Introduction
The purpose of self-monitoring of blood glucose is to take action based on the results of the tests. The three actions that must be taken by insulin-using diabetes patients in response to blood glucose self-testing are, first, to record the blood glucose level, second, to calculate an appropriate dose of insulin, and, third, to administer the dose of insulin. A low-technology solution exists for each of these three actions. In addition, a commonly used high-technology solution exists for the first and third of these three actions (recording the blood glucose level and administering the insulin dose), but no high-technology product is currently approved by the Food and Drug Administration (FDA) for calculating an insulin dose (Figure 1). The currently unavailable high-technology approach to glucose-directed insulin dosing is approved software for calculating a bolus dose of insulin.
Figure 1.
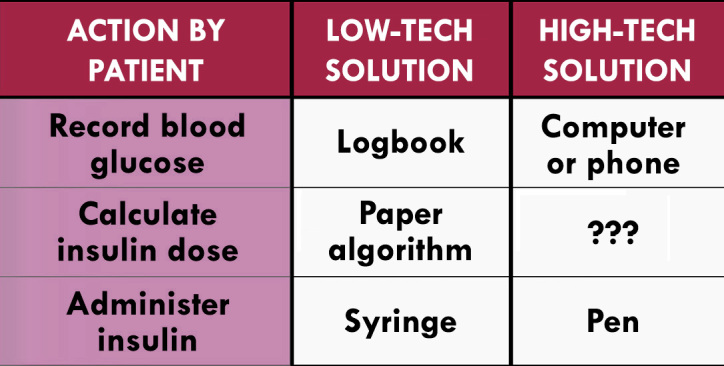
Technology to apply to blood glucose data for administering an appropriate dose of insulin.
In the first article to report a premeal bolus calculator was a system that was intended for use by insulin pump users.1 The bolus formula in that article incorporated five elements: (1) the carbohydrate/insulin ratio (carbo-hydrate bolus dose); (2) the insulin/carbohydrate ratio (correction bolus dose); (3) the target postprandial blood glucose; (4) the current blood glucose level; and (5) the carbohydrate content of the planned meal. The first four of these elements were known in advance and could be preprogrammed. Only the meal content would need to be entered at the time of the meal. Four factors that could affect the dose calculation, but were not accounted for, were as follows: (1) any correction bolus insulin onboard from a recently administered correction bolus insulin dose; (2) any carbohydrate bolus insulin onboard from a recently administered correction bolus insulin dose; (3) exercise either recently since the last dose of insulin or planned soon; or (4) any food onboard since the last dose of insulin. Accounting for these four factors could make for a more accurate bolus calculator to match a lifestyle, food, or physical activity choice with a correct dose.
Products Containing Bolus Calculators
Examples of products that contain or are expected to eventually contain decision-support software for insulin bolus dosing are listed in Table 1. Two examples of blood glucose monitors with insulin bolus dose calculator features (that are approved in Europe but are not approved in the United States) include the following: (1) Roche ACCU-CHEK Aviva Expert Bolus Advisor System and (2) Abbott FreeStyle InsuLinx Blood Glucose Monitoring System.
Table 1.
Products That Contain or Are Expected to Eventually Contain Decision-Support Software for Insulin Bolus Dosing
| 1. Blood glucose monitors |
| 2. Freestanding diabetes insulin guidance systems |
| 3. Software apps for smart phones |
| 4. Software from the medical literature |
| 5. Insulin pumps |
Applications for Smartphones
Many freestanding software applications (apps) to calculate bolus doses of insulin are currently available for smartphones.2 I do not recommend any of them for my patients at this time. These apps, in virtually every case, are lacking three types of important reassuring information. First, these apps generally provide no explanation of the factors or formulas that generate the calculated bolus dose, and the patient does not know whether they might be using a dose of insulin that does not fit their requirements. Second, these apps generally do not explain whether they have any safety mechanisms to avoid accidental overdosages and hypoglycemia, and I have seen none that present data from premarket or postmarket studies of adverse events associated with their use. Third, the qualifications of the writers of these apps are generally unknown, and many might be written by nonmedical people with technical training (such as computer software engineers) but with no medical background. Most importantly, these apps regulate dosing of a potentially dangerous drug (insulin), which puts them under the purview of the FDA, but none have been approved by the FDA. Patients should not use such nonapproved medical software because of the risk of being instructed to administer an unsafe dose of insulin.
