Abstract
Background and Purpose
Current literature provides mixed evidence on disparities by race/ethnicity and socioeconomic status (SES) in discharge outcomes following hospitalization for acute ischemic stroke. Using comprehensive data from eight states, we sought to compare inpatient mortality and length of stay (LOS) by race/ethnicity and SES.
Methods
We examined all 2007 hospitalizations for acute ischemic stroke in all non-Federal acute care hospitals in AZ, CA, FL, MA, NJ, NY, PA and TX. Population was stratified by race/ethnicity (non-Hispanic Whites, non-Hispanic Blacks and Hispanics) and SES, measured by median income of patient zip code. For each stratum we estimated risk-adjusted rates of inpatient mortality and longer LOS (> median LOS). We also compared the hospitals where these subpopulations received care.
Results
Hispanic and Black patients accounted for 14 and 12 percent of all ischemic stroke admissions (N=147,780) respectively and had lower crude inpatient mortality rates (Hispanic=4.5%, Blacks=4.4%; all p-values < 0.001) compared to White patients (5.8%). Hispanic and Black patients were younger and fewer had any form of atrial fibrillation. Adjusted for patient risk, inpatient mortality was similar by race/ethnicity, but was significantly higher for low area-income patients than that for high area-income patients (Odds Ratio=1.08, 95% confidence interval=[1.02, 1.15]). Risk-adjusted rates of longer LOS were higher among minority and low area-income populations.
Conclusions
Risk adjusted inpatient mortality was similar among patients by race/ethnicity but higher among patients from lower income areas. However, this pattern was not evident in sensitivity analyses including the use of mechanical ventilation as a partial surrogate for stroke severity.
Keywords: ischemic stroke, inpatient mortality, length of stay, race, ethnicity, socioeconomic status, risk factors
Although key to understanding the long-standing racial/ethnic disparities in stroke mortality rates, evidence on differences in case fatality following stroke has remained mixed.1, 2 Death certificate data have long indicated that the national death rate from stroke is higher (+48% in 2007) among non-Hispanic Blacks (henceforth referred to as Blacks) and lower (−20% in 2007) among Hispanics than among non-Hispanic Whites (henceforth referred to as Whites).3 Higher stroke mortality can arise from higher incidence or higher case fatality or both.4, 5 Findings from several well-known epidemiologic studies over the last two decades have uniformly indicated that stroke incidence rate is higher among Blacks and Hispanics compared to Whites5–11; however, the magnitude of disparity in stroke incidence is much smaller than that in stroke mortality.4, 5 While this would suggest higher case fatality rates among Blacks compared to Whites, prior studies have been largely inconclusive with studies finding higher, similar or lower case fatality among Blacks compared to Whites across different study populations.4–8, 10, 12–15 Evidence on differences between Hispanics and Whites is also mixed.12, 16 In the absence of a population-representative data source that is both national in scope and has sizable number of minority patients, these differing findings could plausibly be reflective of regional differences, unrepresentative convenience patient cohorts or inadequate sample size, thereby limiting comparability and generalizability.4 Of particular importance is the need to accurately capture low income cohorts in the study population; due to higher incidence of low incomes among racial and ethnic minorities, they may be underrepresented in survey-based population studies.4
With a view to capture a broader national population including larger numbers of minority populations, we pooled administrative data all ischemic stroke discharges from eight states which together accounted for 73% of national Hispanic and 37% of national Black populations. We examined inpatient mortality as the indicator of case fatality; in addition, length of stay (LOS) was also examined as a secondary patient outcome measure.12, 13 We compared outcomes by race/ethnicity and SES. We examined for systematic differences in the type of hospitals where minority and low area-income patients received care.
METHODS
Data Sources
The primary data sources were the state-level inpatient discharge databases (2007) from Arizona, California, Florida, Massachusetts, New Jersey, New York, Pennsylvania and Texas. These cover the universe of all admissions to all non-Federal acute care hospitals.17 These states were selected based on their sizable minority population and completeness of race and ethnicity data; the proportion of acute ischemic stroke admissions with patient race or ethnicity missing (or coded as unknown) was 2.8% and ranged from 0.3% (Texas) to 7.6% (New York). In addition, we obtained zip code-level data on median household income from the 2000 Census.18 We obtained data on hospital characteristics from the American Hospital Association Annual Survey (2007).19
Study Population
To identify acute ischemic stroke admissions for adults aged 18 and older, we followed other recent studies by including admissions with the principal discharge code (ICD-9-CM) of 433.x1, 434.x1 and 436.12, 13 To minimize confounding from scheduled admissions for discretionary treatment (for instance, carotid endarterectomy), we only considered inpatient admissions arising either from admission to the Emergency Department or transfer from another acute care facility. To avoid two admissions being associated with the same outcome, we excluded hospitalizations that resulted in transfer to another acute care hospital. For comparability of patient outcomes by subpopulations, especially by SES, we included admissions of patients who were state residents. From the resulting cohort, we excluded 4.9% admissions with missing key measures; compared with the included cohort, patients in this 4.9% excluded cohort were broadly similar (see Appendix).
Measures
The primary outcome measures were inpatient death and length of stay (LOS) of the index hospitalization for acute ischemic stroke. We examined LOS as a dichotomous measure indicating longer LOS (i.e., 1 = LOS > median LOS) as it is more robust to outliers and skewed distribution.12 Patient risk factors were characterized by comorbid conditions captured by the secondary discharge diagnosis codes (ICD-9-CM).13, 20 We identified patients with the following comorbid conditions: atrial fibrillation, coronary heart disease, congestive heart failure, diabetes and hypertension.21 Indications for other comorbid conditions were collectively grouped using the Charlson comorbidity index.22 Discharge data from all states included separate indicators of race and ethnicity, which were together used to uniformly define four population cohorts: Hispanics, non-Hispanic Whites, non-Hispanic Blacks and Others; the Others included those with missing race or ethnicity.23 Given the absence of individual measures of SES, we followed prior research and used the Census-based median zip code income, matched with patient residence zip code, to stratify patients from each state into three groups based on population quartiles24, 25: lowest quartile zip codes (“low area-income”), second lowest quartile (“medium”) and top two quartiles (“high”).25 Based on prior research on the role of hospital characteristics, we examined several structural measures: number of inpatient beds, number of intensive care unit (ICU) beds, nursing staff (# patients per nurse), mean daily Emergency Department (ED) admission volume, ownership, teaching status and safety-net status (defined as >20 percent of discharges from the hospital covered by Medicaid).26
Estimation
The unit of all analyses was the index patient admission for acute ischemic stroke. We performed bivariate comparisons of patient and hospital characteristics by race/ethnicity and SES. We obtained two sets of risk-adjusted estimates of differences in the outcomes across population subgroups stratified by race/ethnicity and SES; in the first, we adjusted for patient risk factors, and in the second we also adjust for hospital characteristics.12 Each was estimated by hierarchical logistic regression to adjust for clustering within hospitals. We estimated these models for all patients and for subgroups formed by the interaction of race/ethnicity and SES. Standard errors and confidence intervals were estimated to account for heterogeneity across subpopulations. Statistical significance was defined as p-value ≤ 0.05.
