Abstract
Purpose.
We investigated the role of retrograde signaling in the optic nerve on retinal ganglion cell (RGC) electrical responsiveness in the mouse model.
Methods.
Electrical response of RGC was measured by pattern electroretinogram (PERG) in 43 C57BL/6J mice 4 to 6 months old under ketamine/xylazine anesthesia. PERGs were recorded before and at different times after blockade of axon transport with lidocaine at either the retrobulbar level (2 μL, 40 μg/μL) or at level of the superior colliculus (SC, 1 μL, 40 μg/μL). PERGs also were recorded before and at different times after optic nerve crush 1.5 mm behind the eye, followed by TUJ1-positive RGC counts of excised retinas. As controls, PERGs also were recorded after either saline injections or sham optic nerve surgery. The photopic flash electroretinogram (FERG) and visual evoked potential (FVEP) also were recorded before lidocaine and at relevant times afterwards.
Results.
Lidocaine injection caused rapid (retrobulbar ∼10 minutes, SC 1 hour), reversible reduction of PERG amplitude (≥50%). Optic nerve crush caused rapid (10–20 minutes), irreversible reduction of PERG amplitude (70–75%), increase of PERG latency (>25%), as well as RGC loss (88%) 1 month after crush. FVEP was unaltered by lidocaine. For all procedures, the FERG was unaltered.
Conclusions.
As experimental interventions were made at postretinal level(s), PERG changes were likely associated with altered supply of retrogradely-delivered material from the SC. This implies that retrograde transport of target-derived molecules is necessary for normal RGC electrical responsiveness. The time course of early PERG changes is consistent with the speed of fast retrograde axon transport.
Blockage of retrograde axon transport in the retinocollicular pathway with lidocaine causes rapid, reversible decrease of PERG amplitude and increase in PERG latency, implying that intact retrograde signaling is necessary for the normal electrical responsiveness of retinal ganglion cells.
Introduction
Optic nerve diseases, such as glaucoma, optic neuritis, and Leber's hereditary optic neuropathy (LHON), are a family of disorders whose final common pathway is retinal ganglion cell (RGC) degeneration resulting in blindness. Increasing evidence in animal models of glaucoma and optic nerve diseases shows that RGC death is preceded by a stage of optic neuropathy that includes impairment of axon transport.1–8 In experimental models of glaucoma and optic nerve disease, RGC death also has been shown to be preceded by loss of RGC electrical responsiveness that can be measured either at single cell level9 or noninvasively over time with the pattern electroretinogram (PERG).10–14 Importantly, PERG abnormalities in human and mouse glaucoma models may be improved after IOP reduction,15–20 suggesting that loss of PERG signal preceding death is reversible.
Thus, there is interest in investigating the factors that alter RGC electrical responsiveness to design therapeutic strategies to restore impaired function and prolong cell survival. Here, we investigated the role of retrograde signaling on RGC responsiveness in the mouse. We showed that lidocaine injected into the eye orbit or within the superior colliculus (SC) causes reversible reduction of PERG signal. Retrobulbar optic nerve crush causes rapid, irreversible loss of PERG signal that precedes RGC death. Altogether, results suggested that intact retrograde signaling is necessary for normal RGC responsiveness. Preliminary results of our study have been reported previously in abstract form (Chou TH, et al. IOVS 2012;53:ARVO E-Abstract 1956).
Materials and Methods
Animals and Husbandry
Our study was approved by the Animal Care and Use Committee at University of Miami. All experiments were conducted according to the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research. C57BL/6J mice (B6) purchased from the Jackson Laboratory (Bar Harbor, ME) were kept in our AAALAC-certified vivarium, using standard 12:12-hour light-dark cycle and fed with Grain Based Diet (Lab Diet: 500, Opti-diet; PMI Nutrition International, Inc., Brentwood, MO). For the present study, 43 C7BL/6J mice of 3 to 4 months of age were used.
Interventional Procedures
Mice were weighed and anesthetized with intraperitoneal (IP) injections (0.5–0.7 mL/kg) of a mixture of ketamine 42.8 mg/mL and xylazine 8.6 mg/ml. Lidocaine was injected either retrobulbarly or at the level of the SC. Retrobulbar injections of lidocaine (2 μL, 40 μg/μL) were performed with a 23-gauge needle using a supraorbital approach. Care was taken that the procedure did not cause orbital hemorrhage. For intracollicular lidocaine injections, the head fur was shaved and the surgical site prepared with 10% povidone-iodine. An incision of the scalp was performed to expose the skull. A small hole was drilled 2.9 mm behind the bregma and 0.5 mm lateral to the midline of the right hemisphere by using a high-speed dental drill. Lidocaine (1 μL, 40 μg/μL) was injected slowly at a depth of 1.6 mm below the dura using a Hamilton syringe.
Optic nerve crush was performed as described previously.21,22 The left optic nerve was exposed intraorbitally after incision of the temporal conjunctiva followed by blunt dissection, and crushed with jeweler's forceps (Dumont #5; Roboz Surgical Instrument Co., Inc., Gaithersburg, MD) for 5 seconds approximately 1 to 1.5 mm behind the optic disc. To preserve the retinal blood supply, care was taken not to damage the underlying ophthalmic artery. After the surgical procedure, mice received a subcutaneous injection of buprenorphine (0.05 mg/kg; Bedford Laboratories, Bedford, OH) as postoperative analgesic. Eye ointment containing atropine sulfate was applied preoperatively to protect the cornea during surgery.
