Abstract
Purpose
To evaluate IL13Rα2 as an immunotherapeutic target for eliminating glioma stem-like initiating cells (GSC) of high-grade gliomas, with particular focus on the potential of genetically engineered IL13Rα2-specific primary human CD8+ cytotoxic T lymphocytes (IL13-zetakine+ CTL) to target this therapeutically resistant glioma subpopulation.
Experimental Design
A panel of low-passage GSC tumor sphere and serum-differentiated glioma lines were expanded from patient glioblastoma specimens. These glioblastoma lines were evaluated for expression of IL13Rα2 and for susceptibility to IL13-zetakine+ CTL-mediated killing in vitro and in vivo.
Results
We observed that while glioma IL13Rα2 expression varies between patients, for IL13Rα2pos cases this antigen was detected on both GSCs and more differentiated tumor cell populations. IL13-zetakine+ CTL were capable of efficient recognition and killing of both IL13Rα2pos GSC and IL13Rα2pos differentiated cells in vitro, as well as eliminating glioma initiating activity in an orthotopic mouse tumor model. Furthermore, intracranial administration of IL13-zetakine+ CTL displayed robust anti-tumor activity against established IL13Rα2pos GSC tumor sphere-initiated orthotopic tumors in mice.
Conclusions
Within IL13Rα2-expressing high-grade gliomas, this receptor is expressed by GSCs and differentiated tumor populations, rendering both targetable by IL13-zetakine+ CTLs. Thus, our results support the potential utility of IL13Rα2-directed immunotherapeutic approaches for eradicating therapeutically resistant GSC populations.
Keywords: IL13Rα2, glioma stem-like cell, cytolytic T lymphocyte, adoptive T cell therapy
Introduction
The prognosis of patients with high-grade gliomas remains grim despite improvements in standard therapies including surgery, radiation and chemotherapy. The deadly nature of this disease is, in part, attributed to therapeutically resistant subpopulations of glioma stem-like cancer initiating cells (GSC) that display many characteristics of normal stem cells, including expression of stem cell markers and the potential for sustained self-renewal [1, 2]. GSCs exhibit potent tumor-initiating potential and are hypothesized to seed disease recurrence [3–5] because of their resistance to conventional chemotherapy and radiation regimens.
Cellular immunotherapies have the potential to target and eliminate this therapeutically resistant GSC population [6]. Recent promising data have demonstrated that tumor stem cells are susceptible to both CTL and natural killer (NK) perforin-dependent killing mechanisms [7–11]. Further, GSCs and differentiated tumor cells express equivalent levels of markers involved in immunologic synapse formation, and CD8+ CTL can eliminate cell populations capable of tumor engraftment [9]. Although challenges remain in addressing the confounding effects of tumor immuno-suppressive networks, particularly as they relate to specific strategies that may be employed by tumor stem cells [12–14], the intrinsic ability of immune cells to recognize and kill tumor stem cells is sufficiently powerful to warrant efforts to overcome these obstacles.
IL-13 receptor α2 (IL13Rα2) is a cell surface receptor that has received significant attention brain tumor therapy because it is over-expressed by a subset of high-grade gliomas, but not expressed at significant levels by normal brain tissue [15–18]. Our group has developed an IL13Rα2-targeting immunotherapy platform for high-grade gliomas by genetically modifying T cells to express an IL13Rα2-specific chimeric antigen receptor (CAR) termed IL13-zetakine [19]. This CAR recognizes IL13Rα2 via a membrane-tethered IL13 ligand, and initiates cytolytic killing via an intracellular CD3-zeta T cell activating domain. It also incorporates a point mutation in the IL13 ligand domain (E13Y) for preferential binding to IL13Rα2, and reduced affinity to the more ubiquitously expressed IL13 receptor, IL13Rα1 [20]. Previous studies utilizing U87 and other long-established cell lines demonstrate that engineered IL13-zetakine+ T cells exhibit potent MHC-independent, IL13Rα2-specific anti-glioma cytolytic activity, and induce regression of orthotopic xenografts in vivo [19]. Realization of the potential of therapies targeting IL13Rα2 for the treatment of malignant glioma, some of which are in clinical trial [21–24], will hinge, in part, on their ability to eradicate malignant stem/initiating tumor cell subpopulations. Here we assess the expression of IL13Rα2 on stem-like versus differentiated glioma populations, and evaluate the relative susceptibility of glioma cell populations of varying differentiation status to IL13-zetakine+ CTL mediated killing.
Materials and Methods
Cell Lines
Glioma specimens, graded according to World Health Organization (WHO) established guidelines (Supp. Table S1), were obtained from patients in accordance with Institutional Review Board-approved protocols. Tumor specimens were de-identified and given unique patient brain tumor (PBT) numbers. For one tumor obtained from a patient who participated in our adoptive T cell therapy clinical trial, it was also referred to by its unique patient number (UPN) to indicate the patient from which this tumor was derived (PBT015-UPN033). Short-term tumor sphere (TS) cultures of GSCs and adherent lines were expanded and cultured as previously described [9]. In some cases tumor explants were expanded by heterotopic subcutaneous (s.c.) passaging in mice prior to growth and characterization in culture [9], and in such cases the s.c. passage number is reported after the PBT number (for instance, PBT009-2 was s.c. passaged twice, and PBT003-4 and PBT017-4 were s.c. passaged four times). Differentiated lines (DIF) were generated by growing TS in Sato’s Media (DMEM:F12, 2 mmol/L, L-glutamine, 25 mmol/L HEPES, and 7% FCS) for 7 to 14 days. Adherent lines (ADH) were generated by growing freshly dispersed tumor cells directly in Sato’s media and used for assays between passages 7 to 30.
Human peripheral blood mononuclear cells (PBMC) were obtained from healthy donors or patients in accordance with Institutional Review Board-approved protocols. The generation of IL13-zetakine+ (HD003 IL13-zetakine+ clone 2D7) and CD19R+ (HD181 CD19R+ clone E8) CD8+ T cell lines has been described previously [19, 25]. CD8+ T cell lines derived from a patient who participated in our adoptive T cell therapy clinical trial is referred to by its UPN designation (UPN033). Healthy donor T cell lines were de-identified and designated unique healthy donor (HD) numbers. T cell clones were cultured as described [19], and all assays were performed between day 10 through 14 of the stimulation cycle. Lymphoblastoid lines (LCL) were established from Epstein-Barr virus-infected human PBMC [19]. LCL-OKT3 were engineered to express a membrane bound OKT3 single chain antibody (OKT3scFv) as described previously [26].
Flow cytometric analysis
Cell surface expression of IL13Rα2 was detected using goat polyclonal anti-IL13Rα2 (AF146, R&D Systems), followed by murine anti-goat fluorescein isothiocyanate (FITC) (Jackson ImmunoResearch) Supp. Table S2. Cell-surface expression of CD133 was detected as described [9] with phycoerythrin (PE)-conjugated mouse anti-human CD133/1 and anti-human CD133/2 (Miltenyi Biotec) (Supp. Table S2). Percent of immunoreactive cells was calculated using the subtraction method via FCS Express version 3 software (De Novo Software).
Western analysis
Western blots were probed with goat polyclonal anti-IL13Rα2 (AF146) and anti-Olig2 (R&D Systems); rabbit polyclonal anti-Actin (Rockland); and mouse monoclonal anti-β-III Tubulin (Millipore), anti-CD133 (Miltenyi), and anti-GFAP (Sigma-Aldrich) antibodies as per the manufacturers’ instructions (Supp. Table S2). Blots were imaged on the Odyssey Infrared Imaging System (LI-COR) and band intensities were quantified using Odyssey v2.0 software (LI-COR).
Immunofluorescence and Immunohistochemistry
TSs were plated on poly-L-ornithine (Sigma) and mouse laminin (BD Biosciences) coated chamber slides to support adherent growth [27]. When required, cells were grown for 7–10 days in 10% FCS-containing media to promote astrocytic differentiation (GFAP immunoreactive), or 0.5% FCS with 5 µM forskolin (Sigma) to promote neuronal differentiation (β-III Tubulin immunoreactive). Cells were stained with primary antibodies anti-SOX2 (Abcam, Cambridge, MA), anti-Nestin cl. 10C2 (Millipore), anti-GFAP (Sigma), and anti-βIII Tubulin (Millipore), followed by anti-mouse or anti-rabbit Alexa-488 (Invitrogen), and co-stained with 4’,6-diamidino-2-phenylindole (DAPI) mounting solution (Vector Laboratories, Inc.) (Supp. Table S2). Cells were visualized using an AX70 fluorescent microscope (Olympus), and exposure settings for each antibody were kept constant between growth conditions.
