Abstract
Cognitive behavioral therapy (CBT) refers to a popular therapeutic approach that has been applied to a variety of problems. The goal of this review was to provide a comprehensive survey of meta-analyses examining the efficacy of CBT. We identified 269 meta-analytic studies and reviewed of those a representative sample of 106 meta-analyses examining CBT for the following problems: substance use disorder, schizophrenia and other psychotic disorders, depression and dysthymia, bipolar disorder, anxiety disorders, somatoform disorders, eating disorders, insomnia, personality disorders, anger and aggression, criminal behaviors, general stress, distress due to general medical conditions, chronic pain and fatigue, distress related to pregnancy complications and female hormonal conditions. Additional meta-analytic reviews examined the efficacy of CBT for various problems in children and elderly adults. The strongest support exists for CBT of anxiety disorders, somatoform disorders, bulimia, anger control problems, and general stress. Eleven studies compared response rates between CBT and other treatments or control conditions. CBT showed higher response rates than the comparison conditions in 7 of these reviews and only one review reported that CBT had lower response rates than comparison treatments. In general, the evidence-base of CBT is very strong. However, additional research is needed to examine the efficacy of CBT for randomized-controlled studies. Moreover, except for children and elderly populations, no meta-analytic studies of CBT have been reported on specific subgroups, such as ethnic minorities and low income samples.
Keywords: CBT, efficacy, meta-analyses, comprehensive review
Cognitive-behavioral therapy (CBT) refers to a class of interventions that share the basic premise that mental disorders and psychological distress are maintained by cognitive factors. The core premise of this treatment approach, as pioneered by Beck (1970) and Ellis (1962), holds that maladaptive cognitions contribute to the maintenance of emotional distress and behavioral problems. According to Beck’s model, these maladaptive cognitions include general beliefs, or schemas, about the world, the self, and the future, giving rise to specific and automatic thoughts in particular situations. The basic model posits that therapeutic strategies to change these maladaptive cognitions lead to changes in emotional distress and problematic behaviors.
Since these early formulations, a number of disorder-specific CBT protocols have been developed that specifically address various cognitive and behavioral maintenance factors of the various disorders. Although these disorder-specific treatment protocols show considerable differences in some of the specific treatment techniques, they all share the same core model and the general approach to treatment.
Consistent with the medical model of psychiatry, the overall goal of treatment is symptom reduction, improvement in functioning, and remission of the disorder. In order to achieve this goal, the patient becomes an active participant in a collaborative problem-solving process to test and challenge the validity of maladaptive cognitions and to modify maladaptive behavioral patterns. Thus, modern CBT refers to a family of interventions that combine a variety of cognitive, behavioral, and emotion-focused techniques (e.g., Hofmann, 2011; Hofmann, Asmundson, & Beck, in press). Although these strategies greatly emphasize cognitive factors, physiological, emotional, and behavioral components are also recognized for the role that they play in the maintenance of the disorder.
A recent review of meta-analyses of CBT identified 16 quantitative reviews that included 332 clinical trials covering 16 different disorders or populations (Butler, Chapman, Forman, & Beck, 2006). To our knowledge, this was the first review of meta-analytic studies examining the efficacy of CBT for a number of psychological disorders. This article has since become one of the most influential reviews of CBT. However, the search strategy was restrictive, because only one meta-analysis was selected for each disorder. Furthermore, the search only covered the period up to 2004, but many reviews have been published since then. In fact, the majority of studies (84%) was published after 2004. The goal of our review was to provide a comprehensive survey of all contemporary meta-analyses examining the evidence base for the efficacy of CBT to date. The meta-analyses included in the present review were all judged to be methodologically sound.
Methods
Search Strategy and Study Selection
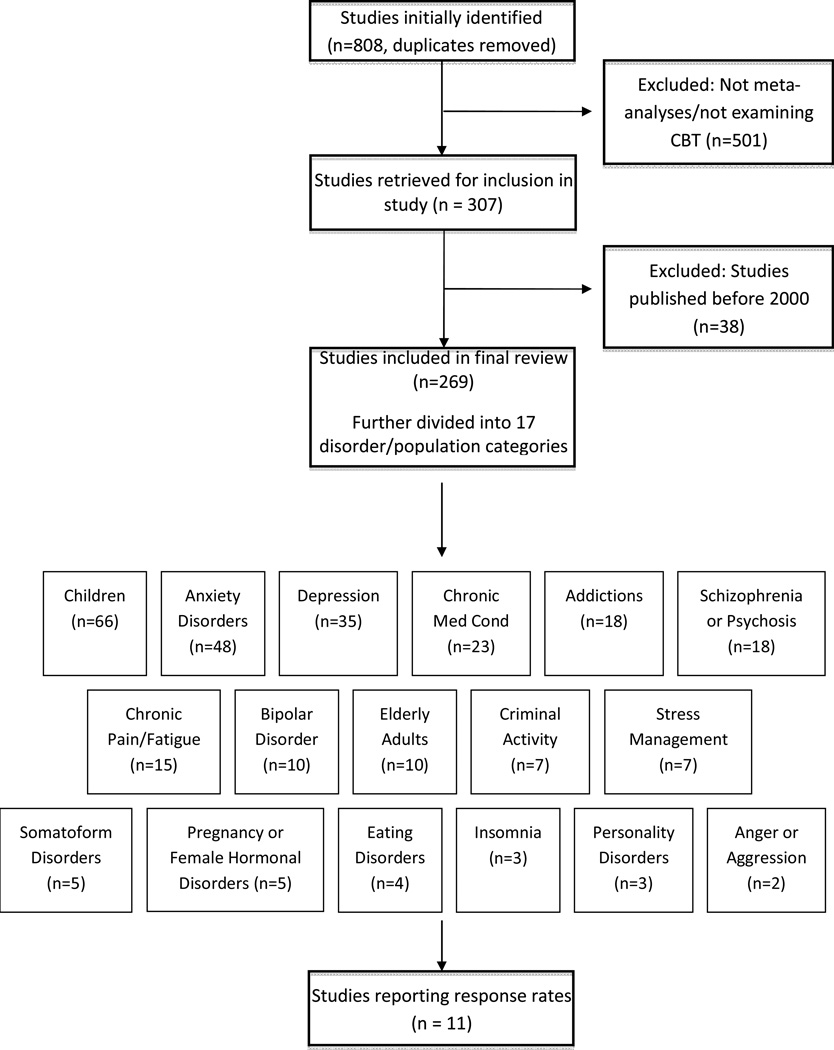
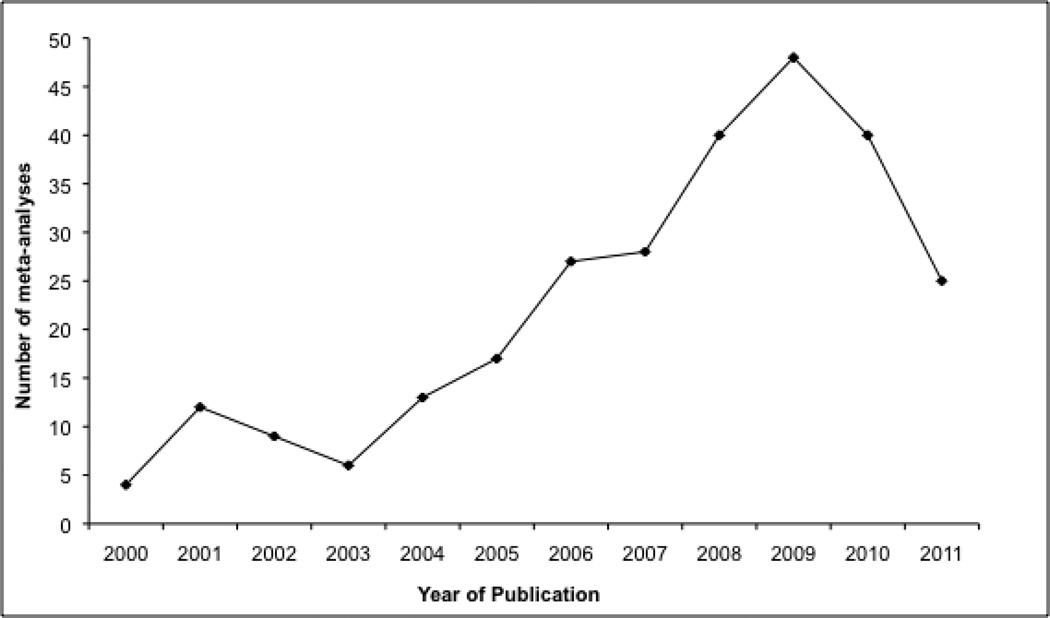
To obtain the articles for this review, we searched PubMed, PsychInfo, and Cochrane library databases using the following key words: meta-analysis AND cognitive behav*, meta-analysis AND cognitive therapy, quantitative review AND cognitive behav*, quantitative review AND cognitive therapy. This initial search yielded 1,163 hits, of which 355 were duplicates and had to be excluded. The remaining 808 non-duplicate articles were further examined to determine if they met specific inclusionary criteria for the purposes of this review. All included studies had to be quantitative reviews (i.e., meta-analyses) of CBT. In order to limit this review to contemporary studies, only articles published since 2000 were included. The final sample included in this review consisted of 269 meta-analyses (Figure 1). Out of those, we described a representative sample of 106 meta-analytic studies. The complete reference list for the final sample of included meta-analyses can be obtained by accessing the webpage www.bostonanxiety.org/cbtreview.html. As already noted, the majority (84%) of these studies was published after 2004, the most recent year covered by the meta-analysis by Butler and colleagues (2006). The number of meta-analytic reviews per year is depicted in Figure 2.
