Abstract
Aims and objectives
This study explores how sleep and energy levels were affected in Chinese women diagnosed with HIV in China employing the Actiwatch actigraphy system to collect data on the women’s sleep characteristics.
Background
The worldwide AIDS pandemic, a major impetus behind the recent focus on global aspects of health, is one area in which the behavioural and biomedical expertise of nursing science is sorely needed. In particular, few studies of HIV+ women have examined the association of HIV-related stress with sleep disturbance and fatigue. Especially, fatigue and sleep disturbances are a common complaint among people with HIV.
Design
A qualitative study with actigraphy device used.
Methods
In-depth interviews were conducted with 19 HIV+ women in Shanghai, China, from December 2009–March 2010 and within this group, nine of the women agreed to wear an Actiwatch actigraphy device for 72 hours.
Results
Two major themes emerged from the in-depth interviews are as follows: sleep disturbance and fatigue. Participants presented varying amounts of sleeplessness, and fatigue resulting from nightmares, worrying about whether to disclose their diagnosis, and whether they might transmit the disease to their partners or children. Among the nine Actiwatch study participants, data shown that those who experienced fragmented sleep also slept more during the daytime.
Conclusions
In this study, Chinese HIV+ women described how stress had caused them to become sleepless. The objective data collected via Actiwatch showed that these women required longer nap times, which indicates they did not have refreshing nocturnal sleep. Designing a culturally acceptable stress management intervention for these women is urgently needed.
Relevance to clinical practice
Sleep and fatigue level should be evaluated in each visit with HIV care. Nurses need to be trained in evaluating the HIV+ patients’ sleep and fatigue status and refer them to psychologist and/or relaxation technique accordingly. Self-management intervention for HIV+ individuals should also include the sleep hygiene into consideration.
Keywords: China, fatigue, HIV, sleep disturbance, women
Introduction
Nursing science and research in the 21st century needs to be increasingly adopting a global perspective. The worldwide AIDS pandemic, the major impetus for the more recent global perspective on health, is one area in which the behavioural and biomedical expertise of nursing science is acutely needed. One specific area in the HIV field that requires combined behavioural and biomedical expertise is sleep research. Nursing science in this area can benefit from capitalising on technological advances that objectively monitor sleep quality.
Background
Women accounted for almost half (47%) of people living with the disease as of the end of 2007 (U.S. Department of Health & Human Services Office 2011). In China, approximately 180,000 Chinese women of reproductive age are HIV+ (UNAIDS 2006) and mother-to-child transmission is rising, with an estimated 9000 cases in 2005 (Ministry of Health People’s Republic of China Joint United Nations Programme on HIV/AIDS World Health Organization 2006).
Sleep disturbances are a common complaint among people with HIV infection (Hudson et al. 2008, Pence et al. 2008, Salahuddin et al. 2009). In HIV-positive individuals, those who are highly fatigued from sleep disturbances are more vulnerable to additional negative consequences of fatigue because of the psychosocial stress they experience (Marion et al. 2009). Fatigue is one of the most frequent and debilitating symptoms of HIV disease (Barroso et al. 2008, Leserman et al. 2008, Scott-Sheldon et al. 2008). Prevalence rates for debilitating fatigue range from 17–60% in people with HIV and from 43–85% in people with AIDS (Barroso et al. 2008, Scott-Sheldon et al. 2008, Salahuddin et al. 2009). Generally, women experience higher fatigue severity and perceive a higher level of stress than men (Voss et al. 2007). Population-based studies especially tend to report higher rates of fatigue for women as compared to men (Lee et al. 2001, Phillips et al. 2004, Salahuddin et al. 2009). In one study, women reported greater sleep disturbances and more severe fatigue than men and experience much more wakeful time during the night than did men (Lee et al. 2007).
Fatigue is described as a lack of energy, sleepiness, exhaustion, an inability to get enough rest or weakness (Adinolfi 2001). Many researchers have documented the relationship between fatigue and higher levels of psychological stress (Leserman et al. 2008, Pence et al. 2008, Salahuddin et al. 2009). Frequently identified causes of fatigue in these individuals include lack of rest; poor exercise habits or improper or inadequate diet; psychological stress, including depression and anxiety; use of recreational drugs; side effects from antiretroviral medications; sleep disturbances; fever; anaemia; and lower CD4 cell counts (Adinolfi 2001, Leserman et al. 2008, Salahuddin et al. 2009).
