Abstract
Background
While the majority of smokers visit a primary care physician each year, only a small proportion of them receive evidence-based tobacco dependence treatment. The Electronic Health Record (EHR) provides an opportunity to prompt clinicians to deliver tobacco dependence treatment in primary care.
Methods
Over one year, Dean Health Systems worked with the UW School of Medicine and Public Health to modify the existing Dean EHR system (Epic Systems Corporation) to improve identification and treatment of adult smokers visiting primary care clinics. Modifications included evidence-based prompts that helped guide medical assistants to identify smokers and prompted clinicians to deliver a brief tobacco cessation intervention (medication and Wisconsin Tobacco Quit Line referral). 18 primary care clinics provided data one year before and one year after implementing the EHR modifications.
Results
A higher percentage of adult patients had their tobacco use status identified after EHR modification compared to pre-implementation, (71.6% vs. 78.4%, p< .001). During the post-implementation year, 6.3% of adult smokers were prescribed tobacco cessation medication, 2.5% of adult smokers had documentation of counseling, and 1.5% of adult smokers had counseling billed (pre-implementation data not available).
Conclusions
This demonstration project showed that a large healthcare system can increase the delivery of tobacco dependence treatment interventions (increased identification of smokers and relatively high rates of delivering specific tobacco dependence clinical interventions) building upon an existing EHR platform. The project demonstrated that brief, evidence-based tobacco dependence interventions can be incorporated into primary care, especially when the EHR is utilized to improve clinic workflow.
INTRODUCTION
More than 70% of smokers visit a primary care physician annually, making the health care visit an unequalled opportunity to assist smokers willing to make a quit attempt.1 Despite substantial evidence that brief cessation interventions during primary care visits promote quitting in different populations, smokers consistently leave these appointments without receiving evidence-based counseling and medication.2–10 Among the factors contributing to this lost opportunity is the fact that few primary care patients visit their clinician with tobacco dependence as their chief complaint, and brief clinic visits are consumed by other presenting problems/symptoms. This focus on the “chief complaint” and the “presenting symptoms” rather than on tobacco use (which is often the primary cause of those symptoms), is highlighted by the fact that the average doctor's appointment is only 23.8 minutes for a prepaid visit and 21.0 minutes for a non-prepaid visit.11 This chief complaint focus is also accentuated by the fact that few clinics have systems in place to efficiently identify and intervene with preventable causes of illness and death, including tobacco dependence.
Electronic medical records (EMRs) have been identified as an opportunity to save time, space, and money, to improve the quality of care, and to communicate information more efficiently in healthcare settings.12, 13 The EMR has also been identified as an efficient medium to identify individuals at high risk for developing diabetes and coronary heart disease and increase health care utilization for these individuals.14 Based on these demonstrated EMR benefits for other chronic diseases, using this technology to intervene with patients who are tobacco dependent is an ideal new focus that could result in substantial health benefits. Past studies have indicated that implementing modifications in the EMR can increase the medical staff's identification of patient tobacco use status and provision of counseling assistance.15, 16 Although counseling assistance increased when the EMR was modified with a tobacco feature, prescription administration did not increase.16 Also, there is limited information regarding the length of the intervention process and how much of the scheduled appointment these additional EMR-based tobacco dependence processes consume.
This paper describes the development and results of a partnership between a major central Wisconsin health delivery system (Dean Health Systems) and a university-based tobacco dependence research center (University of Wisconsin Center for Tobacco Research and Intervention). The goal of this partnership was to develop a set of consistent, time efficient workflow modifications, leveraging the powerful EMR system (Epic Systems Corporation) used by Dean, that would prompt the identification of patients who smoke and subsequent clinical interventions with these patients. The standardized workflow processes were designed to quickly identify smokers who are ready to quit prior to the primary care clinician seeing the patient. Once identified, the EMR was programmed to prompt quick and easy documentation, medication ordering, the provision of a tobacco dependence patient information sheet including information on the Wisconsin Tobacco Quit Line, as well as appropriate charging for the visit. The ultimate goal was to design a tobacco dependence treatment intervention that took 60 seconds or less to complete, keeping the majority of the appointment focused on the chief complaint.
