Abstract
Assisted Living Facility residents are at risk for cognitive decline that precipitates nursing home placement. Cognitive training protects cognition and leads to maintained self-care for community dwelling elders. This pilot study tested an intervention designed to improve reasoning and everyday problem solving for assisted living residents.
Volunteers (N= 4) completed the six Reasoning Exercises in Assisted Living training sessions provided over one month. Pre-intervention, immediate post-intervention, and 3 month follow-up assessments of problem solving were compared. Scores on the Everyday Problems for Cognitively Challenged Elderly (EPCCE) increased 20% from pre (M=11.00, SD = 8.83) to post-intervention (M=19.5, SD=8.35), t=−312, p = .05. After three months, subjects showed sustained EPCCE score improvement (M = 21.75, SD = 4.57, t =−3.95, p = .03).
Assisted living facilities (ALFs) are the fastest growing residential care option designed to meet the needs of the rapidly expanding aging population. ALFs serve older adults who need minimal assistance such as meal provision, personal care assistance, medication administration, and housekeeping supports, enabling them to live in private apartments (in contrast to nursing home care). ALFs currently house 1 million older adults and are estimated to expand two-fold over the next decade (Mollica & Johnson-Lemarche, 2005; National Center for Assisted Living, 2007).
Despite goals of maintaining independence and autonomy, research verifies that ALF residents are at risk for cognitive decline, functional disability, and depression that require more intensive and costly nursing care than many ALFs provide (Aud & Rantz, 2005; Maas & Buckwalter, 2006; Zimmerman et al., 2005). The need for greater assistance with activities of daily living (ADLs) may precipitate nursing home (NH) placement for ALF residents who on average require assistance with 2.3 ADLs compared to 3.8 ADLs for NH residents (National Center for Assisted Living, 2001b). Interventions that limit decline and promote ongoing everyday competency in meeting ADLs and instrumental ADLs (IADLS) may permit elders to remain longer in ALFs and delay nursing home placement. This is important because NH care is twice as costly as ALF care; a national trade survey estimates average annual NH cost at $74, 808 compared to $36, 573 for ALFs (Genworth, 2007).
Adapting to ALF living itself challenges older adults who must relinquish their home in the first step on a trajectory of increasing decline, dependence, and loss of autonomy (Cutchin, Owen, & Chang, 2003; Dobbs, 2004). ALF residents wish to avoid moving to nursing home (NH) care (Aud & Rantz, 2005) and openly express concern about their own cognitive decline. Often they observe cognitive impairment in other residents, and recognize that this is a major factor necessitating nursing home placement (Phillips, Hawes, Spry, & Rose, 2000; Williams & Warren, 2007). Additionally, depression is common, limiting participation in ALF activities that are mentally stimulating (Gruber-Baldini et al., 2005; Rosenblatt et al., 2004)
This study tested the feasibility of a cognitive training program designed to mentally stimulate ALF residents and improve reasoning and applied problem solving for everyday activities needed to remain in ALF residency. This intervention was modeled after an empirically verified randomized clinical trial that achieved cognitive improvement and maintained IADL functioning longitudinally in healthy, community dwelling older adults (Jobe et al., 2001; Willis et al., 2006). Reasoning and applied problem solving skills were selected as the focus of training because these skills are integral to everyday problem solving and selfcare that enable ongoing assisted living residency. This study adds to the limited research testing cognitive interventions such as reality orientation and memory training in ALFs (McDougall, 2000).
ASSISTED LIVING
Assisted living has emerged as a popular approach to the delivery of supportive care, expanding the options for many elders who need only limited assistance and not complex medical care. Assisted living enables older adults to live semi-independently in a residential setting, embracing a philosophy of promoting autonomy, dignity, and privacy for residents (National Center for Assisted Living, 2006). However, the limited research on ALF residents needs to be expanded to define resident characteristics, needs, and preferences, and to identify nursing interventions that optimize functional, emotional, and cognitive health and delay declines leading to nursing home placement (Aud & Rantz, 2005; Hawes & Phillips, 2000).
Despite the growing popularity of ALF care, concern over quality of care, complicated by divergent state licensing requirements, is reflected in statistics that 25% of residents leave ALF care yearly; approximately 75% of these transfer to nursing home (NH) facilities due to needs for more intensive care (Dobbs-Kepper, Chapin, Oslund, Rachlin, & Stover, 2001; Maas & Buckwalter, 2006; Phillips et al., 2000). Although increasing age, marital status, hospitalizations, medical complications, and ADL dependency are all implicated in transitions to NH care (Dobbs-Kepper et al., 2001), cognitive decline has been identified as the primary resident factor implicated in these ALF to NH transitions (Phillips et al., 2000).
ALF residents are at risk for progressive cognitive decline that threatens their ability to remain living in semi-independent ALF care. ALF residents have already experienced initial decline in cognitive, physical, and functional abilities and are at risk for ongoing loss and depression due to chronic disease progression and institutional environments. The typical ALF resident requires assistance with 2.25 ADL activities (bathing, dressing, transferring, toileting, and eating) compared to NH residents who need assistance with an average of 3.75 ADL activities (National Center for Assisted Living, 2001). Assistance with instrumental activities of daily living (IADLs) is typical for ALF residents; 93% use meal preparation and housekeeping services, while 86% are administered medications by staff.
Although ALF facilities have lower levels of staff and less intensive levels of care than NHs, up to two-thirds of ALF residents suffer from dementia and another 25% have a noncognitive psychiatric disorder (Rosenblatt et al., 2004). Older adults with cognitive and psychiatric conditions may select ALF care because they need supervision that is provided in ALFs, but not more intensive nursing care provided in NHs. The need to educate ALF nursing staff to assess and intervene in mental health needs of these older adults is paramount (Maas & Buckwalter, 2006).