To date, there are few research studies focused specifically on fatigue and sleep disturbances in the HIV-positive population in China. However, this does not mean that there are no issues related to fatigue or sleep disturbances. In Chinese culture, complaining of such common maladies as fatigue or lack of sleep is discouraged; therefore, to eliminate culture as a factor in measuring prevalence of these symptoms, more specialised research is needed. Although evidence indicates that greater stress is associated with increased fatigue and sleep disturbances in the general population (Docherty et al. 2006, Thomas et al. 2006), there is a lack of empirical data on this relationship among women with HIV/AIDS.
The study
Aim
In this study, we explored how sleep and energy levels were impacted among Chinese HIV+ women after they learned of their disease.
Design
Snowball sampling methods were then used to identify and enrol a sample of women who were HIV-positive, at least 18 years of age and were willing to share their personal stories with the researchers. The study took place from December 2009–March 2010. With prior consent from all the participants, we audio-recorded the interviews, which were conducted in Mandarin with native-speaking interviewers. All participants received a small payment for their participation. For those who agreed to wear the Actiwatch device, researchers gave detailed instructions in how to use the Actiwatch device after the in-depth interviews.
Participants
As part of a larger mixed-method study, the in-depth interviews were conducted with 19 HIV-positive women in Shanghai, China, and within this group, nine of the women agreed to wear an Actiwatch (Mini Mitter Respironics, Inc., Bend, OR, USA) for a consecutive 72 hours.
Data collection
HIV-positive women who were interested in the study met with the researchers, who then explained the study, answered questions and obtained written consent. In addition to in-depth interviews, Actiwatch actigraphy devices were used to collect objective data and gain more precise knowledge of the women’s sleep characteristics.
In-depth interviews were audio-recorded, conducted in Mandarin and transcribed into Mandarin after the session. Quotations were selected from the transcripts and translated into English for publication. Each interview took about two hours and was carried out in a private location. Bilingual researchers – a social-work doctoral student and a nursing researcher – conducted all the in-depth interviews.
Interviewers used a checklist during interviews to inquire about the participants’ perceptions of sleep disturbances and fatigue both before and after their HIV diagnosis, in addition to other topics that are not discussed in this article. Specific questions included the following: ‘What has your energy level been before and after your diagnosis of HIV?’, ‘How is your sleep quality currently?’ and ‘Have you had any good or bad experiences during night-time sleep?’ The interviewer asked each participant about one specific experience of a dream that they remembered. Generally, the study participants led the discussion, with the interviewers prompting as needed.
Actiwatch (Mini Mitter Respironics, Inc.) is a motion-sensor monitor worn on the non-dominant wrist that is used to record activity over time. For each of the subject’s movements, an accelerometer generates a variable voltage that is digitally processed. Then, the signal is integrated and recorded in on-board memory. There is an event marker on the Actiwatch device for the study participants to indicate bedtime (light off time) and arise time (light on time). In addition, the study participants were asked to keep a three-day sleep diary about their sleep–wake patterns, they completed the sleep diary before bed and immediately after awakening the following morning. Sleep diaries were used to validate the bedtime and arise time indicated from the event markers.
Ethical consideration
Ethical review boards at both the study institutions approved the study.
Data analysis
Qualitative content analysis (Hsieh & Shannon 2005) with Atlas.ti software (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany) was used to code and analyse the data. Two bilingual investigators examined the transcripts separately and identified codes to correspond to concepts in the narratives. The investigators then discussed the coding to resolve any disagreements in the meaning and assignment of codes and general patterns observed in the data.
Results
The study participants’ mean age was 42 years (SD = 9·5 years; range, 29–59). At the time of the study, all of the participants lived in the Shanghai metropolitan area, except for one who lived in Fuzhou City (Fuchien province) and commuted to Shanghai to obtain her medication. More than half of the participants (52%) had migrated to Shanghai from other provinces. One-third (32%) had been on antiretroviral therapy (ART) for at least a year, and 32% had a four-year college degree. Eight of their partners (42%) were also HIV-positive. Almost half (47%) of them were married. Most of the participants (79%) had contacted HIV through their husbands and/or sexual partners. Four of them (21%) were not on ART yet. Of these 19 study participants, nine (47%) had provided the Actiwatch data. Detailed demographics for the nine actigraphy participants are presented in Table 1.
