Abstract
Changes in knee mechanics following anterior cruciate ligament reconstruction (ACLR) have been implicated as a contributor to the development of premature osteoarthritis (OA). However, changes in ambulatory loading in this population have not been well documented. While the magnitude of the external knee moment vector is a major factor in loading at the knee, there is not a comprehensive understanding of the changes in the individual components of the vector following ACL reconstruction. The purpose of this study was to test for differences in the three components of the external knee moment during walking and stair locomotion between ACLR, contralateral and healthy control knees. Forty-five ACLR and 45 healthy control subjects were tested during walking, stair ascent and descent. ACLR knees had a lower first peak adduction moment than contralateral knees during all three activities. Similarly, additional cases of significant differences between ACLR and contralateral knees consisted of lower peak moments for the ACLR than the contralateral knees. These differences were due to both ACLR and contralateral knees as the ACLR knees indicated lower and the contralateral knees greater peak moments compared to healthy control knees. The results suggest a compensatory change involving greater loading in the contralateral knee, perhaps due to lower loading of the ACLR knee. Further, lower knee moments of the ACLR knee suggest that increased joint loading may not be the initiating factor in the development of OA following ACL reconstruction; but rather previous described kinematic or biological changes might initiate the pathway to knee OA.
Keywords: ACL, reconstruction, moments, knee, control
INTRODUCTION
The primary treatment for anterior cruciate ligament (ACL) rupture is surgical reconstruction with the purpose of restoring knee stability and allowing for the return to sports or other demanding activities (Dye and Wojtys, 1999). However, many studies have shown that ambulatory function is not completely restored following ACL reconstruction (Bush-Joseph et al., 2001; Scanlan et al., 2010; Webster and Feller, 2011; Butler et al., 2009). This is important beyond the desire of the patient to return to previous levels of activity as changes in the loading environment at the knee have been suggested as a possible reason for the increased incidence of premature knee osteoarthritis in the ACL reconstructed population (Andriacchi et al., 2004; Andriacchi and Mundermann, 2006; Lohmander et al., 2004; von Porat et al., 2004).
Since the articular contact loads cannot be directly measured with non-invasive means, the external knee moments are frequently used as surrogate measures of knee loading (Erhart et al., 2010; Walter et al., 2010; Schipplein and Andriacchi, 1991). Numerous studies have investigated the individual components of the total moment vector acting at the knee in patients with ACL injury. For example, the external flexion moment following ACL reconstruction has been reported to be lower in magnitude than healthy control knees during gait or other activities (Bush–Joseph et al., 2001; Webster et al., 2005; Hooper et al., 2002) suggesting an inhibition of quadriceps function. However, the moments in the two other anatomical planes are not as well understood.
While the knee adduction moment during gait has been shown to be directly associated with the distribution of load between the medial and lateral knee compartments (Walter et al., 2010; Schipplein and Andriacchi, 1991) and progression (Miyazaki et al., 2002) as well as severity (Sharma et al., 1998; Mundermann et al., 2004) of idiopathic medial osteoarthritis, few studies have characterized this moment in ACL reconstructed (ACLR) knees (Webster and Feller, 2011; Butler et al., 2009).. Moreover, these studies that have examined the adduction moment in ACLR knees report conflicting results where Webster and Feller (2011) found lower adduction moment and Butler et al. (2009) found greater adduction moment compared to healthy controls during gait. Similarly, there is a lack of information on the rotational component of the moment at the knee, yet this information could be important as kinematic alterations have been reported for ACLR knees in the transverse plane (Scanlan et al., 2010; Tashman, 2004), and the rotational component of the moment has been associated with cartilage loss in osteoarthritic knees (Henriksen et al., 2012). Furthermore, greater internal rotation moment was found in knees with moderate osteoarthritis compared to asymptomatic knees during gait (Astephen et al., 2008). Therefore, there is a need for a comprehensive analysis of the three components of the knee moment to gain a better understanding of knee mechanics following ACL reconstruction. Additionally, analysis of more strenuous daily activities, like stair ascent and descent (Taylor et al., 2004), not only can provide more sensitivity in detecting differences in knee mechanics between ACLR and healthy knees than level gait, but can provide a more complete representation of the daily loading sustained by ACLR knees. Thus, such a comprehensive assessment of ACLR knees will help address questions of whether current treatment methods can effectively restore 3D knee function during various activities and may also highlight important changes in mechanical markers associated with increased risk of osteoarthritis.
