Abstract
OBJECTIVE
To assess the impact of early hypertension (HT) control on occurrence of subsequent major cardiovascular events in those with diabetes and recent-onset HT.
RESEARCH DESIGN AND METHODS
Study subjects were 15,665 adults with diabetes but no diagnosed coronary or cerebrovascular disease at baseline who met standard criteria for new-onset HT. Poisson regression models assessed whether adequate blood pressure control within 1 year of HT onset predicts subsequent occurrence of major cardiovascular events with and without adjustment for baseline Framingham Risk Score (FRS) and other covariates.
RESULTS
Mean age was 51.5 years, and mean blood pressure at HT onset was 136.8/80.8 mmHg. In the year after HT onset, mean blood pressure decreased to 131.4/78.0 mmHg and was <130/80 mmHg in 32.9% of subjects and <140/90 mmHg in 80.2%. Over a mean follow-up of 3.2 years, age-adjusted rates of major cardiovascular events in those with mean 1-year blood pressure measurements of <130/80, 130–139/80–89, and ≥140/90 mmHg were 5.10, 4.27, and 6.94 events/1,000 person-years, respectively (P = 0.004). In FRS-adjusted models, rates of major cardiovascular events were significantly higher in those with mean blood pressure ≥140/90 mmHg in the first year after HT onset (rate ratio 1.30 [95% CI 1.01–1.169]; P = 0.04).
CONCLUSIONS
Failure to adequately control BP within 1 year of HT onset significantly increased the likelihood of major cardiovascular events within 3 years. Prompt control of new-onset HT in patients with diabetes may provide important short-term clinical benefits.
The impact of blood pressure reduction on cardiovascular outcomes in patients with type 2 diabetes remains an important clinical and research topic. The UK Prospective Diabetes Study (UKPDS) addressed blood pressure control in patients recently given a diagnosis of diabetes and showed that better blood pressure control reduced the likelihood of cardiovascular events, with an achieved systolic blood pressure (SBP) of 144 mmHg in the intensive arm versus 154 mmHg in the usual-care arm (1,2).
However, several important clinical questions related to treatment of hypertension (HT) in patients with diabetes remain unanswered and are addressed in this report (3–11). First, does early control of HT in patients with diabetes reduce the subsequent occurrence of major cardiovascular events? Second, how long does it take for patients with diabetes and new-onset HT to benefit from lowering of elevated blood pressure? Third, are the putative benefits of early blood pressure control similar in all diabetic patients or do they vary by demographics, baseline cardiovascular risk, or the presence of microvascular complications at HT onset?
Results of these analyses may help providers who make clinical recommendations for the management of blood pressure in patients with type 2 diabetes. This study is especially timely because of the currently active evaluation of blood pressure treatment benefits in type 2 diabetes based on the results of the ACCORD and ADVANCE studies (12,13).
RESEARCH DESIGN AND METHODS
Hypotheses
We hypothesized that blood pressure control in the first year after HT onset would significantly reduce the occurrence of major cardiovascular events (e.g., stroke, myocardial infarction) in a relatively short time. We further hypothesized that such benefits would vary by level of baseline cardiovascular disease (CVD) risk, the presence of microvascular complications of diabetes at HT onset, and the degree of blood pressure control during the first year after HT onset.
Study design and data sources
This retrospective cohort analysis is derived from the Cardiovascular Hypertension Registry of the Cardiovascular Research Network and includes data on all patients identified with HT between 1 January 2003 and 31 December 2009 at one of three integrated health care–delivery systems: HealthPartners, Kaiser Permanente Colorado, and Kaiser Permanente Northern California. Blood pressure readings were most often recorded by nursing staff, who were trained at all three sites in standardized measurement of blood pressure, or by primary care physicians. During the study, nearly all measures of blood pressure were performed manually with aneroid sphygmomanometers rather than digital devices after patients were seated for 5 min in the exam room. Blood pressure readings obtained during emergency department visits, urgent care visits, and hospital admissions were excluded from consideration because they may be influenced by acute conditions and be either higher or lower than blood pressure readings obtained at office visits. The structure of the Cardiovascular Hypertension Registry has previously been described (14,15).