Investigator-Initiated Software
A decision-support software program for dosing insulin in type 2 patients was tested in Spain in a cluster-randomized controlled trial compared with usual bolus dosing calculated without the assistance of the software.3 The 18-month study enrolled 697 subjects treated by 66 physicians. To develop the software, the investigators specified that subjects self-monitor six times per day, and they defined four ranges of glycemia from the test results. This means that 46, which is 4096, patterns of glycemia throughout a day were accounted for by the computer app. The investigators also defined up to 60 types of insulin regimens. Not every glycemic pattern and insulin regimen were compatible, so the total number of treatment recommendations for every glycemic pattern and every insulin dosing pattern was not as high as the product of 4096 times 60,000. Nevertheless, the software identified 75,000 combinations of glycemic patterns and treatment regimens from which to select. In the intervention group, the final glycated hemoglobin (A1C) was 7.19%, with a difference from the start of -0.69% (p = .001), whereas, in the control group, the final A1C was 7.71%, with a difference from the start of -0.09% (p = not significant).
Insulin Pumps
The major insulin pumps all contain bolus-calculating software. Unlike blood glucose monitors or freestanding calculators, the prior bolus dose is always automatically known by the system prior to each recommended bolus dose. Therefore, if there should be a problem with dysglycemia following the use of such software, then the insulin dosing pattern can be studied later. Also, insulin pumps can be programmed to automatically incorporate insulin onboard from prior bolus doses, whereas, with freestanding systems or with the use of blood glucose monitors, the patient must manually enter their bolus doses to receive advice that incorporates bolus insulin onboard.4
Pattern Recognition
If proper safety systems can be designed specifically for blood glucose monitors, then it is likely that bolus-dosing software will gradually become more widely adopted in many countries. A blood glucose monitor with pattern recognition software (the LifeScan OneTouch Verio IQ) has been approved by the FDA. This system provides alerts to the user about patterns but does not provide bolus-dosing recommendations. If a software product that stores, sorts, and analyzes blood glucose data makes no specific treatment recommendations, then the patient can receive some assistance from software without the product having to be as tightly regulated as a formal bolus calculator. This approach is a type of “decision-support light,” which provides less advice than frank decision-support software but is less stringently regulated.
Patients Who Can Benefit
Some patients are particularly likely to benefit from bolus-calculating software. If a patient has difficulty estimating the carbohydrate content of foods or the weight of foods, then decision-support software can be helpful by basing mealtime bolus doses on general descriptions of meals by patients coupled with stored databases of food compositions and carbohydrate contents of various-sized portions.5 Not only patients, but even diabetes educators can have trouble estimating the carbohydrate contents of foods.6 Many patients with diabetes have been shown to have difficulty understanding and using numbers. These patients have a great deal of difficulty calculating mealtime bolus doses and even more trouble combining correction boluses with mealtime boluses. Just as a regulatory agency must account for the risk of using a new medical product, I believe that it is relevant to consider the risk of using existing therapy without the product. Given the problems that some patients have with calculating correct insulin bolus doses, there is a definite need for products in this space, provided that they are both safe and effective.