PERG Recording
A detailed description of the PERG technique has been reported previously.19,23,24 In brief, mice were weighed and anesthetized with intraperitoneal injections (0.5–0.7 mL/kg) of a mixture of ketamine 42.8 mg/mL and xylazine 8.6 mg/ml. Mice then were restrained gently in a custom-made holder that allowed unobstructed vision. The body of the animal was kept at a constant body temperature of 37.0°C using a feedback-controlled heating pad (TCAT-2LV; Physitemp Instruments, Inc., Clifton, NJ). The eyes of anesthetized mice typically were wide open and in a stable position, with optical axes pointing laterally and upwardly.25,26
A PERG electrode (0.25 mm diameter silver wire configured to a semicircular loop of 2 mm radius) was placed on the extrapupillary corneal surface by means of a micromanipulator. A small drop of balanced saline was applied topically every 30 minutes to prevent corneal dryness. Reference and ground electrodes were stainless steel needles inserted under the skin of the posterior scalp along the midline and of the tail, respectively.
Visual stimuli consisted of contrast-reversing (2 reversals/s) horizontal bars (0.05 cycles/deg, 100% contrast, mean luminance 50 cd/m2) generated by a programmable graphic card (VSG; Cambridge Research Systems, Rochester, UK) on a CRT display (Sony Multiscan 500; Sony, New York, NY) whose center was aligned with the projection of the pupil. The pupils were not dilated, and eyes were not refracted for the viewing distance, since the mouse eye has a large depth of focus.27–29 At the viewing distance of 15 cm, the stimulus field covered an area of 69.4 × 63.4 degrees. Three consecutive PERG responses to 600 contrast reversals each were recorded. The responses were superimposed to check for consistency and then averaged (1800 sweeps). The PERG waveform consisted of a major positive peak at around 80 ms to 120 ms (defined as P100) followed by a slower negative wave with a broad trough at around 200 ms to 300 ms (defined as N250).23 The PERG amplitude was the sum of the P100 and N250 amplitudes. The PERG latency was the time to the P100 peak. Representative examples are shown in Figure 1.
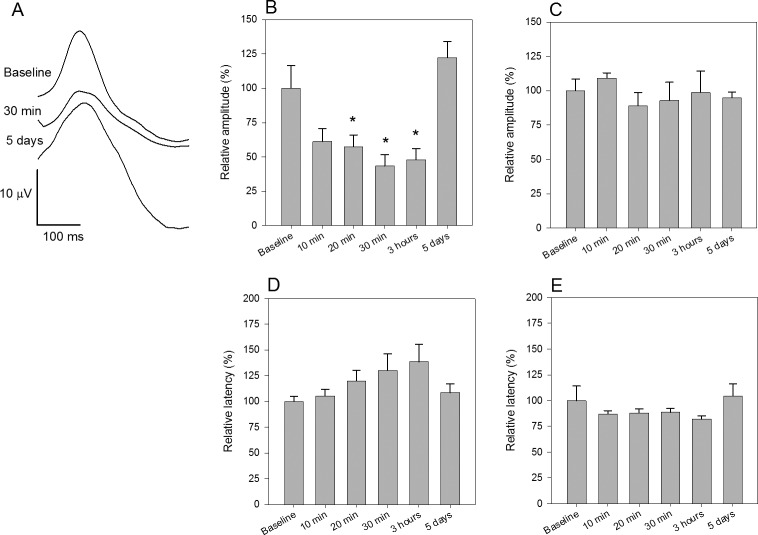
Figure 1. .
Effect of retrobulbar lidocaine injection on PERG. (A) Representative examples of PERG waveforms recorded before, and 30 minutes and 5 days after injection. (B) Mean PERG amplitude (B) and latency (D) before and at different times after injection. (C, E) Mean PERG amplitude (C) and latency (E) before and after retrobulbar saline injection. All data were normalized to mean baseline values ([B] 28.4 μV, SEM 2.7; [D] 94.0 ms, SEM 4.6, n = 9; [C] 26.3 μV, SEM 2.1; [E] 92.5 ms, SEM 10.5, n = 5). Errors bars represent the SEM. Significance (P < 0.05) of the effect compared to baseline is represented by asterisks above bars.
Protocol
After recording a baseline PERG, lidocaine was injected either behind the globe (retrobulbar) or within the SC (intracollicular), and PERG recorded at the first available postinterventional opportunity (approximately 10 minutes for retrobulbar lidocaine and within 1 hour for intracollicular lidocaine), and at different times during the same day and in subsequent days. After recording a baseline PERG, the optic nerve of one side was crushed and the PERG then was recorded at the first available postinterventional opportunity (10–20 minutes after surgery), and at different times during the same day and in subsequent days. One month after optic nerve crush, mice were euthanized, and retinas and optic nerves harvested for RGC immunohistochemistry.
Immunohistochemistry for RGC Counts
Whole mount retinal staining and RGC counting were performed as described previously.21 Antibodies were diluted in blocking solution consisting of 5% normal goat serum (NGS) and 0.3% Triton X-100 in PBS. Retinas were blocked for 1 hour at room temperature, and incubated with primary antibody, mouse neuronal class β-III tubulin (clone TUJ1, 1:400 dilution; Covance, Princeton, NJ) overnight at 4°C, and washed three times for 10 minutes each with PBS. Secondary antibody then was applied (1:200; Jackson Laboratory) and incubated for 1 hour at room temperature. Retinas were washed again three times for 10 minutes each with PBS before a cover slip was attached with Fluoromount-G (Southern Biotech, Birmingham, AL). For RGC counting, 9 to 12 fields of the whole mount retinas immunostained with TUJ1 antibody were sampled randomly at approximately 0.5, 1, and 1.5 mm from the center of the optic nerve in each retinal quadrant under a fluorescence microscope. Quantification of TUJ1-positive RGCs is represented as percentage of TUJ1-positive RGCs compared to the uninjured contralateral retinas. In previous studies of our group (e.g., Park et al.21) as well as of others,30,31 it has been shown that TUJ1-positive cells overlap completely with retrogradely transported FluoroGold-positive cells, but did not overlap with ChAT-positive amacrine cells. Thus, TUJ1 immunoreactivity could be used to estimate the total number of surviving RGCs.
