Abstract
Objective
To estimate the prevalence of infertility using a current duration approach for comparison with a traditional constructed measure.
Design
Cross-sectional survey.
Setting
National Survey of Family Growth, United States, 2002.
Participants
A nationally-representative sample of females aged 15–44 years.
Interventions
None
Main Outcome Measure(s)
Infertility prevalence estimated by two approaches: 1) a constructed measure derived from questions on sexual activity, contraception, relationship status, and pregnancy, and 2) a measure based on estimated time-to-pregnancy (TTP) derived from the respondents’ current duration of pregnancy attempt (i.e., current duration approach). Associations with self-reported descriptive characteristics using weighted logistic regression or parametric survival models for each respective approach.
Results
Infertility prevalence was approximately twofold higher using the current duration approach (15.5%; 95% CI: 8.6, 27.5) versus the constructed measure (7.0%; 95% CI: 6.2, 7.8). Both methods identified similar patterns of increasing age, lower education, nulliparity, and history of gynecologic disorders as being associated with measures of impaired fecundity, while opposing patterns were seen for racial/ethnic identification and poverty status.
Conclusions
Infertility prevalence based on a current duration approach was consistent with other U.S. prospective cohort studies with preconception enrollment. These findings underscore the importance of definition and methodologic approach for estimating the prevalence of infertility.
Keywords: Current duration, fecundity, infertility, epidemiology, reproduction
INTRODUCTION
Infertility, typically defined as the inability of couples to become pregnant after 12 months of regular unprotected sexual intercourse (1), has implications for health status beyond the absence of a timely conceived pregnancy. For example, a longer time-to-pregnancy (TTP) is reported in some studies to increase the risk of adverse pregnancy outcomes (2) and gravid diseases (3), which in turn may influence the development of later onset adult diseases as conceptualized in the ovarian dysgenesis syndrome paradigm (4). From a population perspective, the impact of infertility is considerable ranging from changes in demographic milestones (5), social and economic consequences (6), and health disparities (7). Despite the importance of understanding infertility on an individual and population-level, our knowledge of its descriptive and analytical epidemiology in the United States is limited.
An important methodologic consideration underlying infertility research is the operational definition used, which further impacts interpretation of results and translation of such information to both clinicians and the general public (8). Previous research has shown infertility prevalence varies inversely with the stringency of criteria used for defining infertility (9;10). Choice of definition also translates into wide variation in prevalence estimates across populations ranging between 3.3–26.4% for current infertility and between 2.6–31.8% for lifetime infertility (11). In addition, recognition of the marked demographic shifts in the U.S. population impacts the descriptive epidemiology of infertility. These shifts include: 1) an increase in births to non-married women (37% in 2002 to 46% in 2006–2010); 2) an increase in cohabiting couples (3% in 1982 to 11% in 2006–2010) and a corresponding decline in first marriages (44% in 1982 to 36% in 2006–2010); 3) an increase in mean age at first birth (21.4 in 1970 to 24.9 in 2000); and 4) an increase in surgical sterilization procedures (15.9% in 1965 to 41.1% in 1995) (12–15). Thus, our understanding of the magnitude and scope of infertility requires consideration of both definition and changing sociodemographic context of the referent and study population.
To our knowledge, the incidence of infertility in the United States is unknown. Available albeit limited data from prospective cohort studies in the United States with preconception enrollment of women suggests that approximately 12–18% of women are not pregnant within 12 observed months or cycles of trying (16–18). Such cohort designs are considered the gold standard for estimating the percentage not pregnant after 12 months or cycles; however, they are not necessarily designed to be nationally representative of reproductive-aged individuals in the United States. In light of this critical data gap, population-based prevalence data become paramount for monitoring infertility, such as data collection in the National Survey of Family Growth (NSFG). The NSFG utilizes a cross-sectional design with representative sampling of reproductive-aged U.S. residents and relies on a measure of infertility constructed from respondents’ answers to questions on relationship status and duration, sexual activity, contraceptive use, and pregnancy in the past 12 months. Using this measure, the prevalence of current infertility is estimated to be 7.4% among married women in the United States (19). This figure is appreciably lower than incident infertility estimated from prospective studies in the United States (range: 12–18%) and excludes unmarried couples from estimation procedures. To date, limited attention has been given to alternative approaches for estimating the prevalence of infertility in the United States beyond the constructed measure used in the NSFG.
With global concerns about declining fecundity (20), defined as the biologic capacity of males and females to reproduce, several authors have called for the monitoring of fecundity with more direct measures such as time-to-pregnancy (TTP) (21;22) or the current duration design (23–25). The utility of TTP for assessing fecundity from prospective and retrospective studies has been well described (26–28). In comparison, the current duration design estimates a TTP-like distribution from a cross-sectional sample and relies on a few simple questions aimed at directly identifying women currently at risk for pregnancy (i.e., sexually active, non-contracepting, non-pregnant) at the time of interview and their time spent at risk (i.e., time elapsed from stopping contraception, or beginning of a pregnancy attempt, to inclusion into the study). Presently, two nationally-representative cross-sectional studies of women in Denmark, Germany, and Northern Italy (24) and France (25) have applied a current duration approach. The prevalence of 12-month infertility in the French population was 24%. Most notably, the current duration approach is advantageous in that inferences can be obtained for all women at risk for pregnancy, regardless of pregnancy intentions, and relies on direct querying of respondents, thereby eliminating the need for a constructed measure.
