Abstract
OBJECTIVE
Current recommendations for the use of hemoglobin A1c (HbA1c) in diabetes screening and diagnosis aim to identify those at greatest risk for diabetic microvascular complications. However, there is current controversy regarding the clinical implications of ethnic differences in HbA1c values. The objective of this study was to determine whether the association between HbA1c and retinopathy differs by ethnic group in a representative sample of U.S. adults.
RESEARCH DESIGN AND METHODS
The study was a cross-sectional analysis of 2,945 non-Hispanic white, 1,046 non-Hispanic black, and 1,231 Hispanic American participants aged ≥40 years from the 2005–2008 National Health and Nutrition Examination Survey.
RESULTS
Among nondiabetic adults, the mean HbA1c was 5.5% in non-Hispanic whites, 5.7% in non-Hispanic blacks, and 5.6% in Hispanic Americans. Among those with diagnosed diabetes, mean HbA1c was 6.9% in non-Hispanic whites, 7.5% in non-Hispanic Blacks, and 7.7% in Hispanic Americans. Overall, non-Hispanic blacks had the highest prevalence of retinopathy. In multivariable logistic models, HbA1c clinical categories were strongly associated with prevalent retinopathy. However, the magnitude of the association did not differ by ethnic group (all P values for interaction ≥ 0.7). Similar results were observed with HbA1c modeled continuously (per one percentage point) and stratified by diabetes status (all P for interactions > 0.3).
CONCLUSIONS
We observed no ethnic differences in the association of HbA1c with retinopathy. These data do not support ethnic-specific cut points for HbA1c for diagnosis or screening of diabetes mellitus.
Hemoglobin A1c (HbA1c) was recently recommended for use in the diagnosis of diabetes (1,2). Recommended clinical categories for diabetes diagnosis using HbA1c largely are based on the established association of HbA1c with prevalent retinopathy (3–6) and evidence from clinical trials demonstrating that lowering HbA1c can reduce microvascular complications (7). Nonetheless, recent studies document persistent ethnic differences in HbA1c values (8–12), raising concerns that the performance of HbA1c may differ in certain subpopulations and that new recommendations for the use of HbA1c for diagnosis might be problematic in individuals of non-European ancestry (13–19). Data about the association of HbA1c with clinical outcomes in different ethnic groups are critical to inform this debate.
The objective of this study was to characterize the ethnic-specific associations between HbA1c and retinopathy in the U.S. population aged 40 years and older using data from the 2005–2008 National Health and Nutrition Examination Survey (NHANES) and to formally test for effect modification by ethnicity.
RESEARCH DESIGN AND METHODS
Study population
The NHANES is a cross-sectional, nationally representative survey of the U.S. civilian noninstitutionalized population conducted by the National Center of Health Statistics, Centers for Disease Control and Prevention (20). In this study, we included 2,945 non-Hispanic white, 1,046 non-Hispanic black, and 1,231 Hispanic American participants aged 40 years or older who had complete information on the variables of interest in the 2005–2008 NHANES. A review board for human subjects approved data collection procedures, and written informed consent was obtained from all study participants.
Measurements
HbA1c measurements were obtained using high-performance liquid chromatography standardized to the Diabetes Control and Complication Trial assay (20). Demographic information (including ethnicity, sex, education, and income), smoking history, and health history were determined by self-report. Height, weight, blood pressure, and lipids were measured using standard procedures (21,22). A history of diabetes was defined as self-reported diagnosis of diabetes (not during pregnancy for women) or current insulin use.
Retinal imaging was performed on individuals who were aged ≥40 years using a Canon Non-Mydriatic Retinal Camera CR6–45NM; participants with blindness, eye infections, or eye patches were excluded. Detailed information about methodology is available elsewhere (21,22). Briefly, two 45-degree nonmydriatic digital images of the retina were obtained from each eye, and graders at the University of Wisconsin Ocular Epidemiology Reading Center evaluated the images. Retinopathy level was determined as described by the Early Treatment Diabetic Retinopathy Study (EDTRS) and ranged from 10–80 (23). We defined “any retinopathy” as an EDTRS level of 14 or higher in the worse eye, thereby classifying individuals as having either no retinopathy or mild nonproliferative retinopathy or worse (21,22).
