Abstract
Despite major advances in the development of antiretroviral therapies, currently available treatments have no effect on the production of HIV-Tat protein once the proviral DNA is formed. Tat is a highly neurotoxic and neuroinflammatory protein, but its effects may be modulated by antibody responses against it. We developed an indirect enzyme linked immunosorbent assay and measured anti-Tat antibody titers in CSF of a well characterized cohort of 52 HIV-infected and 13 control individuals. We successfully measured anti-Tat antibodies in CSF of HIV infected individuals with excellent sensitivity and specificity, spanning a broad range of detection from 10,000 to over 100,000 relative light units (RLUs). We analyzed them for relationship to cognitive function, CD4 cell counts and HIV viral load. Anti-Tat antibody levels were higher in those without neurocognitive dysfunction than in those with HIV-associated neurocognitive dysfunction (HAND), and in individuals with lower CD4 cell counts and higher viral loads. We provide details of an assay which may have diagnostic, prognostic, or therapeutic implications for patients with HAND. Active viral replication may be needed to drive the immune response against Tat protein, but this robust immune response against the protein may be neuroprotective.
Keywords: neurotoxicity, neurovirology, dementia, neuroprotection, glutamate, neutralizing antibodies
INTRODUCTION
HIV infects glial cells and can establish a reservoir within the brain. Infected cells in the brain can release neurotoxic viral proteins, including the HIV transactivator protein, Tat (Tornatore et al. 1994a; Tornatore et al. 1994b). The advent of highly active antiretroviral therapy (HAART) has successfully decreased the incidence of HIV dementia by lowering viral load, thus enabling the recovery of CD4+ T cells and restoring immunity (Sacktor et al. 2001). However, the prevalence of HIV-associated neurocognitive disorders (HAND) is actually increasing, because individuals on HAART are living longer (Dore et al. 2003; Neuenburg et al. 2002; Sacktor 2002; Sacktor et al. 2002; Simpson et al. 2003). Once proviral DNA is formed, HAART fails to target the early viral proteins. Of these proteins, Tat is released extracellularly, where it is highly neurotoxic and can be transported along neuronal pathways to cause neuronal injury at distant sites. It interacts with glial cells to induce activation and release of neurotoxic factors, leading to widespread damage. (Rumbaugh and Nath 2006).
Interestingly, some individuals never develop HAND despite severe immune suppression and high viral loads. This suggests that host susceptibility genes play an important role in the neuropathogenesis of this condition. The impact of variations in chemokines and cytokines likely reflects the importance of a host-generated inflammatory cascade (Gonzalez et al. 2002; Quasney et al. 2001). Another possibility is that variations in the host’s adaptive immune response affect susceptibility to HAND. For example, the ability of the host to produce neutralizing antibodies to Tat may affect Tat’s ability to cause neurotoxicity. This may have important implications for development of a vaccine strategy to treat or prevent HIV dementia and other neurological complications of HIV infection.
It is therefore imperative to monitor levels of antibodies to viral proteins within the CNS, as both diagnostic and prognostic markers. HIV infection is unique in that detection of virus or antibody to virus in the spinal fluid is not considered diagnostic of viral invasion of the CNS, whereas diagnosis of other common viral encephalitides, such as Herpes simplex encephalitis, require detection of virus or virus specific antibodies within the CNS. Previous studies have attempted to detect viral proteins and their transcripts within the CNS of infected individuals, but have not proven effective for quantitation due to lack of sensitivity (Hudson et al. 2000; Kruman et al. 1999; Trujillo et al. 1996; Westendorp et al. 1995; Wiley et al. 1996). Tat antibodies have not previously been studied in CSF.
MATERIALS AND METHODS
Study samples
CSF samples used were obtained from Northeastern AIDS Dementia (NEAD) cohort, Johns Hopkins Oxidative Stress cohort, and National NeuroAIDS Tissue Consortium (NNTC). Viral loads and CD4 cell counts were assessed at the same time that the cognitive testing was performed, as described (McArthur et al. 2004). HIV-infected samples were from individuals categorized by Memorial Sloan Kettering (MSK) scale as individuals with no cognitive impairment (MSK=0, n=15), with mild cognitive impairment (MSK=0.5–1, n=20), and with moderate cognitive impairment (MSK≥2, n=17). The HIV-infected individuals in this study showed no correlation between their neurocognitive status and their blood and CSF viral loads and CD4 cell counts. Thus, correlations which we demonstrate based on neurocognitive status should not be confounded by viral load or immune status.
