Abstract
Objective
Suicidal ideation (SI) and thoughts of death are often experienced as fluctuating; therefore a dynamic representation of this highly important indicator of suicide risk is warranted. Theoretical accounts have suggested that affective, behavioral, and interpersonal factors may influence the experience of thoughts of death/suicidal ideation. This study aimed to examine the prospective and dynamic impact of these constructs in relation to thoughts of death and SI.
Method
We assessed adolescents with a recent hospitalization for elevated suicide risk over six months. Using the methodology of the Longitudinal Interval Follow-Up Evaluation (LIFE), weekly ratings for SI, course of depressive illness, affect sensitivity, negative affect intensity, behavioral dysregulation, peer invalidation, and family invalidation were obtained.
Results
Using multilevel modeling, results indicated that: 1) same-week ratings between these constructs and SI were highly correlated at baseline and throughout follow-up; 2) baseline ratings of affect sensitivity, behavioral dysregulation, and peer invalidation were positive prospective predictors of SI at any week of follow-up; 3) weekly ratings of each of these constructs had significant associations with next-week ratings of SI; and 4) ratings of SI had positive significant associations with next-week ratings on each of the constructs.
Conclusions
These results suggest that affective sensitivity, behavioral dysregulation, peer invalidation, and suicidal ideation are highly associated with SI levels both chronically (over months) and acutely (one week to the next), while depression, negative affect intensity, and family invalidation were more acutely predictive of SI. Elevated SI may then aggravate all these factors in a reciprocal manner.
Keywords: suicidal ideation, suicide risk, adolescents, affect dysregulation, invalidation
High levels of suicidal ideation (SI), defined as thoughts, images, and desires for death and/or death by suicide, confers elevated risk for future suicide attempts (Lewinson et al., 1996; Spirito & Esposito-Smythers, 2006) and death by suicide (Beck et al., 1999). Along with direct SI, passive thoughts about death, also known as morbid thinking, are frequently considered a part of the construct of SI (Steer et al., 1993; Joiner et al., 2007) and are a known risk factor for death by suicide (Mandrusiak et al, 2006). Thoughts of death are also frequently used as an indicator of SI in suicide risk assessments (Joiner et al., 1999). However, there is some factor analytic evidence suggesting that thoughts of death may load onto a separate factor from suicidal ideation (Yoder et al., 2008). Regardless as to whether both comprise one factor, both thoughts of death and SI have been found to be predictive of suicidal behavior, and past suicide attempts have also been linked to higher levels of SI in the future (Joiner et al., 2000) – suggesting a potential reciprocal relationship.
Despite its salience as a predictor of suicide risk, SI is often treated as a stable experience that is either absent or present in varying degrees, without recognition of the fluidity of this experience even among those at high risk. This can be seen in most suicide risk assessments, which are primarily single-point measures that average the experience of SI over a period of a few weeks. However, recent research has found that while SI may be somewhat stable for some people, in others it can fluctuate in intensity between weeks or even days (Witte et al., 2005; Witte et al.,, 2006). Perhaps surprisingly, variability in SI has been found to predict increased suicidal behavior relative to those with stable SI (Witte et al., 2005; Witte et al., 2006), and those with the most variable SI may also be the most reactive to issues in their environments. There are many factors that influence variability in SI, with more proximal factors perhaps having the most influence. Identification of these factors and understanding their influence on fluctuations in suicidal behavior may improve our clinical assessment and treatment of SI. The purpose of the following study was to examine weekly time-varying predictors of level of SI, using a 6-month timeline follow-back assessment protocol, in adolescents recently hospitalized for elevated suicide risk.
Suicidal Ideation in Adolescents
Recent data suggest that adolescent suicidal behavior may be on the rise after a recent period of decline (Bridge et al., 2008; Eaton et al., 2008). Although some adult risk factors have also been identified in adolescents, such as suicide attempts (Goldston et al., 1999) and self-injury (Wilkinson et al., 2011), not all have been replicated in this group. Given the prevalence of SI and suicidal behavior in adolescents, it is surprising that no studies to our knowledge have directly explored fluctuations in adolescent SI. Understanding how psychosocial factors, such as bullying by peers, family environment, and affective and behavioral traits, influence changes in SI in this group is crucial, as the very nature of being an adolescent is characterized by constant change in biology, psychology, and social structure.
Proximal Influences on Variability in Suicidal Ideation
There are many factors that are likely to influence weekly levels of SI among adolescents, including intrapersonal, interpersonal, and environmental variables, to environmental variables. One way to efficiently conceptualize some of these factors is through Linehan’s (1993) biosocial theory, which suggests that SI is highly influenced by three primary factors: affective dysregulation, behavioral dysregulation, and interpersonal invalidation.
Affective dysregulation, in general, has been found to have high cross-sectional correlations with measures of variability in SI (Harvey et al., 1989) and prospective associations with suicidal behavior (Yen et al., 2004, 2009). Affective dysregulation consists of two major components: affective intensity and affective sensitivity. Affective intensity involves experiencing affective states at a higher level than others might experience that state given a similar trigger. Intensity of negative emotion may influence the experience of SI, as intense emotions may subsequently lead to intense SI. Affective sensitivity, on the other hand, refers to the threshold needed to activate an emotional state, and with elevated sensitivity the triggers that can activate an emotional state are less dramatic and more frequent in daily life. Affective dysregulation is an important variable for further investigation in adolescents, especially because those with multiple suicide attempts have been found to have worse affective dysregulation that those with single or no attempts (Esposito et al., 2003), and further investigating affective dysregulation in terms of intensity and sensitivity may add to our understanding of this relationship.
Behavioral dysregulation refers to a behavior that is difficult to control and engaging in the behavior has harmful consequences for the person (Selby & Joiner, 2009). Common examples of dysregulated behaviors can include self-injury, binging and/or purging, substance use, and aggressive behaviors. Importantly, impulsivity, a common component in many dysregulated behaviors has been linked to suicidal behavior in adolescent populations (Dougherty et al., 2004; Nock et al., 2009). Behavioral dysregulation has been found to be a warning sign for death by suicide (Mandrusiak et al., 2006). Further investigation of this variable, especially longitudinally, may help to illuminate how it is related to variability of SI.
The final component of Linehan’s (1993) theory involves the suicidal person existing within an invalidating environment. In an invalidating environment, people frequently criticize or punish the individual for expressing emotion. Regarding family emotional invalidation, family dysfunction has been found to be an important contributing variable to suicidality in adolescents (Bridge et al.,, 2006; Brinkman-Sull et al., 2000). While obvious indicators of family emotional invalidation (i.e., physical or sexual abuse) have been linked to later SI (Joiner et al., 2007), less obvious but perhaps more pervasive aspects of family emotional invalidation have not been examined. For example, low feelings of alliance with family appear to be correlated with SI, making a suicide threat, and overall suicide risk (Osman, et al., 1998). Peer emotional invalidation is also likely to contribute to variability in SI, perhaps even more so than family invalidation. For example, feelings of low social acceptance have been linked to SI and suicide attempts in adolescents (Prinstein et al.,, 2001). Importantly, withdrawal from family and friends, has been indicated as an important warning sign for suicidal behavior (Mandrusiak et al., 2006).
Thus, from Linehan’s proposed framework, there is a high potential that affective dysregulation, behavioral dysregulation, and emotional invalidation have dynamic influences on weekly levels of suicidal behavior. Given the rapid changing nature of adolescents’ lives, these variables may have an even greater influence in this population than adults. Yet, to our knowledge, most have not been studied in the context of variability in level of SI, nor have their longitudinal associations with SI been examined in adolescents.
The influences of affective, behavioral, and interpersonal variables on SI only paint part of the picture, however, as the experience of SI is likely to influence subsequent levels of these variables as well. The very presence of elevated SI is likely to influence the way that adolescents respond to emotion events, perhaps with more intense negative affect, or they may become even more sensitive to emotional triggers. Similarly, they may become more behaviorally dysregulated in the presence of elevated SI, potentially trying multiple behaviors to try and cope with or escape from SI. Finally, the presence of SI may influence they way adolescents perceive their interactions with peers or family, or it may actually change those interactions so that people respond to them in even more invalidating ways. Given the broad effect that SI may have on various aspects of life, exploring the dynamic influences of SI on these variables may be just as important as their dynamic influence on SI.
