Abstract
Study Objectives:
Older adults frequently report disruptions in their ability to initiate and maintain sleep. It remains unclear whether these sleep problems are consequent to associated medical comorbidities or if they represent primary sleep disturbances that exist independent of other disorders of senescence. Herein we describe sleep characteristics and associated medical and psychiatric comorbidities among ethnically diverse nondemented older adults.
Methods:
The cross-sectional sample consisted of 702 participants drawn from the Einstein Aging Study (EAS), a community-based study of aging. Sleep onset/maintenance difficulties (SO/MD) were ascertained using responses from the Medical Outcomes Study Sleep Scale (MOS-SS). Participants also completed assessments of medical history, psychological symptoms, and medication use.
Results:
Participants were an average of 80 ± 5.5 years of age and had 14 ± 3.4 years of education. Older adults reported sleeping an average of 6.5 ± 1.2 h/night. Mild SO/MD was reported in 43% of participants, while moderate/severe SO/MD was reported in 12% of participants. Sleep problems were associated with measures of obesity and symptoms of depression and anxiety. SO/MD was not associated with history of common medical conditions. Use rates of insomnia medication were low (0% to 3%).
Conclusions:
The prevalence of SO/MD is high in the elderly community-dwelling population and is associated with common psychiatric disorders. With the exception of obesity, SO/MD is not associated with common medical disorders. Further study is necessary to disentangle the nature of the relationship between sleep disturbance and psychiatric comorbidity among older adults.
Citation:
Zimmerman ME; Bigal ME; Katz MJ; Derby CA; Lipton RB. Are sleep onset/maintenance difficulties associated with medical or psychiatric comorbidities in nondemented community-dwelling older adults? J Clin Sleep Med 2013;9(4):363-369.
Keywords: Sleep, insomnia, older adults, elderly, depression, anxiety, medical history, comorbidities
Advanced age is associated with alterations in sleep patterns and the sleep/wake cycle.1,2 Total sleep time, sleep quality, and slow wave sleep are reduced as a function of age.3 Compared to younger adults, older adults also report a disproportionate number of symptoms consistent with insomnia.4–6 Clinical insomnia is characterized as a complaint of disturbed sleep, despite adequate opportunity to sleep, that results in negative daytime consequences and an inability to adequately carry out activities of daily functioning.7,8 Sleep complaints associated with insomnia include difficulty falling asleep, frequent awakenings during the night, or waking up too early.9 The personal and societal impact of chronic sleep difficulties among older adults is extensive and includes cognitive impairment, high rates of falls and mortality, institutionalization, psychosocial dysfunction, impaired activities of daily living, and decreased health-related quality of life.10–14
It has been suggested that sleep problems and sleep complaints among older adults may be more strongly related to comorbid medical conditions than the aging process itself.15–19 An improved understanding of the prevalence of sleep disturbances and associated comorbidities is necessary to optimize clinical outcomes in the rapidly growing cohort of older adults residing in communities and specialized care facilities. The goal of this report is to describe the prevalence of sleep disturbances and associated medical and psychiatric comorbidities in a community-based sample of over 700 ethnically and racially diverse nondemented older adults.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Older adults frequently report problems falling or staying asleep that negatively impact their ability to function while awake. It is not known if these sleep disruptions are the result of the aging process itself or the increased incidence of medical conditions that often accompany old age.
Study Impact: Difficulties falling and staying asleep were commonly reported among our community-based sample of nondemented older adults. These sleep disturbances were associated with measures of obesity and symptoms of depression and anxiety, but not with other major medical conditions.
METHODS
Study Participants
Study participants were drawn from the Einstein Aging Study (EAS), an ongoing longitudinal community-based study of ethnically and racially diverse individuals aged 70+ residing in the Bronx, New York. The sample under study initially consisted of 841 individuals enrolled in the EAS from October of 2005 to June of 2010. Since there is evidence that older adults with dementia experience a disproportionate amount of abnormal day and nighttime sleep disturbances, we excluded 33 individuals with a diagnosis of dementia based on the criteria provided by the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV). In addition, 42 individuals were excluded who did not provide enough clinical data to assign a final diagnosis. Finally, 64 individuals were excluded who completed core clinical assessments but were not able to return to the clinic for a second visit in which the sleep assessment was administered. Therefore, the final sample of interest for the analyses presented in this report comprised 702 nondemented participants for whom baseline retrospective data on sleep disturbance (questionnaire described in more detail below) were available for analyses. Participants completed neuropsychological and psychosocial assessments and received medical examinations at annual core clinic visits. The study was approved by the Albert Einstein College of Medicine Institutional Review Board, and informed consent was obtained from all participants. EAS study design and methods are described in more detail elsewhere.20 Global cognitive function was assessed with the Blessed Information-Memory-Concentration test (BIMC21).