Previous reports of the incidence of early onset OA (Lohmander et al., 2004; von Porat et al., 2004) and lower knee flexion moment (Bush–Joseph et al., 2001; Webster et al., 2005; Hooper et al., 2002) in ACLR knees, as well as greater adduction (Butler et al., 2009) and internal rotation moment (Astephen et al., 2008) in knees with idiopathic OA motivated this study to test for similar functional abnormalities in ACLR knees during gait and stair ascent/descent. The hypothesis tested in this study consisted of two parts: 1) ACLR knees will exhibit lower external knee flexion moment, and greater adduction and internal rotation moment during gait, stair ascent and stair descent, when compared to the contralateral knees, and 2) These differences will be primarily driven by the ACLR knee, not the contralateral knee, when compared to a healthy control population.
METHODS
Forty-five subjects with unilateral ACL reconstruction and no other history of serious lower limb injury (29.5 ± 6.1 years old, 1.72 ± 0.10 m, 74.4 ± 12.4 kg, 22 left legs, 19 females, 26 months past reconstruction, range 22–36 months past reconstruction, 2.2 months between injury and reconstruction, range 0.4–8.0 months between injury and reconstruction), and forty-five healthy control subjects (30.2 ± 4.68 years old, 1.73 ± 0.09 m, 74.2 ± 12.3 kg, 19 females) with no history of serious injury to either limb participated in this study after providing IRB-approved informed consent. All ACLR subjects had a single-bundle ACL reconstruction performed with a standard trans-tibial technique using an achilles allograft. Also, inclusion criteria were a successful ACL reconstruction based on clinical exam (KT-1000 side-to-side difference < 5 mm), MRI, and self-reported history of knee stability. ACLR subjects with resection of > 25% of the meniscus, clinical instability of the reconstructed knee, history of other serious ligamentous injury to either lower limb, or a history of surgical procedures performed on either lower limb were excluded. Three groups were considered for the analysis: one group of 45 ACLR knees, one group of 45 contralateral knees, and one group of 45 control knees (one knee randomly selected per control subject).
All subjects performed several trials of level walking and stair ascent and descent (step height 20 cm; tread 25 cm) over a force plate (Bertec, Columbus, OH) at a normal self-selected speed until three successful trials had been collected for each activity. A trial was considered successful if the foot of the leg being tested fully stepped on the force plate. Lower-limb kinematics were measured using an optoelectronic motion capture system (Qualisys, Gothenburg, Sweden) and a redundant set of 21 reflective markers according to a previously-described method (Andriacchi et al., 1998; Dyrby and Andriacchi, 2004). Data were collected at 120 Hz. Knee moments were calculated by inverse dynamics (Andriacchi et al., 2005) using the inertia properties of the segments defined in Dempster and Gaughran (1967). The knee moments were expressed as external moments relative to the tibial anatomical frame based upon palpable bony landmarks measured during a standing reference trial (Dyrby and Andriacchi, 2004). Moments were normalized to percent bodyweight and height (%Bw*Ht). A vertical ground reaction force threshold of 10 Newtons was used to detect the beginning and the end of the stance phase and knee moments were normalized to 101 time points (t= 0 to 100%) during this phase.
Two peaks (i.e., 1st and 2nd half of stance) that characterized the maxima of each of the three moment components (ad/abduction moment, flexion/extension moment, and external/internal rotation moment) were analyzed for all trials. The amplitudes of each peak for the three successful trials of each activity were averaged respectively for each knee. This resulted in two values of peak moments (1st and 2nd half of stance) for each of the three moments and each activity per knee. For the three activities, two peaks were also analyzed for the total moment of the knee which was calculated as the Euclidian norm of the three knee joint moment components (Boyer et al., 2011).
Side-to-side differences in each peak of the knee moments were determined between ACLR and contralateral knees with a paired Student’s t-test. In the cases where differences were present between ACLR and contralateral knees, unpaired Student’s t-tests were used to determine which of the ACLR or contralateral knees were significantly different from the control knees. For each of these statistical tests, a Bonferroni-corrected alpha value of 0.0125 was used to determine significance.
RESULTS
Paired student’s t-tests determined that there were no instances of significant demographic differences between the subjects with ACL reconstruction and the healthy control subjects. Additionally, there were no significant differences in gait speed between the subjects with ACL reconstruction and the healthy control subjects (1.38 ± 0.14, 1.39 ± 0.15 m/s respectively, p = 0.76).