Glioblastoma IL13Rα2 immunohistochemistry (IHC) was performed on 5 µm-sections of formalin-fixed paraffin-embedded specimens, treated with EnVision FLEX Target Retrieval Solution Low pH (Dako) in a PT Link pretreatment module (Dako) for antigen retrieval. Sections were then blocked with serum-free protein block (Dako), incubated with 3.33 µg/mL goat polyclonal anti-IL13Rα2 (AF146), and detected using rabbit anti-goat (Dako) and the EnVision FLEX/HRP system (Dako). All staining was performed using the DAKO polymer automated system.
For mouse brain IHC, brains were harvested, fixed and embedded in paraffin as described previously [19]. 10 µm-thick horizontal brain sections were deparaffinized, underwent citrate-based antigen retrieval, and stained with anti-human Nestin cl. 10C2 (Millipore), anti-SOX2 (R&D Systems), anti-Olig2 (R&D Systems) or anti-GFAP (Dako) followed by detection using the EnVision kit (Vector Laboratories) with 50% hematoxylin counterstain.
qPCR
To quantify IL13Rα2 mRNA levels, RNA samples were isolated from cells using the RNeasy Kit (Qiagen), and cDNA was prepared using the Superscript First Strand Synthesis System for RT-PCR kit (Invitrogen). Real-time PCR analysis was performed using SybrGreen (Qiagen) with specific primer pairs for IL13Rα2 (GenBank; NM_000640.2) spanning exon 1–2 and exons 6–7 and β-actin (internal PCR control) (Supp. Table S3). Fold-difference in IL13Rα2 mRNA levels compared to the U251T calibrator line was determined using the Livak method [28].
Cytotoxicity and Cytokine assays
Chromium release assays (CRA) were performed as previously described [29]. Cytokine production was measured by co-culturing T cells with tumor at a 10:1 E:T ratio. In blocking experiments, anti-IL13 antibody (BD Biosciences) and recombinant human IL-13 (Peprotech) were added at the indicated concentrations to responders and stimulators, respectively, 30 minutes prior to plating. After 20–24 hr incubation, supernatants were harvested and assayed using Luminex multiplex bead technology (Upstate), and output data were analyzed via the Bio-Plex Manager 4.0 (BioRad).
Tumor xenografts and tumor volume determination
Mice were maintained under pathogen-free conditions, and all procedures were performed with 6–8 week old NOD-scid or NOD/scid/IL2R−/− (NSG) mice as approved by the COH Institute Animal Care and Use Committee. Intracranial tumor xenografts were performed as previously described [19]. No difference in tumor engraftment between NOD-scid and NSG mouse strains has been observed.
Fixed and paraffin-embedded brains were serially sectioned at 10 um intervals over the entire extent of the tumor. In most cases, every 20th section was stained with a human-specific nestin antibody (any human cell will be tumor) and visualized with DAB. These sections were scanned at high resolution (Chromavision ACIS II). Brain slice images were aligned and DAB+ pixels in each brain slice were segmented and counted using Reconstruct software (http://synapses.clm.utexas.edu/tools/reconstruct/reconstruct.stm) [30]. In some cases, segmentation was based on color and cell density in H+E-stained sections. In all cases pixel area was extrapolated over the 200 um slice interval and total volumes computed accordingly.
Results
Incidence of glioma-associated IL13Rα2 expression is independent of tumor cell differentiation status
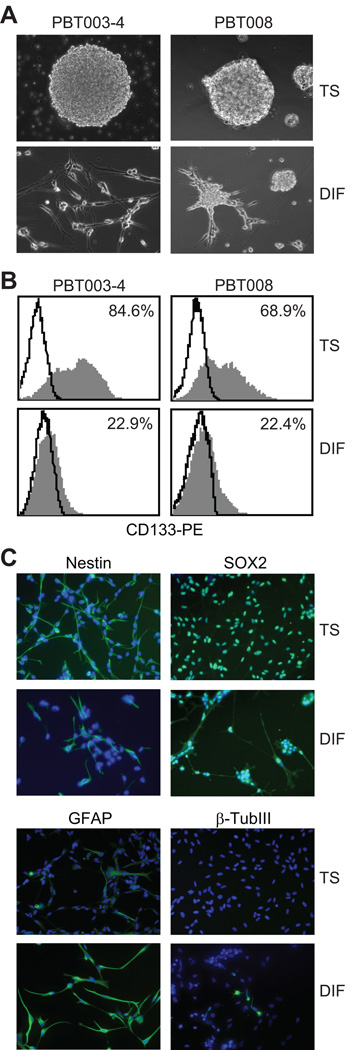
Our group has generated a panel of glioma stem/initiating cell (GSC) lines from patient glioblastoma specimens grown as tumor spheres (TSs) in serum-free media supplemented with EGF and FGF [9]. These GSC TS lines were derived either from freshly dispersed human biopsy specimens or after heterotopic s.c. passaging of patient biopsy tissue in immunocompromised mice [9, 31]. The expanded GSC TS lines exhibit stem cell-like characteristics: formation of secondary TSs as an indication of in vitro self-renewal potential (Fig. 1A), expression of stem cell markers such as CD133, SOX2 and Nestin (Fig. 1B, C), differentiation to express lineage specific markers such as GFAP and β-III tubulin (Fig. 1C), and formation of orthotopic intracranial tumors in immuno-compromised mice (see also [9]; Supp. Table S4).
Figure 1. Characterization of tumor sphere and serum-differentiated cells isolated from primary high-grade glioma specimens.
(A) Representative images of tumor sphere cells grown in serum-free stem cell medium (TS, top panels), and after transfer to differentiating FCS-containing medium (DIF, bottom panels). (B) Flow cytometry of TS and DIF cells stained with anti-CD133 (gray) or isotype control antibody (solid lines). Percentage of CD133+ cells is indicated. (C) Immunofluorescence of PBT003-4 TS and DIF cells stained for stem cell markers nestin and SOX2 (green, top panels); and lineage specific differentiation markers GFAP and β-III tubulin (green, bottom panels). Cell nuclei were stained blue with DAPI.
