Abstract
Purpose
Human Papillomavirus (HPV) vaccine uptake remains low. Although publicly funded programs provide free or low cost vaccines to low-income children, barriers aside from cost may prevent disadvantaged girls from getting vaccinated. Prior studies have shown distance to health care as a potential barrier to utilizing pediatric preventive services. This study examines whether HPV vaccines are geographically accessible for low-income girls in Los Angeles County and whether proximity to safety-net clinics is associated with vaccine initiation.
Methods
Interviews were conducted in multiple languages with largely immigrant, low-income mothers of girls ages 9 to 18 via a county health hotline to assess uptake and correlates of uptake. Addresses of respondents and safety-net clinics that provide the HPV vaccine for free or low cost were geo-coded and linked to create measures of geographic proximity. Logistic regression models were estimated for each proximity measure on HPV vaccine initiation while controlling for other factors.
Results
On average, 83% of the 468 girls had at least one clinic within 3-miles of their residence. The average travel time on public transportation to the nearest clinic among all girls was 21 minutes. Average proximity to clinics differed significantly by race/ethnicity. Latinas had both the shortest travel distances (2.2 miles) and public transportation times (16 minutes) compared to other racial/ethnic groups. The overall HPV vaccine initiation rate was 25%. Increased proximity to the nearest clinic was not significantly associated with initiation. By contrast, mother’s awareness of HPV and daughter’s age were significantly associated with increased uptake.
Conclusions
This study is among the first to examine geographic access to HPV vaccines for underserved girls. Although the majority of girls live in close proximity to safety-net vaccination services, rates of initiation were low. Expanding clinic outreach in this urban area is likely more important than increasing geographic access to the vaccine for this population.
Keywords: HPV vaccine, adolescent, safety-net, geographic information systems (GIS), minority health, low-income
INTRODUCTION
Low income, ethnic minority, and immigrant women experience a higher burden of cervical cancer in the United States (U.S.) [1, 2]. In Los Angeles County (LAC)1, cervical cancer incidence is significantly higher than the national average (12.1 per 100,000 vs. 8.1 per 100,000) [3], with Latina women having the highest rates (18.1 per 100,000) among all ethnic groups [4].
Wide-spread adoption of HPV vaccines has the potential to substantially reduce future cases of cervical cancer as well as other HPV-related cancers and genital warts [5]. Currently, both the bivalent and quadrivalent vaccines are recommended for routine use among girls ages 11 to12 years old and approved for use among girls as young as 9 and up to age 26 [6]. Low-income children who qualify for the federally funded Vaccines for Children (VFC) program can access the vaccines for free or low cost via VFC providers [7].
Currently, adolescent HPV vaccination rates remain low in the U.S. Recent national data revealed only 53% of adolescent girls initiated the HPV vaccine and 35% completed the 3-dose series in 2011 [8]. These rates are much lower than uptake rates for other adolescent vaccines [9]. Unless the vaccine is adopted by all subgroups, including girls that are most at risk for cervical cancer, disparities will likely remain. Existing research on HPV vaccine uptake has focused mainly on individual level factors, including demographic characteristics, vaccine knowledge [10, 11] and acceptability [12, 13]. Recent studies assessing barriers to uptake among disadvantaged groups indicate that less educated, low-income and ethnic minority parents are less likely to have heard of the HPV vaccines or have vaccinated daughters [14, 15].
Few studies have explored geographic access to vaccination services, especially among disadvantaged girls, as a potential barrier to HPV vaccine initiation. Geographic access to care, defined as the relationship between the location of health care providers and the location of clients [16], has been shown to impact the utilization of health services, including HIV testing, asthma management, breast cancer screening, and childhood immunizations [17–20]. Importantly, a recent study found that low-income, urban children living closer to pediatricians were more likely to be up to date with childhood vaccinations [17]. In a similar study, asthmatic children with increased geographic access (i.e. proximity) to providers had better longitudinal asthma management [20]. In response to reducing geographic barriers to primary care services, local health departments and individual health care organizations across the country have implemented mobile van clinics as a strategy to increase access to to underserved communities [21–23]. A prior study, focused on understanding childhood immunizations in states and urban areas, cited mobile health vans and improving clinic hours as strategies for increasing uptake [24]. Despite the growing evidence that distance to vaccination services may be a plausible barrier to uptake, little is known about whether safety-net immunization services are geographically accessible to disadvantaged communities that can benefit most from HPV vaccines.