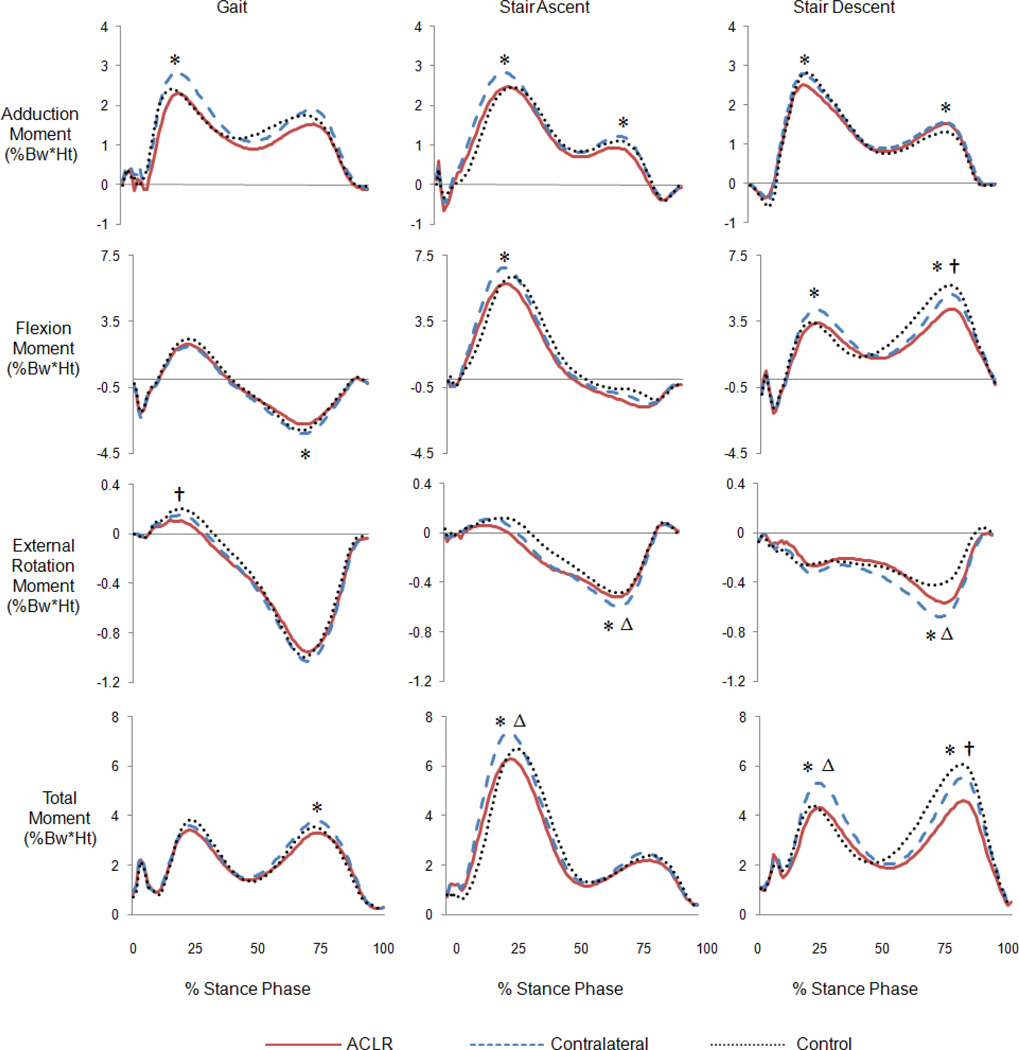
There were numerous cases of significantly lower peak moments of the ACLR knees than contralateral knees during all three activities (Table 1, Fig.1). Specifically, the first peak adduction moment of the ACLR knees was lower than the contralateral knees during gait, and both adduction peaks were lower during stair ascent and descent. Regarding the kinetics in the sagittal plane, the peak flexion moment of the ACLR knees was significantly lower than the contralateral knees during stair ascent (first peak) and stair descent (first and second peaks). The ACLR knees were also significantly lower than the contralateral knees for the peak extension moment during gait (second peak). In the transverse plane, the internal rotation moment of the ACLR knees was lower than with the contralateral knees during stair ascent (second peak) and descent (second peak). The total moment of the ACLR knees was lower than the contralateral knees during gait (second peak), stair ascent (first peak), and stair descent (both peaks). There were no instances where the amplitude of the moment peaks were significantly larger for the ACLR knees compared to the contralateral knees (Table 1, Fig. 1).