Controls
As a control of nonspecific effects of lidocaine injections, the PERG was recorded before and after injections of PBS either retrobulbar or intracollicular, using identical volume and procedures. As a control for nonspecific effects of optic nerve crush, the optic nerve was exposed as described above, but not crushed. As a control for generalized effect of lidocaine/optic nerve crush to outer retinal neurons, a photopic ERG (FERG) was recorded in response to diffuse bright flashes on a rod-saturating background as described previously.23 The FERG was recorded before and after lidocaine/optic nerve crush, at post-treatment times when the PERG had the lowest amplitude compared to baseline. The FERG waveform consisted of a major positive b-wave peaking at approximately 50 ms followed by a slower negative wave also known as photopic negative response (PhNR).23,32 The FERG amplitude was measured from the peak of the b-wave to the trough of the PhNR (see examples in Fig. 4). As a control for postsynaptic effects of retrobulbar lidocaine, flash-evoked VEPs (FVEPs) were recorded in response to diffuse light flashes similarly to the FERG. FVEPs were recorded from stainless steel screws (shaft length 2.4 mm, shaft diameter 1.57 mm; PlasticsOne, Roanoke, VA) inserted chronically into the skull contralateral to the stimulated eye 2 mm lateral to the lambda suture, which corresponds to the monocular visual cortex33,34 (see examples in Fig. 4).
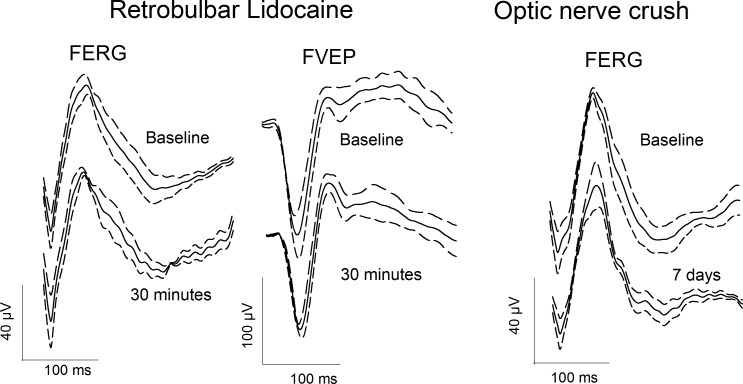
Figure 4. .
Lack of effect of retrobulbar lidocaine and optic nerve crush on FERG and FVEP. Left: Grand average FERG and FVEP waveforms (continuous lines) and superimposed ± SEMs (dashed lines) recorded before and 30 minutes after retrobulbar injection of 2 μL of lidocaine 40 mg/mL. FERGs were recorded from the eye ipsilateral to the injected side. FVEPs were recorded from the monocular visual cortex contralateral to the stimulated eye. Right: Grand average FERG waveforms (continuous lines) and superimposed ± SEMs (dashed lines) recorded before and 7 days after crush of the ipsilateral optic nerve performed 1.5 mm behind the eye.
Statistics
In all experiments, posttreatment PERG changes were expressed as percentage variation compared to the mean baseline value, and analyzed with ANOVA followed by post hoc Dunnett tests. A P value of <0.05 was considered significant.
Results
Retrobulbar Lidocaine
The effect of retrobulbar lidocaine injection on the PERG is summarized in Figure 1. The PERG amplitude tended to decrease (Fig. 1A), while the PERG latency tended to increase (Fig. 1C), already 10 minutes after injection and reached a minimum at around 30 minutes to 1 hour. The PERG amplitude recovered to baseline values within the next 5 days after injection. The effect of retrobulbar lidocaine on PERG amplitude was significant (ANOVA P < 0.001, post hoc comparisons versus baseline group [Dunnett] revealed significant [P < 0.05] changes at 20 and 30 minutes, and 1 hour). PERG latency tended to increase after retrobulbar lidocaine, but the effect was not significant (ANOVA P = 0.14). As shown in Figures 1B and 1D, retrobulbar injection of saline had no effect on PERG amplitude and latency.
