Abstract:
Background:
Falls are a leading cause of unintentional injury among adults age 65 years and older. Loose, unsecured rugs and damaged carpets with curled edges, are recognized environmental hazards that may contribute to falls. To characterize nonfatal, unintentional fall-related injuries associated with rugs and carpets in adults aged 65 years and older.
Methods:
We conducted a retrospective analysis of surveillance data of injuries treated in hospital emergency departments (EDs) during 2001–2008. We used the National Electronic Injury Surveillance System-All Injury Program, which collects data from a nationally representative stratified probability sample of 66 U.S. hospital EDs. Sample weights were used to make national estimates.
Results:
Annually, an estimated 37,991 adults age 65 years or older were treated in U.S. EDs for falls associated with carpets (54.2%) and rugs (45.8%). Most falls (72.8%) occurred at home. Women represented 80.2% of fall injuries. The most common location for fall injuries in the home was the bathroom (35.7%). Frequent fall injuries occurred at the transition between carpet/rug and non-carpet/rug, on wet carpets or rugs, and while hurrying to the bathroom.
Conclusions:
Fall injuries associated with rugs and carpets are common and may cause potentially severe injuries. Older adults, their caregivers, and emergency and primary care physicians should be aware of the significant risk for fall injuries and of environmental modifications that may reduce that risk.
Keywords: Floors, Floor coverings, Fall, Injury
Introduction
Falls are the leading cause of injuries requiring emergency treatment in adults aged 65 and older and lead to more hospital admission and deaths than any other type of trauma.1 They are also associated with increased premature mortality,2,3 loss of independence,4,5 and nursing home placement.6 In addition, fear of falling may lead to avoidance of activities,7-10 potentially reducing physical fitness and mobility and increaseing social isolation, time spent at home, and depression.
Falls in the elderly rarely have a single isolated cause but typically occur because of the interaction of multiple contributing factors. Researchers often classify these as intrinsic and extrinsic factors.11,12 Intrinsic factors include individual susceptibilities that increase fall risk such as chronic functional impairments (e.g. reduced balance or vision loss) and acute illnesses (e.g. pneumonia or myocardial infarction).11-17 Extrinsic or environmental risk factors, which include unsafe walking surfaces, obstacles in path, inappropriate footwear, and poor lighting,11-17 have been shown to play a part in approximately half of all home falls,18 and their importance in increasing risk has long been recognized by researchers19,20 and occupational therapists working with older adults.21,22
Loose throw rugs and area carpets with curled edges or folds are among the extrinsic factors most frequently mentioned in the literature as unsafe and potentially increasing fall risk.20,23,24 Research has shown that hazardous rugs and carpets may be the most common environmental hazard in the homes of older adults,25 with one study finding loose throw rugs in nearly 78% of the homes,26 curled carpet edges in more than 35%,26 an average of more than 11 rugs without nonslip backing in each home.25 These hazards are even more common in homes of frail older adults with disabilities,27 who are at higher risk for falls. Evidence also exists that these flooring types may increase risk of serious fall-related injury. Case control studies have found that both floor mats in hallways and bathmats significantly increased risk of hip fractures21 and that loose rugs / mats and flooring were among the most common objects in the home associated with falls resulting in hip fractures.28
Despite the intuitive connection between environmental hazards such as loose rugs and curled carpet edges and increased risk of falls, longitudinal research has shown mixed results. A hospital-based randomized controlled trial found that more falls occurred in the group housed in rooms with carpeted flooring than in rooms with vinyl flooring.29 Other studies, however, have not shown an association,30 and in one, the presence of loose throw rugs was actually associated with a decreased risk of fall among adults 65–84 years old.31
We chose to examine falls involving these flooring types, as the size and scope of this public health problem has not yet been well-defined. Our study objective is to more fully quantify and characterize fall injuries associated with rugs and carpets in older adults. To do this, we provide the first published U.S. national estimates of non-fatal fall-related injuries associated with these flooring types among adults aged 65 years and older that required emergency care. We hope to use this information to understand the public health burden of these injuries and to identify and prioritize appropriate intervention strategies.
Methods
Study Design and Data Source
This study analyzed data from the 2001–2008 National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP), a collaborative effort between the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control and the U.S. Consumer Product Safety Commission. NEISS-AIP collects data for emergency department visits for all types and causes of injuries from a nationally representative stratified probability sample of 66 hospitals in the United States and its territories having at least six beds and providing 24-hour emergency services. For each initial ED visit, coders record characteristics, including age, sex, and disposition of patients. Also recorded is one principal diagnosis, usually the most severe, as determined by the physician or healthcare provider and recorded in the medical chart, and one primary part of the body injured, on the basis of a fixed number of categories. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes are not available in the medical record at the time these data are collected; therefore, specific types of injuries, such as hip fractures, cannot be accurately identified. Brief two-line narratives about the circumstances of the injury are recorded for each case. Also, up to two products that are involved in an injury incident may be coded, with “product” broadly defined to include consumer products (e.g., walkers, canes, shoes) and other objects that are involved (e.g., floors, walls, or stairs). NEISS-AIP defines a fall injury as one received when a person descends because of the force of gravity and strikes a surface at the same or lower level. More information about NEISS-AIP is available at: http://www.cdc.gov/ncipc/wisqars /nonfatal/datasources.htm.