Depression is common in older adults, especially in institutional settings including ALFs. Depression frequently contributes to failure to participate in social and creative activities (Watson, Garrett, Sloane, Gruber-Baldini, & Zimmerman, 2003). Review of ALF activity calendars and interviews with ALF residents indicate that activities may be poorly attended because they are perceived as too childlike and expose residents to others with increasing levels of cognitive decline (Williams & Warren, 2007). Depression is associated with surrender of self-care activities and functional decline (Revell, 2000). Institutional culture factors that limit participation contribute to depression and discourage use of active thinking processes include patronizing communication used by nursing staff (Williams, 2007), staff attitudes that progressive resident decline is inevitable (Williams & Warren, 2007a), and failure to include residents in planning activities (Chen, Zimmerman, Sloane, & Barrick, 2007).
EVERYDAY COMPETENCE
The Model of Everyday Competence (Willis, 1991) provides a conceptual framework for understanding how older adults, and specifically ALF residents, cope with the day-to-day problems they encounter to successfully maintain current levels of independent living. Everyday competence includes the ability to independently perform seven identified domains necessary for independent living (finances, medication, telephone use, shopping, meal preparation, housekeeping, and transportation) (Lawton & Brody, 1969).
Successful everyday problem solving or competence depends on individual factors (physical and cognitive health) as well as sociocultural factors including social and environmental factors (ALF determined). Mediating factors for solving everyday problems include control and efficacy beliefs and ongoing practice of the competencies. Outcomes of everyday problem solving competency include physical and psychosocial wellbeing.
Within this everyday competence framework, ALF residents have been admitted to an ALF because of inabilities to meet everyday competencies needed to live totally independently. ALF residents may have reduced competencies because of individual physical, cognitive, and emotional states as well as institutional social and environmental factors (such as lack of cognitively stimulating activities). Residents’ IADL and ADLs are frequently met by staff, so that residents fail to practice these activities, losing competency further through disuse. Within this model, nursing interventions can target improving resident physical, cognitive, and emotional states, as well as institutional environments that are supportive and stimulating. Nurses can also support residents in continued practice of everyday competency skills to improve and maintain their current everyday competencies and increase perceived efficacy. These nursing interventions will contribute to ongoing everyday competence that contributes to resident physical and psychosocial wellbeing.
COGNITIVE INTERVENTIONS
The assumption that “use it or lose it” applies to cognitive functions is widespread and has provided impetus for many proprietary brain age products as well as programs supported by aging interest groups such as the American Association of Retired Persons (AARP) and the Alzheimer’s Association. However, research evidence to support the “use it or lose it” premise is equivocal and complicated by research design issues (Salthouse, 2006; K. Williams & Kemper, 2007). Early evidence of the need for cognitive activity to maintain a variety of mental abilities exists for a number of cognitive functions in healthy elders (Willis et al., 2006). Everyday competence depends on using different combinations of mental abilities to accomplish different daily care tasks (Allaire & Marsiske, 1999).
Cognitive training interventions also show promise for persons with mild dementia and cognitive decline. A meta-analysis of cognitive training research involving persons with Alzheimer’s disease recently reported overall effect sizes of 0.47 for a variety of interventions that improved learning, memory, executive functions, ADLs, general cognitive problem solving, depression, and self-rated functioning (Sitzer, Twamley, & Jeste, 2006). This meta-analysis suggests that the increasing population of ALF residents with cognitive decline also may benefit from cognitive interventions.
REASONING AND EVERYDAY PROBLEM SOLVING INTERVENTIONS
Protective effects of cognitive training on cognition, depression, and self-care have been empirically verified for healthy, community dwelling elders (Calero & Garcia-Berben, 1997; Willis et al., 2006). The Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) clinical trial provides evidence of the effectiveness of cognitive training by studying over 2000 older adults in a longitudinal study (Ball et al., 2002). Healthy community dwelling participants were randomly assigned to one of three training conditions or a no-contact control group. One experimental group attended ten training sessions on inductive reasoning skills. Immediate post-training improvements in reasoning skills were noted and continued over 2 years with booster sessions (Willis, 1991).
The five year follow-up for the ACTIVE study reported that the ten-session inductive reasoning intervention, followed by 4 session booster treatments, resulted in better reasoning skills after five years and in less functional (IADL) decline (Willis et al., 2006). Older adult participants were also less likely to suffer significant declines in health-related quality of life (Wolinsky et al., 2006).
The goal of the current study was to test whether cognitive training, specifically targeting reasoning and everyday problem solving, will be accepted by ALF residents and whether it will improve their everyday problem solving performance. Descriptive factors including general cognition, functional abilities (IADL/ADL), emotional status, self efficacy beliefs, and demographic factors were also explored as they relate to everyday problem solving. This pilot study provides an initial step in testing interventions to halt or reduce ongoing decline, disability, and depression to delay costly NH placement and improve quality of life for ALF residents. Older adults living in ALFs include individuals with cognitive abilities ranging from normal cognitive aging, mild cognitive impairment, and dementia. These ALF residents are at risk for progressive decline and may benefit from improved everyday problem solving that increases their competency in performing IADL and ADLs, permitting them to remain living in ALFs.