Table 1.
Peak knee moment values during gait, stair ascent, and stair descent for ACLR, contralateral, and control knees. Significant p-values emboldened.
| Peak Amplitude (%Bw*Ht) | ACLR-Contra | |||||
|---|---|---|---|---|---|---|
| Activity | Phase | Anatomical Plane | ACLR | Contralateral | Control | p |
| Gait | 1st Peak | Adduction | 2.67 ± 0.64 | 2.95 ± 0.57 | 2.94 ± 0.73 | 0.001 |
| Flexion | 2.23 ± 1.29 | 2.16 ± 1.17 | 2.59 ± 1.17 | 0.735 | ||
| External Rotation | 0.17 ± 0.11 | 0.20 ± 0.12 | 0.24 ± 0.11 | 0.035 | ||
| Total | 3.81 ± 0.97 | 4.07 ± 0.76 | 4.02 ± 1.09 | 0.042 | ||
| 2nd Peak | Adduction | 1.65 ± 0.77 | 1.70 ± 0.58 | 1.50 ± 0.57 | 0.612 | |
| Extension | 2.81 ± 0.96 | 3.36 ± 0.88 | 3.17 ± 0.88 | < 0.001 | ||
| Internal Rotation | 0.97 ± 0.24 | 1.04 ± 0.21 | 1.01 ± 0.24 | 0.052 | ||
| Total | 3.36 ± 0.97 | 3.86 ± 0.89 | 3.62 ± 0.82 | < 0.001 | ||
| Stair Ascent | 1st Peak | Adduction | 2.67 ± 0.64 | 3.09 ± 0.88 | 2.68 ± 0.86 | 0.008 |
| Flexion | 6.05 ± 1.54 | 7.01 ± 0.85 | 6.58 ± 1.07 | < 0.001 | ||
| External Rotation | 0.21 ± 0.16 | 0.27 ± 0.16 | 0.27 ± 0.18 | 0.089 | ||
| Total | 6.58 ± 1.52 | 7.64 ± 0.80 | 7.07 ± 1.19 | < 0.001 | ||
| 2nd Peak | Adduction | 1.26 ± 0.63 | 1.49 ± 0.57 | 1.56 ± 0.68 | 0.001 | |
| Extension | 2.10 ± 1.06 | 2.02 ± 1.29 | 1.97 ± 1.25 | 0.586 | ||
| Internal Rotation | 0.56 ± 0.24 | 0.64 ± 0.18 | 0.53 ± 0.21 | 0.012 | ||
| Total | 2.68 ± 0.93 | 2.98 ± 0.94 | 3.19 ± 1.13 | 0.021 | ||
| Stair Descent | 1st Peak | Adduction | 2.72 ± 0.90 | 3.30 ± 0.91 | 2.86 ± 0.91 | < 0.001 |
| Flexion | 3.85 ± 1.68 | 4.64 ± 1.76 | 4.00 ± 1.85 | 0.010 | ||
| Internal Rotation | 0.43 ± 0.21 | 0.51 ± 0.20 | 0.47 ± 0.17 | 0.031 | ||
| Total | 5.04 ± 1.48 | 6.10 ± 1.70 | 5.13 ± 1.78 | 0.001 | ||
| 2nd Peak | Adduction | 1.70 ± 0.63 | 2.10 ± 0.81 | 2.04 ± 0.84 | < 0.001 | |
| Flexion | 4.53 ± 1.60 | 5.35 ± 1.45 | 6.05 ± 1.46 | < 0.001 | ||
| Internal Rotation | 0.64 ± 0.34 | 0.80 ± 0.38 | 0.58 ± 0.36 | < 0.001 | ||
| Total | 4.86 ± 1.64 | 5.79 ± 1.48 | 6.39 ± 1.55 | < 0.001 | ||
Figure 1.
All three moments and the total moment at the knee during gait, stair ascent, and stair descent for ACLR, contralateral, and control knees. (*) indicates significant difference between ACLR and contralateral, (△) indicates significant difference between contralateral and control, and (†) indicates significant difference between ACLR and control knees.