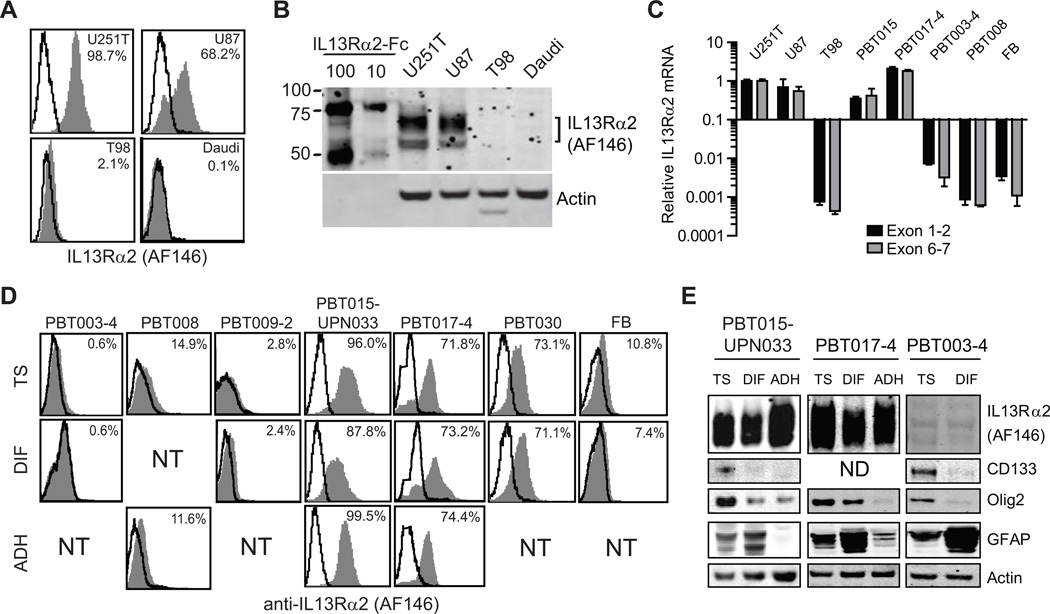
This resource of patient derived GSCs allowed us to assess expression of IL13Rα2 on stem-like TS and serum-differentiated (DIF) glioma lines. For these studies, we compared IL13Rα2 protein and mRNA levels by Western, flow cytometry and reverse transcription qPCR (RT-qPCR) (Fig. 2). The specificity of receptor recognition in these assays was confirmed by detection of this receptor on known IL13Rα2pos glioma lines U251T and U87 [19, 32], but not on the IL13Rα2neg T98 glioma and Daudi lymphoma cell lines [19, 32] (Fig. 2A–C). It is important to note that IL13Rα2-specific commercial antibodies display significant differences in glioma IL13Rα2 detection. We find that clone B-D13 (Cell Sciences) and GW22455A (GenWay) do not recognize an antigen on gliomas that is consistent with either IL13Rα2 mRNA expression or functional recognition of IL13Rα2 by IL13-zetakine CTL (Supp. Fig. S1; Figs. 2 and 4) [19, 32]. These findings raise questions regarding previously published reports which utilized these antibodies, particularly the commonly used anti-IL13Rα2 B-D13 antibody (Cell Sciences), to assess the frequency of IL13Rα2-expression on gliomas [18, 33]. This inconsistency may also underlie the lack of correlation between IL13Rα2 mRNA and protein expression for primary glioma biopsy specimens when the anti-IL13Rα2 B-D13 antibody (Cell Sciences) was used for IHC [34]. We have therefore used the goat polyclonal anti-IL13Rα2 AF146 antibody (R&D Systems) for all experiments as it is the only antibody tested that shows a consistent correlation between IL13Rα2 protein levels and mRNA expression [Western and flow cytometry versus RT-qPCR (Fig. 2 A–C, and Supp. Fig. S1).
Figure 2. IL13Rα2 expression on GSC and differentiated glioma cell lines.
(A) Flow cytometric detection of IL13Rα2 on established glioma cell lines U251T, U87 and T98. Daudi lymphoma is an IL13Rα2neg control cell line. Percentage positive cells are indicated in each histogram. (B) Western blots detecting IL13Rα2 for established glioma cell lines. Recombinant human IL13Rα2-Fc (10ng and 100ng) demonstrates receptor-specific detection by the antibody. (C) RT-qPCR analysis depicting IL13Rα2 mRNA expression by cell lines relative to U251T using primer sets spanning IL13Rα2 exons 1–2 and 6–7. Data was normalized to actin. (D) Tumor sphere (TS), serum-differentiated (DIF), and serum-expanded (ADH) cells analyzed by flow cytometry for expression of IL13Rα2 (grey histograms); solid lines are secondary antibody alone. NT; not tested. (E) Western blots detecting IL13Rα2, CD133, Olig2, GFAP, and α-actin for TS, DIF, and ADH cell lines. ND, not detected.
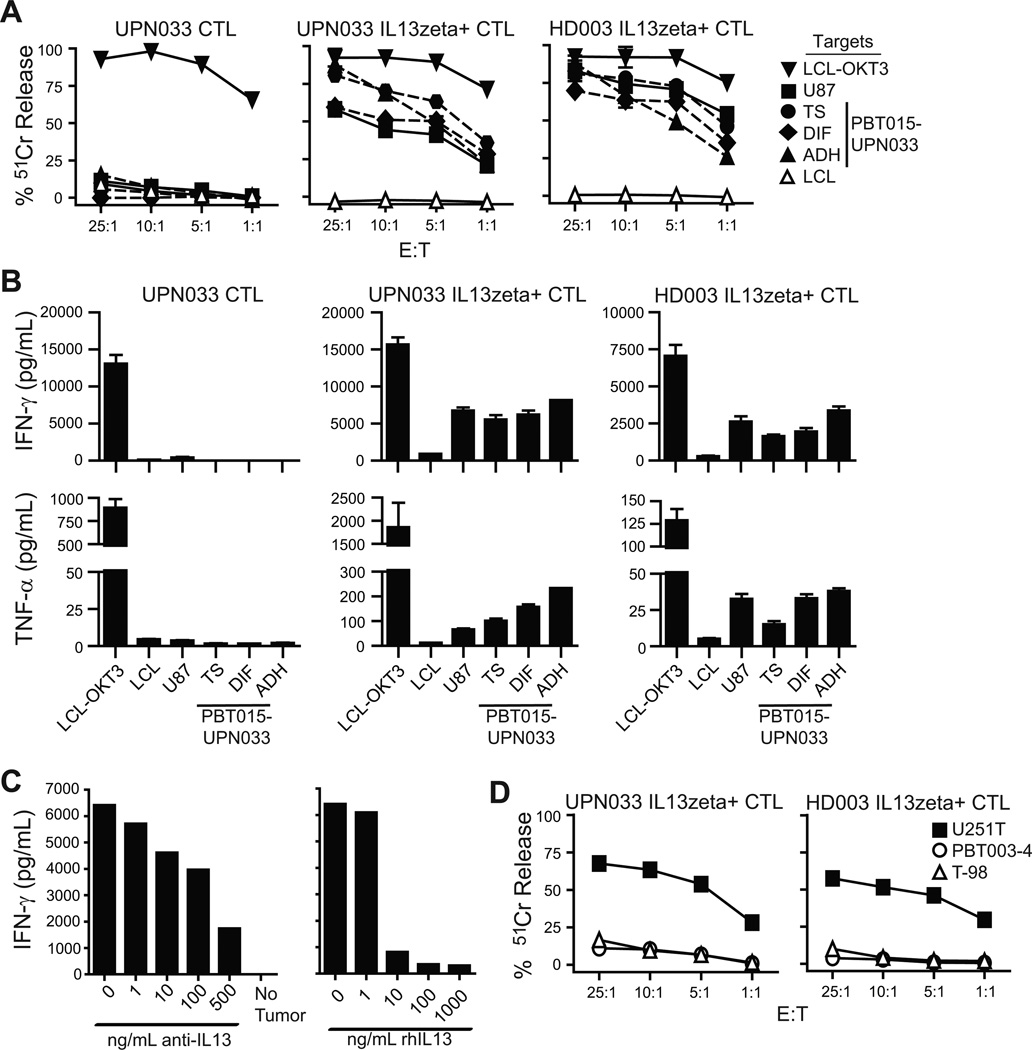
Figure 4. IL13-zetakine+ CTL kill with comparable potency IL13Rα2pos GSCs, differentiated cells, and established glioma cell lines.
(A) CRA measuring the lysis of IL13Rα2pos U87 glioma cells or PBT015-UPN033 derived TS, 7-day serum-differentiated (DIF), or serum-expanded (p15; ADH) cells at increasing effector:target (E:T) ratios. The IL13Rα2neg CD19pos LCL served as an antigen negative control target, and LCL-OKT3 established the maximum capacity of all CTL lines for cytolytic lysis. Graph titles indicate T cell effector lines tested, which include the autologous UPN033 parental CD8+ CTL bulk line (UPN033 CTL) and CD8+ IL13-zetakine+ CTL clone 3C12 (UPN033 IL13zeta+ CTL), and an allogeneic CD8+ IL13-zetakine+ CTL clone 2D7 (HD003 IL13zeta+ CTL). Mean ± S.D. values of 6 wells are depicted. (B) IFN-γ and TNF-α produced by the indicated CD8+ T cell lines after overnight co-culture with tumor targets described in (A). Mean ± S.D. values of 3 replicate measurements from a representative experiment is depicted. (C) Inhibition of PBT015-UPN033 TS driven IFN-γ and TNF-α produced by CD8+ IL13-zetakine+ CTL clone 3C12 as in (B) upon pre-incubation of the CTL with increasing concentrations of blocking rat anti-human IL13 antibody (left panel) or PBT015-UPN033 TS target cells with rhIL13 (right panel). (D) CRA measuring lysis of IL13Rα2neg glioma lines PBT003-4 TS and T98 cells versus IL13Rα2pos U251T by the indicated CD8+ IL13-zetakine+ CTL at increasing E:T ratios. Mean ± S.D. values of wells (n=6) are depicted.