Table 1.
Demographics of sleep actiwatch participants
| Participant | Age | Year of diagnosis | Year on ART | Education | Marital status | Possible HIV transmission route | Occupation |
|---|---|---|---|---|---|---|---|
| 1 | 58 | 2007 | 2008 | Junior college | Widow | BF, after being widowed | Retired |
| 2 | 40 | 2002 | 2002 | High school dropout | Widow | Plasma donor | Janitor |
| 3 | 32 | 2007 | 2009 | Bachelor’s degree | Cohabited with BF | BF | Finance consultant |
| 4 | 33 | 2009 | 2009 | Junior college | Married | IDU | Housewife |
| 5 | 30 | 2009 | 2009 | High school dropout | Divorced | BF before marriage | Labourer |
| 6 | 50 | 2002 | 2002 | Medical school graduate | Divorced | Blood transfusion | Peer support activist |
| 7 | 32 | 2008 | Not Yet | Medical school graduate | Divorced | Extra-marital relationship | Physician |
| 8 | 42 | 1998 | 2005 | Bachelor’s degree | Married | Overseas affair | Retired |
| 9 | 30 | 2010 | Not Yet | Bachelor’s degree | Single, in a relationship | Ex-BF | Business |
BF, boyfriend; ART, antiretroviral therapy; IDU, intravenous drug user.
Two major symptoms/themes were extracted from the in-depth interview: sleep disturbance and fatigue. Each of the themes is discussed in the following section.
Sleep disturbance
Many studies have documented that HIV-positive women experience poor sleep quality (Lee et al. 2001, Marion et al. 2009). Because of sleep disturbance, HIV-positive women encounter significant problems in daily functioning (Marion et al. 2009). Studies report that many issues relate to poor sleep quality, for example, depressive symptoms, progress of the HIV, side effects of the disease and the medicine, financial difficulties, disclosure and anxiety about the future all may contribute to sleeplessness (Penzak et al. 2000, Phillips et al. 2004, Vosvick et al. 2004, Pence et al. 2008, Salahuddin et al. 2009, Zhao et al. 2009).
In this study, many of these HIV-positive women mentioned that after receiving their HIV diagnosis, they began experiencing sleep disturbances and that these disturbances had continued since then, regardless of their current treatment condition. Specifically, nightmares were one of their major concerns. One 42-year-old woman talked about being afraid that she might disclose her diagnosis during sleep-talking and that she had lost sleep over this:
I try not to think about my disease during the day; however, at night, I dream about how hard it is trying not to let people know about my illness, and how everyone finds out about it anyway. Therefore, I believe that even if I do not think about myself and this disease, unconsciously, it will still affect me a lot.
Several women mentioned having vivid nightmares after the HIV diagnosis and talked about how this prevented them from getting deep sleep. One 40-year-old with sleep disturbance a former plasma donor with two teenage children, described it this way:
I have so many nightmares about my kids being hit by a car or something bad happening to my family, and I am so horrified by these scenes that I just can’t sleep…. I am so tired. My sleep pattern is that I lie in bed for about an hour. Then I wake up with a feeling that there is something I need to do. Then, after I clear my mind and realize that I do not have anything urgent to do, I lie down one more time. Basically, I am waking up every one to two hours, and when I have deep sleep, I always get a nightmare. Then, I wake up because of the nightmare, empty my bladder, clear my mind, go back to sleep, and continue the nightmare.
This participant and her husband contracted HIV from selling blood, and her husband died from AIDS before she and her two children relocated to Shanghai. Because of the disease, she was concerned for her children’s future. She continued as follows:
Those nightmares are all basically the same. For example, it’s like someone is trying to kill me. I’m running as fast as I can, and I am out of breath. Or I need to find a restroom urgently. Finally, I find one, but when I walk in, there are many men inside, so I run out. But I still need to pee so badly. I keep walking back and forth worrying that I might expose myself. Or, I am trying to cross a wide river, and when I’m almost at the end, the bridge falls. I even dreamt about a skyscraper being demolished while I was walking under it. One leg was under the debris, and I couldn’t move myself. I wanted to leave, but I couldn’t. Just horrible, horrible dreams. I always wake up in a cold sweat.