METHODS
Design Overview
The goal of this project was to adapt the electronic medical record of a major Wisconsin healthcare system to better identify and intervene with tobacco users in the context of a busy office visit. From February 2007 to January 2008, key staff members from Dean Health Systems (Dean) and the University of Wisconsin Center for Tobacco Research and Intervention (UW-CTRI) met regularly to develop modifications to the Epic Systems Corporation electronic medical record (EMR) program already in use at Dean. Once adapted, the EMR modifications were tested in a pilot clinic before more wide-scale implementation in primary care clinics across the Dean system. The working group at these meetings included Dean representatives (a physician champion as well as health education and information technology specialists) and UW-CTRI representatives (the physician Director and members of the outreach staff who work directly with clinics across Wisconsin to implement evidence-based tobacco dependence systems).
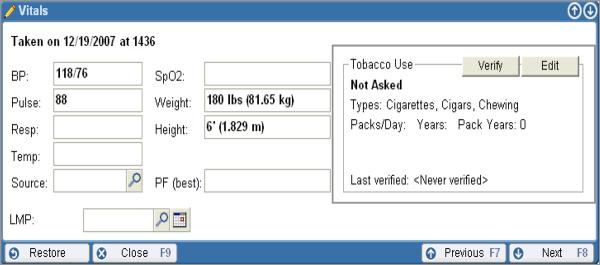
Briefly, the smoking status of the patient was queried and recorded in the vital signs section of the EMR by the medical assistant who “roomed” the patient (Figure 1). The workflow utilized an algorithm that classified patients who smoked on the basis of their willingness to talk to their provider about quitting within the next 30 days. This led to a series of evidence-based prompts that guided the primary care clinician to efficiently offer both tobacco dependence counseling (utilizing the Wisconsin Tobacco Quit Line as a treatment extender) and medication where appropriate as recommended in the United States Public Health Service Clinical Practice Guideline, Treating Tobacco Use and Dependence10 (Figures 2 & 3). These prompts also included other educational information about quitting, Wisconsin Tobacco Quit Line referral information, and a tobacco cessation history survey. Prompts assisted clinicians in counseling smokers both ready and not ready to set a quit date at the time of the clinic visit.
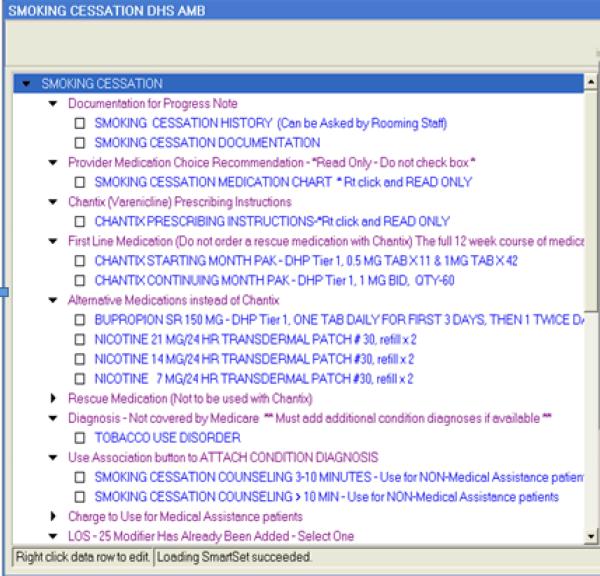
Figure 1.
EMR Screenshot of vitals section containing tobacco identification.
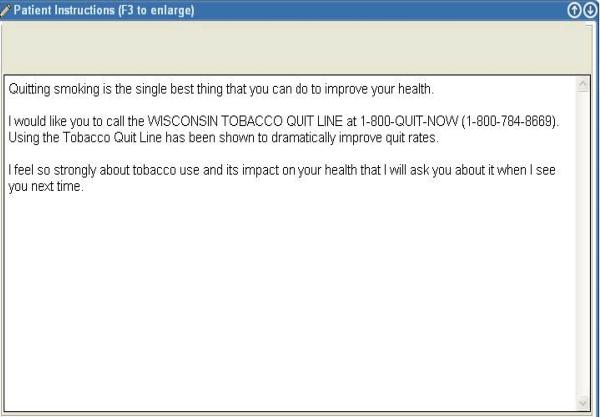
Figure 2.
EMR Screenshot prompted clinical intervention by primary care clinician for smokers able to pick a quit date.
