Abstract
Coinciding with the increasing rates of cannabis abuse has been the recognition of a new clinical condition known as Cannabinoid Hyperemesis Syndrome. Cannabinoid Hyperemesis Syndrome is characterized by chronic cannabis use, cyclic episodes of nausea and vomiting, and frequent hot bathing. Cannabinoid Hyperemesis Syndrome occurs by an unknown mechanism. Despite the well-established anti-emetic properties of marijuana, there is increasing evidence of its paradoxical effects on the gastrointestinal tract and CNS. Tetrahydrocannabinol, cannabidiol, and cannabigerol are three cannabinoids found in the cannabis plant with opposing effects on the emesis response. The clinical course of Cannabinoid Hyperemesis Syndrome may be divided into three phases: prodromal, hyperemetic, and recovery phase. The hyperemetic phase usually ceases within 48 hours, and treatment involves supportive therapy with fluid resuscitation and anti-emetic medications. Patients often demonstrate the learned behavior of frequent hot bathing, which produces temporary cessation of nausea, vomiting, and abdominal pain. The broad differential diagnosis of nausea and vomiting often leads to delay in the diagnosis of Cannabinoid Hyperemesis Syndrome. Cyclic Vomiting Syndrome shares several similarities with CHS and the two conditions are often confused. Knowledge of the epidemiology, pathophysiology, and natural course of Cannabinoid Hyperemesis Syndrome is limited and requires further investigation.
Keywords: Cannabinoid Hyperemesis Syndrome, Cannabis, Marijuana, Nausea, Vomiting
Epidemiology and Introduction
Cannabis is the most commonly used illicit drug in the United States with over 16.7 million users in 2009 [1]. The 18–25 year old age group has the highest prevalence of marijuana use [1]. Each year 2.6 million Americans become new users. The majority of these individuals are less than nineteen years of age [2]. Similarly in Europe, cannabis use is prominent among young adults, with a prevalence that has increased from 5% in 1990 to 15% in 2005 [3]. While the overall prevalence of marijuana use has remained stable in the United States at 4%, the prevalence of cannabis use disorders (i.e. cannabis dependence, cannabis abuse) has continued to rise [4]. Risk factors for developing cannabis use disorders include male race, lower income, living in a Western culture, and being separated, divorced, or widowed [5].
Coinciding with the increasing rates of cannabis abuse has been the recognition of a new clinical condition known as Cannabinoid Hyperemesis Syndrome (CHS). The syndrome was first described in 2004 by Allen and colleagues and is characterized by chronic cannabis use, cyclic episodes of nausea and vomiting, and the learned behavior of hot bathing [6]. This review will provide an overview of cannabinoid pharmacology that focuses on the properties that may contribute to CHS. We review a clinical description of CHS and a proposed clinical evaluation including differential diagnosis and treatment modalities. We conclude with a discussion regarding the shortcomings in our knowledge and suggestions for areas of future research
Pharmacology of Cannabinoids
The Cannabinoid Receptors
Two distinct cannabinoid receptors, CB1 and CB2, have been identified in human and animal models. The CB1 and CB2 receptors function as G-protein coupled receptors that act by inhibiting adenylate cyclase [7]. In the brain, CB1 receptors are localized to the cerebral cortex, hypothalamus, anterior cingulate gyrus, hippocampus, cerebellum, and basal ganglia [8]. In the gastrointestinal system, CB1 receptors are found on both intrinsic and extrinsic neurons, with the enteric nervous system serving as the major site of action [9]. Other organs where CB1 receptors have been identified are the spleen, heart, liver, uterus, bladder, and vas deferens [10]. In comparison, much less is known about the effects of the CB2 receptor. CB2 receptors are expressed primarily by immune cells [11]. In the gastrointestinal system, CB2 receptors are expressed by lamina propria plasma cells and activated macrophages, as well as by the myenteric and submucosal plexus ganglia in human ileum [9,12,13]. CB2 receptors are likely involved in the inhibition of inflammation, visceral pain, and intestinal motility in the inflamed gut [9,14].
The Endogenous Cannabinoids (Endocannabinoids)
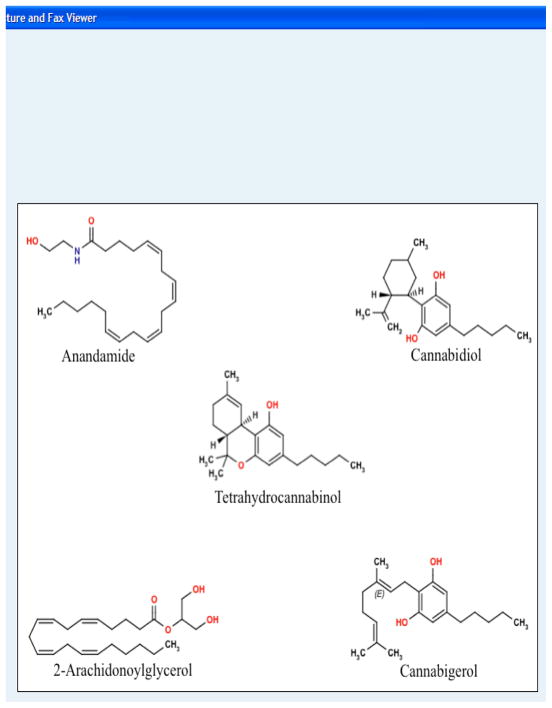
Along with the discovery of the CB1 and CB2 receptors has been the identification of endogenous arachidonic acid derivatives that bind to these receptors (Figure 1). These compounds are referred to as endogenous cannabinoids, or endocannabinoids. The best characterized endocannabinoids are anandamide and 2-arachidonylglycerol (2-AG) [9]. The endocannabinoids are present in both the central nervous system [8] and enteric nervous system [15]. Anandamide and 2-AG are released locally on demand by neurons, are present in small quantities, and undergo rapid inactivation [8]. Endocannabinoids are thought to act as either neuromodulators or neurotransmitters [11]. Anandamide and 2-AG possess similar biochemical structures, but each has a distinct pathway for biosynthesis and degradation. Anandamide is synthesized from the precursor N-arachidonoyl phosphatidylethanolamine, while 2-AG is produced from an inositol-1,2-diacylglycerol precursor [8,16,17]. The metabolism of anandamide is principally carried out via fatty acid amide hydrolase (FAAH), whereas the major enzyme metabolizing 2-AG is monoacylglycerol lipase (MAGL) [18].
Figure 1.
Two well-characterized naturally occurring endocannabinoids are anandamide and 2-arachidonoylglycerol. Cannabinoids discovered in the cannabis plant with known effects on the regulation of emesis include tetrahydrocannabinol, cannabidiol, and cannabigerol.