There are several factors that might be influencing these HIV-positive women’s quality of sleep, and these include discomfort from the disease, side effects of the medication and worrying about the family. One 52-year-old former professional woman who experienced trouble getting to sleep described her issues as follows:
From the first, I did not have good sleep, because in the beginning, my CD4 was so low that I was sick all the time; therefore, I didn’t sleep well. Also, whenever I think about my husband and my son, I just can’t sleep. It’s not that I wake up suddenly during the night; it’s simply that I just cannot get to sleep. I lie on bed for a long while, but my mind is always alert when I’m thinking about my family.
For those women who did not disclose their HIV status to spouses or sexual partners, there were other issues related to sleep. One 48-year-old skill worker woman mentioned that, starting in the early days after her diagnosis, she could no longer sleep deeply at night because she needed to stay alert in case her husband asked her for sex and she needed to think of an excuse to avoid having sex with him. For this reason, she had never enjoyed good sleep during the first few years following her diagnosis. By the time of the study, however, her husband had begun seeking other women for his sexual needs, and they had moved into separate bedrooms, so she could start to get better sleep.
Women who were in their 30s had different perspectives on sleeplessness. One 32-year-old single woman, for example, expressed regret about losing her youth, which kept her awake during nights:
I was so childish for running away with my boyfriend at that time. Because of our financial situation, we needed to sell blood to get some cash. And because of doing that [and contracting HIV], I will never have a good life now. If I didn’t have this [disease], I would definitely be having a wonderful life, a great family. At the worst I might have gotten a divorce in a normal relationship, but I never would have ended up like this.
Experience of fatigue
Fatigue is one of the major complaints reported by the women. Some of them explained that, because of the side effects of ART, they always felt tired. Others mentioned that, because the disease had already progressed to a certain point, they always felt weak and had trouble moving around. In addition to these symptoms, stress is one of the key issues that they all mentioned. One 42-year-old housewife spoke very directly about it, saying that because of her psychological stress, she always felt fatigued and had no energy to do anything. She said the following:
I am under so much stress that I am always tired. Even if there is no one at home, I still cannot sleep. I try to go out and relax, but I cannot. Certain things are always on my mind, especially related to this disease, and it is so hard to forget them.
Besides the stress that came from disclosure and changed family relationships, many women also discussed financial difficulties as one of their major stressors. One 52-year-old retired woman talked about the stress she had being related to money. She felt that if she could have more money to take care of her ailments, and to put some aside in case she needed to pay hospital bills, she would feel less stress.
In this study, women who live with HIV for longer than five years on ART do feel much better and have more energy to go out and meet peers among the local people living with HIV/AIDS (PLWHA) organisation. One 50-year-old former professional woman who was diagnosed with HIV and had been taking ART for eight years stated the following:
I feel good now, I mean right now. But it took me five years to gather myself together. Many new patients, they only take a couple months to recuperate and get their lives back, but for me, during these last five years, I cried every day. I would just start crying when I saw something on TV or in a book that set me off. I don’t know where those tears came from, but it has lasted for five years, till now. During these five years, no one helped me. I didn’t have energy to talk to anyone. I’m tired, really tired.
Objective sleep/activity measurements (TST/WASO)
Objective sleep data were measured by an Actiwatch monitoring device to assess the study participants’ total sleep time (TST) and wake after sleep onset (WASO). One-minute intervals were used in this study to calculate TST in minutes and WASO as a percentage by using Actiware-Sleep 3.4 (Mini Mitter Respironics, Inc.). Nocturnal TST was defined as a sleep period based on the event markers of bedtime/arise time. If the event markers were not available, then the data from the sleep diary were used to estimate a study participant’s TST. A nap was defined as a sleep episode that occurred within 12 hours after the study participant’s rise time, and the average activity levels during the same time period were used to indicate for activity level. These data were then entered into spss version 18.0 software (SPSS Inc., Chicago, IL, USA) for descriptive analysis.
Most of the nine women did not have a regular bedtime or wake time, which indicates that their circadian activity rhythms were weakly synchronised. The average nocturnal TST was 446 minutes (SD = 45) and WASO was 8·9% (SD = 5·7) among the nine women. The average nap time (within 12 hours after arise time) was 189 minutes (SD = 91), and activity level was 70 (SD = 29). There was a negative relationship between WASO and daytime TST (r = −0.57), indicating that those who experienced fragmented sleep also slept more during the daytime. Figure 1 presented a 40-year-old woman’s sleep pattern during the third night monitoring period, and Table 2 includes detailed objective sleep data for each study participant.