Thus, our objective was to apply a current duration approach to estimate the prevalence of 12-month infertility among a general population in the United States using the 2002 NSFG for comparison with the traditional constructed measure. A second study aim was to assess whether the two approaches identify similar at-risk subgroups in relation to the purported sociodemographic and reproductive history risk factors for infertility.
MATERIALS AND METHODS
Design and study population
The study population comprises 7, 643 females aged 15–44 years who participated in the 2002 cycle of the National Survey of Family Growth (NSFG) (29). The target population for the study population was all reproductive-aged women in the United States; thus, respondents were selected based on a multistage area probability sample from 120 areas across the country. Teenagers and black and Hispanic adults were oversampled in this survey. The overall response rate for females aged 15–44 years was 80 percent. Details of the survey and study design have been described previously (19). The NSFG survey was reviewed and approved by Research Ethics Review Board of the Centers for Disease Control and Prevention (CDC) and National Center for Health Statistics (NCHS), and a similar board at the contracting organization, the University of Michigan (19).
Data collection and operational definitions
Data were collected through in-person interviews conducted in households across the United States by trained interviewers using Computer-Assisted Interviewing (CAI) techniques. Female respondents provided information on sociodemographic, family planning, reproductive history, birth intentions, sexual activity, and access to health services. Audio Computer Assisted Self-Interviewing (ACASI) techniques were used to capture sensitive information related to health, pregnancy history, substance use, sexual behavior and practices, sexual orientation, sexually transmitted diseases, income, and public assistance.
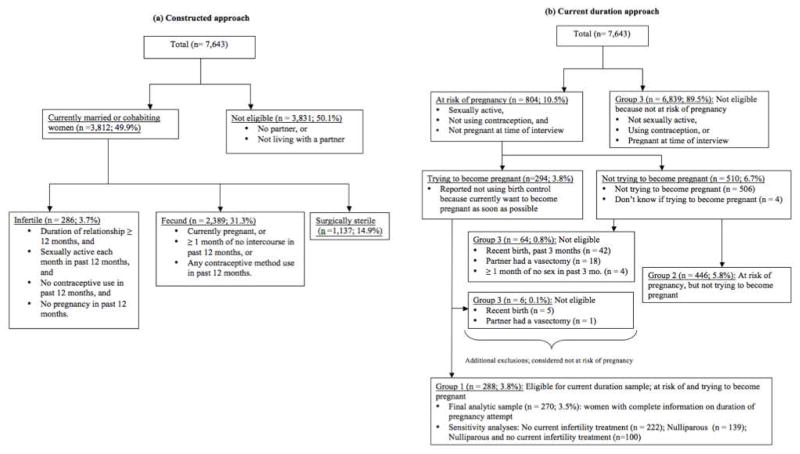
For this study, the following operational definitions were used to define infertility prevalence consistent with the format used by the NSFG for the constructed measure (19) and the current duration approach (30). Since 1982, the constructed measure in the NSFG has been derived from responses to questions on contraceptive use, surgical sterilization, sexual activity, relationship status, duration of partnership, and current or recent pregnancy (Figure 1a) (31). All married or cohabiting respondents (n = 3,812; 49.9% of total) were classified as infertile if they had been in a continuous relationship for 12 months or more with no use of contraception, but sexually active every month for the past 12 months, and did not have a pregnancy (n = 286; 3.7% of total). Women were classified as fecund if they were currently pregnant, regardless of duration of pregnancy attempt, or had used contraception or had not been sexually active for at least 1 month in the last 12 months (n = 2,389; 31.9% of total). All women who reported surgical sterilization were grouped separately (n = 1,137; 14.9% of total), but included as part of the denominator. Women not living with a current partner were excluded from analysis (n = 3,831; 51.1% of total). For this paper, we included both married and cohabiting women unlike earlier approaches restricting to married women only (31).
Figure 1.
Flow chart of women included in the (a) traditional NSFG constructed measure classified by outcome, and (b) the current duration approach classified by eligibility for inclusion in the analysis.
For the current duration approach, we utilized two questions added to the NSFG in 2002 that directly assessed the duration of the respondent’s current pregnancy attempt (Figure 1b). Women who were not using a method of contraception nor pregnant, but were sexually active at the time of interview (n=804 potentially eligible respondents, 10.5%) were asked, “Is the reason you are not using a method of birth control now because you, yourself, want to become pregnant as soon as possible?” Women who responded “Yes” were then asked “How long have you been trying to become pregnant? (number of months or years)”, which was used to determine their current duration of pregnancy attempt (i.e., current duration) in months. Regardless of pregnancy intentions, women were not considered at risk for pregnancy if they had a live or stillbirth within the past 3 months, reported one or more months without intercourse in the past 3 months, or if their current partner had a vasectomy. Women were not included in the current duration analysis if they were not at risk of pregnancy (n=6909, 90.4% of total) or were at risk, but not currently trying to become pregnant (n=510, 6.7% of total). Thus, only 288 (3.8% of total) women were eligible for consideration and 270 (3.5% of total) women available for analysis given information on duration of pregnancy attempt. Based on statistical methods described in detail below, infertility was defined as a TTP greater than 12 months using the current duration approach.