The Exogenous Cannabinoids
Δ9-tetrahydrocannabinol (THC) is the principle active compound in cannabis (Figure 1). The metabolism of THC occurs mainly in the liver via oxidation and hydroxylation reactions. In humans this is carried out largely by the CYP2C isoenzyme subfamily of the cytochrome P450 complex [19]. The true elimination plasma half-life of THC has been difficult to calculate, but several studies have estimated it to be in the range of 20–30 hours [20]. THC is excreted mainly as acid metabolites, with 60–85% cleared through the feces and 20–35% in the urine [20,21].
THC accumulates largely within body fat which serves as a long-term storage site for the drug [20,22]. This characteristic partially explains its prolonged elimination half-life. A large reservoir of stored THC in fat tissue may produce a “reintoxication effect” secondary to increased lipolysis during times of increased stress or food deprivation [23]. These characteristics of THC may have implications in Cannabinoid Hyperemesis Syndrome as these patients are chronic users of cannabis who likely have large lipid stores making them susceptible to increased cannabinoid levels in the plasma during times of stress.
Nearly 100 different metabolites have been identified for THC [24]. The two major metabolites found in humans are 11-hydroxy-Δ9-tetrahydrocannabinol (11-OH-THC) and 11-nor-9-carboxy-THC- Δ9-tetrahydrocannabinol (THC-COOH) [20]. 11-OH-COOH is a psychotropic metabolite that is equipotent to THC in terms of producing psychic effects and lowering intraocular pressure [25]. THC-COOH, in contrast, is a non-psychotropic metabolite that possesses anti-inflammatory and analgesic properties [26].
Cannabidiol (CBD) and cannabigerol (CBG) are two additional cannabinoids found in cannabis that appear to modulate the anti-emetic properties of THC. Cannabidiol, in contrast to THC, is non-psychotropic, has a low affinity for CB1 and CB2 receptors [27], and acts as a partial agonist at the 5-HT1A receptor [28]. CBD enhances the expression of CB1 receptors in the hypothalamus and amplifies the hypothermic effects caused by THC [29]. In animals the effect of CBD on toxin-induced vomiting displays a biphasic response with low doses producing an anti-emetic effect whereas higher doses enhance vomiting [30,31].
Cannabigerol (CBG) is a non-psychotropic cannabinoid that behaves as an antagonist at both the CB1 and 5-HT1A receptors [32]. This antagonism reverses the anti-emetic actions of low-dose CBD, which likely occurs at the 5-HT1A receptor [33]. The pro-emetic properties of CBD (at higher doses) and CBG may play a role in the severe nausea and vomiting observed in patients with Cannabinoid Hyperemesis Syndrome (Figure 2).
Figure 2.
The cannabinoids demonstrate opposing effects on the emesis response. A disruption in this balance causing the pro-emetic properties to overcome the anti-emetic effects may explain the paradox observed in cannabinoid hyperemesis syndrome. Abbreviations: CBD: cannabidiol, CBG: cannabigerol, THC: tetrahydrocannabinol.
The Effects of Cannabinoids in the Brain
Δ9-tetrahydrocannabinol (THC) has several well-established effects in the central nervous system, such as alteration of psychomotor behavior, impairment in short-term memory, stimulation of appetite, and analgesia [8]. Rimonabant, a CB1 antagonist, blocks the appetite stimulating qualities of the cannabinoids in the hypothalamus and has been marketed for the treatment of obesity and metabolic dysfunction [34]. THC exhibits an anti-emetic effect in the central nervous system. In animal models, CB1 receptor activation in the dorsal vagal complex of the brainstem mediates this effect [35,36]. Dronabinol (synthetic THC) and nabilone (a CB1 receptor agonist) are two commercially available cannabinoids for the treatment of chemotherapy-induced nausea and vomiting [37].
In the brain, the cannabinoid system helps regulate several aspects of the endocrine system. CB1 receptor activation in the hypothalamus and pituitary gland results in modulation of all hypothalamic-pituitary axes [38]. Receptor activation leads to inhibitory effects on the release of growth hormone, thyroid hormone, prolactin, and luteinizing hormone [38]. In animal studies mice lacking CB1 receptors demonstrate enhancement in circadian HPA axis activity peaks and impairment in glucocorticoid feedback [39].
The Effects of Cannabinoids in the Gastrointestinal System
The gastrointestinal actions of cannabinoids are mediated chiefly by CB1 receptors (Figure 2). Activation of CB1 receptors result in inhibition of gastric acid secretion, lower esophageal sphincter relaxation [40], altered intestinal motility [41,42], visceral pain, and inflammation [9,43]. CB1 receptor activation reduces gastric motility and results in delayed gastric emptying in rat models [44,45]. In humans, THC given at doses used to prevent chemotherapy-induced nausea and vomiting causes a significant delay in gastric emptying [46]. These findings in humans are further supported by a randomized, placebo-controlled trial with dronabinol that resulted in a significant delay in gastric emptying [47]. In comparison to other adverse effects associated with cannabinoids, delayed gastric emptying appears to be particularly resistant to the development of tolerance [48]. Additionally, intermittent administration of THC results in hypersensitization of the delayed gastric emptying effect [49]. THC’s effect on gastric motility is a paradox, as a delay in gastric emptying would be expected to promote nausea and vomiting [50]. However, nausea and vomiting traditionally do not occur with cannabis use, likely due to the anti-emetic properties of THC on the central nervous system.
Clinical Presentation, work up and differential diagnosis of Cannabinoid Hyperemesis Syndrome
Two case series and numerous individual case reports have been published on Cannabinoid Hyperemesis Syndrome (CHS) (Table 1). Patients present with recurrent episodes of nausea, vomiting, and dehydration with frequent visits to the emergency department. [6,51–62]. Patients are typically young adults with a long history of cannabis use. In nearly all cases there is a delay of several years in the onset of symptoms preceded by chronic marijuana abuse [6]. In one study the average duration of cannabis use prior to onset of recurrent vomiting was 16.3 ± 3.4 years [62]. There are at least four reported cases where the time lag was equal to or less than three years [54,59,60]. Daily marijuana use is characteristic and often reported as exceeding three to five times per day.
Table 1.