Figure 1.
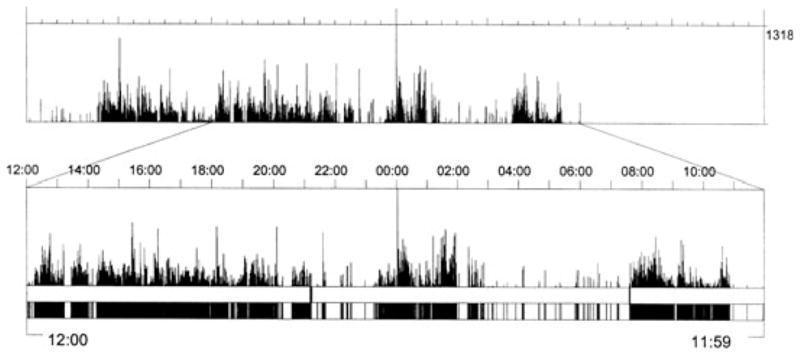
Actigraphy sample. This was a 24-hour rest/activity data (12:00 p.m. to next day 11:59 a.m.) from a 40-year-old woman. Bedtime: 9:10 p.m; arise time: 7:35 a.m.; nocturnal total sleep time: 7·5 hours; wake after sleep onset: 35%.
Table 2.
Descriptive objective sleep data
| ID | Bedtime | Get up time | TST mean (in minutes) | WASO mean (%) | Nap (in minutes) | Daytime activity |
|---|---|---|---|---|---|---|
| 1 | 21:10–23:00 | 04:35–07:35 | 350 | 20·1 | 118 | 108 |
| 2 | 20:27–21:07 | 06:10–08:02 | 498 | 17 | 80 | 101 |
| 3 | 22:15–22:55 | 06:45–07:44 | 466 | 6·3 | 166 | 85 |
| 4 | 23:58–03:11 | 09:14–10:01 | 451 | 5·2 | 172 | 37 |
| 5 | 23:40–23:55 | 06:16–08:48 | 443 | 7·1 | 281 | 49 |
| 6 | 22:00–23:45 | 07:34–08:01 | 501 | 4·9 | 205 | 81 |
| 7 | 21:16–22:56 | 06:20–07:12 | 422 | 8·1 | 72 | 92 |
| 8 | 21:00–22:56 | 06:03–06:26 | 437 | 7·1 | 324 | 35 |
| 9 | 20:12–22:17 | 06:48–07:35 | 444 | 4·1 | 279 | 41 |
TST, nocturnal total sleep time; WASO, wake after sleep onset.
These objective data confirmed that HIV-positive women experienced various kinds of issues related to sleeplessness. Overall, actigraphy participants showed higher naptime than healthy adult women during daytime; however, the length of their night-time sleep is similar to that of healthy adult women. Women diagnosed with HIV for longer period of time (>5 years) generally showed better sleep patterns; however, because of the sample size, it cannot be represented all the cases.
Discussion
There were several limitations in this international study. First, the study samples were limited to HIV-positive women in Shanghai, a metropolitan area influenced by Western cultural attitudes. In our study, many women had contacted HIV from premarital or extra-marital relationships, but this should not be generalised to other HIV-positive women in China. Second, only nine participants wore the actigraphy device to measure their sleep and wake cycle. According to optional recommendations from the American Academy of Sleep Medicine, a minimum of three consecutive 24-hour periods is needed for actigraphic study (Littner et al. 2003). However, a prolonged monitoring time can increase internal validity for sleep/activity data; therefore, the actigraphic data should be explored further in a future study. Third, in this study, the data analysis did not address the women’s usage of ART at the time of the study. Because there might have side effects of sleep disturbance and nightmares related to the ART, in a future study, comparisons should be made between women who are and are not on ART. Last, no participants mentioned depression during the study. That might be because the Chinese culture discourages people from disclosing mental health issues. In addition, we do not know whether sleeplessness reflects underlying depression in these HIV-positive women.
Fatigue and sleep disturbances are major complaints for many HIV-positive patients (Pence et al. 2008, Salahuddin et al. 2009, Yeh et al. 2009). In this study specifically, HIV-positive women frequently reported suffering from insomnia and restlessness while trying to sleep (Hudson et al. 2008, Pinkham & Malinowska-Sempruch 2008, Marion et al. 2009). Moreover, because HIV is a highly stigmatised disease, PLWHA suffer different levels of psychological stress (Chen et al. 2011). Women in China, who assume the care-taker role in the family, bear even more stress when they and their spouses are both HIV-positive (Chen et al. 2007, 2010).