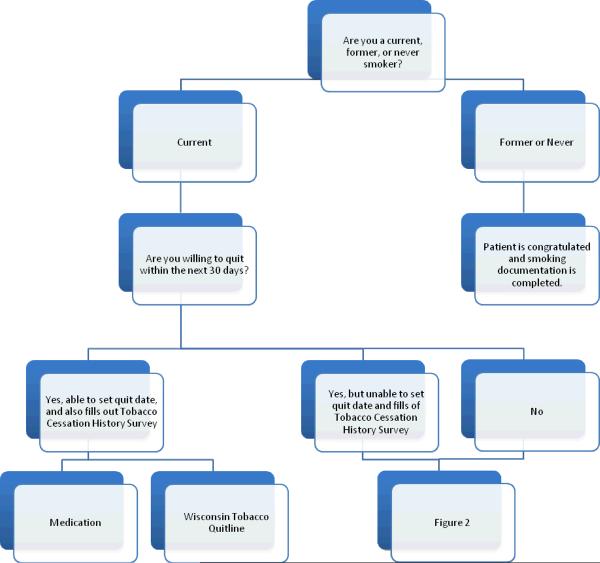
Figure 3.
EMR Screenshot demonstrating printable instructions for patients uninterested in quitting at this time.
The EMR modifications were piloted in one of the Dean primary care clinics in November and December 2007. In February 2008, EMR modifications were implemented in other departments within the Dean system including all of family medicine, internal medicine, OB/GYN, diabetes, cardiology, and psychiatry clinics. By 2009, it was available across the entire Dean system. In this paper, we describe rates of tobacco dependence identification and intervention for one year prior to and one year following implementation of the EMR intervention for the initial 18 general internal medicine and family practice clinics.
Training of staff in each clinic took place over a one-month period in early 2008. A Dean Epic EMR trainer visited each primary care site and provided an onsite Epic training curriculum during regularly scheduled clinician team meetings, which included all staff within the department. The trainings lasted about 20 minutes and included a five minute video describing the program, emphasizing that the intervention was designed to take 60 seconds or less, the purpose of the initiative, the role of both the medical assistant and the clinician, the new Epic screen shots, and the SmartSets available (SmartSets are pre-prepared standardized sets of clinician prompts and messages that help guide treatment for a particular condition). In addition to the basic training, the sites were re-visited if a problem or question occurred after the initial training.
Interventions
The initial EMR modifications were designed to triage all primary care patients into three categories: current tobacco users, former tobacco users, and those who have never used tobacco. A box dedicated to tobacco use (Figure 1) appeared as part of the vital signs window of the EMR (an existing Epic component), to be completed by the medical assistant (MA) who roomed the patient. If tobacco use status was identified as never or former, the intervention was completed. This process took only about 10 seconds and did not involve the health care provider. If the patient was identified as a current tobacco user, the MA was prompted to ask, “Are you willing to talk to your provider about quitting within the next 30 days?” If patients responded no, the roomer loaded a brief message about the importance of quitting and the telephone number of the WI Tobacco Quit Line into the after visit summary that is provided to all patients at the end of their visit. If patients responded yes, they were then asked to manually complete a brief three-question survey about past cessation medications used, how many cigarettes they smoked per day, and a specific date within the next two weeks that they would like to choose for their quit date. Whether the smoker designated a target quit date within the next two weeks divided the patients for intervention into two types (see below). These surveys were left at the clinician's desk in the examination room, serving as a visual prompt that this was a smoker who was interested in quitting. Subsequent smoking cessation interventions for the clinician were prompted by EMR “SmartSets”.
The first type of current smoker included those who indicated they were interested in talking to their clinician about quitting within the next 30 days but were NOT able to commit to a quit date within the next two weeks. For these patients, the clinician emphasized that quitting is very important and then loaded a brief message about this in the patient's after visit summary (AVS). Included in this message was the telephone number for the Wisconsin Tobacco Quit Line should the patient reconsider his/her decision to commit to a specific quit date.
The second type of current smoker included those who indicated that they were interested in talking to their clinician about quitting within the next 30 days and were willing to set a quit date within the next two weeks (the target population). For these patients, the clinician was prompted to open the Smoking Cessation SmartSet (Figure 2), which contained information regarding the Wisconsin Tobacco Quit Line and an EMR-based prescription order form for quick, efficient ordering of one of the seven FDA approved medications for smoking. Based on the worksheet completed by the patient, the clinician prescribed medication that was either new for the patient or had helped in the past. The Wisconsin Tobacco Quit Line number and the appropriate clinic charges were then automatically entered into the visit documentation. This completed the tobacco cessation portion of the visit and the clinician then printed the AVS which contained information regarding the discussed treatment plan and was given to the patient at the conclusion of his/her visit. The entire clinician portion of the tobacco dependence intervention was designed to take less than 60 seconds.