Epidemiology, clinical presentation and follow up of patients with Hyperemesis Cannabis Syndrome - Longitudinal case series and individual case reports
| Publication | Year | Country | n | Gender | Age Started (y) | Frequency (joints/day) | Age of presentation (y) | Illness duration (y) | Prodromal Illness | Abdominal Pain | Hot Bathing (No./day) | Weight Loss (Kg) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Allen J. Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis abuse | 2004 | Australia | 9 | - | 15.7 (12–19) | 88% (≥5–10) | 24.6 (14–44) | 4.7 (0.5–12) | 33% | - | 77% | 66% (≥10) |
| Soriano M. The Cannabis Hyperemesis Syndrome characterized by persistent nausea and vomiting, abdominal pain, and compulsive bathing associated with chronic marijuana use: A report of eight cases in the United States | 2010 | US | 8 | M (62.5%) | 13.3 (9–20) | 75% (≥3–10) | 34.1 (21–35) | 2.6 (1–8) | 100% | 100% | 100% (≥3–8) | 75% (≥10) |
| Patterson D. Cannabinoid Hyperemesis and compulsive bathing: A case series and paradoxical pathophysiological explanation | 2010 | US | 4 | M (100%) | 18.7 (15–27) | 75% (≥4)* | 25.5 (18–39) | 4.75 (8m–9) | - | 50%* | 50% | - |
| Donnino M. Cannabinoid Hyperemesis: A case series | 2009 | US | 3 | M (100%) | 33.5 (23–51)* | 66% (≥2–4) | 29.6 (20–49) | 2.3 (2–3) | - | Yes | Yes | - |
| Miller J. Pediatric Cannabinoid Hyperemesis | 2010 | US | 2 | M (50%) | 17.5 (17–18) | Daily | 16* | 2* | - | Yes* | Yes | - |
| Chang Y. Cannabinoid Hyperemesis relieved by compulsive bathing | 2009 | US | 2 | - | 16 (14–18) | Daily | 17 (14–20) | 8.5 (7–9) | - | Yes | Yes | - |
| Seraina M. Cannabinoid hyperemesis syndrome: an underreported entity causing nausea and vomiting of pregnancy | 2010 | Switzerland | 1 | F | 23 | Daily | 20 | 3 | - | - | Yes | - |
| Sannarangappa V. Cannabinoid hyperemesis | 2009 | Australia | 1 | M | 19 | 8 | 24 | 10 | - | - | Yes | - |
| Sontineni S. Cannabinoid hyperemesis syndrome: Clinical diagnosis of an underrecognised manifestation of chronic cannabis abuse | 2009 | US | 1 | M | 16 | Daily | 22 | 2 months | - | Yes | Yes | - |
| Watts M. Cannabinoid hyperemesis presenting to a New Zealand hospital | 2009 | New Zeeland | 1 | M | 18 | Daily | 29 | 3 | - | Yes | Yes | - |
| Budhraja V. Cannabinoid Hyperemesis Syndrome: Cyclic vomiting, chronic cannabis use, and compulsive bathing | 2008 | US | 1 | M | 16 | Daily | 18 | 8 months | - | Yes | Yes | - |
| Wallace D. Cannabinoid hyperemesis: marijuana puts patients in hot water | 2007 | Australia | 1 | M | 14 | ≥1g/1–2 day | 25 | 5 | - | Yes | Yes | - |
| Singh E. Cannabinoid Hyperemesis | 2006 | US | 1 | M | Childhood | 4 | 43 | 3 | - | Yes | Yes | ≥9 |
| Roche E. Cannabinoid hyperemesis: not just a problem in Adelaide Hills | 2005 | UK | 1 | - | - | - | - | 2 | - | - | Yes | - |
| Publication | Laboratory | UDS (+) | EGD | GES | Psychiatric Dx | Cannabis Cessation (length) | Resolution of Symptoms | Weight Gain (Kg) | Cannabis Resumption | Recurrence of symptoms |
|---|---|---|---|---|---|---|---|---|---|---|
| Allen J. et al 2004 | 44% (Leukocytosis) | 100% | 44% (gastritis) | 1 (delayed); 2 (normal); rest (N/A) | - | 77% (9–48 months) | Yes | 66% (≥5) | 55% | Yes |
| Soriano M. et al 2010 | 12.5% (Leukocytosis) | - | 75% (esophagitis) | 1 (normal) | 25% (depression, panic attacks) | 62.5% (N/A) | Yes (80%) | 80% (≥5) | 25% | Yes |
| Patterson D. et al 2010 | 25% (Hypokalemia) | 50% * | 75% (gastritis) | - | - | 100% (1m-1)° | Yes | - | 100% | Yes |
| Donnino M. et al 2009 | Hypokalemia | Yes | 1 (Normal)* | - | - | 66% (2–14 months) | Yes | - | - | - |
| Miller J. et al 2010 | Hypokalemia | Yes | Esophageal rings, gastritis | - | ADHD, depression | 1 month* | Yes | - | - | - |
| Chang Y, Windish D. 2009 | Leukocytosis | Yes | Normal | Delayed | Bipolar Disorder | - | - | - | - | - |
| Seraina M. et al 2010 | Normal | Yes | - | - | Psychogenic vomiting (?) | Yes° | Yes | - | - | - |
| Sannarangappa V, Tan C. 2009 | Leukocytosis, AKI | - | Normal | - | - | 2◆ | - | - | - | - |
| Sontineni S. et al 2009 | Normal | Yes | Esophagitis, Hiatal hernia | - | - | Yes° | Yes | - | - | - |
| Watts M. 2009 | Normal | - | Normal | - | - | - | - | - | - | - |
| Budhraja V. et al 2008 | Hypokalemia | Yes | Gastritis | - | - | 5 months | Yes | - | - | - |
| Wallace D. et al 2007 | Normal | - | Normal | - | Anxiety, depression, OCD | 2 | Yes | Yes | - | - |
| Singh E, Coyle W. 2006 | Normal | - | - | - | - | 4 months | Yes | - | - | - |
| Roche E, Foster P. 2005 | Neutrophilia | - | Esophagitis | - | - | 3 | Yes | - | - | - |
Rest not reported or not available
Period of time not specified
n Cases reported, OCD Obsessive Compulsive Disorder, Creat Creatinine, ADHD Attention deficit hyperactivity disorder
Rest not reported or not available
Period of time not specified
n Cases reported, OCD Obsessive Compulsive Disorder, AKI Acute Kidney Injury, ADHD Attention deficit hyperactivity disorder
CHS is a recurrent disorder interspersed with symptom-free intervals. It has been proposed to divide CHS into three phases: pre-emetic or prodromal, hyperemetic, and recovery phase [6,62]. The prodromal phase can last for months or years with patients developing early morning nausea, a fear of vomiting, and abdominal discomfort [62]. In this stage patients maintain normal eating patterns, and may increase or continue the use of cannabis because of the believed beneficial effects on relieving nausea [52,56]. The hyperemetic phase is characterized by paroxysms of intense and persistent nausea and vomiting, commonly described as overwhelming and incapacitating. Patients vomit profusely, often without warning and can vomit and retch up to five times per hour [62]. Most patients also present with diffuse but relatively mild abdominal pain. In one series approximately 70% of patients reported marked weight loss of at least 5 kg during their illness [6]. In the emergency department patients are found to be dehydrated but hemodynamically stable. They undergo an extensive diagnostic work up, including laboratory and imaging studies which, in the majority of cases, are unrevealing. During the hyperemetic phase patients stereotypically take numerous hot showers throughout the day. This idiosyncratic behavior appears to be learned and is repeatedly used as the only alleviating measure to control symptoms and rapidly becomes a compulsive behavior. The recovery phase can last for days, weeks, or months and is associated with relative wellness and normal eating patterns. Weight is regained and bathing returns to regular frequency.