Statistical analysis
We used logistic regression models to evaluate the independent association between HbA1c (modeled in clinical categories and continuously) and prevalent retinopathy. We formally tested for interaction by ethnic group. Analyses were stratified by diabetes status, and prevalence estimates were age-standardized to the 2010 U.S. Census to obtain estimates of the proportion of individuals with retinopathy by HbA1c category and diabetes status.
Adjustment variables included age, sex, BMI, hypertension status, history of coronary heart disease, total cholesterol, educational attainment, income level, and smoking status. In analyses modeling HbA1c as a categorical variable, the sample was stratified using clinical categories of HbA1c (in those without diagnosed diabetes: <5.7%, 5.7–6.4%, and ≥6.5%; in those with diagnosed diabetes: <7% and ≥7%). The nondiabetic group with HbA1c values in the normal range (<5.7%) served as the reference group. Sensitivity analyses were conducted modeling HbA1c using deciles (tenths) (4,5) and using different EDTRS cut points to define retinopathy (23). P values for interactions were derived from Wald tests. All analyses incorporated the NHANES sample weights and accounted for the complex sample survey design using standard methods (20).
RESULTS
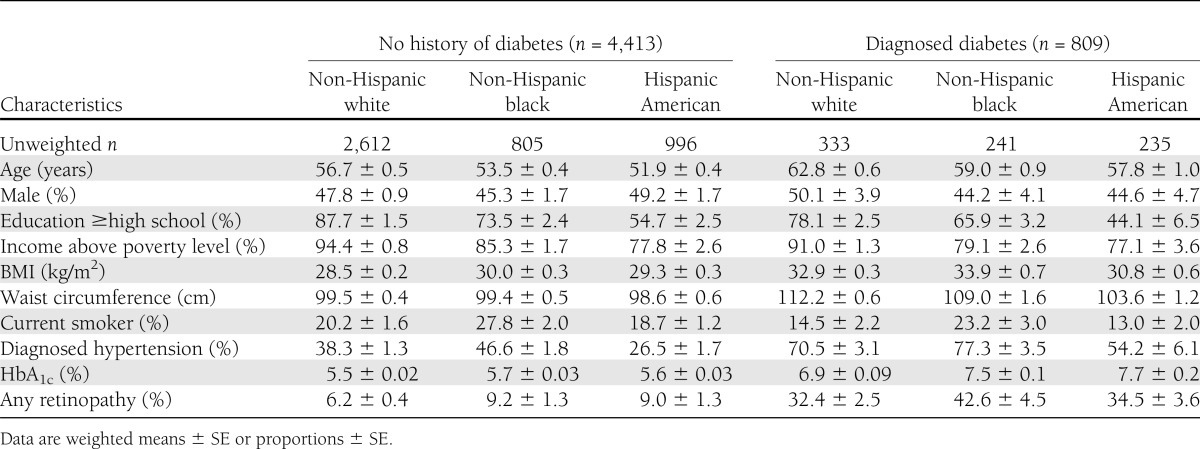
Overall, the mean age was 57 years, the population was 48% male, and the mean HbA1c was 5.7%. Details regarding population characteristics stratified by diabetes status and ethnicity are summarized in Table 1. Among nondiabetic adults, the mean HbA1c was 5.5% in non-Hispanic whites, 5.7% in non-Hispanic blacks (P < 0.001 compared with non-Hispanic whites), and 5.6% in Hispanic Americans (P = 0.002 compared with non-Hispanic whites). Among those with diagnosed diabetes, mean HbA1c was 6.9% in non-Hispanic whites, 7.5% in non-Hispanic Blacks (P = 0.002 compared with non-Hispanic whites), and 7.7% in Hispanic Americans (P < 0.001 compared with non-Hispanic whites). In the subgroup of individuals with diagnosed diabetes, the mean duration of diabetes was 10 years in non-Hispanic whites, 11 years in non-Hispanic blacks, and 9 years in Hispanics; there was no significant difference in mean duration of diabetes by ethnicity (P > 0.05 for each group compared with non-Hispanic whites).
