 157. Wahnschaffe U, Ullrich R, Riecken EO, et al. Celiac disease-like abnormalities in a subgroup of patients with irritable bowel syndrome. Gastroenterology 2001;121:1329–38 [DOI] [PubMed] [Google Scholar]
- 158. Sapone A, Lammers KM, Casolaro V, et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Med 2011;9:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Verdu EF, Huang X, Natividad J, et al. Gliadin-dependent neuromuscular and epithelial secretory responses in gluten-sensitive HLA-DQ8 transgenic mice. Am J Physiol 2008;294:G217–25 [DOI] [PubMed] [Google Scholar]
- 160. Pinier M, Verdu EF, Nasser-Eddine M, et al. Polymeric binders suppress gliadin-induced toxicity in the intestinal epithelium. Gastroenterology 2009;136:288–98 [DOI] [PubMed] [Google Scholar]
- 161. Natividad JM, Huang X, Slack E, et al. Host responses to intestinal microbial antigens in gluten-sensitive mice. PLoS One 2009;4:e6472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Simren M, Axelsson J, Gillberg R, et al. Quality of life in inflammatory bowel disease in remission: the impact of IBS-like symptoms and associated psychological factors. Am J Gastroenterol 2002;97:389–96 [DOI] [PubMed] [Google Scholar]
- 163. Pimentel M, Chang M, Chow EJ, et al. Identification of a prodromal period in Crohn's disease but not ulcerative colitis. Am J Gastroenterol 2000;95:3458–62 [DOI] [PubMed] [Google Scholar]
- 164. Keohane J, O'Mahony C, O'Mahony L, et al. Irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease: a real association or reflection of occult inflammation? Am J Gastroenterol 2010;105:1788, 1789–94; quiz 95. [DOI] [PubMed] [Google Scholar]
- 165. Quigley EM. Commensal bacteria: the link between IBS and IBD? Curr Opin Clin Nutr Metab Care 2011;14:497–503 [DOI] [PubMed] [Google Scholar]
- 166. Scanlan PD, Shanahan F, O'Mahony C, et al. Culture-independent analyses of temporal variation of the dominant fecal microbiota and targeted bacterial subgroups in Crohn's disease. J Clin Microbiol 2006;44:3980–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Conte MP, Schippa S, Zamboni I, et al. Gut-associated bacterial microbiota in paediatric patients with inflammatory bowel disease. Gut 2006;55:1760–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Giaffer MH, Holdsworth CD, Duerden BI. The assessment of faecal flora in patients with inflammatory bowel disease by a simplified bacteriological technique. J Med Microbiol 1991;35:238–43 [DOI] [PubMed] [Google Scholar]
- 169. Giaffer MH, Holdsworth CD, Duerden BI. Virulence properties of Escherichia coli strains isolated from patients with inflammatory bowel disease. Gut 1992;33:646–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Andoh A, Sakata S, Koizumi Y, et al. Terminal restriction fragment length polymorphism analysis of the diversity of fecal microbiota in patients with ulcerative colitis. Inflamm Bowel Dis 2007;13:955–62 [DOI] [PubMed] [Google Scholar]
- 171. Lepage P, Seksik P, Sutren M, et al. Biodiversity of the mucosa-associated microbiota is stable along the distal digestive tract in healthy individuals and patients with IBD. Inflamm Bowel Dis 2005;11:473–80 [DOI] [PubMed] [Google Scholar]
- 172. Kleessen B, Kroesen AJ, Buhr HJ, et al. Mucosal and invading bacteria in patients with inflammatory bowel disease compared with controls. Scand J Gastroenterol 2002;37:1034–41 [DOI] [PubMed] [Google Scholar]
- 173. Schultsz C, Van Den Berg FM, Ten Kate FW, et al. The intestinal mucus layer from patients with inflammatory bowel disease harbors high numbers of bacteria compared with controls. Gastroenterology 1999;117:1089–97 [DOI] [PubMed] [Google Scholar]
- 174. Swidsinski A, Ladhoff A, Pernthaler A, et al. Mucosal flora in inflammatory bowel disease. Gastroenterology 2002;122:44–54 [DOI] [PubMed] [Google Scholar]