Sociodemographic characteristics, infertility treatment, and reproductive health history were obtained from the survey. Reproductive health history included information on parity, pelvic inflammatory disease (PID) treatment, and history of gynecologic disorders (i.e., prior diagnosis of ovarian cysts, uterine fibroids, endometriosis, or problems with ovulation or menstruation). Information on infertility treatment was determined by questions on current or ever receipt of medical help to get pregnant and the type of help received. Women were considered to have initiated infertility treatment during the current pregnancy attempt if they reported they were currently receiving medical treatment (i.e., not advice or testing), or if the timing of their most recent infertility treatment occurred during their current duration of pregnancy attempt.
Statistical analyses
The data were first analyzed comparing descriptive characteristics across three groups of women in the NSFG survey based on their eligibility for the current duration approach: Group 1) women at risk and reported trying to become pregnant (i.e., women eligible for the current duration analysis); Group 2) women at risk of pregnancy but who reported they were not currently trying to become pregnant; and Group 3) women not at risk of pregnancy.
We used the current duration approach to estimate the distribution of the total duration of pregnancy attempt (i.e., estimated TTP) from their reported duration of current pregnancy attempt (n = 270) (24;32). This method yields a summary measure of the estimated TTP and an estimate of infertility prevalence defined as an estimated TTP > 12 months, and is described in further detail below. To implement this approach, we assumed a Pareto distribution censored at 36 months with the confidence intervals calculated from bootstrap samples (33). We corrected for the oversampling used in the survey design by using a weighted maximum likelihood analyses, which was implemented in R (34). For comparison, we estimated the prevalence of infertility using the NSFG constructed measure among married and cohabiting women (n = 3, 812) appropriately accounting for the survey weights using Stata, version 11 (StataCorp, College Station, TX).
Associations between sociodemographic and reproductive health factors were evaluated for each respective method of infertility assessment. Specifically, odds ratios of infertility were assessed for the constructed measure using weighted logistic regression. For the current duration data, time ratios (TR) were estimated using weighted accelerated-failure-time (AFT) regression models, which can be interpreted as the ratio of the median values of the total duration of pregnancy attempt across characteristics (24). As such, a ratio greater than 1 indicates a longer estimated median TTP. Adjusted logistic regression and AFT regression models accounted for age, relationship status, racial and ethnic self-identification, education, poverty level, health insurance, parity, PID treatment, and gynecologic disorders. All regression analyses account for the survey weights and were performed using Stata, version 11 (StataCorp, College Station, TX).
Sensitivity analyses were run to assess the robustness of our results to varying eligibility criteria. In our main analysis we included all women still currently attempting pregnancy regardless of treatment status. Fertility treatment may modify the probability of pregnancy or represent a competing risk (32); hence, analyses were repeated among women who did not initiate infertility treatment during their current pregnancy attempt. This latter approach assumes a pregnancy attempt ends when a fertility treatment is initiated. Analyses also were repeated to estimate infertility among nulliparous women, who may represent a less heterogeneous group with regard to persistency of trying compared to couples with one or more children.
The current-duration approach refers to a statistical method of estimating the distribution of the (unobserved) total duration of pregnancy attempt (i.e., TTP) based on the (observed) current duration of pregnancy attempt at the time of the survey (23;28;32). The statistical assumptions required by this approach are stationarity (i.e., the start of pregnancy attempts are uniform over time) and independence of the observations. Because the current duration sample evaluates only those at risk of pregnancy at the time of the cross-sectional survey, there is an inherent overrepresentation of couples who take longer to become pregnant (i.e., length-biased sampling). This issue is handled in the statistical methods used to implement this approach. The current duration approach, and more generally backward recurrence time survival methods, also allow us to infer the relationship of characteristics to the (unobserved) total duration of pregnancy attempt by using the (observed) current duration of attempt via AFT models (35).
RESULTS
Women considered for the current duration group (Group 1) were compared to those not included (Groups 2 and 3) and found to be statistically significantly different with respect to age, relationship status, education, income, health insurance, parity, gynecologic disorders, and history of medical treatment for pregnancy (Supplemental Table 1). There was a borderline significantly higher proportion of non-tryers (19.3%) versus tryers (10.2) who identified as Non-Hispanic black (p = 0.06), and 7.2% of women trying for pregnancy (Group 1) reported they were not living with a current partner.
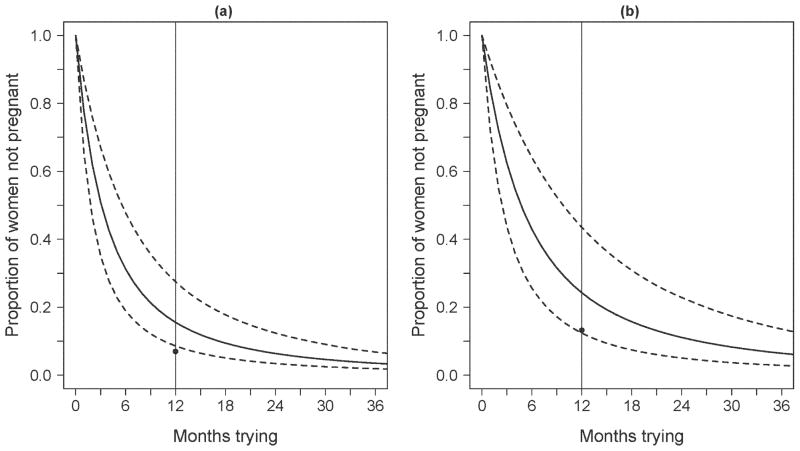
The current duration approach estimated the prevalence of infertility to be 15.5% (95% CI: 8.6, 27.5) among all eligible women (Figure 2a) and 24.3% (95% CI: 12.4, 43.5) among nulliparous women (Figure 2b). In contrast, the constructed measure estimated infertility prevalence to be 7.0% (95% CI: 6.2, 7.8) among all eligible women and 13.2% (95% CI: 11.2, 15.2) among nulliparous women. In sensitivity analyses that excluded women initiating infertility treatment, the current duration approach estimated infertility prevalence to be 12.6% (95% CI: 7.6, 21.4) for all eligible women and 18.3% (95% CI: 11.0, 30.9) for nulliparous women compared with constructed measure estimates of 6.6% (95% CI: 5.8, 7.5) and 11.9% (95% CI: 9.9, 13.9), respectively.