Data collected for the Cardiovascular Hypertension Registry and used in this analysis were extracted from electronic health record (EHR) databases. These included age, sex, race/ethnicity, all ambulatory SBP and diastolic blood pressure (DBP) values, smoking status, height, weight, A1C levels, lipid values, medications (all HT and glucose-control and lipid-control medications), number of primary care and subspecialty care visits per year, and procedure and diagnosis codes related to stroke or myocardial infarction. All three study sites use the EpiCare (Epic Systems, Verona, WI) EHR, and data were extracted from Clarity databases using information system software. Claims databases were also reviewed to ensure complete ascertainment of cardiovascular events because events that occur at hospitals outside the usual care-delivery system may not appear in the EHR but can be identified using claims data.
To confirm that the algorithms designed to identify hypertensive patients were valid and that the analytic data accurately reflected the source data, trained nurse or physician chart auditors conducted a chart review of 450 randomly selected charts (150 from each site). We confirmed that HT onset had, in fact, been documented on the date assigned by the algorithm in 96% of cases and that agreement on blood pressure values between the analytic database and chart records was 98%.
Study subjects and date of HT onset
Study subjects in the Cardiovascular Hypertension Registry had to meet all of these additional criteria to be included in the analyses reported here: 1) meet the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7) criteria for HT based on two consecutive elevated office blood pressure readings (with SBP ≥130 mmHg, DBP ≥80 mmHg, or both) between 1 January 2003 and 31 December 2009, with at least one calendar year of antecedent data that included no evidence of HT; 2) be age 30–74 years on date of HT onset; 3) meet the study definition of diabetes on or before HT onset, or 4) have no evidence of diagnosed cardiovascular comorbid conditions (ICD-9 410–414, 427, 428, 430–436, and 440–443) before HT onset.
We excluded all patients with a diagnosis code for HT or a filled prescription for any blood pressure–lowering medication (even if purportedly given for a different clinical condition) in the year before the date of entry into the Cardiovascular Hypertension Registry because these subjects could not be considered to have new-onset HT. Subjects who had <1 year of follow-up after HT onset were also excluded. Remaining study subjects were then assigned a date of HT onset, defined as the date of their entry into the Cardiovascular Hypertension Registry. In addition, to be included in the analysis, subjects must have had at least two blood pressure readings within 1 year of HT onset to enable classification of blood pressure control status.
Variable definitions
Diabetes status.
Subjects were classified as having diabetes if, in the year before HT onset, they had 1) either one or more inpatient or two or more outpatient ICD-9 codes for diabetes (codes 250.xx), 2) a filled prescription for a diabetes-specific medication, or 3) two or more fasting glucose values ≥126 mg/dL or one or more A1C values ≥7% (16). Subjects whose filled prescription was for either metformin or a thiazolidinediones were required to also have at least one inpatient or outpatient diabetes diagnosis code. Those with diagnosis codes for gestational diabetes mellitus in the year before or after HT onset were excluded from the analysis. The presence of microvascular diabetes complications at baseline was quantified using the Diabetes Complications Severity Index (17).
Blood pressure control status in the year after HT onset.
The mean of office SBP and DBP in the year after HT onset was used to classify subjects according to blood pressure status. Study subjects were classified into one of three categories: 1) mean SBP <130 mmHg and mean DBP <80 mmHg, 2) mean SBP ≥140 mmHg or mean DBP ≥90 mmHg, or 3) all other. Two or more blood pressure measures in the year were required to calculate blood pressure control status.
Baseline cardiovascular risk.