- 175. Swidsinski A, Weber J, Loening-Baucke V, et al. Spatial organization and composition of the mucosal flora in patients with inflammatory bowel disease. J Clin Microbiol 2005;43:3380–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Gophna U, Sommerfeld K, Gophna S, et al. Differences between tissue-associated intestinal microfloras of patients with Crohn's disease and ulcerative colitis. J Clin Microbiol 2006;44:4136–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Prindiville T, Cantrell M, Wilson KH. Ribosomal DNA sequence analysis of mucosa-associated bacteria in Crohn's disease. Inflamm Bowel Dis 2004;10:824–33 [DOI] [PubMed] [Google Scholar]
- 178. Sokol H, Pigneur B, Watterlot L, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci U S A 2008;105:16731–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Simpson J, Neal KR, Scholefield JH, et al. Patterns of pain in diverticular disease and the influence of acute diverticulitis. Eur J Gastroenterol Hepatol 2003;15:1005–10 [DOI] [PubMed] [Google Scholar]
- 180. Humes DJ, Simpson J, Neal KR, et al. Psychological and colonic factors in painful diverticulosis. Br J Surg 2008;95:195–8 [DOI] [PubMed] [Google Scholar]
- 181. Humes D, Smith JK, Spiller RC. Colonic diverticular disease. Clin Evid (Online) 2011;2011:0405. [PMC free article] [PubMed] [Google Scholar]
- 182. Maxwell PR, Rink E, Kumar D, et al. Antibiotics increase functional abdominal symptoms. Am J Gastroenterol 2002;97:104–8 [DOI] [PubMed] [Google Scholar]
- 183. Mendall MA, Kumar D. Antibiotic use, childhood affluence and irritable bowel syndrome (IBS). Eur J Gastroenterol Hepatol 1998;10:59–62 [DOI] [PubMed] [Google Scholar]
- 184. Pimentel M, Chow EJ, Lin HC. Eradication of small intestinal bacterial overgrowth reduces symptoms of irritable bowel syndrome. Am J Gastroenterol 2000;95:3503–6 [DOI] [PubMed] [Google Scholar]
- 185. Pimentel M, Chow EJ, Lin HC. Normalization of lactulose breath testing correlates with symptom improvement in irritable bowel syndrome. a double-blind, randomized, placebo-controlled study. Am J Gastroenterol 2003;98:412–19 [DOI] [PubMed] [Google Scholar]
- 186. Koo HL, DuPont HL. Rifaximin: a unique gastrointestinal-selective antibiotic for enteric diseases. Curr Opin Gastroenterol 2010;26:17–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Pimentel M, Park S, Mirocha J, et al. The effect of a nonabsorbed oral antibiotic (rifaximin) on the symptoms of the irritable bowel syndrome: a randomized trial. Ann Intern Med 2006;145:557–63 [DOI] [PubMed] [Google Scholar]
- 188. Sharara AI, Aoun E, Abdul-Baki H, et al. A randomized double-blind placebo-controlled trial of rifaximin in patients with abdominal bloating and flatulence. Am J Gastroenterol 2006;101:326–33 [DOI] [PubMed] [Google Scholar]
- 189. Pimentel M, Lembo A, Chey WD, et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med 2011;364:22–32 [DOI] [PubMed] [Google Scholar]
- 190. Pimentel M, Morales W, Chua K, et al. Effects of rifaximin treatment and retreatment in Nonconstipated IBS subjects. Dig Dis Sci 2011;56:2067–72 [DOI] [PubMed] [Google Scholar]
- 191. Di Stefano M, Strocchi A, Malservisi S, et al. Non-absorbable antibiotics for managing intestinal gas production and gas-related symptoms. Aliment Pharmacol Ther 2000;14:1001–8 [DOI] [PubMed] [Google Scholar]
- 192. Cuoco L, Salvagnini M. Small intestine bacterial overgrowth in irritable bowel syndrome: a retrospective study with rifaximin. Minerva Gastroenterol Dietol 2006;52:89–95 [PubMed] [Google Scholar]
- 193. Jolley J. High-dose rifaximin treatment alleviates global symptoms of irritable bowel syndrome. Clin Exp Gastroenterol 2011;4:43–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Peralta S, Cottone C, Doveri T, et al. Small intestine bacterial overgrowth and irritable bowel syndrome-related symptoms: experience with Rifaximin. World J Gastroenterol 2009;15:2628–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Yang J, Lee HR, Low K, et al. Rifaximin versus other antibiotics in the primary treatment and retreatment of bacterial overgrowth in IBS. Dig Dis Sci 2008;53:169–74 [DOI] [PubMed] [Google Scholar]