We next evaluated IL13Rα2 on stem-like TS lines and found that expression was highly variable between tumor specimens, with a subset of TSs (i.e., PBT015-UPN033, PBT017-4 and PBT030) expressing significant levels of IL13Rα2 (>70% positive by flow cytometry), and approximately half of the tumor lines (i.e., PBT003-4, PBT008, and PBT009-2) not expressing detectable levels of this receptor by either flow cytometry or Western (Fig. 2D, E, top panels). IL13Rα2 transcript levels, as measured by RT-qPCR, correlated with the observed IL13Rα2 protein expression (Fig. 2C). Our observations are thus in agreement with previous studies showing that the IL13Rα2 receptor is expressed by a subset of patient glioblastoma tumor samples [16, 34].
An expanded normal fetal brain neural stem cell line did not express IL13Rα2 as assessed by flow cytometry and RT-qPCR (Fig. 2C and D). This observation suggests that the IL13Rα2 receptor is not expressed by normal neural stem cells, and is in concordance with previous reports that this receptor is not expressed at significant levels in normal brain tissue [15–17, 35].
Significantly, we find that IL13Rα2 is expressed independently of glioma differentiation status. As exemplified by both the IL13Rα2pos PBT015-UPN033, PBT017-4, PBT030 lines, receptor expression is maintained on the stem-like TS (CD133pos Olig2pos), the 7–14 day serum-differentiated (GFAPpos) (DIF), and the long-term serum-expanded cell populations (ADH) (Fig. 2D, E). A small decrease in IL13Rα2 levels was consistently observed following short-term differentiation, but not after long-term growth in serum-containing media (comparing DIF versus ADH), possibly due to the withdrawal of EGF mitogen [36]. Reciprocally, IL13Rα2neg primary lines (PBT003-4, PBT008 and PBT009-2) do not up-regulate IL13Rα2neg upon differentiation and growth in serum-containing media (Fig. 2D, E). We conclude that while IL13Rα2 expression by high-grade gliomas is heterogeneous between different tumor samples, its expression on any given low-passage glioma line is independent of cell differentiation status. Thus, these data suggest that, for gliomas expressing IL13Rα2, therapeutic strategies targeting this receptor could potentially eliminate the stem-like brain tumor sub-population. These studies also indicate the presence of glioma stem-like tumor initiating populations that do not express IL13Rα2, as detected for the IL13Rα2neg tumors.
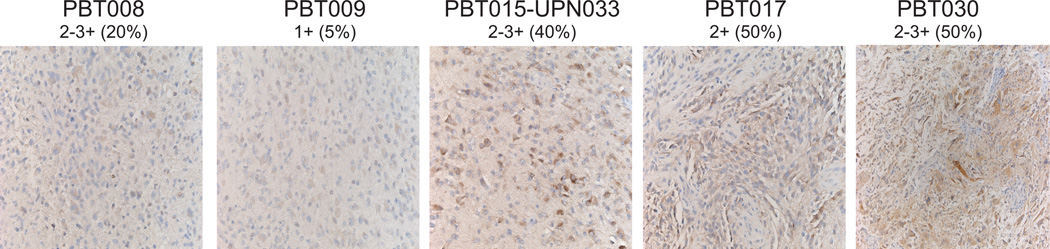
To assess the extent to which expression of IL13Rα2 on expanded primary cell lines correlates with the originating patient tumor, IL13Rα2 immunohistochemistry (IHC) was performed on paraffin-embedded patient tumor tissue. As shown in Fig. 3, patient tumors with the highest overall IL13Rα2 expression levels (≥40% of cells positive) as detected by IHC (PBT015-UPN033, PBT017 and PBT030), generated both TS and DIF/ADH lines with correspondingly high IL13Rα2 expression (compare to Fig. 2D, E). Likewise, patient tumors with low IL13Rα2 levels (≤20% positive cells) gave rise to cell lines that lacked receptor expression (PBT008 and PBT009). Importantly, these findings indicate that expression levels of IL13Rα2 on expanded primary glioma cell lines are consistent with its expression by the originating patient tumor. However, on a cell-by-cell basis, IL13Rα2 expression levels on glioma cells in situ were more variable, as detected by IHC, than those of the corresponding donor-derived TS or ADH cell lines (Fig. 2 vs. Fig. 3) [16, 35]. This difference may be explained by the more heterogeneous cellular composition of glioma tumors in situ.
Figure 3. IL13Rα2 expression on primary patient-derived glioma specimens.
IHC detection of IL13Rα2 on paraffin-embedded patient tumor tissue. Sections where scored blindly by a Neuropathologist for staining intensity (0 not detected; 1+ low; 2+ moderate; 3+ high), and percentages of positive cells are indicated.
IL13Rα2 expression renders GSCs susceptible to IL13-zetakine-mediated T cell killing
We next addressed whether IL13Rα2pos GSC and differentiated tumor lines display comparable sensitivity to CAR-engineered CTL mediated killing. For these studies, primary human IL13-zetakine+ CD8+ CTL lines (Supp Fig. S2A, B) were evaluated for their ability to kill TS and matched differentiated glioma lines in vitro. We observed that autologous (UPN033) or allogeneic (HD003) IL13-zetakine+ T cell clones efficiently lysed IL13Rα2pos PBT015-UPN033 stem-like TSs, as assessed by chromium-release assay (Fig. 4A). For both autologous and allogeneic CTLs, TSs were killed at least as well as matched serum-differentiated (DIF) or serum-expanded (ADH) low-passage primary lines, or established glioma line U87 (average difference in cytotoxicity at all E:T ratios 17% ± 9% with killing of TS ≥ DIFF/ADH lines). Lymphoblastic (LCL) targets engineered to express the membrane bound agonistic antibody scFv-OKT3 (LCL-OKT3), which activates T cells via engagement of the CD3 complex, served as a reference target denoting the maximal activation potential of a T cell line. To establish that the capacity of IL13-zetakine CTLs to target and kill IL13Rα2pos GSCs is not specific to a particular TS line, we demonstrated in a similar set of experiments that IL13Rα2pos PBT017-4 and PBT030 TS, DIF, and ADH cells were also recognized and killed independently of differentiation status (Supp. Fig S3). In all cases the stem-like TS lines were killed with comparable potency as the serum differentiated lines.
Following engagement of TS, DIF, ADH or U87 targets, IL13-zetakine+ CTL clones were also activated to produce Tc1 cytokines interferon-γ (INF-γ) and tumor necrosis factor-α (TNF-α) (Fig. 4B, Supp. Fig. S4). CTL co-culture with PBT015-UPN033 TSs resulted in slightly less Tc1 cytokine production as compared to serum-differentiated (DIF) cells (average± S.D. decrease in INF-γ for TS versus ADH and DIF is 42±7% and 14±2%, respectively; average decrease in TNF-α for TS versus ADH and DIF is 58±2% and 45±13%, respectively). This decrease in T cell mediated INF-γ and TNF-α cytokine release is observed on engagement of all IL13Rα2pos primary glioma lines tested (average 2–3 fold decrease) (Supp. Fig. S4).
Several lines of evidence confirm that the IL13-zetakine+ CTL killing and Tc1 cytokine responses we observed are specific to engagement of IL13Rα2 tumor antigen. First, IL13-zetakine+ CTL clones were not activated for killing or cytokine production when co-incubated with the IL13Rα2neg PBT003-4 TS and T98 glioma lines or the IL13Rα2neg LCL line (Fig. 4A, B, D, and data not shown). Second, blocking CAR-IL13Rα2 engagement by either pre-incubation of PBT015-UPN033 TS targets with recombinant human IL13 (rh-IL13), or IL13-zetakine+ CTL with anti-IL13 antibody eliminated cytokine production (Fig. 4C). Third, the parental UPN033 bulk CTL line, which is not engineered to express the IL13-zetakine CAR, displayed negligible levels of killing (<10% 51Cr-release) and cytokine production (<30 pg/ml INF-γ and <5 pg/ml TNF-α) when challenged with PBT015-UPN033 tumor targets.