Study Sample
For our analysis, cases were defined as adults aged 65 years and older treated at an NEISS-AIP ED for a non-fatal, unintentional fall injury that occurred between January 1, 2001 and December 31, 2008 and that involved a rug or carpet. All cases with product codes 0612 (runners, throw rugs, or door mats, excluding bathmats), 0613 (room-sized, wall-to-wall, or outdoor carpeting, excluding runners), and/or 0676 (rugs or carpets, not specified) were included in this analysis. Additional cases were identified if the brief narrative contained mention of “rug” or “carpet”. Falls involving mats were excluded from analyses because the number of cases was too small (n=146) for meaningful analysis.
Qualitative Case Finding and Data Analysis
The narratives of all potential cases were individually reviewed and excluded if (1) the fall did not actually include a rug or carpet, (2) there was a clear alternative mechanism of fall described (e.g., patient tripped over the leg of a table and landed on carpet), (3) the subject was not standing on the floor or walking when the fall occurred (e.g., patient rolled out of bed and fell onto carpet or patient was standing on a chair, fell, and landed on rug), (4) if the carpet or rug was on a stair, or (5) it was not clear whether the fall involved a rug/carpet (e.g., the patient fell down several steps and landed on the carpeted floor). We excluded stair falls because the circumstances of falls on stairs are sufficiently different from falls on a flat surface to warrant separate analysis. Risk of falling on stairs depends on several factors in addition to floor covering, including, for example, the number of stairs, whether the person is ascending or descending, whether the person is at the top, middle, or bottom of the stairs, and whether guard rails are present.
Occupational injuries were identified by use of the work-related/occupational code and were excluded from analyses since work-related injuries would be covered by occupational safety standards. Despite these exclusion, the final number of useable cases was substantial (n=4,015).
Because rugs and carpets were included together in the same NEISS-AIP product categories, we used the text in the brief narrative comment to categorize them. In addition, because detailed information about the location of injury, such as room within the home or specific location outside the home (e.g., store, professional office, place of worship) is not explicitly captured in the NEISS-AIP dataset, the authors individually reviewed the brief narratives for each case and recorded this information when it was available. For example, bathroom was recorded if the narrative mentioned explicitly that the injury occurred in the bathroom or if the injury occurred when a patient tripped on a rug while getting out of the bathtub. For falls in the home, room could be specifically coded in 12% of the cases, while 88% remained unknown. For falls outside the home, location could be specifically coded in 87% of the cases, while 13% remained unknown.
Quantitative Data Analysis
All estimates were based on weighted data for 4,015 ED visits. Ninety-five percent confidence intervals (CI) were calculated by use of a direct variance estimation procedure that accounted for the sample weights and the complex sampling design. Estimates with coefficients of variation (CVs) greater than 30% were considered unstable, and rates and confidence intervals in such instances were not reported. Analyses were conducted by use of SPSS (SPSS Inc., Chicago, IL) complex samples to account for the sampling design.
Results
Quantitative Findings
On the basis of 4,015 cases in this sample, an estimated 37,991 fall injuries associated with rugs or carpets in adults aged 65 years and older were treated annually in U.S. EDs (Table 1). Approximately 54.2% of the fall injuries were associated with carpets and 45.8% with rugs. A large majority of fall injuries occurred at home (72.8%), while 15.2% occurred at locations outside the home and 12.0% did not include enough information to allow determination of the location. The age group accounting for the most injuries was 75–84 (45.2%). The body part most commonly injured was the head/neck (27.9%). Most patients (72.7%) were treated and then released after being seen in the emergency department.
Table 1: Annual estimates of nonfatal unintentional fall injuries in people age 65 years and older treated in US emergency departments and associated with carpets and rugs, 2001–2008.