Sleep Questionnaire
Sleep disturbance was assessed using the Medical Outcomes Study sleep scale (MOS-SS).22 The MOS-SS was introduced to the EAS in October of 2005. MOS-SS data from the initial administration of the scale were utilized in the current analyses. The MOS-SS consists of 12 questions that require recall over the preceding 4 weeks. Responses generate a measure of sleep quantity (average hours of sleep per night) and 6 subscale scores (sleep disturbance, snoring, wakening with shortness of breath or headache, adequacy of sleep, daytime somnolence, and a global sleep problem index score). MOS-SS subscales and the index score range from 0-100, with higher scores reflecting more problems with the concept indicated. Mild and moderate/severe sleep onset/maintenance difficulties (SO/MD) were chosen as variables of interest based on previous research using criteria established by Katz and McHorney23 that employed 2 questions from the MOS-SS. The sleep initiation question was, “How often during the past four weeks did you have trouble falling asleep?” while the sleep maintenance question was, “How often during the past four weeks did you awaken during your sleep time and have trouble falling asleep again?” Response to either question as “a good bit” or “some” of the time was designated mild SO/MD, while “most” or “all” of the time was designated moderate/severe SO/MD. In the event that a participant reported a pattern of responses that would place them in both designations (e.g., a response of “a good bit” of the time to the initiation question and a response of “all” of the time to the maintenance question), they were assigned to the moderate/severe SO/MD group to maintain independence of the groups. This occurred in 27 (3.8%) cases.
Medical and Psychological History
Participants completed a medical and psychosocial interview during the initial MOS-SS administration. Information was obtained regarding present or past history of myocardial infarction, stroke, coronary artery bypass graft (CABG), diabetes, hypertension, arrhythmia, angina, heart failure, Parkinson disease, cancer, pacemaker, or osteoarthritis. A dichotomous variable indicated whether the participant reported the presence or absence of any of these medical conditions at either the study visit of the initial MOS-SS administration or any previous study visit. An index of cardiovascular comorbidities was calculated to indicate presence of any current or past history of myocardial infarction, stroke, or CABG. An index of total medical comorbidities was calculated to indicate presence of any current or past history of all of the previously listed medical conditions. Body mass index (BMI) was calculated using weight in kilograms divided by height in meters squared. Using published guidelines,24 an individual was designated over-weight with a BMI between 25.0 and 29.9, or designated obese with a BMI ≥ 30.0. Abdominal obesity was defined as a waist circumference ≥ 88 cm in females and ≥ 102 cm in males.
Depressive symptoms at the initial MOS-SS administration were assessed using the 15-item Geriatric Depression Scale (GDS).25 A cut score of 5 or higher is associated with clinically significant symptoms.26 Anxiety symptoms were assessed using the Beck Anxiety Inventory (BAI).27 A cut score ≥ 11 is associated with clinically significant symptoms.28 BAI data were available for a subsample of 208 participants.
Medication Use
Prescribed medications were recorded during the initial MOSSS administration. Based on the guidelines of Bloom and colleagues,7 medications of interest that may be used to treat sleep disturbance in older adults include benzodiazepines, benzodiaze-pine receptor agonists (non-benzodiazepines), melatonin receptor agonists, tricyclic/sedating antidepressants (TCA), and antipsychotics. Medications of interest that may exacerbate or contribute to sleep disturbances include selective serotonin reuptake inhibitors (SSRI), serotonin and norepinephrine reuptake inhibitor (SNRI), β-blockers/antihypertensives, and mood stabilizers.
Statistical Analysis
All analyses were conducted using SPSS 17 (SPSS for Windows, Released 8.23.2008. Chicago: SPSS Inc.). Frequency counts were used to characterize the prevalence rates of SO/ MD, medical history, and medication usage. Analysis of variance (ANOVA), χ2, or independent sample t-tests were used as appropriate to examine SO/MD group (i.e., no SO/MD, mild SO/MD, or moderate/severe SO/MD) differences on demographics, medical and psychiatric variables, medication use, and MOS-SS scores. A Kruskal-Wallis test was used to examine SO/MD group differences on global cognitive function (BIMC). Ordinal logistic regression was used to examine the relationship between age, education, obesity, depression, and anxiety (independent variables) and SO/MD group (dependent variable). In these analyses, obesity, depression, and anxiety were entered as dichotomous variables using clinically signifi-cant categorizations (described above), while age and education were entered as continuous variables. Linear regression was used to examine the relationship between age, education, BMI, depressive symptoms, and anxiety symptoms (entered simultaneously as continuous independent variables) and the MOS-SS global sleep problem index (dependent variable).