Figure 1.
Flow diagram showing effects of inclusionary and exclusionary criteria on final sample selection.
Figure 2.
Number of meta-analyses published by year since 2000. Note that the number of studies corresponding to 2011 only covered studies until September of that year.
Categorization of Meta-analyses
The 269 meta-analyses were categorized into groups to provide the most meaningful and extensive examination of the efficacy of CBT across a range of problem areas and study populations. The major groupings were the following: substance use disorder, schizophrenia and other psychotic disorders, depression and dysthymia, bipolar disorder, anxiety disorders, somatoform disorders, eating disorders, insomnia, personality disorders, anger and aggression, criminal behaviors, general stress, distress due to general medical conditions, chronic pain and fatigue, pregnancy complications and female hormonal conditions. In addition, some meta-analyses specifically examined CBT for disorders in children and elderly adults. For each disorder and population grouping, data were described qualitatively, considering the findings of all meta-analyses within that group. The 269 meta-analyses included a wide variety of studies that employed different methodologies and effect size estimates. Therefore, we used the designation small, medium, and large for the magnitude of effect sizes in our review of the 106 representative meta-analyses (Cohen, 1988). In addition, we provide reported response rates, a widely accepted and common metric in psychiatry, from a subsample of 11 studies that examined the efficacy of CBT in randomized controlled trials.
Results
Addiction and Substance Use Disoder
There was evidence for the efficacy of CBT for cannabis dependence, with evidence for higher efficacy of multi-session CBT versus single session or other briefer interventions, and a lower drop out rate compared to control conditions (Dutra et al., 2008). However, the effect size of CBT was small as compared to other psychosocial interventions (e.g. contingency management, relapse prevention, and motivational approaches) for substance dependence, and agonist treatments showed a greater effect size than CBT in certain drug dependencies, such as opioid and alcohol dependence (Powers, Vedel, & Emmelkamp, 2008).
Treatments for smoking cessation found that coping skills, which were partially based on CBT techniques, were highly effective in reducing relapse in a community sample of nicotine quitters (Song, Huttunen-Lenz, & Holland, 2010), and another meta-analysis noted superiority of CBT (either alone or in combination with nicotine replacement therapy) over nicotine replacement therapy alone (Garcia-Vera & Sanz, 2006). Furthermore, there was evidence for superior performance of behavioral approaches in the treatment of problematic gambling as compared to control treatments (Oakley-Browne et al., 2000). One meta-analysis (Leung & Cottler, 2009) reported larger effect sizes of CBT when this treatment was grouped with other non-pharmacological treatments (such as brief interventions) as compared to pharmacological agents (e.g. naltrexone, carbamazepine, and topiramate), but CBT was not more efficacious than these other briefer, less expensive approaches.
Schizophrenia and Other Psychotic Disorders
Meta-analyses examining the efficacy of psychological treatments for schizophrenia revealed a beneficial effect of CBT on positive symptoms (i.e., delusions and/or hallucinations) of schizophrenia (e.g., Gould et al., 2001; Rector & Beck, 2001). There was also evidence (e.g., Zimmerman et al., 2005) that CBT is a particularly promising adjunct to pharmacotherapy for schizophrenia patients who suffer from an acute episode of psychosis rather than a more chronic condition.
CBT appeared to have little effect on relapse or hospital admission compared to other interventions, such as early intervention services or family intervention (e.g., Bird et al., 2010; Álvarez-Jiménez et al., 2011). However, CBT had a beneficial effect on secondary outcomes. For example, a more recent meta-analysis by Wykes and colleagues (2008) examined controlled trials of CBT for schizophrenia and confirmed findings from previous meta-analyses (e.g., Gould et al., 2001; Rector & Beck, 2001), suggesting that CBT had a small to medium effect size as compared to control conditions on both positive and negative symptoms. In addition, this meta-analysis revealed medium effect sizes for improvements in secondary outcomes that were not the direct targets of treatment, including general functioning, mood, and social anxiety.
Depression and Dysthymia
CBT for depression was more effective than control conditions such as waiting list or no treatment, with a medium effect size (van Straten, Geraedts, Verdonck-de Leeuw, Andersson, & Cuijpers, 2010; Beltman, Oude Voshaar, & Speckens, 2010). However, studies that compared CBT to other active treatments, such as psychodynamic treatment, problem-solving therapy, and interpersonal psychotherapy, found mixed results. Specifically, meta-analyses found CBT to be equally effective in comparison to other psychological treatments (e.g., Beltman, Oude Voshaar, & Speckens, 2010; Cuijpers, Smit, Bohlmeijer, Hollon, & Andersson, 2010; Pfeiffer, Heisler, Piette, Rogers, & Valenstein, 2011). Other studies, however, found favorable results for CBT (e.g. Di Giulio, 2010; Jorm, Morgan, & Hetrick, 2008; Tolin, 2010). For example, Jorm and colleagues (2008) found CBT to be superior to relaxation techniques at post-treatment. Additionally, Tolin (2010) showed CBT to be superior to psychodynamic therapy at both post-treatment and at six months follow-up, although this occurred when depression and anxiety symptoms were examined together.
Compared to pharmacological approaches, CBT and medication treatments had similar effects on chronic depressive symptoms, with effect sizes in the medium-large range (Vos, Haby, Barendregt, Kruijshaar, Corry, & Andrews, 2004). Other studies indicated that pharmacotherapy could be a useful addition to CBT; specifically, combination therapy of CBT with pharmacotherapy was more effective in comparison to CBT alone (Chan, 2006).
Bipolar Disorder
Meta-analyses examining the efficacy of CBT for bipolar disorder revealed small to medium overall effect sizes of CBT at post-treatment, with effects typically diminishing slightly at follow-up. These findings emerged from examinations of both manic and depressive symptoms associated with bipolar disorder (e.g., Gregory, 2010a, 2010b). There is little evidence that CBT as a stand-alone treatment (rather than as an adjunct to pharmacotherapy) is effective for the treatment of bipolar disorder.
In addition to examining CBT for attenuating symptoms of bipolar disorder, some meta-analyses focused on the efficacy of CBT for preventing relapse in bipolar patients. One study (Beynon et al., 2008) examined the efficacy of CBT for preventing relapse and found it to be somewhat effective when comparing CBT vs. treatment as usual. Overall, CBT for bipolar disorder was an effective method of preventing or delaying relapses (e.g., Lam, Burbeck, Wright, & Pilling, 2009; Cakir & Ozerdem, 2010). Furthermore, the efficacy of CBT at preventing relapse did not seem to be influenced by the number of previous manic or depressive episodes.
Anxiety Disorders
In general, CBT is a reliable first-line approach for treatment of this class of disorders (Hofmann & Smits, 2008), with support for significant positive effects of CBT on secondary symptoms such as sleep dysfunction and anxiety sensitivity (Ghahramanlou, 2003). Further, internet-delivered or guided self-help CBT showed some promise in immediate symptom relief as compared to no treatment, but the long-term maintenance with this modality of CBT remains unclear (Öst, 2008; Coull & Morris, 2011).
CBT for social anxiety disorder evidenced a medium to large effect size at immediate post-treatment as compared to control or waitlist treatments, with significant maintenance and even improvement of gains at follow-up (Gil, Carrillo, & Meca, 2001). Further, exposure, cognitive restructuring, social skills training and both group/individual formats were equally efficacious (Powers, Sigmarsson, & Emmelkamp, 2008), with superior performance over psychopharmacology in the long term (Fedoroff & Taylor, 2001). Similarly, interoceptive exposure for treatment of panic disorder was moderately effective and superior to control/pill placebo treatments and applied relaxation (Haby, Donnelly, Corry, & Vos, 2006; Furukawa, Watanabe, & Churchill, 2007). For panic disorder without agoraphobia, combination treatment of CBT and applied relaxation was equal in efficacy to use of either therapy approach alone, and use of either or both were superior to use of medications (Mitte, 2005).
Various CBT techniques for specific phobia (systematic desensitization, exposure, cognitive therapy) were as effective as applied relaxation and applied tension, producing effect sizes in the large range, with long-term maintenance of gains (Ruhmland & Margraf, 2001). For generalized anxiety disorder, CBT was superior as compared to control or pill placebo conditions, and equally efficacious as relaxation therapy, supportive therapy, or psychopharmacology, but less efficacious in comparison to attention placebos and in those with more severe generalized anxiety disorder symptoms.
CBT for post-traumatic stress disorder was equal in efficacy to eye movement desensitization and reprocessing (Bisson et al., 2007), with both being superior to treatment as usual, waitlist, or other treatments (such as supportive counseling) for post-traumatic stress disorder (Bisson & Andrew, 2008). However, it is questionable whether the eye-movement technique is an active treatment ingredient.
Clinical trials also revealed a large effect size for CBT and/or exposure response prevention for obsessive compulsive disorder, with evidence suggesting that a combination of in vivo and imaginal exposures outperformed the use of only in vivo exposures (Ruhmland & Margraf, 2001). Furthermore, CBT was found to be similarly efficacious than clomipramine and selective reuptake inhibitors (Eddy, Dutra, Bradley, & Westen, 2004).
