Abstract
BACKGROUND
Mitochondria-related mechanisms have been suggested to mediate methamphetamine (METH) toxicity. However, changes in brain energetics associated with highenergy phosphate metabolism have not been investigated in METH users. Phosphorus-31 (31P) magnetic resonance spectroscopy (MRS) was used to evaluate changes in mitochondrial high energy phosphates, including phosphocreatine (PCr) and β-nucleoside triphosphate (β-NTP, primarily ATP in brain) levels. We hypothesized that METH users would have decreased high-energy PCr levels in the frontal gray matter.
METHODS
Study participants consisted of 51 METH (age=32.8±6.7) and 23 healthy comparison (age=31.1±7.5) subjects. High-energy phosphate metabolite levels were compared between the groups and potential gender differences were explored.
RESULTS
METH users had lower ratios of PCr to total pool of exchangeable phosphate (PCr/TPP) in the frontal lobe as compared to the healthy subjects (p=0.001). The lower PCr levels in METH subjects were significantly associated with lifetime amount of METH use (p=0.003). A sub-analysis for gender differences revealed that female METH users, who had lower daily amounts (1.1±1.0 gram) of METH use than males (1.4±1.7 gram), had significantly lower PCr/TPP ratios than male METH users, controlling for the amount of METH use (p=0.02).
CONCLUSIONS
The present findings suggest that METH compromises frontal lobe high-energy phosphate metabolism in a dose-responsive manner. Our findings also suggest that the abnormality in frontal lobe high-energy phosphate metabolism might be more prominent in female than in male METH users. This is significant as decreased PCr levels have been associated with depressive symptoms, and poor responses to antidepressant treatment have been reported in those with decreased PCr levels.
Keywords: methamphetamine, phosphorus magnetic resonance spectroscopy, phosphocreatine
1. INTRODUCTION
Methamphetamine (METH) abuse is a disorder characterized by compulsive METH-craving and consumption despite an apparent awareness of serious negative consequences. METH use has been linked to the emergence of psychotic symptoms (Iyo et al., 2004; London et al., 2004; Winslow et al., 2007) as well as morphological, functional, and neurochemical abnormalities in multiple brain areas (Bae et al., 2006; Chung et al., 2007; Ernst et al., 2000; Hwang et al., 2006; Oh et al., 2005). Alterations in monoaminergic neurotransmission (Kokoshka et al., 1998; Ricaurte et al., 1980; Robinson and Berridge, 1993) in the frontal lobe have been related to cognitive impairments in METH users because prefrontal cortical neural networks play a central role in impaired decision-making and inhibitory control (Lubman et al., 2004; Yucel and Lubman, 2007).
In METH toxicity, multiple lines of evidence suggest that dysfunctional energy metabolism plays an important role. For instance, 1) impairments of mitochondrial function have been reported after administration of METH to animals including impairments in mitochondrial electron transport chain enzyme complexes (Brown et al., 2005; Burrows et al., 2000a; Klongpanichapak et al., 2006); 2) METH toxicity involves a depletion of energy stores, evidenced by synergistic metabolic inhibition by METH resulting in depletion of striatal dopamine content (Burrows et al., 2000b); and 3) ex vivo METH exposure has been associated with oxidative cell injury and apoptosis in rat cortical neuron and undifferentiated pheochromocytoma (PC12) cells (Cunha-Oliveira et al., 2006; Oliveira et al., 2002). Considering the evidence for mitochondrial involvement in the potential pathophysiology of METH toxicity, it is not surprising that proton (1H) magnetic resonance spectroscopy (MRS) studies have consistently reported that METH users, relative to healthy comparison subjects, have decreased levels of total creatine (phosphocreatine plus creatine) as well as decreased N-acetylaspartate (NAA, a marker of neuronal viability or integrity (Moffett et al., 2007)) levels (Chang et al., 2005; Ernst et al., 2000; Nordahl et al., 2002; Sailasuta et al., 2010b; Sekine et al., 2002; Smith et al., 2001; Sung et al., 2007; Taylor et al., 2007). As NAA synthesis occurs primarily in the mitochondria (Patel and Clark, 1979), decreased NAA levels in METH users are potentially consistent with compromised brain energetics.
Phosphocreatine (PCr) and adenosine triphosphate (ATP) make up the PCr-ATP energy buffering system in neuronal cells that have high and fluctuating energy demands. The enzyme creatine kinase controls the transfer of a phosphate group from PCr to ADP, thereby replenishing brain ATP. It is reported that PCr serves as a buffer to maintain constant ATP levels so that ATP levels remain relatively stable at the cost of PCr expenditure (Schlattner et al., 2006). In the fluctuating energy requirements of neurons, mitochondrial dysfunction may lead to decreased formation of phosphocreatine mediated by the mitochondrial creatine kinase isoenzyme (Dolder et al., 2001; Wallimann et al., 1998). Regarding region specific deficits, frontal hypometabolism has been reported in METH users using positron emission tomography (PET; Kim et al., 2005; London et al., 2005, 2004). These findings would be consistent with the potential mitochondrial abnormality and decreased PCr levels in the frontal lobe of METH users.
Published neuroimaging studies have reported gender differences in METH toxicity with favorable outcomes in female METH users in terms of frontal glucose metabolism and white matter hyperintensities/integrity (Bae et al., 2006; Chung et al., 2007; Kim et al., 2005), probably reflecting a protective effect of estrogen (Dhandapani and Brann, 2002). However, female psychostimulant users are more sensitive to the reinforcing effects than male users (Anker and Carroll, 2011; Carroll et al., 2004). Also, female METH users have a higher incidence of depression and more severe depressive symptoms than male METH users (Dluzen and Liu, 2008; Hser et al., 2005; Kalechstein et al., 2000). In non-METH users, depression severity has been significantly associated with decreased brain PCr levels (Kato et al., 1992), but it is not known what the effects of METH use will be on brain high energy phosphate metabolism in female METH users.
Phosphorus-31 (31P)-MRS provides a unique method to evaluate changes in high-energy phosphate metabolites such as PCr and beta-nucleoside triphosphate (β-NTP), which arises primarily from ATP in brain (Renshaw et al., 2001). To date, there have been no reports measuring 31P-MRS metabolite levels in METH users relative to healthy subjects. In this study, we aimed to investigate whether METH use significantly altered high energy phosphate metabolism. It was hypothesized that first, METH use would be associated with decreased highenergy PCr levels by 31P-MRS in the frontal cortex, and second, that altered PCr levels will be significantly correlated with lifetime amount of METH use. In addition, we explored possible gender differences in the phosphorus metabolite levels in METH users.
2. METHODS
2.1 Subjects
This was a cross-sectional study in which phosphorus MRS data was acquired to examine brain metabolite alterations related to METH use. The study participants consisted of 51 METH dependent subjects (age=32.8±6.7, female=23) and 23 healthy comparison subjects (age=31.1±7.5, female=11). Each individual underwent two dimensional phosphorus magnetic resonance spectroscopic imaging (2D 31P-MRSI) as well as assessment of clinical and drug abuse history. METH-dependent subjects were evaluated for the severity of their lifetime METH use (METH amount, frequency, duration, and abstinence). Inclusion criteria for METH subjects were as follows: (1) age 18–55 years, (2) subjects who met diagnostic criteria for current methamphetamine abuse or dependence as their preferred drug of abuse as determined by the Structured Clinical Interview for DSM-IV (SCID-IV). A board certified psychiatrist took complete medical histories and physical examinations of the subjects. The SCID-IV was administered by a trained psychologist (ECM), and (3) METH use within the past six months. Exclusion criteria for METH subjects included (1) major medical or neurological disorders, including HIV seropositivity; (2) comorbid psychiatric disorders including schizophrenia, bipolar disorder, and use of other illicit drugs as preferred drug of abuse; (3) major sensorimotor handicaps (e.g., deafness, blindness, and paralysis), full scale IQ <70 or learning disabilities; and (4) contraindications to magnetic resonance imaging.
Healthy comparison (HC) subjects were recruited with the inclusion criteria (1) age 18 to 55 years, (2) no dependence or abuse of alcohol, METH, amphetamine, cocaine, heroin, alcohol, and cannabis, and (3) no psychiatric, neurologic, and medical disease identified by physical examination. The healthy subjects were matched on age and gender with METH users. The healthy subjects had a slightly higher level of education than METH users and this difference was controlled for statistically. Exclusion criteria for the HC subjects were the same as for the METH users. The study protocol was approved by the Institutional Review Boards of the University of Utah and the Department of Human Services of the State of Utah. Written informed consent was obtained from all study subjects before participation.