Data Analysis
Dean Health System provided a de-identified aggregate data set summarizing tobacco use identification rates among all adult patients (18 and older) visiting the 18 targeted primary care clinics for approximately 12 months prior to and 12 months following implementation of the EMR modifications. In addition, for patients who smoked, Dean provided 12 months of post-intervention utilization data on three core components of the EMR-based tobacco dependence treatment intervention: tobacco dependence Smartset usage, tobacco cessation medication prescription rates, and smoking cessation counseling billed.
Descriptive data post-intervention was provided for each clinic and across the 18 clinics. In addition, for the two variables that were available before and after the intervention (whether or not smoking status was assessed, and, smoking status – current, former, never), we assessed changes from pre- to post-intervention using chi-square tests.
Results
Data presented reflect the findings from the 18 initial general internal medicine and family practice clinics. Table 1 provides summary statistics for clinic characteristics and outcomes pre-intervention (N=255,138 patient visits) and post-intervention (N=247,221 patient visits). As shown in Table 1, mean age across clinics at pre- and post-intervention were almost the same (53.6 and 54.0 years, respectively); mean percentages of females across clinics were also almost the same at the two time-points (60.3% and 60.6%, respectively). For the 12 months prior to the intervention, 71.6% of patient visit EMR records reflected documentation of smoking status overall, with a range of 54.8% to 95.7% across the 18 clinics. For the 12 months following the EMR modifications, 78.4% of patient visits documented smoking status in the EMR overall, with a range of 55.6% to 93.8%. This increase from 71.6% to 78.4% was statistically significant (p < .001, chi-square value of 3080.7 [df=1]). Adult smoking rates, based on patient-reported smoking status among patients who were asked about tobacco use, were also assessed; overall, the smoking rate declined from 17.2% pre-intervention (range 9.4% to 25.5%) to 16.1% post-intervention (range 8.9% to 22.7%), p < .001, chi-square value of 111.4 (df=1).
Table 1.
Clinic Characteristics and Outcomes, Pre- and Post-Intervention
| Characteristic or Outcome | Pre-Intervention (12 Months) | Post-Intervention (12 Months) |
|---|---|---|
| Total Number of Patients Seen Across All 18 Clinics | 255,138 | 247,221 |
| Number of Patients Seen Per Clinic, Mean (SD); (Range) | 14,174 (10,063); (2983 – 31,187) |
13,734 (9684); (1775 – 30,692) |
| Patient Age, Mean (SD) Across Clinics | 53.6 (18.8) | 54.0 (19.0) |
| Patient Gender, Mean % Females Across Clinics | 60.3% | 60.6% |
| Adult Smoking Status Identified, % Across Clinics (Range) | 71.6% (54.8% – 95.7%) |
78.6%* (55.6% – 93.8%) |
| Adult Smoking Rate, %1 (Range) | 17.2% (9.4% – 25.5%) |
16.1%** (8.9% – 22.7%) |
| Adult Smokers Prescribed Medication, Mean % Across Clinics (Range) | Not Available | 6.3% (2.9% – 10.2%) |
| Adult Smokers for which Smoking Cessation SmartSet was Used, Mean % Across Clinics (Range) | Not Available - | 2.5% (0% – 10.8%) |
| Adult Smokers Billed for Smoking Cessation Counseling, Mean % Across Clinics (Range) | Not Available | 1.5% (0% – 9.0%) |
Adult Smoking Rates are based on patient-reported smoking status among patients who were asked about tobacco use.
p < .001, chi-square value of 3080.7 (df=1)
p < .001, chi-square value of 111.4 (df=1)
Regarding utilization of the post-intervention SmartSet EMR modifications designed to prompt clinician intervention, 6.3% of identified adult smokers overall were prescribed one of the seven FDA approved medications during the 12 months post intervention with a range of 2.9% to 10.2% across the 18 clinics (Table 3). A lower percentage of identified adult smokers had documentation of utilization of the two other EMR modifications assessed: 2.5% of identified adult smokers overall had documentation that the tobacco dependence treatment EMR SmartSet was used and 1.5% of adult smokers overall had documentation that counseling was billed for during the clinic visit (Table 3).