Across patient risk factors, we found relatively larger differences in age and co-morbidity of atrial fibrillation between Whites and minorities. To assess their relative impact on outcomes, we estimated racial/ethnic differences in outcome rates adjusted for only these two factors. Sensitivity Analyses: Ideally, we would have liked to adjust for initial stroke severity. In the absence of available data on stroke severity, we performed a post-hoc sensitivity analysis adjusted instead for the use of mechanical ventilation, which has been previously shown to be a valid proxy for stroke severity.27 In addition, we also examined if LOS differences by cohorts were associated with inpatient mortality rate differences; for this we re-estimated the LOS regression model including inpatient mortality as a covariate. Due to space limitation, additional findings are reported in an Appendix. All the statistical analyses were performed using Stata Version 12.1. This study was approved by the Boston University Institutional Review Board.
RESULTS
We identified 147,780 hospitalizations for acute ischemic stroke during 2007 in the eight states. Their distribution by race and ethnicity was: Whites =67%, Blacks =14%, Hispanics=11% and Others=8% (Table 1).
Table 1. Patient Risk Factors, Hospital Characteristics and Patient Outcomes by Race/Ethnicity & Socioeconomic Status, 2007.
All acute ischemic discharges for patients aged 18+ in all non-federal hospitals in AZ, CA, FL, MA, NJ, NY, PA and TX
| All | Race/Ethnicity | Socioeconomic Status | |||||
|---|---|---|---|---|---|---|---|
| Whites | Blacks | Hispanics | Low Income |
Medium Income |
High Income |
||
| # admissions | 147,780 | 98,512 | 20,579 | 16,927 | 40,233 | 38,579 | 68,968 |
| Patient Risk Factors | |||||||
| Female% | 53.7 | 54.1 | 56.4 | 50.2 | 53.7 | 53.9 | 53.4 |
| Age (years), % | |||||||
| 18–64 | 29.4 | 23.1 | 47.5 | 39.9 | 34.8 | 28.8 | 26.4 |
| 65–74 | 20.7 | 19.4 | 23.8 | 22.9 | 21.9 | 20.7 | 20.1 |
| 75–84 | 29.8 | 33.0 | 19.4 | 25.0 | 26.8 | 30.3 | 31.2 |
| 85+ | 20.2 | 24.5 | 9.2 | 12.2 | 16.5 | 20.1 | 22.3 |
| Comorbidity, Prevalence, % | |||||||
| Atrial fibrillation | 23.2 | 27.2 | 12.3 | 15.4 | 19.7 | 22.9 | 25.3 |
| Hypertension | 77.6 | 75.0 | 85.6 | 80.8 | 79.2 | 77.5 | 76.7 |
| Diabetes | 34.2 | 28.9 | 44.4 | 49.2 | 39.0 | 34.5 | 31.2 |
| Coronary Heart Disease | 27.5 | 29.7 | 21.6 | 24.4 | 26.8 | 28.2 | 27.5 |
| Congestive Heart Failure | 13.7 | 14.2 | 14.8 | 11.8 | 14.1 | 13.8 | 13.5 |
| Charlson Score | |||||||
| 0 | 47.8 | 47.7 | 46.2 | 48.7 | 46.6 | 47.5 | 48.7 |
| 1 | 14.6 | 15.7 | 12.8 | 12.8 | 14.6 | 15.0 | 14.4 |
| 2 | 24.1 | 23.0 | 26.9 | 26.3 | 25.0 | 24.0 | 23.7 |
| 3+ | 13.4 | 13.6 | 14.1 | 12.1 | 13.8 | 13.6 | 13.1 |
| Socioeconomic Status (patient residence zip code), % | |||||||
| Low Income Area | 27.2 | 19.6 | 50.8 | 43.7 | |||
| Medium Income Area | 26.1 | 27.5 | 21.5 | 24.5 | |||
| High Income Area | 46.7 | 52.9 | 27.7 | 31.8 | |||
| Race and Ethnicity, % | |||||||
| Whites, non-Hispanic | 48.0 | 70.2 | 75.6 | ||||
| Blacks, non-Hispanic | 26.0 | 11.5 | 8.3 | ||||
| Hispanic | 18.4 | 10.7 | 7.8 | ||||
| Hospital Characteristics | |||||||