This study examines the proximity of county operated and affiliated safety-net immunization clinics to a sample of low-income, ethnic minority girls in Los Angeles County who are age eligible for HPV vaccination. The study also assesses the extent to which HPV vaccine uptake is associated with proximity to safety-net immunization clinics.
METHODS
Study Population
We used secondary data from a survey of low-income caregivers of adolescent girls. The original study aimed to identify rates of HPV vaccine uptake and correlates of uptake, primarily psychosocial factors, among girls with caregivers who routinely use the LAC safety-net system [25]. This study expands on the original study to examine whether geographic proximity to safety-net clinics is associated with HPV vaccination. Participants were recruited from the Los Angeles County Department of Public Health’s (LACDPH) Office of Women’s Health’s (OWH) telephone hotline. The OWH toll-free hotline provides services, such as scheduling of cervical and breast cancer screening appointments and disseminating health information, to low-income (<200% federal poverty level) and uninsured women. Hotline services are available in multiple languages, including Spanish, Mandarin, Cantonese, Korean, and English. Between January and November 2009, all in-coming callers and prior callers who were called back for other hotline reminder services were introduced to the study and asked to be screened for study eligibility following the completion of normal hotline services.
Eligibility criteria included female callers that were medical decision-makers for at least one HPV vaccine age eligible girl (9–18 years) in the household. We excluded women who were not between the ages of 18 and 65 years old. Callers with more than one HPV vaccine eligible girl were asked to complete the survey in relation to the girl with the earliest birth month to ensure that surveys were not systematically completed in relation to older or younger girls in the household while at the same time minimizing the burden of the selection process for hotline operators.
Callers of all hotline languages were asked to participate. Among eligible callers, 93% of eligible callers provided informed consent and completed the survey. English speaking participants had slightly lower enrollment rates (81%) compared to Spanish (96%), Korean (97%) and Chinese (98%) speaking callers. Study participants are referred to as “mothers” for simplicity because 85% of women in the study identified themselves as mothers, rather than grandmothers, aunts, or sisters. Mothers were administered a 75-item telephone survey in pencil and paper format that lasted approximately 20–30 minutes.
Safety-net Clinics
We included all clinics that were part of the Los Angeles County Immunization Program’s provider referral list in 2009 (n=155) as likely points of access to free or low cost HPV vaccines for girls in the study sample [26]. These clinics include a combination of county operated health centers or immunization clinics, federally qualified health centers (FQHC) or FQHC look alike clinics, public–private partnership clinics, and other community health or free clinics. All clinics in the LACDPH Immunization Program’s provider referral list have the capacity to provide recommended immunizations for children. Many of the clinics provide a full range of primary care services, while others are freestanding immunization clinics operated by the county. All clinics have health care personnel on site to administer vaccines and are enrolled in the VFC program to provide free or low cost vaccines to underserved children in the area. In addition to VFC funding, clinics also receive Title 317 funding to provide vaccines to underinsured populations. Vaccination services are available to low-income girls at these clinics regardless of their insurance status. Because the number of clinics affiliated with the LACDPH Immunization Program can fluctuate over time due to clinic closures and the expansions, we used the clinic list available in 2009 to match the data collection period of our study. Women who call the OWH telephone hotline routinely ask for referrals to women’s health services via safety-net clinics within the county and routinely use safety-net services. The clinics included in this study are the same clinics that mothers would be referred to by the LACDPH to access free or low cost vaccinations for their daughters. Geographic proximity to these clinics, therefore, encompasses the majority of VFC providers within the county system that provide safety-net vaccination services.