Current Study
Based on the need to establish a better understanding of the affective, behavioral, and interpersonal factors that influence variability in thoughts about death and SI among adolescents, time-varying data on SI were examined over 26 weeks among a sample of adolescents who were recently hospitalized for elevated suicide risk. We hypothesized that high levels, at both baseline and week-prior, of negative affective intensity, affective sensitivity, behavioral dysregulation, and peer and family invalidation would be positive predictors of elevations in weekly SI, beyond baseline and week-prior levels of SI. Furthermore, we also predicted that there would be a reciprocal relationship where higher levels of baseline and week-prior SI would significantly predict subsequent increased levels negative affective intensity and sensitivity, behavioral dysregulation, and invalidation.
Methods
Participants
Participants consisted of 119 adolescents, with additional information provided by their legal guardians/primary caregivers, who were recruited for a naturalistic, follow-up study on the course of emotional functioning in suicidal adolescents over the 6-month period after a psychiatric hospitalization. Inclusion criteria were: fluency in English, and admission to the hospital for concern about suicide risk, presence of suicidal ideation or a suicide plan, or a recent suicide attempt. All participants met hospital criteria for a psychiatric admission on the basis of elevated suicide risk, which typically requires suicidal ideation with a suicide plan. Self-injury without suicidal intent was not counted for inclusion. Exclusion criteria included: Evidence of active psychotic disorder or cognitive impairment that would affect reliability of interviews and self-report.
Participants – adolescent inpatients along with their caregivers – were recruited from the adolescent inpatient unit of a psychiatric hospital in the Northeast. Adolescents were recruited on the basis of having been recently hospitalized for elevated suicide risk (e.g., recent suicide attempt including actual, aborted, or interrupted attempts, self-injurious behavior with simultaneous SI, or SI including the presence of a suicide plan), as assessed by hospital staff during an intake interview during admission to the hospital. Parental consent and adolescent assent were required to proceed with the study intake assessment. This study was approved by the Institutional Review Boards of Brown University and the respective hospital. Adolescents and parents were compensated for their time with a payment of $50 to each, for the baseline interview and for the 6-month follow-up interview.
Of the 119 suicidal adolescent patients enrolled in this study, 81 were female (68%). The sample was 78.5% Caucasian, 10.0% African American, 1.7% American Indian/Alaskan native, and 9.8% fell outside of these categories. Twenty-two patients (18%) endorsed Hispanic ethnicity. The patients’ ages ranged from 12 to 18 years old with a mean age of 15.3 (SD=1.4). Regarding living situation, 78% lived with their biological mother, 34% with their biological father, 24% with a step-parent, 9% lived with adoptive or foster parents, and 3% lived in a residential facility. Approximately 32% of the sample had family incomes below $30,000 annually, while around 35% of the sample had family incomes of over $70,000 annually, indicating the sample was socioeconomically diverse.
Procedure
All participants completed baseline interviews and self-report instruments that assessed demographic information, diagnoses and functioning, past history of suicide attempts and current suicidal ideation, and the predictors of interest to the present study: negative affect intensity, affect sensitivity, behavioral dysregulation, and family and peer invalidation. Approximately 66% of interviews were conducted by doctor-level clinicians, 4% by masters-level clinicians, and 30% were completed by bachelors-level research assistants. All assessors were thoroughly trained to competence by the PI (SY), who is co-director of the Training and Assessment Unit at Brown University and has over 10 years of experience training assessors on clinical interviews, on the Schedule for Affective Disorders and Schizophrenia for School Aged Children (K-SADS) and LIFE interviews. All interviews were audiotaped and reviewed for quality assurance by the principal investigator, and all diagnostic interviews were discussed in case meetings to establish diagnostic consensus. A suicide risk protection protocol was in place during follow-up assessments in the case that a participant reported elevated suicide risk (i.e. presence of suicide plans with intent). Whenever applicable, assessments were administered to both adolescent and caregiver (16 parents, 13%, did not complete the assessments that were administered to their children). When reports were discrepant, consensus scores were determined during weekly case review meetings using all available information including chart review and information from treating physician on the adolescent unit. Discrepant score were defined as when a parent provided a score that was different to the score obtained from the adolescent such that it would result in different diagnostic outcomes.
Following the baseline assessments, patients were then contacted every two months over the next six months (26 weeks). At this time, important life events and main outcome variables were assessed to assist with recall at the full 6-month interview. Additionally, a brief assessment of the primary predictors and outcomes of interest to this study was reviewed, including suicide attempts and ideation, disorders present at baseline, functioning, and negative affect intensity, affective sensitivity, behavioral dysregulation, and family and peer invalidation. At the final 6-month follow-up assessment, a final assessment of these variables was administered, resulting in baseline and follow-up ratings for 6 months.
Baseline Measures
Baseline Clinical Interviews
Schedule for Affective Disorders and Schizophrenia for School Aged Children – Present and Lifetime Versions (K-SADS-PL; Kaufman et al., 1997)
The K-SADS-PL was used to determine psychiatric diagnoses at baseline. This device is a semi-structured diagnostic interview, which provides a reliable and valid assessment of DSM-IV psychopathology in children and adolescents. Inter-rater agreement has been found to be high by the developers (range: 93–100%). Test-retest reliability and kappa coefficients have been found to be in the excellent range for present and lifetime diagnoses. Probes and objective criteria are provided to rate individual symptoms. The K-SADS-PL was administered with adolescent and caregiver participants individually, and consensus ratings were used to establish presence or absence of a diagnosis The KSADS also measures functioning across a number of domains, and for the current study we used the score for perceived quality of peer relationships in some analyses.
Longitudinal Interval Follow-Up Evaluation - Adolescent version – Baseline (LIFE; Keller et al., 1987)
The LIFE is a semi-structured interview rating system with demonstrated reliability for assessing the longitudinal course of psychiatric disorders, and has been used in previous studies investigating adult suicidal behavior (Yen et al., 2003). The diagnostic constructs from this interview have also been used in previous adolescent samples (Birmaher et al., 2009). At baseline, the LIFE-Base version was administered to adolescent and caregiver to gather baseline ratings for variables of interest yielding baseline Psychiatric Status Rating (PSR) scores. This baseline score takes into consideration data gathered from other diagnostic clinical interviews (in the present study, the KSADS-PL) such that baseline PSR scores are obtained for disorders in which the participant meets criteria and functioning across multiple domains. Assignment of follow-up PSR scores is described in the following section. In this study only major depression was used, which was rated on a 6-point scale (full criteria = PSR6, PSR5; partial remission = PSR4, PSR3; full remission = PSR2, PSR1).
The LIFE assessment approach was also extended to operationalize the constructs relevant to Linehan’s (1993) theory that were specifically discussed in the introduction: SI, negative affect intensity, affective sensitivity, behavioral dysregulation, peer invalidation, and family invalidation. Furthermore, empirical studies of suicidal behavior have identified affective and behavioral dysregulation as risk factors for suicidal behavior (Esposito et al., 2004; Yen et al, 2003) and models of affect regulation distinguish between affect intensity (i.e. amplitude) and sensitivity (i.e. threshold). While most assessments treat these constructs as static, in the present study we adapted the LIFE to examine these constructs as time-varying, dynamic predictors and outcomes. The CSR variables were developed to assess for these constructs using questions that would capture the most agreed upon definition for these constructs as well as some questions from validated self-report measures.
Baseline levels of each of the CSR scales were established during the original assessment with higher scores indicating greater severity. The interview questions for assessing each of these constructs consisted of a brief paragraph explaining the construct and providing brief, open examples, followed by the patient endorsing their level for the past month. The descriptions for each of the predictor constructs are located in Table 1, with the exception of depression, which was a PSR assigned on the basis of presence of DSM-IV criteria. We refer to the corresponding ratings as Construct Status Ratings (CSR) to differentiate them from the LIFE PSR variables. A six point CSR scale was used to maintain consistency with the PSR. For this study: CSR 6 = extremely intense, CSR 5 = high, CSR 4 = moderate, CSR 3 = somewhat, CSR 2 = minimal, CSR 1 = not at all. Baseline inter-rater reliability for each construct was assessed with a random sample of 10% of the participants whose interviews were reviewed and rated by a second blind reviewer. Rater agreement was found to be good for all variables, further supporting the extension of the LIFE assessment approach to the CSR variables in this study (suicidal ideation κ = .90; affective sensitivity κ = .95; negative affect intensity κ = 1.0; behavioral dysregulation κ = 1.0; family invalidation κ = .99; peer invalidation κ = .93)1. Because these scales had not been previously validated, we examined convergent validity and reliability with other self-report measures (described below) in the results section.