| # hospitals | 1,282 | 1,248 | 954 | 892 | 1,076 | 1,160 | 1,089 |
| Bed size (# inpatient beds), % | |||||||
| <= 199 | 75.2 | 78.0 | 72.6 | 63.7 | 23.3 | 28.8 | 22.2 |
| 200 to 499 | 15.0 | 14.1 | 13.6 | 23.1 | 48.6 | 50.7 | 52.9 |
| >= 500 | 9.8 | 7.9 | 13.8 | 13.2 | 28.1 | 20.5 | 24.9 |
| ICU beds, % | |||||||
| <= 14 | 24.2 | 26.3 | 16.5 | 23.1 | 29.6 | 34.0 | 28.1 |
| 15 to 36 | 51.2 | 52.0 | 47.9 | 50.9 | 33.1 | 36.5 | 40.9 |
| >= 37 | 24.7 | 21.8 | 35.5 | 26.0 | 37.3 | 29.6 | 31.0 |
| Nursing staff (# patients/nurse), % | |||||||
| <= 2 | 36.6 | 35.8 | 37.5 | 40.1 | 34.7 | 33.4 | 39.6 |
| 2.01 to 3.00 | 36.4 | 35.7 | 36.4 | 39.4 | 37.3 | 36.8 | 35.5 |
| 3.01 to 4.00 | 18.5 | 19.3 | 17.6 | 15.4 | 18.8 | 19.7 | 17.6 |
| > 4.00 | 8.5 | 9.2 | 8.5 | 5.1 | 9.2 | 10.1 | 7.3 |
| Average daily ED volume (# admissions), % | |||||||
| <= 80 | 24.2 | 25.4 | 18.8 | 24.2 | 25.2 | 27.9 | 21.5 |
| 81 to 175 | 45.9 | 47.2 | 40.1 | 44.4 | 41.6 | 44.2 | 49.4 |
| >= 176 | 29.9 | 27.4 | 41.1 | 31.4 | 33.1 | 27.9 | 29.1 |
| Ownership, % | |||||||
| Non Profit | 75.2 | 78.0 | 72.6 | 63.7 | 71.9 | 73.3 | 78.1 |
| For Profit | 15.0 | 14.1 | 13.6 | 23.1 | 16.6 | 16.1 | 13.5 |
| Government, non-Federal | 9.8 | 7.9 | 13.8 | 13.2 | 11.5 | 10.7 | 8.3 |
| Teaching hospital, % | 21.8 | 18.8 | 34.9 | 19.4 | 26.9 | 18.8 | 20.5 |
| Safety Net hospital, % | 30.6 | 24.7 | 41.4 | 45.2 | 44.1 | 30.9 | 22.6 |
| Patient Outcomes | |||||||
| Inpatient Mortality (%) | 5.5 | 5.8 | 4.4 | 4.5 | 5.5 | 5.4 | 5.6 |
| Length of stay | |||||||
| Days, Mean | 6.2 | 5.9 | 7.4 | 6.3 | 6.7 | 6.0 | 6.0 |
| Frequency of stays > 4 days, % | 48.3 | 46.6 | 55.2 | 48.5 | 51.2 | 47.4 | 47.0 |
Notes:
Of the 147,780 discharges, 11,762 were for "Other" race and ethnicity. Due to heterogeneity of this cohort, characteristics are not reported here. However, the “Other” cohort was included in all the statistical analyses.
Charlson Score excludes congestive heart failure, cerebrovascular and diabetes as these are individually specified
p-value is for the test of comparison across race and ethnicity
Patient Risk Factors by Race/Ethnicity & SES
Comparing Whites vs. minorities, we found relatively larger differences in age and prevalence of atrial fibrillation (Table 1). While 58% of Whites were ≥75 years, this proportion was 29% and 37% for Blacks and Hispanics respectively (p<0.001). Among individuals aged 18–64 years, Whites comprised 23% of all admissions, compared to 48% and 40% among Blacks and Hispanics respectively. Prevalence of atrial fibrillation was significantly higher among Whites (27%) than Blacks (12%) and Hispanics (15%; p<0.001). This pattern in the two factors was persistent in every state (Figure 1). Patients also exhibited considerable differences by SES (Table 1). Low income area patients were more often younger and had a higher prevalence of hypertension, diabetes and congestive heart failure, but lower prevalence of atrial fibrillation and coronary heart disease.
Figure 1.
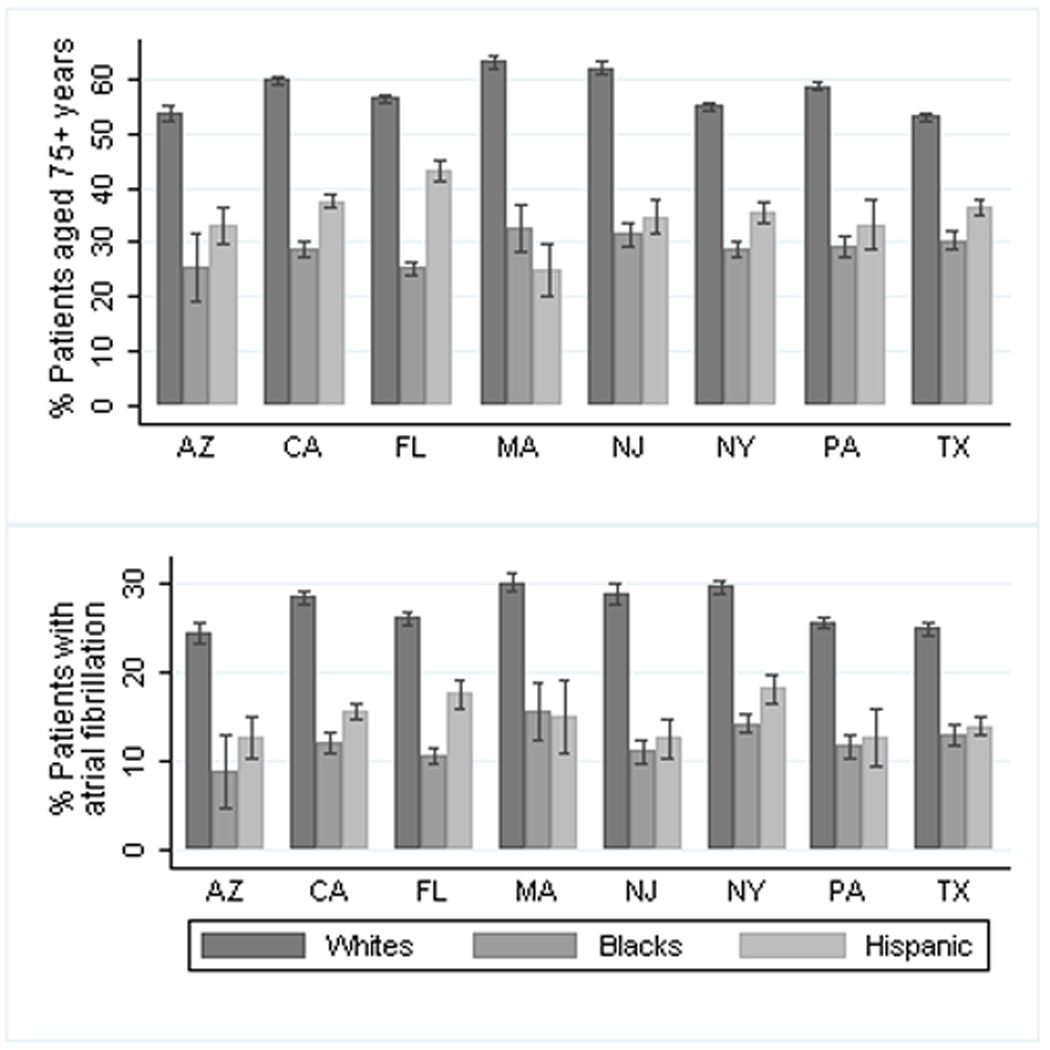
Prevalence of Older Age and Atrial Fibrillation by Race & Ethnicity, 2007
Note: Reported figures are average prevalence rates (%) and 95% confidence intervals.