Somatoform Disorders
Within the somatoform disorders category of DSM-IV, meta-analyses primarily examined the efficacy of psychological interventions for hypochondriasis and body dysmorphic disorder. One meta-analysis found a large mean effect size for CBT, which outperformed other psychological treatments (i.e., psychoeducation, explanatory therapy, cognitive therapy, exposure and response prevention, and behavioral stress management), with effect sizes in the large range, as well as pharmacotherapy treatments (paroxetine, fluoxetine, fluvoxamine, and nefazodone), which also evidenced large effect sizes (Taylor, Asmundson, & Coons, 2005). The mean effect size for control conditions (e.g., wait-list control) was small. These results were partially supported by other evidence, as a more recent meta-analysis found superior outcomes of CBT for hypochondriasis compared to waiting list control, usual medical care or placebo at twelve-month follow-up (Thomson & Page, 2007). However, this meta-analysis also found no differences between CBT and waiting list/placebo at post-treatment.
Meta-analyses comparing the efficacy of CBT to control treatments found that CBT was superior in significantly reducing body dysmorphic disorder symptoms (Ipser, Sander, & Stein, 2009). In comparing relative efficacy of CBT versus pharmacotherapy, effect sizes were large on body dysmorphic disorder severity measures for CBT, and ranged from medium to large for pharmacotherapy (Williams, Hadjistavropoulos, & Sharpe, 2006). In addition, another meta-analysis found that CBT for body image disturbances was effective, with effect sizes ranging from medium to large (Jarry & Ip, 2005).
Eating Disorders
For bulimia nervosa, meta-analyses compared the efficacy of CBT to control treatments and found effect sizes in the medium range (Thompson-Brenner, 2002). However, the effect of behavior therapy was greater than that of CBT, with the average effect size for behavior therapy in the large range (Thompson-Brenner, 2003). Another meta-analysis comparing CBT with control treatments found remission response rates to be higher for CBT, with a medium relative risk ratio (Hay, Bacaltchuk, Stefano, & Kashyap, 2009). When comparing CBT to other psychotherapies, specifically, interpersonal therapy, dialectical behavioral therapy, hypno-behavioral therapy, supportive psychotherapy, behavioral weight loss treatment, and self-monitoring, CBT fared significantly better in remission response rates for bulimia nervosa, with a large relative risk ratio (Hay et al., 2009).
For binge eating disorder, a recent meta-analysis found that psychotherapy and structured self-help yielded large effect sizes, when compared to pharmacotherapy, which yielded medium effect sizes (Vocks et al., 2010). Although this study did not parse out the efficacy of CBT specifically, a majority of the included trials for psychotherapy involved CBT (19 out of 23 trials). Furthermore, a review and meta-analysis by Reas and Grilo (2008) suggested that combination treatment of psychotherapy and medications did not enhance binge-eating outcomes, but may have enhanced weight loss outcomes.
Insomnia
CBT for insomnia (CBT-I) has long been shown to be more efficacious than control treatments. A recent meta-analysis examined its efficacy on both subjective and objective sleep parameters in comparison to a control group for individuals with primary insomnia (Okajima, Komada, & Inoue, 2011). Effect sizes for the efficacy of CBT-I versus control at the end of treatment on subjective sleep measures, which included sleep onset latency, total sleep time, wake after sleep onset, total wake time, time in bed, early morning awakening, and sleep efficiency, ranged from minimal (total sleep time) to large (early morning awakening) (Okajima et al., 2011). For objective measures using a polysomnogram or actigraphic evaluation, effect sizes ranged from small (total sleep time) to large (total wake time) (Okajima et al., 2011). These findings were consistent with results from another meta-analysis, which examined the relative efficacy of behavioral interventions for insomnia including CBT, relaxation, and only behavioral techniques (Irwin, Cole, & Nicassio, 2006). This study reported effect sizes ranging from −.75 to 1.47 for CBT, −.60 to .53 for relaxation techniques, and −.82 to .91 for only behavioral techniques on subjective sleep outcomes.
Personality Disorders
There was one meta-analysis that examined the relative efficacy of CBT versus psychodynamic therapy for the treatment of personality disorders (Leichsenring & Leibing, 2003). The findings indicated a larger overall effect size for psychodynamic therapy compared to CBT. This was consistent with observer-rated measures, which showed a similar pattern of effect sizes: stronger for psychodynamic therapy than for CBT (although this effect size was also large). Self-report measures, however, indicated larger effect sizes for CBT than for psychodynamic therapy.
Another meta-analysis compared the efficacy of eleven different psychological therapies, including CBT, for antisocial personality disorder (Gibbon et al., 2010). Results suggested that compared to control treatment, CBT plus standard maintenance was more efficacious in terms of leaving the study early and cocaine use for outpatients with antisocial personality disorder and comorbid cocaine dependence. However, CBT plus treatment as usual was not better than a control condition for these antisocial personality disorder patients with regard to levels of recent verbal or physical aggression. The relative efficacy of psychological treatments for borderline personality disorder, in particular, was also examined, which yielded no differences between dialectical behavioral therapy and treatment as usual in individuals meeting criteria for borderline personality disorder at six months, or in hospital admissions in the previous three months (Binks et al., 2009).
Anger and Aggression
Two meta-analytic reviews focused on anger control problems and aggression (Del Vecchio & O’Leary, 2004; Saini, 2009). The findings from these meta-analyses suggested that CBT is moderately effective at reducing anger problems. Findings from these reviews also suggested that CBT may be most effective for patients with issues regarding anger expression.
CBT produced medium effect sizes as compared to other psychosocial treatments and control conditions across the two reviews that conducted quantitative analyses. A meta-analysis on the effectiveness of anger treatments for specific anger problems (Del Vecchio & O’Leary, 2004) included only studies in which subjects met clinically significant levels of anger on standardized anger measurements prior to treatment. This meta-analysis examined the effects of CBT, cognitive therapy, relaxation, and ‘other’ (e.g., social skills training, process group counseling) on various anger problems including driving anger, anger suppression, and anger expression difficulties.
Criminal Behaviors
Four separate meta-analytic studies supported the efficacy of CBT for criminal offenders (Illescas, Sanchez-Meca, & Genovés, 2001; Lösel & Schmucker, 2005; Pearson, Lipton, Cleland, & Yee, 2002; Wilson, Bouffard, Mackenzie, 2005). Out of several theoretical orientations and types of psychological interventions for criminal activity, behavior therapy and CBT appeared to be the superior interventions in reducing recidivism rates, both with medium mean effect sizes (Illescas, Sanchez-Meca, & Genovés, 2001). Effect sizes for other interventions ranged from small to medium (Illescas et al., 2001). Another study demonstrated consistent findings with a small weighted mean effect size of behavior therapy or CBT for reducing recidivism (Pearson, Lipton, Cleland, & Yee, 2002). Similarly, Wilson and colleagues (2005) found an overall small-to-medium mean effect size for CBT programs for convicted offenders.
For sexual offenders in particular, physical treatments, such as surgical castration and hormonal treatment, were demonstrated to have greater efficacy in reducing sexual recidivism in comparison to CBT, with large significant odds ratios for both of these alternative interventions (Lösel & Schmucker, 2005). Of the various psychological interventions for sexual offenders, however, classical behavioral and CBT approaches indicated the strongest efficacy, with odds ratios in the medium to large range (Lösel & Schmucker, 2005) as compared to insight-oriented and therapeutic community interventions.
A study of CBT for domestic violence indicated no differences between CBT and the Duluth model (which is based on a feminist psycho-educational approach) for treating domestically violent males (Babcock, Green, & Robie, 2004). The aggregated data from experimental and quasi-experimental studies showed that CBT had an overall small effect size, and the Duluth model had an overall slightly larger, but still small effect size (Babcock et al., 2004).
General Stress
Four meta-analyses examined occupational stress and the majority of their results were quite similar: CBT interventions were more effective in comparison to other intervention types such as organization focused therapies, especially when CBT focused on psycho-social outcomes in employees (Kim, 2007; Richardson & Rothstein, 2008; van der Klink, Blonk, Schene, & van Dijk, 2001). For example, Richardson and Rothstein (2008) found CBT alone to be more effective in comparison to CBT combined with additional psychological components. These studies found a large effect size for overall CBT interventions, large effect size for single-mode CBT interventions, and small effect size for CBT interventions with four or more components. In contrast, Marine and colleagues (2006) chose not to compare CBT with other interventions, such as relaxation techniques for psychological stress, because most interventions comprised both elements and could not be evaluated separately. With respect to stress in parents of children with developmental disabilities, positive effects were found for CBT, but the effect size was relatively small (Singer, Ethridge, & Aldana, 2007). In contrast to the results of Richardson and Rothstein (2008), this meta-analysis found multiple component interventions which combined CBT, behavioral parent training and in some cases other forms of support services, to have a higher and large effect size in comparison to CBT alone (Singer, Ethridge, & Aldana, 2007).