2.2 Magnetic Resonance Imaging and Spectroscopy Data Acquisition and Processing
2.2.1 Structural MR Images
Brain MR imaging was performed using a 3 Tesla Siemens scanner (Trio, Siemens AG, Erlangen, Germany) and a 31P/1H double-tuned volume head coil (Clinical MR Solutions LLC, Brookfield, WI) for transmission and reception. To obtain high resolution T1-weighted anatomical images for tissue segmentation and positioning MRS grids, a three dimensional chemical Magnetization Prepared Rapid Acquisition Gradient Echo (MPRAGE) pulse sequence was used. The parameters for the structural MRI were as follows: T1 weighted image: TR=2000 ms, TE=3.37 ms, TI=1100 ms, average number=1, flip angle=8°, FOV=256 mm, matrix 256×192×144, bandwidth=300 Hz/pixel, slice thickness 1.0 mm and no gap.
2.2.2 31P Magnetic Resonance Spectroscopy
Phosphorus spectra were acquired on the same 3 Tesla Siemens system using the 31P/1H double-tuned volume head coil. The spectra were obtained using a two dimensional-chemical shift imaging (2D-CSI) free induction decay (FID) pulse sequence with TR= 3000, TE=2.3 ms, average number=36, flip angle=90°, vector size=1024, FOV=200×200mm2, slice thickness=2.5 cm, matrix 8×8, sampling bandwidth=2.5 kHz, and voxel dimension=2.5×2.5 cm2. The 2D-CSI grid was positioned covering an axial brain slice just above an imaginary line connecting the anterior commissure and posterior commissure. The acquisition matrix of the 2D-CSI grid was 8x8 with the slice thickness 25mm (Figure 1). Shimming was performed over the excited brain volume. Since MRS data is significantly affected by magnetic field inhomogeneity, high order advanced shimming routine on the Siemens system was used to achieve linewidths of less than or equal to 15 Hz for the unsuppressed water signal. The proton channel was used for shimming, localization, and anatomic imaging. As an a priori region of interest (ROI), frontal lobe spectroscopic data were quantified. Also, as a control region for the comparison, temporoparietal lobe and occipital lobe were included in the spectroscopic and statistical analyses. The frontal lobe was selected as an active ROI because of prior reports suggesting frontal neurochemical abnormalities and hypometabolism in METH users (Kim et al., 2005; London et al., 2005; London et al., 2004; Sailasuta et al., 2010a)
Figure 1.
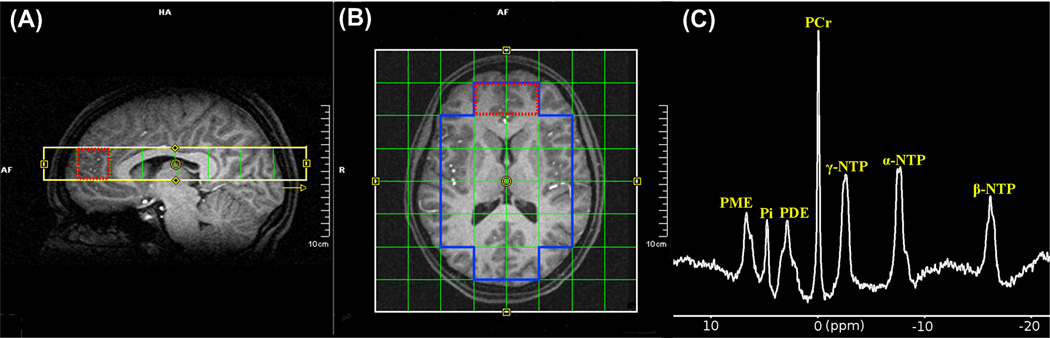
Illustration of two dimensional MRSI grid placement: (A) Sagittal and (B) Axial views. Dotted red line in the figure shows frontal lobe region of interest. (C) A representative 31P spectrum is displayed in frequency domain with 10 Hz exponential filtering. Abbreviations: PCr, phosphocreatine; PME, phosphomonoester; PDE, phosphodiester; α-, β-, γ-NTP (nucleoside triphosphate).
2.2.3 31P-MRS Data Analysis
Before performing 2D Fast Fourier Transform (FFT) on raw data, a Hamming filter was applied to reduce the effect of the point-spread-function, and each free induction decay (FID) was line-broadened with 10 Hz of apodization. After Fourier transformation and frequency shift correction, zero-/first-order phase correction and baseline correction with polynomial interpolation were applied. Metabolite location error resulting from different chemical shift displacement was corrected along in-plane readout and phase-encoding directions. Following that, spatial filtering with a Hamming window function was implemented to reduce the signal contamination from neighboring voxels. The preprocessed 31P-MRSI data was fitted using jMRUI software (Naressi et al., 2001) with the Advanced Method for Accurate, Robust and Efficient Spectral fitting (AMARES) algorithm (Vanhamme et al., 1997). Metabolites of interest were PCr, β-NTP, and their ratio (Figure 1C). Each metabolite concentration was expressed relative to the total pool of exchangeable phosphate (TPP; Blumberg et al., 1999). Referencing 31P metabolites to TPP facilitated effective evaluation of high energy phosphate metabolism (Amess et al., 1997; Cady et al., 2008; Iwata et al., 2008).
From the registered anatomical images, tissue segmentation was performed using FSL (FMRIB's Software Library) software so that cerebrospinal fluid (CSF)-corrected metabolite concentrations as well as gray matter percentage in each voxel could be used as covariates in the statistical analysis. No significant difference in CSF amount was detected in the frontal voxels between METH and control subjects (t72=0.56, p=0.58).
2.2.4 Statistical Analysis
Collected demographic and clinical data were managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at the University of Utah, which is a secure, web-based application designed to support data capture for research studies (Harris et al., 2009). Analysis of variance (ANOVA) was used for between-group comparisons involving continuous demographic data. Generalized Estimating Equations regression modeling was used to evaluate group differences in metabolite levels controlling for age, sex, education level, and tissue partial volume effects (i.e. gray matter, white matter, CSF). Fisher's Exact Test compared groups on categorical variables. To determine the clinical relevance of metabolite changes in METH users, robust multiple regression analyses (White, 1980) were performed to assess the relationship between PCr levels and lifetime amount of METH use or days of abstinence of METH. Partial correlation coefficients were calculated covarying for age and sex. Models with all pair-wise and three-way interactions between covariates were first considered, and interactions not significant were removed from the models. Statistical significance was defined at an alpha level of p=0.05, two-tailed. Stata for Unix, version 12.1 (StataCorp, College Station, TX) was used for all computations.
3. RESULTS
3.1 Demographics and clinical characteristics
There were no significant differences between the METH and the HC groups in terms of age (32.8±6.7 vs. 31.1±7.5 respectively, t72=0.95, p=0.35) and sex (45% vs. 47% female ratio respectively, Fisher's Exact Test, p=0.5). The METH users, however, had lower education level than the HC subjects although this difference was modest (12.7±1.8 vs. 13.9±1.3, respectively, p<0.05). Fifty METH users met lifetime METH dependence DSM-IV criteria and one participant was diagnosed with METH abuse. Table 1 presents study subject characteristics and other demographics in detail. Table 2 presents METH and other drug use history for all METH users.
Table 1.
Clinical characteristics and demographics
| Methamphetamine | Healthy subjects | Significance | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Female | Male | Total | Female | Male | ||||
| Subject demographics | (n=51) | (n=23) | (n=28) | p-value | (n=23) | (n=11) | (n=12) | p-value | |
| Education (years) | 12.7 (1.8)* | 12.6 (2.0) | 12.8 (1.6) | .65 | 13.9 (1.3)* | 13.9(1.2) | 13.9(1.5) | .95 | t72=2.88, p=.005* |
| Handedness (right/left) | 43/8 | 20/3 | 23/5 | .47 | 22/1 | 10/1 | 12/0 | .48 | FET, p=.16 |
| Ethnicity (white/others) | 45/6 | 20/3 | 25/3 | .57 | 21/2 | 10/1 | 11/1 | .74 | FET, p=.52 |
| Onset age of METH use (yrs) | 21.7 (6.6) | 20.4 (5.9) | 22.8 (7.0) | .20 | - | - | - | - | - |
| Duration of METH use (yrs) | 11.1 (7.0) | 9.3 (5.8) | 12.5 (7.6) | .10 | - | - | - | - | - |
| Abstinence of METH use (days) | 38.1 (42.5) | 46.3(54.1) | 31.4(29.2) | .21 | - | - | - | - | - |
| Daily dosage of METH use (g) | 1.3 (1.4) | 1.1(1.0) | 1.4(1.7) | .46 | - | - | - | - | - |
Data are expressed with mean (SD);
Indicates statistical significance between methamphetamine and healthy group;
Abbreviations: METH, methamphetamine; FET, Fisher's Exact Test
Table 2.
