Abstract
Metabolic syndrome is a growing health problem worldwide. It is therefore imperative to develop new strategies to treat this pathology. In the past years, the manipulation of NAD+ metabolism has emerged as a plausible strategy to ameliorate metabolic syndrome. In particular, an increase in cellular NAD+ levels has beneficial effects, likely because of the activation of sirtuins. Previously, we reported that CD38 is the primary NAD+ase in mammals. Moreover, CD38 knockout mice have higher NAD+ levels and are protected against obesity and metabolic syndrome. Here, we show that CD38 regulates global protein acetylation through changes in NAD+ levels and sirtuin activity. In addition, we characterize two CD38 inhibitors: quercetin and apigenin. We show that pharmacological inhibition of CD38 results in higher intracellular NAD+ levels and that treatment of cell cultures with apigenin decreases global acetylation as well as the acetylation of p53 and RelA-p65. Finally, apigenin administration to obese mice increases NAD+ levels, decreases global protein acetylation, and improves several aspects of glucose and lipid homeostasis. Our results show that CD38 is a novel pharmacological target to treat metabolic diseases via NAD+-dependent pathways.
Obesity is a disease that has reached epidemic proportions in developed and developing countries (1–3). In the U.S., >60% of the population is overweight (1,3,4). Obesity is a feature of metabolic syndrome, which includes glucose intolerance, insulin resistance, dyslipidemia, and hypertension. These pathologies are well-documented risk factors for cardiovascular disease, type 2 diabetes, and stroke (4). It is therefore imperative to envision new strategies to treat metabolic syndrome and obesity.
Recently, the role of NAD+ as a signaling molecule in metabolism has become a focus of intense research. It was shown that an increase in intracellular NAD+ levels in tissues protects against obesity (5,6), metabolic syndrome, and type 2 diabetes (5–7). Our group was the first to demonstrate that an increase in NAD+ levels protects against high-fat diet–induced obesity, liver steatosis, and metabolic syndrome (5). This concept was later expanded by others using different approaches, including inhibition of poly-ADP-ribose polymerase (PARP)1 (6) and stimulation of NAD+ synthesis (7).
The ability of NAD+ to affect metabolic diseases seems to be mediated by sirtuins (8). This family of seven NAD+-dependent protein deacetylases, particularly SIRT1, SIRT3, and SIRT6, has gained significant attention as candidates to treat metabolic syndrome and obesity (9). Sirtuins use and degrade NAD+ as part of their enzymatic reaction (8), which makes NAD+ a limiting factor for sirtuin activity (9). In particular, silent mating information regulation 2 homolog 1 (SIRT1) has been shown to deacetylate several proteins, including p53 (10), RelA/p65 (11), PGC1-α (12), and histones (13), among others. In addition, increased expression of SIRT1 (14), increased SIRT1 activity (15), and pharmacological activation of SIRT1 (16) protect mice against liver steatosis and other features of metabolic syndrome when mice are fed a high-fat diet. Given the beneficial consequences of increased SIRT1 activity, great efforts are being directed toward the development of pharmacological interventions aimed at activating SIRT1.
We previously reported that the protein CD38 is the primary NAD+ase in mammalian tissues (17). In fact, tissues of mice that lack CD38 contain higher NAD+ levels (17,18) and increased SIRT1 activity compared with wild-type mice (5,17). CD38 knockout mice are resistant to high-fat diet–induced obesity and other aspects of metabolic disease, including liver steatosis and glucose intolerance, by a mechanism that is SIRT1 dependent (5). These multiple lines of evidence suggest that pharmacological CD38 inhibition would lead to SIRT1 activation through an increase in NAD+ levels, resulting in beneficial effects on metabolic syndrome.
Recently, it was shown that in vitro, CD38 is inhibited by flavonoids, including quercetin (19). Flavonoids are naturally occurring compounds present in a variety of plants and fruits (20). Among them, quercetin [2-(3,4-dihydroxyphenyl)-3,5,7-trihydroxy-4H-chromen-4-one] and apigenin [5,7-dihydroxy-2-(4-hydroxyphenyl)-4H-1-benzopyran-4-one] have been shown to have beneficial effects against cancer (21–24). In fact, apigenin and quercetin ameliorate atherosclerosis (25) and reduce inflammation (26–28). However, the mechanisms of action of flavonoids remain largely unknown. We hypothesized that the effect of some flavonoids in vivo may occur through inhibition of CD38 and an increase in NAD+ levels in tissues, which lead to protection against metabolic syndrome.
Here, we show that CD38 expression and activity regulate cellular NAD+ levels and global acetylation of proteins, including SIRT1 substrates. We confirmed that quercetin is a CD38 inhibitor in vitro and in cells. Importantly, we demonstrate that apigenin is a novel inhibitor of CD38 in vitro and in vivo. Treatment of cells with apigenin or quercetin inhibits CD38 and promotes an increase in intracellular NAD+ levels. An increased NAD+ level decreases protein acetylation through sirtuin activation. Finally, treatment of obese mice with apigenin results in CD38 inhibition, higher NAD+ levels in the liver, and a decrease in protein acetylation. Apigenin treatment improves glucose homeostasis, glucose tolerance, and lipid metabolism in obese mice. Our results clearly demonstrate that CD38 is a novel therapeutic target for the treatment of metabolic diseases and that apigenin and quercetin as well as other CD38 inhibitors may be used to treat metabolic syndrome.
RESEARCH DESIGN AND METHODS
Reagents and antibodies.
All reagents and chemicals were from Sigma-Aldrich. Antibodies for human SIRT1, mouse SIRT1, p65, acetylated p53 (K382), phosphorylated AMP-activated protein kinase (AMPK) (Thr172), AMPK, and acetyl-lysine were from Cell Signaling Technology. Antibody against Nampt was from Bethyl Laboratories. Anti-human CD38 antibody was from R&D Biosystems, and anti-mouse CD38 was from Epitomics.
Cell culture.
A549 cells were kept in RPMI 1640 media supplemented with 10% FBS and penicillin/streptomycin (Invitrogen). Primary CD38 wild-type and knockout mouse embryonic fibroblasts (MEFs) were kept in Dulbecco’s modified Eagle’s medium supplemented with 10% FBS, penicillin/streptomycin, and glutamine. Primary MEFs were isolated form embryos (E18) from wild-type and CD38 knockout mice. Primary MEFs were used between passages 2 and 5. 293T and hepatocellular carcinoma (Hep)G2 cells were kept in Dulbecco’s modified Eagle’s medium supplemented with 10% FBS and penicillin/streptomycin.
Overexpression and small interfering RNA.
Full-length human CD38 was subcloned into a modified pIRES2–enhanced green fluorescent protein vector. For overexpression, 293T cells were transfected for 48 h with Lipofectamine 2000 (Invitrogen) following the manufacturer’s instructions.
For CD38 knockdown experiments, probe no. 2 of a TriFECTa kit against human CD38 was used (cat. no. HSC.RNAI.N001775.12.2; IDT). A549 cells were transfected with 40 nmol small interfering RNA (siRNA) duplex using Lipofectamine 2000 according to the manufacturer’s instructions.
Determination of CD38 activity.