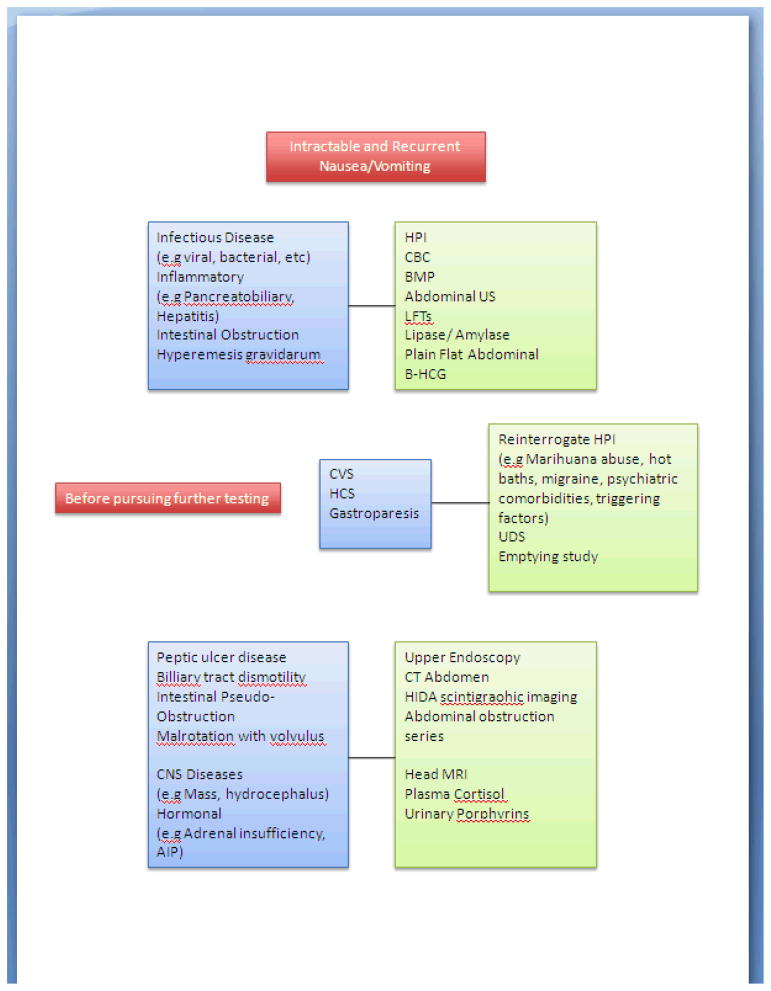
Patients with CHS usually remain misdiagnosed for a considerable time period. In one case series the average number of emergency room visits (7.1 ± 4.3) prior to diagnosis and the delay in diagnosis (for up to 9 years) was substantial [62]. Not surprisingly, the early identification of patients with CHS leads to a reduction in morbidity and costs [6]. The differential diagnosis of nausea and vomiting is extensive and includes a broad range of pathologic conditions affecting the gastrointestinal tract, the peritoneal cavity, CNS, as well as endocrine and metabolic functions [63]. The initial approach to evaluate a patient with cyclical vomiting should start by excluding these vast disorders. In this context a comprehensive history along with initial screening tests should be performed to exclude acute conditions and emergencies (e.g pancreatobiliary disease, intestinal obstruction, pregnancy, etc). This includes laboratory tests (complete blood count and differential, glucose, basic metabolic panel, pancreatic and hepatic enzymes, pregnancy test), urinalysis, urinary drug screen, and plain flat radiographic series [63,64].
Further imaging and invasive testing must be tailored to the individual presentation. For example, associated symptoms like hematemesis should prompt an upper endoscopy, neurological findings would support brain imaging, and pronounced abdominal tenderness justifies an abdominal CT or abdominal radiographic series [64]. In the absence of positive findings on these diagnostic workups the possibility of an underlying motility disorder such as gastroparesis, intestinal pseudo-obstruction or small bowel dysmotility should be considered [63].
In clinical practice CHS is most often confused with cyclic vomiting syndrome (CVS). In fact patients with CHS are often mislabeled as having CVS and vice versa. Confusion exists in the medical literature secondary to a failure to recognize chronic marijuana use as a source of vomiting. For example, in two recently published series of adult patients with CVS, approximately one third of patients reported daily marijuana use [65,66]. Based on the categorization of functional disorders developed by Rome III, chronic marijuana use (CHS) is recognized as a mechanism for nausea and vomiting distinct from CVS [67]. Although both conditions share an astonishing similarity, there are several significant differences. For example, CVS patients usually have important psychological comorbidities including depression and anxiety [64,65]. In addition, CVS patients have a high prevalence of migraine headaches or a family history of migraines. Furthermore, gastric emptying rates in patients with CVS are often accelerated rather than delayed [46,65]. Table 2 summarizes some of the epidemiological and clinical characteristics that may help distinguish CVS and CHS.
Table 2.
Comparison of cyclic vomiting syndrome in adults and cannabis hyperemesis syndrome
| Cyclical Vomiting | Cannabis Hyperemesis Syndrome | |
|---|---|---|
| Age at diagnosis (y) | 34.8 | 29.3 |
| Delay in diagnosis (y) | 7.9 | 3.1 |
| Duration of episodes (days) | 3.8 | N/A |
| Cannabis use | Occasionally | Universal |
| Triggering factors (e.g. infections, psychological stress, etc) | Frequent | Absent |
| Prodrome | Common | Common |
| Clinical findings | ||
| Vomiting | Universal | Universal |
| Abdominal Pain | Common (58–71%) – Moderate to severe | Common – Mild to moderate |
| Compulsive Bathing | Absent | Universal |
| GES | Accelerated | Delayed |
| Comorbidities Psychiatric | Common | Not common |
| Migraine headache | Common (24–70%) | Not common |
| Treatment | Abortive measures (antimigraine agents), supportive care, psychological support | Cannabis cessation, supportive care |
| Prophylaxis | Avoid triggers, TCA | Cannabis cessation |
Data from Abell TL et al, Allen J et al and Soriano M et al.