- 196. Valentin T, Leitner E, Rohn A, et al. Rifaximin intake leads to emergence of rifampin-resistant staphylococci. J Infect 2011;62:34–8 [DOI] [PubMed] [Google Scholar]
- 197. Curry SR, Marsh JW, Shutt KA, et al. High frequency of rifampin resistance identified in an epidemic Clostridium difficile clone from a large teaching hospital. Clin Infect Dis 2009;48:425–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Jiang ZD, DuPont HL, La Rocco M, et al. In vitro susceptibility of Clostridium difficile to rifaximin and rifampin in 359 consecutive isolates at a university hospital in Houston, Texas J Clin Pathol 2010;63:355–8 [DOI] [PubMed] [Google Scholar]
- 199. Shah D, Dang MD, Hasbun R, et al. Clostridium difficile infection: update on emerging antibiotic treatment options and antibiotic resistance. Expert Rev Anti Infect Ther 2010;8:555–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Koo HL, DuPont HL. Current and future developments in travelers' diarrhea therapy. Expert Rev Anti Infect Ther 2006;4:417–27 [DOI] [PubMed] [Google Scholar]
- 201. Tack J. Antibiotic therapy for the irritable bowel syndrome. N Engl J Med 2011;364:81–2 [DOI] [PubMed] [Google Scholar]
- 202. Drossman DA. Treatment for bacterial overgrowth in the irritable bowel syndrome. Ann Intern Med 2006;145:626–8 [DOI] [PubMed] [Google Scholar]
- 203. Guarner F, Requena T, Marcos A. Consensus statements from the workshop “Probiotics and health: scientific evidence”. Nutr Hosp 2010;25:700–4 [PubMed] [Google Scholar]
- 204. Ait-Belgnaoui A, Han W, Lamine F, et al. Lactobacillus farciminis treatment suppresses stress induced visceral hypersensitivity: a possible action through interaction with epithelial cell cytoskeleton contraction. Gut 2006;55:1090–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Kamiya T, Wang L, Forsythe P, et al. Inhibitory effects of Lactobacillus reuteri on visceral pain induced by colorectal distension in Sprague-Dawley rats. Gut 2006;55:191–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Wang B, Mao YK, Diorio C, et al. Luminal administration ex vivo of a live Lactobacillus species moderates mouse jejunal motility within minutes. Faseb J 2010;24:4078–88 [DOI] [PubMed] [Google Scholar]
- 207. Verdu EF, Bercik P, Bergonzelli GE, et al. Lactobacillus paracasei normalizes muscle hypercontractility in a murine model of postinfective gut dysfunction. Gastroenterology 2004;127:826–37 [DOI] [PubMed] [Google Scholar]
- 208. Agrawal A, Houghton LA, Morris J, et al. Clinical trial: the effects of a fermented milk product containing Bifidobacterium lactis DN-173-010 on abdominal distension and gastrointestinal transit in irritable bowel syndrome with constipation. Aliment Pharmacol Ther 2008;29:104–14 [DOI] [PubMed] [Google Scholar]
- 209. Kim HJ, Camilleri M, McKinzie S, et al. A randomized controlled trial of a probiotic, VSL#3, on gut transit and symptoms in diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther 2003;17:895–904 [DOI] [PubMed] [Google Scholar]
- 210. Kim HJ, Vazquez Roque MI, Camilleri M, et al. A randomized controlled trial of a probiotic combination VSL# 3 and placebo in irritable bowel syndrome with bloating. Neurogastroenterol Motil 2005;17:687–96 [DOI] [PubMed] [Google Scholar]
- 211. Zareie M, Johnson-Henry K, Jury J, et al. Probiotics prevent bacterial translocation and improve intestinal barrier function in rats following chronic psychological stress. Gut 2006;55:1553–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212. Francavilla R, Miniello V, Magista AM, et al. A randomized controlled trial of Lactobacillus GG in children with functional abdominal pain. Pediatrics 2010;126:e1445–52 [DOI] [PubMed] [Google Scholar]