Table 1.
Selected characteristics of U.S. adults aged ≥40 years, stratified by diagnosed diabetes status and ethnicity, NHANES 2005–2008
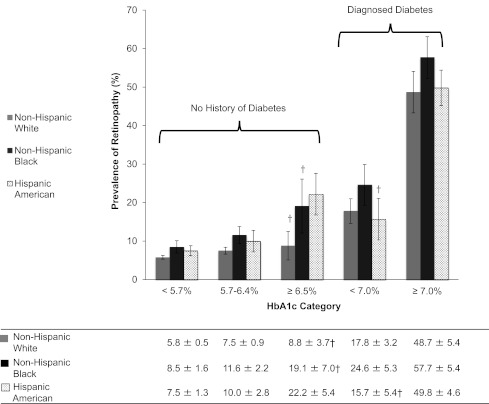
The prevalence estimates for retinopathy by ethnic group and diabetes status are shown in Fig. 1. Among those in the lowest HbA1c category (<5.7%) who were aged ≥40 years with no history of diabetes, the prevalence of retinopathy was 6% (95% CI, 5–7) in non-Hispanic whites, 9% (5–12) in non-Hispanic blacks, and 8% (5–10) in Hispanic Americans. The prevalence of retinopathy in persons with undiagnosed diabetes (HbA1c ≥6.5%) was 9% (1–17) in non-Hispanic whites, 19% (5–34) in non-Hispanic blacks, and 22% (11–33) in Hispanic Americans. In persons with diagnosed diabetes, the prevalence of retinopathy in those with HbA1c <7% was 18% (95% CI, 11–24) in non-Hispanic whites, 25% (95% CI, 14–35) in non-Hispanic blacks, and 16% (95% CI, 4–27) in Hispanic Americans. Finally, the prevalence of retinopathy in those with diagnosed diabetes and HbA1c ≥7% was 49% (37–60) in non-Hispanic whites, 57% (46–69) in non-Hispanic blacks, and 50% (40–59) in Hispanic Americans. The proportion of individuals with more severe retinopathy was higher among non-Hispanic black and Hispanic participants compared with non-Hispanic whites; the proportions of retinopathy severity scores by group are shown in Supplementary Fig. 1.
Figure 1.
Age-adjusted prevalence of any retinopathy by ethnic group and HbA1c category among U.S. adults aged ≥40 years, 2005–2008. Retinopathy was defined as an ETDRS level of 14 or greater (21,22). Estimates are weighted proportions ± SE and are age-standardized to the 2010 U.S. Census population. †Estimate may be unreliable because the SE is greater than 30% of the estimate.