N/A Not available, GES Gastric emptying study, TCA Tricyclic antidepressants
Treatment
The treatment of Cannabinoid Hyperemesis Syndrome can be divided into therapy for the hyperemetic phase and the prevention of relapse. Patients may require hospitalization during the hyperemetic phase secondary to abdominal pain, volume depletion, and severe nausea and vomiting. Supportive therapy, albeit not very effective, serves as the mainstay of treatment during this phase of the syndrome [6,53,62]. For volume depletion aggressive resuscitation with intravenous fluids is needed [6,59,61,62]. Anti-emetic therapy can be tried with 5-HT3 receptor antagonists, D2 receptor antagonists, H1 receptor antagonists, and neurokinin-1 receptor antagonists. However, all have been shown to provide minimal or no improvement in most patients with CHS [54–58,62,68]. Narcotics have also been attempted in a few cases to relieve associated abdominal pain [55,57]. Opioids should be used with caution, however, as they have the potential to cause emesis. [69,70]. Esophagogastroduodenoscopy findings from several patients with CHS have revealed varying grades of esophagitis and gastritis [6,54,57,60–62]. As a result, acid suppression therapy with medications such as proton pump inhibitors should be given routinely.
The most effective treatment during the hyperemetic phase of CHS is the use of hot showers by patients. The effects of this learned behavior are temperature-dependent [6], fast acting [6], but short-lived [6,56,62]. Hot showers improve symptoms of nausea and vomiting [6,52–56,60,62,68,71], abdominal pain [6,56,71], and decreased appetite [68] during the hyperemetic phase. The precise mechanism by which hot bathing produces a rapid reduction in the symptoms of CHS is unknown. It has been proposed that hot bathing may act by correcting the cannabis-induced disequilibrium of the thermoregulatory system of the hypothalamus [6]. Darmani has suggested that cannabis increases the core body temperature while concomitantly decreasing skin temperature thus increasing blood flow to the skin and dissipating excess core body heat [72].
The hyperemetic phase of CHS typically lasts for only 24–48 hours [6], but the risk for relapse is high if the patient returns to cannabis use. Case reports have demonstrated a remission in CHS symptoms upon cessation of cannabis use for extended periods [6,51–54,57,59–62,68,71]. Unfortunately, many of these patients relapse upon resuming cannabis [6,59,61,62]. It has been suggested that many of these patients increase or continue their cannabis use because of their perception that it will have beneficial effects on nausea [52]. Patient education should therefore be provided with emphasis on the paradoxical nature of the symptoms of CHS. Furthermore, some authors have reported referring patients to drug rehabilitation programs in an attempt to raise the likelihood of long-term cannabis cessation [54,71]. Studies have demonstrated the efficacy of outpatient treatment options such as cognitive behavioral therapy and motivational enhancement therapy for marijuana dependence [73].
Shortcomings in our knowledge of CHS and areas for future research
There are several shortcomings in our understanding of CHS. There exists no epidemiological data regarding the incidence and prevalence of CHS among chronic marijuana users. The syndrome is likely underreported given its recent recognition [74,75]. With the large prevalence of marijuana use in the world, why does it appear that so few patients develop CHS? Certain individuals may have a genetic polymorphisms in the cytochrome P450 enzymes responsible for the metabolism of the cannabinoids [62,72]. This could result in excessive levels of pro-emetic cannabinoids or emetogenic metabolites. Such genetic variations have yet to be studied in patients diagnosed with CHS and represent an area for future research.
The mechanism by which cannabis induces hyperemesis is presently unknown. A recent review has explored numerous potential explanations regarding various pharmacokinetic and pharmacodynamic factors of the cannabinoids [72]. The cannabis plant contains over four hundred different chemicals, with sixty possessing cannabinoid structures [76]. The pro-emetic effects of two of these cannabinoids, CBD and CBG, have been discussed in this review and could conceivably play a role in the development of CHS. Additional pharmacological research is needed regarding the pro-emetic effects of additional cannabinoids and their metabolites. Another proposed explanation is that in susceptible individuals the pro-emetic effect of cannabis on the gut (e.g. delayed gastric emptying) overrides its anti-emetic CNS properties [62]. This hypothesis is supported by the demonstration of delayed gastric emptying on gastric emptying scintigraphy in some cases [6,55,62]. Further research is required to investigate the gastrointestinal physiology in these patients during both the acute attacks of hyperemesis and between episodes.
A lack of long-term follow-up is also a major shortcoming in our knowledge of CHS. The majority of reported cases that have provided follow-up included a period of less than one year [6,52,54,56–60,62,68,71]. A greater understanding of the natural course of the syndrome and response to marijuana cessation may be gained with longer lengths of follow-up. Future studies following patients longitudinally for extended periods of time are needed.
Conclusion
Cannabinoid Hyperemesis Syndrome is a new and under recognized clinical entity. Although its prevalence is unknown, numerous publications have preliminarily established its unique clinical characteristics. CHS should be considered as a plausible diagnosis in the setting of patients with recurrent intractable vomiting and strong history of cannabis abuse. Despite the well-established anti-emetic properties of marijuana, there is increasing evidence of its paradoxical effects on the gastrointestinal tract and CNS. Further initiatives are needed to determine this disease prevalence and its other epidemiological characteristics, natural history, and pathophysiology. Additional treatments are needed and efforts to discontinue cannabis abuse are paramount.