Hospital Characteristics
Systematic differences were also found in the hospitals where Whites and minorities received care (Table 1). Out of the 1,282 hospitals with acute ischemic stroke admissions in the eight states, all admissions for Blacks and Hispanics occurred in 954 and 892 hospitals respectively. In terms of hospital size, Blacks and low income-area patients more frequently received care in teaching and safety-net hospitals and hospitals with higher bed size, more ICU beds and ED volume, compared to Whites and Hispanics.
Differences in Inpatient Mortality Rate
The overall average crude inpatient mortality rate was 5.5%; it was significantly lower for Blacks (OR=0.75; 95%CI=[0.70, 0.80]) and Hispanics (OR=0.76; 95%CI=[0.70, 0.82]) than for Whites (Tables 1 and 2). The hierarchical logistic regression model to adjust for patient risk factors indicated very good discrimination (c-statistic=0.74); it also indicates that only a small share (3.0%) of the residual inpatient mortality differences across patients were associated with the hospital where patients were treated (see Appendix). Adjusting for patient risk factors, inpatient mortality rates for Blacks (OR=1.02, 95%CI=[0.94, 1.10]) and Hispanics (OR=0.98, 95%CI=[0.91, 1.07]) were similar to that for Whites. In assessing the impact of different risk factors in mitigating observed differences in inpatient mortality, we note that Whites have higher prevalence of older age, atrial fibrillation, coronary heart disease and congestive heart failure; in addition, hypertension and diabetes - conditions for which prevalence was higher among minorities - were either protective or equivocal of inpatient mortality risk.
Table 2. Unadjusted and Adjusted Inpatient Mortality Rates by Race/Ethnicity and Socioeconomic Status.
| Race/Ethnicity or SES Stratum |
N | Observed Inpatient Mortality, % |
Relative Inpatient Mortality Rates | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted for Patient Characteristics |
Adjusted for Patient and Hospital Characteristics |
|||||||||
| Odds Ratio | 95% Conf. Int |
Odds Ratio | 95% Conf. Int |
Odds Ratio | 95% Conf. Int |
||||||
| Low | High | Low | High | Low | High | ||||||
| Race/Ethnicity | |||||||||||
| White | 98,512 | 5.8 | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | |||
| Black | 20,579 | 4.4 | 0.75 | 0.70 | 0.80 | 1.02 | 0.94 | 1.1 | 0.96 | 0.89 | 1.04 |
| Hispanic | 16,927 | 4.5 | 0.76 | 0.70 | 0.82 | 0.98 | 0.91 | 1.07 | 0.97 | 0.89 | 1.06 |
| Socioeconomic Status | |||||||||||
| Low Income | 40,233 | 5.5 | 0.99 | 0.93 | 1.04 | 1.08 | 1.02 | 1.15 | 1.06 | 1.00 | 1.13 |
| Med. Income | 38,579 | 5.4 | 0.97 | 0.92 | 1.02 | 1.00 | 0.94 | 1.06 | 0.99 | 0.93 | 1.06 |
| High Income | 68,968 | 5.6 | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | |||
Notes:
Adjusted mortality rates obtained by hierarchical logistic regression of inpatient mortality on patient factors (age, sex and comorbidities) and hospital characteristics (nursing staff, ICU beds, teaching status and safety net hospital indicator). In addition indicators of cohorts compared (race/ethnicity or SES) were included. Separate regression models were estimated for each population stratum examined. Indicator for state was included in all regressions.
We also performed comparisons by race/ethnicity separately among patients stratified by SES. Across all three SES cohorts, crude inpatient mortality rates were significantly lower for Blacks and Hispanics relative to that for Whites (see Appendix). However, adjusted inpatient mortality was generally similar by race/ethnicity among all SES strata; one exception was medium area income Hispanics who had significantly lower mortality (OR=0.80, 95%CI=[0.67, 0.96]) relative to Whites. We repeated this comparison analysis separately for each of the eight states and found similarity in risk-adjusted inpatient mortality rates among Blacks in all states and among Hispanics in seven states; however, due to smaller cohort sizes, precision of estimates was lower (see Appendix).
Similar comparison by SES indicated a converse pattern; while crude inpatient mortality rates were similar by SES cohorts, adjusted rate was higher among low area-income patients (OR=1.08, 95%CI=[1.02, 1.15]) when compared to high area-income patients (Table 2). A similar pattern of higher adjusted inpatient mortality for low area-income patients was found among Whites, Blacks and Hispanics, although statistical significance was present only for Whites, the largest cohort.
The hierarchical logistic regression model to adjust for hospital structural factors and patient risk factors indicated similar discrimination (c-statistic=0.74) compared to the model adjusting for patient factors. Further, additional adjustment for hospital factors had little impact on the relative differences in inpatient mortality compared to those obtained by adjusting only for patient risk factors.