In follow-up analyses examining the association of sleep disordered breathing (using snoring as a common symptom) and BMI, Pearson correlations were used to determine the relationship between BMI (as a continuous variable) and the MOSSS snoring subscale. ANOVA was used to examine BMI (as a categorical variable; normal weight, overweight, obese) group differences on the MOS-SS snoring subscale. Ordinal logistic regression was used to examine the relationship between age, education, obesity, depression, anxiety, and the MOS-SS snoring subscale (independent variables) and SO/MD group (dependent variable). In these analyses, obesity, depression, and anxiety were entered as dichotomous variables using clinically significant categorizations while age, education, and snoring were entered as continuous variables. Finally, the primary linear and ordinal logistic regression models described above were repeated with the removal of the BMI/obesity variable and the addition of the MOS-SS snoring variable in order to examine the unique effect of snoring to the results.
RESULTS
Sample Demographic Characteristics and Medical History
Sample demographics and medical history are presented in Table 1. Of reported ethnicity, 68.4% were Caucasian, 26.2% were African American, 3.1% were Hispanic/White, 1.3% were Hispanic/Black, 0.6% were Asian, and 3 participants reported other ethnicities. For the remaining analyses, ethnicity was collapsed into two groups that comprised Caucasians (68.4%) and African American/Other Ethnicity (31.6%).
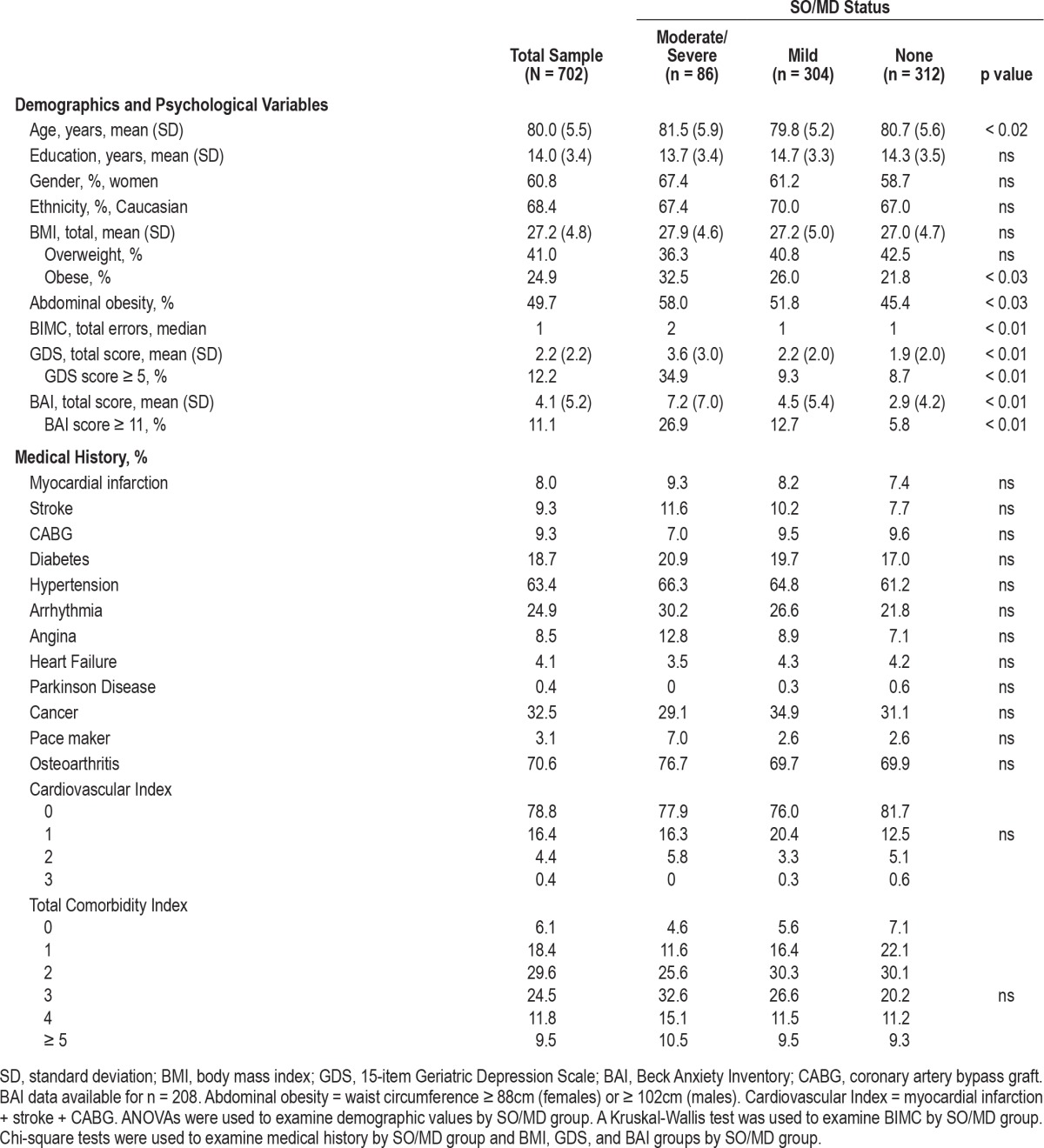
Table 1.