Determination of CD38 activity in cells and tissues was performed as previously described (17). In vitro CD38 activity was measured using 0.1 unit of recombinant human CD38 (R&D Systems) in 0.25 mol/L sucrose and 40 mmol/L Tris-HCl (pH 7.4). The reaction was started by addition of 0.2 mmol/L substrate. Nicotinamide 1,N6-ethenoadenine dinucleotide was used to determine NAD+ase activity and nicotinamide guanine dinucleotide to determine cyclase activity. CD38 activity was expressed as arbitrary fluorescent units per minute (AFU/min).
NAD+ quantification.
NAD+ extraction and quantification was performed as previously described (17). In brief, cells were lysed by sonication in ice-cold 10% trichloroacetic acid, and then the trichloroacetic acid was extracted with two volumes of an organic phase consisting of 1,1,2-trichloro-1,2,2-trifluroethane and trioctylamine. NAD+ concentration was measured by means of an enzymatic cycling assay (18).
Determination of SIRT1 activity.
SIRT1 activity was measured with a fluorimetric assay (Enzo) as previously described (15). One unit of human recombinant SIRT1 was incubated with different concentrations of apigenin plus 100 μmol/L Fluor-de-Lys p53 tetra peptide and 100 μmol/L NAD+. Fluor-de-Lys developer was prepared according to the manufacturer’s recommendations and added to the reactions for 1 h. Fluorescence was read with an excitation of 360 nm and emission at 460 nm.
Mouse studies.
All mice used in this study were maintained in the Mayo Clinic Animal facility. All experimental protocols were approved by the institutional animal care and use committee at Mayo Clinic (protocol no. A33209), and all studies were performed according to the methods approved in the protocol. For generation of obese mice, twelve 20-week-old C57BL/6 mice were placed on a high-fat diet (AIN-93G, modified to provide 60% of calories from fat; Dyets) ad libitum for 4 weeks. Body weight was recorded weekly. After 4 weeks of high-fat diet, mice were randomly divided in two groups and injected daily with 100 mg/kg i.p. apigenin or vehicle for 7 consecutive days while remaining on the high-fat diet. During the treatments, food intake and body weight were monitored daily. There was no difference in these parameters between groups. For the glucose tolerance experiments, mice were housed for 24 h without food, but with water ad libitum, and challenged with one dose of 1.5 g/kg i.p. dextrose. Area under the curve was calculated by the net incremental method (with baseline) and presented as incremental area under the curve.
Gene expression analysis.
RNA from flash-frozen liver tissue was extracted with an RNeasy Mini Kit (Qiagen) according to the manufacturer’s instructions. cDNA was synthesized with the iSCRIP cDNA synthesis kit (BioRad) using 600 ng RNA. Quantitative RT-PCR reactions were performed using 1 µmol/L primers and LightCycler 480 SYBR Green Master (Roche) on a LightCycler 480 detection system (Roche). Calculations were performed by a comparative method (2-ΔCT) using 18S rRNA as an internal control. Primers were designed using the IDT software, and the primer sequences were as follows: long-chain acyl-CoA dehydrogenase (LCAD), forward (Fw) GGTGGAAAACGGAATGAAAGG, reverse (Rv) GGCAATCGGACATCTTCAAAG; medium-chain acyl-CoA dehydrogenase (MCAD), Fw TGTTAATCGGTGAAGGAGCAG, Rv CTATCCAGGGCATACTTCGTG; CPT1a, Fw AGACAAGAACCCCAACATCC, Rv CAAAGGTGTCAAATGGGAAGG; and 18S, Fw CGGCTACCACATCCAAGGAA, Rv GCTGGAATTACCGCGGCT.
Lipid treatment.
Cells were incubated with a mixture of oleic acid and palmitic acid in a 2:1 ratio in culture media supplemented with 1% fatty acid–free BSA (Sigma-Aldrich). Lipids were used at concentrations shown to induce steatosis but not apoptosis (15). Incubations with lipids were performed for 16–24 h.
Statistics.
Values are presented as means ± SEM of three to five experiments unless otherwise indicated. The significance of differences between means was assessed by ANOVA or two-tailed Student t test. A P value <0.05 was considered significant.
RESULTS
CD38 overexpression decreases NAD+ and promotes protein acetylation.
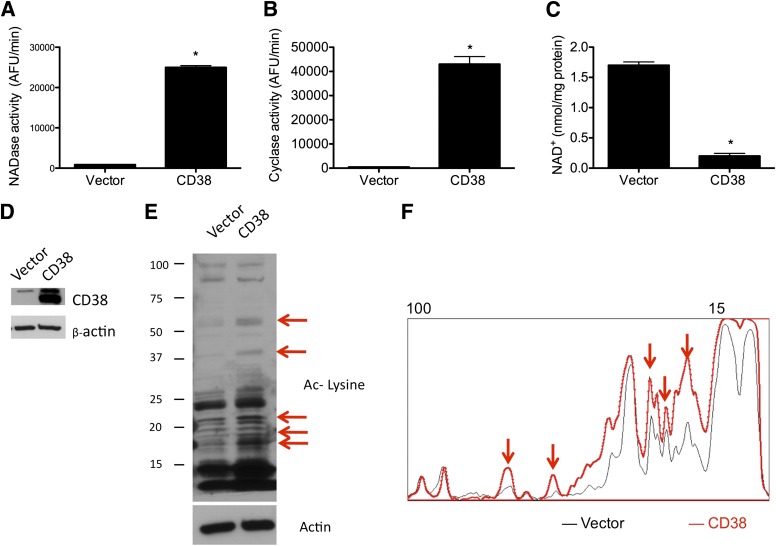
We have previously shown that CD38 is the primary NAD+ase in mammalian tissues (17). CD38-deficient mice have increased NAD+ levels in multiple tissues (5,17). To further characterize the role of CD38 in the regulation of NAD+-dependent cellular events, we studied the effect of CD38 manipulation in cells. We found that cells that overexpress CD38 show a significant increase in NAD+ase and ADP ribosyl cyclase activities (Fig. 1A and B) and a consistent decrease in intracellular NAD+ levels (Fig. 1C). Interestingly, we found that overexpression of CD38 also led to an increase in global protein acetylation (Fig. 1E). The pattern of acetylated proteins was analyzed by plotting an intensity profile of the lanes in the Western blots (Fig. 1F). It is worth noting that CD38 overexpression promotes changes in the level of acetylation of several proteins (red arrows in Fig. 1E and F), while other bands remain unchanged. This is consistent with the fact that only sirtuin deacetylases depend on NAD+ for their activity (8); histone deacetylases of classes I and II have a different enzymatic mechanism that does not require NAD+ (29).
FIG. 1.
CD38 overexpression decreases NAD+ and promotes protein acetylation in cells. 293T cells were transfected with empty vector or human CD38-coding vector. After 48 h, cells were harvested, and NAD+ase activity (A), ADP-ribosyl-cyclase activity (B), and total intracellular NAD+ levels (C) were measured in cell lysates. *P < 0.05, n = 3. D: Western blot for CD38 in 293T cells transfected with empty vector or with human CD38. E: Western blot showing total protein acetylation in cells transfected with empty vector or with human CD38. Anti–acetylated (Ac) lysine antibody was used. Red arrows highlight the main bands that showed variations in intensity. F: Intensity profile of the Western blot shown in E. Western blots were scanned and intensity profile was obtained using ImageJ. Red arrows correspond with intensity of the same bands shown in E.