Poor Numeracy
“Numeracy” is the ability to understand and use numbers in daily life. For individuals with type 1 diabetes using intensive insulin therapies, this skill requires them to be able to (1) count; (2) perform basic math calculations; (3) use fractions, decimals, and percentages; (4) understand graphs, tables, and measurements; and (5) decide when to use these skills.7 Poor numeracy is associated with worse metabolic control.8
A bolus calculator incorporated into a blood glucose monitor can assist patients who have poor numeracy. This was demonstrated in a study where subjects manually calculated two prandial insulin doses and then used a commercial bolus calculator (the FreeStyle InsuLinx Blood Glucose Monitoring System) to determine the insulin doses for the same two blood glucose values.9 One pair of calculations was based on a high glucose test result, and the other pair was based on a normal glucose test result. Of 409 insulin doses manually calculated by the subjects, 63% were incorrect. Surprisingly, even with the use of the bolus calculator, 6% of the dose determinations were incorrect. About half the bolus-calculator-determined errors were results of the users not performing the tests as instructed, rather than the meter calculating the wrong suggested dose, but the remaining errors could not be definitely explained, and the downloads were not available.
Outcomes
A survey of 508 patients with type 1 diabetes in the United Kingdom who were using bolus calculator blood glucose monitors for 4–12 weeks reported three types of psychological benefits attributable to this software. For most patients, the bolus calculator, compared with manual calculation, was easier to use, improved their confidence in the accuracy of their bolus dosage, and reduced their fear of hypoglycemia.10
The BolusCal Study was a 16-week randomized, controlled, open-label, three-arm parallel clinical study of 51 adults with poorly controlled (A1C 8.0–10.5%) type 1 diabetes who were using multiple dose injections daily.11 An inter-vention that combined education about flexible intensive insulin therapy (FIIT) with the use of an automated bolus calculator (ABC) was studied. The ABC that was used was the ACCU-CHEK Aviva Expert. Subjects in the control arm received FIIT education excluding carbohydrate counting. Subjects in the CarbCount arm were taught FIIT and how to count carbohydrates. CarbCount ABC subjects received education that included FIIT and carbohydrate counting, and they were also provided with an ABC. At 16 weeks, the change in A1C was -0.1% (p = .730) in the control arm, -0.8% (p = .002) in the CarbCount arm, and -0.7% (p < .0001) in the CarbCount ABC arm. The difference between the improvements in mean A1C levels for the two interventions was not statistically significant. Flexible intensive insulin therapy and carbohydrate counting (compared with control treatment) improved treatment satisfaction, and the concurrent use of an ABC improved treatment satisfaction further.
A 1-year randomized controlled trial of bolus calculator use was reported in a cohort of 40 insulin-pump-using children from Sweden. Carbohydrate counting with a bolus calculator was compared with both carbohydrate counting with manual calculation of insulin dosing and control therapy without use of carbohydrate counting. No difference in A1C levels between the groups was found. Bolus calculator use was associated with smaller postprandial glucose excursions and a higher proportion of postprandial glucose levels being within the target range, but these improvements were not statistically significant.12
These three studies suffered from being either not controlled (in the United Kingdom study) or not adequately powered (a total of 51 subjects completed the trial in the Denmark study, and 40 subjects completed the trial in the Sweden study). Better studies with well-defined end points and realistic comparator interventions will be needed in order to determine the benefits of bolus calculators. To date, a positive impact on long-term glucose control (A1C) has not been demonstrated with bolus calculators embedded into either pumps or blood glucose monitors.
Clinical Hurdles to Adoption
Several clinical hurdles must be overcome for the current generation of bolus calculators to become more widely adopted. Educational programs aiming to increase caregivers’ knowledge are needed in order to get full benefit of the technology.13 Clinicians might also be reluctant to recommend this tool because there are a variety of methods for calculating a bolus dose such as using various target glucose levels within a range of glucose levels or various calculated durations of insulin action or the various assumptions about when a prior bolus of insulin is subtracted from a currently needed bolus. Aggressive settings (for example, assuming that the duration of action of a prior insulin bolus is very short or not accounting for the effects of exercise) can lead to hidden stacking and hypoglycemia.14 It is possible that there will turn out to be as much variation in the clinical performance (A1C levels) between various future blood glucose monitor bolus calculators as there is now in the analytical performance between blood glucose monitors. On the other hand, an error in bolus dosing will likely lead to an out-of-range glucose test the next time self-monitoring of blood glucose is checked, and this error can then be corrected at the time of the next insulin dose. Therefore, cumulative long-term deviations are not likely to occur even with bolus calculator engines that are suboptimal. Virtually every bolus calculator currently in use does not account for the effect on insulin release caused by dietary fat or protein.15 Evidence suggests that these two dietary components should be accounted for when insulin boluses are calculated.16,17 Finally, like many other technological applications for diabetes, poor compliance undermines benefits of the products.