Table 1.
Assessment Protocol for CSR Variables
| CSR Variable | Interview Assessment |
|---|---|
| Death/Suicidal Ideation | Sometimes when people are upset or feel bad they think about dying or even killing themselves. Do you have these thoughts during these past six months? How often did you have these thoughts? When you had them, how long did they last – a few minutes, an hour or more, almost always? Did you have these thoughts throughout the past month or where there times when you did not have these thoughts? Do you have those thoughts now? Do you have a plan? What is it? Have you told anyone about these thoughts or plans? |
| Negative Affective Intensity | If you put all of your bad feelings together, including some which we have asked about such as sadness, mood swings, and anxiety, but also others that we haven’t talked about like guilt, shame, low self-esteem, how would you rate ALL of these negative feelings over the past month? Where there times when these feelings were really intense and overwhelming and it felt like nothing you could do could change how you would feel? |
| Affective Sensitivity | Were there times when you may have been more sensitive or vulnerable to having these negative feelings than other times? For example, sometimes the slightest provocation (a comment, a look) could really upset you and other times those same circumstances didn’t bother you at all. Can you think about how emotionally vulnerable or sensitive you may have been over the past month? Where there times when you felt really sensitive (or had a low threshold)? Or times when you felt really strong and stable (or had a high threshold)? |
| Behavioral dysregulation | Were there times when your behavior was more out of control than other times? For example, were there times when you found yourself doing things that you didn’t plan on doing to escape a difficult emotion? Or reacting in a way that was unplanned or out of control, such as screaming at someone, throwing things, or getting into a fight? |
| Family Invalidation | Were there times when you did not feel accepted by your family? Or that you could not express your true thoughts or feelings? Or that if you did express your thoughts and feelings, that you would be dismissed, punished, ignored, or made fun of? |
| Peer Invalidation | Were there times when you did not feel accepted by your classmates? Or that you were being left out? Or that you could not express your true thoughts or feelings? Or that if you did express your thoughts and feelings, that you would be dismissed, punished, ignored, or made fun of? How many friends do you have that can confide in? |
Note: CSR = Construct Status Rating
Childhood Interview for Borderline Personality Disorder (CI-BPD)
The CI-BPD is the adolescent adaptation of the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV; Zanarini et al., 1996) a semi-structured diagnostic interview for the DSM-IV personality disorders. The CI-BPD focuses only on BPD, and has multiple subscales. For the present study, we examined only the Impulsivity subscale in order to provide convergent validity for the behavioral dysregulation CSR that was used in this study. For this study, the Impulsivity scale of the CI-BPD was coded as either (1) above threshold or 0 (absent). The DIPD-IV compares favorably to other structured interviews for personality disorders, with good reliability (Zanarini et al., 1987). The kappa inter-rater reliability for BPD diagnosis in this sample was 0.82.
Baseline Self Report Measures
The following measures were used only to provide convergent validity for the CSR constructs from the LIFE interview, because the CSR constructs had not been previously validated in other studies.
Suicide Ideation Questionnaire (SIQ; Reynolds, 1985)
The SIQ is a 30-item self-report instrument designed to assess thoughts about suicide experienced by adolescents during the prior month. Participants responded to items using a 7-point Likert-type scale (0=I never had this thought; 6=almost every day). Excellent internal consistency (α = .97) and construct validity for the SIQ has been reported (Reynolds, 1985). Internal consistency was also extremely high in the present sample (Cronbach’s α = 0.97).
Affect Intensity Measure (AIM; Larsen & Diener, 1987)
The AIM is a 40-item self-report measure assessing the typical strength of an individual’s affective responsiveness and is an important component to understanding emotion regulation processes. It contains three subscales: negative intensity, positive affectivity, and negative reactivity. Items are rated on a 6-point likert scale, where higher scores indicate greater intensity/reactivity. The AIM has strong test-retest reliabilities (.81 for 3 month interval and .75 for 2 year interval) and adequate convergent and discriminant validity (Larsen et al., 1987).
Aggression Questionnaire (AQ; Buss & Perry, 1992)
This is a widely used 34-item measure for assessing hostility and aggression; For this study we only used the total scale score. Previous findings have indicated acceptable reliability and validity (Buss & Perry, 1992). In this study we analyzed both the adolescents’ reporting on the scale (AQ-A) as well as the parents’ report of child’s behavior (AQ-P) to provide evidence of validity for the behavioral dysregulation CSR scale used in the study. In the present sample, alpha was over .90 for both adult and adolescent scales.
Family Assessment Device (FAD; Epstein et al., 1983)
This is a 60-item self-report questionnaire that assesses family functioning. Participants rated their family functioning on a 4-point scale, with higher scores indicating greater family dysfunction. Adequate internal (α = .72 –.92) and test-restest (r = .66 – .76) reliability estimates have been reported (Miller et al., 1985). The global functioning (FAD-GF) score was analyzed for both adolescent and parent report. Internal consistency of the FAD-GF in the present study was strong (α = .91 for adolescents; α = .88 for caregivers).
Longitudinal Follow-Up Measure
Longitudinal Interval Follow-Up Evaluation - Adolescent version – Follow-up
Using information obtained from the LIFE interview and after ascertaining relevant change points during the 6-month follow-up interval, weekly PSRs were assigned for all full threshold diagnoses including major depressive episode and CSRs were assigned for negative affect intensity, affect sensitivity, behavioral dysregulation, and family and peer invalidation. As part of the interview, patients were asked to identify time anchors (e.g., life events, birthdays, holidays) in the preceding six months that assist with recall. Patients were reminded of their original response at baseline and asked whether changes have occurred during the six-month follow-up interval. For each period of change, symptoms were reviewed (for disorders) and constructs were re-evaluated yielding PSR/CSR values for each week of follow-up. Good to excellent inter-rater and test-retest reliabilities have been established for the LIFE Follow-up for several Axis I disorders using a different sample in another longitudinal, naturalistic study with a similar assessment protocol at the same research site (Warshaw et al., 1994; Warshaw et al., 2001). As in the baseline procedure, the predictor constructs of negative affect intensity, affect sensitivity, behavioral dysregulation, peer invalidation and family invalidation and the outcome construct of suicidal ideation utilized a 6-point scale interview rating with weekly scores assigned as: CSR 6 = extremely intense, CSR 5 = high, CSR 4 = moderate, CSR 3 = somewhat, CSR 2 = minimal, CSR 1 = not at all.
Data Analytic Strategy
First, demographic data for the sample were examined, followed by an evaluation of participant attrition from the study. Next, we analyzed correlations between the predictors (i.e., baseline PSR/CSRs) and baseline level of death/suicidal ideation, as well as between the weekly PSR/CSR of the variables with concurrent week rating of SI. We also examined the validity of the CSR measures by examining convergent/divergent correlations with other variables and test-retest reliability over the 6-month follow-up. Next, we ran a hierarchical model that simultaneously used baseline measures to prospectively predict level of SI at any given week. Doing so allowed us to examine the baseline predictors of SI for the entirety of the 6-month follow-up. We also included the 26 weekly ratings of each of the predictor variables in this model, using the previous week’s score to predict the subsequent week’s report of SI, at any given week. For this we created lag-variables for the predictors, which allowed us to examine how experience of these factors the week before may relate to the subsequent week’s level of SI, at any given week. Importantly, this model included depression PSR at baseline and weekly because time varying course of depression has been found to be highly associated with suicidal behaviors (Yen et al., 2003), and we desired to examine the strength of the hypothesized variables after accounting for primary psychopathology. For the final analyses, we ran a separate model using a baseline-SI and lag-SI variable to predict the subsequent weeks’ levels of depression, negative affect intensity, affect sensitivity, behavioral dysregulation, family invalidation, and peer invalidation, at any given week. This was done to examine the residual effects of SI over subsequent weeks.
Because participants hand multiple assessments over time, it was important to account for the nested structure of the data such that there were multiple weekly assessments nested within each participant. To evaluate the level of SI at any given week, the models analyzed in this study used hierarchical generalized linear modeling (HGLM) to account for the nested structure of the data and the non-continuous outcome variable. This nested structure made it important to evaluate weekly predictors of SI (the lag-variables of each predictor) and baseline predictors at their appropriate level simultaneously. Furthermore, the SI-CSR variable consisted of 6 levels indicating increasing severity. Because this was a clinical sample with restricted range of SI scores to those with elevated suicidality, the variable was not continuous and required treatment as a count variable, requiring an alternative distribution and a link function. The statistical modeling program, Mplus (Version 5.2; Muthén & Muthén, 1998–2008), appropriate for these kinds of analyses, was used to evaluate the HGLM model. Relative risk (RR) ratios were calculated from the predictor values, which indicate the amount of fluctuation in risk of elevated SI for every unit of change in the predictor variable. Finally, due to the numerous predictors used in the analyses, we controlled for potential Type 1 error by setting the significance threshold at α=.01.