Measures
Primary Predictor: Geographic Access
Geographic access was defined as spatial and temporal proximity to clinics. We explored the following measures to characterize geographic proximity: 1.) shortest straight-line (Euclidean) distance, 2.) shortest travel distance over a road network, 3.) availability of at least one clinic within a 3-mile radius of residence, 4.) shortest driving time, 5.) shortest public transportation time. Locations of residences for each vaccine eligible girl and safety-net clinics were geo-coded using ArcGIS 10 (ESRI, Redlands, CA). We excluded 11 participants with addresses that could not be geocoded accurately beyond the zip code level.
Straight-line distance was measured as the shortest direct distance (miles) between each respondent’s residence and the nearest clinic. While straight-line distance is often used in the literature, it is less realistic because it ignores physical barriers (e.g. buildings, parks). We also included shortest travel distance; this was measured as the distance (miles) over the LAC road network between the respondent’s residence and the nearest clinic. We also used a dichotomous (yes/no) variable of having at least one available clinic within a 3-mile radius of each girl’s residence. Several prior studies have suggested that average distance to health care facilities in urban areas is between 2 to 5 miles [17, 20, 27]. Geographic measures were obtained using ArcGIS 10 (ESRI, Redlands, CA). Travel time (in minutes) was calculated using the driving direction and public transportation functions in Google Maps. For consistency and completeness of the Google Maps fields, we calculated travel times to clinics for Thursday afternoons at 4 pm based on the assumption that most schools close between 2–3 pm and many clinics close by 5–6 pm. We chose Thursday afternoons to obtain a conservative estimate for travel time based on the notion that traffic congestion is greatest on Thursday and Friday afternoons, but are aware parents may choose to take their daughters to get vaccinated on other weekdays as well. Study findings should be interpreted with the understanding that geographic proximity to clinics was based on the closest clinic to each girl’s residence and that use of clinics located further away may be possible due to a variety of other factors.
Primary Outcome: HPV vaccine initiation
HPV vaccine initiation was a dichotomous (yes/no) outcome for whether an adolescent girl received at least one dose of the HPV vaccine. Mothers were only asked about uptake of the quadrivalent vaccine because the bivalent vaccine was not yet available at the time of interview. Mothers were asked about their awareness of HPV infections and HPV vaccines. Mothers who had knowledge about HPV vaccines were subsequently asked whether their daughter had received any doses of the vaccine. The “initiated” group included mothers who reported their daughters had received at least one dose of the vaccine. The “uninitiated” group included mothers who reported they had never heard of the HPV vaccine and mothers who reported their daughters did not receive any doses of the HPV vaccine. Eleven girls with mothers who reported they had never heard of HPV but also reported that their daughters initiated the HPV vaccine were excluded from the analysis.
Individual level covariates
We included basic demographic information available for mothers (age, race/ethnicity, education, and nativity) and girls (age) from the original survey as covariates for the multivariable models. Race/ethnicity was measured by the following mutually exclusive categories: Latina, Chinese, Korean, African American, and other race. The “other” race category included other Asian subgroups (e.g. Vietnamese), multiracial, and non-Latino white. The hotline targets low-income women with an annual household income of less than 200% federal poverty level, resulting in limited variability in family income across the study sample. Income was therefore excluded as a covariate in the analysis. For daughter’s age, we used the age recommendations for HPV vaccination to transform the age of adolescent girls into three categories (9–10 years – pre-recommendation group, 11–12 years – recommended group, 13–18 years –catch-up group) [28]. We also included the health care access variables available for each adolescent girl (having a usual source of care, insurance type).
Statistical Analysis
Initial descriptive statistics were obtained to describe the study sample and to examine the distributions of the primary outcome and predictor variables. Bivariate associations between geographic access and race/ethnicity were tested using one-way ANOVA tests for continuous measures and Fisher’s exact test for the dichotomous measure. Differences in continuous proximity measures by vaccine initiation were tested using Wilcoxon-Mann-Whitney tests.