Intracollicular Lidocaine
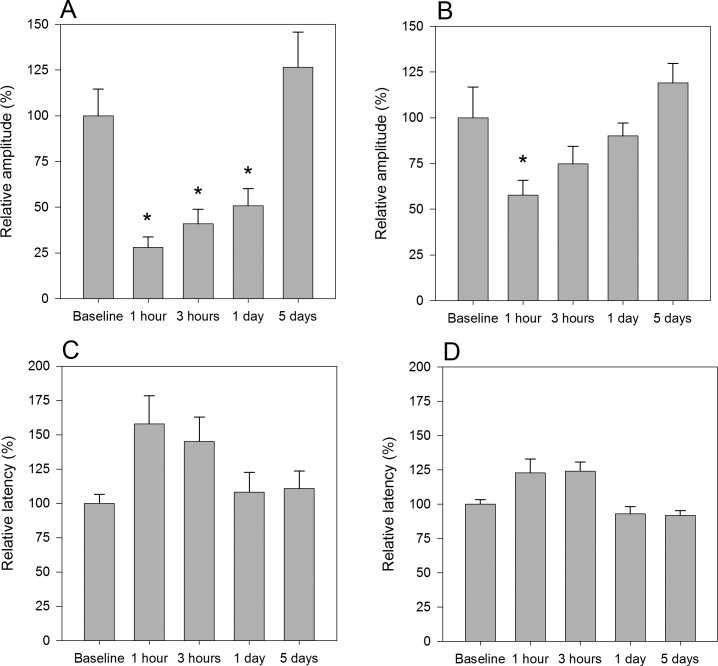
The effect of intracollicular lidocaine injection on the PERG is summarized in Figure 2. The PERG amplitude decreased (Fig. 2A) 1 hour after injection and then progressively tended to a recovery, which was complete within the next 5 days. The effect of intracollicular lidocaine on PERG amplitude was significant (ANOVA P < 0.001, post hoc comparisons versus baseline [Dunnett] revealed significant [P < 0.05] changes at 20 and 30 minutes, and 1 hour). PERG latency tended to increase, but the effect was not significant (ANOVA P = 0.053, Fig. 2C). Intracollicular injection of saline (Fig. 2B) had a smaller effect on PERG amplitude (ANOVA P = 0.009), which was significant (P < 0.05) at 20 minutes only.
Figure 2. .
Effect of intracollicular lidocaine injection on PERG. (A) Mean PERG amplitude recorded before and at different times after intracollicular lidocaine injection. (C) Mean PERG latency before and after lidocaine injection. (B, D) Control experiments with intracollicular saline injection. All data were normalized to mean baseline values ([A] 26.1 μV, SEM 3.8; [C] 83.0 ms, SEM 5.4, n = 5; [B] 25.3 μV, SEM 4.1; [D] 92.5 ms, SEM 2.9). Errors bars represent the SEM. Significance (P < 0.05) of the effect compared to baseline is represented by asterisks above bars.
Optic Nerve Crush
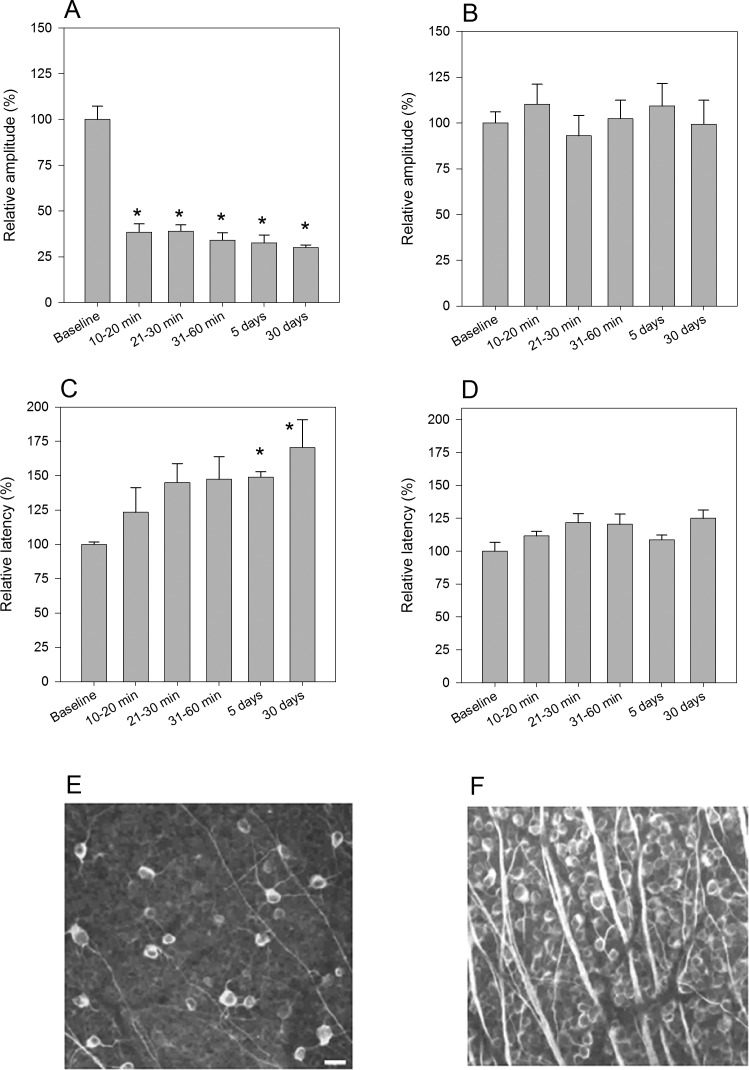
Intraorbital optic nerve crush resulted in much reduced PERG amplitude already 10 to 20 minutes after surgery, which remained approximately at the same reduced level over 1 month observation (Fig. 3A).The effect was significant (ANOVA P < 0.001, post hoc t-tests P < 0.001 for all postsurgical points compared to baseline). One month after optic nerve crush, retinas were harvested, and TUJ1-positive RGCs counted (Fig. 3E) and compared to RGC counts in noninjured retinas (Fig. 3F). TUJ1-positive RGC survival in mice that received optic nerve crush was on average 12% (SEM 1.4). Optic nerve crush also resulted in a progressive increase of PERG latency (Fig. 3C, ANOVA P = 0.033). Post hoc test showed significant (P < 0.05) increase compared to baseline at 5 days and 1 month after surgery. Sham surgery did not result in significant changes of PERG amplitude (Fig. 3B) and latency (Fig. 3D).
Figure 3. .