Results
Clinical Characteristics
All patients had been hospitalized for inpatient psychiatric treatment at least once, and over 41% had more than one previous psychiatric admission. The most commonly diagnosed Axis I disorder was major depressive disorder (85%), followed by attention deficit/hyperactivity disorder (39%), and generalized anxiety disorder (26%). There were 107 (88%) patients being prescribed psychotropic medication at the baseline assessment. Average patient functioning, as assessed by GAF scores rated on the KSADS, was 42.8 (SD=7.6), indicating that overall this was a highly impaired sample of adolescents. Approximately 34% of patients reported a history of abuse (either physical or sexual). The average level of SI at baseline, as measured by the SIQ, was 117.26 (SD=44.66), indicating an extremely high level given the recommended cutoff score for the SIQ indicative of clinical suicide risk is 41 (Reynolds, 1985). Regarding past history of suicidal behavior, 72 (60%) reported a past history of suicide attempt. During the follow-up period for the study, 19 (18%) reported a suicide attempt and 27 (26%) were admitted to the ER, with 24 of those making the visit for suicide related reasons.
Participant Attrition
Due to the intensive nature of collecting data in a clinically severe sample over a period of 6 months, some participant attrition was expected. Overall, 20 patients dropped out after the baseline assessment and during the course of the follow-up assessments, meaning that 82% of the sample completed the full study. The pattern of attrition consisted of 15 patients who did not provide any follow-up data, 2 who provided only 2 months of follow-up data, and 3 who provided only 4 months of follow-up data. No differences were found between those who completed the study versus those who dropped out on initial PSR levels of SI (F(1, 118)=.35, p=.56) and depression (F(1, 118)=.91, p=.76), or with regard to age (F(1, 118)=.16, p=.69), sex (χ2(1)=.02, p=.89), ethnicity (χ2(1)=.55, p=.76), or race (χ2(3)=1.53, p=.68).
In order to account for those missing the majority of the follow-up data, those who dropped out immediately (N=15) were not included in the longitudinal analyses. Missing data for those who dropped out but completed at least one follow-up assessment (N=5) were included in the model with values approximated in Mplus using full-information maximum likelihood (FIML; Anderson, 1957), an appropriate method for handling missing data in hierarchical models (Kline, 2005).
CSR Measure Validation
Because the CSR variables used in this study have not been previously validated, we conducted some preliminary analyses to ensure that they demonstrated construct validity by examining them in relation to other interview and self-report measures obtained for the study. All correlations were Pearson’s correlations, with the exception of the Impulsivity subscale of the CI-BPD for which we used a Kendall-Tau correlation due to the dichotomous structure of the scale. Importantly, all CSR measures demonstrated significant correlations with the corresponding previously validated scales, all in the expected direction. The baseline SI-CSR demonstrated a correlation of r=.35 (p<.01) with the SIQ, the negative affect intensity CSR demonstrated a significant positive correlation with the negative affect intensity subscale of the AIM (r=.25, p<.05), and the affective sensitivity CSR demonstrated a similar significant correlation with the affective sensitivity subscale of the AIM (r=.31, p<.01). Regarding the behavioral dysregulation CSR it was correlated with the Aggression Questionnaire (AQ-A r=.37, p<.01; AQ-P r=.55, p<.01), as well as the Impulsivity criterion of the CI-BPD (r=.42, p<.01). The peer invalidation CSR scale was correlated with the perceived peer relationships functioning scale of the KSADS (r = −.38, p<.01), indicating that high peer invalidation was inversely related to positive perception of peer relationships. Finally, the family invalidation CSR was significantly correlated with the perceived relationship with both mother and father as measured by the FAD general functioning scale (r=.48, p<.01).
We also examined the reliability of the CSR measures by correlating ratings at baseline with the corresponding rating 6 months later. All baseline CSR measures were significantly correlated with the measure of the same variable 6 months later: SI (r=.27, p<.05), behavioral dysregulation (r=.47, p<.001), affective sensitivity (r=.34, p<.001), negative affective intensity (r=.26, p<.05), peer invalidation (r=.53, p<.001), and family invalidation (r=.40, p<.001). Finally, regarding divergent validity, as can be seen in Table 3 although many of the scales demonstrated significant moderate correlations with each other, no scales were so highly correlated that they may be measuring entirely the same construct. Given the evidence presented for convergent and divergent validity between each other and additional measures, as well as evidence of test-retest reliability, the CSR scales used in the current study appear to demonstrate preliminary construct validity.
Table 3.
Means, Standard Deviations, and Correlations of Concurrent Weekly PSR/CSR Measures
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. SI | -- | ||||||
| 2. DEP | .09** | -- | |||||
| 3. AS | .29** | .16** | -- | ||||
| 4. NAI | .51** | .08** | .53** | -- | |||
| 5. BD | .28** | .12** | .34** | .36** | -- | ||
| 6. PeerI | .19** | −.04 | .26** | .33** | .11** | -- | |
| 7. FamI | .27** | .04 | .23** | .33** | .38** | .17** | -- |
|
| |||||||
| MEAN | 2.65 | 3.60 | 3.76 | 3.77 | 3.18 | 2.84 | 3.08 |
| SD | 1.55 | 1.51 | 1.35 | 1.42 | 1.54 | 1.55 | 1.60 |
Note. N=99;
p<0.001;
SI=thoughts of death and suicidal ideation, DEP=depression, AS=affective sensitivity, NAI= negative affective intensity, BD=behavioral dysregulation, PeerI=peer invalidation, FamI=family invalidation.
Variability of Death/Suicidal Ideation
During the 26 weeks of monitoring, participants were rated on a weekly basis regarding their suicidal ideation, with scores ranging from 1 (low) to 6 (high). The average level of SI at any given week was 2.46, with a standard deviation of 1.39. In order to examine if there was substantial variation in SI on a weekly basis, we calculated the intraclass correlation (ICC) for weekly SI, which can serve as an index of consistency of the level of SI between two randomly chosen occasions for each person (Snijders & Bosker, 1999). An ICC of 1 would indicate that there was little within person variance of SI, and an ICC of 0 would indicate high within person variance. There was a significant ICC of .59 (p<.05) for weekly suicidal ideation, which indicated that there was a moderate level of consistency between SI weekly ratings, and that there was significant within person variance in SI level over the 26 weeks.
Concurrent Correlations between Baseline and Weekly PSR/CSR Measures
Table 2 displays the concurrent baseline correlations between the PSR/CSR scores, and Table 3 displays the weekly PSR/CSR scores, which were examined to further examine the relationships between all measures. All baseline PSR/CSR measures were significantly correlated with baseline SI, with most being positively correlated with SI: depression (r=.26, p<.001), affective sensitivity (r=.10, p<.001), negative affect intensity (r=.23, p<.001), and family invalidation (r=.12, p<.001). There were inverse correlations between baseline level of SI and baseline behavioral dysregulation (r= −.11, p<.001) and baseline peer invalidation (r= −.13, p<.001), indicating that lower behavioral dysregulation and peer invalidation were related to higher SI at baseline. When all predictors were examined with regard to partial correlations with weekly SI the following partial correlations were obtained: depression (rp=.02, p>.05), negative affect intensity (rp =.71, p<.001), affective sensitivity (rp=.10, p<.001), peer acceptance (rp=.22, p<.01), family acceptance (rp=.09, p<.001), behavioral dysregulation (rp=.07, p<.01). These findings demonstrate that most constructs had a unique relation with SI to some extent.
Table 2.
Means, Standard Deviations, and Concurrent Correlations of Baseline PSR/CSR Measures
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. SI | -- | ||||||
| 2. DEP | .26** | -- | |||||
| 3. AS | .10** | .18** | -- | ||||
| 4. NAI | .23** | .19** | .24** | -- | |||
| 5. BD | −.11** | −.05* | .18** | .18** | -- | ||
| 6. PeerI | −.13** | .14** | .26** | −.02 | .05* | -- | |
| 7. FamI | .12** | −.20** | .16** | .03 | .13** | .27** | -- |
|
| |||||||
| MEAN | 4.26 | 4.45 | 4.33 | 4.93 | 3.84 | 3.17 | 3.62 |
| SD | 1.39 | 1.22 | 1.23 | .96 | 1.42 | 1.55 | 1.57 |
Note. N=121;
p<.05;
p<0.001;
SI=thoughts of death and suicidal ideation, DEP=depression, AS=affective sensitivity, NAI=negative affective intensity, BD=behavioral dysregulation, PeerI=peer invalidation, FamI=family invalidation.