- 213. Kajander K, Krogius-Kurikka L, Rinttila T, et al. Effects of multispecies probiotic supplementation on intestinal microbiota in irritable bowel syndrome. Aliment Pharmacol Ther 2007;26:463–73 [DOI] [PubMed] [Google Scholar]
- 214. Kajander K, Myllyluoma E, Rajilic-Stojanovic M, et al. Clinical trial: multispecies probiotic supplementation alleviates the symptoms of irritable bowel syndrome and stabilizes intestinal microbiota. Aliment Pharmacol Ther 2008;27:48–57 [DOI] [PubMed] [Google Scholar]
- 215. O'Mahony L, McCarthy J, Kelly P, et al. Lactobacillus and bifidobacterium in irritable bowel syndrome: symptom responses and relationship to cytokine profiles. Gastroenterology 2005;128:541–51 [DOI] [PubMed] [Google Scholar]
- 216. Gade J, Thorn P. Paraghurt for patients with irritable bowel syndrome. A controlled clinical investigation from general practice. Scand J Prim Health Care 1989;7:23–6 [DOI] [PubMed] [Google Scholar]
- 217. Halpern GM, Prindiville T, Blankenburg M, et al. Treatment of irritable bowel syndrome with lacteol fort: a randomized, double-blind, cross-over trial. Am J Gastroenterol 1996;91:1579–85 [PubMed] [Google Scholar]
- 218. Nobaek S, Johansson ML, Molin G, et al. Alteration of intestinal microflora is associated with reduction in abdominal bloating and pain in patients with irritable bowel syndrome. Am J Gastroenterol 2000;95:1231–8 [DOI] [PubMed] [Google Scholar]
- 219. Niedzielin K, Kordecki H, Birkenfeld B. A controlled, double-blind, randomized study on the efficacy of Lactobacillus plantarum 299V in patients with irritable bowel syndrome. Eur J Gastroenterol Hepatol 2001;13:1143–7 [DOI] [PubMed] [Google Scholar]
- 220. Sen S, Mullan MM, Parker TJ, et al. Effect of Lactobacillus plantarum 299v on colonic fermentation and symptoms of irritable bowel syndrome. Dig Dis Sci 2002;47:2615–20 [DOI] [PubMed] [Google Scholar]
- 221. Ligaarden SC, Axelsson L, Naterstad K, et al. A candidate probiotic with unfavourable effects in subjects with irritable bowel syndrome: a randomised controlled trial. BMC Gastroenterol 2010;10:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Dolin BJ. Effects of a proprietary Bacillus coagulans preparation on symptoms of diarrhea-predominant irritable bowel syndrome. Methods Find Exp Clin Pharmacol 2009;31:655–9 [DOI] [PubMed] [Google Scholar]
- 223. Niv E, Naftali T, Hallak R, et al. The efficacy of Lactobacillus reuteri ATCC 55730 in the treatment of patients with irritable bowel syndrome–a double blind, placebo-controlled, randomized study. Clin Nutr 2005;24:925–31 [DOI] [PubMed] [Google Scholar]
- 224. Whorwell PJ, Altringer L, Morel J, et al. Efficacy of an encapsulated probiotic Bifidobacterium infantis 35624 in women with irritable bowel syndrome. Am J Gastroenterol 2006;101:1581–90 [DOI] [PubMed] [Google Scholar]
- 225. Guyonnet D, Chassany O, Ducrotte P, et al. Effect of a fermented milk containing Bifidobacterium animalis DN-173 010 on the health-related quality of life and symptoms in irritable bowel syndrome in adults in primary care: a multicentre, randomized, double-blind, controlled trial. Aliment Pharmacol Ther 2007;26:475–86 [DOI] [PubMed] [Google Scholar]
- 226. Guglielmetti S, Mora D, Gschwender M, et al. Randomised clinical trial: bifidobacterium bifidum MIMBb75 significantly alleviates irritable bowel syndrome and improves quality of life–a double-blind, placebo-controlled study. Aliment Pharmacol Ther 2011;33:1123–32 [DOI] [PubMed] [Google Scholar]
- 227. Kruis W, Chrubasik S, Boehm S, et al. A double-blind placebo-controlled trial to study therapeutic effects of probiotic Escherichia coli nissle 1917 in subgroups of patients with irritable bowel syndrome. Int J Colorectal Dis 2012;27:467–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Kim YG, Moon JT, Lee KM, et al. The effects of probiotics on symptoms of irritable bowel syndrome. Korean J Gastroenterol 2006;47:413–19 [PubMed] [Google Scholar]