Profiles of drug use history
| Substance | Total Number of Subjects |
Mean Age of First Use (yrs) |
Mean Amount of Substance per day |
Frequency Used | Total Number of Subjects Currently Using |
Total Lifetime Amounta |
|---|---|---|---|---|---|---|
| Alcohol | 51 | 13 | 65 ounces | Occasionally to Weekly | 17 | 34 drink-years b |
| Amphetamine | 26 | 19 | Varies | Occasionally | 1 | Varies |
| Methamphetamine | 51 | 22 | 1.81 grams | Daily | 30 | 1923 grams |
| Cocaine | 48 | 20 | 1.49 grams | Occasionally | 1 | 1656 grams |
| Opiates | 22 | 25 | 0.69 grams | Occasionally | 0 | 351 grams |
| Hallucinogens | 36 | 17 | Varies | Rarely to Occasionally | 0 | Varies |
| Cannabis | 50 | 14.5 | 2.42 grams | Weekly | 12 | 3721 grams |
| Nicotine | 47 | 14 | 11 cigarettes | Daily | 41 | 10 pack-yearsc |
| Caffeine | 50 | 9 | 28 ounces | Daily | 49 | 27 cups-years d |
Total lifetime drug amount was estimated using "average daily dosage×frequency×duration."
Total intake calculated in drink-years (1 drink/day in 1 year).
A pack-year is defined as twenty cigarettes smoked everyday for one year (1 pack/day in 1 year).
A cups-year is defined as five cups of coffee everyday for one year.
3.2 Group differences in Metabolite levels
PCr levels in METH users were significantly reduced in the frontal lobe compared with those in HC group but not β-NTP/TPP levels (PCr/TPP, t72=−3.46, p=0.001; β-NTP/TPP, t72=0.56, p=0.58, Figure 2). The statistically significant reduction in PCr levels was maintained after controlling for potential confounding variables such as age, sex, education level, and tissue segmentation (t68=−2.99, p=0.004). As there was a high collinearity between group variable and alcohol amount/nicotine amount consumed, we did not conduct regression analysis adjusting for alcohol, nicotine and caffeine.
Figure 2.
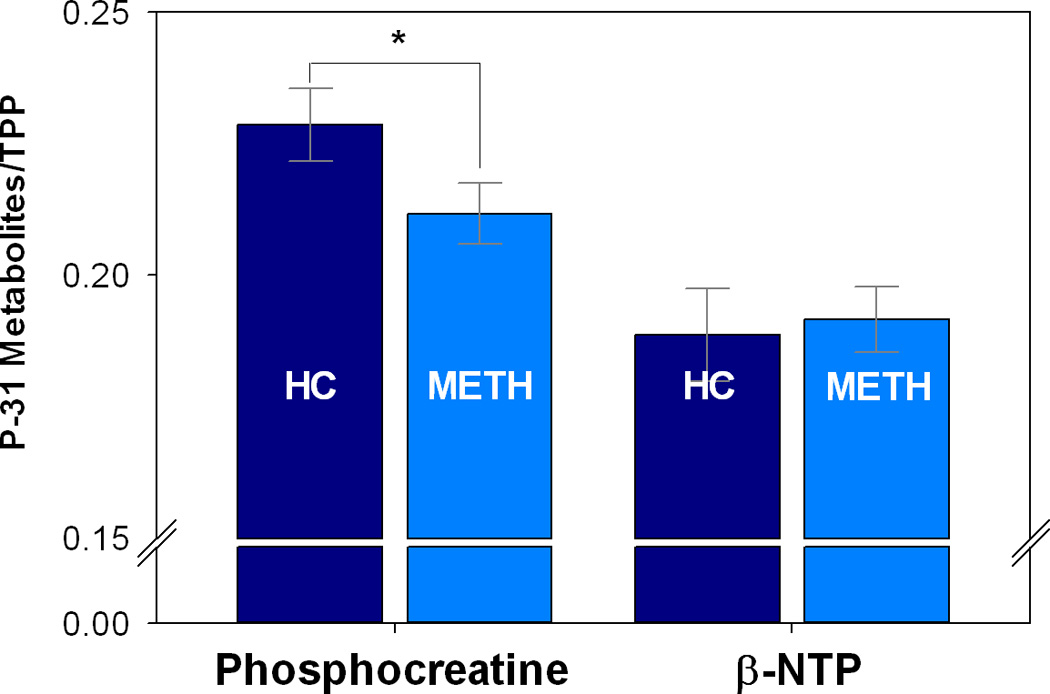
Comparison of frontal lobe phosphorus metabolites levels in methamphetamine (METH, n=51) dependent subjects compared to healthy controls (HC, n=23). Phosphocreatine levels were significantly reduced in METH users compared to HC (p<0.001). There were no significant differences in β-NTP levels between the HC and METH groups. Error bars represent 95% confidence intervals. * Indicates statistically significant difference. Abbreviations: TPP, total pool of exchangeable phosphate.
To ensure that decreased PCr/TPP did not result from increased total TPP values, we repeated our statistical analysis using β-NTP as a denominator, with findings remaining the same. Specifically PCr/β-NTP levels were significantly decreased in METH users compared to the HC subjects (t72=−2.08, p=0.04). Also, to ensure that the MR system did not drift across the study period, absolute measurements (arbitrary institutional unit) of total phosphorus were compared between the groups, with no group differences in TPP levels (p=0.10). Further, to assess test-retest reliability of our 31P-MRS protocol, we scanned nine healthy subjects twice using the exact same protocol. The intraclass correlation coefficient (ICC; Shrout and Fleiss, 1979) for PCr levels was calculated to be 0.72, which suggests good reliability.
Other metabolite levels such as phosphomonoester, phosphodiester, and inorganic phosphate were not significantly different between the groups (see Table 3). We did not find a statistically significant difference in PCr/TPP levels in other brain regions such as temporoparietal lobe (t72=−1.71, p=0.10) and occipital lobe (t72=1.60, p=0.12) between METH and HC subjects.
Table 3.
Phosphorus metabolite levels in the frontal lobe
| Methamphetamine | Healthy | p-value | |||||
|---|---|---|---|---|---|---|---|
| Total | Total | ||||||
| Metabolites† | (n=51) | Female | Male | (n=23) | Female | Male | |
| PCr | .212 (.021)* | .205 (.019)** | .217 (.021)** | .230 (.016)* | .225 (.018) | .231 (.014) | .001* |
| β-NTP | .192 (.022) | .195 (.025) | .189 (.019) | .189 (.020) | .187 (.027) | .190 (.013) | .58 |
| PME | .215 (.037) | .220 (.041) | .210 (.033) | .218 (.022) | .215 (.027) | .221 (.018) | .68 |
| PDE | .286 (.036) | .291 (.036) | .281 (.037) | .292 (.034) | .285 (.034) | .298 (.034) | .47 |
| Pi | .076 (.012) | .080 (.012) | .074 (.013) | .074 (.012) | .073 (.013) | .075 (.012) | .38 |
Data are expressed with mean (SD);
metabolite ratios over total pool of exchangeable phosphate;
Indicates statistically significant PCr differences between methamphetamine and healthy group (p=.001);
Indicates significant PCr differences between female and male methamphetamine users (p=.04). For other metabolites, there were neither group differences nor within-group gender differences.
Abbreviations: PCr, phosphocreatine; β-NTP, beta-nucleoside triphosphate; PME, phosphomonoester; PDE, phosphodiester; Pi, inorganic phosphate.
3.3 PCr levels in female vs. male METH users
Frontal PCr/TPP levels in female METH users were significantly lower (5.3%) than those in male METH users (t49=−2.06, p=0.04, Figure 3). Female METH users reported lower amounts of daily METH use (1.1±1.0 gram) compared to male METH users (1.4±1.7 gram) (t49=−0.75, p=0.46). After adjusting for the daily amount of daily METH use, the significance for betweengroup gender difference of PCr/TPP levels was maintained (t48=−2.41, p=0.02). In the healthy subjects, there were no significant gender differences in either PCr (t21=−0.90, p=0.38), β-NTP (t21=−0.90, p=0.38), or other metabolites (Table 3)
Figure 3.