We elected to use the 10-year Framingham Risk Score (FRS) to quantify baseline cardiovascular risk because the model is well established in the literature; is based on U.S. data; has recently been updated to allow separate estimation of CVD, coronary heart disease, stroke, and congestive heart failure risk; and does not require patient-reported data. We used the version of the FRS that assesses risk of 10-year CVD, including both heart attacks and strokes, based on age, sex, current smoking status, SBP, antihypertension medication treatment, total cholesterol, HDL cholesterol, and diabetes status, as described by D’Agostino et al. (17) Age range in the current study was limited to the age range of 30–74 years used by FRS. Patients with missing values used to construct the FRS were excluded from analysis. More detailed variable definitions are included in Supplementary Fig. 1.
Major cardiovascular events and outcomes.
The dependent variable in the main analysis is time from the date 1 year after HT onset to date of first occurrence of hemorrhagic stroke (430, 431, 432, and 432.9), ischemic stroke (433, 434, 43-001, 43401, 4341-001, 43411, 43491, and 436), or acute myocardial infarction (410.xx and 41000–41090). Only inpatient ICD-9 diagnosis codes were used to ascertain these events. We combined ischemic stroke and hemorrhagic stroke because the rate of hemorrhagic stroke was relatively low. We also examined a composite outcome of these three types of major cardiovascular events. Note that follow-up time began 1 year after HT onset and ended at the first event or censored date.
Plan of analysis
Consistency of data was analyzed across the three sites, and pooled baseline data are presented as means ± SD for continuous variables and frequency distribution for categorical variables. Age-adjusted association of blood pressure control status, treatment initiation, HT recognition, and SBP at onset with occurrence of a major cardiovascular event was analyzed using Poisson regression models. Age-adjusted incident cardiovascular event rates and 95% CIs are presented per 1,000 person-years. Age was included as a linear predictor. Resulting rate ratios (RRs) are equivalent to hazard RRs when rate is constant over the follow-up time, which was true in our analysis. We separately analyzed whether blood pressure control, defined as <130/80 vs. <140/90 mmHg, was associated with occurrence of major cardiovascular events using a Poisson regression model that included FRS, microvascular diabetes complications score, and site. A second model was constructed that included individual risk factors rather than the FRS.
RESULTS
Supplementary Fig. 2 shows inclusion and exclusion of study subjects as a flowchart. From 2003 to 2009, we identified 21,705 subjects with HT onset, of whom 18,842 were ages 30–74 years and had no cardiovascular comorbid condition and, therefore, were eligible for inclusion. Subjects were excluded 1) if either of the two dates of data needed to define HT onset were not specified in the data tables (n = 94), 2) if fewer than two blood pressure measurements were done within 1 year of HT onset (n = 269), or 3) if enrollment ended within 1 year of HT onset (i.e., before the beginning of follow-up time for events) (n = 2,241). Final analytic sample size was 15,665 subjects. Baseline characteristics of patients with no blood pressure in the first year or with no follow-up time were similar to those included in the analysis. The median number of blood pressure measures used to classify blood pressure status in the follow-up period was four. Subjects with missing risk factor values (3.5%) had similar demographics and blood pressure measures at onset but a higher occurrence of major cardiovascular events (10.0 vs. 5.9 per 1,000 person-years).