Differences in Length of Stay
While overall mean LOS was 6.2 days, differences by race/ethnicity were significant: Whites=5.9, Blacks=7.4 and Hispanics=6.3 (p=0.003; Table 1). Correspondingly, rate of longer LOS (LOS > 4 days, the median LOS) was significantly higher among Blacks (OR=1.41, 95%CI=[1.37, 1.46]) and Hispanics (OR=1.08, 95%CI=[1.04, 1.11]) compared to Whites (Table 3). The regression model to adjust for patient risk factor indicated good discrimination (c-statistic=0.70; see Appendix). Adjusting for patient risk factors, the relative rate of longer LOS remained higher among Blacks (OR=1.36, 95%CI=[1.31, 1.41]) and Hispanics (OR=1.19, 95%CI=[1.14, 1.24]). This pattern of higher rate of longer stays among minorities was persistent among subpopulations stratified by SES. Further, comparison among all patients of rates of longer LOS indicated higher crude and adjusted rates of longer stay among low SES patients (OR=1.15, 95%CI=[1.12, 1.19]) than among high SES patients; this pattern was persistent separately among Whites, Blacks and Hispanics (see Appendix). Further adjustment to also account for differences in hospital characteristics, using hierarchical logistic regression model, indicated little change in the relative rates of longer stay by race/ethnicity and SES. Sensitivity analyses indicated that aforementioned cohort differences in LOS were not associated with differences in inpatient mortality.
Table 3. Unadjusted and Adjusted Rate of Longer Length of Stay (>4 days) by Race/Ethnicity and Socioeconomic Status.
| Race/Ethnicity or SES Stratum |
N | Observed Rate of Longer Stays, % |
Relative Rates of Longer Stays | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted for Patient Characteristics |
Adjusted for Patient and Hospital Characteristics |
|||||||||
| Odds Ratio | 95% Conf. Int |
Odds Ratio | 95% Conf. Int |
Odds Ratio | 95% Conf. Int |
||||||
| Low | High | Low | High | Low | High | ||||||
| Race/Ethnicity | |||||||||||
| White | 98,512 | 46.6 | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | |||
| Black | 20,579 | 55.2 | 1.41 | 1.37 | 1.46 | 1.36 | 1.31 | 1.41 | 1.35 | 1.30 | 1.40 |
| Hispanic | 16,927 | 48.5 | 1.08 | 1.04 | 1.11 | 1.19 | 1.14 | 1.24 | 1.18 | 1.13 | 1.23 |
| Socioeconomic Status | |||||||||||
| Low Income | 40,233 | 51.2 | 1.18 | 1.16 | 1.21 | 1.15 | 1.12 | 1.19 | 1.15 | 1.11 | 1.19 |
| Med. Income | 38,579 | 47.4 | 1.02 | 0.99 | 1.04 | 1.05 | 1.02 | 1.08 | 1.05 | 1.02 | 1.09 |
| High Income | 68,968 | 47.0 | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | |||
Notes:
Adjusted mortality rates obtained by hierarchical logistic regression of inpatient mortality on patient factors (age, sex and comorbidities) and hospital characteristics (nursing staff, ICU beds, ownership type, teaching status and safety net status). Indicator for state was included in both regressions.
Role of Older Age and Atrial Fibrillation
In mitigating the observed differences in inpatient mortality, we evaluated the relative role of the two risk factors – older age and presence of atrial fibrillation – whose prevalence was markedly lower among Blacks and Hispanics, compared to Whites (Table 4). Re-estimating the regression, with adjustment made only for these two patient factors, we found similar inpatient mortality by race/ethnicity. In contrast, a converse specification with adjustment made for all patient factors excluding age and presence of atrial fibrillation indicated persistence of lower inpatient mortality among Blacks (OR=0.76, 95%CI=[0.71, 0.83]) and Hispanics (OR=0.83, 95%CI=[0.78, 0.91]; Table 4).
Table 4. Relative Contribution of Risk Factors in Model Prediction of Inpatient Mortality & Length of Stay>4 days.
| Patient Cohort | Odds Ratio (OR) | |||||
|---|---|---|---|---|---|---|
| Model 1 Unadjusted |
Model 2 Adjusted for state residence |
Model 3 Adjusted for patient age and state residence |
Model 4 Adjusted for patient age, atrial fibrillation and state residence |
Model 5 Adjusted for all patient risk factors and state residence |
Model 6 Adjusted for all risk factors excluding patient age and atrial fibrillation |
|
| Inpatient Mortality | ||||||
| White | Reference | Reference | Reference | Reference | Reference | Reference |
| Black | 0.75*** | 0.74*** | 0.94 | 1.02 | 0.98 | 0.76*** |
| Hispanic | 0.76*** | 0.74*** | 0.89** | 0.95 | 0.98 | 0.83*** |
| Length of Stay > 4 days | ||||||
| White | Reference | Reference | Reference | Reference | Reference | Reference |
| Black | 1.41*** | 1.32*** | 1.44*** | 1.52*** | 1.43*** | 1.30*** |
| Hispanic | 1.08*** | 1.18*** | 1.25*** | 1.31*** | 1.29*** | 1.21*** |
Notes:
***, p < 0.001; **, p < 0.01; and * p < 0.05
Models 2 and 4 are based on logistic regressions and models 5 and 6 are based on hierarchical logistic regressions (with hospital level clustering).
Sensitivity Analyses
When added to the model, use of mechanical ventilation was highly correlated with inpatient death (OR=28.9, 95% CI = [27.1, 30.9]; see Appendix). The pattern of disparities in adjusted inpatient mortality rates was different from that without including use of mechanical ventilation: adjusted inpatient mortality rates are significantly lower for Blacks and Hispanics (compared to Whites) but similar for lower area-income patients (compared to high area-income patients).
DISCUSSION
Comparing patient outcomes from acute ischemic stroke by race/ethnicity and SES, this study indicates that, after adjusting for patient risk factors: (a) inpatient mortality rates are similar among Whites, Blacks and Hispanics, but 8% higher among low area-income patients compared to high area-income patients and (b) rates of LOS > 4 days are higher among Blacks (+36%) and Hispanics (+19%) compared to Whites, and among low area-income patients (+15%) compared to high area-income patients. Minorities and lower area-income patients more frequently received care at hospitals with larger bed capacity and patient volumes, as well as those with teaching and safety-net status. However, differences in hospital setting were not associated with differences in patient outcomes by race/ethnicity or SES.