Logistic regression models were used to estimate the association between geographic access and HPV vaccine initiation, while controlling for other factors. African American and “other” race (n=30) categories were omitted from the multivariate analysis because of small numbers and limitations in interpreting results for a heterogeneous group. Statistical significance for all analyses was determined at the p<0.05 level. Only significant covariates in the bivariate analyses were included in the multivariable model. We retained the primary predictor of interest, geographic access, in the multivariate models. All multivariate regression results were obtained as odds ratios with 95% confidence intervals. All analyses were conducted using STATA 10 statistical software (Statacorp, College Station, Texas). This study was approved by the UCLA Institutional Review Board.
RESULTS
Sample Characteristics
Over half (51.6%) of mothers in the sample (n=468) were Latina and a third (33%) were Asian (Table 1). Adolescent girls averaged 13.9 years in age. About a quarter (25%) of all girls in the sample initiated the HPV vaccine. The highest initiation rate was among Latinas (30%), with Chinese, Korean, African American and girls belonging to other racial/ethnic groups at lower rates ranging from 19% to 24% (not statistically significant). Initiation rates were significantly lower among younger girls. Girls with public insurance had the highest rates (32%) of HPV vaccine initiation compared to girls with private insurance (21%) or no insurance (19%). Differences in initiation rates by age and insurance type were statistically significant.
Table 1.
Demographic and Health Care Characteristics of Mothers/Caregivers and Adolescent Girls
| Characteristic | Total Sample % (n) | Initiated HPV Vaccine** % (n) | Did Not Initiate HPV Vaccine*** % (n) | p-value |
|---|---|---|---|---|
|
| ||||
| Mothers/Caregivers | ||||
|
| ||||
| Total | 100.0 (468) | 25.2 (118) | 74.8 (350) | |
| Race/ethnicity | ||||
| Latina | 51.6 (236) | 30.0 (70) | 70.3 (166) | 0.31 |
| Chinese | 19.3 (88) | 23.9 (21) | 76.1 (67) | |
| Korean | 14.2 (65) | 20.0 (13) | 80.0 (52) | |
| African American | 8.1 (37) | 18.9 (7) | 81.1 (30) | |
| Other race | 6.8 (31) | 22.6 (7) | 77.4 (24) | |
| Education | ||||
| < High School Diploma | 49.8 (233) | 27.0 (63) | 73.0 (170) | 0.37 |
| High School Diploma or more | 50.2 (235) | 23.4 (55) | 76.6 (180) | |
| Nativity | ||||
| Foreign-born | 87.6 (410) | 25.9 (106) | 74.2 (304) | 0.39 |
| Born in U.S. | 12.4 (58) | 20.7 (12) | 79.3 (46) | |
| Percent Life in U.S> | ||||
| < 25% life spent in U.S. | 16.7 (78) | 19.2 (15) | 80.8 (63) | 0.18 |
| ≥25% time spent in U.S. | 83.3 (390) | 26.4 (103) | 73.6 (287) | |
| Mother Heard of HPV | ||||
| Yes | 60.7 (284) | 41.6 (118) | 58.5 (166) | <0.001 |
| No | 39.3 (184) | 100.0 (184) | ||
| Age (mean, SD)* | 43.9 (7.1) | 43.4 (7.2) | 44.1 (7.0) | |
|
| ||||
| Adolescent Girls | ||||
|
| ||||
| Age | ||||
| 9–10 years | 14.9 (70) | 5.7 (4) | 94.3 (66) | <0.001 |
| 11–12 years | 19.4 (91) | 26.4 (24) | 73.6 (67) | |
| 13–18 years | 65.6 (307) | 29.3 (90) | 70.7 (217) | |
| Insurance status | ||||
| No Insurance | 31.8 (149) | 18.6 (22) | 85.2 (127) | <0.001 |
| Public | 57.1 (267) | 31.8 (85) | 68.2 (182) | |
| Private | 11.1 (52) | 21.2 (11) | 78.9 (41) | |
| Have Usual Source of Care | ||||
| Yes | 65.6 (307) | 30.3 (93) | 69.7 (214) | <0.001 |
| No | 34.4 (161) | 15.5 (25) | 84.5 (136) | |
Descriptive statistics for mother’s age represent means and standard deviations rather than % and n of sample.
