Abstract
OBJECTIVE
Research has shown that the potential risk for medication errors within the pediatric inpatient population is about 3 times as high as for adults; however, there is limited information regarding the impact of a pediatric pharmacist's contribution to decreasing medication errors and adverse drug events (ADEs). The purpose of this study was to record and analyze all interventions during a 2-month time span in a pediatric teaching hospital to determine the benefit of having a pediatrics-trained clinical pharmacist on the floor.
METHODS
Pediatric pharmacists prospectively collected data for all interventions and medication errors made between July 1 and August 31, 2010. The pediatric hospital comprises 87 beds, and data were collected during the influx of new pediatric resident interns on the general pediatric ward and pediatric and neonatal intensive care units.
RESULTS
During the study period, 1315 interventions were recorded, which is an average of 21 interventions per day. Most interventions were made through order entry. Errors made up 24.5% of all interventions, with the most common cause of error being prescribing. Physicians with the least amount of training made the most errors. Of order pages scanned, 5.9% contained an error in the order; however, only 0.2% of all errors reached the patient.
CONCLUSIONS
This study highlighted the impact a pediatric pharmacist can make on prevention of ADEs and medication errors. Only 0.2% of all errors made during the study period reached the patient owing to interventions made by the pediatric pharmacists, which shows a vast improvement in patient safety.
INDEX TERMS: hospital, medication errors, pediatrics
INTRODUCTION
The incidence of iatrogenic injuries due to medication errors and adverse events are common among hospitalized patients, and medication errors are often preventable.1,2 Multiple studies have evaluated the impact on various systems to reduce errors hospital-wide, including physician order entry, bar code scanning, automation, and the benefits of having a pharmacist in the adult intensive care unit.3–8 As more has been learned about preventing medication errors in the adult population during the past 20 to 30 years, attention has shifted to the pediatric population. Research has shown that the potential risk for medication errors within the pediatric inpatient population is about 3 times as high as that of their adult hospitalized counterparts.2,9
Several explanations have been cited in various literature reports regarding potential causes of increased medication errors and harm to children, including weight-based dosing and resultant calculation errors, medication formulations designed for adults, health care settings designed and built to best accommodate the adult population, inability for children to communicate effectively with providers regarding adverse events that may be occurring, and the inability for young children to tolerate physiologically a medication error owing to developing systems.2,9,10
Despite this information, there is a limited body of literature regarding the impact of a pediatric pharmacist's contribution to decreasing medication errors and adverse drug events (ADEs) in this high-risk population. The purpose of this study was to record and analyze all interventions during a 2-month time span in a pediatric teaching hospital to determine the benefit of having a pediatrics-trained clinical pharmacist on the floor. All interventions made by the pediatric pharmacists between July and August 2010 were prospectively recorded and analyzed. This time frame was chosen because it is often highlighted as the worst time to be checked into a teaching hospital owing to a 10% increase in fatal medication error rates, as compared to other months, due to the influx of inexperienced residents.11
MATERIALS AND METHODS
Our hospital is an 87-bed pediatric teaching hospital, attached to a 370-bed adult community hospital. The pharmacy department provides services 24 hours a day; however, decentralized pediatric coverage is provided for 16.5 hours a day (7:30 am-9 pm) Monday through Friday and for 8 hours a day on Saturday and Sunday, with the pediatric pharmacist being available by phone for questions after hours. The pediatric pharmacists are responsible for covering a 35-bed level III neonatal intensive care unit (NICU), a 9-bed pediatric intensive care unit (PICU), and 43 general inpatient pediatric beds, in addition to entering outpatient pediatric chemotherapy orders. Coverage consists of attending rounds, precepting pharmacy students and residents, and entering pediatric orders into the pharmacy computer system for all the pediatric units listed above.
Main pharmacy (centralized) services include dispensing any bulk medication items, filling for automated dispensing machines (ADMs), preparing intravenous admixtures, and processing pediatric orders from 9 pm to 7:30 am, as well as orders from the adult hospital from 11 pm to 7:30 am.
ADMs are used on all floors throughout the adult and pediatric hospitals. All medications for the patient are loaded in the ADM with the exception of bulk products and intravenous medications. Scanning technology is used to view orders from the nursing units for pharmacist order entry.