Compared to Whites, while observed inpatient mortality rates were 27% and 25% lower among Blacks and Hispanics, respectively, they were almost completely mitigated after adjusting for patient risk factors. Among the risk factors that differed between Whites and minorities, most significant were older age and atrial fibrillation, both of which were markedly less prevalent among Blacks and Hispanics. We found that adjusting only for age and atrial fibrillation contributed to most of the mitigation of differences in inpatient mortality by race/ethnicity.
Our findings of lower observed inpatient mortality rates among Blacks are qualitatively similar to previously reported differences in stroke subtypes among Blacks and Whites.14, 28 One recent study, based on brain imaging, found fewer cardio-embolic strokes and fewer strokes from large vessel atherosclerosis among Blacks compared to Whites.28 As in our study, Blacks were younger and had a higher prevalence of hypertension and diabetes and a lower prevalence of atrial fibrillation, which lends support to the etiologic subtype of small vessel disease.5, 14, 29
Comparisons performed for subpopulations stratified by SES produced the same pattern of racial and ethnic differences in observed inpatient mortality rates which were nearly completely mitigated after adjustment for patient risk factors (except for medium area-income Hispanics). Our findings of higher rates of LOS > 4 days among Blacks and Hispanics, relative to Whites, are consistent with previous findings.12, 13
In contrasting our findings with those from previous studies we distinguish studies based on population-representative data sources (for instance, administrative data) from those based on convenience data (for instance, registry of voluntarily participating providers). Evidence from the former data source type indicates mixed patterns of similar30 or lower13, 30, 31 inpatient mortality among minorities. Of particular relevance are studies that examined administrative data from some of the same states as in this study.13, 30 Using administrative data from New York (2005–06), a recent study found lower risk-adjusted inpatient mortality among Blacks (OR=0.77, 95%CI=[0.61, 0.98]) compared to Whites.13 This contrasts with the finding of similar mortality among Blacks (OR=1.0, 95%=[0.87, 1.17]) for the NY patient subgroup in our study; this may be due to differences in study design and methods. Specifically, that study excluded 39% admissions from 57% hospitals based on rural hospital location or low hospital volume (<10) of black and white stroke patients; in contrast, no such exclusions are made in the current study since our interest is in epidemiologic outcome differences regardless of the hospital setting where care was received. Evidence using convenience data on disparities in outcomes is also mixed.12, 14, 32 Based on data from a large national registry of 1,181 hospitals, a recent study found lower inpatient mortality among Blacks and similar mortality among Hispanics, relative to that for Whites.12
Our findings of higher risk-adjusted inpatient mortality among lower area-income patients are consistent with most previous studies, although these studies are based on non-U.S. data.33, 34 Mechanisms underlying this association are not well known and appear complex, as noted in the broader literature on disparities by income.35, 36 Unobserved patient factors, including higher stroke severity or lower health literacy and different attitudes toward life-sustaining therapies among lower area-income populations, may underlie higher risk-adjusted inpatient mortality; however, this finding has also been noted in other studies using more detailed clinical indications, including stroke severity.37
Our finding of more frequent LOS > 4 days among Blacks and Hispanics, compared to Whites, is consistent with previous studies.12, 13 Stratified analysis also indicated that these differences are prevalent among all three area-income groups. The factors underlying these differences are now well understood. Longer LOS among minorities could be due to unmeasured confounders of small vessel stroke or socio-economic factors (including insurance coverage) that may affect timing of discharge to home or sub-acute care.38
Previous studies have noted the potential role of hospital factors in modifying subgroup differences in stroke outcomes.12, 13, 34 Racial and ethnic differences in structural characteristics of hospitals found in this study mirror those in the other studies; minority patients are more likely to receive care in larger hospitals (# beds, #ICU beds and admission volume), including teaching and safety-net hospitals.12, 13 However, these differences were not associated with a measurable change in the pattern of differences in outcomes by race/ethnicity or SES.
This study has several limitations. Firstly, the administrative data used contains limited clinical information on stroke severity. Sensitivity analysis with use of mechanical ventilation as a proxy indicator of patient severity affects the trends in disparities for adjusted inpatient mortality, indicating lower rates for Blacks and Hispanics compared to Whites and similar rates by SES. Use of mechanical ventilation as measured in the study may not be an accurate proxy of initial stroke severity since it is not possible to distinguish between mechanical ventilation on admission vs. as a later complication. When present at admission, it may be a valid marker of severe stroke or perhaps of severe comorbid lung disease which is decompensated even by minor stroke. Alternatively, if it results from poor oral hygiene, inadequate dysphagia screening and aspiration pneumonia, then adjusting for its presence may in fact adjust away markers of poor stroke care. Nevertheless, these results point to the potential sensitivity of our main findings to unobserved stroke severity. Another limitation is that the diagnosis codes are not confirmed by patient charts.39 However, we found that patient differences in only two of the risk factors – age and presence of atrial fibrillation – mitigated most of the observed differences in inpatient mortality; additional patient comorbidity indicators did not influence relative differences markedly. Also our data does not capture important behavioral risk factors (smoking, physical activity and obesity).2 Not only is smoking strongly associated with stroke severity, its prevalence also varies considerably by race/ethnicity and SES. Our cases of acute ischemic strokes, identified by administrative diagnosis codes, were not confirmed by patient charts.40 Another limitation is that our data cannot distinguish first strokes from secondary strokes. Even though secondary strokes are associated with higher mortality,21 previous evidence indicates only a moderate Black-White difference (33% vs. 30%) in the rate of secondary strokes.12 Also our data does not include out-of-hospital strokes. Two prior studies similar rates (nearly 10%) of strokes (all subtypes) ascertained only in out-of-hospital setting6, 28; these rates were similar among Whites and Blacks.28 The accuracy and consistency of race and ethnicity information, including the extent to which they are patient-reported, is also likely to vary across hospitals. Our selection of the eight states was partly based on completeness of race and ethnicity data; also, all these states had adopted the current federal guidelines for reporting race and ethnicity information.17, 23 Also, our measure of SES is not an individual measure but based on area-level (zip code) income; also, zip codes are more heterogeneous than census tract or block area units,41 the latter are not available in the inpatient discharge data.