CD38 downregulation increases NAD+ and decreases protein acetylation.
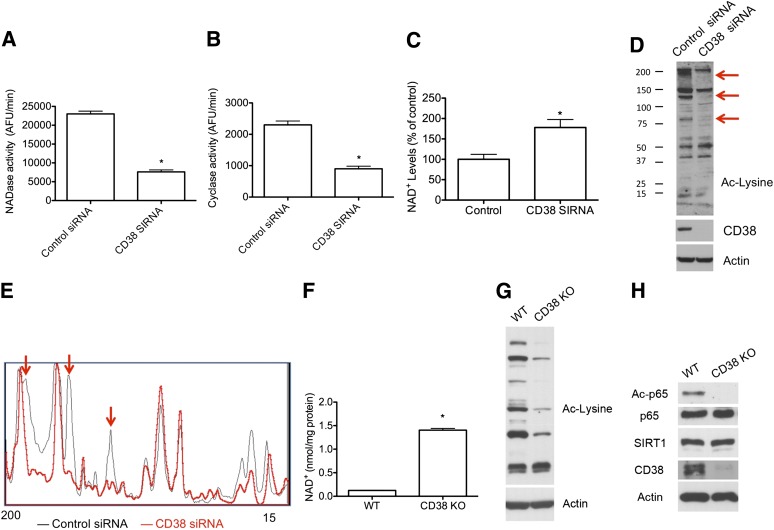
Next, we examined whether CD38 downregulation promotes the opposite effect on cellular NAD+ levels and global protein acetylation. This is of key relevance, since we (5) and other investigators (6,7) have shown that an increase in intracellular NAD+ levels protects against metabolic diseases and aging. We transfected cells with control or CD38 siRNA. Cells treated with CD38 siRNA had decreased NAD+ase and ADP ribosyl-cyclase activities (Fig. 2A and B) and a significant increase in intracellular NAD+ levels (Fig. 2C), consistent with the diminished CD38 NAD+ase activity. Moreover, the increase in NAD+ levels was accompanied by a decrease in global protein acetylation (Fig. 2D and E). Finally, we isolated primary MEFs from wild-type and CD38 knockout mice and measured NAD+ levels and protein acetylation. We found that CD38 knockout MEFs have increased NAD+ levels (Fig. 2F) and decreased global protein acetylation (Fig. 2G). We also analyzed p65/RelA acetylation at K310, a site that is an accepted target for cellular SIRT1 activity (7,11). We found that CD38 knockout MEFs show no detectable p65/RelA (K310) acetylation compared with wild-type cells, despite having similar total p65/RelA protein (Fig. 2H) and similar SIRT1 levels. This indicates that SIRT1 activity is increased in the CD38 knockout MEFs.
FIG. 2.
CD38 downregulation increases NAD+ and decreases protein acetylation in cells. A549 cells were transfected with a scrambled siRNA (control siRNA) or human CD38 siRNA. After 72 h, cells were harvested and NAD+ase activity (A), ADP-ribosyl-cyclase activity (B), and total intracellular NAD+ levels (C) were measured from cell lysates. *P < 0.05, n = 3. D: Western blot showing total protein acetylation in cells transfected with control siRNA or with human CD38 siRNA. Anti–acetylated (Ac) lysine antibody was used. Red arrows highlight the main bands that showed variations in intensity. E: Intensity profile of the Western blot shown in D. Western blots were scanned and intensity profile was obtained using Image J. Red arrows correspond with intensity of the same bands showed in D. F–H: Primary MEFs were purified and cultured from wild-type (WT) and CD38 knockout (KO) mice. F: Intracellular NAD+ levels (*P < 0.05, n = 3). G: Western blot from wild-type and CD38 knockout MEFs showing total protein acetylation in these cells. H: Representative Western blot in wild-type and CD38 knockout MEFs. Acetylated RelA/p65 (K310), total RelA/p65, SIRT1, CD38, and actin antibodies were used.
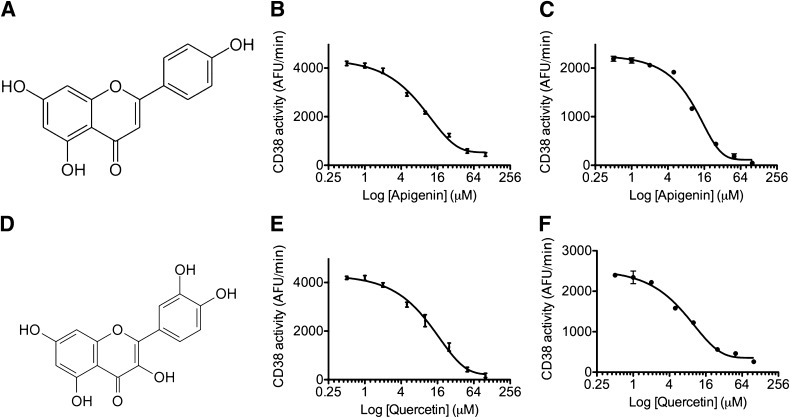
Apigenin and quercetin inhibit CD38 activity in vitro.
By use of high-throughput analysis to search for inhibitors of CD38, we found that several flavonoids, including quercetin and apigenin, inhibit CD38 in vitro. The complete screen will be published elsewhere. Recently, Kellenberger et al. (19) also published a list of flavonoids that act as CD38 inhibitors in vitro, many of which were also confirmed by our analysis. Quercetin was one of the compounds found by Kellenberger et al. (19) to inhibit CD38 in vitro. Apigenin, however, was demonstrated to be a novel CD38 inhibitor. We proceeded to further characterize these compounds in vitro and in cells.
The effect of apigenin and quercetin on CD38 activity in vitro was studied using the soluble ectodomain of human CD38 (17). We found that apigenin (Fig. 3A) inhibits in vitro CD38 activity with a half-maximal inhibitory concentration (IC50) of 10.3 ± 2.4 μmol/L for the NAD+ase activity and an IC50 of 12.8 ± 1.6 μmol/L for the ADP-ribosyl-cyclase activity (Fig. 3B and C). In vitro, quercetin (Fig. 3D) inhibits CD38 NAD+ase activity with an IC50 of 13.8 ± 2.1 μmol/L (Fig. 3E) and ADP-ribosyl-cyclase activity with an IC50 of 15.6 ± 3.5 μmol/L (Fig. 3F).
FIG. 3.
The flavonoids apigenin and quercetin inhibit CD38 activity in vitro. A: Chemical structure of apigenin. B and C: In vitro NAD+ase (B) and ADP-ribosyl-cyclase (C) activity using human recombinant-purified CD38 and different concentrations of apigenin. D: Chemical structure of quercetin. E and F: In vitro CD38 NAD+ase activity (E) and ADP-ribosyl-cyclase activity (F) using human recombinant-purified CD38 and different concentrations of apigenin. In all the measurements, compounds were used in the 0.5–100 μmol/L concentration range. Each measurement was done by triplicate. Data points were fitted to a standard competitive inhibition curve using a nonlinear regression program (GraphPad Prism) to yield the IC50 value.