Figure 2.
Estimation of the proportion of women not yet pregnant as a function of the number of months trying for pregnancy among (a) all women (n = 270) and (b) nulliparous women (n = 139) who reported currently trying and their duration of pregnancy attempt. The solid curve is the survival function for the time until pregnancy or end of attempt and the dotted curves indicate 95% confidence intervals (CI). The solid vertical line at 12 months corresponds to infertility estimates of (a) 15.5% (95% CI: 8.6, 27.5) and (b) 24.3% (95% CI: 12.4, 43.5) for the current duration approach. The corresponding infertility estimates represented by black circles are (a) 7.0% (95% CI: 6.2, 7.8) and (b) 13.2% (95% CI: 11.2, 15.2) based on the constructed measure.
A comparison of sociodemographic and reproductive history characteristics for the current duration approach (Table 1) and the construct measure (Table 2) showed similar patterns of conception delay with increasing age, lower education, nulliparity, and gynecologic disorders in adjusted analyses. In contrast, opposing patterns of conception delay were found by race/ethnic self-identification and poverty level. Finally, the odds of infertility were lower among cohabiting women compared to married women using the constructed measure, but showed little difference in estimated TTP using current duration design. By design, women not living with a current partner were included in the current duration analysis and found to be associated with shorter TTP compared to married women (Table 1).
Table 1.
Time ratios (TR) and 95% confidence intervals (CI) for the association between descriptive characteristics and time-to-pregnancy using the current duration approach
| Characteristics | N | Weighted%a | Mean CDb | Unadjusted | Adjusted |
|---|---|---|---|---|---|
| TR (95% CI) | TR (95% CI) | ||||
| Total | 270 | - | 27.5 | - | - |
| Sociodemographic | |||||
| Age (y) | |||||
| 15–24 | 44 | 13.7 | 11.5 | 1.00 | 1.00 |
| 25–29 | 62 | 21.7 | 22.1 | 0.97 (0.38, 2.45) | 1.78 (1.03, 3.10) |
| 30–34 | 60 | 29.0 | 19.9 | 1.09 (0.49, 2.42) | 1.84 (1.10, 3.09) |
| 35–39 | 48 | 22.5 | 28.6 | 0.94 (0.34, 2.59) | 2.33 (1.36,3.99) |
| 40–44 | 32 | 13.1 | 69.7 | 1.38 (0.06, 34.3) | 4.07 (1.67,9.89) |
| Relationship status | |||||
| Married | 180 | 80.9 | 28.9 | 1.00 | 1.00 |
| Cohabiting | 35 | 11.7 | 26.6 | 1.47 (0.98, 2.20) | 0.98 (0.59, 1.61) |
| Not cohabiting | 31 | 7.4 | 15.2 | 0.60 (0.38, 0.95) | 0.58 (0.36, 0.91) |
| Race/ethnic identification | |||||
| Non-Hispanic white | 130 | 65.4 | 30.9 | 1.00 | 1.00 |
| Non-Hispanic black | 32 | 10.7 | 17.0 | 0.51 (0.32, 0.81) | 0.54 (0.28, 1.02) |
| Non-Hispanic other | 15 | 5.2 | 18.3 | 1.08 (0.53, 2.21) | 1.30 (0.81, 2.10) |
| Hispanic | 69 | 18.7 | 23.9 | 0.73 (0.51, 1.05) | 0.71 (0.47, 1.06) |
| Education (y) | |||||
| 0–11 | 60 | 17.9 | 27.0 | 1.00 | 1.00 |
| 12 | 60 | 22.8 | 26.8 | 0.93 (0.55, 1.59) | 0.73 (0.42, 1.28) |
| 13–15 | 51 | 23.5 | 44.7 | 1.27 (0.71, 2.26) | 0.83 (0.43, 1.60) |
| 16+ | 75 | 35.9 | 16.7 | 0.80 (0.45, 1.41) | 0.40 (0.21, 0.76) |
| Percent of poverty level | |||||
| ≥ 300 | 111 | 52.9 | 25.9 | 1.00 | 1.00 |
| 150–299 | 60 | 21.8 | 38.8 | 0.89 (0.56, 1.40) | 1.07 (0.70, 1.65) |
| < 150 | 75 | 25.3 | 21.6 | 0.76 (0.52, 1.10) | 0.76 (0.49, 1.19) |
| Health Insurance | |||||
| Any | 190 | 81.3 | 27.8 | 1.00 | 1.00 |
| None | 56 | 18.7 | 26.4 | 0.98 (0.65, 1.46) | 1.18 (0.72, 1.91) |
| Reproductive history | |||||
| Parity | |||||
| Parous | 127 | 49.9 | 21.9 | 1.00 | 1.00 |
| Nulliparous | 119 | 50.1 | 33.9 | 1.81 (1.27, 2.57) | 2.24 (1.59, 3.16) |
| Pelvic Inflammatory Disease | |||||
| Never treated | 231 | 94.0 | 27.2 | 1.00 | 1.00 |
| Ever treated | 15 | 6.0 | 32.6 | 1.59 (0.77, 3.31) | 1.46 (0.85, 2.52) |
| Gynecologic disordersc | |||||
| No | 150 | 54.9 | 24.6 | 1.00 | 1.00 |
| Yes | 96 | 45.1 | 31.9 | 1.44 (0.98, 2.11) | 1.55 (1.13, 2.13) |
Values are weighted percentages of each characteristic in the sample
Values are weighted means of reported current duration (CD) of pregnancy attempt in months used to estimate total duration of pregnancy attempt (time-to-pregnancy, TTP)
Ever received a diagnosis of ovarian cysts, fibroids, endometriosis, or ovulation/menstruation problems
Table 2.