Percentages and n’s in this column represent the proportion and sample size of girls that have initiated the HPV vaccine within each demographic category.
Percentages and n’s in this column represent the proportion and sample size of girls that have NOT initiated the HPV vaccine within each demographic category.
Geographic Access to Clinics
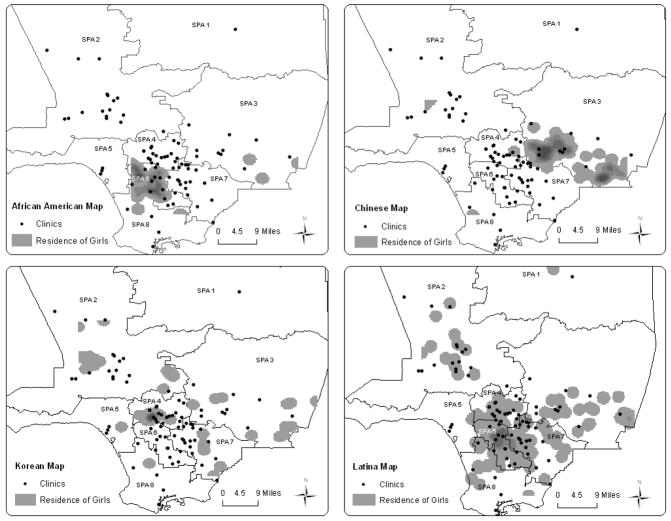
The locations of safety-net immunization clinics and residence of adolescent girls in the sample are shown in Figure 1. For purposes of health care delivery and planning, the county is divided in eight Service Planning Areas (SPAs). The majority of clinics are located in the metro (SPA 4 - central regions around downtown) and south (SPA 6) Los Angeles areas of the county, matching areas of the county with greatest population density and poorest neighborhoods. Residential locations are also geographically clustered by race/ethnicity, with the majority of Latina and African American girls living in central and south Los Angeles and Chinese girls living in the eastern part of the county, providing evidence of the immigrant and ethnic enclaves within the Los Angeles Area [29].
Figure 1. Safetynet Immunization Clinics and Residence* of Vaccine-Eligible Girls by Race/ethnicity.
*Residential locations are shown with surrounding buffers (gray regions) for confidentiality. Darker gray regions correspond to overlapping residential buffers of multiple girls. Exact residential locations were used to calculate geographic access measures in the analyses.
Geographic access differed significantly across racial/ethnic groups (Table 2). Over 90% of Latina girls had a clinic within 3-miles compared to 68% of Chinese girls and 70% of Korean girls. Driving time to the nearest clinic was longest for Chinese and Korean (7.5 minutes) girls compared to Latina (4.8 minutes) and African American (6.0 minutes) girls. These differences, although significantly different, indicate driving time to the nearest clinic is relatively short for all racial/ethnic groups in the sample. Public transportation time followed a similar pattern for racial/ethnic differences but revealed that mothers without access to a personal vehicle would have to spend more than three times the amount of time (average of 21.4 minutes) to take their daughter to the nearest clinic compared to the average driving time.
Table 2.