Effect of optic nerve crush on PERG and RGC death. (A, C) Mean PERG amplitude (A) and latency (C) before and at different times after optic nerve crush 1.5 mm behind the globe. (B, D) Mean PERG amplitude (B) and latency (D) in control mice that received sham surgery. All data were normalized to mean baseline values ([A] 21.7 μV, SEM 2.4; [C] 83.6 ms, SEM 1.1; [B] 18.3 μV, SEM 1.8; [D] 81.3, SEM 2.4). Errors bars represent the SEM (n = 5). Significance (P < 0.05) of the effect compared to baseline is represented by asterisks above bars. (E, F) Representative examples of TUJ1-positive RGC in mice that received optic nerve crush 1 month before (E) and in control, sham injured mice (F). RGC survival in mice that received optic nerve crush was 12% (SEM 1.4). Scale bar: 10 μm.
Control FERG and Photopic Visual Evoked Potential (FVEP)
The FERG was recorded before retrobulbar lidocaine/optic nerve crush and at post treatment times at which the PERG had the lowest amplitude compared to baseline. Individual FERG waveforms were averaged and displayed in Figure 4 as grand-average ± SEM. For retrobulbar lidocaine and optic nerve crush, pre- and post treatment FERGs had virtually identical grand-average waveform. Figure 4 also shows that the FVEP had very similar waveform recorded before and after retrobulbar lidocaine injection.
Discussion
Axon transport defects are a common theme in neurodegenerative diseases,35 including glaucoma,3,5,36,37 and may have a role in the pathogenesis of RGC death.8,38 Little is known on the relationship between reduced axon transport and RGC function.39 Here, we addressed this problem by recording the PERG—a signal that depends on the physiologic integrity of RGC—before and after manipulations at postretinal level that impair retrograde signaling in the retinocollicular pathway. Lidocaine is a well established method to block axon transport40–42 without damaging optic nerve structures,43 and acts at very low concentrations.44 At sufficient concentrations, lidocaine also is known to alter signal conduction by blocking voltage-gated sodium channels in the neuronal cell membrane,45 thereby suppressing postsynaptic activity. As FVEPs were not altered significantly after retrobulbar lidocaine, our results indicated that the action of lidocaine on sodium channels was insufficient to impair signal conduction along the optic nerve. Insufficient blockage of sodium channels also suggests that a direct action of lidocaine on action potentials of RGCs is unlikely. It also is unlikely that lidocaine entered the retina via the cardiovascular system and impaired directly RGC spiking activity, as in this case the concentration of lidocaine at the retina would have been minimal. Finally, it is unlikely that optic nerve crush caused ischemic damage to the retina, as shown in previous studies.21,22 For lidocaine injection and optic nerve crush, the FERG—a signal originating in the outer retina—was unaltered. This suggested that the effects of all manipulations did not cause generalized retinal dysfunction.
Altogether, as the effects of all postretinal manipulations on PERG were qualitatively similar and major unspecific effects on RGC could be ruled out, the results strongly suggested that PERG changes were linked to altered supply of retrogradely-delivered material via axon transport. Reversible blockade of axon transport was not expected to cause damage to RGC,43,46 whereas for optic nerve crush RGC loss was expected to start approximately 5 days after surgery.21,47 However, the effects of the optic nerve crush could include an acute physiologic effect on RGC signaling48 that added to the effect mediated by impairment of retrograde signaling.
The main result of our study is that lidocaine injections caused rapid, reversible reduction of PERG signal to at least 50% of its baseline value. PERG effects after intracollicular lidocaine injection could be measured within 1 hour after treatment, and recovered progressively over 4 days. After retrobulbar lidocaine injection, PERG effects could be measured as early as 10 to 20 minutes posttreatment, reached a maximum at 30 minutes, and recovered within 5 days. The effects of retrobulbar optic nerve crush on PERG also could be measured as early 10 to 20 minutes after surgery, and remained stable at reduced level over 1-month follow-up, after which histology demonstrated a drastic (88%) decrease of TUJ1-positive RGC counts in the retina. That the earliest effects on PERG of retrobulbar lidocaine were rather similar in magnitude and time course to those obtained with retrobulbar optic nerve crush suggested that the latter also were mediated largely by impairment of retrograde axon transport rather that direct injury to RGC.48 Dramatic losses of PERG signal after either optic nerve section49 or crush32 in the mouse have been reported before, but these studies were not designed to monitor early postsurgical events.
Our study provided only a reasonable approximation of the time course of the PERG effects, as there were constraints due the time needed for the experimental procedures. For retrobulbar injection and optic nerve crush, the earliest opportunity to record a postprocedural PERG was approximately 10 minutes. For intracollicular injections, the earliest opportunity was 1 hour later. Thus, we cannot exclude that the PERG effects could have manifested somewhat earlier compared to the values we were able to measure. If we assume 10 to 15 minutes postprocedural delay for proximal interventions (retrobulbar lidocaine, optic nerve crush) and 60 minutes delay for distal intervention (intracollicular lidocaine); if we also assume that the delay was due to the speed of retrograde axon transport, and the retinocollicular distance would be approximately 11 mm,50 then the corresponding velocities of axon transport would be approximately 0.12 mm/min (1.5 mm distance/12.5 min) and 0.18 mm/min (11 mm distance/60 min). These calculated velocities are well in the range of those reported for fast retrograde transport in a number of studies.1,51 It should be taken into account that the mouse optic nerve has an unmyelinated portion of 0.6 to 0.8 mm immediately adjacent to the sclera.52 This might have represented a vulnerable location that drove the earliest effect of retrobulbar lidocaine.