Distress Due to General Medical Conditions
Limited well-controlled studies existed in the study of non-ulcer dyspepsia, multiple sclerosis, physical disability following traumatic injury, non-epileptic seizures, post-concussion syndrome, chronic obstructive pulmonary disease, hypertension, Type II diabetes, and burning mouth syndrome (e.g. Soo et al., 2004; Thomas, Thomas, Hillier, Galvin, & Baker, 2006; Baker, Brooks, Goodfellow, Bodde, & Aldenkamp, 2007; Ismail, Winkley, & Rabe-Hesketh, 2004). However, cancer was studied more rigorously and with more robust methodological attention, indicating small to medium effect sizes of individual CBT as compared to patient education only in gynecological and head/neck cancers (Zimmerman & Heinrichs, 2006; Luckett, Britton, Clover, & Rankin, 2011), on secondary outcomes such as quality of life, psychological distress (i.e., depression and anxiety), and pain. Further, CBT was shown to be equally effective as exercise interventions in treating cancer-related fatigue (Kangas, Bovbjerg, & Montgomery, 2008).
Small to medium effect sizes were observed in treatment of secondary symptoms (anxiety and stress) experienced by individuals who were HIV positive, with particular efficacy (particularly for stress management) in reducing anger symptoms as compared to supportive therapy (Crepaz et al., 2008), but not for outcomes such as low cell count, medication adherence, or when used with marginalized populations such as ethnic minorities and women (Crepaz et al., 2008; Rueda et al., 2006).
CBT was shown to be superior in the treatment of secondary symptoms of spinal cord injury as compared to controls in assertiveness skills, coping, depression and quality of life (Dorstyn, Mathias, & Denson, 2011), better than placebo or diet/exercise alone (Shaw, O’Rourke, Del Mar, & Kenardy, 2005), but equal to yoga/education in depressive symptoms (Martinez-Devesa, Perera, Theodoulou, & Waddell, 2010). CBT was only slightly more effective than usual care or waitlist condition in the treatment of irritable bowel syndrome, with peppermint oil having greater efficacy in providing relief in this particular disorder (Enck, Junne, Klosterhalfen, Zipfel, & Martens, 2010).
Chronic Pain and Fatigue
Meta-analyses examining the efficacy of psychosocial treatments for chronic pain have investigated chronic low back pain, fibromyalgia, rheumatoid arthritis, chronic fatigue syndrome, chronic musculoskeletal pain, and non-specific chest pain. These reviews have examined the effect of a range on treatments on chronic pain, including relaxation techniques, mindfulness-based techniques, acceptance-based techniques, biofeedback, psycho-education, and behavioral and cognitive-behavioral treatments. Results of these meta-analyses revealed varying effect sizes for these treatments depending on the type of chronic pain targeted; however, CBT treatments for chronic pain were consistently in the small to medium effect size range.
Similar results were found in a meta-analysis examining psychological treatments for fibromyalgia (Glombiewski et al., 2010). This meta-analysis revealed that CBT was superior to other psychological treatments for decreasing pain intensity. Pre-post analyses revealed a medium effect size for CBT as compared to a small effect size for all other psychological treatments combined (excluding CBT). CBT treatments for chronic fatigue syndrome were moderately effective (e.g., Malouff et al., 2008; Price et al., 2008). Malouff and colleagues (2008) conducted a meta-analysis revealing a medium effect size in post-treatment fatigue for participants receiving CBT versus those in control conditions.
Pregnancy Complications and Female Hormonal Conditions
One meta-analysis found CBT to be more effective in comparison to control conditions for perinatal depression (Sockol, Epperson, & Barber, 2011), and another meta-analysis found beneficial effects of CBT for postnatal depression, but these results need to be interpreted with caution because it is difficult to causally link depression with pregnancy and hormonal changes in these studies (Dennis, & Hodnett, 2007). Further, Bledsoe and Grote (2006) found greater decreases in depression for women experiencing non-psychotic major depression in pregnancy and postnatal periods treated with combination treatment in comparison to antidepressant medication alone, which was itself more effective in comparison to CBT alone. The effect size for postnatal treatments was large in comparison to the small to medium effects of prenatal treatments, but when pharmacological treatments were excluded, the effect size for postnatal treatments decreased to the medium range.
For the treatment of premenstrual syndrome, Busse and colleagues (2009) found that CBT significantly reduced depressive and anxiety symptoms associated with this syndrome, as indicated by a medium effect size. Once again, these results need to be interpreted carefully due to the small number of well-controlled studies on which these reviews were based.
CBT for Special Populations
Children
Within internalizing symptoms, there was support for the preferential use of CBT approaches in treatment of anxiety disorders in children and adolescents, with effect sizes in the large range (Santacruz et al., 2002; James, Soler, & Weatherall, 2005). Further, CBT treatment for obsessive compulsive disorder as compared to alternative approaches (no treatment, other psychosocial treatments and medications such as clomipramine and fluvoxamine) resulted in significantly better outcomes (Phillips, 2003; Guggisberg, 2005). The data supporting CBT for depression was less strong, but still in the medium effect size range across meta-analyses, with maintenance in 6-month follow-up periods (Santacruz et al., 2002). In addition, CBT seemed to work equally well as other psychotherapies (i.e. interpersonal therapy and family systems therapy), but was regarded as superior to selective reuptake inhibitors due to reduced chance of side effects and greater cost effectiveness (Haby, Tonge, Littlefield, Carter & Vos, 2004). The studies on efficacy of CBT for addressing suicidal behaviors were scarce (Robinson, Hetrick, & Martin, 2011), and warrant further investigation.
The picture was more mixed for other disorders, with CBT showing equal efficacy in reducing disruptive classroom behaviors and aggressive/antisocial behaviors, as other psychosocial treatments, better efficacy as compared to no treatment or treatment as usual, and less efficacy than pharmacological approaches (Lösel & Beelmann, 2003; Özabaci, 2011). Similarly, CBT for attention deficit hyperactivity disorder showed some efficacy, but was not superior to medications (Van der Oord, Prins, Oosterlaan, & Emmelkamp, 2008). The efficacy of behavioral techniques (e.g. motivational enhancement and behavioral contingencies) was small to medium for the treatment of adolescent smoking and substance use as compared to no treatment, but not more so than other psychotherapies. In addition, there was a medium to large effect size of CBT over waitlist across meta-analyses examining chronic headache pain. Finally, the data on efficacy for CBT in juvenile sex offenders, childhood sexual abuse survivors, childhood obesity, fecal incontinence, and juvenile diabetes was limited, showing preliminary support for CBT as compared to no treatment, but equal efficacy to other psychosocial approaches (Walker, McGovern, Poey, & Otis, 2005; Macdonald, Higgins, & Ramchandani, 2006).
Elderly Adults
With respect to mood disorders, with depression as the most commonly examined disorder, nearly all meta-analyses showed that CBT was more effective than waiting list control conditions, but equally effective in comparison to other active treatment methods, such as reminiscence, (an intervention that uses recall of past events, feelings and thoughts to facilitate pleasure, quality of life or adaptation to the present; Peng, Huang, Chen, & Lu, 2009), psychodynamic therapy, and interpersonal therapy (Krishna et al., 2011; Wilson, Mottram, & Vassilas, 2008). Pinquart and colleagues (2007), however, found a large effect size for CBT, whereas the effect sizes for the other active treatment conditions were in the medium-large range. When long-term outcomes were examined, results of one meta-analysis indicated that treatment gains of CBT for depression were maintained at 11-months follow-up (Krishna et al., 2011), but long-term follow-up data remained scarce in the other meta-analyses. In a meta-analysis assessing the additive effects of CBT and pharmacological approaches, Peng and colleagues (2009) found that CBT was more effective in comparison to placebo, but CBT as an adjunct to antidepressant medication did not increase the effectiveness of antidepressants in this population.
For anxiety disorders in the elderly, CBT (alone or augmented with relaxation training) did not enhance outcomes beyond relaxation training alone (Thorp et al., 2009), although many of these studies were uncontrolled. In contrast to the findings by Thorp and colleagues (2009), Hendriks and colleagues (2008) found that anxiety symptoms were significantly decreased following CBT than after either a waiting-list control condition or other treatment methods. Additionally, CBT significantly alleviated accompanying symptoms of worry and depression when compared to waiting-list control or an active control condition.
Response Rates of Randomized Controlled Studies
The meta-analytic studies that provided response rates are listed in Table 1. The response rates of CBT varied between 38% for treating obsessive compulsive disorder (Eddy et al., 2004) and 82% for treating body dysmorphic disorder (Ipser et al, 2009). In contrast, the response rates of the waitlist groups ranged from 2% for the treatment of bulimia nervosa (Thompson-Brenner, 2003) to 14% for generalized anxiety disorder (Hunot et al., 2007). CBT also demonstrated higher response rates in comparison to treatment as usual in treatment of generalized anxiety disorder and chronic fatigue (Price et al., 2008), and higher or equal response rates as compared to other therapies or psychopharmacological interventions in most studies. CBT only produced a lower response rate than psychodynamic therapy for the personality disorders (47% vs. 59%; Leichsenring & Leibing, 2003).
Table 1.