The medical staff comprises attending physicians and pediatric, family practice, and transitional year residents, as well as medical students. Pediatric residents cover all areas of the pediatric hospital, with general pediatrics accounting for the largest number of residents on the team. The general pediatric inpatient physician team consists of 2 attending physicians, 2 senior residents (second and/or third year), 4 intern residents (2 pediatric and 2 family practice or transitional year), and 2 to 4 medical students. In contrast, the PICU physician team is made up of 1 attending physician and 1 senior resident (second or third year). The NICU physician team consists of 2 attending physicians, 2 nurse practitioners, 1 senior resident (second or third year), and 1 intern resident. Rounding throughout the hospital occurs around the same time in all units, such that the pediatric pharmacist will often divide their time between the units by patient load, type of patients, and recommendations for patient care. If a pharmacy resident or student is on a pediatric rotation, he or she will also attend rounds. During the study time period, no pharmacy resident or student was on any of the pediatric services.
Data were collected prospectively from July 1, 2010, to August 31, 2010, by the 3 pediatric pharmacists. Any intervention made was recorded on a study intervention sheet and was logged into an Excel spreadsheet (Microsoft Corporation, Redmond, WA) by a single observer and coded as “yes” or “no” for having the potential to cause error or harm, or did result in an error to the patient. Interventions were defined as dose optimization, drug therapy recommendation, laboratory draw needed, error (prescribing/order entry/ administration), compatibility, drug administration question, drug information request, or other (Figure 1).
Figure 1.
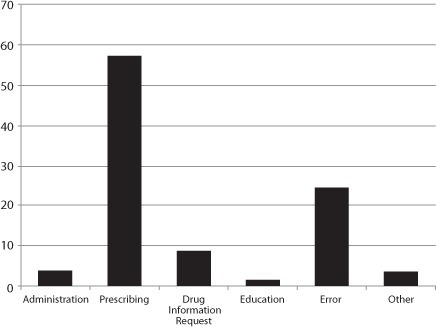
Type of pharmacy intervention.
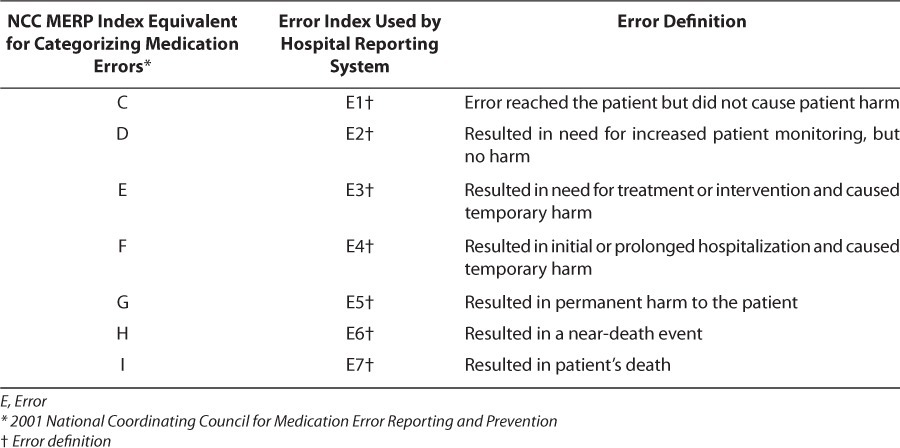
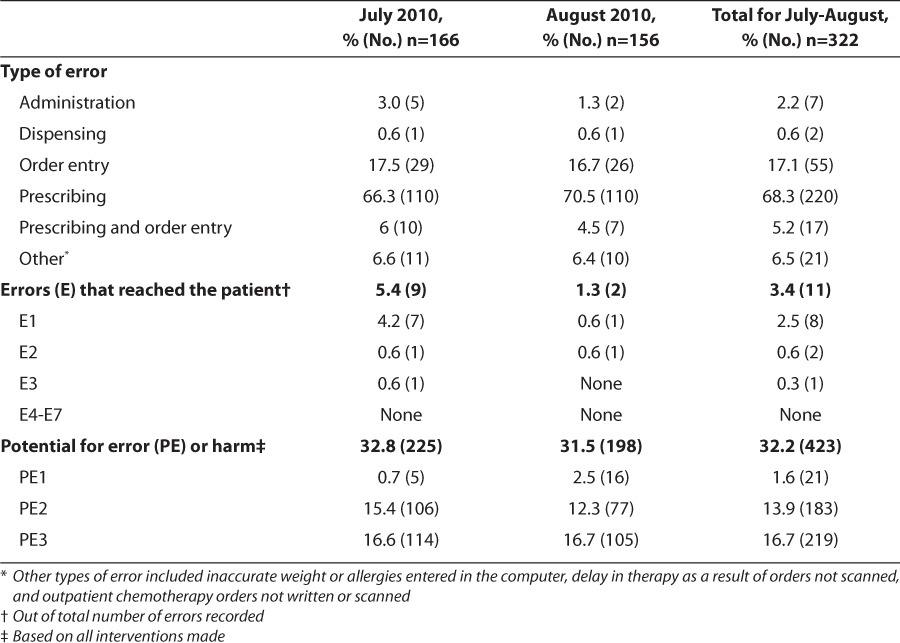
Errors were further broken down into potential errors that were prevented and did not reach the patient and errors that did reach the patient. Potential errors were coded PE1 through PE3 and are defined in Table 1. Errors were coded as E1 through E7 on the basis of the hospital's system for reporting errors. These are defined in Table 2.