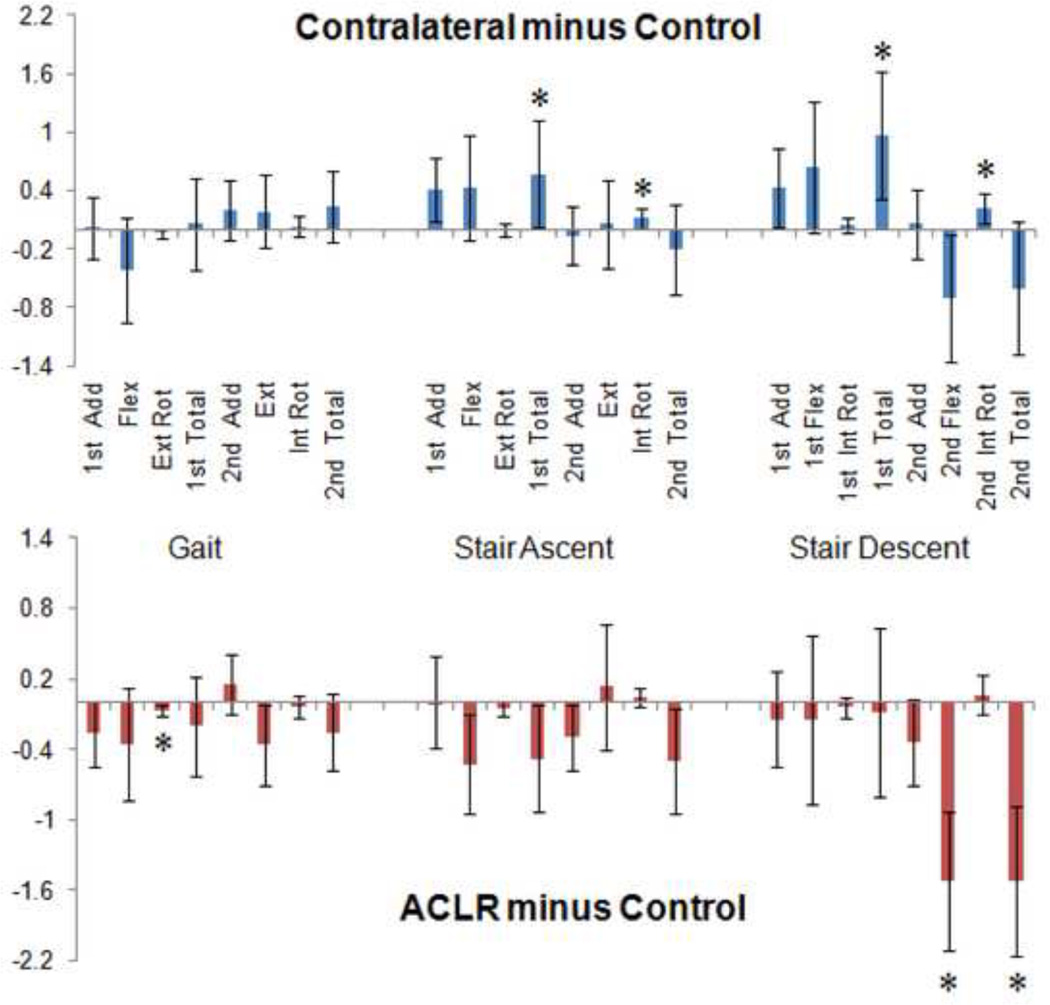
When testing for which knee of the ACLR subjects (i.e., ACLR or contralateral) was different from the healthy control knees, the ACLR knees had significantly lower external rotation moment peak during gait (first peak) and lower second flexion moment peak and second total moment peak during stair descent compared to the control knees (Fig. 1 & Fig. 2). On the other hand, the contralateral knees had significantly greater internal rotation peak for stair ascent and descent (second peaks), and greater first total moment peak during stair ascent and descent compared to the control knees.
Figure 2.
Differences between the means of contralateral and control knee peak moments, and between the means of ACLR and controls knee peak moments. Asterisk indicates significance (p < 0.0125). Brackets represent 95% confidence intervals for differences between the means.