- 229. Kajander K, Hatakka K, Poussa T, et al. A probiotic mixture alleviates symptoms in irritable bowel syndrome patients: a controlled 6-month intervention. Aliment Pharmacol Ther 2005;22:387–94 [DOI] [PubMed] [Google Scholar]
- 230. Williams E, Stimpson J, Wang D, et al. Clinical trial: a multistrain probiotic preparation significantly reduces symptoms of irritable bowel syndrome in a double-blind placebo-controlled study. Aliment Pharmacol Ther 2009;29:97–103 [DOI] [PubMed] [Google Scholar]
- 231. Drouault-Holowacz S, Bieuvelet S, Burckel A, et al. A double blind randomized controlled trial of a probiotic combination in 100 patients with irritable bowel syndrome. Gastroenterol Clin Biol 2008;32:147–52 [DOI] [PubMed] [Google Scholar]
- 232. Sinn DH, Song JH, Kim HJ, et al. Therapeutic effect of Lactobacillus acidophilus-SDC 2012, 2013 in patients with irritable bowel syndrome. Dig Dis Sci 2008;53:2714–18 [DOI] [PubMed] [Google Scholar]
- 233. Enck P, Zimmermann K, Menke G, et al. A mixture of Escherichia coli (DSM 17252) and Enterococcus faecalis (DSM 16440) for treatment of the irritable bowel syndrome–a randomized controlled trial with primary care physicians. Neurogastroenterol Motil 2008;20:1103–9 [DOI] [PubMed] [Google Scholar]
- 234. Simren M, Ohman L, Olsson J, et al. Clinical trial: the effects of a fermented milk containing three probiotic bacteria in patients with irritable bowel syndrome—a randomized, double-blind, controlled study. Aliment Pharmacol Ther 2010;31:218–27 [DOI] [PubMed] [Google Scholar]
- 235. Sondergaard B, Olsson J, Ohlson K, et al. Effects of probiotic fermented milk on symptoms and intestinal flora in patients with irritable bowel syndrome: a randomized, placebo-controlled trial. Scand J Gastroenterol 2011;46:663–72 [DOI] [PubMed] [Google Scholar]
- 236. Hong KS, Kang HW, Im JP, et al. Effect of probiotics on symptoms in korean adults with irritable bowel syndrome. Gut Liver 2009;3:101–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237. Bausserman M, Michail S. The use of Lactobacillus GG in irritable bowel syndrome in children: a double-blind randomized control trial. J Pediatr 2005;147:197–201 [DOI] [PubMed] [Google Scholar]
- 238. Gawronska A, Dziechciarz P, Horvath A, et al. A randomized double-blind placebo-controlled trial of Lactobacillus GG for abdominal pain disorders in children. Aliment Pharmacol Ther 2007;25:177–84 [DOI] [PubMed] [Google Scholar]
- 239. Guandalini S, Magazzu G, Chiaro A, et al. VSL#3 improves symptoms in children with irritable bowel syndrome: a multicenter, randomized, placebo-controlled, double-blind, crossover study. J Pediatr Gastroenterol Nutr 2010;51:24–30 [DOI] [PubMed] [Google Scholar]
- 240. O'Sullivan MA, O'Morain CA. Bacterial supplementation in the irritable bowel syndrome. A randomised double-blind placebo-controlled crossover study. Dig Liver Dis 2000;32:294–301 [DOI] [PubMed] [Google Scholar]
- 241. Brenner DM, Moeller MJ, Chey WD, et al. The utility of probiotics in the treatment of irritable bowel syndrome: a systematic review. Am J Gastroenterol 2009;104:1033–49; quiz 50. [DOI] [PubMed] [Google Scholar]
- 242. Hoveyda N, Heneghan C, Mahtani KR, et al. A systematic review and meta-analysis: probiotics in the treatment of irritable bowel syndrome. BMC Gastroenterology 2009;9:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243. McFarland LV, Dublin S. Meta-analysis of probiotics for the treatment of irritable bowel syndrome. World J Gastroenterol 2008;14:2650–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Moayyedi P, Ford AC, Talley NJ, et al. The efficacy of probiotics in the treatment of irritable bowel syndrome: a systematic review. Gut 2010;59:325–32 [DOI] [PubMed] [Google Scholar]
- 245. Snook J, Shepherd HA. Bran supplementation in the treatment of irritable bowel syndrome. Aliment Pharmacol Ther 1994;8:511–14 [DOI] [PubMed] [Google Scholar]