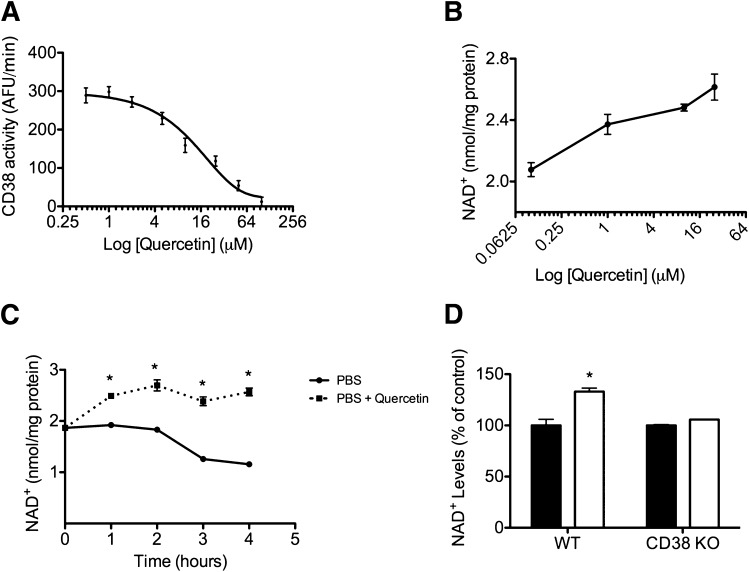
CD38 inhibition by quercetin and apigenin increases NAD+ levels in cells.
Although several flavonoids can inhibit purified recombinant CD38 in vitro (19), it is not known what effects these compounds have in cells. First, we measured the effect of quercetin on endogenous cellular CD38 activity. Inhibition of CD38 activity by quercetin in cells (IC50 = 16.4 ± 1.8 μmol/L) resembles the effect on the recombinant protein (Fig. 4A). Furthermore, we found that quercetin promotes an increase in intracellular NAD+ in a dose-dependent manner (Fig. 4B). To further confirm this effect, we incubated cells in PBS and measured intracellular NAD+ levels over time. We found that in untreated cells, NAD+ levels decrease with time (Fig. 4C), probably as a result of the removal of NAD+ precursors from the culture media. However, when the cells were treated with quercetin, NAD+ levels were stable over time, suggesting that inhibition of CD38 is enough to maintain intracellular NAD+ levels in the absence of NAD+ precursors. Finally, in order to confirm that the effect of quercetin on cellular NAD+ levels was dependent on CD38, we measured NAD+ after incubation with quercetin in wild-type and CD38 knockout MEFs. We found that quercetin promotes an increase in NAD+ in the wild-type MEFs but does not further increase NAD+ levels in CD38 knockout MEFs (Fig. 4D), indicating that the effect of quercetin on NAD+ levels is CD38 dependent.
FIG. 4.
CD38 inhibition by quercetin increases NAD+ levels in cells. A: Endogenous CD38 NAD+ase activity was measured in protein lysates from A549 cells. Quercetin was used in the 0.5–100 μmol/L concentration range. Each measurement was done in triplicate. Data points were fitted to a standard competitive inhibition curve using a nonlinear regression program (GraphPad Prism) to yield the IC50 value. B: NAD+ dose-response curve in A549 cells treated with quercetin. Cells were incubated with quercetin for 6 h before NAD+ extraction. *P < 0.05, n = 3. C: NAD+ time course in A549 cells incubated in PBS (●) or in PBS plus quercetin (50 μmol/L) (■). *P < 0.05, n = 3. D: Intracellular NAD+ levels in wild-type (WT) and CD38 knockout (KO) MEFs treated with vehicle (control) (■) or with quercetin (50 μmol/L) (□) for 6 h. NAD+ levels were expressed as percent of change with respect to the control for both cells. Total NAD+ levels were significantly higher in CD38 knockout MEFs. (See Fig. 2F.) *P < 0.05, n = 3.
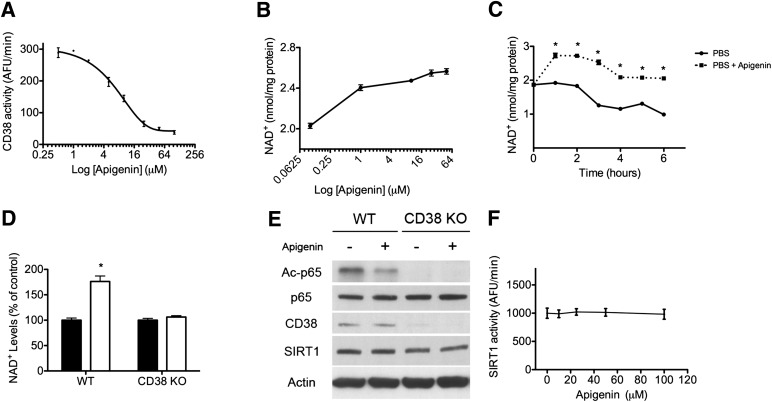
Apigenin also inhibits CD38 activity in cells (Fig. 5A). In fact, inhibition of cellular CD38 was very similar to that observed with the purified recombinant protein (IC50 = 14.8 ± 2.2 μmol/L in cells and 10.3 ± 2.4 μmol/L in vitro). Apigenin treatment increased NAD+ levels in cells in a dose-dependent manner (Fig. 5B) and protected against NAD+ depletion when cells were incubated in PBS (Fig. 5C). Furthermore, treatment of CD38 knockout MEFs with apigenin had no effect on NAD+ levels (Fig. 5D), indicating that the effect of apigenin on NAD+ levels is mediated by CD38. Interestingly, we found that treatment of wild-type MEFs with apigenin decreased acetylation of RelA/p65 (Fig. 5E). However, in the CD38 knockout MEFs, RelA/p65 acetylation levels were undetectable in the control, and therefore we could not determine the effect of apigenin (Fig. 5E). These results are consistent with the effect of apigenin in intracellular NAD+ levels in these cells (Fig. 5D). Quercetin has been shown to activate SIRT1 in vitro (30), suggesting that it may activate SIRT1 activity by two different mechanisms. To rule out a possible direct effect of apigenin on SIRT1 activity, we measured in vitro recombinant SIRT1 activity in the presence of different concentrations of apigenin. We observed that apigenin does not activate SIRT1 directly (Fig. 5F). Combined, these results clearly demonstrate that apigenin inhibits CD38 in cells and by doing so promotes an increase in NAD+ levels that stimulates NAD+-dependent deacetylases.
FIG. 5.
CD38 inhibition by apigenin increases NAD+ and decreases protein acetylation in cells. A: Endogenous CD38 NAD+ase activity was measured in protein lysates from A549 cells. Apigenin was used in the 2.5–100 μmol/L concentration range. Each measurement was done in triplicate. Data points were fitted to a standard competitive inhibition curve using a nonlinear regression program (GraphPad Prism) to yield the IC50 value. B: NAD+ dose-response curve in A549 cells treated with apigenin. Cells were incubated with apigenin for 6 h before NAD+ extraction. C: NAD+ time course in A549 cells incubated in PBS (●) or in PBS plus 25 μmol/L apigenin (■) (*P < 0.05, n = 3). D: Intracellular NAD+ levels in wild-type (WT) and CD38 knockout (KO) MEFs treated with vehicle (control) (■) or with apigenin (25 μmol/L) (□) for 6 h. NAD+ levels were expressed as percent change with respect to the control for both cells. Total NAD+ levels were significantly higher in CD38 knockout MEFs. (See Fig. 2F.) *P < 0.05, n = 3. E: Western blot of wild-type and CD38 knockout MEFs that were treated with vehicle or apigenin as described in D. Samples were immunoblotted for acetylated (Ac)-p65 (K310), total p65, CD38, SIRT1, and actin. F: In vitro SIRT1 activity using recombinant-purified human SIRT1. SIRT1 activity was measured in the presence of different concentrations of apigenin (0–100 μmol/L). Activity was determined in the linear portion of the reaction.