Our findings demonstrate that expression of the IL13Rα2 tumor associated antigen is necessary for IL13-zetakine+ CTL killing. Importantly these data establish that both IL13Rα2pos GSCs and differentiated cells are targeted and killed by IL13-zetakine engineered CTLs, and therefore cells with stem/progenitor-like properties are not intrinsically resistant to CTL-mediated killing.
IL13-zetakine+ CTL can ablate the tumor initiating activity of IL13Rα2pos GSCs in vivo
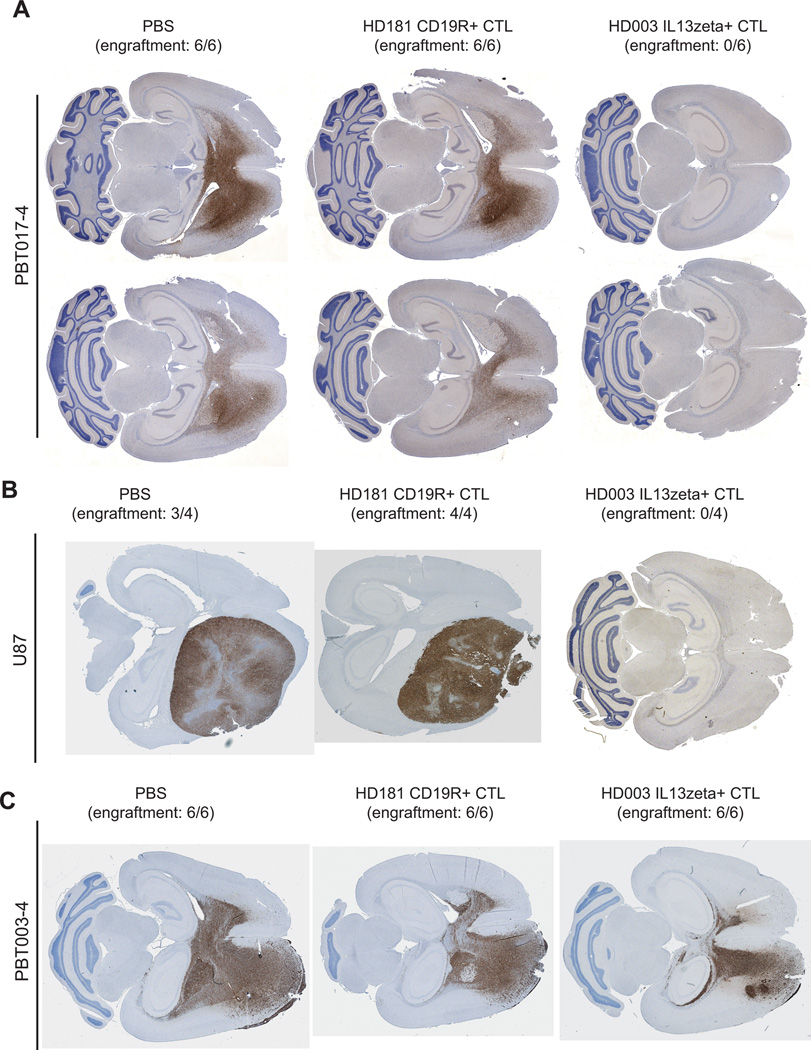
A hallmark characteristic of GSCs is their capacity to initiate in vivo tumor formation at low cell numbers. To address the possibility that a minor tumor-initiating subpopulation of IL13Rα2pos cells may evade IL13-zetakine-mediated recognition, an in vivo tumor engraftment assay was performed. This assay establishes that capacity of CTL to eliminate glioma tumor initiating populations (i.e. the functional definition of GSCs), by providing an in vivo read-out of cell populations that resist CTL killing (see Fig. 6 of ref. [9] in which antigen-negative tumor populations evaded CTL recognition and initiated tumor). For this study, PBT017-4 TSs were co-injected i.c. into NOD-scid mice with either IL13-zetakine+ CTL, or a non-specific CTL line expressing a CD19-specific CAR, or PBS. Because as few as 100 PBT017-4 TS cells can initiate highly invasive tumors in NOD-scid mice [9], this assay is expected to detect a minor tumor-initiating population (<0.1%) resistant to IL13-zetakine-mediated CTL killing. We observed that co-injection of IL13-zetakine+ CTL, but not PBS or control CD19R+ CTL, ablated the engraftment potential of PBT017-4 cells (Fig. 5A). Similarly, IL13-zetakine+ CTL, but not PBS or control CD19R+ CTL, also ablated the tumor-initiating potential of the established glioma cell line U87 grown under differentiating conditions (serum-containing media) (Fig 5B). As a control for antigen specificity, we demonstrate that IL13-zetakine+ CTL do not ablate the tumor initiating activity of the IL13Rα2neg line, PBT003 TSs (Fig 5C), consistent with the lack of in vitro killing of PBT003 when co-cultured with IL13-zetakine CTL (Fig 4D). This study demonstrated that IL13-zetakine+ CTL can eliminate the tumor initiating activity of both IL13Rα2pos GSC and differentiated subpopulations.
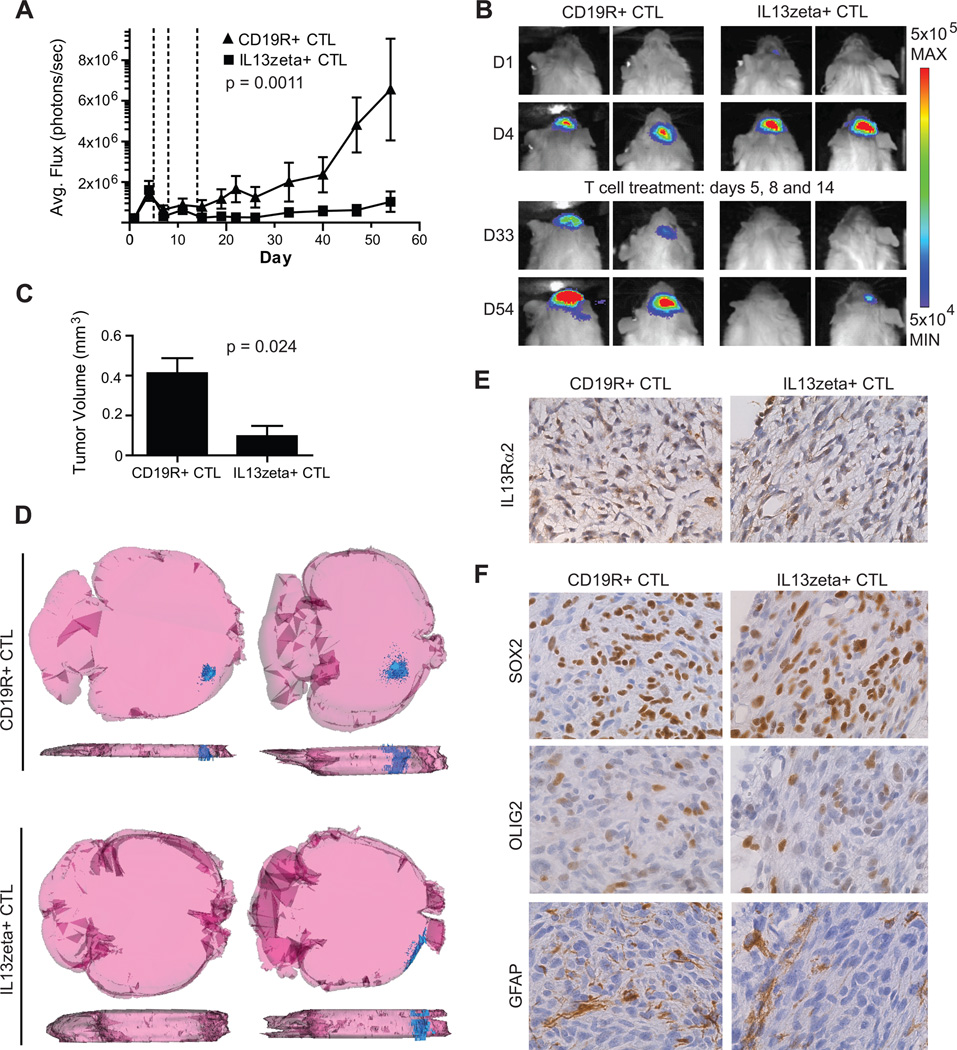
Figure 6. Regression of established GSC-initiated xenografts after adoptive transfer of IL13-zetakine+ T cells.