At present, the trend in bolus calculator decision support is to provide a real-time recommendation for a specific situation. No commercially available data management software from major manufacturers of blood glucose monitors, pumps, or continuous glucose sensors systema-tically analyzes historical data sets in order to provide ongoing therapeutic recommendations or adjustments of daily insulin doses.18
Business Hurdles to Adoption
From a commercial standpoint, there are business hurdles that must be overcome for companies to commercialize these products and get them into the hands of consumers. Commercialization in any country will require that the country’s device regulatory body (e.g., FDA) will classify the decision-support software as safe. Also manufacturers’ advertising claims will need to present their products’ effectiveness accurately to be in compliance with that country’s commercial regulatory body (e.g., Federal Trade Commission). Clear guidelines from these regulatory bodies will speed up the commercialization process. The paucity of outcome data might make it difficult for patients to receive coverage for additional costs that may be associated with this type of feature in a blood glucose monitor. Finally, to the extent that patients act upon the advice of software for dosing a medication, and because there is no so-called learned intermediary in the process to filter the instructions or discuss the risks of the software product, patients will need to be warned by the manufacturers how to interpret instructions, or there could be legal liability for the manufacturers.19
Conclusions
As health care professionals seek to empower patients with diabetes to care for themselves, and as the societal aspirations for control of diabetes become higher, it is natural that a tool that could provide decisions support for patients will become more widely desired, and where available, it will become more widely adopted. The problem of poor numeracy alone calls for a numerical support tool, and a bolus calculator fills that need. I do not believe that all bolus calculators need to use the exact same standardized rules, because standardization can sometimes stifle innovation. However, the manufacturers should make their rules available so that patients’ health care professionals can understand the basis for dosing recommendations. An ideal bolus calculator would come with predetermined settings from the factory but would allow some modifications of settings for certain patients who have atypical dosing requirements. Patients with type 1 diabetes can expect to see many useful technological tools becoming widely adopted in the future, and decision-support bolus calculation software is one of the more promising tools.
Glossary
Abbreviations
- (A1C)
glycated hemoglobin
- (ABC)
automated bolus calculator
- (app)
application
- (FDA)
Food and Drug Administration
- (FIIT)
flexible intensive insulin therapy
References
- 1.Gross TM, Kayne D, King A, Rother C, Juth S. A bolus calculator is an effective means of controlling postprandial glycemia in patients on insulin pump therapy. Diabetes Technol Ther. 2003;5(3):365–369. doi: 10.1089/152091503765691848. [DOI] [PubMed] [Google Scholar]
- 2.Rao A, Hou P, Golnik T, Flaherty J, Vu S. Evolution of data management tools for managing self-monitoring of blood glucose results: a survey of iPhone applications. J Diabetes Sci Technol. 2010;4(4):949–957. doi: 10.1177/193229681000400426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sáenz A, Brito M, Morón I, Torralba A, García-Sanz E, Redondo J. Development and validation of a computer application to aid the physician’s decision-making process at the start of and during treatment with insulin in type 2 diabetes: a randomized and controlled trial. J Diabetes Sci Technol. 2012;6(3):581–588. doi: 10.1177/193229681200600313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walsh J, Roberts R, Bailey T. Guidelines for optimal bolus calculator settings in adults. J Diabetes Sci Technol. 