References
- 1.United States Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Office of Applied Studies. National Survey on Drug Use and Health. ICPSR29621-v1. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]; 2009. 2010-11-16. [DOI] [Google Scholar]
- 2.Foley JD. Adolescent use and misuse of marijuana. Adolesc Med Clin. 2006;17:319–34. doi: 10.1016/j.admecli.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 3.European Monitoring Centre of Drugs and Drug Addiction. Annual report 2006: the state of the drugs problem in Europe. Report No: 92-9168-266-7. Office for Official Publications of the European Communities; Luxembourg: [Google Scholar]
- 4.Compton WM, Grant BF, Colliver JD, et al. Prevalence of marijuana use disorder in the United States: 1991–1992 and 2001–2002. JAMA. 2004;291:2214–21. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- 5.Stinson FS, Ruan WJ, Pickering R, et al. Cannabis use disorders in the USA: prevalence, correlates and co-morbidity. Psychol Med. 2006;36:1447–60. doi: 10.1017/S0033291706008361. [DOI] [PubMed] [Google Scholar]
- 6.Allen JH, de Moore GM, Heddle R, et al. Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis use. Gut. 2004;53:1566–1570. doi: 10.1136/gut.2003.036350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howlett AC, Johnson MR, Melvin LS, et al. Nonclassical Cannabinoid analgetics inhibit adenylate cyclase: development of a cannabinoid receptor model. Mol Pharmacol. 1988;33:297–302. [PubMed] [Google Scholar]
- 8.Iverson L. Cannabis and the brain. Brain. 2003;126:1252–70. doi: 10.1093/brain/awg143. [DOI] [PubMed] [Google Scholar]
- 9.Izzo AA, Camilleri M. Emerging role of cannabinoids in gastrointestinal and liver diseases: basic and clinical aspects. Gut. 2008;57:1140–55. doi: 10.1136/gut.2008.148791. [DOI] [PubMed] [Google Scholar]
- 10.Pertwee RG. Pharmacology of cannabinoid CB1 and CB2 receptors. Pharmacol Ther. 1997;74:129–80. doi: 10.1016/s0163-7258(97)82001-3. [DOI] [PubMed] [Google Scholar]
- 11.Pertwee RG. Pharmacology of cannabinoid receptor ligands. Curr Med Chem. 1999;6:635–64. [PubMed] [Google Scholar]
- 12.Wright K, Rooney N, Feeney M, et al. Differential expression of cannabinoid receptors in the human colon: cannabinoids promote epithelial wound healing. Gastroenterology. 2005;129:437–53. doi: 10.1016/j.gastro.2005.05.026. [DOI] [PubMed] [Google Scholar]
- 13.Wright KL, Duncan M, Sharkey KA. Cannabinoid CB(2) receptors in the gastrointestinal tract: a regulatory system in states of inflammation. Br J Pharmacol. 2008;153:263–70. doi: 10.1038/sj.bjp.0707486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mathison R, Ho W, Pittman QJ, et al. Effects of cannabinoid receptor-2 activation on accelerated gastrointestinal transit in lipopolysaccharide-treated rats. Br J Pharmacol. 2004;142:1247–54. doi: 10.1038/sj.bjp.0705889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duncan M, Davison JS, Sharkey KA. Review article: endocannabinoids and their receptors in the enteric nervous system. Aliment Pharmacol Ther. 2005;22:667–83. doi: 10.1111/j.1365-2036.2005.02648.x. [DOI] [PubMed] [Google Scholar]
- 16.Cadas H, di Tomaso E, Piomelli D. Occurrence and biosynthesis of endogenous cannabinoid precursors, N-arachidonoyl phosphatidylethanolamine, in rat brains. J Neurosci. 1997;17:1226–42. doi: 10.1523/JNEUROSCI.17-04-01226.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DiMarzo V, Fontana A, Cadas H, et al. Formation and inactivation of endogenous cannabinoid anandamide in central neurons. Nature. 1994;372:686–91. doi: 10.1038/372686a0. [DOI] [PubMed] [Google Scholar]
- 18.Giuffrida A, Beltramo M, Piomelli D. Mechanisms of endocannabinoid inactivation: biochemistry and pharmacology. J Pharmacol Exp Ther. 2001;298:7–14. [PubMed] [Google Scholar]
- 19.Watanabe K, Matsunaga T, Yamamoto I, et al. Involvement of CYP2C in the metabolism of cannabinoids by human hepatic microsomes from an old woman. Biol Pharm Bull. 1995;18:1138–41. doi: 10.1248/bpb.18.1138. [DOI] [PubMed] [Google Scholar]
- 20.Grotenhermen F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. 2003;42:327–60. doi: 10.2165/00003088-200342040-00003. [DOI] [PubMed] [Google Scholar]
- 21.Wall ME, Sadler BM, Brine D, et al. Metabolism, disposition, and kinetics of delta-9 tetrahydrocannabinol, in men and women. Clin Pharmacol Ther. 1983;34:352–63. doi: 10.1038/clpt.1983.179. [DOI] [PubMed] [Google Scholar]
- 22.Kreuz DS, Axelrod J. Delta-9-tetrahydrocannabinol: localization in body fat. Science. 1973;179:391–3. doi: 10.1126/science.179.4071.391. [DOI] [PubMed] [Google Scholar]
- 23.Gunasekaran N, Long LE, Dawson BL, et al. Reintoxication: the release of fat-stored delta(9)-tetrahydrocannabinol (THC) into blood is enhanced by food deprivation or ACTH exposure. Br J Pharmacol. 2009;158:1330–7. doi: 10.1111/j.1476-5381.2009.00399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harvey DJ, Brown NK. Comparative in vitro metabolism of the cannabinoids. Pharmacol Biochem Behav. 1991;40:533–40. doi: 10.1016/0091-3057(91)90359-a. [DOI] [PubMed] [Google Scholar]
- 25.Perez-Reyes M, Timmons M, Lipton M, et al. Intravenous injection in man of delta-9-tetrahydro-cannabinol and 11-OH-delta-9-tetrahydrocannabinol. Science. 1972;177:633–5. doi: 10.1126/science.177.4049.633. [DOI] [PubMed] [Google Scholar]
- 26.Burstein SH. The cannabinoid acids: nonpsychoactive derivatives with therapeutic potential. Pharmacol Ther. 1999;82:87–96. doi: 10.1016/s0163-7258(98)00069-2. [DOI] [PubMed] [Google Scholar]
- 27.Mechoulam R, Parker LA, Gallily R. Cannabidiol: an overview of some pharmacological aspects. J Clin Pharmacol. 2002;42:11–19. doi: 10.1002/j.1552-4604.2002.tb05998.x. [DOI] [PubMed] [Google Scholar]