Table 1.
Potential Error Definition
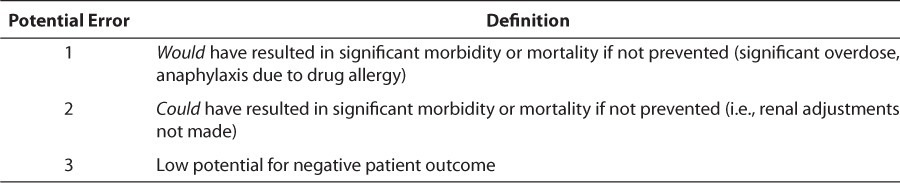
Table 2.
Error Definition
The interventions were logged into an Excel spreadsheet to determine the total number of interventions made during the study period. The information was further analyzed to determine the total number of errors that reached the patient, the errors that were prevented, as well as the potential for error or harm. In addition, the total number of pages ordered that were scanned into the pharmacy computer system were reviewed to determine an error rate per page scanned. The total number of individual medication orders was not available for analysis.
RESULTS
During a 2-month time span, a total of 1315 interventions were recorded by the pediatric pharmacists, which is an average of 21 interventions per day. The total number of order pages received during this time period was 7408; however, each order could have had multiple medications and the potential for multiple interventions. Given the limitations of the pharmacy computer database, the total number of individual orders could not be determined. Most images scanned (n=5432) were completed by the pediatric pharmacists and were eligible for inclusion of interventions. Order images completed by a non-pediatric pharmacist (1976) were excluded from the analysis of interventions because they were not involved in the study or tracking of interventions. Of the order pages included in the study, 5.9% contained an error in the order; however, only 0.2% of all errors reached the patient (Figure 2).
Figure 2.
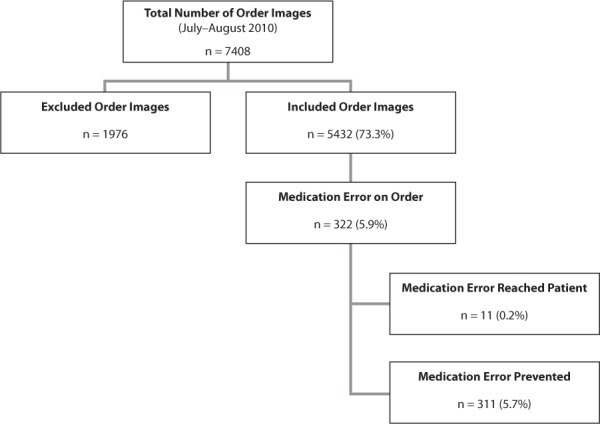
Order images and medication error rates.
Of the 11 errors (0.2%) that reached the patient, 1 was a dispensing error, 3 were nurse administration errors, and the remaining 7 were prescribing errors that were missed upon pharmacist order entry and verification. Of note, 4 of the prescribing errors resulted in a 2- to 4-fold overdose or underdose, whereby the patient received more than 1 dose before the error was discovered.