Control groups included individuals with other neuro-inflammatory or neuro-infectious diseases (n=8) and non-inflammatory controls (normal pressure hydrocephalus, n=5). These individuals did not have risk factors for HIV infection. All samples had been centrifuged prior to storage, hence only cell free CSF was used. Table 1 provides a summary of clinical details of HIV-infected individuals. Table 2 provides clinical data regarding controls. Data on each individual patient is available in Table 3.
Table 1.
Summary of the clinical data of HIV-infected individuals used in this study: HIV infected individuals without dementia (HIV+ normal) (MSK 0) (n=15), with mild cognitive impairment (MSK 0.5–1) (n=20), with moderate cognitive impairment (MSK≥2) (n=17). Blood and CSF viral loads represent copies/ml and CD4 cells represent lymphocyte cell count per μl.
| age (median) | SEX (n) | blood viral load (n) | CSF viral load (n) | CD4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| male | female | unknown | <400 | >400 | <400 | >400 | unavailable | average | median | <250 (n) | >250 (n) | ||
| HIV+ Normal | 47.5 | 9 | 5 | 1 | 9 | 5 | 11 | 3 | 0 | 372.8 | 319.5 | 6 | 8 |
| HIV+ mild cog impair | 45.5 | 15 | 5 | 0 | 15 | 5 | 14 | 3 | 3 | 297.8 | 268.5 | 9 | 11 |
| HIV+ mod cog impair | 47 | 14 | 3 | 0 | 10 | 7 | 14 | 2 | 1 | 347.1 | 320 | 10 | 7 |
Table 2.
Summary of the clinical diagnosis of HIV-negative individuals used in this study: Neuro-inflammatory control individuals (n=8) and non-inflammatory control individuals (n=5).
| Sex (n) | Diagnosis (n) | |||||
|---|---|---|---|---|---|---|
| Male | Female | Neurosar-coidosis | Multiple Sclerosis | Transverse Myelitis/Multiple Sclerosis | Normal Pressure Hydrocephalus | |
| Neuro-Inflammatory | 5 | 3 | 2 | 5 | 1 | 0 |
| Non-Inflammatory | 3 | 2 | 0 | 0 | 0 | 5 |
Table 3.
Clinical data of HIV-infected individuals used in this study: HIV infected individuals without dementia (HIV-no dementia) (MSK 0) (n=15), with mild cognitive impairment (MSK 0.5–1) (n=20), with moderate cognitive impairment (MSK≥2) (n=17). Blood and CSF viral loads represent copies/ml and CD4 cells represent lymphocyte cell count per μl.
| age | sex | Yr HIV inf | Blood VL | CSF VL | CD4 | date of death | |
|---|---|---|---|---|---|---|---|
| HIV-Normal | 61 | F | 1994 | ND | ND | 419 | |
| 48 | M | 1988 | 17629 | 17290 | 101 | 4/14/2006 | |
| 48 | M | 1988 | <400 | ND | 1113 | ||
| 47 | M | 1981 | 20916 | 507 | 36 | ||
| 33 | F | 1992 | 14280 | 434 | 152 | ||
| 46 | F | 1989 | <50 | ND | 418 | ||
| 62 | M | 1988 | <50 | ND | 651 | ||
| 66 | M | 1992 | <50 | ND | 150 | ||
| 44 | M | 1991 | 1805 | <50 | 354 | ||
| 41 | F | 1994 | <50 | <50 | 663 | ||
| 54 | M | 1995 | <50 | <50 | 285 | ||
| 52 | F | 1995 | <50 | <50 | 618 | ||
| 37 | M | 2001 | 32256 | <50 | 12 | ||
| 31 | M | 2005 | <50 | <50 | 247 | ||
|
| |||||||
| HIV-mild cog impair | 57 | M | 1990 | ND | ND | 405 | |
| 57 | M | 1989 | ND | ND | 221 | 2/19/2006 | |
| 40 | M | 1993 | <400 | ND | 189 | ||
| 41 | M | 1991 | <400 | 1399 | 202 | ||
| 49 | M | 1996 | <400 | <50 | 170 | ||
| 52 | M | 1992 | <50 | ND | 250 | ||
| 62 | M | 1988 | <50 | unavail | 287 | ||
| 45 | F | 1991 | 66328 | 2869 | 2 | ||
| 45 | M | 1995 | 13586 | unavail | 48 | ||