(A) EGFP-ffLuc+ PBT030-2 TSs (1×105) were stereotacitcally implanted into the right forebrain of NSG mice. On days 5, 8 and 14 (dotted vertical lines), mice received either 2×106 IL13-zetakine+ CTL clone 2D7 (HD003 IL13zeta+ CTL) (n=10) or CD19R+ CTL clone E8 (HD181 CD19R+ CTL) (n=8). Quantification of tumor growth kinetics using Xenogen Living Image to measure average ffLuc flux (photons/sec) demonstrates that IL13-zetakine+ CTLs induce tumor growth regression when compared with CD19R+ CTLs (p = 0.0011, two-way ANOVA with repeated natural log transformed measures on time, days 15–54). (B) Representative Xenogen images for two mice at days 1 and 4 before T cell administration and at days 33 and 54 post T cell treatment. (C, D, E, F) Xenograft tumors (i.c.) of PBT017-4 (1×105) were treated as described in (A) on days 5, 8 and 13. On day 28 (15 days post last T cell administration) mice brains were harvested and tumor volume was quantified by IHC. (C) Graph depicts the mean tumor volume (mm3) ± standard error for IL13-zetakine+ CTL (n=4) versus CD19R+ CTL (n=4) treated tumors (p = 0.024, two-tailed Student’s t-test). (D) The smallest (left) and largest (right) reconstructed tumors (blue pseudo-color) from each group are shown from both the dorsal (top) and sagittal (bottom) views. (E) anti-IL13Rα2 IHC, and (F) anti-SOX2, anti-OLIG2 and anti-GFAP IHC on paraffin sections of persisting tumors following adoptive transfer of glioma-specific IL13-zetakine+ CTL and control CD19R+ CTLs.
Figure 5. IL13Rα2-specific CTLs ablate the tumor initiation population of IL13Rα2-expressing GSCs.
(A) PBT017-4 TS (2×105) were co-injected i.c. with the specified CTL (2×106) or PBS into NOD-scid mice; n = 6 mice per group. Mice were euthanized after 8 weeks, and harvested brains were analyzed by IHC for tumor engraftment using anti-human nestin (number of mice with engrafted tumors per group of 6 is indicated). Representative images from 2 mice per group are depicted (tiled horizontal brain sections). (B) U87 cells (2×105), and (C) PBT003-4 TS cells (2×105) were co-injected i.c. with CAR+ CTLs or PBS in NOD-scid mice as described in (A)
Regression of established GSC TS-initiated xenografts after adoptive transfer of IL13-zetakine+ T cells
We next evaluated the capacity of IL13-zetakine+ CTL to induce regression of established GSC TS-initiated tumors. For these studies we examined the anti-tumor efficacy of IL13-zetakine+ T cells against two IL13Rα2pos GSC TS lines, PBT030-2 and PBT017-4 (Fig. 2 and Supp. Fig S5). To facilitate imaging of tumor growth kinetics, PBT030-2 TSs were engineered by lentiviral transduction to express a fusion protein consisting of EGFP and firefly luciferase (ffLuc) (EGFP-ffLuc) [9]. EGFP-ffLuc+ PBT030 or non-engineered PBT017-4 TS cells were orthotopically implanted into the right forebrain of NOD-scid IL2Rγnull (NSG) mice. Five days later, after tumor establishment, mice were treated i.c. with three infusions of either IL13-zetakine+ CD8+ CTL clone 2D7 or control CD19R+ CD8+ CTL clone E8. By comparing ffLuc+ tumor flux over time (PBT030-2; Fig. 6A and 6B), and by quantifying tumor volume 15 days after the last T cell treatment by IHC (PBT017-4; Fig. 6C, and 6D), we demonstrate that IL13-zetakine+ CTL, as compared to control CD19R+ CTL, mediate statistically significant anti-glioma activity against both PBT030-2 and PBT017-4 established tumors.
The ability of IL13-zetakine CTL to regress GSC-initiated established glioblastoma tumors is consistent with our previous observations that IL13-zetakine+ CTL can kill IL13Rα2pos TS cells (Fig. 4) and ablate their tumor initiating activity (Fig. 5). For those mice in which residual tumor was detected following treatment with IL13-zetakine+ CTL, we sought to understand the etiology of tumor escape by evaluating the expression of IL13Rα2 as well as stem (Sox2 and Olig2) and differentiated (GFAP) markers by IHC 15 days after the last T cell treatment (day 28 post tumor injection). We found that IL13-zetakine+ CTL and control CD19R+ CTL treated tumors express comparable levels IL13Rα2 (Fig. 6E), suggesting that residual tumors did not evade therapy due to antigen loss. At this 15 day time point, we were not able to detect any persisting CD3+ human T cells by IHC (data not shown). Also, we detect comparable levels of SOX2, Olig2 and GFAP (Fig. 6F), suggesting that there is no major difference in the frequency of stem-like versus differentiated cells in the recurrent tumor following IL13-zetakine+ CTL mediated tumor targeting. While the largest IL13-zetakine+ CTL treated tumor was found in the leptomeninges (Fig 6D), the significance of this engraftment pattern is not clear since this highly invasive PBT017-4 line (Fig. 5) is known to engraft at this anatomical site. Taken together these data indicate that exposure to IL13-zetakine+ CTL has the capacity to reduce tumor growth and tumor burden of established IL13Rα2-expressing tumors. At the same time, these data also suggest that a more potent CAR+ T cell capable of sustained persistence may be required to completely eliminate all IL13Rα2-expressing tumor cells.
Discussion
While immunotherapy strategies targeting IL13Rα2 for brain tumors are being clinically pursued [21–24] based on its selective expression on malignant versus normal brain tissue [17, 18], the power of IL13Rα2-directed therapies will depend in part on the ability of these approaches to be effective against the highly tumorigenic glioma cancer stem-like population [3, 4]. Our data provide direct evidence that IL13Rα2 expression is not limited to differentiated glioma cells, and that IL13Rα2-targeting can potentially eliminate the refractory GSC component of malignant gliomas. We demonstrate that GSC TSs derived from IL13Rα2pos glioma tumors express IL13Rα2, and that its expression renders the IL13Rα2pos GSC population susceptible to IL13-zetakine+ CAR-engineered T cell cytolytic lysis. Importantly, in vitro GSC TSs were killed at equivalent potency as matched differentiated glioma lines. We also show that IL13-zetakine+ CTL ablate the in vivo tumor initiating activity of IL13Rα2pos GSCs and, further, mediate robust anti-tumor activity and limit progression of established IL13Rα2pos GSC TS-initiated intracranial tumors in mice.
While our work and others have demonstrated that GSCs are intrinsically susceptible to effector T cell killing [7, 9, 10], mechanisms to suppress and/or evade immune function and effector T cell killing are likely employed by GSCs. Recent studies suggest that GSCs may reduce T cell activation-dependent proliferation and down-modulate T cell activation-dependent cytokine production [12, 37]. We also find that GSC TSs are less potent at stimulating IL13-zetakine+ CTLs for antigen-dependent INF-γ and TNF-α cytokine production- (Fig. 4; Supp. Fig S4). The underlying mechanism of these compromised functionalities and the consequences for anti-tumor efficacy remain to be resolved. In addition, the malignant stem cell niche is associated with secreted TGF-β and VEGF, as well as activated STAT3 [12], important signals known to inhibit immune responses and thus may protect GSCs in established tumors from efficient T cell eradication [38–40]. Despite these hurdles, our findings that CD8+ CTLs can be engineered to successfully kill the otherwise therapeutically resistant GSC population suggests that efforts to overcome these obstacles are worthwhile.