Discussion
This demonstration project, designed to improve the identification and intervention of clinic patients who smoke by leveraging the power of an EMR, showed promising results: the proportion of adult patients whose tobacco use status was identified and documented significantly increased, and a meaningful number of those identified smokers received EMR-prompted clinical interventions.
A large body of research10 has highlighted the critical importance of identifying and documenting tobacco use status as an essential first step in prompting clinicians and health systems to deliver evidence-based treatment interventions to their patients who smoke. While a system to identify smokers was in place at Dean Health System prior to this set of EMR modifications, this project provides preliminary evidence that implementing an efficient, time-limited, consistent, and easy to learn set of workflow changes designed to address tobacco dependence results in higher rates of tobacco user identification and may enhance intervention rates.
This project also demonstrates that health systems can effectively implement a tobacco dependence treatment initiative. From the start, the project focused on developing a tobacco treatment intervention that took 60 seconds or less for the clinician. The project also emphasized that the EMR-based intervention was tailored for smokers willing to set a quit date within the next two weeks, typically representing only a few patients each day for the average clinician. As more health systems are encouraged to address tobacco use as part of an increasing focus of performance measures that include rates of identifying smokers and counseling them to quit, this demonstration project shows that tobacco dependence can be efficiently addressed via EMR prompts.
While we don't have data regarding the rates of clinical tobacco cessation interventions prior to the implementation of these EMR modifications, the results regarding clinical interventions following implementation are encouraging. Overall, 6.3% of smokers following the EMR changes were prescribed one of the FDA approved medications for tobacco dependence. This finding is consistent with some of the most effective clinical interventions for tobacco dependence in the published literature.17, 18 For example, in a NEJM article by Curry and colleagues describing an aggressive tobacco dependence program implemented in Group Health Cooperative of Puget Sound clinics, the highest rate of smoking cessation medication use was 6.9%.17 In our demonstration project with Dean Health System, rates of SmartSet use and billable counseling were less than medication use (2.5% and 1.5%, respectively), but these values may underestimate their actual usage – given that 6.3% of adult smokers left their clinic visit with a smoking cessation prescription medication that requires at least some clinician intervention to deliver.
The promise of the EMR led President Obama and the U.S. Congress in 2009 to allocate approximately $19 billion of the American Recovery and Reinvestment Act (ARRA) to implement electronic health record technology. It is estimated that by 2020, more than 90% of patients will have their health information housed within an EMR. The anticipated universal application of EMR technology provides an unequaled opportunity to fundamentally change the way we address the most pressing chronic diseases in America, including the leading preventable cause of morbidity and mortality: tobacco dependence.
This demonstration project has limitations. First, because the EMR modifications were introduced as a package, the effects from individual components cannot be determined. In addition, we don't have baseline data on rates of clinician interventions such as smoking cessation medication prescriptions within Dean clinics, but the reported post-intervention rates compare favorably with some of the most referenced examples of effective tobacco dependence treatment delivery. The study was cross sectional and focused on a single health care system, Dean (a large multispecialty clinic primarily based in an urban setting), and thus the results may differ when applied in other systems, possibly with other patient populations. We also did not monitor the time it took to deliver the intervention (goal was 60 seconds or less of clinician time) or the degree to which clinicians followed the protocol. And, while there was a statistically significant increase in the rate of smoker identification, this wasn't observed in every clinic. Finally, this was not a randomized trial with control clinics without the intervention, thus we can't rule out the influence of temporal trends and other factors, such as changes in tobacco control policies in Wisconsin that may have contributed to the increased rate of smoker identification and the high rates of prescribing smoking cessation medications.
In conclusion, this project demonstrated the capacity of a large health care system to implement enhanced tobacco dependence treatment interventions across their primary care clinics, utilizing the potential of the EMR platform. Associated with this enhancement was a statistically significant increase in rates of smoker identification and relatively high rates of clinical intervention with adult patients who smoke. The results are promising regarding the feasibility and potential of the EMR to influence the delivery of tobacco dependence clinical treatments.
Figure 4.
Clinic workflow diagram for adult patients who smoke presenting to primary care clinics.
Acknowledgments
The project was supported by contract #HHSN261200900453P from the National Institutes of Health, National Cancer Institute.