| 42 | M | 1986 | <400 | <400 | 460 | ||
| 49 | M | 2001 | <50 | <50 | 543 | ||
| 42 | F | 1992 | <50 | <50 | 617 | ||
| 49 | M | 1993 | 21777 | 3072 | 204 | ||
| 55 | F | 1994 | <50 | <50 | 455 | ||
| 50 | M | 1989 | <50 | unavail | 490 | ||
| 46 | F | 1993 | <50 | <50 | 173 | ||
| 38 | M | 1985 | >100000 | 97 | 5 | ||
| 44 | M | 2004 | <50 | <50 | 302 | ||
| 45 | M | 1992 | <50 | <50 | 494 | ||
| 37 | F | 1996 | 5538 | <50 | 439 | ||
|
| |||||||
| HIV-mod cog impair | 50 | M | 1986 | <400 | <50 | 983 | |
| 41 | M | 1992 | 29381 | ND | 15 | 5/22/2004 | |
| 44 | M | 1996 | 38207 | 9656 | 28 | ||
| 45 | M | 1997 | 170352 | ND | 165 | ||
| 61 | M | 1985 | 1096 | ND | 57 | ||
| 51 | M | 1992 | <50 | ND | 665 | ||
| 49 | F | 1995 | <50 | ND | 671 | ||
| 46 | M | 1998 | <50 | ND | 320 | ||
| 42 | F | 1992 | 928 | 161 | 309 | ||
| 46 | M | 1986 | 221756 | 1618 | 395 | ||
| 46 | M | 1990 | <50 | <50 | 422 | ||
| 55 | M | 1985 | 285 | unavail | 135 | ||
| 47 | M | 1997 | 83 | <50 | 417 | ||
| 51 | M | 1989 | 65836 | 336 | 2 | ||
| 34 | M | 1999 | <50 | <50 | 520 | ||
| 54 | F | 1988 | <50 | <50 | 215 | ||
| 59 | M | 1986 | <50 | <50 | 582 | ||
Use of the specimens required for this study was approved by the Johns Hopkins Institutional Review Board.
Preparation of the ELISA Plate
A white opaque 96-well maxisorp plate (Nunc) was coated with Tat1-72 at 2μg/ml in carbonate buffer (Na2CO3 1.59g/l, NaHCO3 2.93g/l, pH 9.6) and incubated overnight at 4°C. Recombinant Tat1-72 was produced in our laboratory, as published previously (Ma and Nath 1997; Turchan et al. 2001). The plate was then treated with blocking buffer (1% bovine serum albumin/0.1% Tween-20 in phosphate buffered saline [PBS], pH 7.4) for 2 hours at room temperature. Anti-tat antibodies were then added at 100μl/well serially diluted 10-fold in blocking buffer to generate standard curves with concentrations as low as 10−3 pg/μl. We used either affinity-purified rabbit anti-Tat polyclonal antibodies (pABs) to whole Tat (generated in our laboratory) or mouse anti-Tat monoclonal antibody (mAB) to the C-terminus that was purified from a hybridoma cell line (NIH AIDS Research and Reference Reagent Program, Bethesda, MD, USA; cat#7383).
After the antibodies were incubated for 2 hours at room temperature, the plate was washed 3 times with washing buffer (0.1% Tween-20 in PBS, pH 7.4). Biotinylated antibodies, 100μl/well, diluted 1000-fold in blocking buffer, were incubated for 1 hour at room temperature: biotinylated goat anti-mouse antibody (Chemicon cat#AP130B) was used for wells incubated with mouse monoclonal antibodies and biotinylated goat anti-rabbit antibody (Chemicon cat#AP132B) for wells incubated with rabbit polyclonal antibodies. The plate was washed thereafter and streptavidin-HRP (BioRad cat#170-6528), 100μl/well, also diluted 1000-fold in blocking buffer, was incubated for 1 hour at room temperature. The plate was washed again and subsequently developed with SuperSignal Femto Sensitivity substrate (Pierce cat#37074), 100 μl/well. The luminescence was measured within 5 minutes at 425 nm on a microplate reader (SpectraMax, Molecular Devices). These antibodies were found to have higher titer binding values, demonstrating optimal coating of Tat1-72 to the plate.