| Characteristic | Total of Carpets and Rugs | Carpets | Rugs | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Annual estimate | Percent | 95% CI | Annual estimate | Percent | 95% CI | Annual estimate | Percent | 95% CI | |
| Total | 37991 | 100.0 | 20583 | 54.2 | 47.9-60.3 | 17408 | 45.8 | 39.7-52.1 | |
| Gender | |||||||||
| Men | 7512 | 19.8 | 18.3-21.3 | 3784 | 18.4 | 16.6-20.3 | 3728 | 21.4 | 19.1-23.9 |
| Women | 30467 | 80.2 | 78.7-81.7 | 16787 | 81.6 | 79.7-83.4 | 13680 | 78.6 | 76.1-80.9 |
| Location | |||||||||
| Home | 27649 | 72.8 | 67.6-77.4 | 14825 | 72.0 | 65.6-77.7 | 12823 | 73.7 | 68.3-78.4 |
| Outside home | 5785 | 15.2 | 12.6-18.2 | 3306 | 16.1 | 12.7-20.1 | 2479 | 14.2 | 11.8-17.0 |
| Unknown | 4557 | 12.0 | 7.8-18.0 | 2452 | 11.9 | 7.7-18.0 | 2105 | 12.1 | 7.6-18.8 |
| Age group (years) | |||||||||
| 65-74 | 8950 | 23.6 | 21.3-25.9 | 4254 | 20.7 | 18.2-23.4 | 4696 | 27.0 | 24.1-30.1 |
| 75-84 | 16159 | 42.5 | 40.0-45.1 | 8677 | 42.2 | 38.5-46.0 | 7483 | 43.0 | 40.5-45.5 |
| 85+ | 12882 | 33.9 | 31.5-36.4 | 7653 | 37.2 | 34.0-40.5 | 5229 | 30.3 | 27.5-32.7 |
| Injury Diagnosis | |||||||||
| Contusion | 10016 | 26.0 | 23.7-29.2 | 5640 | 27.4 | 24.6-30.4 | 4376 | 25.1 | 21.7-28.9 |
| Fracture | 15861 | 41.7 | 39.2-44.4 | 8775 | 42.6 | 40.0-45.3 | 7086 | 40.7 | 36.8-44.7 |
| Laceration | 4624 | 12.2 | 10.5-14.0 | 1988 | 9.7 | 8.0-11.6 | 2636 | 15.1 | 12.9-17.7 |
| Internal Injury | 2551 | 6.7 | 5.2-8.6 | 1467 | 7.1 | 5.6-9.0 | 1084 | 6.2 | 4.4-8.7 |
| Strain/sprain | 2859 | 7.5 | 6.5-8.7 | 1776 | 8.6 | 7.2-10.2 | 1083 | 6.2 | 4.9-7.9 |
| Other | 2080 | 5.5 | 4.3-6.9 | 937 | 4.6 | 3.5-6.0 | 1143 | 6.6 | 5.0-8.6 |
| Body part injured | |||||||||
| Head/neck | 10584 | 27.9 | 25.8-30.0 | 5388 | 26.2 | 23.5-29.0 | 5197 | 29.9 | 26.8-33.1 |
| Upper trunk | 5333 | 14.0 | 12.9-15.3 | 2817 | 13.7 | 12.0-15.6 | 2516 | 14.5 | 12.6-16.5 |
| Lower trunk | 9205 | 24.2 | 22.5-26.1 | 5574 | 27.1 | 25.2-29.0 | 3630 | 20.9 | 18.2-23.8 |
| Arm/hand | 5926 | 18.2 | 17.1-19.4 | 3705 | 18.0 | 16.5-19.6 | 3222 | 18.5 | 16.3-20.9 |
| Leg/Foot | 5726 | 15.1 | 13.9-16.3 | 2988 | 14.5 | 13.1-16.1 | 2738 | 15.7 | 13.9-17.8 |
| Other/unknown | 217 | 0.6 | 112 | 0.5 | 104 | 0.6 | |||
| Disposition | |||||||||
| Treated & released | 27634 | 72.7 | 69.4-75.8 | 14689 | 71.4 | 68.0-74.5 | 12945 | 74.4 | 69.7-78.5 |
| Hospitalized or transferred | 9988 | 26.3 | 23.3-29.5 | 5726 | 27.8 | 24.7-31.2 | 4262 | 24.5 | 20.5-28.9 |
| Other | 370 | 0.1 | 168 | 0.8 | 201 | 1.2 | |||
Table 1 also compares characteristics of fall injuries associated with carpets and rugs. Generally, we found few significant differences in injuries associated with the two flooring types. Notably, a significantly larger percentage of the younger old (65-74 years) were injured on rugs rather than carpets (27.0% vs. 20.7%), while a significantly larger percentage of the older old (85+ years) were injured on carpets (37.2% vs. 30.3%). Also, a significantly larger percentage of patients falling on rugs suffered laceration than those falling on carpets (15.1% vs. 9.7%), while a significantly larger percentage of carpet fallers injured their lower trunk (27.1% vs. 20.9%).
Women represented 80.2% of these rug and carpet-associated fall-related injuries. Characteristics of the injuries for men and women were generally similar, including similar rates of hospitalization, with a few notable exceptions. Women had significantly higher percentages of fracture (43.5% vs. 34.5%) (Table 2). Men had significantly higher percentages of head/neck injuries (33.7% vs. 26.4%).