Odds ratios (OR) and 95% confidence intervals (CI) for the association between descriptive characteristics and infertility using the traditional constructed measure
| Characteristics | N | Weighted %a | Infertile %b | Unadjusted | Adjusted |
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | ||||
| Total | 3,812 | - | 7.0 | - | - |
| Sociodemographic | |||||
| Age (y) | |||||
| 15–24 | 639 | 13.5 | 4.1 | 1.00 | 1.00 |
| 25–29 | 741 | 17.6 | 6.3 | 1.59 (0.85, 2.97) | 1.82 (0.91,3.66) |
| 30–34 | 853 | 21.1 | 8.1 | 2.09 (1.17, 3.74) | 2.77 (1.44, 5.35) |
| 35–39 | 812 | 22.8 | 6.1 | 1.54 (0.85, 2.80) | 2.29 (1.13, 4.63) |
| 40–44 | 767 | 25.1 | 9.0 | 2.35 (1.38, 4.00) | 3.64 (1.87, 7.06) |
| Relationship status | |||||
| Married | 3,080 | 83.6 | 7.4 | 1.00 | 1.00 |
| Cohabiting | 732 | 16.4 | 5.0 | 0.66 (0.41, 1.08) | 0.51 (030, 0.86) |
| Race/ethnic identification | |||||
| Non-Hispanic white | 2,235 | 69.8 | 6.7 | 1.00 | 1.00 |
| Non-Hispanic black | 492 | 8.9 | 10.7 | 1.68 (1.04, 2.71) | 1.98 (1.28, 3.06) |
| Non-Hispanic other | 191 | 5.5 | 5.3 | 0.78 (0.43, 1.43) | 0.92 (0.50, 1.69) |
| Hispanic | 894 | 15.8 | 7.0 | 1.06 (0.76, 1.49) | 1.24 (0.88, 1.73) |
| Education (y) | |||||
| 0–11 | 797 | 18.1 | 7.9 | 1.00 | 1.00 |
| 12 | 924 | 25.6 | 6.5 | 0.80 (0.50, 1.30) | 0.71 (0.45, 1.13) |
| 13–15 | 1,059 | 28.2 | 6.4 | 0.79 (0.52, 1.20) | 0.67 (0.45, 1.01) |
| 16+ | 1,032 | 28.2 | 7.5 | 0.94 (0.62, 1.43) | 0.63 (0.37, 1.07) |
| Percent of poverty level | |||||
| ≥ 300 | 1,706 | 47.0 | 8.0 | 1.00 | 1.00 |
| 150–299 | 1,129 | 29.9 | 5.3 | 0.65 (0.44, 0.94) | 0.74 (0.49, 1.13) |
| < 150 | 977 | 23.1 | 7.0 | 0.86 (0.57, 1.29) | 1.10 (0.72, 1.68) |
| Health Insurance | |||||
| Any | 3,176 | 85.9 | 6.8 | 1.00 | 1.00 |
| None | 636 | 14.1 | 8.2 | 1.22 (0.88, 1.70) | 1.37 (0.96, 1.95) |
| Reproductive history | |||||
| Parity | |||||
| Parous | 2,925 | 78.1 | 5.3 | 1.00 | 1.00 |
| Nulliparous | 887 | 21.9 | 13.2 | 2.73 (2.07, 3.60) | 4.33 (2.85, 6.59) |
| Pelvic Inflammatory Disease | |||||
| Never treated | 3,583 | 94.2 | 6.9 | 1.00 | 1.00 |
| Ever treated | 229 | 5.8 | 8.4 | 1.23 (0.70, 2.17) | 1.06 (0.60, 1.87) |
| Gynecologic disorderc | |||||
| No | 2,563 | 65.1 | 5.8 | 1.00 | 1.00 |
| Yes | 1,239 | 34.9 | 9.2 | 1.65 (1.22, 2.24) | 1.53 (1.10, 2.13) |
Values are weighted percentages of each characteristic in the sample
Values are weighted percentages of current infertility
Ever received a diagnosis of ovarian cysts, fibroids, endometriosis, or ovulation/menstruation problems
DISCUSSION
Using the novel current duration approach, we estimated the prevalence of infertility to be approximately two times greater than the estimate derived from the traditionally applied constructed measure (15.5% vs. 7.0%, respectively), which remained consistent across sensitivity analyses. In addition, the confidence intervals for these estimates do not overlap, suggesting significant differences in prevalence estimates based upon choice of approach. The higher U.S. prevalence estimate using the current duration approach is comparable with the 24% prevalence estimate reported in France based upon the current duration approach (25). Moreover, our estimate is consistent with percentage considered infertile based on prospective cohort studies with preconception enrollment in the United States (range: 12–18%) (16–18). Our findings suggest that the current duration approach appears to be a feasible alternative method for providing population-based infertility estimates using the NSFG and, based on this approach, a higher percentage of couples trying to become pregnant may experience infertility.