Pooled meta-analytic response rates for CBT versus other conditions across disorders.
| Disorder | Author (year) | Number of Studies |
CBT | MED | OT | PBO | TAU | WL | Comparison |
|---|---|---|---|---|---|---|---|---|---|
| Boderline Personality Disorder |
Ipser et al. (2009) | 2 | 82%1 | 56%1 | - | 18%1 | - | - | CBT, MED>PBO |
| Panic disorder | Siev et al. (2008) | 5 | 77% | - | 50% | - | - | - | CBT>OT |
| Anger/Aggression | Del Vecchio & O'Leary (2004) | 23 | 66–69% | - | 65–70% | - | - | - | CBT = OT |
| Depression | Leichsenring (2001) | 6 | 51–87% | - | 45–70% | - | - | - | CBT>OT |
| Childhood Anxiety | James et al. (2005) | 13 | 56% | - | - | 28%2 | - | - | CBT>PBO |
| Chronic Fatigue | Malouff et al. (2008) | 5 | 50% | - | - | - | - | - | - |
| Personality Disorders | Leichsenring & Leibing (2003) | 25 | 47%3 | - | 59%4 | - | - | - | CBT<OT |
| Generalized Anxiety Disorder |
Hunot et al. (2007) | 8 | 46%5 | - | - | - | 14% | 14% | CBT=OT; CBT>TAU,WL |
| Chronic Fatigue | Price et al. (2008) | 6 | 40% | - | - | - | 26% | - | CBT>TAU |
| Bulimia Nervosa | Thompson-Brenner (2003) | 26 | 40–44% | - | - | 27% | - | 2% | CBT>PBO, WL |
| Obsessive Compulsive Disorder |
Eddy et al. (2004) | 3 | 38–50% | - | - | - | - | - | - |
Note. The table shows response rate percentages for CBT (from highest to lowest) compared to each comparison condition for every meta-analaytic study reporting such data across disorder groups; -: no data reported; >: higher efficacy; <: lower efficacy; =: equal efficacy. MED = Medication/ pharmacological approaches; OT = Other therapies (consisting of relaxation therapy, supportive therapy, or psychodynamic therapy); PBO = placebo/control treatments; TAU= Treatment as usual; WL= Waitlist treatment; BDD: Body dysmorphic disorder; PD: Panic disorder without agoraphobia; GAD = Generalized anxiety disorder; OCD = Obsessive-compulsive disorder.
One study;
heterogeneous response rate pooling placebo/control, waitlist, and supportive treatment conditions;
11 studies;
14 studies;
response rate of OT not reported in paper; stated as being equal to CBT (as indicated in comparison column)
Discussion
CBT is arguably the most widely studied form of psychotherapy. We identified 269 meta-analytic reviews that examined CBT for a variety of problems, including substance use disorder, schizophrenia and other psychotic disorders, depression and dysthymia, bipolar disorder, anxiety disorders, somatoform disorders, eating disorders, insomnia, personality disorders, anger and aggression, criminal behaviors, general stress, distress due to general medical conditions, chronic pain and fatigue, distress related to pregnancy complications and female hormonal conditions. Additional meta-analytic reviews examined the efficacy of CBT for various problems in children and elderly adults. The vast majority of studies (84%) was published after 2004, which was the last year of coverage of the review by Butler and colleagues (2006), making the present study the most comprehensive and contemporary review of meta-analytic studies of CBT to date.
For the treatment of addiction and substance use disorder, the effect sizes of CBT ranged from small to medium, depending on the type of the substance of abuse. CBT was highly effective for treating cannabis and nicotine dependence, but less effective for treating opioid and alcohol dependence. For treating schizophrenia and other psychotic disorders, the empirical literature suggested appreciable efficacy of CBT particularly for positive symptoms and secondary outcomes in the psychotic disorders, but lesser efficacy than other treatments (e.g. family intervention or psychopharmacology) for chronic symptoms or relapse prevention.
The meta-analytic literature on the efficacy of CBT for depression and dysthymia was mixed with some studies suggesting strong evidence and others reporting weak support. Some authors have suggested that the strong effects in some studies may be an overestimation due to a publication bias (Cuijpers, et al., 2010). Similarly, the efficacy of CBT for bipolar disorder was small to medium in the short-term in comparison to treatment as usual. However, there was limited evidence for the superiority of CBT alone over pharmacological approaches; for the treatment of depressive symptoms in bipolar disorder, the use of CBT was well supported. However, the long-term superiority compared to other treatments is still uncertain.
The efficacy of CBT for anxiety disorders was consistently strong, despite some notable heterogeneity in the specific anxiety pathology, comparison conditions, follow-up data, and severity level. Large effect sizes were reported for the treatment of obsessive compulsive disorder, and at least medium effect sizes for social anxiety disorder, panic disorder, and post-traumatic stress disorder. Medium to large CBT treatment effects were reported for somatoform disorders, such as hypochondriasis and body dysmorphic disorder. However, more studies using larger trials and greater sample sizes are needed to draw more conclusive findings with regard to CBT’s relative efficacy in comparison to other active treatments.
For the treatment of bulimia, CBT was considerably more effective than other forms of psychotherapies, but less is known for other eating disorders. Similarly, CBT demonstrated superior efficacy as compared to other interventions for treating insomnia when examining sleep quality, total sleep time, waking time, and sleep efficiency outcomes. However, although there were small effects of CBT for sleep problems among older adults (aged 60+), these effects may not be long lasting (Montgomery & Dennis, 2009).
For personality disorders, there was some evidence for superior efficacy of CBT as compared to other psychosocial treatments for the personality disorders. However, the studies showed considerable variation in measurement methods, comorbid disorders, and demographic variables. CBT also produced medium to large effect sizes for treating anger and aggression (e.g., Saini, 2009), although a greater number of well-controlled studies are needed to more adequately parse out the specific efficacy of CBT compared to the psychosocial treatments for anger on the whole. Similarly, more studies are needed before any firm conclusions can be drawn about the efficacy of this treatment for criminal behaviors.
As a stress management intervention, CBT was more effective that other treatments, such as organization-focused therapies. However, more research on the long-term effects of CBT for occupational stress is needed. Furthermore, there are open questions about the relative efficacy of CBT versus pharmacological approaches to stress management. Similarly, several common concerns recurred across meta-analytic examinations of CBT for chronic medical conditions, chronic fatigue and chronic pain, namely: (1) a scarcity of studies and small sample sizes; (2) poor methodological design of studies that are included in meta-analyses; and (3) grouping of CBT with a host of other psychotherapies (such as psychodynamic therapy, hypnotherapy, mindfulness, relaxation, and supportive counseling), which made it difficult to parse out whether there are any superior effects of CBT in the majority of medical conditions examined.
There was preliminary evidence for CBT for treating distress related to pregnancy complications and female hormonal conditions. However, more research is needed due to a scarcity of follow-up data and low quality studies. This appeared to be a highly promising area for CBT given that the alternative – pharmacological treatments – can be associated with serious risks of adverse effects for pregnant women and breastfeeding mothers.
In our review of meta-analyses, CBT tailored to children showed robust support for treating internalizing disorders, with benefits outweighing pharmacological approaches in mood and anxiety symptoms. The evidence was more mixed for externalizing disorders, chronic pain, or problems following abuse. Moreover, there remains a need for a greater number of high-quality trials in demographically diverse samples. Similarly, CBT was moderately efficacious for the treatment of emotional symptoms in the elderly, but no conclusions about long-term outcomes of CBT or combination therapies consisting of CBT, and medication could be made.
Finally, our review identified 11 studies that compared response rates between CBT and other treatments or control conditions. In 7 of these reviews, CBT showed higher response rates than the comparison conditions, and in only one review (Leichsenring & Leibig, 2003), which was conducted by authors with a psychodynamic orientation, reported that CBT had lower response rates than comparison treatments.
In sum, our review of meta-analytic studies examining the efficacy of CBT demonstrated that this treatment has been used for a wide range of psychological problems. In general, the evidence-base of CBT is very strong, and especially for treating anxiety disorders. However, despite the enormous literature base, there is still a clear need for high-quality studies examining the efficacy of CBT. Furthermore, the efficacy of CBT is questionable for some problems, which suggests that further improvements in CBT strategies are still needed. In addition, many of the meta-analytic studies included studies with small sample sizes or inadequate control groups. Moreover, except for children and elderly populations, no meta-analytic studies of CBT have been reported on particular subgroups, such as ethnic minorities and low income samples.
Despite these weaknesses in some areas, it is clear that the evidence-base of CBT is enormous. Given the high cost-effectiveness of the intervention, it is surprising that many countries, including many developed nations, have not yet adopted CBT as the first-line intervention for mental disorders. A notable exception is the Improving Access to Psychological Therapies initiative by the National Health Commissioning in the United Kingdom (Rachman & Wilson, 2008). We believe that it is time that others follow suit.
Acknowledgments
The authors would like to acknowledge the following research assistants who provided crucial and much-appreciated assistance with background literature reviews, initial identification of articles, and obtained articles for use by the authors: Dan Brager, Rachel Kaufmann, Rebecca Grossman, and Brian Hall.
Dr. Hofmann is a paid consultant of Merck Pharmaceutical (Schering-Plough) for work unrelated to this study. This study was partially supported by NIMH grants MH-078308 and MH-081116 awarded to Dr. Hofmann and MH-73937.