- 28.Russo EB, Burnett A, Hall B, et al. Agonistic properties of Cannabidiol at 5-HT1a receptors. Neurochem Res. 2005;30:1037–43. doi: 10.1007/s11064-005-6978-1. [DOI] [PubMed] [Google Scholar]
- 29.Hayakawa K, Mishima K, Hazekawa M, et al. Cannabidiol potentiates pharmacologic effects of Δ 9 -tetrahydrocannabinol via CB1 receptor-dependent mechanism. Brain Res. 2008;1188:157–164. doi: 10.1016/j.brainres.2007.09.090. [DOI] [PubMed] [Google Scholar]
- 30.Parker LA, Kwiatkowska M, Burton P, et al. Effect of cannabinoids on lithium-induced vomiting in the Suncus murinus(house musk shrew) Psychopharmacology. 2004;171:156–61. doi: 10.1007/s00213-003-1571-2. [DOI] [PubMed] [Google Scholar]
- 31.Kwiatkowska M, Parker LA, Burton P, et al. A comparative analysis of the potential of cannabinoids and ondansetron to suppress cisplatin-induced emesis in the Suncus murinus (house musk shrew) Psychopharmacology. 2004;174:254–9. doi: 10.1007/s00213-003-1739-9. [DOI] [PubMed] [Google Scholar]
- 32.Cascio MG, Gauson LA, Stevenson LA, et al. Evidence that the plant cannabinoid cannabigerol is a highly potent alpha 2-adrenoceptor agonist and moderately potent 5HT1A receptor antagonist. Br J Pharmacol. 2010;159:129–41. doi: 10.1111/j.1476-5381.2009.00515.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rock EM, Goodwin JM, Limebeer CL, et al. Interaction between non-psychotropic cannabinoids in marihuana: effect of cannabigerol (CBG) on the anti-nausea or anti-emetic effects of cannabidiol (CBD) in rats and shrews. Psychopharmacology. 2011 doi: 10.1007/s00213-010-2157-4. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 34.Pi-Sunyer FX, Aronne LJ, Heshmati HM, et al. Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: a randomized controlled trial. JAMA. 2006;295:761–75. doi: 10.1001/jama.295.7.761. [DOI] [PubMed] [Google Scholar]
- 35.Darmani NA. The potent emetogenic effects of the endocannabinoid, 2-AG (2-arachidonoylglycerol), are blocked by delta (9)-tetrahydrocannabinol and other cannabinoids. J Pharmacol Exp Ther. 2002;300:34–42. doi: 10.1124/jpet.300.1.34. [DOI] [PubMed] [Google Scholar]
- 36.Van Sickle MD, Oland LD, Ho W, et al. Cannabinoids inhibit emesis through CB1 receptors in the brainstem of the ferret. Gastroenterology. 2001;121:767–74. doi: 10.1053/gast.2001.28466. [DOI] [PubMed] [Google Scholar]
- 37.Walsh D, Nelson KA, Mahmoud FA. Established and potential therapeutic applications of cannabinoids in oncology. Support Care Cancer. 2003;11:137–43. doi: 10.1007/s00520-002-0387-7. [DOI] [PubMed] [Google Scholar]
- 38.Pagotto U, Marsicano G, Cota D, et al. The emerging role of the endocannabinoid system in endocrine regulation and energy balance. Endocr Rev. 2006;27:73–100. doi: 10.1210/er.2005-0009. [DOI] [PubMed] [Google Scholar]
- 39.Cota D, Steiner MA, Marsicano G, et al. Requirement of cannabinoid receptor type 1 for the basal modulation of hypothalamic-pituitary-adrenal axis function. Endocrinology. 2007;148:1574–81. doi: 10.1210/en.2005-1649. [DOI] [PubMed] [Google Scholar]
- 40.Lehmann A, Blackshaw LA, Brandon L, et al. Cannabinoid receptor agonism inhibits transient lower esophageal sphincter relaxation and reflux in dogs. Gastroenterology. 2002;123:1129–34. doi: 10.1053/gast.2002.36025. [DOI] [PubMed] [Google Scholar]
- 41.Hinds NM, Ullrich K, Smid SD. Cannabinoid 1 (CB1) receptors coupled to cholinergic motorneurones inhibit neurogenic circular muscle contractility in the human colon. Br J Pharmacol. 2006;148:191–99. doi: 10.1038/sj.bjp.0706710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Esfandyari T, Camilleri M, Busciglio I, et al. Effects of a cannabinoid receptor agonist on colonic motor and sensory functions in humans: a randomized, placebo-controlled study. Am J Physiol Gastrointest Liver Physiol. 2007;293:137–45. doi: 10.1152/ajpgi.00565.2006. [DOI] [PubMed] [Google Scholar]
- 43.Pertwee RG. Cannabinoids and the gastrointestinal tract. Gut. 2001;48:859–67. doi: 10.1136/gut.48.6.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krowicki ZK, Moerschbaecher JM, Winsauer PJ, et al. Delta9-tetrahydrocannabinol inhibits gastric motility in the rat through cannabinoid CB1 receptors. Eur J Pharmacol. 1999;371:187–96. doi: 10.1016/s0014-2999(99)00165-x. [DOI] [PubMed] [Google Scholar]
- 45.Izzo AA, Mascolo N, Capasso R, et al. Inhibitory effect of cannabinoid agonists on gastric emptying in the rat. Naunyn Schmiedebergs Arch Pharmacol. 1999;360:221–3. doi: 10.1007/s002109900054. [DOI] [PubMed] [Google Scholar]
- 46.McCallum RW, Soykan I, Sridhar KR, et al. Delta-9-tetrahydrocannabinol delays the gastric emptying of solid food in humans: a double-blind, randomized study. Aliment Pharmacol Ther. 1999;13:77–80. doi: 10.1046/j.1365-2036.1999.00441.x. [DOI] [PubMed] [Google Scholar]
- 47.Esfandyari T, Camilleri M, Ferber I, et al. Effect of a cannabinoid agonist on gastrointestinal transit and postprandial satiation in healthy human subjects: a randomized, placebo-controlled study. Neurogastroenterol Motil. 2006;18:831–8. doi: 10.1111/j.1365-2982.2006.00834.x. [DOI] [PubMed] [Google Scholar]
- 48.Abalo R, Cabezos PA, Lopez-Miranda V, et al. Selective lack of tolerance to delayed gastric emptying after daily administration of WIN 55,212-2 in the rat. Neurogastroenterol Motil. 2009;21:1002–80. doi: 10.1111/j.1365-2982.2009.01315.x. [DOI] [PubMed] [Google Scholar]
- 49.Abalo R, Cabezos PA, Vera G, et al. Cannabinoid-induced delayed gastric emptying is selectively increased upon intermittent administration in the rat: role of CB1 receptors. Neurogastroenterol Motil. 2011;23:457–77. doi: 10.1111/j.1365-2982.2011.01677.x. [DOI] [PubMed] [Google Scholar]