Table 2: Annual estimates by gender of nonfatal unintentional fall injuries in people age 65 years and older treated in US emergency departments and associated with carpets and rugs, 2001–2008.
| Characteristic | Men | Women | ||||
|---|---|---|---|---|---|---|
| Annual estimate | Percent | 95% CI | Annual estimate | Percent | 95% CI | |
| Flooring Type | ||||||
| Carpet | 3784 | 50.4 | 43.5-57.2 | 16787 | 55.1 | 48.7-61.4 |
| Rug | 3728 | 49.6 | 42.8-56.5 | 13680 | 44.9 | 38.6-51.3 |
| Location | ||||||
| Home | 5485 | 73.0 | 66.5-78.7 | 22150 | 72.7 | 67.5-77.4 |
| Outside home | 1054 | 14.0 | 10.9-18.0 | 4731 | 15.5 | 12.7-18.8 |
| Unknown | 972 | 12.9 | 7.9-20.1 | 3585 | 11.8 | 7.7-17.6 |
| Age group (years) | ||||||
| 65-74 | 1940 | 25.8 | 21.8-30.3 | 7010 | 23.0 | 20.7-25.5 |
| 75-84 | 3167 | 42.2 | 38.6-45.8 | 12979 | 42.6 | 40.0-45.2 |
| 85+ | 2405 | 32.0 | 27.6-36.8 | 10477 | 34.4 | 31.8-37.1 |
| Injury Diagnosis | ||||||
| Contusion | 2084 | 27.7 | 23.3-32.7 | 7932 | 26.0 | 23.4-28.8 |
| Fracture | 2592 | 34.5 | 29.2-40.2 | 13256 | 43.5 | 40.9-46.1 |
| Laceration | 1142 | 15.2 | 11.8-19.4 | 3482 | 11.4 | 9.7-13.4 |
| Internal Injury | 692 | 9.2 | 6.9-12.1 | 1859 | 6.1 | 4.7-7.9 |
| Strain/sprain | 551 | 7.3 | 5.2-10.3 | 2309 | 7.6 | 6.5-8.9 |
| Other | 452 | 6.0 | 4.2-8.4 | 1629 | 5.3 | 4.2-6.8 |
| Body part injured | ||||||
| Head/neck | 2528 | 33.7 | 29.9-37.7 | 8056 | 26.4 | 24.4-28.6 |
| Upper trunk | 1170 | 15.6 | 12.8-18.8 | 4163 | 13.7 | 12.2-15.2 |
| Lower trunk | 1652 | 22.0 | 18.6-25.8 | 7540 | 24.7 | 22.8-26.8 |
| Arm/hand | 1123 | 14.9 | 12.0-18.5 | 5804 | 19.0 | 17.9-20.3 |
| Leg/Foot | 1012 | 13.5 | 11.7-15.5 | 4714 | 15.5 | 14.1-17.0 |
| Other/unknown | 28 | 0.4 | -- | 189 | 0.6 | -- |
| Disposition | ||||||
| Treated & released | 5537 | 73.7 | 67.5-79.1 | 22084 | 72.5 | 69.2-75.6 |
| Hospitalized or transferred | 1833 | 24.4 | 19.2-30.4 | 8155 | 26.8 | 23.7-30.0 |
| Other | 141 | 1.9 | -- | 228 | 0.7 | -- |
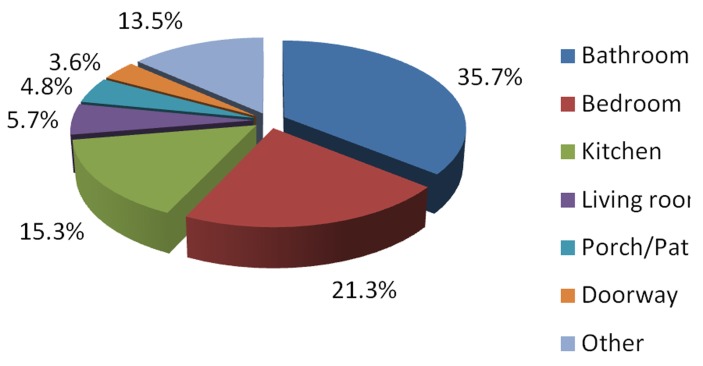
We evaluated the location in the home where fall injuries associated with rugs or carpets occurred for case files for which this information was available (333 of 4,015 cases; Figure 1). We excluded injuries occurring on carpeted or rug-covered stairs. The most common locations in the home where these injuries occurred were the bathroom (35.7%) and bedroom (21.3%). For falls occurring outside the home (detail not shown), the most common locations for fall injuries were nursing home / assisted living / group home (25.8%) and store / shopping mall / bank (19.2%).
Figure 1: Room/location in home where fall injuries occurred (n=333).
Qualitative Findings
Through qualitative review of the case narratives, we noted characteristic circumstances surrounding fall injuries. Older adults commonly fell and injured themselves at the transition between carpet/rug and non-carpet/rug. Wet carpets or rugs often contributed to falls. Patients frequently suffered an injurious fall while “hurrying to” or “trying to get to” the bathroom.