DISCUSSION
The results of this study only partly supported the first hypothesis because the ACLR knees exhibited significantly lower external knee flexion moment compared to their contralateral knees during stair ascent and descent but not during gait. Additionally, the ACLR knees exhibited lower peak adduction moment during all activities and lower internal rotation moment during stair ascent and descent compared to the contralateral knees, whereas it was hypothesized that these peaks would be greater for the ACLR group compared to the contralateral group. The second hypothesis was not supported at all as the significant side-to-side differences observed with the ACLR subjects were not only primarily driven by the ACLR knees. When compared to a healthy control group, the ACLR knees of the ACLR subjects reported lower moments and the contralateral knees of the ACLR subjects indicated greater moments. Side-to-side differences in total moment peaks suggest that there is lower ACLR and greater contralateral knee total loading as the external moments at the knee require internal muscle forces to sustain posture and forward propulsion. Indeed, further evaluation of the shape of the total moment curves during gait in Figure 1 reveals a similarity to the shape of the tibial contact force curve found in a study by D’Lima et al. (2006) which used an instrumented tibial prosthesis during gait. Both curves begin with an initial transient peak at heel strike and continue with two larger peaks, roughly equal in magnitude, during the rest of stance. Given this interpretation of the total moment as a surrogate measure for joint loading, it is likely that the contralateral knees sustain greater forces than normal while the ACLR knees sustain lower forces.
As ACLR knees have been shown to be associated with increased risk of early onset OA (Lohmander et al., 2004; von Porat et al., 2004), it was expected that the moments at the knee would be greater for the ACLR knees, indicating higher loading for this group of knees. However, the moments of the ACLR knees were shown to be lower during the activities studied. It is possible that the amount of loading at the knee is not the initiating factor for the development of premature OA, but rather kinematic (Scanlan et al., 2010; Papannagari et al., 2006) and even biological changes (Marks and Donaldson, 2005) following injury and surgery. Nevertheless, knee moments and kinematics are closely linked (Schipplein and Andriacchi 1991; Andriacchi and Dyrby, 2005), and kinematics have been shown to be altered following ACL reconstruction (Scanlan et al., 2010; Papannagari et al., 2006). Also, it is likely that as OA develops over time, the external moments at the knee will become a significant contributor to the progression of the disease (Miyazaki et al., 2002).
As the contralateral knees exhibited greater moments compared to both the ACLR and control knees, it appears that they are providing compensation for the ACLR knees in order to account for a lack of adequate function such as: stability, muscular strength, proprioception etc. This was especially true during stair ascent and descent as differences in peak knee moments between ACLR and contralateral knees were more pronounced than during level gait. This is likely due to the greater muscular demand during these activities (Taylor et al., 2004). Thus restoration of muscle function of the ACLR knees may not have reached normal levels at approximately 26 months after reconstruction.
Altered moments in the contralateral knees have implications on the development of OA as well (Andriacchi et al., 2004). Although the rate of incidence was much higher for ACLR knees, Lohmander et al. (2004) found radiographic osteoarthritic changes in both ACLR (55/67) and uninjured contralateral knees (19/65) in female soccer players at approximately twelve years following unilateral ACL reconstruction. Combined with the results of the current study, this suggests that changes in joint function and not only changes associated directly with the injury influence the development of early onset OA in this population.
The findings of this study must be interpreted in the context of this particular cohort. Specifically, graft type (Webster and Feller, 2011), graft orientation (Scanlan et al., 2009), and quadriceps strength (Bush-Joseph et al., 2001) have been associated with the moments at the knee following ACL reconstruction. Therefore, surgical technique and rehabilitation protocols likely have a direct effect on the knee moments following ACL reconstruction surgery and must be considered. Additionally, the consideration of the amount of time from injury and surgery must be considered when interpreting joint mechanics as other studies have shown greater joint moments in ACLR knees in populations further than from surgery than the current study (Butler et al., 2009). In spite of these limitations, the conclusions regarding a muscular deficit on the reconstructed side are consistent with clinical studies of quadriceps atrophy following ACL injury. Further, the conclusion of a compensatory adaptation of the contralateral knee to a deficit of the reconstructed knee is meaningful irrespective of the cause of the deficit on the reconstructed knee. Finally, it is important to note that the interpretation of the intersegmental forces at the knee solely based on external moments is limited because it does not take other factors that can affect the internal loading of the knee, such as co-contraction of the quadriceps and hamstrings muscles, into account. Additional studies utilizing EMG would be helpful in determining differences in co-contraction and better characterizing the intra-articular loading in an ACLR population during gait, stair ascent and descent. Also, additional studies are warranted to understand the mechanical mechanism behind the differences in knee moments between the ACLR and contralateral knees. A better understanding of the loading at the knee would possibly allow for improved restoration of knee function after ACL injury and long term joint health.