Clinical trials for recurrent high-grade gliomas using IL13-zetakine redirected CTLs are in early feasibility/safety stages, and while transient tumor regressions have been observed, sustained regressions are still an unrealized outcome (Jensen unpublished and [22, 24]). The present study focused on the potential barrier of GSCs as a therapeutically resistant reservoir of tumor cells. We provide evidence that disease recurrence following IL13Rα2 directed therapies is not due to the absence of IL13Rα2 expression by all GSC subpopulations, but rather that other mechanisms of escape may also be at play. Further, we demonstrate that IL13-zetakine CTLs can target and kill IL13Rα2pos GSCs and regress established GSC-initiated tumors. However, for established tumors, IL13Rα2-expressing glioma populations were not completely eliminated suggesting that a more powerful T cell product is needed. To this end, CAR-engineered T cell lines optimized for T cell persistence and/or serial tumor killing are under development [26, 41, 42].
Additionally, clinical targeting of IL13Rα2pos cells may selectively eliminate not only malignant cells, but also cells within the micro-environment that are involved in immune evasion. Of particular interest, tumor infiltrating macrophages (CD11b high/Gr-1 intermediate) have been shown to up-regulate cell surface IL13Rα2 expression in the tumor micro-environment, and are stimulated by IL-13 to secrete TGF-β, resulting in inhibition of antigen-specific CTL function [43]. Blocking induction of IL13Rα2 on tumor-infiltrated macrophages correspondingly inhibits TGF-β production, and restores the anti-tumor activity of CD8+ T cells. In these ways, targeting IL13Rα2 expressed by other cells in the tumor microenvironment may also enhance the efficacy of clinically targeting this receptor.
Importantly, the heterogeneity of IL13Rα2 receptor expression by high-grade gliomas, rather than persistence of refractory GSC populations, is anticipated to be a critical barrier to overcome in order to achieve improved clinical responses (Fig 2 and [16, 34, 44, 45]). A guiding principle now emerging from a variety of clinical trials suggests that immunotherapeutic approaches targeting single antigens will not be sufficient for durable long-term anti-tumor responses. Our data demonstrating that IL13Rα2 is expressed by a subset of glioma stem-like initiating populations susceptible to cell immunotherapy highlight the relevance of translational strategies targeting IL13Rα2 for malignant glioma, particularly when incorporated into combinatorial targeting approaches.
Supplementary Material
Translational Relevance.
Patient-to-patient heterogeneity of malignant gliomas, together with the presence of the glioma stem-like cancer initiating cells (GSCs), thought to be responsible for disease progression and recurrence, have proven to be barriers to disease eradication. In light of these challenges, our study focused on the utility of IL13Rα2-directed therapies for targeting the tumorigenic GSC population of high-grade gliomas. Our findings provide evidence that for the subset of patients with IL13Rα2-positive tumors, immune-based therapies targeting IL13Rα2 have the potential to eliminate both the GSC and bulk differentiated populations.
Acknowledgements
We thank Gustavo Mendez, COH Cytogenetics, and Pathology shared resources for technical assistance, Suzette Blanchard for statistical advice, Dr. Julie Ostberg for manuscript preparation, and Vaidehi Mahadev for helpful discussions. This research was supported by NCI (RO1 CA103959), NIH (CCSG P30 CA 33572), General Clinical Research Center (M01 RR00043), and a generous donation from Joan and Larry Flax.
Footnotes
MCJ is an inventor of licensed patents and equity holder in ZetaRx, Inc a licensee of these patents. Other authors have no conflicts of interest to disclose.
References
- 1.Dirks PB. Brain tumor stem cells: bringing order to the chaos of brain cancer. J Clin Oncol. 2008;26:2916–2924. doi: 10.1200/JCO.2008.17.6792. [DOI] [PubMed] [Google Scholar]
- 2.Li Z, Wang H, Eyler CE, Hjelmeland AB, Rich JN. Turning cancer stem cells inside out: an exploration of glioma stem cell signaling pathways. J Biol Chem. 2009;284:16705–16709. doi: 10.1074/jbc.R900013200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hadjipanayis CG, Van Meir EG. Tumor initiating cells in malignant gliomas: biology and implications for therapy. J Mol Med. 2009;87:363–374. doi: 10.1007/s00109-009-0440-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou BB, Zhang H, Damelin M, Geles KG, Grindley JC, Dirks PB. Tumour-initiating cells: challenges and opportunities for anticancer drug discovery. Nat Rev Drug Discov. 2009;8:806–823. doi: 10.1038/nrd2137. [DOI] [PubMed] [Google Scholar]
- 5.Eyler CE, Rich JN. Survival of the fittest: cancer stem cells in therapeutic resistance and angiogenesis. J Clin Oncol. 2008;26:2839–2845. doi: 10.1200/JCO.2007.15.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ji J, Black KL, Yu JS. Glioma stem cell research for the development of immunotherapy. Neurosurg Clin N Am. 2010;21:159–166. doi: 10.1016/j.nec.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed N, Salsman VS, Kew Y, Shaffer D, Powell S, Zhang YJ, et al. HER2-specific T cells target primary glioblastoma stem cells and induce regression of autologous experimental tumors. Clin Cancer Res. 2010;16:474–485. doi: 10.1158/1078-0432.CCR-09-1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmidt P, Kopecky C, Hombach A, Zigrino P, Mauch C, Abken H. Eradication of melanomas by targeted elimination of a minor subset of tumor cells. Proc Natl Acad Sci U S A. 2011;108:2474–2479. doi: 10.1073/pnas.1009069108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown CE, Starr R, Martinez C, Aguilar B, D'Apuzzo M, Todorov I, et al. Recognition and killing of brain tumor stem-like initiating cells by CD8+ cytolytic T cells. Cancer Res. 2009;69:8886–8893. doi: 10.1158/0008-5472.CAN-09-2687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castriconi R, Daga A, Dondero A, Zona G, Poliani PL, Melotti A, et al. NK cells recognize and kill human glioblastoma cells with stem cell-like properties. J Immunol. 2009;182:3530–3539. doi: 10.4049/jimmunol.0802845. [DOI] [PubMed] [Google Scholar]
- 11.Wu A, Wiesner S, Xiao J, Ericson K, Chen W, Hall WA, et al. Expression of MHC I and NK ligands on human CD133+ glioma cells: possible targets of immunotherapy. J Neurooncol. 2007;83:121–131. doi: 10.1007/s11060-006-9265-3. [DOI] [PubMed] [Google Scholar]
- 12.Wei J, Barr J, Kong LY, Wang Y, Wu A, Sharma AK, et al. Glioblastoma cancer-initiating cells inhibit T-cell proliferation and effector responses by the signal transducers and activators of transcription 3 pathway. Mol Cancer Ther. 2010;9:67–78. doi: 10.1158/1535-7163.MCT-09-0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wei J, Barr J, Kong LY, Wang Y, Wu A, Sharma AK, et al. Glioma-associated cancerinitiating cells induce immunosuppression. Clin Cancer Res. 2010;16:461–473. doi: 10.1158/1078-0432.CCR-09-1983. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.Wu A, Wei J, Kong LY, Wang Y, Priebe W, Qiao W, et al. Glioma cancer stem cells induce immunosuppressive macrophages/microglia. Neuro Oncol. 2010;12:1113–1125. doi: 10.1093/neuonc/noq082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Debinski W, Gibo DM, Hulet SW, Connor JR, Gillespie GY. Receptor for interleukin 13 is a marker and therapeutic target for human high-grade gliomas. Clin Cancer Res. 1999;5:985–990. [PubMed] [Google Scholar]