References
- 1.Tomar SL, Husten CG, Manley MW. Do dentists and physicians advise tobacco users to quit? J Am D Assoc. 1996;127:259–265. doi: 10.14219/jada.archive.1996.0179. [DOI] [PubMed] [Google Scholar]
- 2.Fang CY, Ma GX, Miller SM, et al. A brief smoking cessation intervention for Chinese and Korean American smokers. Prev Med. 2006;43:321–324. doi: 10.1016/j.ypmed.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Ferreira-Borges C. Effectiveness of a brief counseling and behavioral intervention for smoking cessation in pregnant women. Prev Med. 2005;41:295–302. doi: 10.1016/j.ypmed.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Fiore MC, Jorenby DE, Schensky AE, et al. Smoking status as the new vital sign: effect on assessment and intervention in patients who smoke. Mayo Clin Proc. 1995;70:209–213. doi: 10.4065/70.3.209. [DOI] [PubMed] [Google Scholar]
- 5.Glasgow RE, Whitlock EP, Eakin EG, et al. A brief smoking cessation intervention for women in low-income planned parenthood clinics. Am J Public Health. 2000;90:786–789. doi: 10.2105/ajph.90.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stead LF, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database of Systematic Reviews. 2008;(Issue 2) doi: 10.1002/14651858.CD000165.pub3. Art. No.: CD000165. DOI: 10.1002/14651858.CD000165.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Molyneux A, Lewis S, Leivers U, et al. Clinical trial comparing nicotine replacement therapy (NRT) plus brief counseling, brief counseling alone, and minimal intervention on smoking cessation in hospital inpatients. Thorax. 2003;58:484–488. doi: 10.1136/thorax.58.6.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rissel C, Salmon A, Hughes AM. Evaluation of a (pilot) stage-tailored brief smoking cessation intervention among hospital patients presenting to a hospital pre-admission clinic. Australian Health Review. 2000;23:83–93. doi: 10.1071/ah000083. [DOI] [PubMed] [Google Scholar]
- 9.Cokkinides VE, Ward E, Jemal A, et al. Under-use of smoking-cessation treatments: results from the National Health Interview Survey, 2000. Am J Prev Med. 2005;28:119–122. doi: 10.1016/j.amepre.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 10.Fiore MC, Jaén CR, Baker TB, et al. Clinical Practice Guideline. U.S. Department of Health and Human Services. Public Health Service; Rockville, MD: May, 2008. [Google Scholar]
- 11.Mechanic D, McAlpine DD, Rosenthal M. Are patient's office visits with physicians getting shorter? N Engl J Med. 2001;344:198–204. doi: 10.1056/NEJM200101183440307. [DOI] [PubMed] [Google Scholar]
- 12.Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential Health Benefits, Saving and Costs. Health Aff. 2005;24:1103–1117. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 13.Shea S, Hripcsak G. Accelerating the use of electronic health records in physician practices. N Engl J Med. 2010;362:192–195. doi: 10.1056/NEJMp0910140. [DOI] [PubMed] [Google Scholar]
- 14.Hivert MF, Grant RW, Shrader P, Meigs JB. Identifying primary care patients at risk for future diabetes and cardiovascular disease using electronic health records. BMC Health Services Research. 2009;9 doi: 10.1186/1472-6963-9-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bentz CJ, Bayley KB, Bonin KE, et al. Provider feedback to improve 5A's tobacco cessation in primary care: A cluster randomized clinical trial. Nicotine and Tobacco Research. 2007;9:341–349. doi: 10.1080/14622200701188828. [DOI] [PubMed] [Google Scholar]
- 16.Linder JA, Ma J, Bates DW, Middleton B, Stafford RS. Electronic health record use and the quality of ambulatory care in the United States. Arch Intern Med. 2007;167(13):1400–1405. doi: 10.1001/archinte.167.13.1400. [DOI] [PubMed] [Google Scholar]
- 17.Curry SJ, Grothaus LC, McAfee T, Pabiniak C. Use and cost effectiveness of smoking-cessation services under four insurance plans in a health maintenance organization. N Engl J Med. 1998;339:673–679. doi: 10.1056/NEJM199809033391006. [DOI] [PubMed] [Google Scholar]
- 18.Woods SS, Haskins AE. Increasing reach of quit line services in a US state with comprehensive tobacco treatment. Tob Control. 2007;16:i33–i36. doi: 10.1136/tc.2007.019935. [DOI] [PMC free article] [PubMed] [Google Scholar]