Previous research using a constructed measure suggests that infertility may be declining in the United States (31). This trend triggered much speculation and debate in the literature (36–39), particularly due to assumptions required for women not at risk for pregnancy (36) and the exclusion of non-married women (37). The sensitivity of 12-month infertility estimates relative to assumptions in the method of construction was recently demonstrated in a population-based study of Canadian couples (10). In this study, we apply two different methods aimed at estimating the prevalence of current infertility in the United States. A major difference in the two approaches relates to how one handles the denominator when deriving an estimate of infertility prevalence. The constructed measure includes women at risk and not at risk of pregnancy, which makes the implicit assumption that those not at risk of pregnancy (i.e., using contraception, etc.) are fecund. The current duration approach relaxes this assumption by including only women at risk of pregnancy at the time of interview and then appropriately accounts for the length-biased sampling in the statistical analysis. An additional consideration when comparing these measures is how women report their reproductive history – either directly (current duration) or indirectly (constructed measure). To our knowledge, this study is the first application of the current duration design for estimating infertility in a nationally-representative sample of women in the United States. In comparison, nationally-representative infertility estimates from France were based on time since discontinuing contraception (25) and showed minimal difference between all women at risk for pregnancy and those who reported trying to become pregnant (24% versus 23%, respectively).
While we corroborated some risk factors for infertility between estimation approaches, differences were observed for sociodemographic characteristics, such as racial and ethnic self-identification and poverty level. Reasons for these differences may be partially attributable to inclusion criteria and methodologic assumptions required for each approach. For example, the questions used to obtain current duration information were restricted to women reporting they were trying to become pregnant. Because pregnancy intentions may differ by sociodemographic characteristics (40), this may influence associations with fecundity status as reported in this study. We did observe a borderline statistically significant difference in the prevalence of black women at risk for pregnancy who reported they were not trying (19%) compared to trying (10%) to become pregnant (this was not observed for other racial and ethnic groups) (Supplemental Table 1). However, it is important to note that the current duration sample, by design, represents a length-biased sample, which is corrected for in the parametric survival analysis, but not in the cross-tabulation provided in Supplemental Table 1. In addition, the current duration sample did not require exclusion of women not living with their current partner, as was the case for the constructed measure. When we restricted the current duration sample to married or cohabiting couples we found minimal changes to infertility prevalence (17.6%; 95% CI: 10.3, 30.6) and overall patterns of association. Thus, the identification of at-risk subgroups may be influenced by choice of methodologic approach.
This study is unique in that we applied a current duration approach to estimate infertility from a nationally-representative population of U.S. women. With the addition of two simple direct questions to the NSFG in 2002, we were able to compare across two different indicators of infertility. Unlike the constructed measure, the current duration estimate did not rely on assumptions related to fecundity status among those not at risk of pregnancy nor restrict on relationship status. The utility of estimating TTP is that it may allow for cross-disciplinary comparisons for clinical and population-based studies as well as greater flexibility in defining time periods of interest (i.e., TTP > 6, 12, or 24 months) depending on characteristics of the population, such as age. Finally, ascertainment of duration of pregnancy attempt or contraceptive discontinuation in cross-sectional surveys provides a simple direct approach suitable for inclusion in existing population-based surveys.
Both approaches come with limitations. Given the cross-sectional design, the temporal nature of characteristics associated with infertility and issues with retrospective reporting of information need to be considered. In addition to limitations of the constructed measure discussed previously, a limitation of the current duration design is the lack of prospective follow-up to distinguish between pregnancy attempts ending in a pregnancy or due to other reasons, such as the couple stopped trying or initiated infertility treatment. Prevalent cohort designs have been proposed to overcome this limitation (30). Finally, the stationarity assumption assumes no temporal trends in initiation of pregnancy attempts across groups. The continuous survey design implemented by the NSFG after 2006 provides an opportunity to assess this assumption in greater detail (41). Specific to this study, we were also limited to women who reported trying for pregnancy, who may not be representative of the larger population of women at risk of pregnancy. This limitation could be easily overcome in future studies by expanding the survey question to include all at risk time (i.e., time from contraceptive discontinuation) regardless of pregnancy intentions. Further strengths and limitations of the current duration design over prospective or retrospective collection of TTP information have been highlighted previously (30).
These findings are timely in light of the recent National Public Health Action Plan for the Detection, Prevention, and Management of Infertility released for public commentary by the Center for Disease Control and Prevention (CDC) in May 2012 (42). The action plan highlighted the need for uniform measures of infertility across clinical and population-based studies and the strengthening of surveillance systems to monitor infertility in the United States. We believe the current duration approach provides a feasible alternative approach for monitoring infertility, since it focuses on those at risk for pregnancy and relaxes assumptions impacting the denominator. In addition, it relies on a few simple direct questions to derive an estimate of infertility from cross-sectional designs facilitating its use in existing national health surveys. The comparability of our estimate with other gold-standard prospective cohort studies suggests that this approach may also be useful for comparisons across different types of study designs. In the context of a National Public Health Action Plan for infertility, an important first step is to ensure the magnitude and scope of infertility is well defined for the U.S. population to improve public health guidelines and recommendations. More specifically, additional data gaps remain for understanding the etiology, identifying at-risk subgroups, and improving clinical services for infertility. These ambitious goals are within the context of efforts to ameliorate the unintended consequences of infertility for men, women, and couples.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge Drs. Niels Keiding, Oluf Hansen, and Ditte Sorensen for their feedback on the current duration method and programs for implementing this approach.