What is the retrograde signal(s) whose reduced supply caused reduced electric responsiveness of RGC? Our study does not provide direct answers to this important question, which will be addressed in a subsequent study. A reasonable hypothesis is that target-derived brain derived neurotrophic factor (BDNF) may represent a likely molecular candidate. Available evidence shows that intraocular pressure elevation in an experimental glaucoma model causes obstructed axon transport of BDNF and its receptor, TrkB, eventually leading to RGC death.38 BDNF has been shown to depolarize neurons just as rapidly as the neurotransmitter glutamate, even at very low concentrations.53–55 Rapid actions of neurotrophins include changes in neuronal excitability, synaptic transmission, and neural plasticity. Of interest, intracollicular injection of saline also temporarily reduced the PERG signal, although to a smaller/shorter extent compared to intracollicular lidocaine injection. It is possible that intracollicular injection of 1 μL saline mechanically caused temporary impairment of the target-derived supply of retrogradely-transported material that sustains RGC responsiveness. RGC responsiveness also may be sustained in part by other postsynaptic targets, such as the dorsal geniculate nucleus and the suprachiasmatic nucleus.
In conclusion, our results showed that impairment of retrograde signaling causes rapid, substantial decrease of PERG amplitude and increase in PERG latency that may be reversible. Results implied that intact retrograde signaling is necessary for the normal electrical responsiveness of retinal ganglion cells. Numerous reports of early PERG impairment in glaucoma,56,57 optic nerve diseases,58 and diabetes59,60 at least in part may be due to altered axon transport. Also, recovery of PERG amplitude losses after either IOP lowering15,17,18,61,62 or removal of pituitary tumors63 may be related to restoration of axon transport. Thus, the PERG may represent a promising marker of early, reversible axonal dysfunction preceding RGC death in glaucoma and optic nerve diseases.64
Footnotes
Supported by National Institutes of Health (NIH)–National Eye Institute RO1 EY019077 (VP), NIH Center Grant P30-EY014801 (VP), Ziegler Foundation (KKP), Kirchgessner Foundation (KKP), and an unrestricted grant to Bascom Palmer Eye Institute from Research to Prevent Blindness, Inc.
Disclosure: T.-H. Chou, None; K.K. Park, None; X. Luo, None; V. Porciatti, None
References
- 1. Morgan JE. Circulation and axonal transport in the optic nerve. Eye (Lond). 2004; 18: 1089–1095 [DOI] [PubMed] [Google Scholar]
- 2. Whitmore AV, Libby RT, John SW. Glaucoma: thinking in new ways-a role for autonomous axonal self-destruction and other compartmentalised processes? Prog Retin Eye Res. 2005; 24: 639–662 [DOI] [PubMed] [Google Scholar]
- 3. Buckingham BP, Inman DM, Lambert W, et al. Progressive ganglion cell degeneration precedes neuronal loss in a mouse model of glaucoma. J Neurosci. 2008; 28: 2735–2744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Soto I, Oglesby E, Buckingham BP, et al. Retinal ganglion cells downregulate gene expression and lose their axons within the optic nerve head in a mouse glaucoma model. J Neurosci. 2008; 28: 548–561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Crish SD, Sappington RM, Inman DM, Horner PJ, Calkins DJ. Distal axonopathy with structural persistence in glaucomatous neurodegeneration. Proc Natl Acad Sci. 2010; 107: 5196–5201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carelli V, Ross-Cisneros FN, Sadun AA. Optic nerve degeneration and mitochondrial dysfunction: genetic and acquired optic neuropathies. Neurochem Int. 2002; 40: 573–584 [DOI] [PubMed] [Google Scholar]
- 7. Chidlow G, Ebneter A, Wood JP, Casson RJ. The optic nerve head is the site of axonal transport disruption, axonal cytoskeleton damage and putative axonal regeneration failure in a rat model of glaucoma. Acta Neuropathol. 2011; 121: 737–751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vidal-Sanz M, Salinas-Navarro M, Nadal-Nicolas FM, et al. Understanding glaucomatous damage: anatomical and functional data from ocular hypertensive rodent retinas. Prog Retin Eye Res. 2012; 31: 1–27 [DOI] [PubMed] [Google Scholar]
- 9. Weber AJ, Harman CD. Structure-function relations of parasol cells in the normal and glaucomatous primate retina. Invest Ophthalmol Vis Sci. 2005; 46: 3197–3207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Saleh M, Nagaraju M, Porciatti V. Longitudinal evaluation of retinal ganglion cell function and IOP in the DBA/2J mouse model of glaucoma. Invest Ophthalmol Vis Sci. 2007; 48: 4564–4572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Howell GR, Libby RT, Marchant JK, et al. Absence of glaucoma in DBA/2J mice homozygous for wild-type versions of Gpnmb and Tyrp1. BMC Genet. 2007; 8: 45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Enriquez-Algeciras M, Ding D, Chou TH, et al. Evaluation of a transgenic mice model of multiple sclerosis with non invasive methods. Invest Ophthalmol Vis Sci. 2011; 52: 2405–2411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Howell GR, Soto I, Zhu X, et al. Radiation treatment inhibits monocyte entry into the optic nerve head and prevents neuronal damage in a mouse model of glaucoma. J Clin Invest. 