Sample demographics and medical history by sleep onset/maintenance difficulty (SO/MD) status
SO/MD Characteristics
Demographics by SO/MD group are shown in Table 1. A total of 304 (43.3%) participants met criteria for mild SO/MD, 86 (12.3%) met criteria for moderate/severe SO/MD, and 312 (44.4%) did not meet criteria for SO/MD. When BMI was dichotomized according to obesity status (present or absent), there was a linear-by-linear association (χ2 = 4.8, p < 0.03), reflecting a trend for increasing prevalence of obesity with increasing severity of SO/MD. There was also a linear-by-linear association (χ2 = 4.9, p < 0.03) for abdominal obesity such that participants with moderate/severe SO/MD exhibited the highest proportion of abdominal obesity. Participants with mild SO/MD were younger than those with moderate/severe SO/MD (p < 0.01) and those without SO/MD (p < 0.03). When depressive symptoms were dichotomized into clinically significant categorizations, there was a linear-by-linear association (χ2 = 26.5, p < 0.01), reflecting a trend for proportions by SO/MD group with older adults with moderate/severe SO/MD reporting the highest proportion of depressive symptoms. When anxiety symptoms were dichotomized into clinically significant categorizations, there was a linear-by-linear association (χ2 = 9.1, p < 0.01), reflecting a trend for proportions by SO/MD group with older adults with moderate/severe SO/MD reporting the highest proportion of anxiety symptoms. Ordinal logistic regression revealed that SO/MD group was associated with age (p < 0.02) and clinically significant anxiety symptoms (p < 0.01), but not with education (p < 0.40), obesity (p < 0.21), or clinically significant depressive symptoms (p < 0.87). Chi-square analyses indicated that there were no relationships between SO/MD status and other common medical conditions, including the cardiovascular summary index and the total medical comorbidity index.
Medication Use
As displayed in Table 2, a minority of participants used medication that may be used to treat insomnia. A greater proportion of older adults with moderate/severe SO/MD were taking antipsychotics (χ2 = 8.7, p < 0.01) and non-benzodiazepines (χ2 = 9.0, p < 0.01). There was a linear-by-linear association for non-benzodiazepines (χ2 = 4.8, p < 0.03), whereby older adults with moderate/severe SO/MD reported taking the highest proportion of non-benzodiazepines.
Table 2.