The general pediatric ward accounted for the largest number of interventions at 63.9%, followed by the PICU with 17%. Most interventions were made through pharmacist order entry, accounting for 24.6% of interventions, followed closely by phone calls from providers or nursing staff. Rounding with the team showed substantial benefit as well, resulting in 18.5% of all interventions recorded. Resident physicians with fewer years of training required the most interventions by the pharmacist and had the most prescribing errors (Table 3, Figures 3 and 4). The most common type of intervention coded was a “drug therapy recommendation,” which accounted for 46% of all interventions recorded. This intervention was coded for a pharmacist's recommended change in medication selection given the patient's presentation, culture results, allergies, or other factors influencing the choice of medication to use. More importantly, errors made up 24.5% of all interventions recorded, with the most common cause of error being prescribing, accounting for 68.3% of all errors during this time period. Prescribing errors were defined as an incomplete order resulting in missing information (such as route, frequency, or strength), wrong dose/rate or drug, wrong patient, poor handwriting or unclear order, allergy/contraindication present, or other prescribing error (order against hospital policy, chemotherapy medication indicated/ not indicated per roadmap, etc). Wrong dose/ wrong rate accounted for 28% of all prescribing errors, of which 44% were for dose too large and approximately 16% were for dose too small. Of the cases where dosing was determined to be too high, more than one-third would have resulted in a greater than 2-fold overdose had it not been prevented (Figure 5).
Table 3.
Total Interventions
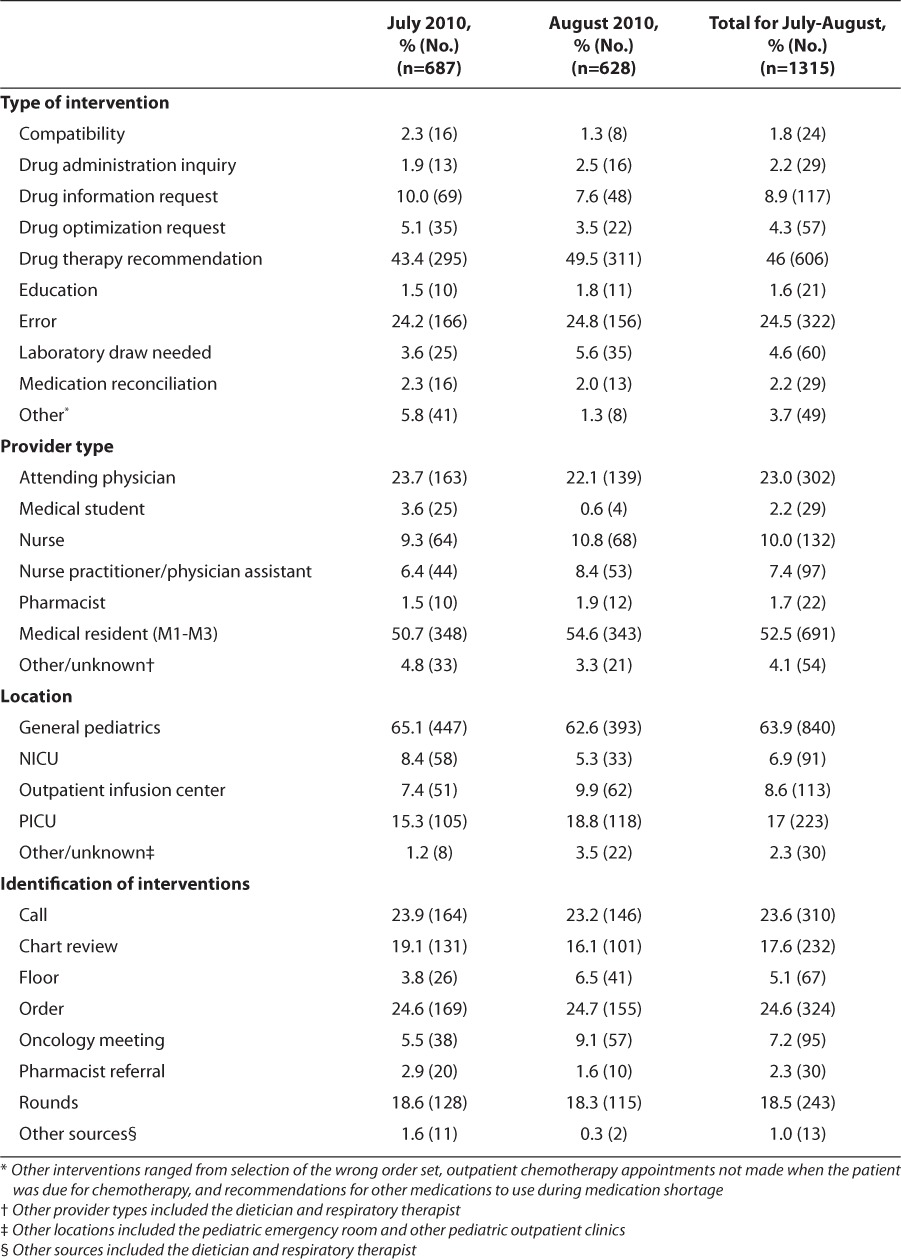
Figure 3.