2011;5(1):129–135. doi: 10.1177/193229681100500118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pańkowska E, Błazik M. Bolus calculator with nutrition database software, a new concept of prandial insulin programming for pump users. 2010;4(3):571–576. doi: 10.1177/193229681000400310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shapira G, Yodfat O, HaCohen A, Feigin P, Rubin R. Bolus guide: a novel insulin bolus dosing decision support tool based on selection of carbohydrate ranges. J Diabetes Sci Technol. 2010;4(4):893–902. doi: 10.1177/193229681000400418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kerr D. Poor numeracy: the elephant in the diabetes technology room. J Diabetes Sci Technol. 2010;4(6):1284–1287. doi: 10.1177/193229681000400601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, Gregory RP, Fuchs L, Malone R, Cherrington A, Pignone M, DeWalt DA, Elasy TA, Rothman RL. Association of numeracy and diabetes control. Ann Intern Med. 2008;148(10):737–746. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- 9.Sussman A, Taylor EJ, Patel M, Ward J, Alva S, Lawrence A, Ng R. Performance of a glucose meter with a built-in automated bolus calculator versus manual bolus calculation in insulin-using subjects. J Diabetes Sci Technol. 2012;6(2):339–344. doi: 10.1177/193229681200600218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barnard K, Parkin C, Young A, Ashraf M. Use of an automated bolus calculator reduces fear of hypoglycemia and improves confidence in dosage accuracy in patients with type 1 diabetes mellitus treated with multiple daily insulin injections. J Diabetes Sci Technol. 2012;6(1):144–149. doi: 10.1177/193229681200600117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schmidt S, Meldgaard M, Serifovski N, Storm C, Christensen TM, Gade-Rasmussen B, Nørgaard K. Use of an automated bolus calculator in MDI-treated type 1 diabetes: the BolusCal Study, a randomized controlled pilot study. Diabetes Care. 2012;35(5):984–990. doi: 10.2337/dc11-2044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Enander R, Gundevall C, Strömgren A, Chaplin J, Hanas R. Carbohydrate counting with a bolus calculator improves postprandial blood glucose levels in children and adolescents with type 1 diabetes using insulin pumps. Pediatr Diabetes. 2012 doi: 10.1111/j.1399-5448.2012.00883.x. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 13.Rossetti P, Vehí J, Revert A, Calm R, Bondia J. Commentary on “Performance of a glucose meter with a built-in automated bolus calculator versus manual bolus calculation in insulin-using subjects.”. J Diabetes Sci Technol. 2012;6(2):345–347. doi: 10.1177/193229681200600219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walsh J, Roberts R. Pumping insulin. 4th ed. San Diego: Torrey Pines Press; 2006. [Google Scholar]
- 15.Schwartz FL, Guo A, Marling CR, Shubrook JH. Analysis of use of an automated bolus calculator reduces fear of hypoglycemia and improves confidence in dosage accuracy in type 1 diabetes mellitus patients treated with multiple daily insulin injections. J Diabetes Sci Technol. 2012;6(1):150–152. doi: 10.1177/193229681200600118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pańkowska E. A review of the “bolus guide,” a new insulin bolus dosing support tool based on selection of carbohydrate ranges. J Diabetes Sci Technol. 2010;4(4):903–905. doi: 10.1177/193229681000400419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pańkowska E, Błazik M, Groele L. Does the fat-protein meal increase postprandial glucose level in type 1 diabetes patients on insulin pump: the conclusion of a randomized study. Diabetes Technol Ther. 2012;14(1):16–22. doi: 10.1089/dia.2011.0083. [DOI] [PubMed] [Google Scholar]
- 18.Klonoff DC. Improved outcomes from diabetes monitoring: the benefits of better adherence, therapy adjustments patient education, and telemedicine support. J Diabetes Sci Technol. 2012;6(3):486–490. doi: 10.1177/193229681200600301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roberts WT, 3rd, Faegre Baker Daniels. Will the FDA’s proposed DTC ad rule further erode the learned intermediary doctrine? http://www.faegrebd.com/11384. Accessed July 22, 2012.