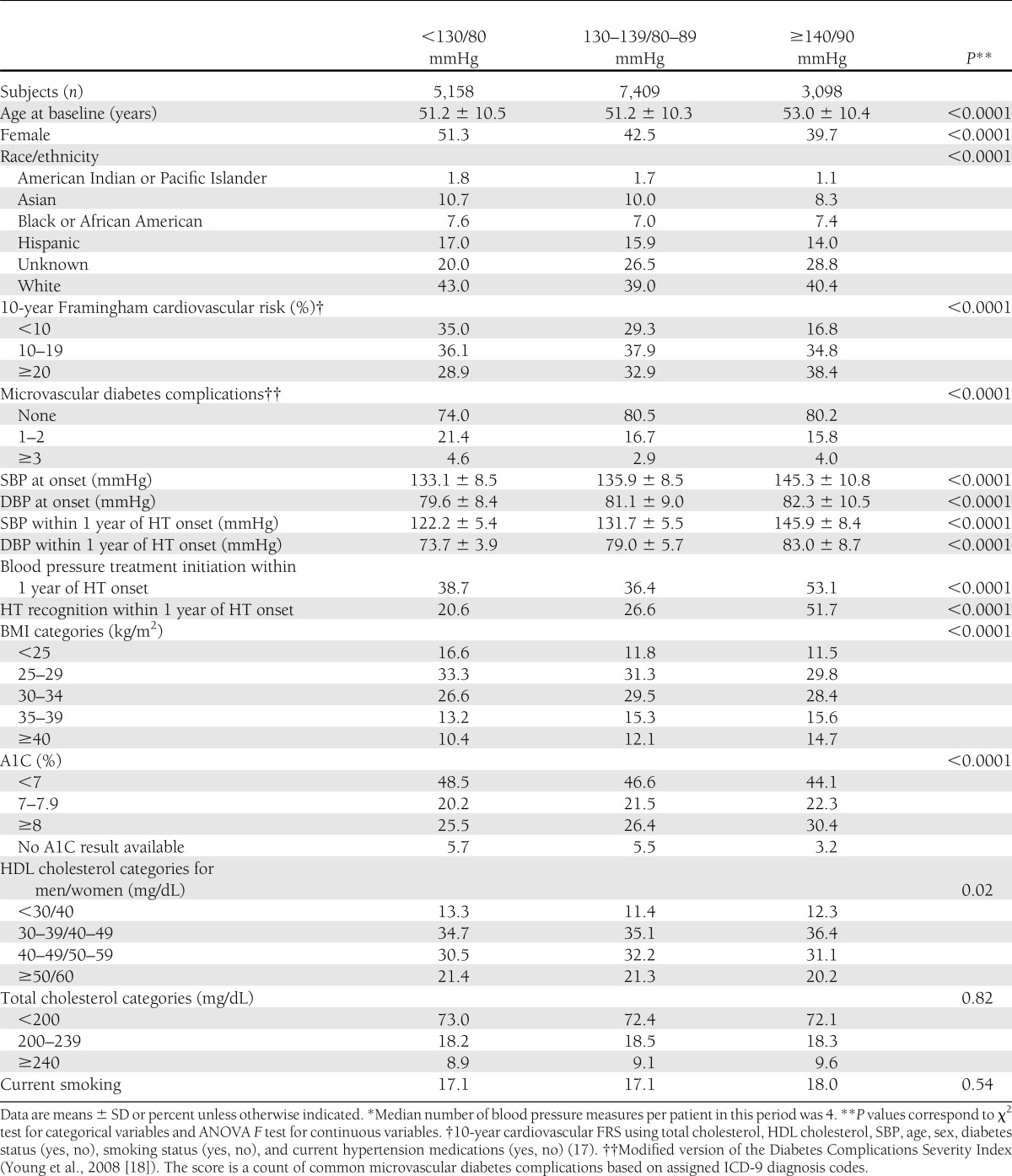
Table 1 shows baseline and follow-up characteristics of study subjects classified by achieved blood pressure levels in the year after HT onset. Compared with patients with blood pressure <130/80 mmHg, patients with blood pressure ≥140/90 mmHg were older (53 vs. 51 years) and more likely to be male (39.7 vs. 51.3%) with higher 10-year FRS (23.1 vs. 16.5%), higher SBP (145.3 vs. 133.1 mmHg), and higher DBP (82.3 vs. 79.6 mmHg) at HT onset. Patients with blood pressure in the 130–139/80–89 mmHg range had risk factor patterns that resembled those of patients with blood pressure <130/80 mmHg.
Table 1.