This study provides a report of all three external moments at ACLR and contralateral knees during gait and stair locomotion, as well as reference moments of a healthy control population. In general, the peak knee moments of the ACLR knees were lower compared to contralateral knees. This result was due to differences in both ACLR and contralateral knees as ACLR knee moments were lower and contralateral knee moments were greater when compared to a healthy control population. The contralateral knees appear to be functioning in such a way as to compensate for the lower moments at the ACLR knees. These changes in joint function in both knees are indicative of altered loading conditions, which have been suggested as a contributor to the development of early onset osteoarthritis of the knee following ACL injury (Andriacchi et al., 2004).
ACKNOWLEDGEMENTS
This study was funded by AR039421 from the National Institute of Health. Support was also provided by the Department of Veterans Affairs. The authors would also like to thank Katerina Blazek, Jessica Asay, Barbara Elspas, Chris Dyrby, and Charlene Sellers for their assistance in patient recruitment and testing.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflict of interest to disclose.
REFERENCES
- 1.Andriacchi TP, Mundermann A, Smith RL, Alexander EJ, Dyrby CO, Koos S. A framework for the in vivo patho-mechanics of osteoarthritis at the knee. Annals of Biomedical Engineering. 2004;32(3):447–457. doi: 10.1023/b:abme.0000017541.82498.37. [DOI] [PubMed] [Google Scholar]
- 2.Andriacchi TP, Alexander EJ, Toney MK, Dyrby CO, Sum J. A point cluster method for in vivo motion analysis: applied to a study of knee kinematics. Journal of Biomechanical Engingeering. 1998;120:743–749. doi: 10.1115/1.2834888. [DOI] [PubMed] [Google Scholar]
- 3.Andriacchi TP, Dyrby CO. Interactions between kinematics and loading during walking for the normal and ACL deficient knee. Journal of Biomechanics. 2005;38:293–298. doi: 10.1016/j.jbiomech.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Andriacchi TP, Johnson TS, Hurwit DE, Nataraja RN. Musculoskeletal dynamics, locomotion, and clinical applications. In: Mow VC, Huiskes R, editors. Basic Orthopaedic Biomechanics and Mechano-Biology. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. pp. 91–122. [Google Scholar]
- 5.Andriacchi TP, Mundermann A. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Current Opinion in Rheumatology. 2006;18(5):514–518. doi: 10.1097/01.bor.0000240365.16842.4e. [DOI] [PubMed] [Google Scholar]
- 6.Astephen J, Deluzio K, Caldwell G, Dunbar M, Hubley-Kozey C. Gait and neuromuscular pattern changes are associated with differences in knee osteoarthritis severity levels. Journal of Biomechanics. 2008;41:868–876. doi: 10.1016/j.jbiomech.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 7.Boyer KA, Angst MS, Asay J, Giori NJ, Andriacchi TP. Sensitivity of gait parameters to the effects of anti-inflammatory and opioid treatments in knee osteoarthritis patients. Journal of Orthopedic Research. 2011;30(7):1118–11124. doi: 10.1002/jor.22037. [DOI] [PubMed] [Google Scholar]
- 8.Bush-Joseph C, Hurwitz D, Patel R, Bahrani Y, Garretson R, Bach B, Andriacchi TP. Dynamic function after anterior cruciate ligament reconstruction with autologous patellar tendon. American Journal of Sports Medicine. 2001;29(1):36–41. doi: 10.1177/03635465010290011101. [DOI] [PubMed] [Google Scholar]
- 9.Butler RJ, Minick KI, Ferber R, Underwood F. Gait mechanics after ACL reconstruction: implications for the early onset of knee osteoarthritis. British Journal of Sports Medicine. 2009;43:366–370. doi: 10.1136/bjsm.2008.052522. [DOI] [PubMed] [Google Scholar]
- 10.D’Lima D, Shantanu P, Steklov N, Slamin J, Colwell C. Tibial forces measured in vivo after total knee arthroplasty. Journal of Arthroplasty. 2006;21(2):255–262. doi: 10.1016/j.arth.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 11.Dempster WT, Gaughran GR. Properties of body segments based on height and weight. American Journal of Anatomy. 1967;120:33–54. [Google Scholar]
- 12.Dye S, Wojtys E, Fu F, Fithian D, Gillquist J. Factors contributing to function of the knee joint after injury or reconstruction of the anterior cruciate ligament. Journal of Bone and Joint Surgery. 1999;80A:1380–1393. [PubMed] [Google Scholar]