MOS-SS subscale scores and medication use by sleep onset/maintenance difficulty (SO/MD) status
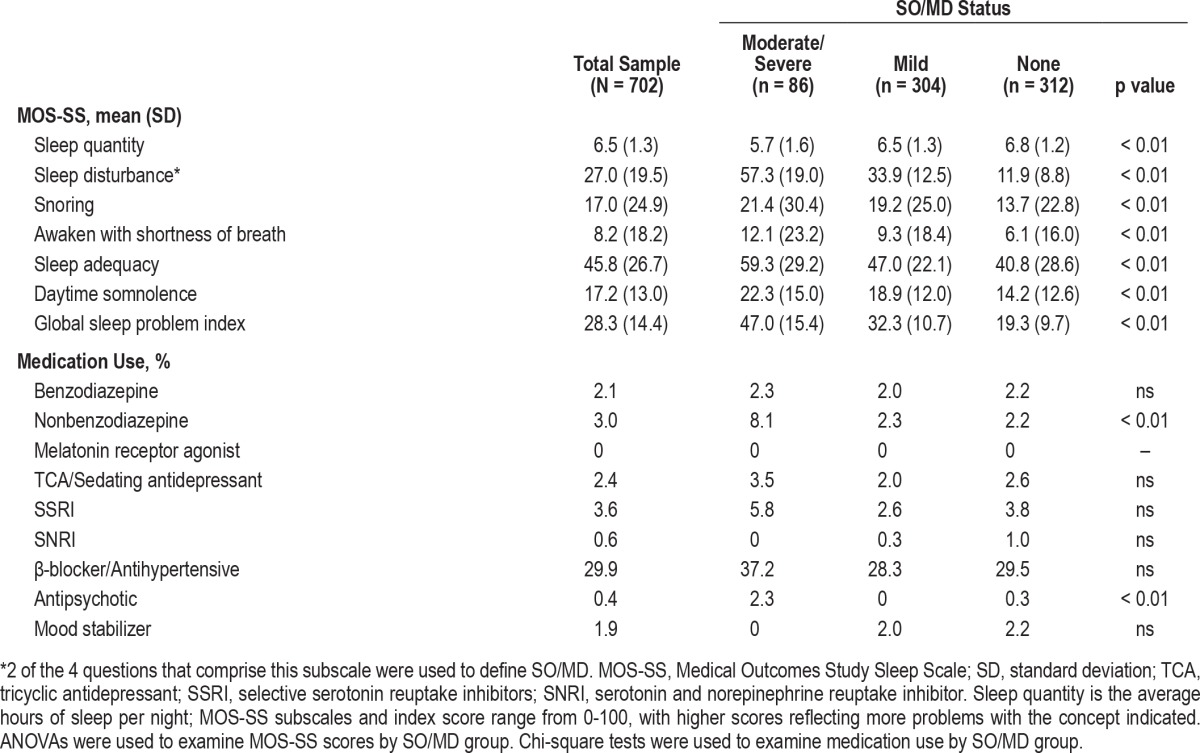
MOS-SS Characteristics
MOS-SS characteristics are shown in Table 2. Linear regression revealed that the global sleep problem index was associated with age (p < 0.02) and anxiety symptoms (p < 0.01), but not with education (p < 0.43), BMI (p < 0.27) or depressive symptoms (p < 0.27).
MOS-SS Snoring Subscale Characteristics
In follow-up analyses, individuals with higher BMI reported a higher prevalence of snoring on the MOS-SS snoring subscale (r = 0.16, p < 0.01). There also were significant group differences among normal weight, overweight, and obese older adults on the MOS-SS snoring subscale in the expected direction, with obese individuals reporting more frequent snoring (F2,653 = 11.76, p < 0.01). As shown in Table 2, ANOVA revealed a relationship between SO/MD group and snoring (p < 0.01), where older adults with moderate/severe SO/MD reported the highest rates of snoring. Ordinal logistic regression indicated that the addition of snoring to the model described above did not change the overall pattern of findings; i.e., age (p < 0.02) and anxiety (p < 0.01) remained significant correlates of SO/MD status while education (p < 0.37), depression (p < 0.89), obesity (p < 0.37), and snoring (p < 0.18) were not. Because BMI and snoring were significantly associated, the linear and ordinal logistic models were repeated with the removal of the BMI/obesity variable and the addition of the MOS-SS snoring variable. In the linear regression model, anxiety remained significantly associated with the MOS-SS global sleep problem index (p < 0.01), but snoring was not associated (p < 0.61). In the ordinal logistic model, anxiety again remained significantly associated with SO/MD (p < 0.01), but snoring was not associated (p < 0.29).
DISCUSSION
Herein we characterize sleep difficulties and their association with medical and psychiatric comorbidities in a community-based sample of ethnically and racially diverse older adults. We found high prevalence rates of mild (43%) and moderate/ severe (12%) sleep onset/maintenance difficulties consistent with symptoms of insomnia. In addition, sleep problems were strongly associated with measures of obesity and symptoms of depression and anxiety, but not with medical history.