Characteristics of patients with diabetes and new-onset hypertension classified by blood pressure control status in the year after date of onset*
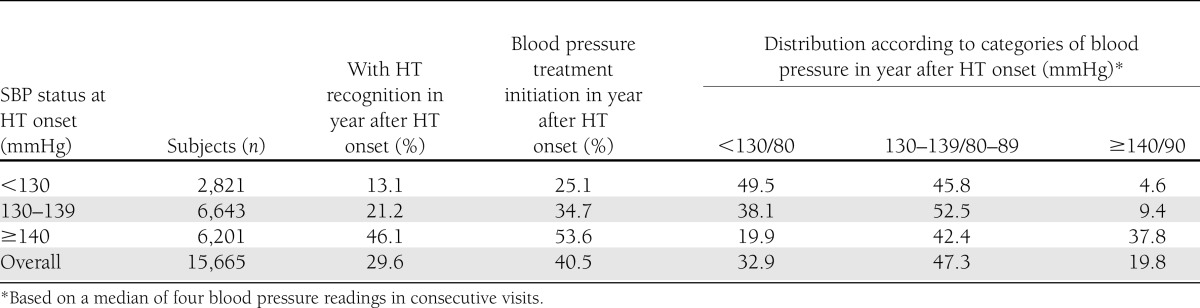
In the first year after new-onset HT, 32.9% of subjects had mean blood pressure <130/80 mmHg and 80.2% had mean blood pressure <140/90 mmHg, leaving 19.8% with mean blood pressure ≥140/90 mmHg (Table 2). Blood pressure control (<130/80 mmHg) was similar in those initiating (31.5%) versus not initiating (33.9%) blood pressure–lowering medication. Rates of HT recognition and initiation of blood pressure–lowering medications increased, while rates of blood pressure control decreased with higher SBP levels at HT onset.
Table 2.
Percent of subjects with hypertension recognition, treatment initiation, and categories of blood pressure in the year after hypertension onset in patients with diabetes
Age-adjusted rates of major cardiovascular events over a mean of 3.2 years (38 months) of follow-up are reported in Table 3. Lower SBP at HT onset and better blood pressure control status in the first year after HT onset were associated with fewer major cardiovascular events and fewer myocardial infarctions. However, HT recognition and treatment initiation in the first year were not associated with subsequent cardiovascular events.
Table 3.
Age-adjusted rates of major cardiovascular events per 1,000 person-years of follow-up time as a function of SBP at HT onset and of the three measures in the year after hypertension onset: hypertension control status, medication initiation, and recognition
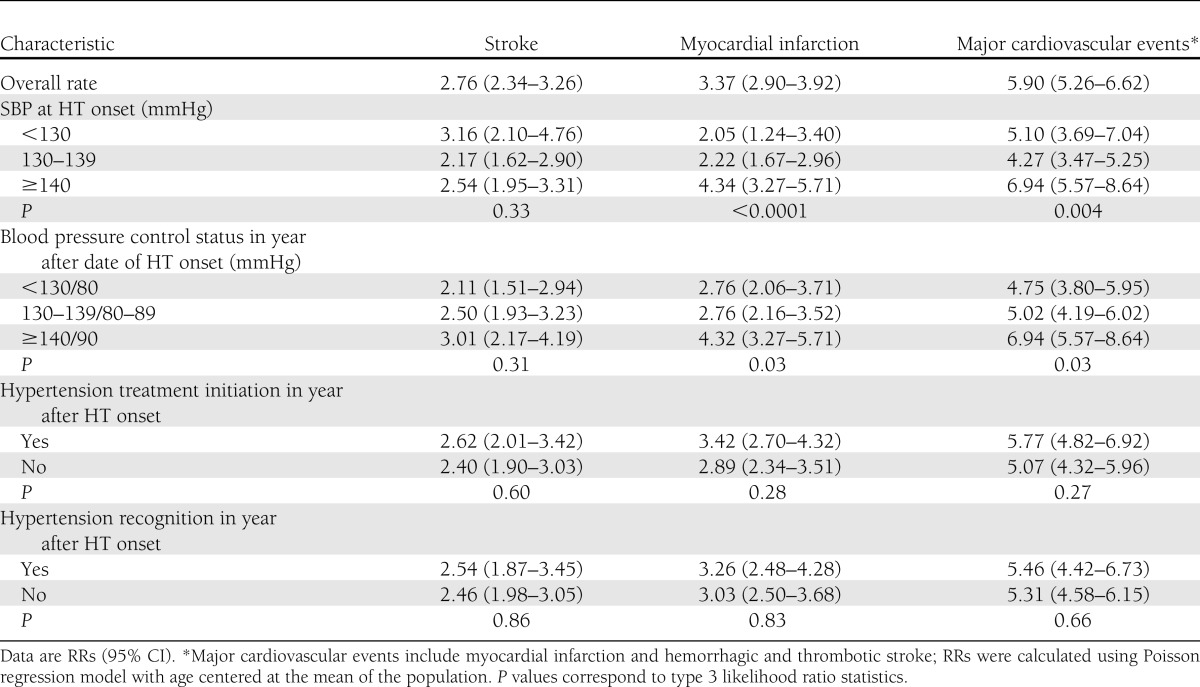
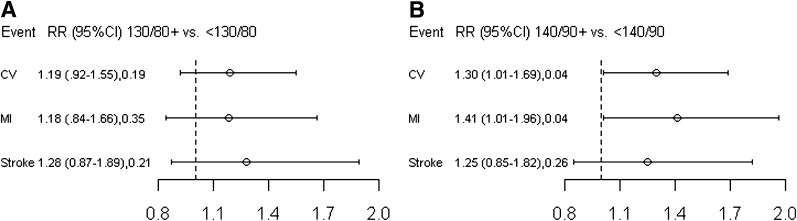
Figure 1 presents the incidence RRs (95% CI) of the fully adjusted models for stroke, myocardial infarction, and all CVD events 1) comparing sustained HT blood pressure (≥140/90 mmHg) with blood pressure control (<140/90 mmHg) and 2) comparing sustained HT blood pressure (≥130/80 mmHg) with blood pressure control (<130/80 mmHg) after adjustment for baseline FRS (which includes age, sex, SBP, total cholesterol, HDL cholesterol, presence