2012; 122: 1246–1261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yu H, Koilkonda RD, Chou TH, et al. Gene delivery to mitochondria by targeting modified adenoassociated virus suppresses Leber's hereditary optic neuropathy in a mouse model. Proc Natl Acad Sci U S A. 2012; 109: E1238–E1247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ventura LM, Porciatti V. Restoration of retinal ganglion cell function in early glaucoma after intraocular pressure reduction: a pilot study. Ophthalmology. 2005; 112: 20–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ventura LM, Golubev I, Feuer WJ, Porciatti V. Pattern electroretinogram progression in glaucoma suspects [ published online ahead of print November 7, 2011]. J Glaucoma. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sehi M, Grewal DS, Goodkin ML, Greenfield DS. Reversal of retinal ganglion cell dysfunction after surgical reduction of intraocular pressure. Ophthalmology. 2010; 117: 2329–2336 [DOI] [PubMed] [Google Scholar]
- 18. Nagaraju M, Saleh M, Porciatti V. IOP-dependent retinal ganglion cell dysfunction in glaucomatous DBA/2J mice. Invest Ophthalmol Vis Sci. 2007; 48: 4573–4579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Porciatti V, Nagaraju M. Head-up tilt lowers IOP and improves RGC dysfunction in glaucomatous DBA/2J mice. Exp Eye Res. 2010; 90: 452–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ventura LM, Feuer WJ, Porciatti V. Progressive loss of retinal ganglion cell function is hindered with IOP-lowering treatment in early glaucoma. Invest Ophthalmol Vis Sci. 2012; 53: 659–663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Park KK, Liu K, Hu Y, et al. Promoting axon regeneration in the adult CNS by modulation of the PTEN/mTOR pathway. Science. 2008; 322: 963–966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Templeton JP, Geisert EE. A practical approach to optic nerve crush in the mouse. Mol Vis. 2012; 18: 2147–2152 [PMC free article] [PubMed] [Google Scholar]
- 23. Porciatti V, Saleh M, Nagaraju M. The pattern electroretinogram as a tool to monitor progressive retinal ganglion cell dysfunction in the DBA/2J mouse model of glaucoma. Invest Ophthalmol Vis Sci. 2007; 48: 745–751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Porciatti V. The mouse pattern electroretinogram. Doc Ophthalmol. 2007; 115: 145–153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Drager UC, Hubel DH. Physiology of visual cells in mouse superior colliculus and correlation with somatosensory and auditory input. Nature. 1975; 253: 203–204 [DOI] [PubMed] [Google Scholar]
- 26. Oommen BS, Stahl JS. Eye orientation during static tilts and its relationship to spontaneous head pitch in the laboratory mouse. Brain Res. 2008; 1193: 57–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Remtulla S, Hallett PE. A schematic eye for the mouse, and comparisons with the rat. Vision Res. 1985; 25: 21–31 [DOI] [PubMed] [Google Scholar]
- 28. Schmucker C, Schaeffel F. A paraxial schematic eye model for the growing C57BL/6 mouse. Vision Res. 2004; 44: 1857–1867 [DOI] [PubMed] [Google Scholar]
- 29. Artal P, Herreros de Tejada P, Munoz Tedo C, Green DG. Retinal image quality in the rodent eye. Vis Neurosci. 1998; 15: 597–605 [DOI] [PubMed] [Google Scholar]
- 30. Robinson GA, Madison RD. Axotomized mouse retinal ganglion cells containing melanopsin show enhanced survival, but not enhanced axon regrowth into a peripheral nerve graft. Vision Res. 2004; 44: 2667–2674 [DOI] [PubMed] [Google Scholar]
- 31. Brown NL, Patel S, Brzezinski J, Glaser T. Math5 is required for retinal ganglion cell and optic nerve formation. Development. 2001; 128: 2497–2508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Miura G, Wang MH, Ivers KM, Frishman LJ. Retinal pathway origins of the pattern ERG of the mouse. Exp Eye Res. 2009; 89: 49–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Porciatti V, Pizzorusso T, Maffei L. The visual physiology of the wild type mouse determined with pattern VEPs. Vision Res. 1999; 39: 3071–3081 [DOI] [PubMed] [Google Scholar]
- 34. Rossi FM, Pizzorusso T, Porciatti V, Marubio LM, Maffei L, Changeux JP. Requirement of the nicotinic acetylcholine receptor beta 2 subunit for the anatomical and functional development of the visual system. Proc Natl Acad Sci U S A. 2001; 98: 6453–6458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Roy S, Zhang B, Lee VM, Trojanowski JQ. Axonal transport defects: a common theme in neurodegenerative diseases. Acta Neuropathol. 2005; 109: 5–13 [DOI] [PubMed] [Google Scholar]
- 36. Almasieh M, Wilson AM, Morquette B, Cueva Vargas JL, Di Polo A. The molecular basis of retinal ganglion cell death in glaucoma. Prog Retin Eye Res. 2012; 31: 152–181 [DOI] [PubMed] [Google Scholar]
- 37. Salinas-Navarro M, Mayor-Torroglosa S, Jimenez-Lopez M, et al. A computerized analysis of the entire retinal ganglion cell population and its spatial distribution in adult rats. Vision Res. 2009; 49: 115–126 [DOI] [PubMed] [Google Scholar]
- 38. Pease ME, McKinnon SJ, Quigley HA, Kerrigan-Baumrind LA, Zack DJ. Obstructed axonal transport of BDNF and its receptor TrkB in experimental glaucoma. Invest Ophthalmol Vis Sci. 2000; 41: 764–774 [PubMed] [Google Scholar]