Clinical insomnia is defined as difficulty initiating or maintaining sleep, frequent nighttime or early morning awakenings, or poor quality sleep that is chronically non-restorative and results in negative daytime consequences.8,29 A confluence of evidence suggests that insomnia is among the most common sleep complaints reported by elderly adults.4 An important study of older adults by Foley and colleagues19 reported chronic sleep complaints in over 50% of older adults, with 43% reporting sleep difficulties consistent with insomnia and 25% reporting daytime napping. A 2003 survey found that 46% of adults aged 65 to 74 and 50% of adults aged 75 to 84 reported symptoms of insomnia.16 Other studies11,30 also support our finding that sleep onset and sleep maintenance difficulties are a widespread sleep disturbance in community-dwelling older adults.
It has been suggested that sleep problems among older adults may be more strongly related to comorbid medical and psychiatric conditions than the aging process itself.15 With the exception of obesity, we did not find that SO/MD were associated with measures of common medical conditions. However, the average age of our sample was relatively advanced and the report of medical conditions was generally low, with the exception of hypertension. Therefore, the lack of a relationship between medical conditions and SO/MD in our sample may be due to survivor effects inherent in observational community-based studies of adults of advanced age. In addition, results from community-based studies often differ from those of clinic-based studies due to Berkson's selection bias, which may occur in clinic or hospital settings when comorbid diseases appear to be related to the primary exposure of interest simply because comprehensive evaluations are taking place or because individuals with multiple medical conditions are more likely to seek treatment in a clinic. In agreement with our findings, others have shown a robust relationship between sleep disruption and symptoms of depression and anxiety.31 Although only 12% of our total sample reported clinically significant depressive symptoms, this rate was elevated to nearly 35% in older adults with moderate/severe SO/MD, and a similar trend was observed for anxiety symptoms. Our finding of a strong association between sleep disturbance and obesity is also in agreement with the extant literature, which suggests that there is a complex bidirectional relationship between several different sleep disorders and obesity (for review, see Beccuti32). Short sleep duration (usually < 6 h/night) is a risk factor for the development of obesity,33 and high BMI is associated with worse sleep quality in both middle-aged and older adults.34 It should be noted that in our study, SO/MD status was not associated with mean BMI; a relationship only emerged when BMI was categorized into the clinically significant designation of obesity. This suggests a nonlinear or threshold effect of the influence of body mass on sleep disturbance whereby older adults do not experience negative effects of increased BMI on sleep until they reach a clinical threshold where they can be termed “obese.” Obesity and obstructive sleep apnea (OSA) also have a well-documented relationship, with reported OSA prevalence rates in severely obese individuals undergoing bariatric surgery of up to 93.6% in men and 73.5% in women.35,36 Analyses in our sample using snoring as a common symptom of sleep apnea support this literature, with older adults who have higher BMI or moderate/severe SO/MD more frequently reporting snoring. However, replication of our primary models with snoring rather than BMI as independent variables did not change the pattern of findings, suggesting that the relationship between anxiety and sleep disturbance among older adults in our sample is stronger than that of either BMI or self-report of snoring. Nonetheless, the strength of the association between sleep, obesity, and psychological symptoms, as well as the convergence of these findings with the extant literature highlight the critical need for careful assessment and treatment of these comorbid conditions.
It is well known that older adults use multiple medications for a variety of reasons. Some medications, such selective serotonin reuptake inhibitors (SSRI), may contribute to the emergence or exacerbation of sleep disturbances among older adults.7 In our sample, use of these medications was relatively low. Of the three drug classes approved by the Food and Drug Administration for treatment of insomnia, benzodiazepines (2%) and non-benzodiazepines (3%) had low rates of use, while no one in our sample reported using melatonin receptor agonists. Trazodone is a non-tricyclic antidepressant with sedating properties that is commonly prescribed to treat patients with co-morbid depression and insomnia.37 In this study, we combined reports of trazodone use with tricyclic antidepressants and found a usage rate of approximately 2%. Overall, these rates are lower than those in a recent report from the Canadian Community Health Study, in which 16% of adults over the age of 60 indicated that they had taken a sleep medication over the past year,38 although this figure included over-the-counter medications. When medication use was examined as a function of SO/ MD in our sample, individuals with moderate/severe SO/MD were more likely to be taking nonbenzodiazepine and antipsychotic pharmaceuticals.
There are several limitations that require further discussion. In this study, the measures of primary interest were self-report. Nonetheless, self-report remains a valuable source of information from community-based samples and often forms the foundation upon which more detailed assessments can be designed and implemented. In addition, there is likely a strong bidirectional relationship between sleep disturbances and medical and psychological disorders in the older adult. Longitudinal studies are needed to address the direction and nature of these complex relationships. This study also did not record non-pharmacological or behavioral treatments for insomnia, such as cognitive behavioral therapy. Therefore, there are dimensions of treatments for insomnia and other sleep problems that this observational study was not specifically designed to address.