CD38 inhibition by apigenin increases NAD+ and decreases protein acetylation in mice.
Apigenin and quercetin have been shown to ameliorate atherosclerosis in mice (25) and to protect against lipid accumulation in cells (25). However, the mechanism of action has not been elucidated. In fact, while most flavonoids activate AMPK, which could explain some of the metabolic effects observed, apigenin is a very poor AMPK activator (25).
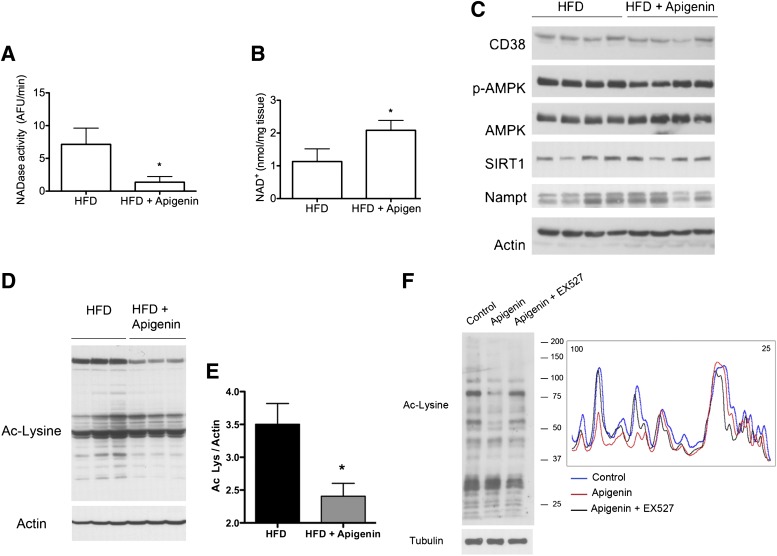
Based on the results obtained in cells, we tested whether apigenin inhibits CD38 in vivo using a model of high-fat diet–induced obesity (5,15). We fed adult mice a high-fat diet for 4 weeks. After, we divided the mice randomly in two groups. Each group was injected daily with apigenin (100 mg/kg) or vehicle (DMSO) for a week. We found that mice that had been injected with apigenin had decreased CD38 activity in the liver (Fig. 6A), which correlated with an increase in hepatic NAD+ levels compared with control mice (Fig. 6B). We then examined whether the apigenin treatment had an effect on the level of expression of several proteins involved in NAD+ metabolism. As shown in Fig. 6C, we found no significant differences in the expression of CD38, SIRT1, or Nampt, the primary regulator of the NAD+ salvage pathway. Furthermore, we did not see any changes in phosphorylation or total levels of AMPK (Fig. 6C). However, when we analyzed the liver samples using an acetyl-lysine antibody, we found that the apigenin treatment resulted in a statistically significant decrease in global acetylation of proteins (Fig. 6D and E).
FIG. 6.
CD38 inhibition by apigenin increases NAD+ and decreases protein acetylation in vivo. A–E: Mice were fed a high-fat diet (HFD) for 4 weeks and then split in two groups. One group was injected with apigenin (100 mg/kg i.p.) and the other with vehicle (DMSO) with a single dose daily for 1 week. A: CD38 activity in the liver at the end of the treatment with apigenin (*P < 0.05, n = 6 animals per group). B: NAD+ levels in the liver after the treatment (*P < 0.05, n = 6 animals per group). C: At the end of the treatment, liver samples were obtained and immunoblotted for CD38, phosphorylated (p)-AMPK (Thr172), AMPK, SIRT1, Nampt, and actin. D: Liver samples were immunoblotted for global acetylation of proteins using an anti–acetylated (Ac) lysine (Lys) antibody. Western blots were scanned and an intensity profile was obtained using Image J. The area under the curve is shown. (*P < 0.05, n = 3 per group.) F: Human HepG2 cells were incubated with vehicle (DMSO), apigenin (25 μmol/L), or apigenin plus EX527 (10 μmol/L) for 6 h. Cell lysates were immunoblotted for acetylated lysine to determine total protein acetylation levels (left panel). The intensity profile of the Western blot was obtained using Image J (right panel).
To determine the relevance of SIRT1 in the deacetylation of proteins triggered by apigenin treatment, we used human HepG2 cells: a well-accepted cellular model for studying hepatic cellular signaling (15,25,31). We found that treatment with apigenin decreases total protein acetylation—an effect that is lost in the presence of the SIRT1 inhibitor EX527 (Fig. 6F). Furthermore, treatment of HepG2 cells with apigenin decreased acetylation of p53 at K382 and also of RelA/p65 at K310: sites that are deacetylated by SIRT1 (Supplementary Fig. 1). This effect was reverted when cells were also incubated with the sirtuin inhibitor nicotinamide (Supplementary Fig. 1). Taken together, these results show that apigenin inhibits CD38 in vivo and is associated with increased NAD+ and decreased protein acetylation, likely through the activation of SIRT1.
CD38 inhibition by apigenin improves glucose homeostasis in vivo and promotes fatty acid oxidation in the liver.