- 50.Parkman HP, Fass R, Foxx-Orenstein AE. Treatment of patients with diabetic gastroparesis. Gastroenterol Hepatol. 2010;6:1–16. [PMC free article] [PubMed] [Google Scholar]
- 51.Roche E, Foster PN. Cannabinoid hyperemesis: not just a problem in Adelaide Hills. Gut. 2005;54:731. [PMC free article] [PubMed] [Google Scholar]
- 52.Singh E, Coyle W. Cannabinoid hyperemesis. Am J Gastroenterol. 2008;103:1048–9. doi: 10.1111/j.1572-0241.2007.01772_11.x. [DOI] [PubMed] [Google Scholar]
- 53.Wallace D, Martin AL, Park B. Cannabinoid hyperemesis: marijuana puts patients in hot water. Aust Psychiatry. 2007;15:156–8. doi: 10.1080/10398560701196778. [DOI] [PubMed] [Google Scholar]
- 54.Budhraja V, Narang T, Slaiman A. Cannabinoid hyperemesis syndrome: cyclic vomiting, chronic cannabis use and compulsive bathing. Practical Gastroeneterol. 2008;32:79–80. [Google Scholar]
- 55.Chang YH, Windish D. Cannabinoid hyperemesis relieved by compulsive bathing. Mayo Clin Proc. 2009;84:76–78. doi: 10.4065/84.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sannarangappa V, Tan C. Cannabinoid hyperemesis. Intern Med J. 2009;39:777–8. doi: 10.1111/j.1445-5994.2009.02047.x. [DOI] [PubMed] [Google Scholar]
- 57.Sontineni SP, Chaudhary S, Sontineni V, et al. Cannabinoid hyperemesis syndrome: clinical diagnosis of an under recognized manifestation of chronic cannabis abuse. World J Gastroenterol. 2009;15:1264–6. doi: 10.3748/wjg.15.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Watts M. Cannabinoid hyperemesis presenting to a New Zealand hospital. N Z Med J. 2009;122:116–8. [PubMed] [Google Scholar]
- 59.Donnino MW, Cocchi MN, Miller J, et al. Cannabinoid hyperemesis: a case series. J Emerg Med. 2009;40:63–6. doi: 10.1016/j.jemermed.2009.07.033. [DOI] [PubMed] [Google Scholar]
- 60.Miller JB, Walsh M, Patel PA, et al. Pediatric cannabinoid hyperemesis: two cases. Pediatr Emerg Care. 2010;26:919–20. doi: 10.1097/PEC.0b013e3181fe9189. [DOI] [PubMed] [Google Scholar]
- 61.Patterson DA, Smith E, Monahan M, et al. Cannabinoid hyperemesis and compulsive bathing: a case series and paradoxical pathophysiological explanation. J Am Board Fam Med. 2010;23:790–3. doi: 10.3122/jabfm.2010.06.100117. [DOI] [PubMed] [Google Scholar]
- 62.Soriano-Co M, Batke M, Cappell MS. The cannabis hyperemesis syndrome characterized by persistent nausea and vomiting, abdominal pain, and compulsive bathing associated with chronic marijuana use: a report of eight cases in the United States. Dig Dis Sci. 2010;55:3113–9. doi: 10.1007/s10620-010-1131-7. [DOI] [PubMed] [Google Scholar]
- 63.Quigley E, Hasler W, Parkman H. AGA Technical review on nausea and vomiting. Gastroenterology. 2001;120:263–86. doi: 10.1053/gast.2001.20516. [DOI] [PubMed] [Google Scholar]
- 64.Abell TL, Kim CH, Malagelada JR. Idiopathic cyclic nausea and vomiting—a disorder of gastrointestinal motility. Mayo Clin Proc. 1988;63:1169–1175. doi: 10.1016/s0025-6196(12)65401-9. [DOI] [PubMed] [Google Scholar]
- 65.Namin F, Patel J, Lin Z, Sarosiek I, Foran P, Esmaeili P, et al. Clinical, psychiatric and manometric profile of cyclic vomiting syndrome in adults and response to tricyclic therapy. Neurogastroenterol Motility. 2007;19:196–202. doi: 10.1111/j.1365-2982.2006.00867.x. [DOI] [PubMed] [Google Scholar]
- 66.Hejazi RA, Reddymasu SC, Namin F, Lavenbarg T, Foran P, McCallum RW. Efficacy of tricyclic antidepressant therapy in adults with cyclic vomiting syndrome: a two-year follow-up study. J Clin Gastroenterol. 2010;44:18–21. doi: 10.1097/MCG.0b013e3181ac6489. [DOI] [PubMed] [Google Scholar]
- 67.Tack J, Talley N, Camilleri M, et al. Functional Gastroduodenal Disorders. Gastroenterology. 2006;130:1466–79. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 68.Schmid SM, Lapaire O, Huang DJ, et al. Cannabinoid hyperemesis syndrome: an underreported entity causing nausea and vomiting of pregnancy. Arch Gynecol Obstet. 2010 doi: 10.1007/s00404-010-1811-8. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 69.Porreca F, Ossipov MH. Nausea and vomiting side effects with opioid analgesics during treatment of chronic pain: mechanisms, implications, and management options. Pain Med. 2009;10:654–62. doi: 10.1111/j.1526-4637.2009.00583.x. [DOI] [PubMed] [Google Scholar]
- 70.Cepeda MS, Farrar JT, Baumgarten M, Boston R, Carr DB, Strom BL. Side effects of opioids during short-term administration: effect of age, gender, and race. Clin Pharmacol Ther. 2003;74:102–12. doi: 10.1016/S0009-9236(03)00152-8. [DOI] [PubMed] [Google Scholar]
- 71.Chepyala P, Olden KW. Cyclic vomiting and compulsive bathing with chronic cannabis abuse. Clin Gastroenterol Hepatol. 2008;6:710–12. doi: 10.1016/j.cgh.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 72.Darmani NA. Cannabinoid-induced hyperemesis: A conundrum-from clinical recognition to basic science mechanisms. Pharmaceuticals. 2010;3:2163–77. doi: 10.3390/ph3072163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Budney AJ, Roffman R, Stephens RS, et al. Marijuana dependence and its treatment. Addict Sci Clin Pract. 2007;4:4–16. doi: 10.1151/ascp07414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Budhraja V. Confirming the diagnosis of cannabinoid hyperemesis syndrome. Mayo Clin Proc. 2009;84:483. doi: 10.1016/S0025-6196(11)60569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Byrne A, Hallinan R, Wodak A. Cannabis hyperemesis causation questioned. Gut. 2006;55:132. [PMC free article] [PubMed] [Google Scholar]
- 76.Watson SJ, Benson JA, Joy JE. Marijuana and Medicine: assessing the science base: a summary of the 1999 Institute of Medicine Report. Arch Gen Psychiat. 2000;57:547–52. doi: 10.1001/archpsyc.57.6.547. [DOI] [PubMed] [Google Scholar]