of diabetes, smoking status, and HT treatment), study site, and microvascular diabetes complications. Similar results were observed in separate models that adjusted for cardiovascular risk factors independently (SBP, HDL cholesterol, smoking, age, and sex) rather than adjusting for them in the aggregate using the FRS (data not shown). Subjects with sustained blood pressure ≥140/90 mmHg, compared with those with blood pressure <140/90 mmHg in the first year after HT onset, had higher likelihood of subsequent stroke (RR 1.25 [95% CI 0.85–1.82], P = 0.26), myocardial infarction (1.41 [1.01–1.96], P = 0.04), and any cardiovascular event (1.30 [1.01–1.69], P = 0.04). RRs were smaller and not statistically significant when comparing major cardiovascular event rates of those with blood pressure ≥130/80 mmHg versus those with blood pressure <130/80 mmHg.
Figure 1.
Adjusted incidence RRs (95% CI) for stroke, myocardial infarction (MI), and other major cardiovascular (CV) events estimated based on mean level of blood pressure control in the year after hypertension onset. Categories of blood pressure control in the year after hypertension onset include the following: above versus below 130/80 mmHg (A) and above versus below 140/90 mmHg (B). Major cardiovascular events are defined as myocardial infarction, hemorrhagic stroke, or thrombotic stroke in the mean 38-month follow-up period. Poisson regression models included FRS, microvascular diabetes complications, and site.
We evaluated whether benefits of early blood pressure control vary significantly by baseline FRS or baseline presence of microvascular diabetes complications. In stratified analysis, the absolute number of events prevented by early blood pressure control was highest among those with FRS ≥20% (blood pressure <130/80 mmHg, 6.8/1,000 person-years, vs. blood pressure ≥140/90, 10.6/1,000 person-years) and lower among those with FRS <10% (3.4 vs. 5.8/1,000 person-years), with P = 0.14. Similar results were observed for microvascular diabetes complications, with no significant effect modification (P = 0.25).