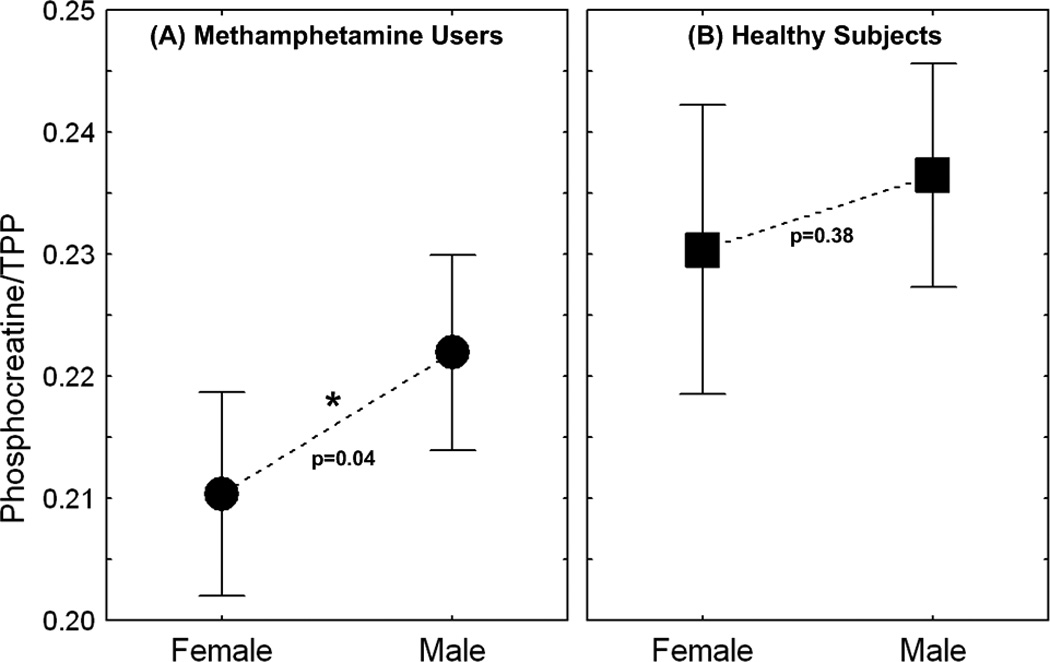
Comparison of gender difference in PCr levels. (A) In METH-dependent subjects, female METH users (n=23) had significantly lower PCr levels compared to male METH users (n=28). (B) Healthy subjects did not show significant gender difference. Error bars represent 95% confidence intervals. * Indicates statistically significant difference. Abbreviations: TPP, total pool of exchangeable phosphate.
3.4 Relationship between Frontal lobe PCr levels and lifetime METH amount
There was significant relationship between frontal lobe PCr levels and total amount of lifetime METH use (Figure 4), before (t49=−3.17, p=0.003), and after (t47=−2.87, p=0.006) controlling for age and education.
Figure 4.
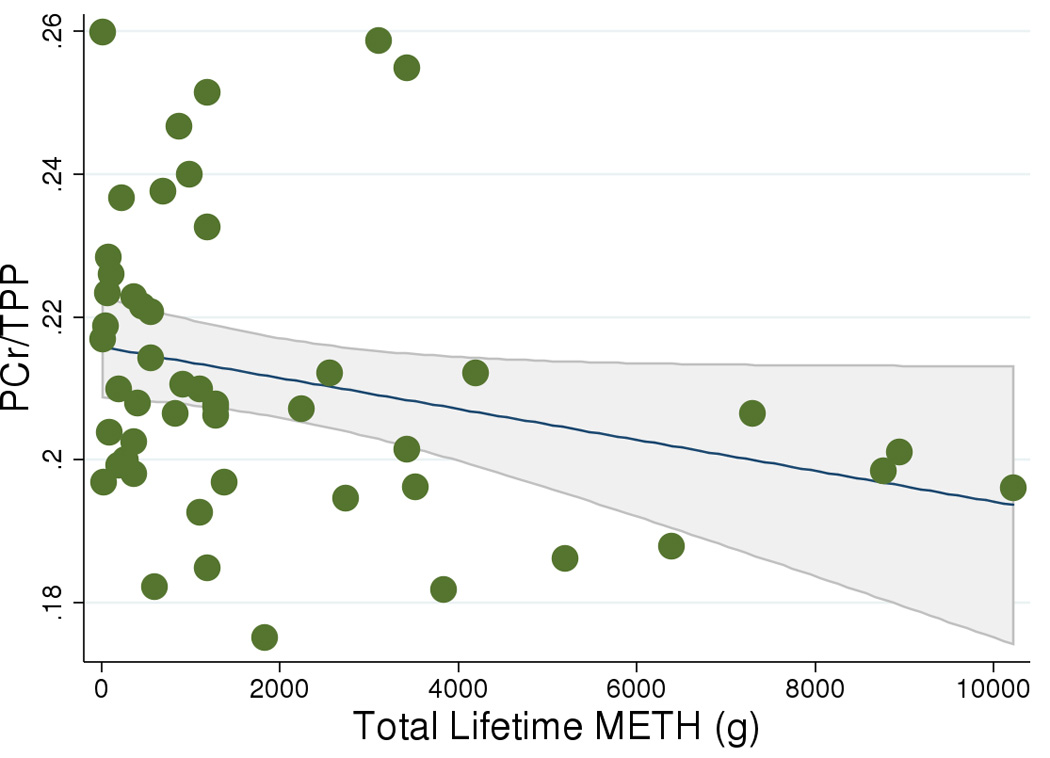
Significant relationship (p=0.003) between PCr/TPP levels and total amount of lifetime METH use (gram) in METH-dependent subjects (regression analysis using robust estimator of variance (White, 1980). Gray line and area denote predicted 95% confidence interval. Abbreviations: TPP, total pool of exchangeable phosphate.
3.5 Relationship between Frontal lobe PCr levels and duration of abstinence from METH
There was a trend toward a negative relationship between frontal lobe PCr levels and duration of METH abstinence but this was not statistically significant (t49=−1.49, p=0.14).
4. DISCUSSION
In this study, we found that METH users have abnormal PCr levels in the frontal lobe compared with the HC subjects. To the best of our knowledge, this is the first 31P-MRS study reporting abnormal brain cellular energetics in human METH users.
Our findings are consistent with the prior neuroimaging reports regarding metabolic hypofrontality in METH users. For example, 18F-fluorodeoxyglucose (FDG) PET studies have noted lower FDG uptake in the frontal lobe and cingulate (Kim et al., 2005; London et al., 2005; 2004) and in the striatum (Volkow et al., 2001a). Also, single photon emission computed tomography (SPECT) studies have reported decreased frontal blood flow in METH users (Hwang et al., 2006).
Of particular relevance to the decreased PCr levels and mitochondrial dysfunction in METH users, several 31P-MRS studies of individuals with primary mitochondrial disease have reported decreased PCr levels in the resting state of muscles (Argov et al., 1987; Arnold et al., 1985; Hoang et al., 1998) as well as in affected brain regions (Barbiroli et al., 1995,1993). Importantly, when there was no clinical brain involvement in the mitochondrial disease, patients had normal PCr levels (Rango et al., 2001). The abnormal PCr levels in our METH users are consistent with results observed in opioid-dependent subjects. For example, heroin-dependent subjects were reported to have decreased PCr levels (−15.3%) at the onset of methadone maintenance treatment (Silveri et al., 2004). Notably, decreased PCr levels in opiate-dependent polydrug abusers tended to recover after methadone maintenance therapy (Kaufman et al., 1999).
The alteration of PCr levels only in the frontal lobe of METH users suggest that the damage induced by METH may be region-specific rather than global in terms of brain energetics. The frontal lobe is more metabolically active than other brain regions (Ivancevic et al., 2000; Loessner et al., 1995) and frontal lobe dysfunction is commonly associated with chronic METH use (Henry et al., 2010). We previously reported that compromised frontal executive function was significantly correlated with reduced frontal glucose metabolism in METH dependent subjects (Kim et al., 2005). Therefore, it is possible that the reduced PCr levels may be a 31PMRS metabolic biomarker of hypofrontality in METH users.
The present phosphorus MRS findings are consistent with the existing proton MRS literature. For instance, reduced NAA levels, which are known to reflect the functional status of mitochondria have been associated with human METH use (Chang et al., 2005; Ernst et al., 2000; Nordahl et al., 2002; Sailasuta et al., 2010b; Sekine et al., 2002; Smith et al., 2001; Sung et al., 2007; Taylor et al., 2007). Of note, NAA is generated by L-aspartate N-acetyltransferase, an enzyme predominantly located in the mitochondria. Further, decreased PCr levels in our 31P-MRS findings are in line with the prior 1H-MRS reports of decreased total creatine plus phosphocreatine levels in METH users (Ernst et al., 2000).