- 246. Francis CY, Whorwell PJ. Bran and irritable bowel syndrome: time for reappraisal. Lancet 1994;344:39–40 [DOI] [PubMed] [Google Scholar]
- 247. Roberfroid M. Prebiotics: the concept revisited. J nutrition 2007;137:830S–7S [DOI] [PubMed] [Google Scholar]
- 248. Gibson GR, Roberfroid MB. Dietary modulation of the human colonic microbiota: introducing the concept of prebiotics. J nutrition 1995;125:1401–12 [DOI] [PubMed] [Google Scholar]
- 249. Florent C, Flourie B, Leblond A, et al. Influence of chronic lactulose ingestion on the colonic metabolism of lactulose in man (an in vivo study). J Clin Invest 1985;75:608–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250. Silk DB, Davis A, Vulevic J, et al. Clinical trial: the effects of a trans-galactooligosaccharide prebiotic on faecal microbiota and symptoms in irritable bowel syndrome. Aliment Pharmacol Ther 2009;29:508–18 [DOI] [PubMed] [Google Scholar]
- 251. Andriulli A, Neri M, Loguercio C, et al. Clinical trial on the efficacy of a new symbiotic formulation, flortec, in patients with irritable bowel syndrome: a multicenter, randomized study. J Clin Gastroenterol 2008;42(Suppl 3):S218–23 [DOI] [PubMed] [Google Scholar]
- 252. Bittner AC, Croffut RM, Stranahan MC. Prescript-assist probiotic-prebiotic treatment for irritable bowel syndrome: a methodologically oriented, 2-week, randomized, placebo-controlled, double-blind clinical study. Clin Ther 2005;27:755–61 [DOI] [PubMed] [Google Scholar]
- 253. Bittner AC, Croffut RM, Stranahan MC, et al. Prescript-assist probiotic-prebiotic treatment for irritable bowel syndrome: an open-label, partially controlled, 1-year extension of a previously published controlled clinical trial. Clin Ther 2007;29:1153–60 [DOI] [PubMed] [Google Scholar]
- 254. Colecchia A, Vestito A, La Rocca A, et al. Effect of a symbiotic preparation on the clinical manifestations of irritable bowel syndrome, constipation-variant. Results of an open, uncontrolled multicenter study. Minerva Gastroenterol Dietol 2006;52:349–58 [PubMed] [Google Scholar]
- 255. Tsuchiya J, Barreto R, Okura R, et al. Single-blind follow-up study on the effectiveness of a symbiotic preparation in irritable bowel syndrome. Chin J Dig Dis 2004;5:169–74 [DOI] [PubMed] [Google Scholar]
- 256. Dear KL, Elia M, Hunter JO. Do interventions which reduce colonic bacterial fermentation improve symptoms of irritable bowel syndrome? Dig Dis Sci 2005;50:758–66 [DOI] [PubMed] [Google Scholar]
- 257. Shepherd SJ, Gibson PR. Fructose malabsorption and symptoms of irritable bowel syndrome: guidelines for effective dietary management. J Am Diet Assoc 2006;106:1631–9 [DOI] [PubMed] [Google Scholar]
- 258. Nanda R, James R, Smith H, et al. Food intolerance and the irritable bowel syndrome. Gut 1989;30:1099–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259. Kaptchuk TJ, Friedlander E, Kelley JM, et al. Placebos without deception: a randomized controlled trial in irritable bowel syndrome. PLoS One 2010;5:e15591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Cremonini F, Delgado-Aros S, Camilleri M. Efficacy of alosetron in irritable bowel syndrome: a meta-analysis of randomized controlled trials. Neurogastroenterol Motil 2003;15:79–86 [DOI] [PubMed] [Google Scholar]
- 261. Johnston JM, Kurtz CB, Macdougall JE, et al. Linaclotide improves abdominal pain and bowel habits in a phase IIb study of patients with irritable bowel syndrome with constipation. Gastroenterology 2010;139:1877–86.e2 [DOI] [PubMed] [Google Scholar]
- 262. Evans BW, Clark WK, Moore DJ, et al. Tegaserod for the treatment of irritable bowel syndrome and chronic constipation. Cochrane Database Syst Rev 2004;(4):CD003960. [DOI] [PubMed] [Google Scholar]
- 263. Landy J, Al-Hassi HO, McLaughlin SD, et al. Review article: faecal transplantation therapy for gastrointestinal disease. Aliment Pharmacol Ther 2011;34:409–15 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.