CONCLUSIONS
In adults with diabetes, adequate blood pressure control in the first year after HT onset was associated with lower rates of any subsequent major cardiovascular event or myocardial infarction (but not with lower rates of stroke) in the 38-month mean follow-up period when analyzed in multivariable models. Compared with patients with mean blood pressure <140/90 mmHg, those with mean blood pressure ≥140/90 mmHg during the first year after HT onset had higher rates of major cardiovascular events (RR 1.30 [95% CI 1.01–1.69]; P = 0.04). These data support the hypothesis that adequate blood pressure control within a year of HT onset is an important clinical goal and suggest that achieving blood pressure <140/90 mmHg may confer most of the short-term benefits available from blood pressure lowering in such patients.
The observation that blood pressure control within the first year after HT onset may influence rates of some major cardiovascular events within 38 months of mean follow-up suggests that insufficient attention has been devoted to the aggressive early management of blood pressure in patients with diabetes. The study subjects were relatively young at HT onset, with a mean age of 52 years, and important clinical effects detected after only 3 years of follow-up may become more pronounced over a longer follow-up period.
Degree of initial blood pressure elevation at HT onset, baseline FRS, and baseline severity of diabetes all predict greater likelihood of subsequent cardiovascular events in the next 3 years. Although the relative risk of cardiovascular events in relation to degree of HT control was similar across strata of FRS and microvascular diabetes complications, subgroups of diabetic patients with higher absolute baseline cardiovascular risks may benefit the most from early blood pressure control. Resolution of this issue is not possible in this study owing to limited power, so larger or longer studies are needed to fully resolve this clinical question.
Many patients with baseline SBP elevations of 130–139 mmHg reverted to normal levels of blood pressure within the first year without identification or treatment. This suggests that JNC-7 diagnostic criteria for HT for those with diabetes (two consecutive blood pressure measurements of ≥130/80 mmHg on different days) may identify many patients whose office blood pressure elevations reflect transiently elevated blood pressure related to cooccurrence of a time-limited medical or psychological condition such as pain or stress.
Several factors constrain the interpretation of our data. First, the observational study design precludes causal inference. Second, generalizability may be limited because study subjects were insured patients receiving care at only three health systems. Third, routine blood pressure measures obtained at community clinics are subject to rounding errors and other sources of inaccuracy (19,20). However, study sites used defined blood pressure measurement protocols and, periodically, trained nursing staff in blood pressure measurement. In addition, we classified onset of HT and HT control status based on multiple blood pressure readings to attenuate misclassification related to measurement error. Fourth, our ascertainment of incident cardiovascular events may be incomplete. However, incomplete ascertainment of myocardial infarction and stroke is likely to be minimal when both clinical and claims data are available, as they were in this study.
In summary, among adults with diabetes, control of blood pressure to <140/90 mmHg within 1 year of HT onset significantly reduced the likelihood of major cardiovascular events within the next 3 years. Prompt identification and control of HT in patients with diabetes may provide very important short-term clinical benefits.
Supplementary Material
Acknowledgments
This project was funded under contract no. HHSA290-2005-0033I from the Agency for Healthcare Research and Quality (AHRQ), Department of Health and Human Services (DHHS), as part of the Developing Evidence to Inform Decisions about Effectiveness (DEcIDE) program.
No potential conflicts of interest relevant to this article were reported.
P.J.O. wrote the manuscript and obtained funding. G.V.-B. analyzed data, drafted RESEARCH DESIGN AND METHODS and RESULTS, and edited and reviewed the manuscript. J.A.S., E.D.P., J.R.D., and K.L.M. reviewed and edited the manuscript. N.K.T. analyzed data. D.J.M. reviewed and edited the manuscript and obtained funding. P.J.O. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
The authors of this report are responsible for its content. Statements in the report should not be construed as endorsed by the AHRQ or the DHHS.
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc12-0284/-/DC1.