DISCLOSURE STATEMENT
This study was funded by Merck Sharpe & Dohme. Dr. Zimmerman has received research funding from Merck Sharp & Dohme Corporation. Drs. Zimmerman and Derby and Ms. Katz are co-investigators on NIH grant AG03949. Dr. Derby has received research support from Bristol-Myers Squibb, and S and L Marx Foundation. Dr. Lipton is the principal investigator of NIH grant AG03949 and has served as a consultant for Merck, Inc. He has also received research support from the National Headache Foundation and the Migraine Research Fund. He serves on the editorial boards of Neurology and Cephalalgia and as senior advisor to Headache. He holds stock options in eNeura Therapeutics. He also serves as an advisory board member, consultant, or has received honoraria from Allergan, American Headache Society, Autonomic Technologies, Boston Scientific, Bristol-Myers Squibb, Cognimed, Colucid, Eli Lilly, Endo, eNeura Therapeutics, GlaxoSmithKline, MAP, Merck, Nautilus Neuro-science, Novartis, NuPathe, and Pfizer. Dr. Bigal is a full-time employee of Merck, Inc. and owns stocks and stock options in Merck, Inc.
ACKNOWLEDGMENTS
The authors thank Charlotte Magnotta for assistance with participant recruitment, Betty Forro, Alicia Gomez, Wendy Ramratan, and Mary Joan Sebastian for assistance with clinical and neuropsychological assessments, Michael Potenza for assistance with data management, and all of the study participants who generously gave their time in support of this research. The work presented in this paper was supported by National Institutes of Health (NIH) grant AG03949 and Merck Sharp & Dohme Corporation.
REFERENCES
- 1.Ohayon MM, Vecchierini MF. Normative sleep data, cognitive function and daily living activities in older adults in the community. Sleep. 2005;28:981–9. [PubMed] [Google Scholar]
- 2.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 3.Kamel NS, Gammack JK. Insomnia in the elderly: cause, approach, and treatment. Am J Med. 2006;119:463–9. doi: 10.1016/j.amjmed.2005.10.051. [DOI] [PubMed] [Google Scholar]
- 4.Cooke JR, Ancoli-Israel S. Sleep and its disorders in older adults. Psychiatr Clin North Am. 2006;29:1077–93. doi: 10.1016/j.psc.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment. Prevalence and correlates. Arch Gen Psychiatry. 1985;42:225–32. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- 6.Neubauer DN. Sleep problems in the elderly. Am Fam Physician. 1999;59:2551–60. [PubMed] [Google Scholar]
- 7.Bloom HG, Ahmed I, Alessi CA, et al. Evidence-based recommendations for the assessment and management of sleep disorders in older persons. J Am Geriatr Soc. 2009;57:761–89. doi: 10.1111/j.1532-5415.2009.02220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vaz Fragoso CA, Gill TM. Sleep complaints in community-living older persons: a multifactorial geriatric syndrome. J Am Geriatr Soc. 2007;55:1853–66. doi: 10.1111/j.1532-5415.2007.01399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Institutes of Health State of the Science Conference Statement on Manifestations and Management of Chronic Insomnia in Adults. Sleep. 2005;28:1049–57. doi: 10.1093/sleep/28.9.1049. [DOI] [PubMed] [Google Scholar]
- 10.Enright PL, Newman AB, Wahl PW, Manolio TA, Haponik EF, Boyle PJ. Prevalence and correlates of snoring and observed apneas in 5,201 older adults. Sleep. 1996;19:531–8. doi: 10.1093/sleep/19.7.531. [DOI] [PubMed] [Google Scholar]
- 11.Schubert CR, Cruickshanks KJ, Dalton DS, Klein BE, Klein R, Nondahl DM. Prevalence of sleep problems and quality of life in an older population. Sleep. 2002;25:889–93. [PubMed] [Google Scholar]
- 12.Cricco M, Simonsick EM, Foley DJ. The impact of insomnia on cognitive functioning in older adults. J Am Geriatr Soc. 2001;49:1185–9. doi: 10.1046/j.1532-5415.2001.49235.x. [DOI] [PubMed] [Google Scholar]
- 13.Stone KL, Ancoli-Israel S, Blackwell T, et al. Actigraphy-measured sleep characteristics and risk of falls in older women. Arch Intern Med. 2008;168:1768–75. doi: 10.1001/archinte.168.16.1768. [DOI] [PubMed] [Google Scholar]
- 14.Dew MA, Hoch CC, Buysse DJ, et al. Healthy older adults' sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med. 2003;65:63–73. doi: 10.1097/01.psy.0000039756.23250.7c. [DOI] [PubMed] [Google Scholar]