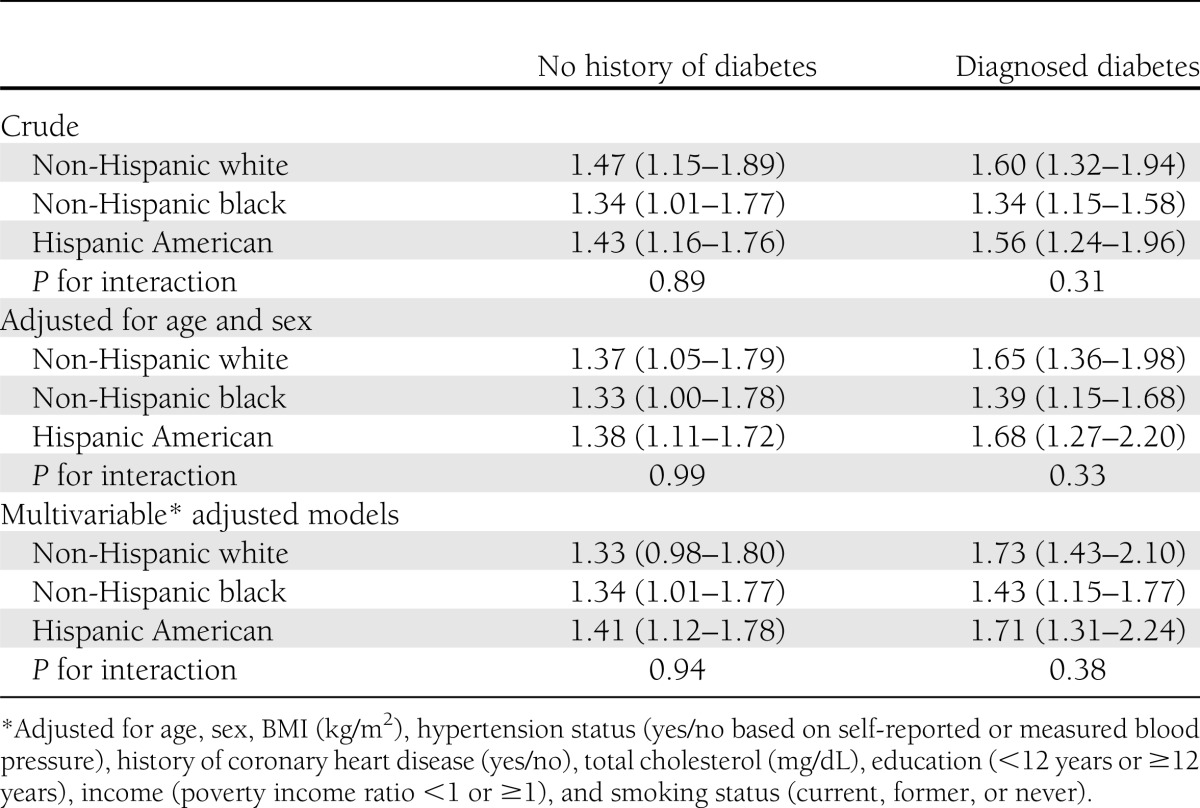
In crude and adjusted logistic models (Table 2), HbA1c categories were strongly associated with prevalent retinopathy. The magnitude of the association did not differ by ethnic group (all P for interactions ≥ 0.7). Similar results were observed in analyses with HbA1c modeled continuously (per one percentage point) and stratified by diabetes status (Table 3 and Supplementary Fig. 2). Additional adjustment for diabetes duration or insulin use in the subgroup of participants with diagnosed diabetes did not materially alter our results. Our results were similar in a sensitivity analysis examining the association of HbA1c categorized into tenths (Supplementary Fig. 3). Our results were also robust to different definitions of retinopathy (Supplementary Tables 1 and 2). Finally, results from linear regression models (log-transforming retinopathy score) and ordinal logistic regression models predicting retinopathy severity were also similar (results not shown).
Table 2.