DESIGN AND METHODS
A quasi-experimental pretest/posttest design was used to test the feasibility of the Reasoning Exercises in Assisted Living (REAL) intervention for older adults in one ALF. Although quasi-experimental designs present risks to internal and external validity, they are appropriate for pilot studies in the systematic development and testing of nursing interventions (Conn, Rantz, Wipke-Tevis, & Maas, 2001; Whittemore & Grey, 2002). Resident volunteers participated in the individual REAL training sessions with the investigator, provided twice weekly over a three week period; each session lasted 60 minutes. The six-session intervention was preceded and followed by individual assessments lasting 60 minutes, to evaluate everyday problem solving performance as well as descriptive factors (general mental status, depression, engagement in activities, and perceived efficacy). Measures were again repeated after a3-month interval. Subjective comments about the training program also were elicited from the participants to evaluate and modify the REAL program.
Following approval by the investigator’s university Human Subjects Protection Committee, subjects were recruited from a 40 bed ALF unit, part of a Continuous Care Retirement Community (CCRC) located in a major Midwestern metropolitan area. The investigator presented an overview of the study at a neighborhood meeting. Those residents expressing interest in the study were later contacted individually to explain the study in greater detail and to obtain signed consent of the resident (and as appropriate, surrogate decision makers). Inclusion criteria included ability to communicate with the investigator in English and a Mini Mental Status Exam score of at least 20 (to assure comprehension of the training materials).
INTERVENTION
The REAL intervention was developed by the investigator to provide training and practice in reasoning and problem solving skills pertinent to meeting resident ADL/IADL needs. The intervention was designed to increase resident reasoning and problem solving skills to enhance everyday problem solving that in turn, increases and maintains competency in IADL/ADL performance, avoiding increasing needs for care and NH placement. Reasoning skills were targeted based on the success of the ACTIVE intervention that not only improved community dwelling elders’ reasoning performance, but prevented expected declines in IADL function over five years (Willis et al., 2006).
Inductive reasoning focuses on identifying patterns that are applied to new situations. Examples include identifying what comes next in a series of letters, numbers, or words. Reasoning strategies of scanning information, reading out loud, underlining or highlighting key or repeated information, and using lines to separate information into smaller units or chunks were introduced in the introductory session and reviewed in each subsequent session (Saczynski, Willis, & Schaie, 2002).
To create a meaningful learning experience applicable to lives of ALF residents, a framework for successful problem solving in aging was also incorporated into the training program framework (Charness, 1985). Participants were introduced to problem solving steps: 1) understand what the problem is, 2) identify what the goal for problem solving (outcome) is, and 3) try small steps to solve the problem (selectively using the reasoning strategies described above). Both problem solving steps and reasoning strategies were presented at the start and end of each session and incorporated into the problem solving exercises.
The six sessions each featured topics relating to everyday problems typically encountered by ALF residents. The first session introduced problem solving steps and reasoning strategies in application to symbol and word series problems, setting up ALF activity schedules, and identifying patterns in medication regimens. The second session featured use of resources such as phone lists and senior directories, selecting resources from lists, and using order forms. Session three introduced prescription drug labeling information and involved practice in selecting specific information to answer questions. Practice on filling in medication schedules of progressive complexity (using pattern identification) and extracting pertinent information regarding over-the-counter medications were also included. In session four, participants used problem solving for food preference and nutritional requirements to make healthy menu selections when eating in restaurants. The fifth session included education about nutritional labeling and application to nutritional and menu problems. The final session included one or two examples of problems from each previous session, as well as more challenging problems.
The REAL training materials were reviewed and modified with input from experts in cognitive psychology, older adult education, and assisted living. All materials were assessed at 5th to 6th grade Flesch-Kincaid reading level. Prior to implementation, the entire training program was pilot tested with a 90 year old resident in a separate ALF. Modifications to improve the materials, order materials by increasing complexity, and include other topics applicable to older adults living in ALF care were incorporated. Additional problems were added to assure that each session approximated one hour in length.
The sessions were provided in the resident’s individual apartment by the investigator at a time and day (twice weekly) convenient for the resident. Prior to starting each session lighting adequacy, noise control, and availability of hearing aids and eyeglasses were assured. The training materials were presented in a workbook format, with colorful illustrations and large (20 point) font sizes. Materials were presented at a table or on a clip board. Subjects used pens and highlighters in problem solving and to complete charts and fill in answer blanks. Costs of the intervention (including estimates of recruitment, travel and intervention time, and materials) were estimated at $400 for each subject.
DATA COLLECTION
Demographic data were collected from each participant’s ALF medical record. This included age; race; ethnicity; marital status; education; occupational background; months in ALF residency; hospitalizations during this time; medical diagnoses; medications; and existence of hearing, communication, and cognitive impairments.
Pre and post-training assessments of everyday problem solving were collected in separate one hour sessions within one week prior to the first session, within one week of completing the sixth training session, and again after 3 months. Subjects were queried and provided rest breaks as needed during the assessments. Baseline descriptive measures of IADL/ADL functioning, problem solving self-efficacy, depression, engagement, and general cognition were collected at baseline and are described below.
MEASURES
The primary measure of interest for this pilot study was everyday problem solving performance. Descriptive measures were also assessed for relationships to problem solving and functional (IADL/ADL) performance. The investigator administered pre, post, and follow-up assessments and also provided all the REAL training sessions. To minimize potential bias, the assessment data were completed and given to a research assistant to enter into computer files for analysis. The post training assessments were completed without having reference to pre-training scores.
Everyday Problems for Cognitively Challenged Elderly
The Everyday Problems for Cognitively Challenged Elderly (EPCCE) is a 32-item measure of everyday task abilities that tests global cognitive processes and higher-order executive functions in the performance of IADLs (Willis, 1993; Willis et al., 1998). Sixteen written stimuli, such as a prescription label, are presented. Each stimuli is followed by two problem solving questions. Difficulty increases through the testing. Domains related to complex IADL tasks tested include finances, medications, transportation, phone use, household management, and meal preparation. This test is a shorter, less complex version of the Everyday Problems Test validated for use in mildly demented and low educational status elders (Willis, 1996). Reliability is established at .90 (Cronbach’s alpha) for the test. Scores on EPCCE also correlate with direct observations of IADL tasks as well as caregiver reports (Willis et al., 1998).