- 16.Jarboe JS, Johnson KR, Choi Y, Lonser RR, Park JK. Expression of interleukin-13 receptor alpha2 in glioblastoma multiforme: implications for targeted therapies. Cancer Res. 2007;67:7983–7986. doi: 10.1158/0008-5472.CAN-07-1493. [DOI] [PubMed] [Google Scholar]
- 17.Joshi BH, Puri RA, Leland P, Varricchio F, Gupta G, Kocak M, et al. Identification of interleukin-13 receptor alpha2 chain overexpression in situ in high-grade diffusely infiltrative pediatric brainstem glioma. Neuro Oncol. 2008;10:265–274. doi: 10.1215/15228517-2007-066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kawakami M, Kawakami K, Takahashi S, Abe M, Puri RK. Analysis of interleukin-13 receptor alpha2 expression in human pediatric brain tumors. Cancer. 2004;101:1036–1042. doi: 10.1002/cncr.20470. [DOI] [PubMed] [Google Scholar]
- 19.Kahlon KS, Brown C, Cooper LJ, Raubitschek A, Forman SJ, Jensen MC. Specific recognition and killing of glioblastoma multiforme by interleukin 13-zetakine redirected cytolytic T cells. Cancer Res. 2004;64:9160–9166. doi: 10.1158/0008-5472.CAN-04-0454. [DOI] [PubMed] [Google Scholar]
- 20.Debinski W, Gibo DM, Obiri NI, Kealiher A, Puri RK. Novel anti-brain tumor cytotoxins specific for cancer cells. Nat Biotechnol. 1998;16:449–453. doi: 10.1038/nbt0598-449. [DOI] [PubMed] [Google Scholar]
- 21.Kawakami K, Terabe M, Kioi M, Berzofsky JA, Puri RK. Intratumoral therapy with IL13-PE38 results in effective CTL-mediated suppression of IL-13Ralpha2-expressing contralateral tumors. Clin Cancer Res. 2006;12:4678–4686. doi: 10.1158/1078-0432.CCR-06-0192. [DOI] [PubMed] [Google Scholar]
- 22.Kunwar S, Chang S, Westphal M, Vogelbaum M, Sampson J, Barnett G, et al. Phase III randomized trial of CED of IL13-PE38QQR vs Gliadel wafers for recurrent glioblastoma. Neuro Oncol. 2010;12:871–881. doi: 10.1093/neuonc/nop054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saka M, Amano T, Kajiwara K, Yoshikawa K, Ideguchi M, Nomura S, et al. Vaccine therapy with dendritic cells transfected with Il13ra2 mRNA for glioma in mice. J Neurosurg. 2009;113:270–279. doi: 10.3171/2009.9.JNS09708. [DOI] [PubMed] [Google Scholar]
- 24.Yaghoubi SS, Jensen MC, Satyamurthy N, Budhiraja S, Paik D, Czernin J, et al. Noninvasive detection of therapeutic cytolytic T cells with 18F-FHBG PET in a patient with glioma. Nat Clin Pract Oncol. 2009;6:53–58. doi: 10.1038/ncponc1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cooper LJ, Topp MS, Serrano LM, Gonzalez S, Chang WC, Naranjo A, et al. T-cell clones can be rendered specific for CD19: toward the selective augmentation of the graft-versus-B-lineage leukemia effect. Blood. 2003;101:1637–1644. doi: 10.1182/blood-2002-07-1989. [DOI] [PubMed] [Google Scholar]
- 26.Wang X, Berger C, Wong CW, Forman SJ, Riddell SR, Jensen MC. Engraftment of human central memory-derived effector CD8+ T cells in immunodeficient mice. Blood. 2011;117:1888–1898. doi: 10.1182/blood-2010-10-310599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pollard SM, Yoshikawa K, Clarke ID, Danovi D, Stricker S, Russell R, et al. Glioma stem cell lines expanded in adherent culture have tumor-specific phenotypes and are suitable for chemical and genetic screens. Cell Stem Cell. 2009;4:568–580. doi: 10.1016/j.stem.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 28.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 29.Stastny MJ, Brown CE, Ruel C, Jensen MC. Medulloblastomas expressing IL13Ralpha2 are targets for IL13-zetakine+ cytolytic T cells. J Pediatr Hematol Oncol. 2007;29:669–677. doi: 10.1097/MPH.0b013e3181468c68. [DOI] [PubMed] [Google Scholar]
- 30.Fiala JC. Reconstruct: a free editor for serial section microscopy. J Microsc. 2005;218:52–61. doi: 10.1111/j.1365-2818.2005.01466.x. [DOI] [PubMed] [Google Scholar]
- 31.Hodgson JG, Yeh RF, Ray A, Wang NJ, Smirnov I, Yu M, et al. Comparative analyses of gene copy number and mRNA expression in glioblastoma multiforme tumors and xenografts. Neuro Oncol. 2009;11:477–487. doi: 10.1215/15228517-2008-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu AH, Low WC. Molecular cloning and identification of the human interleukin 13 alpha 2 receptor (IL-13Ra2) promoter. Neuro Oncol. 2003;5:179–187. doi: 10.1215/S1152-8517-02-00051-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ogden AT, Waziri AE, Lochhead RA, Fusco D, Lopez K, Ellis JA, et al. Identification of A2B5+CD133- tumor-initiating cells in adult human gliomas. Neurosurgery. 2008;62:505–514. doi: 10.1227/01.neu.0000316019.28421.95. discussion 14-5. [DOI] [PubMed] [Google Scholar]
- 34.Saikali S, Avril T, Collet B, Hamlat A, Bansard JY, Drenou B, et al. Expression of nine tumour antigens in a series of human glioblastoma multiforme: interest of EGFRvIII, IL- 13Ralpha2, gp100 and TRP 2 for immunotherapy. J Neurooncol. 2007;81:139–148. doi: 10.1007/s11060-006-9220-3. [DOI] [PubMed] [Google Scholar]
- 35.Wykosky J, Gibo DM, Stanton C, Debinski W. Interleukin-13 receptor alpha 2, EphA2, and Fos-related antigen 1 as molecular denominators of high-grade astrocytomas and specific targets for combinatorial therapy. Clin Cancer Res. 2008;14:199–208. doi: 10.1158/1078-0432.CCR-07-1990. [DOI] [PubMed] [Google Scholar]
- 36.Hu N, Gibo DM, Debinski W. Cytokine up-regulation of IL13Rα2 in GBM cells leads to an increased potency of recombinant IL13 cytotoxin. Cancer Therapy. 2005;3:531–542. [Google Scholar]
- 37.Di Tomaso T, Mazzoleni S, Wang E, Sovena G, Clavenna D, Franzin A, et al. Immunobiological characterization of cancer stem cells isolated from glioblastoma patients. Clin Cancer Res. 2010;16:800–813. doi: 10.1158/1078-0432.CCR-09-2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kandalaft LE, Motz GT, Busch J, Coukos G. Angiogenesis and the Tumor Vasculature as Antitumor Immune Modulators: The Role of Vascular Endothelial Growth Factor and Endothelin. Curr Top Microbiol Immunol. 2011;344:129–148. doi: 10.1007/82_2010_95. [DOI] [PubMed] [Google Scholar]
- 39.Thomas DA, Massague J. TGF-beta directly targets cytotoxic T cell functions during tumor evasion of immune surveillance. Cancer Cell. 2005;8:369–380. doi: 10.1016/j.ccr.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 40.Yu H, Kortylewski M, Pardoll D. Crosstalk between cancer and immune cells: role of STAT3 in the tumour microenvironment. Nat Rev Immunol. 2007;7:41–51. doi: 10.1038/nri1995. [DOI] [PubMed] [Google Scholar]
- 41.Berger C, Jensen MC, Lansdorp PM, Gough M, Elliott C, Riddell SR. Adoptive transfer of effector CD8 T cells derived from central memory cells establishes persistent T cell memory in primates. J Clin Invest. 2008;118:294–305. doi: 10.1172/JCI32103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cartellieri M, Bachmann M, Feldmann A, Bippes C, Stamova S, Wehner R, et al. Chimeric antigen receptor-engineered T cells for immunotherapy of cancer. J Biomed Biotechnol. 2010;2010:956304. doi: 10.1155/2010/956304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fichtner-Feigl S, Terabe M, Kitani A, Young CA, Fuss I, Geissler EK, et al. Restoration of tumor immunosurveillance via targeting of interleukin-13 receptor-alpha 2. Cancer Res. 2008;68:3467–3475. doi: 10.1158/0008-5472.CAN-07-5301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Debinski W, Gibo DM, Slagle B, Powers SK, Gillespie GY. Receptor for interleukin 13 is abundantly and specifically over-expressed in patients with glioblastoma multiforme. Int J Oncol. 1999;15:481–486. doi: 10.3892/ijo.15.3.481. [DOI] [PubMed] [Google Scholar]
- 45.Debinski W, Miner R, Leland P, Obiri NI, Puri RK. Receptor for interleukin (IL) 13 does not interact with IL4 but receptor for IL4 interacts with IL13 on human glioma cells. J Biol Chem. 1996;271:22428–22433. doi: 10.1074/jbc.271.37.22428. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.