As can be seen in Table 3, the concurrent correlations between the same-week PSR/CSR scores for all variables were significantly correlated with weekly level of SI, with all being positive correlations. These significant, positive correlations indicated that during the weeks when the adolescents were experiencing elevated SI, they were also experiencing elevated problems regarding depression (r=.09, p<.01), negative affective intensity (r=.51, p<.01), affective sensitivity (r=.29, p<.01), behavioral dysregulation (r=.28, p<.01), peer invalidation (r=.19, p<.01), and family invalidation (r=.27, p<.01). Interestingly, the weekly PSR/CSR correlations appeared stronger than the baseline correlations of the same measures, providing some evidence for the incremental value of weekly assessment for these constructs. These findings provide further validity for the creation of the CSR scales for this study.
Baseline PSR/CSR Prediction of Future Weekly Level of Suicidal Ideation
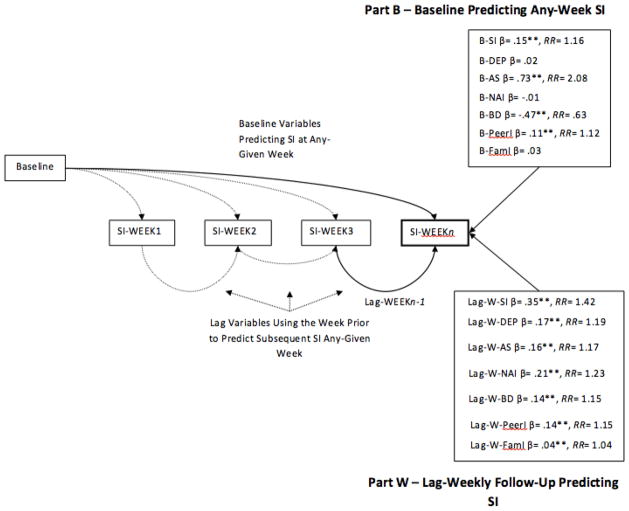
In order to examine our first hypothesis, that negative affective intensity, affective sensitivity, behavioral dysregulation, and peer and family invalidation at baseline would predict SI at any given week during follow-up, a HGLM model with all predictors simultaneously included was analyzed. In the HGLM model2, week (or time) was a significant predictor of weekly SI (β= −.026, SE=.001, p<.001, RR =.74), indicating that weekly level of SI tended to decrease within patients during the 6 month follow-up period. The values for the baseline predictors of any-week SI are displayed Figure 1 – Part B. As expected, almost all of the baseline variables were significant predictors of weekly SI: baseline SI (β=.15, SE=.03, p<.001, RR=1.16), affective sensitivity (β=.73, SE=.02, p<.001, RR=2.08), and peer invalidation (β=.11, SE=.03, p<.001, RR=1.12). However, behavioral dysregulation (β= −.47, SE=.02, p<.001, RR=.63), had a significant inverse/reverse relationship with SI, indicating higher levels of behavioral dsyregulation PSR/CSR predicted lower SI. These results held even after controlling for significant age (β= −.20, SE=.021, p<.001, RR=.82) and sex (β= −.56, SE=.071, p<.001, RR=.58) effects, which indicated that younger patients and male adolescents had higher levels of SI any given week. Baseline level of depression (β=.02, SE=.01, p=.10), negative affect intensity (β= −.01, SE=.04, p=.60), and family invalidation (β=.03, SE=.02, p=.40) were not significant predictors of weekly SI.
Figure 1.
Note: B = baseline, W=weekly, SI = thoughts of death and suicidal ideation, DEP= depression, AS = affective sensitivity, NAI = negative affective intensity, BD = behavioral dysregulation, PeerI = peer invalidation, FamI = family invalidation; **p<.001.
PSR/CSR Prediction of Next-Week Level of Suicidal Ideation
The next component of our first hypothesis involved investigating our predictor variables at one week in predicting level of SI the subsequent week. As can be seen in Figure 1 – Part W, the following were significant positive predictors of subsequent weekly SI3: lag-weekly SI (β=.35, SE=.01, p<.001, RR=1.42), lag-weekly behavioral dysregulation BD (β=.14, SE=.01, p<.001, RR=1.15), lag-weekly family invalidation (β=.04, SE=.01, p<.001, RR=1.04), lag-weekly affective sensitivity AS (β=.16, SE=.01, p<.001, RR =1.17), lag-weekly negative affective intensity (β=.21, SE=.01, p<.001, RR=1.23), lag-weekly peer invalidation (β=.14, SE=.01, p<.001, RR=1.15), and lag-weekly depression (β=.17, SE=.01, p<.001, RR=1.19).
Because adolescents with a history of past suicide attempts have been found to have higher levels of affective and behavioral dysregulation (Esposito et al., 2003), we decide to further evaluate the model with past attempt status as a covariate. We also examined the influence of attempting suicide during the follow-up period as a covariate. First, having a history of a previous suicide attempt was not significant predictive of SI level at any given week during monitoring (β=.03, SE=.02, p=.22). Further exploration indicated a significant effect of attempt status on SI when the other predictor variables were not included (β=1.16, SE=.01, p<.001, RR = 3.19), so having a previous suicide attempt may potentially be influenced by the CSR variables in the model. Next, attempt status occurring during the follow-up period was significantly related to increased suicidal ideation any given week during monitoring (β=.17, SE=.04, p<.001, RR=1.19), as would be expected. When attempt status before and after follow-up were included in the model all CSR variables maintained significance, with the exception of baseline peer acceptance which was no longer a significant predictor of SI at any given week (β=.01, SE=.01, p=.90).
Suicidal Ideation in Prediction of Next-Week PSR/CSR Variables
Part of exploring the temporal dynamics of SI involves not only the potential influences of key variables (i.e., affective sensitivity, peer invalidation) on subsequent SI, but also the potential effects of SI on the subsequent levels of those same variables. The effects of elevated SI at any given week may influence the levels of these contributing variables and potentially make them worse the subsequent week. In order to examine these effects, we created a lag-weekly SI variable in the same manner applied to the predictors in the previous analyses. Slightly modified HGLM equations as those portrayed previously were used for these analyses, with the exception that they involved multiple outcome variables with baseline and lag-weekly SI as the primary predictors (controlling again for age and sex).
Lag-weekly SI was a predictor of elevated affective sensitivity (β= .09, SE=.001, p<.001, RR = 1.09), negative affective intensity (β= .10, SE=.001, p<.001, RR = 1.10), behavioral dysregulation (β= .10, SE=.001, p<.001, RR = 1.10), peer invalidation (β= .09, SE=.001, p<.001, RR = 1.09) and family invalidation (β= .08, SE=.001, p<.001, RR = 1.08). Lag-weekly SI was not a significant predictor of the subsequent week’s level of depression (β= .01, SE=.01, p= .20). These findings suggest that SI may have reciprocal effects on the variables that may contribute to it, resulting in worse acute functioning.
Sex Moderation Effects
Because there may have been some sex effects, we reanalyzed the model including sex as a predictor of SI. Sex was a significant predictor of death/suicidal ideation (β = −.149, SE=.014, p<.001), indicating elevated SI for males. However, when sex was included in the model the primary path loadings and significant paths did not change, suggesting that sex was not solely driving the effects of some variables on SI. However, we examined the potential moderating influence of sex on the constructs using individual HGLM analyses. Because of the number of analyses, a Bonferroni corrected alpha of .003 to reduce Type 1 Error. Results indicated that results were primarily the same across sexes, with the exception of a few variables, including lag-weekly affective sensitivity (β= −.76, SE=.01, p<.001, RR = .47), baseline family invalidation (β= −.91, SE=.01, p<.001, RR = .40), lag-weekly family invalidation (β= −.76, SE=.01, p<.001, RR = .47), and lag-weekly behavioral dysregulation (β= −.75, SE=.01, p<.001, RR = .47). When graphed, each of the significant sex moderation effects indicated that when males experience elevated levels of these constructs, higher subsequently elevations in weekly SI were indicated.