Instrumental Activities of Daily Living/Activities of Daily Living
The Minimum Data Set for Home Care (MDS-HC) Instrumental Activities of Daily Living (IADL) and Activities of Daily Living (ADL) scales were used to elicit resident reports of their functional status. IADL items include cognitively demanding activities such as meal preparation, housework, financial management, telephone use, and shopping, each rated for actual performance and capacity on a 6 point scale (ranging from “independent” to “does not do”). The ADL self-performance scale rates bathing, personal hygiene, dressing upper and lower body, walking, locomotion, toileting, bed mobility, and eating for performance on the same six-point scale. Higher scores reflect increased needs for assistance. This functional measure was selected because is was designed specifically for older adults in home and assisted living settings, and is widely used in aging research to allow for generalization of findings (Teresi, Lawton, & Holmes, 1997). Reliability on individual tool items have an average weighted Kappa value of .74 (Morris et al., 1997). Pearson’s correlation coefficients for the MDS-HC assessment with established measures of cognitive and functional impairment range from .74–.81 (Landi et al., 2000).
A facility specific functional status tool, required by state regulations and used to determine graduated costs for ALF care, was also used as a measure of functional status. This staff completed data was extracted from the facility medical record and rates 28 ADL and IADL activities on a four point scale (ranging from “independent” to “total assist”) with possible scores ranging from 0 to 51.
Depression
The Center for Epidemiological Studies Depression 10-item scale was used to measure depression (Radloff, 1977). Designed for screening and research, it assesses for six components of depression including mood, feelings of guilt and worthlessness, feelings of helplessness and hopelessness, psychomotor retardation, and sleep disturbance during the past week. Higher scores reflect greater risk of depression. The 10-item CESD correlates (kappa = .97, p< .001) with the original 20 item version (Andresen, Malmgren, Carter, & Patrick, 1994; Radloff & Teri, 1986) as well as ratings of affect. Retest correlations have ranged from r = .59 to r = .71 (Andresen et al., 1994).
Mini Mental Status Exam
The ten minute Mini Mental Status Exam (MMSE) screening test evaluates general mental function and is used as a screening test for dementia with lower scores indicating reduced cognitive abilities (Folstein, Folstein, & McHugh, 1975). Retest reliability correlations are established at above r = .80 levels. It has established validity as a research tool for older adults residing in a variety of residential care settings and is useful to assess intervention effects on cognition (Kurlowicz & Wallace, 1999).
Assisted Living Social Activity Scale
This 11-item Assisted Living Social Activity Scale (AL-SAS) was developed from existing surveys of elderly long-term care and community populations to assess resident social engagement in private and group activities and outings that can provide cognitive stimulation. It assesses activity participation during the past week. Reliability of the AL-SAS is .74 (Zimmerman et al., 2003).
Self-efficacy
Self-efficacy was assessed using a five-item scale designed to reflect the goals of the training. Items queried confidence with solving problems related to resources, medications, food choices, and using reasoning and problem solving skills in everyday situations. Responses were scaled from 1 “not confident” to 4 “extremely confident”. A fifth question asked how often respondents used reasoning strategies and problem solving skills with responses ranging from 1 “never” to 4 “all of the time”.
PROCEDURE
The study was initiated and the intervention provided during spring. All participants completed a signed informed consent prior to participation and were assured of confidentiality and only aggregate reporting of results. Following completion of the six training sessions and pre and post-assessment sessions, participants were presented with a $20 honorarium. A three month follow-up reassessment was completed in late summer 2007. Descriptive data and paired t-tests comparing pre and post-assessments of EPCCE scores were computed. It must be acknowledged that the small sample size prohibited assessment of normal distribution of data, an assumption for paired t tests. Nonparametric analyses also were computed and verified the findings.
RESULTS
Six ALF residents were initially enrolled in the study. Prior to completing the baseline assessment, one participant dropped out of the study due to “scheduling difficulties.” The remaining five participants completed the intervention sessions on schedule. However, one subject moved to another ALF prior to the three month follow-up. Four subjects completed the entire study. Demographic information about these participants who completed the entire study is provided in Table 2.
Table 2.
Baseline Demographic Data and EPCCE Scores
| Subject | Age | Gender | Month in ALF |
Level of Care |
MMSE | EPCCE Score Baseline |
EPCCE Score Post |
EPCCE Score F/U |
|---|---|---|---|---|---|---|---|---|
| 1 | 82 | F | 38 | 43 | 27 | 5 | 9 | 16 |
| 2 | 88 | F | 30 | 16 | 29 | 24 | 28 | 27 |
| 3 | 85 | M | 2 | 10 | 25 | 9 | 24 | 23 |
| 4 | 85 | M | 3 | 29 | 27 | 6 | 17 | 21 |
The age of participants ranged from 82–88 years and length of residency ranged from 2 weeks to 3 years. MMSE scores ranged from 25–30, above the range of mild cognitive impairment. Educational level of all participants was beyond high school and two subjects graduated from college. Residents reported engaging in an average of 2.9 activities in the past week and reported mean depression scores of 14.4. Three residents were diagnosed with dementia and one was under treatment for depression. Residents rated their confidence in using reasoning and problem solving at baseline as 2.9 on a four point scale.