References
- Álvarez-Jiménez M, Parker AG, Hetrick SE, McGorry PD, Gleeson JF. Preventing the second episode: a systematic review and meta-analysis of psychosocial and pharmacological trials in first-episode psychosis. Schizophrenia Bulletin. 2011;37:619–630. doi: 10.1093/schbul/sbp129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babcock JC, Green CE, Robie C. Does batterers' treatment work? A meta-analytic review of domestic violence treatment. Clinical Psychology Review. 2004;23:1023–1053. doi: 10.1016/j.cpr.2002.07.001. [DOI] [PubMed] [Google Scholar]
- Baker GA, Brooks JL, Goodfellow L, Bodde N, Aldenkamp A. Treatments for non-epileptic attack disorder. Cochrane Database of Systematic Reviews. 2007;1:CD006370. doi: 10.1002/14651858.CD006370. [DOI] [PubMed] [Google Scholar]
- Beck AT. Cognitive therapy: Nature and relation to behavior therapy. Behavior Therapy. 1970;1:184–200. [Google Scholar]
- Beltman MW, Oude Voshaar RC, Speckens AE. Cognitive-behavioural therapy for depression in people with a somatic disease: meta-analysis of randomised controlled trials. The British Journal of Psychiatry. 2010;197:11–19. doi: 10.1192/bjp.bp.109.064675. [DOI] [PubMed] [Google Scholar]
- Beynon S, Soares-Weiser K, Woolacott N, Duffy S, Geddes JR. Psychosocial interventions for the prevention of relapse in bipolar disorder: systematic review of controlled trials. The British Journal of Psychiatry. 2008;192:5–11. doi: 10.1192/bjp.bp.107.037887. [DOI] [PubMed] [Google Scholar]
- Binks C, Fenton M, McCarthy L, Lee T, Adams CE, Duggan C. Psychological therapies for people with borderline personality disorder. Cochrane Database of Systematic Reviews. 2006;1:CD005652. doi: 10.1002/14651858.CD005652. [DOI] [PubMed] [Google Scholar]
- Bird V, Premkumar P, Kendall T, Whittington C, Mitchell J, Kuipers E. Early intervention services, cognitive-behavioural therapy and family intervention in early psychosis: systematic review. The British Journal of Psychiatry. 2010;197:350–356. doi: 10.1192/bjp.bp.109.074526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisson J, Andrew M. Psychological treatment of post-traumatic stress disorder (PTSD) Cochrane Database of Systematic Reviews. 2008;3:CD003388. doi: 10.1002/14651858.CD003388.pub2. [DOI] [PubMed] [Google Scholar]
- Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S. Psychological treatments for chronic post-traumatic stress disorder. Systematic review and meta-analysis. The British Journal of Psychiatry. 2007;190:97–104. doi: 10.1192/bjp.bp.106.021402. [DOI] [PubMed] [Google Scholar]
- Bledsoe SE, Grote NK. Treating depression during pregnancy and the postpartum: A preliminary meta-analysis. Research on Social Work Practice. 2006;16:109–120. [Google Scholar]
- Busse JW, Montori VM, Krasnik C, Patelis-Siotis I, Guyatt GH. Psychological intervention for premenstrual syndrome: a meta-analysis of randomized controlled trials. Psychotherapy and Psychosomatics. 2009;78:6–15. doi: 10.1159/000162296. [DOI] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Cakir S, Ozerdem A. Psychotherapeutic and psychosocial approaches in bipolar disorder: a systematic literature review. Turkish Journal of Psychiatry. 2010;21:143–154. [PubMed] [Google Scholar]
- Chan EK-H. Efficacy of cognitive-behavioral, pharmacological, and combined treatments of depression: A meta-analysis. Calgary: University of Calgary; 2006. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Coull G, Morris PG. The clinical effectiveness of CBT-based guided self-help interventions for anxiety and depressive disorders: a systematic review. Psychological Medicine. 2011;41:2239–2252. doi: 10.1017/S0033291711000900. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Passin WF, Herbst JH, Rama SM, Malow RM, Purcell DW, Wolitski RJ HIV/AIDS Prevention Research Synthesis (PRS) Team. Meta-analysis of cognitive-behavioral interventions on HIV-positive persons' mental health and immune functioning. Health Psychology. 2008;27:4–14. doi: 10.1037/0278-6133.27.1.4. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Smit F, Bohlmeijer E, Hollon SD, Andersson G. Efficacy of cognitive-behavioural therapy and other psychological treatments for adult depression: meta-analytic study of publication bias. The British Journal of Psychiatry. 2010;196:173–178. doi: 10.1192/bjp.bp.109.066001. [DOI] [PubMed] [Google Scholar]
- Del Vecchio T, O'Leary KD. Effectiveness of anger treatments for specific anger problems: A meta-analytic review. Clinical Psychology Review. 2004;24:15–34. doi: 10.1016/j.cpr.2003.09.006. [DOI] [PubMed] [Google Scholar]
- Dennis C-L, Hodnett ED. Psychosocial and psychological interventions for treating postpartum depression. Cochrane database of systematic reviews. 2007;4:CD006116. doi: 10.1002/14651858.CD006116.pub2. [DOI] [PubMed] [Google Scholar]
- Di Giulio G. Therapist, client factors, and efficacy in cognitive behavioural therapy: A meta-analytic exploration of factors that contribute to positive outcome. Ottawa: University of Ottawa; 2010. [Google Scholar]
- Dorstyn D, Mathias J, Denson L. Efficacy of cognitive behavior therapy for the management of psychological outcomes following spinal cord injury: A meta-analysis. Journal of Health Psychology. 2011;16:374–391. doi: 10.1177/1359105310379063. [DOI] [PubMed] [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. The American Journal of Psychiatry. 2008;165:179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- Eddy KT, Dutra L, Bradley R, Westen D. A multidimensional meta-analysis of psychotherapy and pharmacotherapy for obsessive-compulsive disorder. Clinical Psychology Review. 2004;24:1011–1030. doi: 10.1016/j.cpr.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Ellis A. Reason and emotion in psychotherapy. New York: Lyle Stuart; 1962. [Google Scholar]
- Enck P, Junne F, Klosterhalfen S, Zipfel S, Martens U. Therapy options in irritable bowel syndrome. European Journal of Gastroenterology & Hepatology. 2010;22:1402–1411. doi: 10.1097/MEG.0b013e3283405a17. [DOI] [PubMed] [Google Scholar]
- Fedoroff I, Taylor S. Psychological and pharmacological treatments of social phobia: a meta-analysis. Journal of Clinical Psychopharmacology. 2001;21:311–324. doi: 10.1097/00004714-200106000-00011. [DOI] [PubMed] [Google Scholar]
- Furukawa TA, Watanabe N, Churchill R. Combined psychotherapy plus antidepressants for panic disorder with or without agoraphobia: systematic review. Cochrane Database of Systematic Reviews. 2007;1:CD004364. doi: 10.1002/14651858.CD004364.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Vera MP, Sanz J. Análisis de la situación de los tratamientos para / dejar de fumar basados en terapia cognitivo-conductual y en parches de nicotina / Analysis of the situation of treatments for smoking cessation based on cognitive-behavioral therapy and nicotine patches. Psicooncología. 2006;3:269–289. [Google Scholar]
- Ghahramanlou M. Cognitive behavioral treatment efficacy for anxiety disorders: A meta-analytic review. Unpublished Dissertation. Fairleigh Dickinson University; 2003. [Google Scholar]
- Gibbon S, Duggan C, Stoffers J, Huband N, Völlm BA, Ferriter M, Lieb K. Psychological interventions for antisocial personality disorder (Review) Cochrane Database Systematic Reviews. 2010;6:CD007668. doi: 10.1002/14651858.CD007668.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gil PJM, Carrillo FXM, Meca JS. Effectiveness of cognitive-behavioural treatment in social phobia: A meta-analytic review. Psychology in Spain. 2001;5:17–25. [Google Scholar]
- Glombiewski J, Sawyer A, Gutermann J, Koenig K, Rief W, Hofmann S. Psychological treatments for fibromyalgia: a meta-analysis. Pain. 2010;151:280–295. doi: 10.1016/j.pain.2010.06.011. [DOI] [PubMed] [Google Scholar]
- Gould RA, Mueser KT, Bolton E, Mays V, Goff D. Cognitive therapy for psychosis in schizophrenia: An effect size analysis. Schizophrenia Research. 2001;48:335–342. doi: 10.1016/s0920-9964(00)00145-6. [DOI] [PubMed] [Google Scholar]
- Gregory VL. Cognitive-behavioral therapy for depression in bipolar disorder: a meta-analysis. Journal of Evidence Based Social Work. 2010;7(4):269–279. doi: 10.1080/15433710903176088. [DOI] [PubMed] [Google Scholar]
- Gregory VL. Cognitive-behavioral therapy for mania: A meta-analysis of randomized controlled trials. Social work in Mental Health. 2010;8:483–494. [Google Scholar]
- Guggisberg KW. Methodological review and meta-analysis of treatments for child and adolescent obsessive-compulsive disorder. Salt Lake City: University of Utah; 2005. [Google Scholar]
- Haby MM, Donnelly M, Corry J, Vos T. Cognitive behavioural therapy for depression, panic disorder and generalized anxiety disorder: a meta-regression of factors that may predict outcome. The Australian and New Zealand Journal of Psychiatry. 2006;40:9–19. doi: 10.1080/j.1440-1614.2006.01736.x. [DOI] [PubMed] [Google Scholar]