Unadjusted and adjusted odds ratios for retinopathy by ethnicity, diagnosed diabetes status, and HbA1c category among adults aged ≥40 years, NHANES 2005–2008
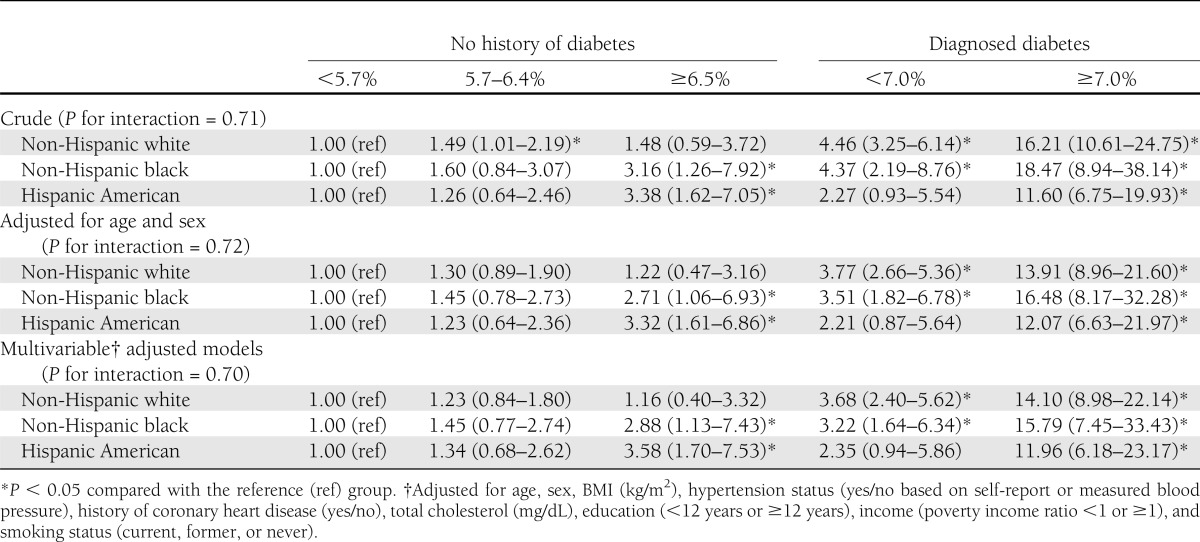
Table 3.
Odds ratios per one percentage point HbA1c for retinopathy by ethnicity and diabetes status among adults aged ≥40 years, NHANES 2005–2008
CONCLUSIONS
We found no ethnic differences in the association of HbA1c with prevalent retinopathy in this nationally representative sample of U.S. adults aged 40 years and older. Consistent with previous studies (9,24–27), the prevalence of retinopathy was substantially higher in non-Hispanic blacks and Hispanics compared with non-Hispanic whites. This may partially reflect ethnic disparities in the diagnosis of diabetes and management of hyperglycemia among individuals with diabetes. Consistent with previous analyses of NHANES data (12,28,29), we observed higher HbA1c values in non-Hispanic blacks and Hispanics compared with non-Hispanic whites. However, we found no evidence that ethnic group modified the relative association of HbA1c with prevalent retinopathy. These findings are consistent with other studies that have demonstrated similar patterns of association between HbA1c with microvascular conditions (6) and long-term vascular outcomes in non-Hispanic white and black populations (30). Our results were robust to different categorizations of HbA1c and definitions of retinopathy.
Current clinical diagnostic categories for HbA1c largely are based on cross-sectional analyses of the association of HbA1c with retinopathy (1,3,31), where the primary goal was to identify points along the continuum of HbA1c where the likelihood of microvascular abnormalities increase (4,6,26). Taken together, our results support the current guidelines for the use of HbA1c for the diagnosis of diabetes and suggest that current clinical cut points should be interpreted similarly in whites, blacks, and Hispanics. These results should help alleviate concerns regarding the use of HbA1c for diagnosis and monitoring of diabetes in diverse populations.
Important strengths of this study include the rigorous and standardized measurement of HbA1c, retinopathy, and covariates in NHANES. Our analyses included large numbers of non-Hispanic blacks and Hispanic Americans using nationally representative data from the U.S. civilian, noninstitutionalized population. Nonetheless, because retinopathy is relatively uncommon in the general population, our estimates for certain population subgroups (for example, non-Hispanics without diabetes and with HbA1c ≥6.5% and Hispanics with diagnosed diabetes and HbA1c <7%) are imprecise. Furthermore, because of the cross-sectional nature of this study, we are unable to establish the temporality of the observed associations.