Treatment of CSF Samples
CSF samples were first heat-inactivated at 60°C for 30 minutes and then pre-treated with protease inhibitor cocktail (Sigma cat#P8340), 1 mM ethylenediaminetetraacetic acid (EDTA), and 1 mM ethylene glycol tetraacetic acid (EGTA) to prevent non-specific interactions, stabilize the proteins, and disrupt the immune complexes.
Detection of anti-Tat Antibody
CSF sample was added, in duplicate at 100 μl/well and compared against normal CSF. After a 2-hour room temperature incubation, the plates were washed 3 times with washing buffer (0.1% v/v Tween-20 in PBS, pH 7.4). The plates were then incubated for 1 hour at room temperature with biotinylated anti-human antibodies (Chemicon cat#AP114B), diluted 1000-fold each in blocking buffer (1% w/v bovine serum albumin/0.1% v/v Tween-20 in phosphate buffered saline [PBS], pH 7.4). Wash steps were repeated, following which streptavidin-horse radish peroxidase (HRP), diluted 1000-fold in blocking buffer, was incubated on each plate for 1 hour at room temperature. The plates were washed again thereafter and analyzed using the SuperSignal Femto Sensitivity substrate (Pierce cat#37074). The luminescence was measured within 5 minutes at 425 nm on a microplate reader (SpectraMax, Molecular Devices).
Statistical Analysis
To determine relative levels of anti-Tat antibodies in individuals’ samples, the relative light units of HIV+ CSF samples were normalized against the RLU obtained from noninflammatory control CSF, used as a blank. Each plate had its own blank to account for plate-to-plate variability. “Undetectable” anti-Tat levels were defined as data points in the HIV positive groups that were less than the mean plus one standard deviation of the HIV negative controls. All data were analyzed using GraphPad Prism 5 by ANOVA using Newman-Keuls post-test comparison.
RESULTS
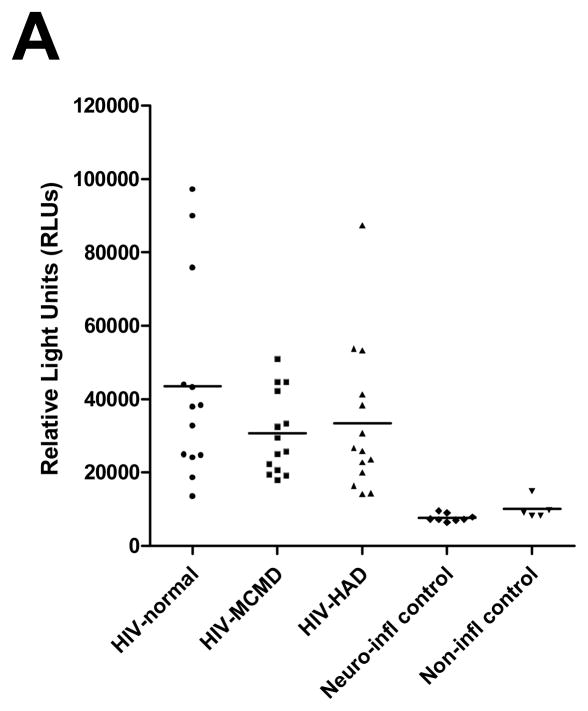
The biotin-avidin based chemiluminescent ELISA has enabled us to achieve excellent sensitivity and specificity, spanning a broad range of detection from 10,000 to over 100,000 RLUs for the anti-Tat antibodies in HIV-infected individuals (see figure 1).
Fig 1.