Constant brain adenosine triphosphate levels are critical for cell survival and proper human brain functioning (Niizuma et al., 2009). In high energy phosphate metabolism, PCr-ATP buffering and the creatine kinase system (PCr2+ + ADP- ↔ Cr + ATP2+) play important roles in maintaining constant ATP levels. No significant differences in the β-NTP levels between METH users and HC subjects suggest a possible compensatory or homeostatic mechanism in maintaining ATP levels in METH users. Although the precise mechanisms remain unclear, creatine and PCr have been reported to have neuroprotective effects in various brain disorders including ischemic stroke and Alzheimer’s disease (Beard and Braissant, 2010). Therefore, our finding of decreased PCr levels may indicate an increased susceptibility to neurotoxic changes in METH users. This suggests a potential treatment target, as exogenous creatine supplementation, which increases PCr levels in healthy volunteers (Lyoo et al., 2003), might provide beneficial effects directly targeting the underlying pathophysiology of METH-induced mitochondrial toxicity. However, further study would be required to confirm the possible therapeutic effects of oral creatine in METH users.
Gender differences in METH toxicity have been reported in previous neuroimaging studies of diffusion tensor imaging and white matter hyperintensities (Bae et al., 2006; Chung et al., 2007). Male METH users had lower fractional anisotropy values and greater severity of white matter hyperintensites than female METH users. In the present 31P-MRS study, however, decreased PCr levels were more prominent in females. The exact mechanism responsible for lower PCr levels in female METH users is unclear and has yet to be elucidated. However, since lower brain levels of PCr have also been associated with severe depression (Kato et al., 1992) and worse outcomes in response to antidepressant treatment (Iosifescu et al., 2008), our findings may be related to the higher incidence of depression in female METH users (Semple et al., 2007). Indeed, METH abuse is associated with increased risk of depression and suicide attempts compared to rates observed in the general population (Glasner-Edwards et al., 2009). Also, METH abusers have higher female/male ratios (46%) than heroin (11%) or cocaine (29%) abusers (Cohen et al., 2007; Holdcraft and Iacono, 2004; Hser et al., 2008). Therefore, the relatively large reduction of PCr levels in female METH users highlights the potential consequences of bioenergetic impairment that merit special clinical attention in female subjects. Another possible underlying mechanism for lower PCr in female METH users may be related to the effect of gonadal hormones on brain PCr levels. For example, estrogen has been reported to stimulate brain-specific cytosolic creatine kinase activity (Kaye, 1983). Therefore, the higher estrogen levels in females may contribute to the decreased PCr levels through the forward (i.e. regenerating ATP) creatine kinase activity in the PCr-ATP buffer system. Although it was not statistically significant, we found slightly lower PCr levels in female healthy subjects. Interestingly, a recent PET study demonstrated decreased prefrontal metabolism in females but not in male cocaine users (Volkow et al., 2011). This observation suggests that gonadal hormones may be associated with increased risk of abnormal high energy phosphate metabolism. However, further study will be required to clarify the relationship between hormone levels and brain high energy phosphate changes.
The significant relationship between total amount of METH use and the PCr levels illustrates that heavy METH users might manifest as an abnormality in high energy phosphates in a dose-responsive manner. These findings raise the possibility that heavy METH users may benefit from agents which facilitate the recovery of frontal lobe PCr levels. A non-significant negative association between frontal lobe PCr levels and duration of METH abstinence suggests that recovery of PCr levels may not occur during the moderate levels of simple abstinence (95% confidence limits: 26 to 50 days). Indeed, the negative trend suggests that longer abstinence may result in PCr levels that remain low or even decline further. These findings are consistent with persistently lower striatal, but not thalamic, FDG metabolism in METH users compared to HC even after 12 to 17 months of abstinence (Wang et al., 2004), as well as significantly reduced striatal dopamine transporter levels in METH users compared to HC even after 11 months of abstinence (Volkow et al., 2001b).
4.1 Study Limitations
When considering our findings, several factors should be taken into consideration. The 31PMRS data are reported by ratio to TPP with no absolute 31P metabolite concentration. Although this is a standard practice in the MRS literature, decreased PCr/TPP may have originated from increased TPP levels (Jansen et al., 2006; Jayakumar et al., 2010). However, even when we use a different denominator such as β-NTP, we observe similar results. Also, metabolite ratio measures have been compared favorably with absolute measures (Klunk et al., 1994). Therefore, decreased PCr/TPP ratios are likely to reflect decreased PCr levels.
Female subjects were not scanned at the same phase of the menstrual cycle in the present study. Since prior published studies suggest hormonal levels are related to subjective reports of stimulation after D-amphetamine administration (Reed et al., 2010; White et al., 2002), phosphorus metabolite levels may also fluctuate across the menstrual cycle in the females, placing the lack of the control of menstrual phase as a limitation of this study. However, since the female subjects were randomly scanned for both controls and METH users, we believe that the variance in PCr levels was similar between groups, and hence the menstrual phase variation did not significantly affect our findings.
Multiple comparisons were performed in statistical analysis for our metabolites of interest, PCr and β-NTP. As we used an a priori hypothesis in our research design, corrections for multiple comparisons were not attempted. Therefore, readers should be aware of possible type I errors arising from our analysis.
The METH subject enrollment criteria involved the inclusion of subjects who identified METH as their drug of choice. Therefore, the characteristics of our cohort may not represent general METH users and our findings may not be generalized to other METH-dependent populations. On the other hand, all METH users abused other drugs to some degree and decreased PCr levels in METH users may be, in part, due to polysubstance abuse. Self report of drug use history in METH subjects might have resulted in some degree of uncertainty including underreport of drug use behaviors.
Because the location of our 2D-CSI grid was immediately superior to the AC-PC line, we could not include subgenual cingulate or cerebellum as regions-of-interest to evaluate whether these brain regions have abnormalities in high energy phosphorus metabolism. Since the subgenual cingulate is reported to be associated with depression (Drevets et al., 2008; Mayberg et al., 2005), a study design including this brain region will be important in future studies.
5. CONCLUSION
Overall, the present study provides evidence of altered high-energy phosphate metabolism in METH users. Our findings suggest that (1) METH use is associated with dose-dependent decreases in high-energy PCr levels, which may imply a decreased energetic buffer due to mitochondrial dysfunction; and (2) female METH users may be more vulnerable than male METH users in terms of high-energy phosphate neurochemistry. Further study is warranted to explore the relationship between the altered phosphorus metabolism and cognitive as well as psychiatric symptoms. Also, a longitudinal study design would shed light on within-subject changes in high energy phosphate metabolism following long-term abstinence and/or treatment. Efforts to characterize the relationship between the changes in high energy phosphates and psychiatric symptomatology have the potential to generate novel treatment strategies for METH toxicity.
Acknowledgments
Role of funding source
This study was supported by funding from NIH 1R01DA027135 (PFR). The funding agency had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented in part at the 73rd annual meeting of the College on Problems of Drug Dependence, Hollywood, FL, June 18-23, 2011
Contributors
Authors Yurgelun-Todd, Sung, and Renshaw designed the study and wrote the protocol. Author Sung wrote the first draft of the manuscript and undertook the statistical analysis. Authors Shi, Kondo, Lundberg, McGlade, Hellem, Huber, Fiedler, Harrell, Nickerson, Kim and Jeong participated in data collection and interpretation. Authors Renshaw and Yurgelun-Todd wrote the final draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of interest
Dr. Renshaw is a consultant for Kyowa Hakko and Ridge Diagnostics. Dr. Yurgelun-Todd is a consultant for Eli Lilly, and Novartis, and has research support from Kyowa Hakko.