Resident 1: This female resident was a 82 year old divorced, retired professional. She moved to the ALF facility from the nursing home section of this Continuous Care Retirement Community (CCRC) over 3 years ago. She was not diagnosed or currently treated for depression or dementia. Her primary limitations were ambulation, she was wheelchair bound except for transferring and ambulating short distances inside her apartment. She participated in few facility activities, preferring to watch TV in her apartment.
Resident 2 was an 88 year old retired professional who moved into the ALF from an adjacent state 2 years ago to be closer to her extended family. She participated in most activities including the crossword puzzle club, entertainment programs, and daily walks in the facility. Her limitations included macular degeneration and walker use for ambulation. She continued to read large print books but had given up her artwork.
Resident 3 was an 85 year old veteran who worked in a profession, which required much outdoor activity. He had suffered a stroke several years ago and had residual hemiplegia necessitating wheelchair use. He maintained responsibility for his own finances although he was diagnosed and treated for dementia. He moved to the ALF 2 months earlier from another area ALF facility and has not participated in many activities.
Resident 4 is an 85 year old retired professional whose wife died 6 months ago. After her death, he fell and fractured his hip. He suffered complications and had a long recovery from the fracture, including several months of rehabilitation in the nursing home unit of the CCRC. He expressed concerns about recent memory loss and decided not to drive any more. He was computer savvy prior to his accident and continued to participate in numerous musical and social activities.
EVERYDAY PROBLEM SOLVING SCORES
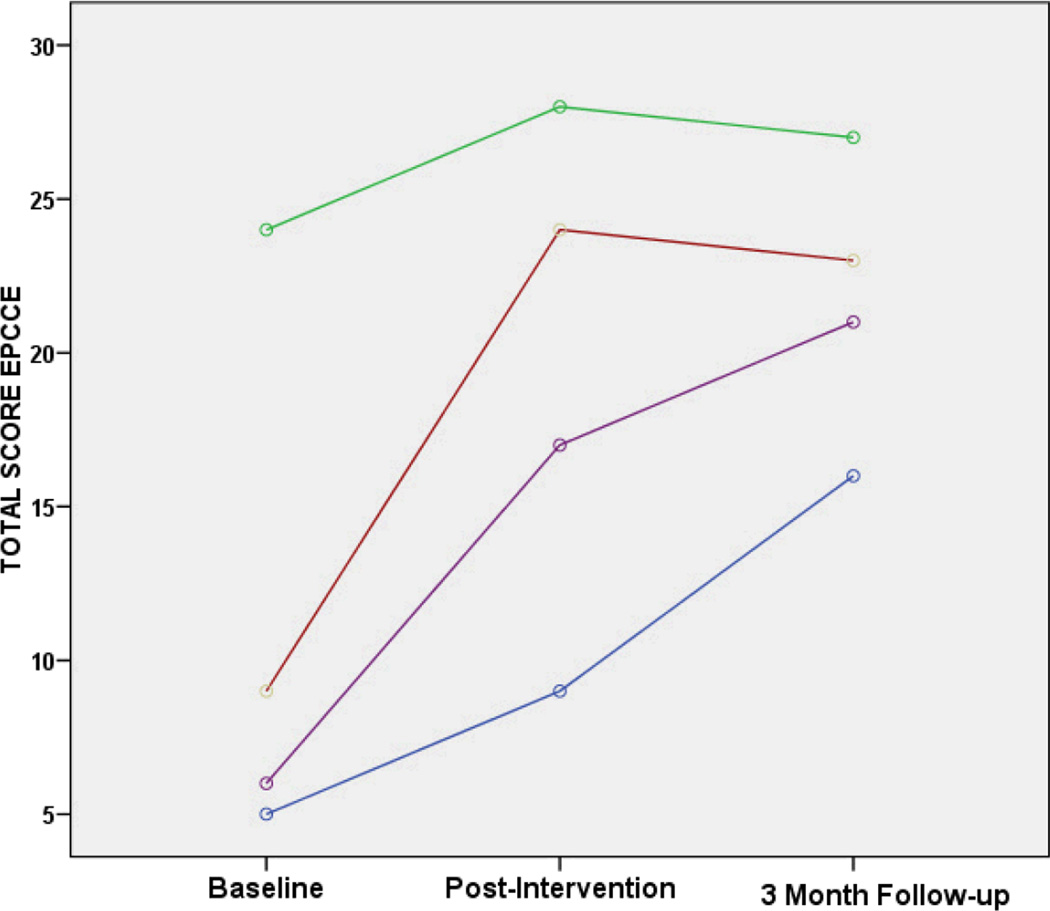
All the participants improved on the number of items answered correctly on the EPCCE test immediately after the intervention. Performance on the EPCCE assessment varied between participants. Pre-training scores ranged from 16% to 75% correct and improved to 28% to 88% correct at post-training. Resident 3 showed the largest gain, improving from 28% correct at pre-training to 75% at post-training (a 48% score increase).
The total number of correct answers increased 20%, from pre (M=11.00, SD = 8.83) to post-intervention (M=19.5, SD=8.35), t=−3.12, p = .05. Because subjects continue the EPCCE until missing two questions for two consecutive stimuli, a measure comparing items answered correctly to the total number attemped also was computed. This accuracy score (percent of questions answered that were correctly) also increased after the training. Pre-training percent correct was M=63.93 (SD = 15.27) and increased 11% to M = 75.34 (SD = 6.07) post-intervention. After three months, post-intervention levels of correct answers were sustained (M = 21.75, SD = 4.57) and remained significantly improved from baseline (t = −3.95, p = .03). Response accuracy also remained relatively stable after three months (M = 70.86, SD = 9.97).