Discussion
The purpose of this study was to explore important predictors of variability in death/suicidal ideation in adolescents over a six-month period. Significant associations were found between hypothesized constructs from Linehan’s (1993) theory and weekly level of SI, including both baseline and weekly assessments. Baseline SI and week-prior SI were among the strongest predictors of the experience of future elevations in SI. The findings can best be summarized as follows: 1) for the most part, concurrent significant positive correlations were found between suicidal ideation and each of the predictor constructs, for both baseline and throughout follow-up; 2) baseline indices of SI, affect sensitivity, and peer invalidation were significant positive, prospective predictors of elevated SI at any given week over the subsequent six months; 3) prior week levels of affective dysregulation, behavioral dysregulation, family and peer invalidation, and depression were all significant predictors of the subsequent week’s level of SI; and 4) prior week suicidal ideation significantly predicted subsequent elevated affective sensitivity, negative affective intensity, behavioral dysregulation, peer invalidation, and family invalidation. Collectively, these findings suggest that affective and behavioral dysregulation and invalidation are related to SI level both chronically (over months) and acutely (from one week to the next), and visa versa. Importantly, the primary constructs exhibited also demonstrated unique relations with SI, even when accounting for shared variance with the other variables.
Negative Affectivity and Suicidal Ideation
Results of this study provided further evidence for the link between affect dysregulation and SI, however, there were also some important differences between the two facets of affective dysregulation. First, it was both interesting and informative that negative affective intensity and affective sensitivity had different baseline prospective predictions, with affective sensitivity being a significant predictor of future levels of SI and negative affective intensity being non-predictive. This difference speaks to the notion that these are two different constructs embedded within the larger construct of affective dysregulation, which is arguably too heterogeneous. One potential explanation for this difference may be that experience of high negative affective intensity may tend to be more of a threshold predictor of experience of SI in general (yes/no). Affective sensitivity, on the other hand, may be a stronger contributor to fluctuations in level of SI. Future research should also examine the role of depression in moderating affective sensitivity and negative affective intensity in relation to SI, as there is some evidence that depressed adolescents demonstrate elevated levels of both (Larson et al., 1990).
The findings of the current study suggest that the affective dysregulation component of Linehan’s (1993) theory may have an even more important role on SI in adolescents, particularly given this group appears to be prone to more affective dysregulation than adults (Hare et al., 2008). Difficulties regulating affect in adolescence have also been found to predict continued difficulties into adulthood (Beauchaine & Neuhaus, 2008), suggesting that the link between SI and affective dysregulation may have its roots in adolescents. This may be because the ability to regulate affect is highly impacted by the family environment (Shipman & Zeman, 2001; Crowell et al., 2009). These findings bolster the need for early intervention regarding adaptive and health affect regulation skills, as learning these skills intuitively may not happen for some time. They also point out that a major component of affective dysregulation may be interpersonal, and in challenging family environments it can be difficult for adolescents to learn and apply adaptive skills. Thus, in treating affective dysregulation examining interpersonal facets of the adolescent’s life may be crucial.
Invalidation and Suicidal Ideation
Regarding invalidation, the baseline concurrent correlation for family invalidation and SI was positively correlated, as expected, while there was a significant negative correlation observed for the association between suicidal ideation and peer invalidation. One explanation for the reverse association for peer invalidation and suicidal ideation may be that patients may have experienced outreach and support from their peer network as a result of their suicidal crisis and hospitalization. Conversely, a psychiatric hospitalization is likely to cause more stress on a family, and potentially even more invalidation, thus potentially explaining the discrepant findings between peer and family invalidation and their respective association with concurrent baseline suicidal ideation.
Regarding the prospective and week-prior findings, baseline peer invalidation predicted elevated suicidal ideation during follow-up, and both peer and family invalidation one week predicted elevated SI the subsequent week during follow-up. These findings further highlight the role of invalidation in the fluctuation of SI, and lend further evidence to Linehan’s (1993) notion that invalidating environments may contribute to SI. Many of the findings regarding invalidation are also consistent with adult models of suicidality, such as the Interpersonal Theory of Suicide (Van Orden et al., 2010). In this model of suicide, one of the key factors necessary for severe suicidal behavior is feeling a lack of belonging. Based on these findings, it is not surprising that when adolescents are feeling invalidated by their family and friends they would experience increased death/suicidal ideation. Furthermore, perceived invalidation during childhood has been found to predicted increased relationship problems during adulthood (Selby et al., 2008), demonstrating the potential impact of invalidation on later development.
Behavioral Dysregulation and Suicidal Ideation
Behavioral dysregulation had a significant, yet negative, correlation with baseline suicidal ideation. On the other hand, it had a significant positive week-prior and concurrent week correlation with SI during the follow-up weeks. These differences may be due to the unique circumstances of hospitalization. As the baseline assessments were conducted during hospitalization and baseline scores were based on current week status, being in a restricted setting limits opportunities for behavioral dysregulation and problematic peer interactions. Additionally, although many in the sample made a suicide attempt that precipitated hospitalization, even those who did not attempt at the time of admission were at elevated risk and endorsed elevated SI. It may be that some adolescents rated themselves as being low on behavioral dysregulation because they did not attempt in the context of high SI.
The findings of this study show that the relationship between behavioral dysregulation and SI are complex and dynamic, especially in adolescence. Behavioral dysregulation may be particularly complex in adolescence, as similar behaviors in adulthood may be a bit more isolated (i.e. self-injury or drug use at home), yet in adolescence these behaviors also exist within the family environment (Crowell et al., 2009). Such behaviors occurring in adolescence may result in worsening attitudes from family or friends who have difficulty understanding the adolescent’s behavior and increase invalidating behavior (Linehan, 1993; Selby & Joiner, 2009), thus making an already bad situation even worse. Treating SI in adolescents may benefit not only from addressing issues with behavioral dysregulation, but also addressing family reactions to such behavior.
Influences of Suicidal Ideation
Finally, given the differences in short term and long term influence of affective dysregulation and peer invalidation on SI, it was somewhat surprising to find that the effects of SI on the subsequent weekly levels of all affect, behavioral, and invalidation variables were more stable. Essentially, the potential effects of affect dysregulation and peer invalidation on SI may be short-lived, for better or worse. Yet, the experience of SI may have detrimental effects on subsequent affective, interpersonal, and behavioral experience. This may be because of a positive feedback loop such that experience of suicidal ideation increase sensitivity and intensity of emotions, reduces the ability to handle stressful interpersonal problems, and increases behavioral dysregulation to cope with negative affect. These findings are in line with escape theories of suicide (Baumeister, 1990), which suggest that with increases of suicidal ideation individuals have more difficulty regulating stress and behavior due to the cognitive disruptions caused by SI. These findings also have important treatment implications, as teaching participants to use skills to cope with SI may be inhibited by the presence of SI, which may make it more difficult for those participants to implement skills. Additional care and attention to helping participants implement skills use in when experiencing SI may be warranted.
Moderation by Sex
When the predictors of weekly suicidal ideation were examined with regard to moderation by sex, most predictors were relatively the same across sex. However, males demonstrated higher weekly suicidal ideation if they also reported elevated baseline family invalidation, prior week family invalidation, prior week affective sensitivity, and prior week behavioral dysregulation. These findings may suggest that adolescent males may be more reactive to the family environment and experience of dysregulated behaviors, which may elevate subsequent SI. These findings suggest that special attention on these constructs in males demonstrating SI may be warranted in clinical assessments.
Limitations
There are some limitations with the current study that should be considered when interpreting the findings. First, variability in level of SI was examined at a weekly level. This can be problematic because SI has been found to fluctuate drastically even within days (Witte et al., 2006). Capturing suicidal ideation variability in finer time increments would need to be conducted in real-time via electronic means and this may be a direction for future research. Despite this limitation, this study finds a middle ground between rapidly fluctuating SI and chronic SI, capturing change on a macro-level. A second limitation was that the only truly prospective analyses in this study were baseline PSR/CSR measures predicting future weekly levels of SI, whereas the lag-week predictions of next-week SI were retrospective except at baseline, 2, 6, and 6-month ratings.