- Haby MM, Tonge B, Littlefield L, Carter R, Vos T. Cost-effectiveness of cognitive behavioural therapy and selective serotonin reuptake inhibitors for major depression in children and adolescents. The Australian and New Zealand Journal of Psychiatry. 2004;38:579–591. doi: 10.1080/j.1440-1614.2004.01421.x. [DOI] [PubMed] [Google Scholar]
- Hay PP, Bacaltchuk J, Stefano S, Kashyap P. Psychological treatments for bulimia nervosa and binging. Cochrane Database of Systematic Reviews. 2009;4:CD000562. doi: 10.1002/14651858.CD000562.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriks GJ, Oude Voshaar RC, Keijsers GPJ, Hoogduin CAL, van Balkom AJLM. Cognitive-behavioural therapy for late-life anxiety disorders: a systematic review and meta-analysis. Acta Psychiatrica Scandinavica. 2008;117:403–411. doi: 10.1111/j.1600-0447.2008.01190.x. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. An introduction to modern CBT: Psychological solutions to mental health problems. Oxford, UK: Wiley-Blackwell; 2011. [Google Scholar]
- Hofmann SG, Asmundson GJ, Beck AT. The science of cognitive therapy. Behavior Therapy. doi: 10.1016/j.beth.2009.01.007. (in press). [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Smits JAJ. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. The Journal of Clinical Psychiatry. 2008;69:621–632. doi: 10.4088/jcp.v69n0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunot V, Churchill R, Silva de Lima M, Teixeira V. Psychological therapies for generalised anxiety disorder. Cochrane Database of Systematic Reviews. 2007;1:CD001848. doi: 10.1002/14651858.CD001848.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Illescas SR, Sánchez-Meca J, Genovés VG. Treatment of offenders and recidivism: Assessment of the effectiveness of programmes applied in Europe. Psychology in Spain. 2001;5:47–62. [Google Scholar]
- Ipser J, Sander C, Stein D. Pharmacotherapy and psychotherapy for body dysmorphic disorder. Cochrane Database of Systematic Reviews. 2009;1:CD005332. doi: 10.1002/14651858.CD005332.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin MR, Cole JC, Nicassio PM. Comparative meta-analysis of behavioral interventions for insomnia and their efficacy in middle-aged adults and in older adults 55+ years of age. Health Psychology. 2006;25:3–14. doi: 10.1037/0278-6133.25.1.3. [DOI] [PubMed] [Google Scholar]
- Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. The Lancet. 2004;363(9421):1589–1597. doi: 10.1016/S0140-6736(04)16202-8. [DOI] [PubMed] [Google Scholar]
- James A, Soler A, Weatherall R. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database of Systematic Reviews. 2005;4:CD004690. doi: 10.1002/14651858.CD004690.pub2. [DOI] [PubMed] [Google Scholar]
- Jarry J, Ip K. The effectiveness of stand-alone cognitive-behavioural therapy for body image: A meta-analysis. Body Image. 2005;2:317–331. doi: 10.1016/j.bodyim.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Morgan AJ, Hetrick SE. Relaxation for depression. Cochrane Database of Systematic Reviews. 2008;4:CD007142. doi: 10.1002/14651858.CD007142.pub2. [DOI] [PubMed] [Google Scholar]
- Kangas M, Bovbjerg DH, Montgomery GH. Cancer-related fatigue: a systematic and meta-analytic review of non-pharmacological therapies for cancer patients. Psychological Bulletin. 2008;134:700–741. doi: 10.1037/a0012825. [DOI] [PubMed] [Google Scholar]
- Kim JH. A meta-analysis of effects of job stress management interventions (SMIs) Taehan Kanho Hakhoe Chi. 2007;37:529–539. doi: 10.4040/jkan.2007.37.4.529. [DOI] [PubMed] [Google Scholar]
- Krishna M, Jauhari A, Lepping P, Turner J, Crossley D, Krishnamoorthy A. Is group psychotherapy effective in older adults with depression? A systematic review. International Journal of Geriatric Psychiatry. 2011;26:331–340. doi: 10.1002/gps.2546. [DOI] [PubMed] [Google Scholar]
- Lam DH, Burbeck R, Wright K, Pilling S. Psychological therapies in bipolar disorder: the effect of illness history on relapse prevention - a systematic review. Bipolar Disorders. 2009;11:474–482. doi: 10.1111/j.1399-5618.2009.00724.x. [DOI] [PubMed] [Google Scholar]
- Leichsenring F. Comparative effects of short-term psychodynamic psychotherapy and cognitive-behavioral therapy in depression: a meta-analytic approach. Clinical Psychology Review. 2001;21:401–419. doi: 10.1016/s0272-7358(99)00057-4. [DOI] [PubMed] [Google Scholar]
- Leichsenring F, Leibing E. The effectiveness of psychodynamic therapy and cognitive behavior therapy in the treatment of personality disorders: a meta- analysis. The American Journal of Psychiatry. 2003;160:1223–1232. doi: 10.1176/appi.ajp.160.7.1223. [DOI] [PubMed] [Google Scholar]
- Leung KS, Cottler LB. Treatment of pathological gambling. Current Opinion in Psychiatry. 2009;22:69–74. doi: 10.1097/YCO.0b013e32831575d9. [DOI] [PubMed] [Google Scholar]
- Lösel F, Beelmann A. Effects of child skills training in preventing antisocial behavior: A systematic review of randomized evaluations. The ANNALS of the American Academy of Political and Social Science. 2003;587:84–109. [Google Scholar]
- Lösel F, Schmucker M. The effectiveness of treatment for sexual offenders: A comprehensive meta-analysis. Journal of Experimental Criminology. 2005;1:117–146. [Google Scholar]
- Luckett T, Britton B, Clover K, Rankin NM. Evidence for interventions to improve psychological outcomes in people with head and neck cancer: a systematic review of the literature. Supportive Care in Cancer, Official Journal of the Multinational Association of Supportive Care in Cancer. 2011;19:871–881. doi: 10.1007/s00520-011-1119-7. [DOI] [PubMed] [Google Scholar]
- Macdonald GM, Higgins JP, Ramchandani P. Cognitive-behavioural interventions for children who have been sexually abused. Cochrane Database of Systematic Reviews. 2006;4:CD001930. doi: 10.1002/14651858.CD001930.pub2. [DOI] [PubMed] [Google Scholar]
- Malouff JM, Thorsteinsson EB, Rooke SE, Bhullar N, Schutte NS. Efficacy of cognitive behavioral therapy for chronic fatigue syndrome: a meta-analysis. Clinical Psychology Review. 2008;28:736–745. doi: 10.1016/j.cpr.2007.10.004. [DOI] [PubMed] [Google Scholar]
- Marine A, Ruotsalainen JH, Serra C, Verbeek JH. Preventing occupational stress in healthcare workers (Review) Cochrane Database of Systematic Reviews. 2009;4:CD002892. doi: 10.1002/14651858.CD002892.pub2. [DOI] [PubMed] [Google Scholar]
- Martinez-Devesa P, Perera R, Theodoulou M, Waddell A. Cognitive behavioural therapy for tinnitus. Cochrane database of systematic reviews. 2010;9:CD005233. doi: 10.1002/14651858.CD005233.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitte K. A meta-analysis of the efficacy of psycho- and pharmacotherapy in panic disorder with and without agoraphobia. Journal of Affective Disorder. 2005;88:27–45. doi: 10.1016/j.jad.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Montgomery P, Dennis JA. Cognitive behavioural interventions for sleep problems in adults aged 60+ Cochrane database of systematic reviews. 2009;1:CD003161. doi: 10.1002/14651858.CD003161. [DOI] [PubMed] [Google Scholar]
- Oakley-Browne M, Adams P, Mobberley P. Interventions for pathological gambling. Cochrane database of systematic reviews. 2000;2:CD001521. doi: 10.1002/14651858.CD001521. [DOI] [PubMed] [Google Scholar]
- Okajima I, Komada Y, Inoue Y. A meta-analysis on the treatment effectiveness of cognitive behavioral therapy for primary insomnia. Sleep and Biological Rhythms. 2011;9:24–34. [Google Scholar]
- Öst LG. Cognitive behavior therapy for anxiety disorders: 40 years of progress. Nordic Journal of Psychiatry. 2008;62:5–10. doi: 10.1080/08039480802315590. [DOI] [PubMed] [Google Scholar]
- Özabaci N. Cognitive behavioural therapy for violent behaviour in children and adolescents: A meta-analysis. Children and Youth Services Review. 2011;33(10):1989–1993. [Google Scholar]
- Pearson FS, Lipton DS, Cleland CM, Yee DS. The effects of behavioral/cognitive-behavioral programs on recidivism. Crime & Delinquency. 2002;48:476–496. [Google Scholar]
- Peng X-D, Huang C-Q, Chen L-J, Lu Z-C. Cognitive behavioural therapy and reminiscence techniques for the treatment of depression in the elderly: a systematic review. The Journal of International Medical Research. 2009;37:975–982. doi: 10.1177/147323000903700401. [DOI] [PubMed] [Google Scholar]
- Pfeiffer PN, Heisler M, Piette JD, Rogers MAM, Valenstein M. Efficacy of peer support interventions for depression: a meta-analysis. General Hospital Psychiatry. 2010;33:29–36. doi: 10.1016/j.genhosppsych.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips AS. A meta-analysis of treatments for pediatric obsessive-compulsive disorder. Manhattan, Kansas: Kansas State University; 2003. [Google Scholar]