Discussion
This study is, to our knowledge, the first national report of non-fatal, unintentional fall injuries associated with a rug or carpet and sustained by adults age 65 years or older who were treated in EDs. With nearly 38,000 adults requiring emergency treatment annually, rug and carpet-associated fall injuries are clearly an issue worthy of public health attention, although in the context of over 2.2 million fall injuries annually in older adults requiring emergency treatment,1 this is just one piece of a much larger picture.
Several aspects of rug and carpet-associated fall injuries in our study are consistent with fall injuries in general among older adults, suggesting that the injuries suffered may be similar to those from falls not associated with these flooring types. Most of the injuries occurred in the home. This is consistent with falls research, which has suggested that 70–80% of falls occur in and around an older adult’s home.5,32 This is likely because community-dwelling older adults, particularly those who are frail and therefore at increased fall risk, spend most of their time at home and, therefore, have more exposure to environmental hazards in the home. Our results showed generally increasing percentages of fall injuries in advancing age groups, with a decrease in the highest age group. This is consistent with previous research, which has shown that risk of experiencing a fall at home increases with advancing age.33-35
In our study, women represented more than 80% of those injured. Evidence exists that older women may fall more frequently than older men, perhaps because of greater impairment of balance and the muscle power required to counteract destabilization.36-41 Women are also more likely to suffer an injury from falling.42 Notably, that study found fractures were 2.2 times more common in women than in men and injuries of the arm/hand were 2.0 times as common. This increased risk of fractures in women, which is consistent with our findings, is thought to be due to higher rates of osteoporosis and decreased bone mass.43 In addition, cultural gender roles may have an impact on these findings, as women may be more likely than men to seeking medical care sooner after the injury.44
In our study, a significantly higher percentage of male fallers suffered head and neck injuries. Previous research has shown that adult men are more likely than women to suffer a traumatic brain injury45,46 and were more likely to require hospitalization.47 This may be due to greater vulnerability or other differences in the underlying causes or circumstances of their falls.42 One notable difference between our findings and current falls research in general is that we found similar hospitalization rates for men and women for rug and carpet-related fall injuries, despite recent research on fall injuries in general, which found that women are 1.8 times more likely to be hospitalized.42 Our finding of rough equivalence may be potentially explained by an increase in hospitalization for fracture-related injuries for women in our sample being balanced by greater hospitalization rates for head / neck injury for men, or it may provide evidence that rug and carpet--associated falls are different from other falls in another way.
That older adults commonly suffered fall injuries at the edge between carpet and non-carpeted floor in this study is not surprising. Transition areas often have differences in floor height48 and may pose a problem for the rubber tips of canes or crutches.49 Transitions frequently occur at areas of light differences, which pose additional risks.50-52 In this sample, the bathroom was the most frequent location in the home for fall injuries to occur, supporting recent literature that suggests that bathroom falls are common.53 Previous reports have found that bathrooms are the most common site for environmental hazards in the home,54 with 45% of older adult fallers having throw rugs in their bathrooms.31 These rugs are likely to get wet, making them potentially even more hazardous, particularly if they are not secured to the floor. Older adults engage in balance-displacing activities in the bathroom, such as transferring to/from the bathtub and toilet.
Our work is subject to several limitations. We cannot evaluate how many steps those in the sample took on rugs and carpets vs. other flooring types, so it is not possible to use analytic epidemiology to evaluate risk. In addition, this report includes only non-fatal injuries treated in EDs. We are missing injuries that were treated in physician offices, free-standing medical centers, or other clinics, as well as those injuries that did not require medical attention. Injuries that proved fatal before or in the ED were excluded because NEISS-AIP does not provide detailed information about fatal injuries. However, only approximately 0.5% of unintentional injuries result in death.1
Also, we relied on the product code and the two-line brief narrative comment in NEISS-AIP to categorize these fall injuries and to decide which cases to exclude. These brief narratives are variable in their clarity and comprehensiveness and they rely on accurate and complete patient history, physician documentation in the medical record, and abstraction for the NEISS database. One strength of our approach, however, was that by qualitatively evaluating the data, we were able to glean details that may be important for fall prevention programs including an emphasis on the transition between carpet/rug and non-carpet/rug, wet carpet or rugs, and situations such as “hurrying to the bathroom.”
Further, as most of the fall injuries under study were likely unwitnessed, the causative relevance of the rug or carpet as an environmental hazard depends on the victim’s self-report, including the victim’s identification of the hazard and willingness to report it. This self-reporting method may have led to over- and under-reporting, but given the tendency for older persons and their family members to blame the environment for falls, over-reporting is more probable.32
In addition, identifying falls that are meaningfully associated with a flooring type is challenging because nearly all fall victims ultimately land on the floor, whether or not it played an important causal role in the event. We have tried to systematically remove from our analysis all files for which the rug or carpet played only an obviously incidental role (a patient who syncopized and landed on the carpet, for example).
Rugs and carpets may vary dramatically in such characteristics as size, fiber type, pile height, face weight, fiber density, color, pattern, and padding thickness, all of which may significantly affect the associated risk of fall and fall injury and none of which we were able to capture in this study.