- 15.Ancoli-Israel S. Sleep and its disorders in aging populations. Sleep Med. 2009;10(Suppl 1):S7–11. doi: 10.1016/j.sleep.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 16.Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res. 2004;56:497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Vitiello MV, Moe KE, Prinz PN. Sleep complaints cosegregate with illness in older adults: clinical research informed by and informing epidemiological studies of sleep. J Psychosom Res. 2002;53:555–9. doi: 10.1016/s0022-3999(02)00435-x. [DOI] [PubMed] [Google Scholar]
- 18.Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult - a mini-review. Gerontology. 2010;56:181–9. doi: 10.1159/000236900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18:425–32. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 20.Katz MJ, Lipton RB, Hall CB, et al. Age-specific and sex-specific prevalence and incidence of mild cognitive impairment, dementia, and Alzheimer dementia in blacks and whites: a report from the Einstein Aging Study. Alzheimer Dis Assoc Disord. 2012;26:335–43. doi: 10.1097/WAD.0b013e31823dbcfc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blessed G, Tomlinson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br J Psychiatry. 1968;114:797–811. doi: 10.1192/bjp.114.512.797. [DOI] [PubMed] [Google Scholar]
- 22.Hays RD, Martin SA, Sesti AM, Spritzer KL. Psychometric properties of the Medical Outcomes Study Sleep measure. Sleep Med. 2005;6:41–4. doi: 10.1016/j.sleep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 23.Katz DA, McHorney CA. The relationship between insomnia and health-related quality of life in patients with chronic illness. J Fam Pract. 2002;51:229–35. [PubMed] [Google Scholar]
- 24.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303:235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 25.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 26.Julian LJ, Gregorich SE, Earnest G, et al. Screening for depression in chronic obstructive pulmonary disease. COPD. 2009;6:452–8. doi: 10.3109/15412550903341463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–7. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 28.Karsten J, Nolen WA, Penninx BW, Hartman CA. Subthreshold anxiety better defined by symptom self-report than by diagnostic interview. J Affect Disord. 2011;129:236–43. doi: 10.1016/j.jad.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 29.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 30.Paudel ML, Taylor BC, Diem SJ, et al. Association between depressive symptoms and sleep disturbances in community-dwelling older men. J Am Geriatr Soc. 2008;56:1228–35. doi: 10.1111/j.1532-5415.2008.01753.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Motivala SJ, Levin MJ, Oxman MN, Irwin MR. Impairments in health functioning and sleep quality in older adults with a history of depression. J Am Geriatr Soc. 2006;54:1184–91. doi: 10.1111/j.1532-5415.2006.00819.x. [DOI] [PubMed] [Google Scholar]
- 32.Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011;14:402–12. doi: 10.1097/MCO.0b013e3283479109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lauderdale DS, Knutson KL, Rathouz PJ, Yan LL, Hulley SB, Liu K. Cross-sectional and longitudinal associations between objectively measured sleep duration and body mass index: the CARDIA Sleep Study. Am J Epidemiol. 2009;170:805–13. doi: 10.1093/aje/kwp230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Phillips BG, Hisel TM, Kato M, et al. Recent weight gain in patients with newly diagnosed obstructive sleep apnea. J Hypertens. 1999;17:1297–300. doi: 10.1097/00004872-199917090-00009. [DOI] [PubMed] [Google Scholar]
- 36.Sareli AE, Cantor CR, Williams NN, et al. Obstructive sleep apnea in patients undergoing bariatric surgery—a tertiary center experience. Obes Surg. 2011;21:316–27. doi: 10.1007/s11695-009-9928-1. [DOI] [PubMed] [Google Scholar]
- 37.Walsh JK, Schweitzer PK. Ten-year trends in the pharmacological treatment of insomnia. Sleep. 1999;22:371–5. [PubMed] [Google Scholar]
- 38.Neutel CI, Patten SB. Sleep medication use in Canadian seniors. Can J Clin Pharmacol. 2009;16:e443–452. [PubMed] [Google Scholar]