Financial support:
The 2002 National Survey of Family Growth (NSFG) was conducted by the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics (NCHS) with the support and assistance of a number of other organizations and individuals, with the participation and funding support of the following programs of the U.S. Department of Health and Human Services:
Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD), National Institutes of Health (NIH)
Office of Population Affairs
CDC’s National Center for Health Statistics (CDC/NCHS)
CDC’s Division of HIV/AIDS Prevention (CDC/DHAP)
CDC’s Division of Sexually Transmitted Disease Prevention (CDC/DSTDP)
CDC’s Division of Reproductive Health (CDC/DRH)
Office of the Assistant Secretary for Planning and Evaluation (OASPE)
Children’s Bureau of the Administration for Children and Families.
Analyses and preparation of the manuscript was funded by the Intramural Research Program, NICHD, NIH. Results were presented at the 25th Annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research, Minneapolis, MN, June 2012 and the National Institutes of Health Research Festival, Bethesda, MD, October 2012.
Footnotes
Author disclosure statement:
M.E.T has nothing to disclose. A.C.M has nothing to disclose. J.F.L has nothing to disclose. R.B.K. has nothing to disclose. A.C.T. has nothing to disclose. R.S. has nothing to disclose. G.M.L has nothing to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Zegers-Hochschild F, Adamson GD, de MJ, Ishihara O, Mansour R, Nygren K, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520–1524. doi: 10.1016/j.fertnstert.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 2.Raatikainen K, Harju M, Hippelainen M, Heinonen S. Prolonged time to pregnancy is associated with a greater risk of adverse outcomes. Fertil Steril. 2010;94:1148–1151. doi: 10.1016/j.fertnstert.2009.10.058. [DOI] [PubMed] [Google Scholar]
- 3.Basso O, Weinberg CR, Baird DD, Wilcox AJ, Olsen J. Subfecundity as a correlate of preeclampsia: a study within the Danish National Birth Cohort. Am J Epidemiol. 2003;157:195–202. doi: 10.1093/aje/kwf194. [DOI] [PubMed] [Google Scholar]
- 4.Buck Louis GM, Cooney MA, Peterson CM. The ovarian dysgenesis syndrome. Journal of Developmental Origins of Health and Disease. 2011;2:25–35. [Google Scholar]
- 5.Lutz W, Skirbekk V. Policies Addressing the Tempo Effect in Low-Fertility Countries. Population and Development Review. 2005;31:699–720. [Google Scholar]
- 6.Wolf DA, Lee RD, Miller T, Donehower G, Genest A. Fiscal Externalities of Becoming a Parent. Population and Development Review. 2011;37:241–266. doi: 10.1111/j.1728-4457.2011.00410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bitler M, Schmidt L. Health disparities and infertility: impacts of state-level insurance mandates. Fertil Steril. 2006;85:858–865. doi: 10.1016/j.fertnstert.2005.11.038. [DOI] [PubMed] [Google Scholar]
- 8.Buck GM, Sever LE, Batt RE, Mendola P. Life-style factors and female infertility. Epidemiology. 1997;8:435–441. doi: 10.1097/00001648-199707000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Marchbanks PA, Peterson HB, Rubin GL, Wingo PA. Research on infertility: definition makes a difference. The Cancer and Steroid Hormone Study Group. Am J Epidemiol. 1989;130:259–267. doi: 10.1093/oxfordjournals.aje.a115332. [DOI] [PubMed] [Google Scholar]
- 10.Bushnik T, Cook JL, Yuzpe AA, Tough S, Collins J. Estimating the prevalence of infertility in Canada. Hum Reprod. 2012;27:738–746. doi: 10.1093/humrep/der465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gurunath S, Pandian Z, Anderson RA, Bhattacharya S. Defining infertility--a systematic review of prevalence studies. Hum Reprod Update. 2011;17:575–588. doi: 10.1093/humupd/dmr015. [DOI] [PubMed] [Google Scholar]
- 12.Martinez G, Daniels K, Chandra A. National Health Statistics Reports. Vol. 51. Hyattsville, MD: National Center for Health Statistics; 2012. Fertility of Men and Women Aged 15–44 Years in the United States: National Survey of Family Growth, 2006–2010. [PubMed] [Google Scholar]
- 13.Copen CE, Daniels K, Vespa J, Mosher WD. First marriages in the United States: Data from the 2006–2010 National Survey of Family Growth. Vol. 49. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 14.Mathews TJ, Hamilton BE. Mean age of mother, 1970–2000. Natl Vital Stat Rep. 2002;51:1–13. [PubMed] [Google Scholar]
- 15.Chandra A. Surgical sterilization in the United States: prevalence and characteristics, 1965–95. Vital Health Stat 23. 1998;20:1–33. [PubMed] [Google Scholar]
- 16.Buck Louis GM, Sundaram R, Schisterman EF, Sweeney AM, Lynch CD, Gore-Langton RE, et al. Heavy metals and couple fecundity, the LIFE Study. Chemosphere. 2012;87:1201–1207. doi: 10.1016/j.chemosphere.2012.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zinaman MJ, Clegg ED, Brown CC, O’Connor J, Selevan SG. Estimates of human fertility and pregnancy loss. Fertil Steril. 1996;65:503–509. [PubMed] [Google Scholar]