To summarize, we found that the significantly lower rates of observed inpatient mortality among Blacks and Hispanics, compared to that among Whites, is primarily associated with differences in patient risk factors; specifically, adjusting for younger age and lower rate of atrial fibrillation among Blacks and Hispanics completely mitigates the differences in observed inpatient mortality. Also, we found significantly higher risk-adjusted rates among low area-income patients compared to high area-income patients. However, this pattern was not evident in sensitivity analyses including the use of mechanical ventilation as a partial surrogate for stroke severity. Further research in potential differences in patient severity or process of care is needed to identify the sources of this differential outcome rate by race/ethnicity and SES.
Supplementary Material
Acknowledgments
Sources of funding:
This research has been funded by NIH grants 1R21NS062677 (PI=Amresh Hanchate) and 1R01HL106029-01 (PI=Elaine Hylek).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
None of the authors have a conflict of interest. Dr. Lee Schwamm is Chair of the Get With The Guidelines Steering Committee (unpaid) and a consultant to the Massachusetts Department of Public Health. The views expressed in this article are those of the authors and do not necessarily represent the views of the National Institutes of Health, Boston University or Department of Veterans Affairs.
References
- 1.NHLBI. Morbidity & Mortality: 2009 Chart Book on Cardiovascular, Lung, and Blood Diseases. Bethesda, MD: National Institutes of Health; 2009. [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart Disease and Stroke Statistics—2012 Update. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. Writing Group Members. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Center for Health Statistics. Health, United States, 2010: With Special Feature on Death and Dying. 2011 [PubMed]
- 4.Broderick JP, Ferioli S. Assessing stroke incidence and mortality Across the United States. Annals of neurology. 2011;69:595–596. doi: 10.1002/ana.22437. [DOI] [PubMed] [Google Scholar]
- 5.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, Cushman M, Moy CS, Soliman EZ, Kissela BM, Howard G. Disparities in stroke incidence contributing to disparities in stroke mortality. Annals of neurology. 2011;69:619–627. doi: 10.1002/ana.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kissela B, Schneider A, Kleindorfer D, Khoury J, Miller R, Alwell K, Woo D, Szaflarski J, Gebel J, Moomaw C, Pancioli A, Jauch E, Shukla R, Broderick J. Stroke in a biracial population: the excess burden of stroke among blacks. Stroke. 2004;35:426–431. doi: 10.1161/01.STR.0000110982.74967.39. [DOI] [PubMed] [Google Scholar]
- 7.Kleindorfer D, Broderick J, Khoury J, Flaherty M, Woo D, Alwell K, Moomaw CJ, Schneider A, Miller R, Shukla R, Kissela B. The unchanging incidence and case-fatality of stroke in the 1990s: a population-based study. Stroke. 2006;37:2473–2478. doi: 10.1161/01.STR.0000242766.65550.92. [DOI] [PubMed] [Google Scholar]
- 8.Rosamond WD, Folsom AR, Chambless LE, Wang C-H, McGovern PG, Howard G, Copper LS, Shahar E. Stroke Incidence and Survival Among Middle-Aged Adults: 9-Year Follow-Up of the Atherosclerosis Risk in Communities (ARIC) Cohort. Stroke. 1999;30:736–743. doi: 10.1161/01.str.30.4.736. [DOI] [PubMed] [Google Scholar]
- 9.Morgenstern LB, Smith MA, Lisabeth LD, Risser JMH, Uchino K, Garcia N, Longwell PJ, McFarling DA, Akuwumi O, Al-Wabil A, Al-Senani F, Brown DL, Moye LA. Excess Stroke in Mexican Americans Compared with Non-Hispanic Whites: The Brain Attack Surveillance in Corpus Christi Project. Am. J. Epidemiol. 2004;160:376–383. doi: 10.1093/aje/kwh225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White H, Boden-Albala B, Wang C, Elkind MS, Rundek T, Wright CB, Sacco RL. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005;111:1327–1331. doi: 10.1161/01.CIR.0000157736.19739.D0. [DOI] [PubMed] [Google Scholar]
- 11.Northern Manhattan Stroke Study Collaborators. Sacco RL, Boden-Albala B, Gan R, Chen X, Kargman DE, Shea S, Paik MC, Hauser WA. Stroke Incidence among White, Black, and Hispanic Residents of an Urban Community. American journal of epidemiology. 1998;147:259–268. doi: 10.1093/oxfordjournals.aje.a009445. [DOI] [PubMed] [Google Scholar]
- 12.Schwamm LH, Reeves MJ, Pan W, Smith EE, Frankel MR, Olson D, Zhao X, Peterson E, Fonarow GC. Race/Ethnicity, Quality of Care, and Outcomes in Ischemic Stroke. Circulation. 2010;121:1492–1501. doi: 10.1161/CIRCULATIONAHA.109.881490. [DOI] [PubMed] [Google Scholar]
- 13.Xian Y, Holloway RG, Noyes K, Shah MN, Friedman B. Racial Differences in Mortality Among Patients With Acute Ischemic Stroke. Annals of Internal Medicine. 2010;154:152–159. doi: 10.1059/0003-4819-154-3-201102010-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stansbury JP, Jia H, Williams LS, Vogel WB, Duncan PW. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke. 2005;36:374–386. doi: 10.1161/01.STR.0000153065.39325.fd. [DOI] [PubMed] [Google Scholar]
- 15.Kuhlemeier K, Stiens S. Racial disparities in severity of cerebrovascular events. Stroke. 1994;25:2126–2131. doi: 10.1161/01.str.25.11.2126. [DOI] [PubMed] [Google Scholar]
- 16.Lisabeth LD, Risser JMH, Brown DL, Al-Senani F, Uchino K, Smith MA, Garcia N, Longwell PJ, McFarling DA, Al-Wabil A, Akuwumi O, Moye LA, Morgenstern LB. Stroke Burden in Mexican Americans: The Impact of Mortality Following Stroke. Annals of Epidemiology. 2006;16:33–40. doi: 10.1016/j.annepidem.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 17.Schoenman JA, Sutton JP, Kintala S, Love D, Maw R. The Value of Hospital Discharge Databases. NORC at the University of Chicago. 2005 [Google Scholar]