In this study, Chinese women described how stress caused them to experience sleeplessness. In many cases, the stress resulted from thinking about the future of their dependents, and because they perceived themselves to have lost their primary role as women, which was to live in a happy family, with loving husbands and children by their side. Following an HIV+ diagnosis, it took many years for them to adjust their minds to their new reality and to get themselves focused back on their current lives.
The objective data collected from Actiwatch showed that these women required nap times, which indicates they did not have refreshing nocturnal sleep. In addition, the average activity level during the daytime was 70, which implies that these women had a normal amount of activities compared with HIV-women. To date, no data are available to compare activity levels between the two populations; however, our study participants’ daytime activity levels were lower than those of patients with advanced lung cancer (Levin et al. 2005). Physiological indicators may be particularly important for the Chinese population as well. Because of China’s socially conservative culture, many Chinese may hesitate to express their feelings verbally include to their healthcare providers.
Disclosure is also one of the dilemmas for these women who cannot sleep at night. They wonder: If they disclose their HIV status, will they and their families be stigmatised by their friends and relatives? On the other hand, if they do not disclose, they cannot get the support they need from others, especially their husbands or sexual partners. These HIV-positive women are in a bind: they want to protect their husbands but do not want to disclose their status. So, they may choose to suffer, as one participant did for example, by staying alert (and awake) all night to avoid having sex with a partner. In this kind of scenario, a woman may want to keep the appearance of being part of an intimate husband-and-wife relationship, but without the physical contact. Currently in China, within a sexual relationship, condom use is still very uncommon. If one partner asks the other to use condom, it implies that the person asking must have a disease. Especially in a marriage, it is felt that there is no need to use a condom, because the marriage is assumed to be built on trust and monogamy. Therefore, asking these HIV-positive women’s husbands to use condoms is difficult, except in cases where both partners have been educated on HIV-related issues.
Generally, more public education about safe sex is needed in China, and peer support is important for HIV-positive women to be able to get back to the routine of daily living. In the future, interventions need to be designed that will decrease stress, enhance sleep quality and decrease fatigue. However, without a good social support system and assistance, HIV-positive women will continue to suffer from fatigue and sleeplessness.
Conclusion
To remain relevant and influential, nursing science in 21st century needs to continue to innovate and grow to focus on global health. Nursing can contribute to issues that require a biobehavioural expertise that includes HIV and sleep research. In addition, research is increasingly technologically advanced, and sleep research is no exception. In this study conducted in China, we focused on HIV-related global health and using actigraphy as the biobehavioural approach to measure objective sleep to push nursing science forward. This study showed that women have always had different expectations placed on them than have men. In addition to the burden of taking care of a husband, children and older parents or in-laws, HIV-positive women in China suffer the physical and social distress caused by this life-threatening disease. In this study, participants presented sleep disturbance and fatigue caused by factors ranging from worrying about disclosure to worrying about transmitting the disease to intimate partners. Future study should focus on designing a culturally acceptable stress management intervention to these women in need.
Acknowledgments
This publication resulted (in part) from research supported by the University of Washington Center for AIDS Research (CFAR), an NIH funded program (P30 AI027757), which is supported by the following NIH Institutes and Centers (NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NCCAM) through an international pilot grant awarded to Dr Wei-Ti Chen and by the University of Washington’s (UW) School of Nursing Research & Intramural Funding Program (RIFP). The publication was also supported in part by MH074364 and MH074364-S1 from the National Institute of Mental Health (Simoni, PI) and Dr Chen’s developmental fund from Yale University, School of Nursing. We would also like to acknowledge Yinyin Tu, Ren-Fang Zhang, Li-Jun Zha, Xiaoling Wang, the Association for the Benefit of PLWHA (Beautiful Life-Shanghai) and all of the study participants.
Footnotes
Contributions
Study design: WC, CS, JS; data collection and analysis: WC, SL, CS, JS, CP, MB, HL and manuscript preparation: WC, SL, CS, JS, CP, MB, HL.