Relative Light Units of an ELISA for anti-Tat antibodies detected in spinal fluid of HIV-infected individuals without dementia (HIV-Normal) (MSK 0) (n=15; 86.7% > mean+1SD), with mild cognitive impairment (HIV-MCMD) (MSK 0.5–1) (n=20; 70% > mean+1SD), with moderate cognitive impairment (HIV-HAD) (MSK≥2) (n=17; 82.4% > mean+1SD), HIV negative controls (n=5), and neuro-inflammatory controls (n=8). Anti-Tat levels in spinal fluid of all HIV groups are significantly higher than in controls. The points in the figure represent individual patient data and lines represent the mean. Statistical analysis was by ANOVA, with Newman-Keuls post-test.
Detection of antibodies to Tat
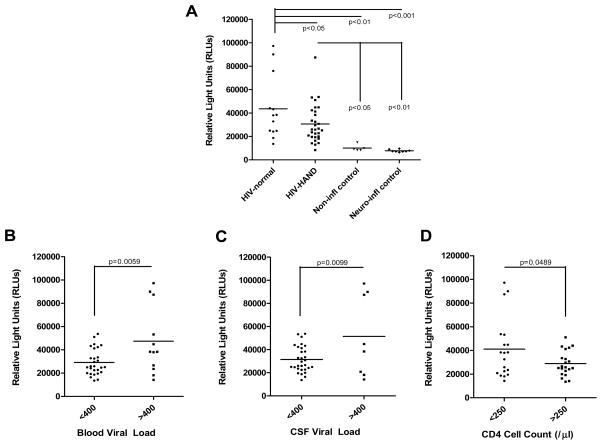
CSF anti-Tat antibody levels were significantly higher in HIV-infected individuals without HAND compared to individuals with HAND (figure 2a). Highest levels of antibodies were present in HIV-infected patients with normal cognition. 3/15 had levels >70,000 RLUs while none of the patients with mild impairment and only 1/37 with HAND had such high levels.
Fig 2.
Detection of Antibodies to Tat in the CSF of individuals infected with HIV: (A) Relative Light Units of an ELISA for anti-Tat antibodies detected in spinal fluid of HIV-infected individuals without dementia (HIV-Normal) (MSK 0) (n=15; 86.7%>mean+1SD), with HIV-associated neurocognitive disorder (HAND) (MSK≥0.5) (n=37; 83.8%>mean+1SD), HIV negative controls (n=5), and neuro-inflammatory controls (n=8). Anti-Tat levels in spinal fluid of the HIV-Normal group were significantly higher than in HIV-HAND (p<0.05). Antibody level was significantly higher in HIV-infected individuals without dementia than the HIV negative individuals (p<0.01) and the neuro-inflammatory control individuals (p<0.001). CSF anti-Tat levels are higher in individuals with higher serum and CSF viral loads and lower CD4 cell counts. (B) In the CSF of individuals with HIV (n=51), anti-Tat levels are significantly higher in the group with serum viral load >400 copies/ml (p<0.01). (C) In the CSF of individuals with HIV (n=47), anti-Tat levels are significantly higher in the group with CSF viral load >400 copies/ml (p<0.01). (D) In the CSF of individuals with HIV (n=51), anti-Tat levels are significantly higher in the group with CD4 cell level <250 cells/μl (p<0.05). In all panels, the points in the figure represent individual patient data and lines represent the mean. Statistical analysis was by ANOVA with Newman-Keuls post-test for (A) and by unpaired t-test for (B, C, D).
Next, we determined if CSF anti-Tat levels might depend on HIV RNA viral load in either serum (figure 2b) or CSF (figure 2c). Using a cutoff of 400 copies/ml, individuals with higher viral loads have significantly higher anti-Tat levels. Similarly, we hypothesized that CSF anti-Tat levels might vary with CD4 count. (Figure 2d) demonstrates that individuals with less than 250 CD4 lymphocytes/μl have significantly higher anti-Tat levels than those who are not as immunocompromised.
DISCUSSION
HIV Tat has been strongly implicated as a cause of neurotoxicity in individuals with HAND. We therefore hypothesized that levels of anti-Tat in the spinal fluid might have a relationship with presence of HAND. We have hypothesized that anti-Tat antibodies neutralize Tat function, so that patients with high antibody levels might have less severe dementia. The data in figure 2a supports this hypothesis, indicating that CSF levels of anti-Tat antibody are inversely correlated with HAND severity. These results are also consistent with the neuroprotective properties of this antibody seen in in vitro studies (Rumbaugh et al. 2012).