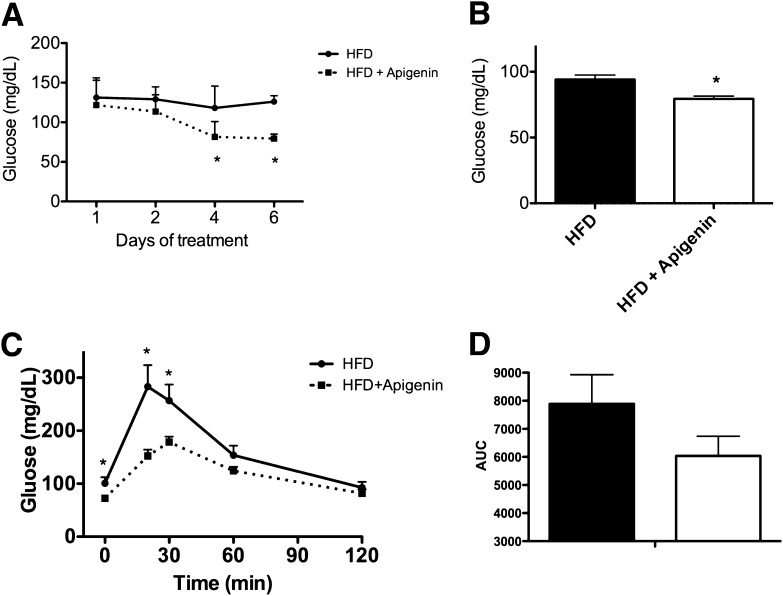
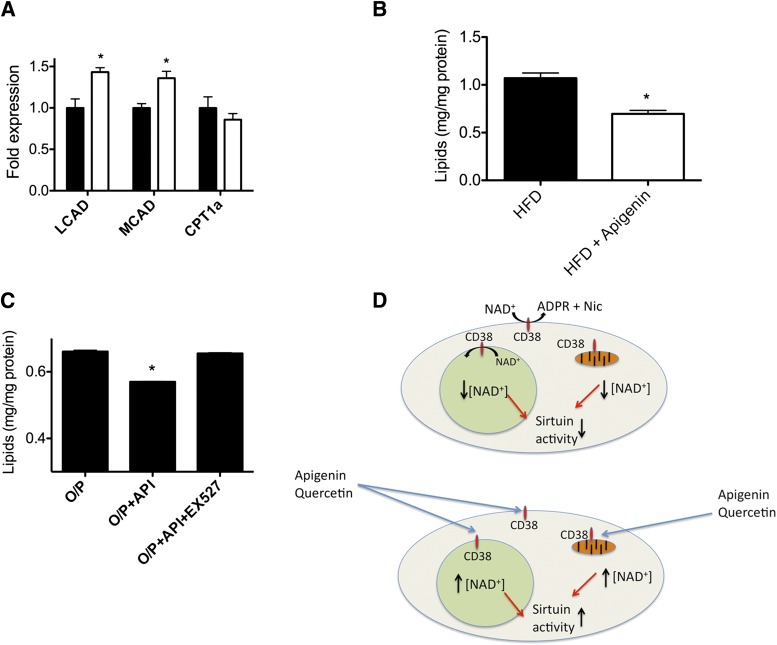
Finally, we tested whether apigenin protects against high-fat diet–induced hyperglycemia. We found that after 4 days of treatment, the mice treated with apigenin had significantly lower blood glucose levels compared with the control mice (Fig. 7A). Fasting blood glucose levels were also significantly lower after 1 week of treatment with apigenin (Fig. 7B). Moreover, we found that 1 week of treatment with apigenin was enough to improve glucose homeostasis in the mice (Fig. 7C and D). SIRT1 activation promotes fatty acid oxidation in the liver by inducing the expression of several enzymes involved in fatty acid and cholesterol metabolism (32). In fact, SIRT1 activation in the liver prevents liver steatosis (5,14,15). Mice treated with apigenin had increased expression of the enzymes MCAD and LCAD in the liver (Fig. 8A), suggesting that apigenin treatment enhanced fatty acid oxidation. We confirmed these data by measuring total triglyceride content in the liver. Indeed, we found that the mice treated with apigenin had lower triglyceride levels in the liver compared with control mice (Fig. 8B), showing that apigenin promotes hepatic lipid oxidation. To further confirm this finding, we measured lipid accumulation in cells, using an in vitro model of hepatic steatosis (15). We found that apigenin decreases lipid accumulation in cells and that this effect was completely blocked by the SIRT1 inhibitor EX527 (Fig. 8C). Together, these results show that inhibition of CD38 by apigenin, and perhaps by other flavonoids, constitutes a pharmacological approach to activate sirtuins and treat high-fat diet–induced metabolic disorders. Furthermore, our results point to CD38 as a novel pharmacological target to treat metabolic diseases.
FIG. 7.
CD38 inhibition by apigenin improves glucose homeostasis in vivo and improves lipid metabolism in the liver. Mice were fed a high-fat diet (HFD) for 4 weeks and then split in two groups. One group was injected with apigenin (100 mg/kg i.p.) and the other with vehicle (DMSO) with a single dose daily for 1 week. A: Blood glucose levels were measured during the week of apigenin treatment in ad libitum feeding conditions (*P < 0.05, n = 6 per group). ●, HFD; ■, HFD plus apigenin. B: Blood glucose levels were measured after 24 h of fasting on day 7 of treatment with apigenin (*P < 0.05, n = 6 per group). C: Glucose tolerance test in mice after 7 days of treatment with apigenin (■) or vehicle (●) (*P < 0.05, n = 6 per group). D: Area under the curve (AUC) calculated for the glucose tolerance test shown in C. ■, HFD; □, HFD plus apigenin.
FIG. 8.
CD38 inhibition by apigenin promotes fatty acid oxidation in the liver. A: mRNA expression of lipid oxidation markers LCAD, MCAD, and CPT1a in the liver measured by RT-PCR in mice treated with apigenin (□) or vehicle (■) (*P < 0.05, n = 6 per group). B: Total triglyceride (TG) content in the liver of mice treated with apigenin or vehicle (*P < 0.05, n = 6 per group). HFD, high-fat diet. C: Total triglycerides levels in HepG2 cells incubated with 0.5 mmol/L oleate/palmitate (O/P) (2:1 ratio), oleate/palmitate plus 25 μmol/L apigenin (API), or oleate/palmitate plus apigenin plus 10 μmol/L EX527 (*P < 0.05, n = 3). D: Working model for apigenin and quercetin effect on CD38. In cells, CD38 maintains low intracellular NAD+ levels with a consequent low sirtuin activity. The inhibition of CD38 in different subcellular compartments leads to an increase in NAD+ levels, which becomes available for sirtuin activation. We propose that the effect of apigenin will activate nuclear and cytoplasmic and also mitochondrial sirtuins, where CD38 has been shown to be expressed.
DISCUSSION
The alarming expansion of metabolic diseases has triggered a considerable effort in the development of pharmacological strategies to prevent and treat them. In this regard, the study of sirtuins and specifically SIRT1 has become of great relevance due to the many beneficial effects of their action (8,9). In fact, how to achieve SIRT1 activation in vivo is a subject of intense investigation. One of the strategies to achieve such activation has been the use of drugs that directly target SIRT1. Resveratrol (16) and SRT1720 (33) are two of the early SIRT1-activating compounds that improve metabolism and protect against metabolic disorders, although there is a debate about their mechanism of action (34–36). Another mechanism to achieve SIRT1 activation in vivo is to raise intracellular levels of NAD+ either by increased synthesis or diminished degradation (5–7,18). Previously, we have shown that the enzyme CD38 is the principal regulator of intracellular NAD+ levels in mammalian tissues (17). In fact, we were the first to show that increasing NAD+ levels by deletion of CD38 protects against diet-induced obesity through SIRT1 activation (5). Other research groups later confirmed the importance of NAD+ in the prevention of metabolic diseases. Yoshino et al. (7) showed that administration of nicotinamide mononucleotide (a NAD+ precursor) to mice protects against high-fat diet–induced metabolic disorders. Bai et al. (6) obtained similar results using PARP1 knockout mice. Taken together, the evidence shows that pharmacological interventions that increase NAD+ are a promising avenue for treating metabolic disorders. However, the mechanism by which cellular NAD+ is increased may have different long-term outcomes. We followed survival of wild-type, CD38 knockout, and PARP1 knockout mice fed a high-fat diet. Preliminary studies with small numbers of mice suggest that CD38 knockout mice have increased average and maximum life span compared with wild-type mice when they are fed a high-fat diet. However, in the PARP1 knockout mice, which also have increased cellular NAD+ levels (6), the outcome was opposite this (Supplementary Fig. 2), with the PARP1 knockout mice having a decreased life span compared with the wild-type mice. This difference in survival could be explained by the fact that PARP1 is involved in genomic stability (37) and DNA repair both in the nucleus (37) and in mitochondria (38,39). This suggests that although CD38 and PARP1 knockout mice have similar protection against metabolic disorders, they may have distinct effects on longevity.