Another limitation was that the CSR variables were not previously validated prior to this study. In response to this concern we provided evidence of construct validity by finding significant positive correlations for the CSR variables with other validated measures and divergent validity from each other, suggesting that the CSR constructs demonstrated adequate validity for the analyses of the current study. Furthermore, the lack of previous validation of the CSR scales was ameliorated to some extent by the novelty of the approach of using these measures to assess construct levles on a weekly basis over 6 months, which allows for a more dynamic assessment of such constructs than a single administration self-report measure. Nonetheless, future validation work should be done with the CSR variables to confirm that they are valid construct measures. In addition to lack of previous validation, the CSR variables were assessed frequently and multiple times at each assessment, which may have resulted in potential reporting or recall bias, although the LIFE interview uses time anchors to help control for this issue.
In addition, all patients were hospitalized for suicide risk, exhibited very high levels of suicidal ideation, and received treatment. Hospitalization may have influenced the construct measures, potentially reducing experience of behavioral dysregulation or triggers of affective dysregulation, due to the restricted settings. However, the majority of the data was collected post-hospitalization, so these issues may be more relevant to the findings at baseline.” Future studies should also examine the potential role of response to treatment in relation to the variables in this study, as this study was a naturalistic following of adolescents who receive a variety of differing treatments. Finally, because data were not collected on participant’s consent/refusal rates, it is unclear how representative the study sample is relative to other hospitalized youth.
Conclusions
The findings of this study highlight the dynamic nature of SI in adolescents and some important factors that may contribute to fluctuations in SI. Importantly, baseline indices of SI, affect sensitivity, and peer invalidation were significant positive, prospective predictors of elevated SI and have important prognostic implications for adolescents hospitalized for suicidality. In clinical settings it is important to consider the impact of acute problems in these functional areas on elevations in SI, especially in adolescents. Furthermore, vigilant monitoring even in the face of perceived improvements may help decrease future suicidal behavior and hospitalizations. It may also be important for providers to have patience when anticipating improvements with respect to patients’ affective, behavioral, interpersonal functioning following elevated SI, as the findings of this study suggest that elevations in SI may have a lingering impact on functioning in patients with this level of acuity. With continued research of the various factors that contribute to SI, and changes in SI, we may be able to refine our assessment ability and possibly intervene sooner if adolescent patients reveal a pattern of elevated risk.
Acknowledgments
Funding for this project was provided by National Institute of Mental Health grant K23 MH069904 to Shirley Yen.
Footnotes
These κ-values are higher than κ-values for individual disorders likely because CSR variables consisted of only one scale score versus multiple scores for each of many diagnostic criteria for a diagnosis.
Regarding the HGLM models, the response distribution for SI was Poisson, which accounts for the count-nature distribution of the SI-CSR variable, with a natural logarithm transformation link so that it is consistent with the Poisson distribution. Level 1 assesses the weekly predictors of SI by adjusting the individual Level 2 intercept, and Level 2 assesses the baseline predictors of SI and includes a random intercept, with individual level error in measurement of weekly SI. The base model was an individual-level intercept for weekly SI modified by the week plus random error. The predictor model involved adding specific predictors to the base model. From each of the predictor weights we also calculated relative risk ratios (RR) which are standardized indices that indicate amount of changes in the level of the outcome variable (SI) relative to the change of each predictor variable by one standardized unit. Model comparison was evaluated with the following fit-indices: log-likelihood (H0), AIC, and BIC. Larger H0 values indicate better fit, whereas smaller AIC and BIC values indicate better fit (Burnham & Anderson, 2004). Based on these fit indices, the model with predictors (H0 = −4,769.61, AIC= 9,569.21, BIC = 9,655.19) provided incremental fit to the data beyond the baseline model (H0= −34,218.70, AIC=68,441.40, BIC=68,453.20). There was a significant random intercept in both the base model (β=2.31, SE=.011, p<.001) and the predictor model (β=5.64, SE=.001, p<.001).
Upon initial analysis, the majority of the week-prior predictors were significant inverse predictors of suicidal ideation, contrary to our hypotheses and previous research. This unexpected finding indicated that suppression effects might have resulted in the sign reversals for some predictors. Based on the recommendations by Gaylord-Harden et al. (2010), one major potential for net suppression (where the direction of a variable is the opposite direction as theoretically predicted) was the inclusion of multiple correlated measures in the prediction of SI. The recommended way to test for such suppression effects is to run the analysis with all predictors to determine significance, but then to run each predictor individually to determine if there was a change in the direction of the relationship. Gaylord-Harden et al. (2010) recommend that if the univariate analysis is in the expected direction, then the negative direction of the multivariate weight should not be interpreted as being in the opposite direction hypothesized. Upon examination with this approach, we indeed discovered that suppression was accounting for the reverse direction of most of the variables. As we originally expected, and consistent with previous research, week prior affective sensitivity, negative affect intensity, peer invalidation, and depression all significantly and positively predicted subsequent week SI level when examined individually. As in the original model, week prior family invalidation, behavioral dysregulation, and SI level maintained significant positive associations with SI. We also examined the significant baseline predictors in the model to ensure that suppression effects were not occurring with these variables. In these follow-up analyses, however, suppression effects were not indicated as all of the significant baseline predictors from the model maintained their significant paths in the original direction.
Contributor Information
Edward A. Selby, Department of Psychology, Rutgers University.
Anthony Spirito, Department of Psychiatry and Human Behavior, Warren Alpert Medical School of Brown University.
References
- Anderson TW. Maximum likelihood estimates for a multivariate normal distribution when some observations are missing. Journal of the American Statistical Association. 1957;52:200–203. [Google Scholar]
- Axelson D, Birmaher B, Brent D, et al. A preliminary study of the K-SADS Mania Rating Scale for children and adolescents. Journal of Child and Adolescent Psychopharmacology. 2003;13:463–470. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- Baumeister RF. Suicide as escape from self. Psychological Review. 1990;97:90–113. doi: 10.1037/0033-295x.97.1.90. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Neuhaus E. Impulsivity and vulnerability to psychopathology. In: Beauchaine TP, Hinshaw SP, editors. Child Psychopathology. Hoboken, NJ: Wiley; 2008. pp. 129–156. [Google Scholar]
- Beck AT, Brown GK, Steer RA, Dahlsgaard KK, Grisham JR. Suicide ideation at its worst point: A predictor of eventual suicide in psychiatric outpatients. Suicide and Life-Threatening Behavior. 1999;29:1–9. [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, Houck P, Ha W, Iyengar S, Kim E, Yen S, Hower H, Esposito C, Goldstein T, Ryan N, Keller M. Four-year longitudinal course of children and adolescents with bipolar spectrum disorder: The course and outcome of bipolar youth (COBY) study. American Journal of Psychiatry. 2009;166:795–804. doi: 10.1176/appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry. 2006;47:372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Greenhouse JB, Weldon AH, Campo JV, Kelleher KJ. Suicide trends among youths aged 10–19 years in the United States, 1996–2005. Journal of the American Medical Association. 2008;300:1025–1026. doi: 10.1001/jama.300.9.1025. [DOI] [PubMed] [Google Scholar]
- Brinkman-Sull DC, Overholster JC, Silverman E. Risk of future suicide attempts in adolescent psychiatric inpatients at 18-month follow-up. Suicide and Life-Threatening Behavior. 2000;30:327–340. [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Multimodel inference: Understanding AIC and BIC in model selection. Sociological Methods and Research. 2004;33:261–304. [Google Scholar]