Our ability to develop and apply quantitative chemiluminescent indirect ELISAs depended on a number of variables. A chemiluminescent end-point has increased sensitivity compared to using a colorimetric end-point. Anti-Tat detection was further optimized by pre-treating the CSF to stabilize the free proteins. Future studies might further demonstrate the specificity of this assay through use of blocking antigen.
Antibodies are typically thought of as marking toxins, bacteria, or infected cells for destruction by effectors such as complement molecules or phagocytic cells. Antibodies have also been shown to neutralize these toxic or infectious processes by binding to antigenic determinants on the harmful agent, thereby hindering the interaction of the agent with its receptor. One of the major proposed mechanisms of Tat-mediated neurotoxicity is binding and stimulation of NMDA receptors by Tat, producing excitotoxicity (Haughey et al. 2001; Prendergast et al. 2002; Self et al. 2004). Perhaps, the neuroprotective ability of an anti-Tat antibody is dependent on its ability to interfere with Tat’s interaction with glial cells and Tat-mediated excitotoxicity.
HIV enters the brain within days to weeks of infection, establishes restricted infection in astrocytes and a productive infection in microglia/macrophages (Davis et al. 1992; Mankowski et al. 2002; Resnick et al. 1988). It may be years before individuals develop any dementing signs or symptoms, or they may never develop dementia at all (Davis et al. 1992; Mankowski et al. 2002; Resnick et al. 1988), suggesting a host susceptibility factor as a key determinant. At least partly, this may be due to the presence or absence of an effective anti-Tat immune response.
It may seem counterintuitive that neuroprotective anti-Tat antibodies are higher in patients with lower CD4 counts, which are often the same patients who have neurocognitive dysfunction. However, in our cohort, there was no correlation between CD4 count and neurocognitive status. Thus, the correlation between high anti-Tat and low CD4 count in this study may be taken to mean that even patients with a low CD4 count can, at least in some cases, mount a humoral response to Tat, which may, in fact, help to explain why, in this cohort, no correlation was seen between CD4 count and neurocognitive status. Antibody levels to Tat were also higher in individuals with higher viral load. This may indicate that active Tat production is necessary for driving the antibody response, and it is possible that the antibody response may be an indirect measure for Tat production, which has been technically challenging to measure at low concentrations.
Future work should include individuals screened at regular intervals in order to assess whether baseline CSF anti-Tat levels can predict subsequent development of HAND, or whether these levels vary significantly in a single individual over a longitudinal timeframe. Such work should also carefully scrutinize the HAART regimens of individuals to determine whether more or less CSF penetrating regimens correlate with higher or lower CSF anti-Tat levels. Such a longitudinal study could also assess whether changes in anti-Tat levels that may become evident over time, perhaps associated with changes in HAART regimen, can predict a better prognosis.
The ability to detect anti-Tat antibody levels in the CSF by a relatively easy ELISA technique as described here may also have important implications for therapeutic development to treat or prevent HAND. One possible treatment would be development of a vaccine strategy or perhaps the use of a therapeutic monoclonal antibody against Tat. Efficient development of such a therapy would require the ability to easily monitor anti-Tat antibodies in the CSF.
Acknowledgments
This research was funded by NIH grants to Drs. Sacktor, McArthur, Nath, and Rumbaugh, who report no other disclosures.
Footnotes
Ms. Bachani reports no disclosures.