Contributor Information
Wei-Ti Chen, Assistant Professor, School of Nursing, Yale University, New Haven, CT.
Shih-Yu Lee, Associate Professor, Byrdine F Lewis School of Nursing, Georgia State University, Atlanta, GA.
Cheng-Shi Shiu, Doctoral Candidate, School of Social Service Administration, University of Chicago, Chicago, IL.
Jane M Simoni, Professor, Department of Psychology, University of Washington, Seattle, WA, USA.
Chengen Pan, Nurse, Shanghai Public Health Clinical Center, Shanghai.
Meijuan Bao, Nursing Director, Shanghai Public Health Clinical Center, Shanghai.
Hongzhou Lu, Executive Director, Shanghai Public Health Clinical Center, Shanghai, China.
References
- Adinolfi A. Assessment and treatment of HIV-related fatigue. The Journal of the Association of Nurses in AIDS Care. 2001;12(Suppl):29–34. doi: 10.1177/105532901773742266. (quiz 35–28) [DOI] [PubMed] [Google Scholar]
- Barroso J, Pence BW, Salahuddin N, Harmon JL, Leserman J. Physiological correlates of HIV-related fatigue. Clinical Nursing Research. 2008;17:5–19. doi: 10.1177/1054773807311382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WT, Starks H, Shiu CS, Fredriksen-Goldsen K, Simoni J, Zhang F, Pearson C, Zhao H. Chinese HIV-positive patients and their healthcare providers: contrasting Confucian versus Western notions of secrecy and support. ANS Advances in Nursing Science. 2007;30:329–342. doi: 10.1097/01.ANS.0000300182.48854.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WT, Shiu CS, Simoni J, Fredriksen-Goldsen K, Zhang F, Zhao H. Optimizing HIV care by expanding the nursing role: patient and provider perspectives. Journal of Advanced Nursing. 2010;66:260–268. doi: 10.1111/j.1365-2648.2009.05165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WT, Shiu CS, Simoni JM, Zhao H, Bao MJ, Lu H. In sickness and in health: a qualitative study of how Chinese women with HIV navigate stigma and negotiate disclosure within their marriages/partnerships. AIDS Care. 2011;23(Suppl 1):120–125. doi: 10.1080/09540121.2011.554521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Docherty SL, Sandelowski M, Preisser JS. Three months in the symptom life of a teenage girl undergoing treatment for cancer. Research in Nursing and Health. 2006;29:294–310. doi: 10.1002/nur.20143. [DOI] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Hudson AL, Portillo CJ, Lee KA. Sleep disturbances in women with HIV or AIDS: efficacy of a tailored sleep promotion intervention. Nursing Research. 2008;57:360–366. doi: 10.1097/01.NNR.0000313501.84604.2c. [DOI] [PubMed] [Google Scholar]
- Lee KA, Portillo CJ, Miramontes H. The influence of sleep and activity patterns on fatigue in women with HIV/AIDS. The Journal of the Association of Nurses in AIDS Care. 2001;12(Suppl):19–27. doi: 10.1177/105532901773742257. [DOI] [PubMed] [Google Scholar]
- Lee SY, Lee KA, Rankin SH, Weiss SJ, Alkon A. Sleep disturbance, fatigue, and stress among Chinese-American parents with ICU hospitalized infants. Issues in Mental Health Nursing. 2007;28:593–605. doi: 10.1080/01612840701354505. [DOI] [PubMed] [Google Scholar]
- Leserman J, Barroso J, Pence BW, Salahuddin N, Harmon JL. Trauma, stressful life events and depression predict HIV-related fatigue. AIDS Care. 2008;20:1258–1265. doi: 10.1080/09540120801919410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin RD, Daehler MA, Grutsch JF, Quiton J, Lis CG, Peterson C, Gupta D, Watson K, Layer D, Huff-Adams S, Desai B, Sharma P, Wallam M, Delioukina M, Ball P, Bryant M, Ashford M, Copeland D, Ohmori M, Wood PA, Hrushesky WJ. Circadian function in patients with advanced non-small-cell lung cancer. British Journal of Cancer. 2005;93:1202–1208. doi: 10.1038/sj.bjc.6602859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littner M, Kushida CA, Anderson WM, Bailey D, Berry RB, Davila DG, Hirshkowitz M, Kapen S, Kramer M, Loube D, Wise M, Johnson SF. Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: an update for 2002. Sleep. 2003;26:337–341. doi: 10.1093/sleep/26.3.337. [DOI] [PubMed] [Google Scholar]