- 18.Tietze C. Fertility after discontinuation of intrauterine and oral contraception. Int J Fertil. 1968;13:385–389. [PubMed] [Google Scholar]
- 19.Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat 23. 2005;25:1–160. [PubMed] [Google Scholar]
- 20.Bonde JP, Olsen J. Interpreting trends in fecundity over time. BMJ. 2008;336:339–340. doi: 10.1136/bmj.39463.522708.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olsen J, Rachootin P. Invited commentary: monitoring fecundity over time--if we do it, then let’s do it right. Am J Epidemiol. 2003;157:94–97. doi: 10.1093/aje/kwf178. [DOI] [PubMed] [Google Scholar]
- 22.Joffe M. Invited commentary: the potential for monitoring of fecundity and the remaining challenges. Am J Epidemiol. 2003;157:89–93. doi: 10.1093/aje/kwf177. [DOI] [PubMed] [Google Scholar]
- 23.Weinberg CR, Gladen BC. The beta-geometric distribution applied to comparative fecundability studies. Biometrics. 1986;42:547–560. [PubMed] [Google Scholar]
- 24.Keiding N, Kvist K, Hartvig H, Tvede M, Juul S. Estimating time to pregnancy from current durations in a cross-sectional sample. Biostatistics. 2002;3:565–578. doi: 10.1093/biostatistics/3.4.565. [DOI] [PubMed] [Google Scholar]
- 25.Slama R, Hansen OK, Ducot B, Bohet A, Sorensen D, Giorgis AL, et al. Estimation of the frequency of involuntary infertility on a nation-wide basis. Hum Reprod. 2012;27:1489–1498. doi: 10.1093/humrep/des070. [DOI] [PubMed] [Google Scholar]
- 26.Joffe M, Key J, Best N, Keiding N, Scheike T, Jensen TK. Studying time to pregnancy by use of a retrospective design. Am J Epidemiol. 2005;162:115–124. doi: 10.1093/aje/kwi172. [DOI] [PubMed] [Google Scholar]
- 27.Buck GM, Lynch CD, Stanford JB, Sweeney AM, Schieve LA, Rockett JC, et al. Prospective pregnancy study designs for assessing reproductive and developmental toxicants. Environ Health Perspect. 2004;112:79–86. doi: 10.1289/ehp.6262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scheike TH, Keiding N. Design and analysis of time-to-pregnancy. Stat Methods Med Res. 2006;15:127–140. doi: 10.1191/0962280206sm435oa. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. [Accessed June 22, 2012];National Survey of Family Growth. Available at: http://www.cdc.gov/nchs/nsfg.htm.
- 30.Slama R, Ducot B, Carstensen L, Lorente C, de La RE, Leridon H, et al. Feasibility of the current-duration approach to studying human fecundity. Epidemiology. 2006;17:440–449. doi: 10.1097/01.ede.0000221781.15114.88. [DOI] [PubMed] [Google Scholar]
- 31.Stephen EH, Chandra A. Declining estimates of infertility in the United States: 1982–2002. Fertil Steril. 2006;86:516–523. doi: 10.1016/j.fertnstert.2006.02.129. [DOI] [PubMed] [Google Scholar]
- 32.Keiding N, Hansen OK, Sorensen D, Slama R. The Current Duration Approach to Estimating Time to Pregnancy. Scandinavian Journal of Statistics. 2012;39:185–204. [Google Scholar]
- 33.Efron B, Tibshirani RJ. An introduction to the bootstrap. London: Chapman & Hall; 1993. [Google Scholar]
- 34.R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2012. [Google Scholar]
- 35.Yamaguchi K. Accelerated Failure-Time Mover-Stayer Regression Models for the Analysis of Last-Episode Data. Sociological Methodology. 2003;33:81–110. [Google Scholar]
- 36.Guzick DS, Swan S. The decline of infertility: apparent or real? Fertil Steril. 2006;86:524–526. doi: 10.1016/j.fertnstert.2006.05.027. [DOI] [PubMed] [Google Scholar]
- 37.Thornton KL, Goldman MB. Impact of subgroup analysis on estimates of infertility. Fertil Steril. 2006;86:531–533. doi: 10.1016/j.fertnstert.2006.05.028. [DOI] [PubMed] [Google Scholar]
- 38.Olive DL, Pritts EA. Estimating infertility: the devil is in the details. Fertil Steril. 2006;86:529–530. doi: 10.1016/j.fertnstert.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 39.Barnhart KT. The challenge and enjoyment of the interpretation of epidemiologic data. Fertil Steril. 2006;86:527–528. doi: 10.1016/j.fertnstert.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 40.Greil AL, McQuillan J, Johnson K, Slauson-Blevins K, Shreffler KM. The hidden infertile: infertile women without pregnancy intent in the United States. Fertil Steril. 2010;93:2080–2083. doi: 10.1016/j.fertnstert.2009.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Groves RM, Mosher WD, Lepkowski JM, Kirgis NG. Planning and development of the continuous National Survey of Family Growth. Vital Health Stat 1. 2009;48:1–64. [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. [Accessed June 22, 2012];Infertility and Public Health. Available at: http://www.cdc.gov/reproductivehealth/Infertility/PublicHealth.htm.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.