References
- Davis LE, Hjelle BL, Miller VE, Palmer DL, Llewellyn AL, Merlin TL, Young SA, Mills RG, Wachsman W, Wiley CA. Early viral brain invasion in iatrogenic human immunodeficiency virus infection. Neurology. 1992;42:1736–1739. doi: 10.1212/wnl.42.9.1736. [DOI] [PubMed] [Google Scholar]
- Dore GJ, McDonald A, Li Y, Kaldor JM, Brew BJ National HIVSC . Marked improvement in survival following AIDS dementia complex in the era of highly active antiretroviral therapy. AIDS (London, England) 2003;17:1539–1545. doi: 10.1097/00002030-200307040-00015. [DOI] [PubMed] [Google Scholar]
- Gonzalez E, Rovin BH, Sen L, Cooke G, Dhanda R, Mummidi S, Kulkarni H, Bamshad MJ, Telles V, Anderson SA, Walter EA, Stephan KT, Deucher M, Mangano A, Bologna R, Ahuja SS, Dolan MJ, Ahuja SK. HIV-1 infection and AIDS dementia are influenced by a mutant MCP-1 allele linked to increased monocyte infiltration of tissues and MCP-1 levels. Proceedings of the National Academy of Sciences of the United States of America. 2002;99:13795–13800. doi: 10.1073/pnas.202357499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haughey NJ, Nath A, Mattson MP, Slevin JT, Geiger JD. HIV-1 Tat through phosphorylation of NMDA receptors potentiates glutamate excitotoxicity. Journal of neurochemistry. 2001;78:457–467. doi: 10.1046/j.1471-4159.2001.00396.x. [DOI] [PubMed] [Google Scholar]
- Hudson L, Liu J, Nath A, Jones M, Raghavan R, Narayan O, Male D, Everall I. Detection of the human immunodeficiency virus regulatory protein tat in CNS tissues. Journal of neurovirology. 2000;6:145–155. doi: 10.3109/13550280009013158. [DOI] [PubMed] [Google Scholar]
- Kruman II, Nath A, Maragos WF, Chan SL, Jones M, Rangnekar VM, Jakel RJ, Mattson MP. Evidence that Par-4 participates in the pathogenesis of HIV encephalitis. The American journal of pathology. 1999;155:39–46. doi: 10.1016/S0002-9440(10)65096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma M, Nath A. Molecular determinants for cellular uptake of Tat protein of human immunodeficiency virus type 1 in brain cells. J Virol. 1997;71:2495–2499. doi: 10.1128/jvi.71.3.2495-2499.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mankowski JL, Clements JE, Zink MC. Searching for clues: tracking the pathogenesis of human immunodeficiency virus central nervous system disease by use of an accelerated, consistent simian immunodeficiency virus macaque model. The Journal of infectious diseases. 2002;186(Suppl 2):S199–208. doi: 10.1086/344938. [DOI] [PubMed] [Google Scholar]
- McArthur JC, McDermott MP, McClernon D, St Hillaire C, Conant K, Marder K, Schifitto G, Selnes OA, Sacktor N, Stern Y, Albert SM, Kieburtz K, deMarcaida JA, Cohen B, Epstein LG. Attenuated central nervous system infection in advanced HIV/AIDS with combination antiretroviral therapy. Arch Neurol. 2004;61:1687–96. doi: 10.1001/archneur.61.11.1687. [DOI] [PubMed] [Google Scholar]
- Neuenburg JK, Brodt HR, Herndier BG, Bickel M, Bacchetti P, Price RW, Grant RM, Schlote W. HIV-related neuropathology, 1985 to 1999: rising prevalence of HIV encephalopathy in the era of highly active antiretroviral therapy. Journal of acquired immune deficiency syndromes (1999) 2002;31:171–177. doi: 10.1097/00126334-200210010-00007. [DOI] [PubMed] [Google Scholar]
- Prendergast MA, Rogers DT, Mulholland PJ, Littleton JM, Wilkins LH, Jr, Self RL, Nath A. Neurotoxic effects of the human immunodeficiency virus type-1 transcription factor Tat require function of a polyamine sensitive-site on the N-methyl-D-aspartate receptor. Brain research. 2002;954:300–307. doi: 10.1016/s0006-8993(02)03360-7. [DOI] [PubMed] [Google Scholar]
- Quasney MW, Zhang Q, Sargent S, Mynatt M, Glass J, McArthur J. Increased frequency of the tumor necrosis factor-alpha-308 A allele in adults with human immunodeficiency virus dementia. Annals of Neurology. 2001;50:157–162. [PubMed] [Google Scholar]