Finally, our ability to draw conclusions about in which rooms in the home falls most commonly occurred was limited by the absence of this information in the narrative comments of a large percentage of the cases.
Conclusion
Falls in the elderly are an important public health problem, and our research demonstrates that a significant number of these falls are associated with rugs and carpets. Older adults and their families and caregivers should be aware of these risks. Emergency physicians, when treating an older patient for a fall injury, may consider asking the patient about the environmental circumstances surrounding the incident and suggesting potential environmental modifications. Primary care physicians should counsel their patients at high risk for falls to be mindful of potentially dangerous rugs or carpets. Fall injuries may be affected by securing rugs with adhesive tape or using non-skid backing, checking for and repairing curled carpet edges. Bathrooms, transitions between rug/carpeted areas and non-rug/carpeted areas, and wet rugs or carpets are particularly dangerous. Notably, evidence to date only shows reduction in falls for home modification programs when implemented by an occupational therapist.55 Environmental modifications should be combined with other effective fall prevention strategies such exercise to increase lower body strength, regular vision checks, and frequent assessment for fall risks including a medication review by health care providers.56 More research is needed to determine the safest flooring types for older adults and other environmental modifications that may reduce falls. Increasing awareness of the potential hazards associated with rugs and carpets, combined with simple environmental changes may benefit older adults by decreasing the risk for fall injuries.
Acknowledgements
We are grateful to Rosemary Bakker for sharing her expertise on home design for older adults and for offering us the opportunity to view her in-press manuscript. We are grateful to Therese Crahan and the National Association of Home Builders for sharing elements of that organization’s Certified Aging-in-Place Specialist (CAPS) curriculum. We thank Lowell Gerson, who offered his thoughts and opinions on falls and on emergency medicine. We appreciate Health Professions Press for sharing an advance copy of Rein Tideiksaar’s Falls in Older Persons: Prevention and Management, 4th Edition. We thank the Kottke family for their hospitality during Tony Rosen’s work in Atlanta, GA.
Footnotes
Funding:None
Competing interests:None declared
Ethical approval:Not required
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
References
- 1. Center for Diseases Control and Prevention(CDC). Web-based Injury Statistics Query and Reporting System (WISQARS). http://www.cdc.gov/injury/ wisqars/, accessed 6 April 2010. [Google Scholar]
- 2.Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992 Jul;82(7):1020–3. doi: 10.2105/ajph.82.7.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sterling DA, O'Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001 Jan;50(1):116–9. doi: 10.1097/00005373-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Kiel DP, O'Sullivan P, Teno JM, Mor V. Health care utilization and functional status in the aged following a fall. Med Care. 1991 Mar;29(3):221–8. doi: 10.1097/00005650-199103000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Schiller JS, Kramarow EA, Dey AN. Fall injury episodes among noninstitutionalized older adults: United States, 2001-2003. Adv Data. 2007 Sep 21;(392):1–16. [PubMed] [Google Scholar]
- 6.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997 Oct 30;337(18):1279–84. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 7.Fletcher PC, Hirdes JP. Restriction in activity associated with fear of falling among community-based seniors using home care services. Age Ageing. 2004 May;33(3):273–9. doi: 10.1093/ageing/afh077. [DOI] [PubMed] [Google Scholar]
- 8.Kressig RW, Wolf SL, Sattin RW, O'Grady M, Greenspan A, Curns A, et al. Associations of demographic, functional, and behavioral characteristics with activity-related fear of falling among older adults transitioning to frailty. J Am Geriatr Soc. 2001;49(11):1456–62. doi: 10.1046/j.1532-5415.2001.4911237.x. [DOI] [PubMed] [Google Scholar]
- 9.Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol. 1994 May;49(3):M140–7. doi: 10.1093/geronj/49.3.m140. [DOI] [PubMed] [Google Scholar]
- 10.Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ. Fear of falling and restriction of mobility in elderly fallers. Age Ageing. 1997 May;26(3):189–93. doi: 10.1093/ageing/26.3.189. [DOI] [PubMed] [Google Scholar]