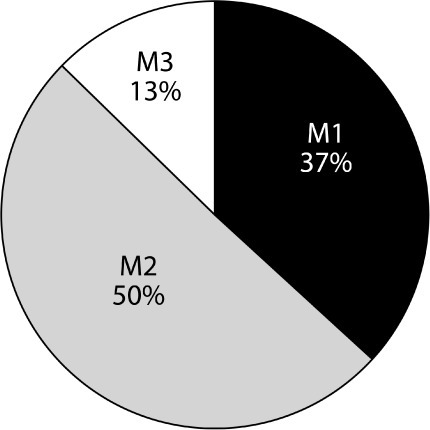
Interventions by resident year (M1-M3) for July and August.
M1, resident year 1; M2, resident year 2; M3, resident year 3.
Figure 4.
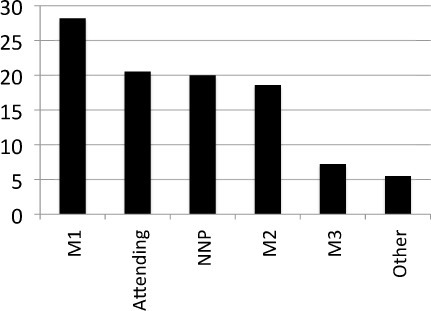
Prescribing errors by practitioner type. “Other” provider types included the dietician and respiratory therapist.
NNP, neonatal nurse practitioner; M1, resident year 1; M2, resident year 2; M3, resident year 3.
Figure 5.
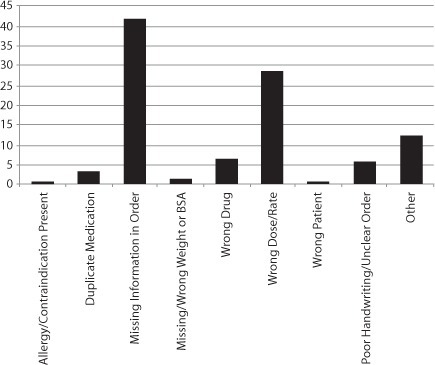
Number and type of prescribing errors. BSA, body surface area
Of the errors recorded, very few reached the patient and of those that did, most did not result in patient harm. However, it was determined there was a potential for error or harm to the patient in 32.2% of all interventions made. Of those, 15.5% were coded as PE1 or PE2, indicating this error may have resulted in significant morbidity or mortality if not prevented. The most common cause for a potential error was due to missing information in the order (route, frequency, or strength). Prevention of an overdose or duplication of therapy was cited to occur in 10.4% of the interventions noted (Table 4).
Table 4.
Summary of Error Types
DISCUSSION
With greater than 1300 interventions in 2 months, the results of this study indicate the value and ability of pediatrics-trained clinical pharmacists to detect and prevent medication errors from reaching the patient. Of the interventions recorded, nearly one-third had the potential for error or harm to the patient and one-half of those were determined to have the potential to cause significant morbidity or mortality if not prevented. The multitude of other interventions made and recorded highlight the important role a pediatric clinical pharmacist can play when integrated into the inpatient pediatric team.
Most errors in this study occurred on the general pediatric ward and the least number of errors occurred in the NICU. The higher number of residents with less training and the heterogeneity of the pediatric population could help explain the increase in pediatric errors. In contrast, the NICU at our institution is a more homogenous population with a more experienced physician team and fewer resident physicians. In addition, fewer medications are used by this population than by the general pediatric population and a reduced pharmacy presence in rounds could help explain the discrepancies in medication errors noted.