Here, we describe for the first time that the flavonoid apigenin is a CD38 inhibitor, and both apigenin and quercetin promote changes in intracellular NAD+ levels. This increase in NAD+ levels leads to changes in protein acetylation likely due to an increase in sirtuin activity. Furthermore, we show that apigenin improves glucose homeostasis and reduces lipid content in the liver in a model of high-fat diet–induced obesity. Our results suggest that lipid oxidation is increased by a SIRT1-dependent mechanism. However, it could also happen that fatty acid synthesis or export is altered, since SIRT1 has been shown to regulate both processes (40,41). Our results demonstrate that CD38 is a promising pharmacological target to promote sirtuin actions and to treat metabolic diseases.
Flavonoids, including apigenin and quercetin, have broad beneficial effects (20). These two flavonoids ameliorate atherosclerosis in mouse genetic models (25). Although some of the beneficial effects of flavonoids on metabolism are believed to be AMPK mediated (25), this has not been clearly elucidated. Indeed, apigenin is a very weak AMPK activator in vivo (25), which suggests an additional mechanism of action. Our findings provide mechanistic evidence that flavonoids can promote an increase in NAD+ levels through inhibition of CD38, resulting in changes in protein acetylation, most likely through stimulation of SIRT1 (Fig. 8D). Although we show here that CD38 inhibition affects SIRT1 activity, it is likely that other sirtuins will also be stimulated by CD38 inhibition. Interestingly, CD38 is also present and active in the mitochondria (42,43), where it may regulate mitochondrial NAD+ levels and mitochondrial sirtuin activity.
It is likely that, similar to what happens with many other natural compounds, apigenin and quercetin have other cellular targets besides CD38. However, we clearly show that the increase in cellular NAD+ levels promoted by these compounds depends on CD38. More importantly, our findings support the idea that pharmacological inhibition of CD38 can be achieved as a strategy to treat obesity and obesity-related diseases. Further research will help to develop highly selective CD38 inhibitors that may be used as an approach to treat metabolic syndrome in humans.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported in part by grants from the American Federation for Aging Research and from the Mayo Foundation; by the Strickland Career Development Award; by the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health (NIH), grant DK-084055; by Mayo-UOFM Decade of Discovery Grant 63-01; and by Minnesota Obesity Council Grant DK-50456-15. D.A.S. is supported by grants from the NIH/National Institute on Aging, the Juvenile Diabetes Research Foundation, the United Mitochondrial Disease Foundation, and the Glenn Foundation for Medical Research. C.E. is supported by American Heart Association postdoctoral fellowship award 11POST7320060 and A.P.G. by a fellowship from the Portuguese Foundation for Science and Technology (SFRH/BD/44674/2008).
E.N.C. and M.T.B. are inventors in a patent for CD38 and obesity (U.S. patent no. 8143014). E.N.C. and D.A.S. are inventors on a provisional patent for apigenin as a CD38 inhibitor to treat metabolic syndrome. D.A.S. is a consultant for Sirtris, a GlaxoSmithKline company aiming to develop medicines that target sirtuins. No other potential conflicts of interest relevant to this article were reported.
C.E. measured CD38 activity, measured effect of compounds in NAD+ levels, evaluated the effect of CD38 and CD38 inhibitors on protein acetylation, performed in vivo experiments, analyzed tissue samples, performed the lipid measurements, wrote the manuscript, designed experiments, discussed and analyzed data, and corrected the manuscript. V.N. measured CD38 activity, evaluated the effect of CD38 and CD38 inhibitors on protein acetylation, performed in vivo experiments, analyzed tissue samples, performed the longevity studies, designed experiments, discussed and analyzed data, and corrected the manuscript. N.L.P. performed the library screening, performed qPCR, designed experiments, discussed and analyzed data, and corrected the manuscript. V.C. measured CD38 activity and evaluated the effect of CD38 and CD38 inhibitors on protein acetylation. A.P.G. performed qPCR. M.T.B. performed the longevity studies. L.O. analyzed tissue samples. T.A.W. measured CD38 activity. D.A.S. and E.N.C. developed the original idea, designed experiments, discussed and analyzed data, and corrected the manuscript. E.N.C. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank Caroline Shamu and the staff at Harvard’s Institute of Chemistry and Cell Biology facility, where the small-molecule screen was conducted.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db12-1139/-/DC1.
REFERENCES
- 1.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA 2004;291:2847–2850 [DOI] [PubMed] [Google Scholar]
- 2.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 2012;70:3–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spiegel AM, Alving BM. Executive summary of the Strategic Plan for National Institutes of Health Obesity Research. Am J Clin Nutr 2005;82(Suppl.):211S–214S [DOI] [PubMed] [Google Scholar]
- 4.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet 2005;365:1415–1428 [DOI] [PubMed] [Google Scholar]
- 5.Barbosa MT, Soares SM, Novak CM, et al. The enzyme CD38 (a NAD glycohydrolase, EC 3.2.2.5) is necessary for the development of diet-induced obesity. FASEB J 2007;21:3629–3639 [DOI] [PubMed] [Google Scholar]
- 6.Bai P, Cantó C, Oudart H, et al. PARP-1 inhibition increases mitochondrial metabolism through SIRT1 activation. Cell Metab 2011;13:461–468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoshino J, Mills KF, Yoon MJ, Imai S. Nicotinamide mononucleotide, a key NAD(+) intermediate, treats the pathophysiology of diet- and age-induced diabetes in mice. Cell Metab 2011;14:528–536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haigis MC, Sinclair DA. Mammalian sirtuins: biological insights and disease relevance. Annu Rev Pathol 2010;5:253–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chalkiadaki A, Guarente L. Sirtuins mediate mammalian metabolic responses to nutrient availability. Nat Rev Endocrinol 2012;8:287–296 [DOI] [PubMed] [Google Scholar]
- 10.Vaziri H, Dessain SK, Ng Eaton E, et al. hSIR2(SIRT1) functions as an NAD-dependent p53 deacetylase. Cell 2001;107:149–159 [DOI] [PubMed] [Google Scholar]
- 11.Yeung F, Hoberg JE, Ramsey CS, et al. Modulation of NF-kappaB-dependent transcription and cell survival by the SIRT1 deacetylase. EMBO J 2004;23:2369–2380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rodgers JT, Lerin C, Haas W, Gygi SP, Spiegelman BM, Puigserver P. Nutrient control of glucose homeostasis through a complex of PGC-1alpha and SIRT1. Nature 2005;434:113–118 [DOI] [PubMed] [Google Scholar]