- 11.Tinetti ME, Speechley M. Prevention of falls among the elderly. N Engl J Med. 1989 Apr 20;320(16):1055–9. doi: 10.1056/NEJM198904203201606. [DOI] [PubMed] [Google Scholar]
- 12.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988 Dec 29;319(26):1701–7. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 13.Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? Med Clin North Am. 2006 Sep;90(5):807–24. doi: 10.1016/j.mcna.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 14.Pynoos J, Steinman BA, Nguyen AQ. Environmental assessment and modification as fall-prevention strategies for older adults. Clin Geriatr Med. 2010 Nov;26(4):633–44. doi: 10.1016/j.cger.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nickens H. Intrinsic factors in falling among the elderly. Arch Intern Med. 1985 Jun;145(6):1089–93. [PubMed] [Google Scholar]
- 16.Bueno-Cavanillas A, Padilla-Ruiz F, Jimenez-Moleon JJ, Peinado-Alonso CA, Galvez-Vargas R. Risk factors in falls among the elderly according to extrinsic and intrinsic precipitating causes. Eur J Epidemiol. 2000;16(9):849–59. doi: 10.1023/a:1007636531965. [DOI] [PubMed] [Google Scholar]
- 17.Akyol AD. Falls in the elderly: what can be done? Int Nurs Rev. 2007 Jun;54(2):191–6. doi: 10.1111/j.1466-7657.2007.00505.x. [DOI] [PubMed] [Google Scholar]
- 18.Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA. 1989 May 12;261(18):2663–8. [PubMed] [Google Scholar]
- 19.Josephson KR, Fabacher DA, Rubenstein LZ. Home safety and fall prevention. Clin Geriatr Med. 1991 Nov;7(4):707–31. [PubMed] [Google Scholar]
- 20.Rubenstein LZ. The importance of including the home environment in assessment of frail older persons. J Am Geriatr Soc. 1999 Jan;47(1):111–2. doi: 10.1111/j.1532-5415.1999.tb01911.x. [DOI] [PubMed] [Google Scholar]
- 21.Clemson L, Cumming RG, Roland M. Case-control study of hazards in the home and risk of falls and hip fractures. Age Ageing. 1996 Mar;25(2):97–101. doi: 10.1093/ageing/25.2.97. [DOI] [PubMed] [Google Scholar]
- 22.Cumming RG, Thomas M, Szonyi G, Salkeld G, O'Neill E, Westbury C, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: a randomized trial of falls prevention. J Am Geriatr Soc. 1999 Dec;47(12):1397–402. doi: 10.1111/j.1532-5415.1999.tb01556.x. [DOI] [PubMed] [Google Scholar]
- 23.Waller JA. Falls among the elderly: human and environmental factors. Accid Anal Prev. 1978;10:21–33. [Google Scholar]
- 24.Bakker R. Elderdesign: home modifications for enhanced safety and self-care. Care Manag J. 1999 Feb;1(1):47–54. [PubMed] [Google Scholar]
- 25.Stevens M, Holman CD, Bennett N. Preventing falls in older people: impact of an intervention to reduce environmental hazards in the home. J Am Geriatr Soc. 2001 Nov;49(11):1442–7. doi: 10.1046/j.1532-5415.2001.4911235.x. [DOI] [PubMed] [Google Scholar]
- 26.Gill TM, Williams CS, Robison JT, Tinetti ME. A population-based study of environmental hazards in the homes of older persons. Am J Public Health. 1999 Apr;89(4):553–6. doi: 10.2105/ajph.89.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gill TM, Robison JT, Williams CS, Tinetti ME. Mismatches between the home environment and physical capabilities among community-living older persons. J Am Geriatr Soc. 1999 Jan;47(1):88–92. doi: 10.1111/j.1532-5415.1999.tb01906.x. [DOI] [PubMed] [Google Scholar]
- 28.Norton R, Campbell AJ, Lee-Joe T, Robinson E, Butler M. Circumstances of falls resulting in hip fractures among older people. J Am Geriatr Soc. 1997 Sep;45(9):1108–12. doi: 10.1111/j.1532-5415.1997.tb05975.x. [DOI] [PubMed] [Google Scholar]
- 29.Donald IP, Pitt K, Armstrong E, Shuttleworth H. Preventing falls on an elderly care rehabilitation ward. Clin Rehabil. 2000 Apr;14(2):178–85. doi: 10.1191/026921500677888641. [DOI] [PubMed] [Google Scholar]
- 30.Gill TM, Williams CS, Tinetti ME. Environmental hazards and the risk of nonsyncopal falls in the homes of community-living older persons. Med Care. 2000 Dec;38(12):1174–83. doi: 10.1097/00005650-200012000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Sattin RW, Rodriguez JG, DeVito CA, Wingo PA. Home environmental hazards and the risk of fall injury events among community-dwelling older persons. Study to Assess Falls Among the Elderly (SAFE) Group. J Am Geriatr Soc. 1998 Jun;46(6):669–76. doi: 10.1111/j.1532-5415.1998.tb03799.x. [DOI] [PubMed] [Google Scholar]
- 32. Tideiksaar R. Falling in old age : prevention and management. 2nd ed. New York: Springer Pub Co, 1997. [Google Scholar]
- 33.Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol. 1989 Jul;44(4):M112–7. doi: 10.1093/geronj/44.4.m112. [DOI] [PubMed] [Google Scholar]