- 18.U.S. Census Bureau. Population Profile of the United States: 2000 (Internet Release) 2008 [Google Scholar]
- 19.American Hospital Association. AHA Annual Survey Database. Chicago: 2010. [Google Scholar]
- 20.Agency for Healthcare Research and Quality. Guide to Inpatient Quality Indicators: Quality of Care in Hospitals - Volume, Mortality and Utilization. 2011 [Google Scholar]
- 21.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J. Heart Disease and Stroke Statistics—2011 Update. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldstein LB, Samsa GP, Matchar DB, Horner RD. Charlson Index comorbidity adjustment for ischemic stroke outcome studies. Stroke. 2004;35:1941–1945. doi: 10.1161/01.STR.0000135225.80898.1c. [DOI] [PubMed] [Google Scholar]
- 23.Federal Registrar. Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity. Federal Registrar. 1997;62:58781–58790. [Google Scholar]
- 24.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial Trends in the Use of Major Procedures among the Elderly. N Engl J Med. 2005;353:683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 25.Skinner JS, Weinstein JN, Sporer SM, Wennberg JE. Racial, Ethnic, and Geographic Disparities in Rates of Knee Arthroplasty among Medicare Patients. The New England Journal of Medicine. 2003;349:1350–1359. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 26.Birkmeyer JD, Dimick JB, Birkmeyer NJO. Measuring the quality of surgical care: structure, process, or outcomes? Journal of the American College of Surgeons. 2004;198:626–632. doi: 10.1016/j.jamcollsurg.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 27.Horner RD, Sloane RJ, Kahn KL. Is use of mechanical ventilation a reasonable proxy indicator for coma among Medicare patients hospitalized for acute stroke? Health Services Research. 1998;32:841–859. [PMC free article] [PubMed] [Google Scholar]
- 28.Markus HS, Khan U, Birns J, Evans A, Kalra L, Rudd AG, Wolfe CD, Jerrard-Dunne P. Differences in stroke subtypes between black and white patients with stroke: the South London Ethnicity and Stroke Study. Circulation. 2007;116:2157–2164. doi: 10.1161/CIRCULATIONAHA.107.699785. [DOI] [PubMed] [Google Scholar]
- 29.Hajat C, Tilling K, Stewart JA, Lemic-Stojcevic N, Wolfe CD. Ethnic differences in risk factors for ischemic stroke: a European case-control study. Stroke; a journal of cerebral circulation. 2004;35:1562–1567. doi: 10.1161/01.STR.0000131903.04708.b8. [DOI] [PubMed] [Google Scholar]
- 30.Polsky D, Lave J, Klusaritz H, Jha A, Pauly MV, Cen L, Xie H, Stone R, Chen Z, Volpp K. Is lower 30-day mortality posthospital admission among blacks unique to the Veterans Affairs health care system? Medical Care. 2007;45:1083–1089. doi: 10.1097/MLR.0b013e3180ca960e. [DOI] [PubMed] [Google Scholar]
- 31.Volpp KG, Stone R, Lave JR, Jha AK, Pauly M, Klusaritz H, Chen H, Cen L, Brucker N, Polsky D. Is thirty-day hospital mortality really lower for black veterans compared with white veterans? Health Serv Res. 2007;42:1613–1631. doi: 10.1111/j.1475-6773.2006.00688.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wolfe CD, Smeeton NC, Coshall C, Tilling K, Rudd AG. Survival differences after stroke in a multiethnic population: follow-up study with the South London stroke register. BMJ. 2005;331:431. doi: 10.1136/bmj.38510.458218.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cox AM, McKevitt C, Rudd AG, Wolfe CDA. Socioeconomic status and stroke. The Lancet Neurology. 2006;5:181–188. doi: 10.1016/S1474-4422(06)70351-9. [DOI] [PubMed] [Google Scholar]
- 34.Saposnik G, Jeerakathil T, Selchen D, Baibergenova A, Hachinski V, Kapral MK for the Stroke Outcome Research Canada Working G. Socioeconomic Status, Hospital Volume, and Stroke Fatality in Canada. Stroke. 2008;39:3360–3366. doi: 10.1161/STROKEAHA.108.521344. [DOI] [PubMed] [Google Scholar]
- 35.Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in Quality: Addressing Socioeconomic, Racial, and Ethnic Disparities in Health Care. JAMA. 2000;283:2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 36.Gornick ME, Eggers PW, Reilly TW, Mentnech RM, Fitterman LK, Kucken LE, Vladeck BC. Effects of Race and Income on Mortality and Use of Services among Medicare Beneficiaries. N Engl J Med. 1996;335:791–799. doi: 10.1056/NEJM199609123351106. [DOI] [PubMed] [Google Scholar]
- 37.Borrell LN, Diez Roux AV, Rose K, Catellier D, Clark BL. Neighbourhood characteristics and mortality in the Atherosclerosis Risk in Communities Study. International journal of epidemiology. 2004;33:398–407. doi: 10.1093/ije/dyh063. [DOI] [PubMed] [Google Scholar]
- 38.van Straten A, van der Meulen JHP, van den Bos GAM, Limburg M. Length of Hospital Stay and Discharge Delays in Stroke Patients. Stroke. 1997;28:137–140. doi: 10.1161/01.str.28.1.137. [DOI] [PubMed] [Google Scholar]
- 39.Schoenman JA, Sutton JP, Elixhauser A, Love D. Understanding and enhancing the value of hospital discharge data. Med Care Res Rev. 2007;64:449–468. doi: 10.1177/1077558707301963. [DOI] [PubMed] [Google Scholar]
- 40.Goldstein LB. Accuracy of ICD-9-CM Coding for the Identification of Patients With Acute Ischemic Stroke : Effect of Modifier Codes. Stroke. 1998;29:1602–1604. doi: 10.1161/01.str.29.8.1602. [DOI] [PubMed] [Google Scholar]
- 41.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