The data presented do not support the contention that HbA1c is artifactually elevated in non-Hispanic black populations, as has been claimed by some experts. Indeed, the higher prevalence of retinopathy in non-Hispanic blacks without diagnosed diabetes and across HbA1c categories highlights a need for more aggressive screening and prevention efforts to mitigate microvascular complications in this group. Overall, our results support current recommendations for the use of HbA1c for diagnosis of diabetes, not only in non-Hispanic white populations, but also for non-Hispanic black and Hispanic individuals.
Supplementary Material
Acknowledgments
J.K.B. has received National Institutes of Health (NIH)/National Heart, Lung, and Blood Institute Grant T32-HL-00702. F.L.B. has received NIH/National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Grant K24-DK-62222 and the Johns Hopkins Diabetes Research and Training Center/NIDDK Grant P60-DK-079637. E.S. has received NIH/NIDDK Grants K01-DK-076595 and R01-DK-089174.
No potential conflicts of interest relevant to this article were reported.
J.K.B. conducted the analyses and wrote the draft of the manuscript. F.L.B. and E.S. provided input on the interpretation of data and reviewed and edited the manuscript. E.S. was involved in the planning of methods and supervision of data analysis. J.K.B. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc12-0404/-/DC1.
References
- 1.American Diabetes Association Executive summary: Standards of medical care in diabetes—2012. Diabetes Care 2012;35(Suppl 1):S4–S10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: abbreviated report of a WHO consultation [report online], 2011. Available from http://www.who.int/diabetes/publications/report-hba1c_2011.pdf Accessed 20 August 2012 [PubMed] [Google Scholar]
- 3.Colagiuri S, Lee CMY, Wong TY, Balkau B, Shaw JE, Borch-Johnsen K, DETECT-2 Collaboration Writing Group Glycemic thresholds for diabetes-specific retinopathy: implications for diagnostic criteria for diabetes. Diabetes Care 2011;34:145–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheng YJ, Gregg EW, Geiss LS, et al. Association of A1C and fasting plasma glucose levels with diabetic retinopathy prevalence in the U.S. population: Implications for diabetes diagnostic thresholds. Diabetes Care 2009;32:2027–2032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davidson MB, Schriger DL, Peters AL, Lorber B. Relationship between fasting plasma glucose and glycosylated hemoglobin: potential for false-positive diagnoses of type 2 diabetes using new diagnostic criteria. JAMA 1999;281:1203–1210 [DOI] [PubMed] [Google Scholar]
- 6.Selvin E, Ning Y, Steffes MW, et al. Glycated hemoglobin and the risk of kidney disease and retinopathy in adults with and without diabetes. Diabetes 2011;60:298–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang L, Krzentowski G, Albert A, Lefebvre PJ. Risk of developing retinopathy in Diabetes Control and Complications Trial type 1 diabetic patients with good or poor metabolic control. Diabetes Care 2001;24:1275–1279 [DOI] [PubMed] [Google Scholar]
- 8.Herman WH, Dungan KM, Wolffenbuttel BHR, Buse JB, Fahrbach JL, Jiang H, Martin S. Racial and ethnic differences in mean plasma glucose, hemoglobin A1c, and 1,5-anhydroglucitol in over 2000 patients with type 2 diabetes. J Clin Endocrinol Metab 2009;94:1689–1694 [DOI] [PubMed] [Google Scholar]
- 9.Kirk JK, Passmore LV, Bell RA, et al. Disparities in A1C levels between Hispanic and non-Hispanic white adults with diabetes: a meta-analysis. Diabetes Care 2008;31:240–246 [DOI] [PubMed] [Google Scholar]
- 10.Likhari T, Gama R. Glycaemia-independent ethnic differences in HbA(1c) in subjects with impaired glucose tolerance. Diabet Med 2009;26:1068–1069 [DOI] [PubMed] [Google Scholar]