The EPCCE test is not timed, stimuli and questions become progressively more difficult. The test is stopped when the respondent incorrectly answers two questions for two consecutive stimuli. The total number of questions attempted during the EPCCE test also increased from M = 16 (SD = 8.48) at baseline to M = 25 (SD = 7.74) post-intervention (t = −3.81, p = .03). After three months, subjects continued improvement from baseline on the number of items attempted (M = 30.5, SD = 1.5), also significantly more than at baseline (t = 3.84, p = .031). The individual baseline, post-intervention, and 3 month follow-up scores are presented in Table 2 and Figure 1. Comparison of mean changes on EPCCE performance is presented in Table 3.
Figure 1.
Comparison of Everyday Problems for Cognitively Challenged Elderly (EPCCE) scores (baseline, post-intervention, and at three month follow-up) for four residents.
Table 3.
Mean (Standard Deviation) Scores for Everyday Problems for Cognitively Challenged Elderly at Baseline, Post-Intervention, and 3 Month Follow-up
| Measure | Pre-training Mean (SD) |
Post-Intervention Mean (SD) |
3 Month Follow-up Mean (SD) |
|---|---|---|---|
| Total number correct | 11.00a (8.83) | 19.5b (8.35) | 21.75b (4.57) |
| Percentage answered correctly | 63.93 (15.27) | 75.34 (12.15) | 70.86 (4.99) |
| Number of questions completed | 16a (8.48) | 25 (7.74) | 30.5b (1.5) |
Note: Means with different superscripts differ significantly at p<.05
DISCUSSION
This pilot demonstrated that ALF residents readily participated in the 6-session REAL program. One participant dropped out of the study, prior to completing the baseline assessment. This may reflect an unwillingness to participate in pre-training assessments similar to intelligence tests. A second subject completed the study through the post-intervention assessment, but had moved out of the ALF (to a different ALF) at the follow-up. This is not suprising considering statistics that indicate up to 20% of residents leave ALFs annuallly (Hawes, Phillips, & Rose, 2000). Comments of each participant were noted to further revise and improve the sessions. Some residents reported the initial training sessions were too easy, but all agreed that later sessions were challenging. All reported that they enjoyed attending the sessions and learning new information. The participants also reported that the training sessions occupied otherwise idle time.
This pilot study was a preliminary feasibility study that demonstrated that a reasoning and problem solving training program can be provided to ALF residents at minimal cost. The gains noted by comparing pre and post and three month follow-up assessments are encouraging but must be interpreted with caution. Because of the small sample size, the paired t-test assumption of normally distributed data could not be assured. Replication of this research with a larger sample and a control group is needed to assess the effectiveness of the intervention. Future research should also evaluate the cost-effectiveness of cognitive interventions for ALF residents and potential effects on maintaining IADL/ADL performance and delaying nursing home placement.
The aim of the REAL training program was to improve reasoning and problem solving skills for the participants. All the residents completing the study improved on total EPCCE score after the intervention. After three months, two subjects continued to improve on EPCCE score, while two had slightly decreased scores.
The EPCCE test was well received by participants and scores on this measure varied in this ALF population. Designed for persons with cognitive impairments or low socio-educational level elders, this measure also had no ceiling or floor effects and was sensitive to change in this population of elderly ALF residents who were all octogenarians (as typical ALF residents are). It is therefore a valuable tool for future research in elders at advanced ages.
The EPCCE test was administered during each of the three assessment sessions. Thus, it may be concluded that a practice effect is responsible for score increases. Since the REAL training program itself provided intensive practice in everyday problem solving similar to those in the EPCCE, it is assummed that the larger effect was due to the training sessions, and not just the repeating of the same assessment test. The pre and post-assessments occurred approximately one month apart with a three month interval until the follow-up assessment. Participants were not given appraisal of right or wrong responses on the EPCCE and probably would not remember the specific items over the month between pre and post-intervention and the three months until the follow-up assessment session.
Relationships between demographic measures of depression, self-efficacy, activity engagement, and general cognition should all be explored in future research as potential factors influencing everyday problem solving, IADL/ADL performance, and length of stay in ALF residences. Follow-up assessments will be important to determine whether skills gained in a short cognitive training intervention are maintained over time and whether residents continue to use the REAL problem solving steps and reasoning strategies introduced in the program. The need for booster sessions to reinforce skills training should be assessed in follow-up studies.
Future research is also needed to develop other nursing interventions to stimulate cognitive health and IADL/ADL functioning for older adults, especially for at risk elders in supportive care settings. Determining correct doseages of interventions will be important as will methods to tailor materials to challenge older individuals who differ greatly on speed and accuracy of performance. The potential for group cognitive training classes in residential care settings should be explored.
Despite the appeal of the immediate improvements in reasoning and problem solving skills for older adults in ALF settings, the translation of improved cognitive abilities to actual problems must be assessed. Despite the use of the performance based EPCCE measure, this test only simulates real life problem solving. Translation of the cognitive training gains to functional abilities (both IADL and ADL) holds the most promise for improving nursing care of older adults. Longitudinal studies will be needed to assess potential effects on maintaining everyday problem solving competency and whether these abilities will maintain IADL/ADL performance to permit ALF residents to remain in semi-independent living and to delay nursing home placement.
Table 1.
Framework of Everyday Competence for Assisted Living
| ANTECEDENTS | MEDIATORS | OUTPUTS | OUTCOMES |
|---|---|---|---|
| Individual Factors | Practice | Self-Care Competency | Well-Being |
| Health | Efficacy | IADLs | Physical |
| Cognition | ADLs | Psychological | |
| Environmental Factors | Independent Living | ||
| Social | |||
| Physical | |||
| Cultural | |||
| Family | |||
| Staff | |||
| Activities |
Model of Everyday Competency for ALF residents, extended from Willils' (1991) model for community dwellling elders. Bold italicized print indicates ALF specific factors added based on empirical data from ALFs (Williams & Warren, 2007).