REFERENCES
- Amess PN, Penrice J, Cady EB, Lorek A, Wylezinska M, Cooper CE, D'Souza P, Tyszczuk L, Thoresen M, Edwards AD, Wyatt JS, Reynolds EO. Mild hypothermia after severe transient hypoxia-ischemia reduces the delayed rise in cerebral lactate in the newborn piglet. Pediatr. Res. 1997;41:803–808. doi: 10.1203/00006450-199706000-00002. [DOI] [PubMed] [Google Scholar]
- Anker JJ, Carroll ME. Females are more vulnerable to drug abuse than males: evidence from preclinical studies and the role of ovarian hormones. Curr. Top Behav. Neurosci. 2011;8:73–96. doi: 10.1007/7854_2010_93. [DOI] [PubMed] [Google Scholar]
- Argov Z, Bank WJ, Maris J, Peterson P, Chance B. Bioenergetic heterogeneity of human mitochondrial myopathies: phosphorus magnetic resonance spectroscopy study. Neurology. 1987;37:257–262. doi: 10.1212/wnl.37.2.257. [DOI] [PubMed] [Google Scholar]
- Arnold DL, Taylor DJ, Radda GK. Investigation of human mitochondrial myopathies by phosphorus magnetic resonance spectroscopy. Ann. Neurol. 1985;18:189–196. doi: 10.1002/ana.410180205. [DOI] [PubMed] [Google Scholar]
- Bae SC, Lyoo IK, Sung YH, Yoo J, Chung A, Yoon SJ, Kim DJ, Hwang J, Kim SJ, Renshaw PF. Increased white matter hyperintensities in male methamphetamine abusers. Drug Alcohol Depend. 2006;81:83–88. doi: 10.1016/j.drugalcdep.2005.05.016. [DOI] [PubMed] [Google Scholar]
- Barbiroli B, Montagna P, Cortelli P, Iotti S, Lodi R, Barboni P, Monari L, Lugaresi E, Frassineti C, Zaniol P. Defective brain and muscle energy metabolism shown by in vivo 31P magnetic resonance spectroscopy in nonaffected carriers of 11778 mtDNA mutation. Neurology. 1995;45:1364–1369. doi: 10.1212/wnl.45.7.1364. [DOI] [PubMed] [Google Scholar]
- Barbiroli B, Montagna P, Martinelli P, Lodi R, Iotti S, Cortelli P, Funicello R, Zaniol P. Defective brain energy metabolism shown by in vivo 31P MR spectroscopy in 28 patients with mitochondrial cytopathiesJCereb. Blood Flow Metab. 1993;13:469–474. doi: 10.1038/jcbfm.1993.61. [DOI] [PubMed] [Google Scholar]
- Beard E, Braissant O. Synthesis and transport of creatine in the CNS: importance for cerebral functions. J. Neurochem. 2010;115:297–313. doi: 10.1111/j.1471-4159.2010.06935.x. [DOI] [PubMed] [Google Scholar]
- Blumberg RM, Taylor DL, Yue X, Aguan K, McKenzie J, Cady EB, Weiner CP, Mehmet H, Edwards AD. Increased nitric oxide synthesis is not involved in delayed cerebral energy failure following focal hypoxic-ischemic injury to the developing brain. Pediatr. Res. 1999;46:224–231. doi: 10.1203/00006450-199908000-00016. [DOI] [PubMed] [Google Scholar]
- Brown JM, Quinton MS, Yamamoto BK. Methamphetamine-induced inhibition of mitochondrial complex II: roles of glutamate and peroxynitrite. J Neurochem. 2005;95:429–436. doi: 10.1111/j.1471-4159.2005.03379.x. [DOI] [PubMed] [Google Scholar]
- Burrows KB, Gudelsky G, Yamamoto BK. Rapid and transient inhibition of mitochondrial function following methamphetamine or 3,4-methylenedioxymethamphetamine administration. Eur. J. Pharmacol. 2000a;398:11–18. doi: 10.1016/s0014-2999(00)00264-8. [DOI] [PubMed] [Google Scholar]
- Burrows KB, Nixdorf WL, Yamamoto BK. Central administration of methamphetamine synergizes with metabolic inhibition to deplete striatal monoamines. J. Pharmacol. Exp. Ther. 2000b;292:853–860. [PubMed] [Google Scholar]
- Cady EB, Iwata O, Bainbridge A, Wyatt JS, Robertson NJ. Phosphorus magnetic resonance spectroscopy 2 h after perinatal cerebral hypoxia-ischemia prognosticates outcome in the newborn piglet. J. Neurochem. 2008;107:1027–1035. doi: 10.1111/j.1471-4159.2008.05662.x. [DOI] [PubMed] [Google Scholar]
- Carroll ME, Lynch WJ, Roth ME, Morgan AD, Cosgrove KP. Sex and estrogen influence drug abuse. Trends Pharmacol. Sci. 2004;25:273–279. doi: 10.1016/j.tips.2004.03.011. [DOI] [PubMed] [Google Scholar]
- Chang L, Ernst T, Speck O, Grob CS. Additive effects of HIV and chronic methamphetamine use on brain metabolite abnormalities. Am. J, Psychiatry. 2005;162:361–369. doi: 10.1176/appi.ajp.162.2.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung A, Lyoo IK, Kim SJ, Hwang J, Bae SC, Sung YH, Sim ME, Song IC, Kim J, Chang KH, Renshaw PF. Decreased frontal white-matter integrity in abstinent methamphetamine abusers. Int. J. Neuropsychopharmacol. 2007;10:765–775. doi: 10.1017/S1461145706007395. [DOI] [PubMed] [Google Scholar]
- Cohen JB, Greenberg R, Uri J, Halpin M, Zweben JE. Women with methamphetamine dependence: research on etiology and treatment. J. Psychoactive Drugs Suppl. 2007;4:347–351. doi: 10.1080/02791072.2007.10399896. [DOI] [PubMed] [Google Scholar]
- Cunha-Oliveira T, Rego AC, Cardoso SM, Borges F, Swerdlow RH, Macedo T, de Oliveira CR. Mitochondrial dysfunction and caspase activation in rat cortical neurons treated with cocaine or amphetamine. Brain Res. 2006;1089:44–54. doi: 10.1016/j.brainres.2006.03.061. [DOI] [PubMed] [Google Scholar]
- Dhandapani KM, Brann DW. Protective effects of estrogen and selective estrogen receptor modulators in the brain. Biol. Reprod. 2002;67:1379–1385. doi: 10.1095/biolreprod.102.003848. [DOI] [PubMed] [Google Scholar]
- Dluzen DE, Liu B. Gender differences in methamphetamine use and responses: a review. Gend. Med. 2008;5:24–35. doi: 10.1016/s1550-8579(08)80005-8. [DOI] [PubMed] [Google Scholar]
- Dolder M, Wendt S, Wallimann T. Mitochondrial creatine kinase in contact sites: interaction with porin and adenine nucleotide translocase, role in permeability transition and sensitivity to oxidative damage. Biol. Signals Recept. 2001;10:93–111. doi: 10.1159/000046878. [DOI] [PubMed] [Google Scholar]
- Drevets WC, Savitz J, Trimble M. The subgenual anterior cingulate cortex in mood disorders. CNS Spectr. 2008;13:663–681. doi: 10.1017/s1092852900013754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst T, Chang L, Leonido-Yee M, Speck O. Evidence for long-term neurotoxicity associated with methamphetamine abuse: a 1H MRS study. Neurology. 2000;54:1344–1349. doi: 10.1212/wnl.54.6.1344. [DOI] [PubMed] [Google Scholar]
- Glasner-Edwards S, Marinelli-Casey P, Hillhouse M, Ang A, Mooney LJ, Rawson R Methamphetamine Treatment Project Corporate, A. Depression among methamphetamine users: association with outcomes from the Methamphetamine Treatment Project at 3-year follow-up. J. Nerv. Ment. Dis. 2009;197:225–231. doi: 10.1097/NMD.0b013e31819db6fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry BL, Minassian A, Perry W. Effect of methamphetamine dependence on everyday functional ability. Addict. Behav. 2010;35:593–598. doi: 10.1016/j.addbeh.2010.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoang TQ, Bluml S, Dubowitz DJ, Moats R, Kopyov O, Jacques D, Ross BD. Quantitative proton-decoupled 31P MRS and 1H MRS in the evaluation of Huntington's and Parkinson's diseases. Neurology. 1998;50:1033–1040. doi: 10.1212/wnl.50.4.1033. [DOI] [PubMed] [Google Scholar]
- Holdcraft LC, Iacono WG. Cross-generational effects on gender differences in psychoactive drug abuse and dependence. Drug Alcohol Depend. 2004;74:147–158. doi: 10.1016/j.drugalcdep.2003.11.016. [DOI] [PubMed] [Google Scholar]
- Hser YI, Evans E, Huang YC. Treatment outcomes among women and men methamphetamine abusers in California. J. Subst. Abuse Treat. 2005;28:77–85. doi: 10.1016/j.jsat.2004.10.009. [DOI] [PubMed] [Google Scholar]