- 13.Dyrby CO, Andriacchi TP. Secondary motions of the knee during weight bearing and non-weight bearing activities. Journal of Orthopedic Research. 2004;22:794–800. doi: 10.1016/j.orthres.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 14.Erhart JC, Dyrby CO, D’Lima DD, Colwell C, Andriacchi TP. Changes in in vivo knee loading with a variable-stiffness intervention shoe correlate with changes in the knee adduction moment. Journal of Orthopedic Research. 2010;28(12):1548–1553. doi: 10.1002/jor.21183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henriksen M, Hinman RS, Creaby MW, Cicuttini F, Metcalf BR, Bowled KA, Bennell KL. Rotational knee load predicts cartilage loss over 12 months in knee osteoarthritis. Proceedings of the 2012 World Congress on OA. 2012;20(1):S17–S18. [Google Scholar]
- 16.Hooper D, Morrissey M, Drechsler W. Gait analysis 6 and 12 months after anterior cruciate ligament reconstruction surgery. Clinical Orthopaedics and Related Research. 2002;403:168–178. doi: 10.1097/00003086-200210000-00025. [DOI] [PubMed] [Google Scholar]
- 17.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis and Rheumatology. 2004;50:3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 18.Marks PH, Donaldson MLC. Inflammatory cytokine profiles associated with chondral damage in the anterior cruciate ligament-deficient knee. Journal of Arthroscopy and Related Surgery. 2005;21(11):1342–1347. doi: 10.1016/j.arthro.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 19.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Annals of the Rheumatic Diseases. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mundermann A, Dyrby CO, Hurwitz DE, Sharma L, Andriacchi TP. Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity: reduced walking speed. Arthritis and Rheumatology. 2004;50:1172–1178. doi: 10.1002/art.20132. Erratum in: Arthritis and Rheumatology. 2004;50:4073. [DOI] [PubMed] [Google Scholar]
- 21.Papannagari R, Gill T, DeFrate LE, Moses JM, Petruska A, Li G. In vivo kinematics of the knee after anterior cruciate ligament reconstruction. American Journal of Sports Medicine. 2006;34(12):2006–2012. doi: 10.1177/0363546506290403. [DOI] [PubMed] [Google Scholar]
- 22.Scanlan SF, Chaudhari AMW, Dyrby CO, Andriacchi TP. Differences in tibial rotation during walking in ACL reconstructed and healthy contralateral knees. Journal of Biomechanics. 2010;43:1817–1822. doi: 10.1016/j.jbiomech.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scanlan SF, Blazek K, Chaudhari AMW, Safran MR, Andriacchi TP. Graft orientation influences the knee flexion moment during walking in patients with anterior cruciate ligament reconstruction. American Journal of Sports Medicine. 2009;37(11):2173–2178. doi: 10.1177/0363546509339574. [DOI] [PubMed] [Google Scholar]
- 24.Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during walking. Journal of Orthopedic Research. 1991;9:113–119. doi: 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- 25.Sharma L, Hurwitz DE, Thonar EJ, Sum JA, Lenz ME, Dunlop DD, Schnitzer TJ, Kirwan-Mellis G, Andriacchi TP. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis and Rheumatology. 1998;41:1233–1240. doi: 10.1002/1529-0131(199807)41:7<1233::AID-ART14>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 26.Tashman S. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. American Journal of Sports Medicine. 2004;32(4):975–983. doi: 10.1177/0363546503261709. [DOI] [PubMed] [Google Scholar]
- 27.Taylor WR, Heller MO, Bergmann G, Duda G. Tibio-femoral loading during human gait and stair climbing. Journal of Orthopedic Research. 2004;22:625–632. doi: 10.1016/j.orthres.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 28.von Porat A, Roos E, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Annals of the Rheumatic Diseases. 2004;63(3):269–273. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walter J, D’Lima D, Colwell C, Fregly B. Decreased knee adduction moment does not guarantee decreased medial contact force during gait. Journal of Orthopedic Research. 2010;28(10):1348–1354. doi: 10.1002/jor.21142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Webster K, Wittwer J, O’Brien J, Feller J. Gait patterns after anterior cruciate ligament reconstruction are related to graft type. American Journal of Sports Medicine. 2005;33(2):247–254. doi: 10.1177/0363546504266483. [DOI] [PubMed] [Google Scholar]
- 31.Webster K, Feller J. The knee adduction moment in hamstring and patellar tendon anterior cruciate ligament reconstructed knees. Knee Surgery, Sports Traumatology, Arthroscopy. 2011 Dec 24; doi: 10.1007/s00167-011-1835-z. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]