Acknowledgments
Supported by the Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) K-12 Program (P. Thomas, PI) at the Kansas University Medical Center, School of Medicine.
REFERENCES
- Allaire JC, Marsiske M. Everyday cognition: Age and intellectual ability correlates. Psychology and Aging. 1999;14(4):627–644. doi: 10.1037//0882-7974.14.4.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Aud MA, Rantz M. Admissions to skilled nursing facilities from assisted living facilities. Journal of Nursing Care Quality. 2005;20(1):16–25. doi: 10.1097/00001786-200501000-00005. [DOI] [PubMed] [Google Scholar]
- Ball K, Berch DB, Helmers KF, Jobe JB, Leveck MD, Marsiske M, et al. Effects of cognitive training interventions with older adults: A randomized controlled trial. JAMA: Journal of the American Medical Association. 2002;288(18):2271–2281. doi: 10.1001/jama.288.18.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calero MD, Garcia-Berben TM. A self-training program in inductive reasoning for low-education elderly: Tutor-guided training vs. self-training. Archives of Gerontology and Geriatrics. 1997;24:249–259. doi: 10.1016/s0167-4943(96)00762-5. [DOI] [PubMed] [Google Scholar]
- Charness N. Aging and problem solving performance. In: Charness N, editor. Aging and human performance. Chichester, U.K.: John Wiley and Sons; 1985. pp. 225–259. [Google Scholar]
- Chen CK, Zimmerman S, Sloane PD, Barrick AL. Assisted living policies promoting autonomy and their relationship to resident depressive symptoms. American Journal of Geriatric Psychiatry. 2007;15(2):122–128. doi: 10.1097/01.JGP.0000247163.49665.5b. [DOI] [PubMed] [Google Scholar]
- Conn VS, Rantz MJ, Wipke-Tevis DD, Maas ML. Designing effective nuring interventions. Research in Nursing and Health. 2001;24:433–442. doi: 10.1002/nur.1043. [DOI] [PubMed] [Google Scholar]
- Cutchin MP, Owen SV, Chang PJ. Becoming "at home" in assisted living residences: Exploring place integration processes. Journals of Gerontology. Series B: Psychological Sciences and Social Sciences. 2003;43:5–22. doi: 10.1093/geronb/58.4.s234. [DOI] [PubMed] [Google Scholar]
- Dobbs-Kepper D, Chapin R, Oslund P, Rachlin R, Stover J. Resident and facility factors related to residents' length of stay in assisted living and residential health care facilities: A longitudinal analysis. Lawrence, KS: University of Kansas School of Social Welfare; 2001. [Google Scholar]
- Dobbs D. The adjustment to a new home. Journal of Housing for the Elderly. 2004;18(1):51–71. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. 'Mini Mental State': A practical method for grading the cognitive stat of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Genworth Financial. [Retrieved August 31];Cost of Care Survey. 2007 [Electronic Version]. from http://www.genworth.com. [Google Scholar]
- Gruber-Baldini AL, Zimmerman S, Boustani M, Watson LC, Williams CS, Reed PS. Characteristics associated with depression in long-term care residents with dementia. Gerontologist. 2005;45(1):50–55. doi: 10.1093/geront/45.suppl_1.50. [DOI] [PubMed] [Google Scholar]
- Hawes C, Phillips C, Rose M. High service or high privacy assisted living facilities, their residents and staff: Results from a national survey. Washington, D.C.: U.S. Department of Helath and Human Services; 2000. [Google Scholar]
- Jobe JB, Smith DM, Ball K, Tennstedt SL, Marsiske M, Willis SL, et al. ACTIVE: A cognitive intervention trial to promote independence in older adults. Controlled Clinical Trials. 2001;22:453–479. doi: 10.1016/s0197-2456(01)00139-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurlowicz L, Wallace M. The Mini Mental State Examination (MMSE) In: Wallace M, editor. Try This: Best Pracies in Nursing Care to Older Adults. New York: Hartford Institute for Geriatic Nursing; 1999. [Google Scholar]
- Landi F, Tua E, Graziano O, Carrara B, Sgadari A, Rinaldi C, et al. Minimum data set for home care: A valide instrument to assess frail older people living in the community. Medical Care. 2000;38(12):1184–1190. doi: 10.1097/00005650-200012000-00005. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–185. [PubMed] [Google Scholar]
- Maas M, Buckwalter KC. Providing quality care in Assisted Living Facilities: Recommendations for enhanced staffing and staff training. Journal of Gerontological Nursing. 2006;32:14–20. doi: 10.3928/00989134-20061101-04. [DOI] [PubMed] [Google Scholar]
- McDougall G. Memory improvement in assisted living elders. Issues in Mental Health Nursing. 2000;21(2):217–233. doi: 10.1080/016128400248202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollica R, Johnson-Lemarche H. State Residential Care and Assisted Living Policy: 2004. [Retrieved May 24, 2007];2005 from http://www.nashp.org. [Google Scholar]
- Morris Fries, Steel Ikegami, Bernabei Carpenter, et al. Comprehensive clinical assessment in community setting: Applicability of the MDS-HC. Journal of the American Geriatrics Society. 1997;45(8):1017–1024. doi: 10.1111/j.1532-5415.1997.tb02975.x. [DOI] [PubMed] [Google Scholar]
- National Center for Assisted Living. Assisted living: independence, choice, and dignity. 2001 from http://www.ncal.org/about/alicd.pdf. [Google Scholar]