It is noteworthy that resident physicians with the least number of years in training had the highest percentage of prescribing errors and need for pharmacist intervention. Despite second-year residents having the highest number of pharmacist interventions, first-year residents had the highest percentage of prescribing errors among all provider types. Second-year residents have a greater familiarity with the pediatric pharmacists than first-year residents, as well as having a greater comfort level in asking questions. Second-year residents are also staffing the PICU for the first time, which may help explain the higher percentages for pharmacist interventions in this group.
During the study period 11 documented, known errors reached the patient. Greater than 60% of these errors were prescribing errors that were missed upon pharmacist order entry and verification. Many of the prescribing errors can be attributed to the complexities of dosing in the pediatric population, as drug references for some medications are mg/kg/dose and others are mg/kg/day divided. Some of the prescribing errors missed by the pharmacist upon order entry may be explained by the lack of pediatric dosing knowledge and training by non-pediatric pharmacists, as well as the lack of dose-checking computer software at our institution.
It is likely that some errors were not accounted for in this study. Errors were only included if the pharmacist was aware the error had occurred; therefore, nursing administration errors and near misses are largely underreported in this study. In addition, the researchers could not determine the total number of pediatric medications written to produce an error rate per patient days given the pharmacy computer system limitations.
There are limited studies documenting the cost avoidance, prevention of medication errors and harm, and optimization of drug therapy associated with having clinical pharmacists in pediatrics. In 1987, Folli et al12 published their results relating to medication error prevention by clinical pharmacists in two children's hospitals. This study showed an error rate of 4.9 and 4.5 per 1000 medication orders in the two hospitals. Children younger than 2 years and pediatric intensive care patients tended to have received the greatest proportion of orders containing medication errors, whereas neonatal patients received the lowest rate. It was also noted the error rate was greatest among physicians with the least amount of training. The authors concluded pharmacist involvement in the review of medication orders dramatically reduced the potential harm from errors.
Kaushal et al9 evaluated medication errors in pediatric patients and discovered a 3-fold higher potential ADE rate than that of adults. Causes for the higher potential error rate have been speculated to be due to the challenges for ordering, dispensing, and administering of medications due to weight-based dosing, medication formulation, communication skills of children, and a child's innate physiology and inability to compensate for medication errors. This study reported a rate of 5.7% for errors, of which 19% were deemed preventable. Contrary to the study of Folli and collleagues,12 neonates in the NICU experienced a higher medication error rate and potential for ADEs than neonates in other pediatric wards. In addition, most medication errors were considered to be dosing errors and occurred during the stage of drug ordering. The investigators concluded that “ward-based clinical pharmacists potentially could have prevented the majority of errors.”
Holdsworth et al13 examined the impact and incidence of ADEs in pediatric inpatients and found that 61% of all ADEs were considered to be preventable. The most common error discovered was underdosing, followed by wrong drug choice and overdosing. Opiates and antibiotics tended to be the most commonly implicated medications prescribed that resulted in errors. The patients more often affected were children who had longer lengths of stay owing to increased medication exposure.
One study reviewed 200 cases of 10-fold prescribing errors, of which 45% were considered potentially serious and 19.5% occurred among pediatric patients. In addition, 10-fold errors accounted for 5.33% of all errors detected during the study period.14 In light of the pediatric studies reporting a higher rate for potential ADEs, the American Academy of Pediatrics released a policy statement in 2003 to help hospitals better prevent medication errors in pediatric patients.15 In 2008, the Joint Commission reiterated the American Academy of Pediatrics' guidance with the release of recommendations and mandates to aid in protection of children from ADEs caused by medication errors.2
In a review of the economic effects of clinical pharmacy interventions, De Rijdt et al5 reported a reduction in preventable ADEs, optimization of antibiotic therapy, as well as cost avoidance associated with clinical pharmacy services in the adult population. In one study4 reviewing the cost implications of having a critical care pharmacist present in the adult intensive care unit, cost avoidance for ADEs totaled between $205,919 and $280,421 in a 4.5-month time period, proving the financial benefit and incentives to having clinical pharmacists on the unit.