References
- 1.UK Prospective Diabetes Study Group Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. BMJ 1998;317:713–720 [PMC free article] [PubMed] [Google Scholar]
- 2.Holman RR, Paul SK, Bethel MA, Neil HA, Matthews DR. Long-term follow-up after tight control of blood pressure in type 2 diabetes. N Engl J Med 2008;359:1565–1576 [DOI] [PubMed] [Google Scholar]
- 3.Tuomilehto J, Rastenyte D, Birkenhäger WH, et al. Systolic Hypertension in Europe Trial Investigators Effects of calcium-channel blockade in older patients with diabetes and systolic hypertension. N Engl J Med 1999;340:677–684 [DOI] [PubMed] [Google Scholar]
- 4.Hansson L, Zanchetti A, Carruthers SG, et al. HOT Study Group Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet 1998;351:1755–1762 [DOI] [PubMed] [Google Scholar]
- 5.Zanchetti A, Hansson L, Clement D, et al. HOT Study Group Benefits and risks of more intensive blood pressure lowering in hypertensive patients of the HOT study with different risk profiles: does a J-shaped curve exist in smokers? J Hypertens 2003;21:797–804 [DOI] [PubMed] [Google Scholar]
- 6.UK Prospective Diabetes Study Group Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703–713 [PMC free article] [PubMed] [Google Scholar]
- 7.Schrier RW, Estacio RO, Jeffers B. Appropriate blood pressure control in NIDDM (ABCD) Trial. Diabetologia 1996;39:1646–1654 [DOI] [PubMed] [Google Scholar]
- 8.Estacio RO, Jeffers BW, Hiatt WR, Biggerstaff SL, Gifford N, Schrier RW. The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin-dependent diabetes and hypertension. N Engl J Med 1998;338:645–652 [DOI] [PubMed] [Google Scholar]
- 9.Estacio RO, Jeffers BW, Gifford N, Schrier RW. Effect of blood pressure control on diabetic microvascular complications in patients with hypertension and type 2 diabetes. Diabetes Care 2000;23(Suppl. 2):B54–B64 [PubMed] [Google Scholar]
- 10.Cooper-DeHoff RM, Gong Y, Handberg EM, et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA 2010;304:61–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cushman WC, Evans GW, Byington RP, et al. ACCORD Study Group Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575–1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Curb JD, Pressel SL, Cutler JA, et al. Systolic Hypertension in the Elderly Program Cooperative Research Group Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. JAMA 1996;276:1886–1892 [PubMed] [Google Scholar]
- 13.Patel A, MacMahon S, Chalmers J, et al. ADVANCE Collaborative Group Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet 2007;370:829–840 [DOI] [PubMed] [Google Scholar]
- 14.Selby JV, Lee J, Swain BE, et al. Trends in time to confirmation and recognition of new-onset hypertension, 2002-2006. Hypertension 2010;56:605–611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maddox TM, Ross C, Tavel HM, et al. Blood pressure trajectories and associations with treatment intensification, medication adherence, and outcomes among newly diagnosed coronary artery disease patients. Circ Cardiovasc Qual Outcomes 2010;3:347–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Connor PJ, Rush WA, Pronk NP, Cherney LM. Identifying diabetes mellitus or heart disease among health maintenance organization members: sensitivity, specificity, predictive value, and cost of survey and database methods. Am J Manag Care 1998;4:335–342 [PubMed] [Google Scholar]
- 17.Young BA, Lin E, Von Korff M, et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care 2008;14:15–23 [PMC free article] [PubMed] [Google Scholar]
- 18.D’Agostino RB, Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008;117:743–753 [DOI] [PubMed] [Google Scholar]
- 19.Verberk WJ, Kroon AA, Thien T, et al. Prevalence of the white-coat effect at multiple visits before and during treatment. J Hypertens 2006;24:2357–2363 [DOI] [PubMed] [Google Scholar]
- 20.Thavarajah S, White WB, Mansoor GA. Terminal digit bias in a specialty hypertension faculty practice. J Hum Hypertens 2003;17:819–822 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.