- National Center for Assisted Living. Assisted living: independence, choice, and dignity. 2006 [Google Scholar]
- National Center for Assisted Living. Assisted Living Resident Profile. National Center for Assisted Living; 2007. [Google Scholar]
- Phillips CD, Hawes C, Spry K, Rose M. Residents leaving assisted living: Descriptive and analytic results from a national survey (a report prepared for the US Department of Health and Human Services, ASPE, and Research Triangle Institute under contract HHS-100-94-0024 and HHS 100-98-0013) College Station, Texas: Texas A & M University System Health Science Center; 2000. [Google Scholar]
- Radloff LF, Teri L. Use of the center for epidemiological studies-depression scale with older adults. Clinical Gerontologist. 1986;5(1/2):119–136. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for use in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Revell AJ. Depression and activities of daily living: Clinical comments. Clinical Gerontologist. 2000;21(3):73–75. [Google Scholar]
- Rosenblatt A, Samus QM, Steel CD, Baker AS, Harper MG, Brandt J, et al. The Maryland assisted living study: Prevalence, recognition, and treatment of dementia and other psychiatric disorders in the assisted living population of central Maryland. Journal of the American Geriatrics Society. 2004;52(10):1618–1625. doi: 10.1111/j.1532-5415.2004.52452.x. [DOI] [PubMed] [Google Scholar]
- Saczynski JS, Willis SL, Schaie KW. Strategy use in reasoning training with older adults. Aging Neuropsychology and Cognition. 2002;9(1):48–60. [Google Scholar]
- Salthouse TA. Mental exercise and mental aging: Evaluating the validity of the "use it or lose it" hypothesis. Perspectives on Psychological Science. 2006;1(1):68–87. doi: 10.1111/j.1745-6916.2006.00005.x. [DOI] [PubMed] [Google Scholar]
- Sitzer DI, Twamley EW, Jeste DV. Cognitive training in Alzheimer's disease: A meta-analysis of the literature. Acta Psychiatrica Scandinavica. 2006;114:75–90. doi: 10.1111/j.1600-0447.2006.00789.x. [DOI] [PubMed] [Google Scholar]
- Teresi J, Lawton M, Holmes D, Ory M. Measurement in elderly chronic care populations. In: Morris J, Morris S, editors. ADL Assessment Measures for Use with Frail Elders. New York: Springer Publishing Co; 1997. [Google Scholar]
- Watson LC, Garrett JM, Sloane PD, Gruber-Baldini AL, Zimmerman SP. Depression in Assisted Living: Results From a Four-State Study. American Journal of Geriatric Psychiatry September/October. 2003;11(5):534–542. [PubMed] [Google Scholar]
- Whittemore R, Grey M. The systematic development of nursing interventions. Journal of Nursing Scholarship. 2002;34(2):115–120. doi: 10.1111/j.1547-5069.2002.00115.x. [DOI] [PubMed] [Google Scholar]
- Williams K, Kemper S. Interventions to optimize cognitive aging: A review of the research evidence. 2007 [Google Scholar]
- Williams KN. Promoting elder women's cognitive and physical functioning in assisted living. University of Kansas Medical Center; 2007. Unpublished Research data. [Google Scholar]
- Williams KN, Warren CAB. Communication in assisted living. 2007 doi: 10.1016/j.jaging.2007.09.003. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis SL. Cognition and everday competence. In: Schaie KW, editor. Annual Review of Gerontology and geriatrics. New York: Springer; 1991. [Google Scholar]
- Willis SL. Test manual for the Everyday Problems for Cognitively Challenged Elderly. The Pennsylvania State University; 1993. [Google Scholar]
- Willis SL. Everyday cogntiive competence in elderly person: Concepual issues and empirical findings. The Gerontologist. 1996;36:595–601. doi: 10.1093/geront/36.5.595. [DOI] [PubMed] [Google Scholar]
- Willis SL, Allen-Burge R, Dolan MM, Bertrand RM, Yesavage JA, Taylor JL. Everyday problem solving among individuals with Alzheimer's disease. The Gerontologist. 1998;38(5):569–577. doi: 10.1093/geront/38.5.569. [DOI] [PubMed] [Google Scholar]
- Willis SL, Tennstedt SL, Marsiske M, Ball K, Elias J, Mann Koepke K, et al. Long-term effects of cogntive training on everyday functional outcomes in older adults. Journal of the American Medical Association. 2006;296(23):2805–2814. doi: 10.1001/jama.296.23.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolinsky FD, Unverzagt FW, Smith DM, Jones R, Wright E, Tennstedt SL. The Effects of the ACTIVE Cognitive Training Trial on Clinically Relevant Declines in Health-Related Quality of Life. Journals of Gerontology Series B-Psychological Sciences & Social Sciences. 2006;61(5):S281–S287. doi: 10.1093/geronb/61.5.s281. [DOI] [PubMed] [Google Scholar]
- Zimmerman S, Scott AC, Park NS, Hall SA, Wetherby MM, Gruber-Baldini AL, et al. Social engagement and its relationship to service provision in residential care and assisted living. Social Work Research. 2003;27(1):6–17. [Google Scholar]
- Zimmerman S, Sloane PD, Eckert JK, Gruber-Baldini AL, Morgan LA, Hebel JR, et al. How good is assisted living? Findings and implications from an outcomes study. Journal of Gerontology: Social Sciences. 2005;60B(4):S195–S204. doi: 10.1093/geronb/60.4.s195. [DOI] [PubMed] [Google Scholar]