- Marion I, Antoni M, Pereira D, Wohlgemuth W, Fletcher MA, Simon T, O’sullivan MJ. Distress, sleep difficulty, and fatigue in women co-infected with HIV and HPV. Behavioral Sleep Medicine. 2009;7:180–193. doi: 10.1080/15402000902976721. [DOI] [PubMed] [Google Scholar]
- Ministry of Health People’s Republic of China Joint United Nations Programme on HIV/AIDS World Health Organization. 2005 Updates on the HIV/AIDS Epidemic and Response in China. Ministry of Health People’s Republic of China Joint United Nations Programme on HIV/AIDS World Health Organization; Beijing: 2006. [Google Scholar]
- Pence BW, Barroso J, Leserman J, Harmon JL, Salahuddin N. Measuring fatigue in people living with HIV/AIDS: psychometric characteristics of the HIV-related fatigue scale. AIDS Care. 2008;20:829–837. doi: 10.1080/09540120701694063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penzak SR, Reddy YS, Grimsley SR. Depression in patients with HIV infection. American Journal of Health-System Pharmacy. 2000;57:376–386. doi: 10.1093/ajhp/57.4.376. (quiz 387–379) [DOI] [PubMed] [Google Scholar]
- Phillips KD, Sowell RL, Rojas M, Tavakoli A, Fulk LJ, Hand GA. Physiological and psychological correlates of fatigue in HIV disease. Biological Research for Nursing. 2004;6:59–74. doi: 10.1177/1099800404264846. [DOI] [PubMed] [Google Scholar]
- Pinkham S, Malinowska-Sempruch K. Women, harm reduction and HIV. Reproductive Health Matters. 2008;16:168–181. doi: 10.1016/S0968-8080(08)31345-7. [DOI] [PubMed] [Google Scholar]
- Salahuddin N, Barroso J, Leserman J, Harmon JL, Pence BW. Daytime sleepiness, nighttime sleep quality, stressful life events, and HIV-related fatigue. The Journal of the Association of Nurses in AIDS Care. 2009;20:6–13. doi: 10.1016/j.jana.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Sheldon LA, Kalichman SC, Carey MP, Fielder RL. Stress management interventions for HIV+ adults: a meta-analysis of randomized controlled trials, 1989 to 2006. Health Psychology. 2008;27:129–139. doi: 10.1037/0278-6133.27.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas KS, Bardwell WA, Ancoli-Israel S, Dimsdale JE. The toll of ethnic discrimination on sleep architecture and fatigue. Health Psychology. 2006;25:635–642. doi: 10.1037/0278-6133.25.5.635. [DOI] [PubMed] [Google Scholar]
- UNAIDS. [accessed 9 May 2007];Uniting the World Against AIDS. 2006 Available at: http://www.unaids.org/en/Goals/UNGASS/default.asp.
- U.S. Department of Health and Human Services Office. [accessed 9 July 2012];HIV/AIDS. 2011 Available at: http://www.womenshealth.gov/hiv-aids/aids-worldwide/
- Voss J, Portillo CJ, Holzemer WL, Dodd MJ. Symptom cluster of fatigue and depression in HIV/AIDS. Journal of Prevention & Intervention in the Community. 2007;33:19–34. doi: 10.1300/J005v33n01_03. [DOI] [PubMed] [Google Scholar]
- Vosvick M, Gore-Felton C, Ashton E, Koopman C, Fluery T, Israelski D, Spiegel D. Sleep disturbances among HIV-positive adults: the role of pain, stress, and social support. Journal of Psychosomatic Research. 2004;57:459–463. doi: 10.1016/j.jpsychores.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Yeh ML, Liu HY, Ko WC, Lee HC, Ko NY. HIV-related symptoms in patients with HIV infection enrolled in an HIV case management program in Taiwan. Hu Li Za Zhi. 2009;56:35–42. [PubMed] [Google Scholar]
- Zhao G, Li X, Kaljee L, Zhang L, Fang X, Zhao J, Lin D, Lin X, Stanton B. Psychosocial consequences for children experiencing parental loss due to HIV/AIDS in central China. AIDS Care. 2009;21:769–774. doi: 10.1080/09540120802511943. [DOI] [PubMed] [Google Scholar]