- Hser YI, Huang D, Brecht ML, Li L, Evans E. Contrasting trajectories of heroin, cocaine, and methamphetamine use. J. Addict. Dis. 2008;27:13–21. doi: 10.1080/10550880802122554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang J, Lyoo IK, Kim SJ, Sung YH, Bae S, Cho SN, Lee HY, Lee DS, Renshaw PF. Decreased cerebral blood flow of the right anterior cingulate cortex in long-term and short-term abstinent methamphetamine users. Drug Alcohol Depend. 2006;82:177–181. doi: 10.1016/j.drugalcdep.2005.09.011. [DOI] [PubMed] [Google Scholar]
- Iosifescu DV, Bolo NR, Nierenberg AA, Jensen JE, Fava M, Renshaw PF. Brain bioenergetics and response to triiodothyronine augmentation in major depressive disorder. Biol. Psychiatry. 2008;63:1127–1134. doi: 10.1016/j.biopsych.2007.11.020. [DOI] [PubMed] [Google Scholar]
- Ivancevic V, Alavi A, Souder E, Mozley PD, Gur RE, Benard F, Munz DL. Regional cerebral glucose metabolism in healthy volunteers determined by fluordeoxyglucose positron emission tomography: appearance and variance in the transaxial, coronal, and sagittal planes. Clin. Nucl. Med. 2000;25:596–602. doi: 10.1097/00003072-200008000-00005. [DOI] [PubMed] [Google Scholar]
- Iwata O, Iwata S, Bainbridge A, De Vita E, Matsuishi T, Cady EB, Robertson NJ. Supra- and sub-baseline phosphocreatine recovery in developing brain after transient hypoxia-ischaemia: relation to baseline energetics, insult severity and outcome. Brain. 2008;131:2220–2226. doi: 10.1093/brain/awn150. [DOI] [PubMed] [Google Scholar]
- Iyo M, Sekine Y, Mori N. Neuromechanism of developing methamphetamine psychosis: a neuroimaging study. Ann. N.Y. Acad. Sci. 2004;1025:288–295. doi: 10.1196/annals.1316.036. [DOI] [PubMed] [Google Scholar]
- Jansen JF, Backes WH, Nicolay K, Kooi ME. 1H MR spectroscopy of the brain: absolute quantification of metabolites. Radiology. 2006;240:318–332. doi: 10.1148/radiol.2402050314. [DOI] [PubMed] [Google Scholar]
- Jayakumar PN, Gangadhar BN, Venkatasubramanian G, Desai S, Velayudhan L, Subbakrishna D, Keshavan MS. High energy phosphate abnormalities normalize after antipsychotic treatment in schizophrenia: a longitudinal 31P MRS study of basal ganglia. Psychiatry Res. 2010;181:237–240. doi: 10.1016/j.pscychresns.2009.10.010. [DOI] [PubMed] [Google Scholar]
- Kalechstein AD, Newton TF, Longshore D, Anglin MD, van Gorp WG, Gawin FH. Psychiatric comorbidity of methamphetamine dependence in a forensic sample. J. Neuropsychiatry Clin. Neurosci. 2000;12:480–484. doi: 10.1176/jnp.12.4.480. [DOI] [PubMed] [Google Scholar]
- Kato T, Takahashi S, Shioiri T, Inubushi T. Brain phosphorous metabolism in depressive disorders detected by phosphorus-31 magnetic resonance spectroscopy. J. Affect. Disord. 1992;26:223–230. doi: 10.1016/0165-0327(92)90099-r. [DOI] [PubMed] [Google Scholar]
- Kaufman MJ, Pollack MH, Villafuerte RA, Kukes TJ, Rose SL, Mendelson JH, Cohen BM, Renshaw PF. Cerebral phosphorus metabolite abnormalities in opiatedependent polydrug abusers in methadone maintenance. Psychiatry Res. 1999;90:143–152. doi: 10.1016/s0925-4927(99)00017-7. [DOI] [PubMed] [Google Scholar]
- Kaye AM. Enzyme induction by estrogen. J. Steroid Biochem. 1983;19:33–40. [PubMed] [Google Scholar]
- Kim SJ, Lyoo IK, Hwang J, Sung YH, Lee HY, Lee DS, Jeong DU, Renshaw PF. Frontal glucose hypometabolism in abstinent methamphetamine users. Neuropsychopharmacology. 2005;30:1383–1391. doi: 10.1038/sj.npp.1300699. [DOI] [PubMed] [Google Scholar]
- Klongpanichapak S, Govitrapong P, Sharma SK, Ebadi M. Attenuation of cocaine and methamphetamine neurotoxicity by coenzyme Q10. Neurochem. Res. 2006;31:303–311. doi: 10.1007/s11064-005-9025-3. [DOI] [PubMed] [Google Scholar]
- Klunk WE, Xu CJ, Panchalingam K, McClure RJ, Pettegrew JW. Analysis of magnetic resonance spectra by mole percent: comparison to absolute units. Neurobiol. Aging. 1994;15:133–140. doi: 10.1016/0197-4580(94)90153-8. [DOI] [PubMed] [Google Scholar]
- Kokoshka JM, Metzger RR, Wilkins DG, Gibb JW, Hanson GR, Fleckenstein AE. Methamphetamine treatment rapidly inhibits serotonin, but not glutamate, transporters in rat brain. Brain Res. 1998;799:78–83. doi: 10.1016/s0006-8993(98)00472-7. [DOI] [PubMed] [Google Scholar]
- Loessner A, Alavi A, Lewandrowski KU, Mozley D, Souder E, Gur RE. Regional cerebral function determined by FDG-PET in healthy volunteers: normal patterns and changes with age. J. Nucl. Med. 1995;36:1141–1149. [PubMed] [Google Scholar]
- London ED, Berman SM, Voytek B, Simon SL, Mandelkern MA, Monterosso J, Thompson PM, Brody AL, Geaga JA, Hong MS, Hayashi KM, Rawson RA, Ling W. Cerebral metabolic dysfunction and impaired vigilance in recently abstinent methamphetamine abusers. Biol. Psychiatry. 2005;58:770–778. doi: 10.1016/j.biopsych.2005.04.039. [DOI] [PubMed] [Google Scholar]
- London ED, Simon SL, Berman SM, Mandelkern MA, Lichtman AM, Bramen J, Shinn AK, Miotto K, Learn J, Dong Y, Matochik JA, Kurian V, Newton T, Woods R, Rawson R, Ling W. Mood disturbances and regional cerebral metabolic abnormalities in recently abstinent methamphetamine abusers. Arch. Gen. Psychiatry. 2004;61:73–84. doi: 10.1001/archpsyc.61.1.73. [DOI] [PubMed] [Google Scholar]
- Lubman DI, Yucel M, Pantelis C. Addiction, a condition of compulsive behaviour? Neuroimaging and neuropsychological evidence of inhibitory dysregulation. Addiction. 2004;99:1491–1502. doi: 10.1111/j.1360-0443.2004.00808.x. [DOI] [PubMed] [Google Scholar]
- Lyoo IK, Kong SW, Sung SM, Hirashima F, Parow A, Hennen J, Cohen BM, Renshaw PF. Multinuclear magnetic resonance spectroscopy of high-energy phosphate metabolites in human brain following oral supplementation of creatine-monohydrate. Psychiatry Res. 2003;123:87–100. doi: 10.1016/s0925-4927(03)00046-5. [DOI] [PubMed] [Google Scholar]
- Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, Schwalb JM, Kennedy SH. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45:651–660. doi: 10.1016/j.neuron.2005.02.014. [DOI] [PubMed] [Google Scholar]
- Moffett JR, Ross B, Arun P, Madhavarao CN, Namboodiri AM. N-Acetylaspartate in the CNS: from neurodiagnostics to neurobiology. Prog. Neurobiol. 2007;81:89–131. doi: 10.1016/j.pneurobio.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naressi A, Couturier C, Devos JM, Janssen M, Mangeat C, de Beer R, Graveron-Demilly D. Java-based graphical user interface for the MRUI quantitation package. MAGMA. 2001;12:141–152. doi: 10.1007/BF02668096. [DOI] [PubMed] [Google Scholar]
- Niizuma K, Endo H, Chan PH. Oxidative stress and mitochondrial dysfunction as determinants of ischemic neuronal death and survival. J. Neurochem. 2009;109(Suppl 1):133–138. doi: 10.1111/j.1471-4159.2009.05897.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordahl TE, Salo R, Possin K, Gibson DR, Flynn N, Leamon M, Galloway GP, Pfefferbaum A, Spielman DM, Adalsteinsson E, Sullivan EV. Low N-acetyl-aspartate and high choline in the anterior cingulum of recently abstinent methamphetaminedependent subjects: a preliminary proton MRS study. Magnetic resonance spectroscopy. Psychiatry Res. 2002;116:43–52. doi: 10.1016/s0925-4927(02)00088-4. [DOI] [PubMed] [Google Scholar]