- Resnick L, Berger JR, Shapshak P, Tourtellotte WW. Early penetration of the blood-brain-barrier by HIV. Neurology. 1988;38:9–14. doi: 10.1212/wnl.38.1.9. [DOI] [PubMed] [Google Scholar]
- Rumbaugh JA, Bachani M, Li W, Butler TR, Smith KJ, Bianchet MA, Wang T, Prendergast MA, Sacktor N, Nath A. HIV immune complexes prevent excitotoxicity by interaction with NMDA receptors. Neurobiol Dis. 2012 doi: 10.1016/j.nbd.2012.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumbaugh JA, Nath A. Developments in HIV neuropathogenesis. Curr Pharm Des. 2006;12:1023–44. doi: 10.2174/138161206776055877. [DOI] [PubMed] [Google Scholar]
- Sacktor N. The epidemiology of human immunodeficiency virus-associated neurological disease in the era of highly active antiretroviral therapy. Journal of neurovirology. 2002;8(Suppl 2):115–121. doi: 10.1080/13550280290101094. [DOI] [PubMed] [Google Scholar]
- Sacktor N, Lyles RH, Skolasky R, Kleeberger C, Selnes OA, Miller EN, Becker JT, Cohen B, McArthur JC, Multicenter ACS. HIV-associated neurologic disease incidence changes:: Multicenter AIDS Cohort Study, 1990–1998. Neurology. 2001;56:257–260. doi: 10.1212/wnl.56.2.257. [DOI] [PubMed] [Google Scholar]
- Sacktor N, McDermott MP, Marder K, Schifitto G, Selnes OA, McArthur JC, Stern Y, Albert S, Palumbo D, Kieburtz K, De Marcaida JA, Cohen B, Epstein L. HIV-associated cognitive impairment before and after the advent of combination therapy. Journal of neurovirology. 2002;8:136–142. doi: 10.1080/13550280290049615. [DOI] [PubMed] [Google Scholar]
- Self RL, Mulholland PJ, Nath A, Harris BR, Prendergast MA. The human immunodeficiency virus type-1 transcription factor Tat produces elevations in intracellular Ca2+ that require function of an N-methyl-D-aspartate receptor polyamine-sensitive site. Brain research. 2004;995:39–45. doi: 10.1016/j.brainres.2003.09.052. [DOI] [PubMed] [Google Scholar]
- Simpson DM, McArthur JC, Olney R, Clifford D, So Y, Ross D, Baird BJ, Barrett P, Hammer AE. Lamotrigine for HIV-associated painful sensory neuropathies: a placebo-controlled trial. Neurology. 2003;60:1508–14. doi: 10.1212/01.wnl.0000063304.88470.d9. [DOI] [PubMed] [Google Scholar]
- Tornatore C, Chandra R, Berger JR, Major EO. HIV-1 infection of subcortical astrocytes in the pediatric central nervous system. Neurology. 1994a;44:481–487. doi: 10.1212/wnl.44.3_part_1.481. [DOI] [PubMed] [Google Scholar]
- Tornatore C, Meyers K, Atwood W, Conant K, Major E. Temporal patterns of human immunodeficiency virus type 1 transcripts in human fetal astrocytes. Journal of virology. 1994b;68:93–102. doi: 10.1128/jvi.68.1.93-102.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trujillo JR, Navia BA, Worth J, Lucey DR, McLane MF, Lee TH, Essex M. High levels of anti-HIV-1 envelope antibodies in cerebrospinal fluid as compared to serum from patients with AIDS dementia complex. J Acquir Immune Defic Syndr Hum Retrovirol. 1996;12:19–25. doi: 10.1097/00042560-199605010-00003. [DOI] [PubMed] [Google Scholar]
- Turchan J, Anderson C, Hauser KF, Sun Q, Zhang J, Liu Y, Wise PM, Kruman I, Maragos W, Mattson MP, Booze R, Nath A. Estrogen protects against the synergistic toxicity by HIV proteins, methamphetamine and cocaine. BMC Neurosci. 2001;2:3. doi: 10.1186/1471-2202-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westendorp MO, Frank R, Ochsenbauer C, Stricker K, Dhein J, Walczak H, Debatin KM, Krammer PH. Sensitization of T cells to CD95-mediated apoptosis by HIV-1 Tat and gp120. Nature. 1995;375:497–500. doi: 10.1038/375497a0. [DOI] [PubMed] [Google Scholar]
- Wiley CA, Baldwin M, Achim CL. Expression of HIV regulatory and structural mRNA in the central nervous system. AIDS (London, England) 1996;10:843–847. doi: 10.1097/00002030-199607000-00007. [DOI] [PubMed] [Google Scholar]