- Pinquart M, Duberstein PR, Lyness JM. Effects of psychotherapy and other behavioral interventions on clinically depressed older adults: a meta-analysis. Aging & Mental Health. 2007;11:645–657. doi: 10.1080/13607860701529635. [DOI] [PubMed] [Google Scholar]
- Powers MB, Sigmarsson SR, Emmelkamp PMG. A meta-analytic review of psychological treatments for social anxiety disorder. International Journal of Cognitive Therapy. 2008;1:94–113. [Google Scholar]
- Powers MB, Vedel E, Emmelkamp PMG. Behavioral couples therapy(BCT) for alcohol and drug use disorders: a meta-analysis. Clinical Psychology Review. 2008;28:952–962. doi: 10.1016/j.cpr.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Price JR, Mitchell E, Tidy E, Hunot V. Cognitive behaviour therapy for chronic fatigue syndrome in adults. Cochrane Database of Systematic Reviews. 2008;3:CD001027. doi: 10.1002/14651858.CD001027.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachman S, Wilson GT. Expansion in the provision of psychological treatment in the United Kingdom. Behaviour Research and Therapy. 2008;46:293–295. doi: 10.1016/j.brat.2008.01.005. [DOI] [PubMed] [Google Scholar]
- Reas DL, Grilo CM. Review and meta-analysis of pharmacotherapy for binge-eating disorder. Obesity. 2008;16(9):2024–2038. doi: 10.1038/oby.2008.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rector NA, Beck AT. Cognitive behavioral therapy for schizophrenia: an empirical review. The Journal of Nervous and Mental Disease. 2001;189:278–287. doi: 10.1097/00005053-200105000-00002. [DOI] [PubMed] [Google Scholar]
- Richardson KM, Rothstein HR. Effects of occupational stress management intervention programs: a meta-analysis. Journal of Occupational Health Psychology. 2008;13:69–93. doi: 10.1037/1076-8998.13.1.69. [DOI] [PubMed] [Google Scholar]
- Robinson J, Hetrick SE, Martin C. Preventing suicide in young people: systematic review. The Australian and New Zealand Journal of Psychiatry. 2011;45:3–26. doi: 10.3109/00048674.2010.511147. [DOI] [PubMed] [Google Scholar]
- Rueda S, Park-Wyllie LY, Bayoumi A, Tynan AM, Antoniou TA, Rourke SB, Glazier RH. Patient support and education for promoting adherence to highly active antiretroviral therapy for HIV/AIDS. Cochrane database of systematic reviews. 2006;3:CD001442. doi: 10.1002/14651858.CD001442.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhmland M, Margraf J. Effektivität psychologischer Therapien von spezifischer Phobie und Zwangsstörung: Meta-Analysen auf Störungsebene / Efficacy of psychological treatments for specific phobia and obsessive compulsive disorder. Verhaltenstherapie. 2001;11:14–26. [Google Scholar]
- Saini M. A meta-analysis of the psychological treatment of anger: developing guidelines for evidence-based practice. The Journal of the American Academy of Psychiatry and the Law. 2009;37:473–488. [PubMed] [Google Scholar]
- Santacruz I, Orgilés M, Rosa AI, Sánchez-Meca J, Méndez X, Olivares J. Generalized anxiety, separation anxiety and school phobia: The predominance of cognitive-behavioural therapy / Ansiedad generalizada, ansiedad por separación y fobia escolar: el predominio de la terapia cognitivo-conductual. Behavioral Psychology/Psicología Conductual. 2002;10(3):503–521. [Google Scholar]
- Shaw K, O’Rourke P, Del Mar C, Kenardy J. Psychological interventions for overweight or obesity. Cochrane database of systematic reviews. 2005;2:CD003818. doi: 10.1002/14651858.CD003818.pub2. [DOI] [PubMed] [Google Scholar]
- Singer GH, Ethridge BL, Aldana SI. Primary and secondary effects of parenting and stress management interventions for parents of children with developmental disabilities: a meta-analysis. Mental Retardation and Developmental Disabilities Research Reviews. 2007;13:357–369. doi: 10.1002/mrdd.20175. [DOI] [PubMed] [Google Scholar]
- Sockol LE, Epperson CN, Barber JP. A meta-analysis of treatments for perinatal depression. Clinical Psychology Review. 2011;31:839–849. doi: 10.1016/j.cpr.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song F, Huttunen-Lenz M, Holland R. Effectiveness of complex psycho-educational interventions for smoking relapse prevention: an exploratory meta-analysis. Journal of Public Health. 2010;32:350–359. doi: 10.1093/pubmed/fdp109. [DOI] [PubMed] [Google Scholar]
- Soo S, Moayyedi P, Deeks J, Delaney B, Lewis M, Forman D. Psychological interventions for non-ulcer dyspepsia. Cochrane Database of Systematic Reviews. 2004;2:CD002301. doi: 10.1002/14651858.CD002301.pub2. [DOI] [PubMed] [Google Scholar]
- Taylor S, Asmundson GJG, Coons MJ. Current directions in the treatment of hypochondriasis. Journal of Cognitive Psychotherapy. 2005;19:285–304. [Google Scholar]
- Thomas PW, Thomas S, Hillier C, Galvin K, Baker R. Psychological interventions for multiple sclerosis. Cochrane Database of Systematic Reviews. 2006;1:CD004431. doi: 10.1002/14651858.CD004431.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson-Brenner HJ. Implications for the treatment of bulimia nervosa: A meta-analysis of efficacy trials and a naturalistic study of treatment in the community. Michigan: University of Michigan; 2002. [Google Scholar]
- Thomson AB, Page LA. Psychotherapies for hypochondriasis. Cochrane Database of Systematic Reviews. 2007;4:CD006520. doi: 10.1002/14651858.CD006520.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorp SR, Ayers CR, Nuevo R, Stoddard JA, Sorrell JT, Wetherell JL. Meta-analysis comparing different behavioral treatments for late-life anxiety. The American Journal of Geriatric Psychiatry. 2009;17:105–115. doi: 10.1097/JGP.0b013e31818b3f7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF. Is cognitive-behavioral therapy more effective than other therapies? A meta-analytic review. Clinical Psychology Review. 2010;30:710–720. doi: 10.1016/j.cpr.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ. The benefits of interventions for work-related stress. American Journal of Public Health. 2001;91:270–276. doi: 10.2105/ajph.91.2.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Oord S, Prins PJ, Oosterlaan J, Emmelkamp PM. Efficacy of methylphenidate, psychosocial treatments and their combination in school-aged children with ADHD: A meta-analysis. Clinical Psychology Review. 2008;28:783–800. doi: 10.1016/j.cpr.2007.10.007. [DOI] [PubMed] [Google Scholar]
- Van Straten A, Geraedts A, Verdonck-de Leeuw I, Andersson G, Cuijpers P. Psychological treatment of depressive symptoms in patients with medical disorders: a meta-analysis. Journal of Psychosomatic Research. 2010;69:23–32. doi: 10.1016/j.jpsychores.2010.01.019. [DOI] [PubMed] [Google Scholar]
- Vocks S, Tuschen-Caffier B, Pietrowsky R, Rustenbach SJ, Kersting A, Herpertz S. Meta-analysis of the effectiveness of psychological and pharmacological treatments for binge eating disorder. The International Journal of Eating Disorders. 2010;43:205–217. doi: 10.1002/eat.20696. [DOI] [PubMed] [Google Scholar]
- Vos T, Haby MM, Barendregt JJ, Kruijshaar M, Corry J, Andrews G. The burden of major depression avoidable by longer-term treatment strategies. Archives of General Psychiatry. 2004;61(11):1097–1103. doi: 10.1001/archpsyc.61.11.1097. [DOI] [PubMed] [Google Scholar]
- Walker DF, McGovern SK, Poey EL, Otis KE. Treatment effectiveness for male adolescent sexual offenders: a meta-analysis and review. Journal of Child Sexual Abuse. 2005;13:281–293. doi: 10.1300/j070v13n03_14. [DOI] [PubMed] [Google Scholar]
- Williams J, Hadjistavropoulos T, Sharpe D. A meta-analysis of psychological and pharmacological treatments for body dysmorphic disorder. Behaviour Research and Therapy. 2006;44:99–111. doi: 10.1016/j.brat.2004.12.006. [DOI] [PubMed] [Google Scholar]
- Wilson DB, Bouffard LA, Mackenzie DL. A quantitative review of structured, group-oriented, cognitive-behavioral programs for offenders. Criminal Justice and Behavior. 2005;32:172–204. [Google Scholar]
- Wilson KCM, Mottram PG, Vassilas CA. Psychotherapeutic treatments for older depressed people. Cochrane Database of Systematic Reviews. 2008;1:CD004853. doi: 10.1002/14651858.CD004853.pub2. [DOI] [PubMed] [Google Scholar]
- Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: Effect sizes, clinical models, and methodological rigor. Schizophrenia Bulletin. 2008;34(3):523–537. doi: 10.1093/schbul/sbm114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann G, Favrod J, Trieu VH, Pomini V. The effect of cognitive behavioral treatment on the positive symptoms of schizophrenia spectrum disorders: a meta-analysis. Schizophrenia Research. 2005;77:1–9. doi: 10.1016/j.schres.2005.02.018. [DOI] [PubMed] [Google Scholar]
- Zimmermann T, Heinrichs N. Psychosoziale Interventionen für Frauen mit Krebserkrankungen der Genitalorgane / Psychosocial interventions for women with genital cancers. Verhaltenstherapie & Verhaltensmedizin. 2006;27:125–141. [Google Scholar]