- Oh JS, Lyoo IK, Sung YH, Hwang J, Kim J, Chung A, Park KS, Kim SJ, Renshaw PF, Song IC. Shape changes of the corpus callosum in abstinent methamphetamine users. Neurosci. Lett. 2005;384:76–81. doi: 10.1016/j.neulet.2005.04.082. [DOI] [PubMed] [Google Scholar]
- Oliveira MT, Rego AC, Morgadinho MT, Macedo TR, Oliveira CR. Toxic effects of opioid and stimulant drugs on undifferentiated PC12 cells. Ann. N.Y. Acad. Sci. 2002;965:487–496. doi: 10.1111/j.1749-6632.2002.tb04190.x. [DOI] [PubMed] [Google Scholar]
- Patel TB, Clark JB. Synthesis of N-acetyl-L-aspartate by rat brain mitochondria and its involvement in mitochondrial/cytosolic carbon transport. Biochem. J. 1979;184:539–546. doi: 10.1042/bj1840539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rango M, Bozzali M, Prelle A, Scarlato G, Bresolin N. Brain activation in normal subjects and in patients affected by mitochondrial disease without clinical central nervous system involvement: a phosphorus magnetic resonance spectroscopy study. J. Cereb. Blood Flow Metab. 2001;21:85–91. doi: 10.1097/00004647-200101000-00011. [DOI] [PubMed] [Google Scholar]
- Reed SC, Levin FR, Evans SM. The effects of progesterone pretreatment on the response to oral d-amphetamine in Women. Horm. Behav. 2010;58:533–543. doi: 10.1016/j.yhbeh.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renshaw PF, Parow AM, Hirashima F, Ke Y, Moore CM, Frederick Bde B, Fava M, Hennen J, Cohen BM. Multinuclear magnetic resonance spectroscopy studies of brain purines in major depression. Am. J. Psychiatry. 2001;158:2048–2055. doi: 10.1176/appi.ajp.158.12.2048. [DOI] [PubMed] [Google Scholar]
- Ricaurte GA, Schuster CR, Seiden LS. Long-term effects of repeated methylamphetamine administration on dopamine and serotonin neurons in the rat brain: a regional study. Brain Res. 1980;193:153–163. doi: 10.1016/0006-8993(80)90952-x. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res. Brain Res. Rev. 1993;18:247–291. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- Sailasuta N, Abulseoud O, Harris KC, Ross BD. Glial dysfunction in abstinent methamphetamine abusers. J. Cereb. Blood Flow Metab. 2010a;30:950–960. doi: 10.1038/jcbfm.2009.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sailasuta N, Abulseoud O, Hernandez M, Haghani P, Ross BD. Metabolic Abnormalities in Abstinent Methamphetamine Dependent Subjects. Subst. Abuse. 2010b;2010:9–20. doi: 10.4137/sart.s4625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlattner U, Tokarska-Schlattner M, Wallimann T. Mitochondrial creatine kinase in human health and disease. Biochim. Biophys. Acta. 2006;1762:164–180. doi: 10.1016/j.bbadis.2005.09.004. [DOI] [PubMed] [Google Scholar]
- Sekine Y, Minabe Y, Kawai M, Suzuki K, Iyo M, Isoda H, Sakahara H, Ashby CR, Jr, Takei N, Mori N. Metabolite alterations in basal ganglia associated with methamphetamine-related psychiatric symptoms. A proton MRS study. Neuropsychopharmacology. 2002;27:453–461. doi: 10.1016/S0893-133X(02)00321-4. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Zians J, Strathdee SA, Patterson TL. Psychosocial and behavioral correlates of depressed mood among female methamphetamine users. J. Psychoactive Drugs Suppl. 2007;4:353–366. doi: 10.1080/02791072.2007.10399897. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol. Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Silveri MM, Pollack MH, Diaz CI, Nassar LE, Mendelson JH, Yurgelun-Todd DA, Renshaw PF, Kaufman MJ. Cerebral phosphorus metabolite and transverse relaxation time abnormalities in heroin-dependent subjects at onset of methadone maintenance treatment. Psychiatry Res. 2004;131:217–226. doi: 10.1016/j.pscychresns.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Smith LM, Chang L, Yonekura ML, Grob C, Osborn D, Ernst T. Brain proton magnetic resonance spectroscopy in children exposed to methamphetamine in utero. Neurology. 2001;57:255–260. doi: 10.1212/wnl.57.2.255. [DOI] [PubMed] [Google Scholar]
- Sung YH, Cho SC, Hwang J, Kim SJ, Kim H, Bae S, Kim N, Chang KH, Daniels M, Renshaw PF, Lyoo IK. Relationship between N-acetyl-aspartate in gray and white matter of abstinent methamphetamine abusers and their history of drug abuse: a proton magnetic resonance spectroscopy study. Drug Alcohol Depend. 2007;88:28–35. doi: 10.1016/j.drugalcdep.2006.09.011. [DOI] [PubMed] [Google Scholar]
- Taylor MJ, Schweinsburg BC, Alhassoon OM, Gongvatana A, Brown GG, Young-Casey C, Letendre SL, Grant I, Group H. Effects of human immunodeficiency virus and methamphetamine on cerebral metabolites measured with magnetic resonance spectroscopy. J. Neurovirol. 2007;13:150–159. doi: 10.1080/13550280701194230. [DOI] [PubMed] [Google Scholar]
- Vanhamme L, van den Boogaart A, Van Huffel S. Improved method for accurate and efficient quantification of MRS data with use of prior knowledge. J. Magn. Reson. 1997;129:35–43. doi: 10.1006/jmre.1997.1244. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Chang L, Wang GJ, Fowler JS, Franceschi D, Sedler MJ, Gatley SJ, Hitzemann R, Ding YS, Wong C, Logan J. Higher cortical and lower subcortical metabolism in detoxified methamphetamine abusers. Am. J. Psychiatry. 2001a;158:383–389. doi: 10.1176/appi.ajp.158.3.383. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Chang L, Wang GJ, Fowler JS, Leonido-Yee M, Franceschi D, Sedler MJ, Gatley SJ, Hitzemann R, Ding YS, Logan J, Wong C, Miller EN. Association of dopamine transporter reduction with psychomotor impairment in methamphetamine abusers. Am. J. Psychiatry. 2001b;158:377–382. doi: 10.1176/appi.ajp.158.3.377. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Tomasi D, Wang GJ, Fowler JS, Telang F, Goldstein RZ, Alia-Klein N, Wong C. Reduced metabolism in brain "control networks" following cocaine-cues exposure in female cocaine abusers. PLoS One. 2011;6:e16573. doi: 10.1371/journal.pone.0016573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallimann T, Dolder M, Schlattner U, Eder M, Hornemann T, O'Gorman E, Ruck A, Brdiczka D. Some new aspects of creatine kinase (CK): compartmentation, structure, function and regulation for cellular and mitochondrial bioenergetics and physiology. Biofactors. 1998;8:229–234. doi: 10.1002/biof.5520080310. [DOI] [PubMed] [Google Scholar]
- Wang GJ, Volkow ND, Chang L, Miller E, Sedler M, Hitzemann R, Zhu W, Logan J, Ma Y, Fowler JS. Partial recovery of brain metabolism in methamphetamine abusers after protracted abstinence. Am. J. Psychiatry. 2004;161:242–248. doi: 10.1176/appi.ajp.161.2.242. [DOI] [PubMed] [Google Scholar]
- White H. A Heteroskedasticity-Consistent Covariance Matrix Estimator and a Direct Test for Heteroskedasticity. Econometrica. 1980;48:817–838. [Google Scholar]
- White TL, Justice AJ, de Wit H. Differential subjective effects of D-amphetamine by gender, hormone levels and menstrual cycle phase. Pharmacol. Biochem. Behav. 2002;73:729–741. doi: 10.1016/s0091-3057(02)00818-3. [DOI] [PubMed] [Google Scholar]
- Winslow BT, Voorhees KI, Pehl KA. Methamphetamine abuse. Am. Fam. Physician. 2007;76:1169–1174. [PubMed] [Google Scholar]
- Yucel M, Lubman DI. Neurocognitive and neuroimaging evidence of behavioural dysregulation in human drug addiction: implications for diagnosis, treatment and prevention. Drug Alcohol Rev. 2007;26:33–39. doi: 10.1080/09595230601036978. [DOI] [PubMed] [Google Scholar]