- 13.Imai S, Armstrong CM, Kaeberlein M, Guarente L. Transcriptional silencing and longevity protein Sir2 is an NAD-dependent histone deacetylase. Nature 2000;403:795–800 [DOI] [PubMed] [Google Scholar]
- 14.Pfluger PT, Herranz D, Velasco-Miguel S, Serrano M, Tschöp MH. Sirt1 protects against high-fat diet-induced metabolic damage. Proc Natl Acad Sci USA 2008;105:9793–9798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Escande C, Chini CC, Nin V, et al. Deleted in breast cancer-1 regulates SIRT1 activity and contributes to high-fat diet-induced liver steatosis in mice. J Clin Invest 2010;120:545–558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baur JA, Pearson KJ, Price NL, et al. Resveratrol improves health and survival of mice on a high-calorie diet. Nature 2006;444:337–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aksoy P, White TA, Thompson M, Chini EN. Regulation of intracellular levels of NAD: a novel role for CD38. Biochem Biophys Res Commun 2006;345:1386–1392 [DOI] [PubMed] [Google Scholar]
- 18.Aksoy P, Escande C, White TA, et al. Regulation of SIRT 1 mediated NAD dependent deacetylation: a novel role for the multifunctional enzyme CD38. Biochem Biophys Res Commun 2006;349:353–359 [DOI] [PubMed] [Google Scholar]
- 19.Kellenberger E, Kuhn I, Schuber F, Muller-Steffner H. Flavonoids as inhibitors of human CD38. Bioorg Med Chem Lett 2011;21:3939–3942 [DOI] [PubMed] [Google Scholar]
- 20.Ross JA, Kasum CM. Dietary flavonoids: bioavailability, metabolic effects, and safety. Annu Rev Nutr 2002;22:19–34 [DOI] [PubMed] [Google Scholar]
- 21.Budhraja A, Gao N, Zhang Z, et al. Apigenin induces apoptosis in human leukemia cells and exhibits anti-leukemic activity in vivo. Mol Cancer Ther 2012;11:132–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hwang YP, Oh KN, Yun HJ, Jeong HG. The flavonoids apigenin and luteolin suppress ultraviolet A-induced matrix metalloproteinase-1 expression via MAPKs and AP-1-dependent signaling in HaCaT cells. J Dermatol Sci 2011;61:23–31 [DOI] [PubMed] [Google Scholar]
- 23.Caltagirone S, Rossi C, Poggi A, et al. Flavonoids apigenin and quercetin inhibit melanoma growth and metastatic potential. Int J Cancer 2000;87:595–600 [DOI] [PubMed] [Google Scholar]
- 24.Birt DF, Mitchell D, Gold B, Pour P, Pinch HC. Inhibition of ultraviolet light induced skin carcinogenesis in SKH-1 mice by apigenin, a plant flavonoid. Anticancer Res 1997;17:85–91 [PubMed] [Google Scholar]
- 25.Zang M, Xu S, Maitland-Toolan KA, et al. Polyphenols stimulate AMP-activated protein kinase, lower lipids, and inhibit accelerated atherosclerosis in diabetic LDL receptor-deficient mice. Diabetes 2006;55:2180–2191 [DOI] [PubMed] [Google Scholar]
- 26.Suou K, Taniguchi F, Tagashira Y, Kiyama T, Terakawa N, Harada T. Apigenin inhibits tumor necrosis factor α-induced cell proliferation and prostaglandin E2 synthesis by inactivating NFκB in endometriotic stromal cells. Fertil Steril 2011;95:1518–1521 [DOI] [PubMed] [Google Scholar]
- 27.Kang OH, Lee JH, Kwon DY. Apigenin inhibits release of inflammatory mediators by blocking the NF-κB activation pathways in the HMC-1 cells. Immunopharmacol Immunotoxicol 2011;33:473–479 [DOI] [PubMed] [Google Scholar]
- 28.Lee JH, Zhou HY, Cho SY, Kim YS, Lee YS, Jeong CS. Anti-inflammatory mechanisms of apigenin: inhibition of cyclooxygenase-2 expression, adhesion of monocytes to human umbilical vein endothelial cells, and expression of cellular adhesion molecules. Arch Pharm Res 2007;30:1318–1327 [DOI] [PubMed] [Google Scholar]
- 29.Haberland M, Montgomery RL, Olson EN. The many roles of histone deacetylases in development and physiology: implications for disease and therapy. Nat Rev Genet 2009;10:32–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Howitz KT, Bitterman KJ, Cohen HY, et al. Small molecule activators of sirtuins extend Saccharomyces cerevisiae lifespan. Nature 2003;425:191–196 [DOI] [PubMed] [Google Scholar]
- 31.Li Y, Xu S, Giles A, et al. Hepatic overexpression of SIRT1 in mice attenuates endoplasmic reticulum stress and insulin resistance in the liver. FASEB J 2011;25:1664–1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rodgers JT, Puigserver P. Fasting-dependent glucose and lipid metabolic response through hepatic sirtuin 1. Proc Natl Acad Sci USA 2007;104:12861–12866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Milne JC, Lambert PD, Schenk S, et al. Small molecule activators of SIRT1 as therapeutics for the treatment of type 2 diabetes. Nature 2007;450:712–716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pacholec M, Bleasdale JE, Chrunyk B, et al. SRT1720, SRT2183, SRT1460, and resveratrol are not direct activators of SIRT1. J Biol Chem 2010;285:8340–8351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Borra MT, Smith BC, Denu JM. Mechanism of human SIRT1 activation by resveratrol. J Biol Chem 2005;280:17187–17195 [DOI] [PubMed] [Google Scholar]
- 36.Price NL, Gomes AP, Ling AJ, et al. SIRT1 is required for AMPK activation and the beneficial effects of resveratrol on mitochondrial function. Cell Metab 2012;15:675–690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Anders CK, Winer EP, Ford JM, et al. Poly(ADP-Ribose) polymerase inhibition: “targeted” therapy for triple-negative breast cancer. Clin Cancer Res 2010;16:4702–4710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rossi MN, Carbone M, Mostocotto C, et al. Mitochondrial localization of PARP-1 requires interaction with mitofilin and is involved in the maintenance of mitochondrial DNA integrity. J Biol Chem 2009;284:31616–31624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lapucci A, Pittelli M, Rapizzi E, Felici R, Moroni F, Chiarugi A. Poly(ADP-ribose) polymerase-1 is a nuclear epigenetic regulator of mitochondrial DNA repair and transcription. Mol Pharmacol 2011;79:932–940 [DOI] [PubMed] [Google Scholar]
- 40.Xu F, Gao Z, Zhang J, et al. Lack of SIRT1 (Mammalian Sirtuin 1) activity leads to liver steatosis in the SIRT1+/- mice: a role of lipid mobilization and inflammation. Endocrinology 2010;151:2504–2514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yamazaki Y, Usui I, Kanatani Y, et al. Treatment with SRT1720, a SIRT1 activator, ameliorates fatty liver with reduced expression of lipogenic enzymes in MSG mice. Am J Physiol Endocrinol Metab 2009;297:E1179–E1186 [DOI] [PubMed] [Google Scholar]
- 42.Yamada M, Mizuguchi M, Otsuka N, Ikeda K, Takahashi H. Ultrastructural localization of CD38 immunoreactivity in rat brain. Brain Res 1997;756:52–60 [DOI] [PubMed] [Google Scholar]
- 43.Liang M, Chini EN, Cheng J, Dousa TP. Synthesis of NAADP and cADPR in mitochondria. Arch Biochem Biophys 1999;371:317–325 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.