- 34.Nevitt MC, Cummings SR, Hudes ES. Risk factors for injurious falls: a prospective study. J Gerontol. 1991 Sep;46(5):M164–70. doi: 10.1093/geronj/46.5.m164. [DOI] [PubMed] [Google Scholar]
- 35.Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002 May;18(2):141–58. doi: 10.1016/s0749-0690(02)00002-2. [DOI] [PubMed] [Google Scholar]
- 36.Bassey EJ. Longitudinal changes in selected physical capabilities: muscle strength, flexibility and body size. Age Ageing. 1998 Dec;27(Suppl 3):12–6. doi: 10.1093/ageing/27.suppl_3.12. [DOI] [PubMed] [Google Scholar]
- 37.Caserotti P, Aagaard P, Simonsen EB, Puggaard L. Contraction-specific differences in maximal muscle power during stretch-shortening cycle movements in elderly males and females. Eur J Appl Physiol. 2001 Mar;84(3):206–12. doi: 10.1007/s004210170006. [DOI] [PubMed] [Google Scholar]
- 38.Prudham D, Evans JG. Factors associated with falls in the elderly: a community study. Age Ageing. 1981 Aug;10(3):141–6. doi: 10.1093/ageing/10.3.141. [DOI] [PubMed] [Google Scholar]
- 39.Winner SJ, Morgan CA, Evans JG. Perimenopausal risk of falling and incidence of distal forearm fracture. BMJ. 1989 Jun 3;298(6686):1486–8. doi: 10.1136/bmj.298.6686.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wolfson L, Whipple R, Derby CA, Amerman P, Nashner L. Gender differences in the balance of healthy elderly as demonstrated by dynamic posturography. J Gerontol. 1994 Jul;49(4):M160–7. doi: 10.1093/geronj/49.4.m160. [DOI] [PubMed] [Google Scholar]
- 41.Simpson AH, Lamb S, Roberts PJ, Gardner TN, Evans JG. Does the type of flooring affect the risk of hip fracture? Age Ageing. 2004 May;33(3):242–6. doi: 10.1093/ageing/afh071. [DOI] [PubMed] [Google Scholar]
- 42.Stevens JA, Sogolow ED. Gender differences for non-fatal unintentional fall related injuries among older adults. Inj Prev. 2005 Apr;11(2):115–9. doi: 10.1136/ip.2004.005835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Greenspan SL, Myers ER, Maitland LA, Resnick NM, Hayes WC. Fall severity and bone mineral density as risk factors for hip fracture in ambulatory elderly. JAMA. 1994 Jan;271(2):128–33. [PubMed] [Google Scholar]
- 44. World Health Organization.WHO Global Report on Falls Prevention in Older Age. 2007, http://www.who.int/ageing/publications/-Falls_prevention7March.pdf,accessed 20 March 2012. [Google Scholar]
- 45.Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: epidemiology, outcomes, and future implications. J Am Geriatr Soc. 2006 Oct;54(10):1590–5. doi: 10.1111/j.1532-5415.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Coronado VG, Thomas KE, Sattin RW, Johnson RL. The CDC traumatic brain injury surveillance system: characteristics of persons aged 65 years and older hospitalized with a TBI. J Head Trauma Rehabil. 2005 Jun;20(3):215–28. doi: 10.1097/00001199-200505000-00005. [DOI] [PubMed] [Google Scholar]
- 47. Centers for Disease Control and Prevention (CDC).Nonfatal fall-related traumatic brain injury among older adults--California, 1996-1999. MMWR Morb Mortal Wkly Rep. 2003 Apr;52(13):276-8. [PubMed] [Google Scholar]
- 48. McCullagh MC. Home modification. Am J Nurs. 2006 Oct;106(10):54-63; quiz 63 -4. [DOI] [PubMed] [Google Scholar]
- 49. Gulwadi GB, KellerAB. Falls in healthcare settings. Health Design 2009, http://www.healthcaredesignmagazine.com, accessed 20 March 2012. [Google Scholar]
- 50. Tideiksaar R. Falls in older people : prevention and management. 4th ed. Baltimore, MD: Health Professions Press, 2010. [Google Scholar]
- 51. Tideiksaar R. Preventing falls: how to identify risk factors, reduce complications. Geriatrics. 1996 Feb;51(2):43-6, 49-50, 53, quiz 54-5. [PubMed] [Google Scholar]
- 52.Tideiksaar R. Geriatric falls in the home. Home Healthc Nurse. 1986 Mar;4(2):14–23. doi: 10.1097/00004045-198603000-00004. [DOI] [PubMed] [Google Scholar]
- 53. Centers for Disease Control and Prevention (CDC).Nonfatal bathroom injuries among persons aged >/=15 years--United States, 2008. MMWR Morb Mortal Wkly Rep. 2011Jun10;60(22):729-33. [PubMed] [Google Scholar]
- 54.Huang TT. Home environmental hazards among community-dwelling elderly persons in Taiwan. J Nurs Res. 2005 Mar;13(1):49–57. [PubMed] [Google Scholar]
- 55. Stevens JA, Sogolow ED. Preventing Falls: What Works A CDC Compendium of Effective Community-based Interventions from Around the World. Atlanta, Georgia: National Center for Injury Prevention and Control, 2008. [Google Scholar]
- 56. Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011Jan;59(1):148-57. [DOI] [PubMed] [Google Scholar]