- 11.Selvin E, Steffes MW, Ballantyne CM, Hoogeveen RC, Coresh J, Brancati FL. Racial differences in glycemic markers: a cross-sectional analysis of community-based data. Ann Intern Med 2011;154:303–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ziemer DC, Kolm P, Weintraub WS, Vaccarino V, Rhee MK, Twombly JG, Narayan KMV, Koch DD, Phillips LS. Glucose-independent, black-white differences in hemoglobin A1c levels: a cross-sectional analysis of 2 studies. Ann Intern Med 2010;152:770–777 [DOI] [PubMed] [Google Scholar]
- 13.Bloomgarden ZT. A1C: recommendations, debates, and questions. Diabetes Care 2009;32:e141–e147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bonora E, Tuomilehto J. The pros and cons of diagnosing diabetes with A1C. Diabetes Care 2011;34(Suppl 2):S184–S190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cohen RM. A1C: does one size fit all? Diabetes Care 2007;30:2756–2758 [DOI] [PubMed] [Google Scholar]
- 16.Dagogo-Jack S. Pitfalls in the use of HbA1(c) as a diagnostic test: the ethnic conundrum. Nat Rev Endocrinol 2010;6:589–593 [DOI] [PubMed] [Google Scholar]
- 17.Herman WH, Cohen RM. Hemoglobin A1c: teaching a new dog old tricks. Ann Intern Med 2010;152:815–817 [DOI] [PubMed] [Google Scholar]
- 18.Kilpatrick ES, Bloomgarden ZT, Zimmet PZ. Is haemoglobin A1c a step forward for diagnosing diabetes? BMJ 2009;339:b4432. [DOI] [PubMed] [Google Scholar]
- 19.Rubinow KB, Hirsch IB. Reexamining metrics for glucose control. JAMA 2011;305:1132–1133 [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: questionnaires, datasets, and related documentation, 2010. Available from http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm Accessed 29 April 2011
- 21.Centers for Disease Control and Prevention. 2005-2006 National Health and Nutrition Examination Survey: survey operations manuals, brochures, consent documents, 2010. Available from http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/current_nhanes_05_06.htm Accessed 29 April 2011
- 22.Centers for Disease Control and Prevention. 2007-2008 National Health and Nutrition Examination Survey: survey operations manuals, brochures, consent documents, 2010. Available from http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/current_nhanes_07_08.htm Accessed 29 April 2011
- 23.Grading diabetic retinopathy from stereoscopic color fundus photographs–an extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 1991;98(5 Suppl):786–806 [PubMed] [Google Scholar]
- 24.Emanuele N, Sacks J, Klein R, et al. Veterans Affairs Diabetes Trial Group Ethnicity, race, and baseline retinopathy correlates in the veterans affairs diabetes trial. Diabetes Care 2005;28:1954–1958 [DOI] [PubMed] [Google Scholar]
- 25.Selvin E, Steffes MW, Ballantyne CM, Hoogeveen RC, Coresh J, Brancati FL. Racial differences in glycemic markers: a cross-sectional analysis of community-based data. Ann Intern Med 2011;154:303–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wong TY, Klein R, Islam FMA, et al. Diabetic retinopathy in a multi-ethnic cohort in the United States. Am J Ophthalmol 2006;141:446–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang X, Saaddine JB, Chou CF, et al. Prevalence of diabetic retinopathy in the United States, 2005-2008. JAMA 2010;304:649–656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris MI, Klein R, Cowie CC, Rowland M, Byrd-Holt DD. Is the risk of diabetic retinopathy greater in non-Hispanic blacks and Mexican Americans than in non-Hispanic whites with type 2 diabetes? A U.S. population study. Diabetes Care 1998;21:1230–1235 [DOI] [PubMed] [Google Scholar]
- 29.Selvin E, Zhu H, Brancati FL. Elevated A1C in adults without a history of diabetes in the U.S. Diabetes Care 2009;32:828–833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 2010;362:800–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.International Expert Committee International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32:1327–1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.