This prospective study highlighted the impact a pediatric pharmacist can make on the optimization of medication therapy and prevention of medication errors. The overall error rate per order image scanned was 5.9% during this time period; however, 5.7% of those errors were prevented by the pediatric pharmacist, showing a vast improvement in patient safety. Prevention of medication errors requires a team approach, and clinical pharmacists play an integral role in preventing medication errors and ADEs, as well as assisting in optimizing drug therapy for the pediatric population.
ACKNOWLEDGMENTS
I would like to acknowledge and thank Katy Juhl, PharmD, and Hilary Corson, PharmD, for their assistance in collection of the data.
ABBREVIATIONS
- ADEs
adverse drug events
- ADMs
automated dispensing machines
- BSA
body surface area
- NICU
neonatal intensive care unit
- PICU
pediatric intensive care unit
Footnotes
DISCLOSURE The authors declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria.
REFERENCES
- 1.Bates DW, Cullen D, Laird N. Incidence of adverse drug events and potential adverse drug events: implications for prevention. JAMA. 1995;274(1):29–34. et al. [PubMed] [Google Scholar]
- 2.The Joint Commission. Preventing pediatric medication errors. April 2008. p. 39. www.jointcommission.org/SentinelEventAlert/sea_39.htm. Accessed July 2011. [PubMed]
- 3.Davydov L, Caliendo GC, Smith LG. Analysis of clinical intervention documentation by dispensing pharmacists in a teaching hospital. Hosp Pharm. 2003;38(4):346–350. et al. [Google Scholar]
- 4.Kopp BJ, Mrsan M, Erstad BL. Cost implications of and potential adverse events prevented by interventions of a critical care pharmacist. Am J Health Syst Pharm. 2007;64(23):2483–2487. doi: 10.2146/ajhp060674. et al. [DOI] [PubMed] [Google Scholar]
- 5.De Rijdt T, Willems L, Simoens S. Economic effects of clinical pharmacy interventions: a literature review. Am J Health Syst Pharm. 2008;65(12):1161–1172. doi: 10.2146/ajhp070506. [DOI] [PubMed] [Google Scholar]
- 6.Leape LL, Cullen DJ, Clapp MD. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA. 1999;282(3):1311–1316. doi: 10.1001/jama.282.3.267. et al. [DOI] [PubMed] [Google Scholar]
- 7.Teich JM, Merchia PR, Schmiz J. Effects of computerized order entry on prescribing practices. Arch Intern Med. 2000;160(18):2741–2747. doi: 10.1001/archinte.160.18.2741. et al. [DOI] [PubMed] [Google Scholar]
- 8.Bates DW, Teich JM, Lee J. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999;6(4):313–321. doi: 10.1136/jamia.1999.00660313. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaushal R, Bates DW, Landrigan C. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285(16):2114–2120. doi: 10.1001/jama.285.16.2114. et al. [DOI] [PubMed] [Google Scholar]
- 10.Fortescue EB, Kaushal R, Landrigan CP. Prioritizing strategies for preventing medication errors and adverse events in pediatric inpatients. Pediatrics. 2003;111(4, pt 1):722–729. doi: 10.1542/peds.111.4.722. et al. [DOI] [PubMed] [Google Scholar]
- 11.Phillips DP, Barker GE. A July spike in fatal medication errors: a possible effect of new medical residents. J Gen Intern Med. 2010;25(8):774–779. doi: 10.1007/s11606-010-1356-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Folli HL, Poole RL, Benitz WE. Medication error prevention by clinical pharmacists in two children's hospitals. Pediatrics. 1987;79(5):718–722. et al. [PubMed] [Google Scholar]
- 13.Holdsworth MT, Fichtl RE, Behta M. Incidence and impact of adverse drug events in pediatric inpatients. Arch Pediatr Adolesc Med. 2003;157(1):60–65. doi: 10.1001/archpedi.157.1.60. et al. [DOI] [PubMed] [Google Scholar]
- 14.Lesar TS. Tenfold medication dose prescribing errors. Ann Pharmacother. 2002;36(12):1833–1839. doi: 10.1345/aph.1C032. [DOI] [PubMed] [Google Scholar]
- 15.Stucky ER, American Academy of Pediatrics Committee on Drugs and American Academy of Pediatrics Committee on Hospital Care Prevention of medication errors in the pediatric inpatient setting. Pediatrics. 2003;112(2):431–436. doi: 10.1542/peds.112.2.431. [DOI] [PubMed] [Google Scholar]