- Buss AH, Perry M. The aggression questionnaire. Journal of Personality and Social Psychology. 1992;63:452–459. doi: 10.1037//0022-3514.63.3.452. [DOI] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality disorder: Elaborating and extending Linehan’s theory. Psychological Bulletin. 2009;135:495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Marsh DM, Papaqeorqiou DT, Swann AC, Moeller GF. Laboratory measured behavioral impulsivity relates to suicide attempt history. Suicide and Life-Threatening Behavior. 2004;34:374–385. doi: 10.1521/suli.34.4.374.53738. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Lim C, Brender ND, Wechsler H. Youth risk behavior surveillance- United States, 2007. Morbidity and Mortality Weekly Report Surveillance Summaries. 2008;57:1–131. [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. Journal of Marital and Family Therapy. 1983;9:171–180. [Google Scholar]
- Esposito C, Spirito A, Boergers J, Donaldson D. Affective, behavioral, and cognitive functioning in adolescents with multiple suicide attempts. Suicide and Life-Threatening Behavior. 2003;33:389–399. doi: 10.1521/suli.33.4.389.25231. [DOI] [PubMed] [Google Scholar]
- Gaylord-Harden NK, Cunningham JA, Holmbeck GN, Grant KE. Suppressor effects in coping research with African American adolescents from low-income communitites. Journal of Consulting and Clinical Psychology. 2010;78:843–855. doi: 10.1037/a0020063. [DOI] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Reboussin B, Reboussin D, Frazier PH, Harris A. Cognitive risk factors and suicide attempts among formerly hospitalized adolescents: A prospective naturalistic study. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:91–99. doi: 10.1097/00004583-200101000-00021. [DOI] [PubMed] [Google Scholar]
- Hare TA, Tottenham N, Galvan A, Voss HU, Glover GH, Casey BJ. Biological substrates of emotional reactivity and regulation in adolescence during an emotional go-nogo task. Biological Psychiatry. 2008;63:927–934. doi: 10.1016/j.biopsych.2008.03.015015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE, Rudd MD, Rajab MH. The modified scale for suicidal ideation: Factors of suicidality and their relation to clinical and diagnostic variables. Journal of Abnormal Psychology. 1997;106:260–265. doi: 10.1037//0021-843x.106.2.260. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Rudd MD, Rouleau MR, Wagner KD. Parameters of suicidal crises vary as a function of previous attempts in youth inpatients. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:876–880. doi: 10.1097/00004583-200007000-00016. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Sachs-Ericsson NJ, Wingate LR, Brown JS, Anestis MD, Selby EA. Childhood physical and sexual abuse and lifetime number of suicide attempts: A persistent and theoretically important relationshiop. Behaviour Research and Therapy. 2007;45:539–547. doi: 10.1016/j.brat.2006.04.007. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Walker RL, Rudd MD, Jobes DA. Scientizing and routinizing the assessment of suicidality in outpatient practice. Professional Psychology: Research and Practice. 1999;30:447–453. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2. New York: Guilford Press; 2005. [Google Scholar]
- Larsen RJ, Diener E. Affect intensity as an individual difference characteristic: A review. Journal of Research in Personality. 1987;21:1–39. [Google Scholar]
- Larsen RJ, Diener E, Cropanzano RS. Cognitive operations associated with individual differences in affect intensity. Journal of Personality and Social Psychology. 1987;53:767–774. doi: 10.1037//0022-3514.53.4.767. [DOI] [PubMed] [Google Scholar]
- Larson R, Raffaelli M, Richards MH, Ham M, Jewell L. Ecology of depression in late childhood and early adolescence: A profile of daily stress and activities. Journal of Abnormal Psychology. 1990;99:92–102. doi: 10.1037//0021-843x.99.1.92. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seely JR. Adolescent suicidal ideation and attempts: Prevalence, risk factors, and clinical implications. Clinical Psychology: Science and Practice. 1996;3:25–46. [Google Scholar]
- Linehan MM. Cognitive behavioral treatment of borderline personality disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- Mandrusiak M, Rudd MD, Joiner TE, Berman AL, Van Orden KA, Witte T. Warning signs for suicide on the internet: A descriptive study. Suicide and Life-Threatening Behavior. 2006;36:263–271. doi: 10.1521/suli.2006.36.3.263. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles: Author; 1998–2008. [Google Scholar]
- Miller IW, Epstein NB, Bishop DS, Keitner GI. The McMaster Family Assessment Device: Reliability and validity. Journal of Marital and Family Therapy. 1985;11:345–356. [Google Scholar]
- Nock MK, Prinstein MJ, Sterba SK. Revealing the form and function of self-injurious thoughts and behaviors: A real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology. 2009;118:816–827. doi: 10.1037/a0016948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A, Downs WR, Kopper B, Barrios FX, Baker MT, Osman JR, Besett TM, Linehan MM. The reasons for living inventory for adolescents (RFL-A): Development and psychometric properties. Journal of Clinical Psychology. 1998;54:1063–1078. doi: 10.1002/(sici)1097-4679(199812)54:8<1063::aid-jclp6>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Boergers J, Spirito A. Adolescents’ and their friends’ health-risk behavior: Factors that alter or add to peer influence. Journal of Pediatric Psychology. 2001;26:287–298. doi: 10.1093/jpepsy/26.5.287. [DOI] [PubMed] [Google Scholar]
- Reynolds WM. Suicide Ideation Questionnaire. Odessa, FL: Psychological Assessment Resources; 1985. [Google Scholar]
- Selby EA, Braithwaite SR, Joiner TE, Jr, Fincham FD. Features of borderline personality disorder, perceived childhood emotional invalidation, and dysfunction within current romantic relationships. Journal of Family Psychology. 2008;22:885–893. doi: 10.1037/a0013673. [DOI] [PubMed] [Google Scholar]
- Selby EA, Joiner TE., Jr Cascades of emotion: The emergence of borderline personality disorder from emotional and behavioral dysregulation. Review of General Psychology. 2009;13:219–229. doi: 10.1037/a0015687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shipman KL, Zeman J. Socialization of children’s emotion regulation in mother-child dyads: A developmental psychopathology perspective. Development and Psychopathology. 2001;13:317–336. doi: 10.1017/s0954579401002073. [DOI] [PubMed] [Google Scholar]
- Snijders W, Bosker R. Multilevel analysis: An introduction to basic and advanced multilevel modeling. London: Sage; 1999. [Google Scholar]
- Spirito A, Esposito-Smythers C. Attempted and completed suicide in adolescence. Annual Review of Clinical Psychology. 2006;2:237–266. doi: 10.1146/annurev.clinpsy.2.022305.095323. [DOI] [PubMed] [Google Scholar]
- Steer RA, Rissmiller DJ, Ranieri WF, Beck AT. Dimensions of suicidal ideation in psychiatric inpatients. Behaviour Research and Therapy. 1993;31:229–236. doi: 10.1016/0005-7967(93)90090-h. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Dyck I, Allsworth J, Stout RL, Keller MB. Maintaining reliability in a long-term monitoring program using the longitudinal interval follow-up evaluation. Journal of Psychiatric Research. 2001;35:297–305. doi: 10.1016/s0022-3956(01)00030-9. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Keller MB, Stout RL. Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. Journal of Psychiatric Research. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- Wilkinson P, Kelvin R, Roberts C, Dubicka B, Goodyer I. Nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT) American Journal of Psychiatry. 2011;168:495–501. doi: 10.1176/appi.ajp.2010.10050718. [DOI] [PubMed] [Google Scholar]
- Witte TK, Fitzpatrick KK, Joiner TE, Jr, Schmidt NB. Variability in suicidal ideation: A better predictor of suicide attempts than intensity or duration of ideation? Journal of Affective Disorders. 2005;88:131–136. doi: 10.1016/j.jad.2005.05.019. [DOI] [PubMed] [Google Scholar]
- Witte TK, Fitzpatrick KK, Warren KL, Schatschneider C, Schmidt NB. Naturalistic evaluation of suicidal ideation: Variability and relation to attempt status. Behaviour Research and Therapy. 2006;44:1029–1040. doi: 10.1016/j.brat.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea MT, Pagano M, Sanislow C, Grilo CM, McGlashan TH, Skodol AE, Bender DS, Zanarini MC, Gunderson JG, Morey LC. Axis I and axis II disorders as predictors of prospective suicide attempts: Findings from the collaborative longitudinal personality disorders study. Journal of Abnormal Psychology. 2003;112:375–381. doi: 10.1037/0021-843x.112.3.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Skodol AE, Grilo CM, Edelen RL, Stout RL, Morey LC, Zanarini MC, Markwitz JC, McGlashan TH, Daversa MT, Gunderson JG. Personality traits as prospective predictors of suicide attempts. Acta Psychiatrica Scandinavica. 2009;120:222–229. doi: 10.1111/j.1600-0447.2009.01366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoder KA, Whitbeck LB, Hoyt DR. Dimensionality of thoughts of death and suicide: Evidence from a study of homeless adolescents. Social Indicators Research. 2008;86:83–100. [Google Scholar]
- Zanarini MC, Frankenburg FR, Chauncey DL, Gunderson JG. The Diagnostic Interview for Personality Disorders: Interrater and test-retest reliability. Comprehensive Psychiatry. 1987;28:467–480. doi: 10.1016/0010-440x(87)90012-5. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Young L. The Diagnostic Interview for DSM-IV Personality Disorder. Belmont, MA: McLean Hospital, Laboratory for the Study of Adult Development; 1996. [Google Scholar]
- Zlotnick C, Donaldson D, Spirito A, Pearlstein T. Affect regulation and suicide attempts in adolescent inpatients. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:193–797. doi: 10.1097/00004583-199706000-00016. [DOI] [PubMed] [Google Scholar]