- 39. Weber AJ, Harman CD, Viswanathan S. Effects of optic nerve injury, glaucoma, and neuroprotection on the survival, structure, and function of ganglion cells in the mammalian retina. J Physiol. 2008; 586: 4393–4400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Byers MR, Fink BR, Kennedy RD, Middaugh ME, Hendrickson AE. Effects of lidocaine on axonal morphology, microtubules, and rapid transport in rabbit vagus nerve in vitro. J Neurobiol. 1973; 4: 125–143 [DOI] [PubMed] [Google Scholar]
- 41. Bisby MA. Inhibition of axonal transport in nerves chronically treated with local anesthetics. Exp Neurol. 1975; 47: 481–489 [DOI] [PubMed] [Google Scholar]
- 42. Fink BR, Kish SJ. Reversible inhibition of rapid axonal transport in vivo by lidocaine hydrochloride. Anesthesiology. 1976; 44: 139–146 [DOI] [PubMed] [Google Scholar]
- 43. Fagiolini M, Caleo M, Strettoi E, Maffei L. Axonal transport blockade in the neonatal rat optic nerve induces limited retinal ganglion cell death. J Neurosci. 1997; 17: 7045–7052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kanai A, Hiruma H, Katakura T, Sase S, Kawakami T, Hoka S. Low-concentration lidocaine rapidly inhibits axonal transport in cultured mouse dorsal root ganglion neurons. Anesthesiology. 2001; 95: 675–680 [DOI] [PubMed] [Google Scholar]
- 45. Catterall WA. Molecular mechanisms of gating and drug block of sodium channels. Novartis Found Symp. 2002; 241: 206–218, discussion 218–232 [PubMed] [Google Scholar]
- 46. Wang X, Baldridge WH, Chauhan BC. Acute endothelin-1 application induces reversible fast axonal transport blockade in adult rat optic nerve. Invest Opht Vis Sci. 2008; 49: 961–967 [DOI] [PubMed] [Google Scholar]
- 47. Bien A, Seidenbecher CI, Bockers TM, Sabel BA, Kreutz MR. Apoptotic versus necrotic characteristics of retinal ganglion cell death after partial optic nerve injury. J Neurotrauma. 1999; 16: 153–163 [DOI] [PubMed] [Google Scholar]
- 48. Mandolesi G, Madeddu F, Bozzi Y, Maffei L, Ratto GM. Acute physiological response of mammalian central neurons to axotomy: ionic regulation and electrical activity. FASEB J. 2004; 18: 1934–1936 [DOI] [PubMed] [Google Scholar]
- 49. Porciatti V, Pizzorusso T, Cenni MC, Maffei L. The visual response of retinal ganglion cells is not altered by optic nerve transection in transgenic mice overexpressing Bcl-2. Proc Natl Acad Sci U S A. 1996; 93: 14955–14959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chan KC, Li J, Kau P, et al. In vivo retinotopic mapping of superior colliculus using manganese-enhanced magnetic resonance imaging. Neuroimage. 2011; 54: 389–395 [DOI] [PubMed] [Google Scholar]
- 51. Caleo M. Different rates of horseradish peroxidase transport in the optic nerve of neonatal and adult rats. Neuroscience. 1996; 72: 725–730 [DOI] [PubMed] [Google Scholar]
- 52. May CA, Lutjen-Drecoll E. Morphology of the murine optic nerve. Invest Ophthalmol Vis Sci. 2002; 43: 2206–2212 [PubMed] [Google Scholar]
- 53. Kafitz KW, Rose CR, Konnerth A. Neurotrophin-evoked rapid excitation of central neurons. Prog Brain Res. 2000; 128: 243–249 [DOI] [PubMed] [Google Scholar]
- 54. Kafitz KW, Rose CR, Thoenen H, Konnerth A. Neurotrophin-evoked rapid excitation through TrkB receptors. Nature. 1999; 401: 918–921 [DOI] [PubMed] [Google Scholar]
- 55. Blum R, Kafitz KW, Konnerth A. Neurotrophin-evoked depolarization requires the sodium channel Na(V)1.9. Nature. 2002; 419: 687–693 [DOI] [PubMed] [Google Scholar]
- 56. Ventura LM, Porciatti V, Ishida K, Feuer WJ, Parrish RK 2nd. Pattern electroretinogram abnormality and glaucoma. Ophthalmology. 2005; 112: 10–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bach M, Hoffmann MB. Update on the pattern electroretinogram in glaucoma. Optom Vis Sci. 2008; 85: 386–395 [DOI] [PubMed] [Google Scholar]
- 58. Holder GE. Pattern electroretinography (PERG) and an integrated approach to visual pathway diagnosis. Prog Retin Eye Res. 2001; 20: 531–561 [DOI] [PubMed] [Google Scholar]
- 59. Di Leo MA, Falsini B, Caputo S, Ghirlanda G, Porciatti V, Greco AV. Spatial frequency-selective losses with pattern electroretinogram in type 1 (insulin-dependent) diabetic patients without retinopathy. Diabetologia. 1990; 33: 726–730 [DOI] [PubMed] [Google Scholar]
- 60. Ventura LM, Golubev I, Feuer WJ, Porciatti V. The PERG in diabetic glaucoma suspects with no evidence of retinopathy. J Glaucoma. 2009; 19: 243–247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Nesher R, Trick GL, Kass MA, Gordon MO. Steady-state pattern electroretinogram following long term unilateral administration of timolol to ocular hypertensive subjects. Doc Ophthalmol. 1990; 75: 101–109 [DOI] [PubMed] [Google Scholar]
- 62. Colotto A, Salgarello T, Giudiceandrea A, et al. Pattern electroretinogram in treated ocular hypertension: a cross-sectional study after timolol maleate therapy. Ophthalmic Res. 1995; 27: 168–177 [DOI] [PubMed] [Google Scholar]
- 63. Ventura LM, Venzara FX III, Porciatti V. Reversible dysfunction of retinal ganglion cells in non-secreting pituitary tumors. Doc Ophthalmol. 2009; 118: 155–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Porciatti V, Ventura LM. Retinal ganglion cell functional plasticity and optic neuropathy: a comprehensive model. J Neuroophthalmol. 2012; 32: 354–358 [DOI] [PMC free article] [PubMed] [Google Scholar]