Geographic Access to Nearest Safety-Net immunization Clinic by Race/Ethnicity 508
| All (n=468) | Latino (n=236) | Chinese (n=88) | Korean (n=65) | African American (n=37) | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Continuous Geographic Access Measures | Mean, SD | Mean, SD | Mean, SD | Mean, SD | Mean, SD | p-value1 |
| Straight-line distance to nearest clinic (Miles) | 1.73 (1.28) | 1.37 (0.98) | 2.34 (1.51) | 2.13 (1.56) | 1.63 (0.91) | <0.001 |
| Travel distance to nearest clinic (Miles) | 2.70 (2.03) | 2.17 (1.50) | 3.55 (2.27) | 3.14 (2.86) | 3.27 (2.21) | <0.001 |
| Public transportation time to nearest clinic (Minutes) | 21.4 (18.3) | 16.1 (10.1) | 26.7 (15.2) | 24.6 (15.2) | 18.7 (15.3) | <0.001 |
| Driving time to nearest clinic (Minutes) | 6.24 (4.84) | 4.77 (3.29) | 7.53 (4.36) | 7.52 (4.61) | 5.97 (4.08) | <.0.001 |
|
| ||||||
| Categorical Geographic Access Measures | % (n) | % (n) | % (n) | % (n) | % (n) | p-value2 |
|
| ||||||
| Clinic within… | <0.001 | |||||
| 1 mile | 35.9 (164) | 44.5 (105) | 20.5 (18) | 35.4 (23) | 24.3 (9) | |
| 2 miles | 69.6 (318) | 82.6 (195) | 55.7 (49) | 49.2 (32) | 62.2 (23) | <0.001 |
| 3 miles | 83.5 (382) | 92.0 (217) | 68.2 (60) | 70.8 (46) | 91.9 (34) | <0.001 |
| Clinic within driving time of… | ||||||
| <10 Minutes | 24.0 (102) | 29.9 (67) | 15.2 (12) | 20.3 (13) | 13.3 (4) | <0.001 |
| 10–30 Minutes | 56.9 (242) | 63.0 (141) | 48.1 (38) | 42.2 (27) | 76.7 (23) | <0.001 |
| > 30 Minutes | 19.1 (81) | 7.1 (16) | 37.7 (29) | 37.5 (24) | 10.0 (3) | <0.001 |
Means and standard deviations for all races combined and by each racial/ethnic subgroup are presented for continuous measures
Proportions and sample sizes for all races combined and by each racial/ethnic subgroup are presented for categorical measures
P value for one-way ANOVA F-test for differences in distance by race/ethnicity
P value for Fisher’s exact test for differences in proportion of girls with at least 1 clinic by race/ethnicity
Geographic Access and HPV Vaccine Initiation
The bivariate analyses showed that girls who were Latina, covered by public insurance, and had a usual source of care had greater odds of initiating the HPV vaccine (Table 3). Overall, geographic access measures were not significantly associated with HPV vaccine initiation in the bivariate or multivariable analyses. Results from the multivariable models using travel distance and public transportation time as geographic access measures are shown in Table 3. We present findings from models using travel distance and public transportation time based on their specificity (e.g. travel distance vs. straight-line distance) and their relevance to our study sample (e.g. public transportation time over driving time). Results were similar for multivariable models using straight-line distance, driving time, and having a clinic within three miles of each girl’s residence (data not shown).
Table 3.
Bivariate and Multivariate Correlates of HPV Vaccine Initiation^
| Bivariate OR (95% CI) | Multivariable Model with Travel Distance OR (95% CI) | Multivariable Model with Public Transportation Time OR (95% CI) | |
|---|---|---|---|
|
| |||
| Geographic Access | |||
|
| |||
| Straight-line Distance | 0.92 (0.77, 1.09) | -- | -- |
| Travel Distance | 0.93 (0.83, 1.04) | 0.85 (0.62, 1.16) | -- |
| Clinic within 3 miles | 1.05 (0.59, 1.87) | -- | -- |
| Public Trans. Time | 0.99 (0.98, 1.01) | -- | 0.99 (0.98, 1.01) |
| Driving Time | 0.96 (0.91, 1.02) | -- | -- |
|
| |||
| Mother/Caregiver | |||
|
| |||
| Race/ethnicity | |||
| Latina | *1.58 (1.05, 2.41) | 1.0 | 1.0 |
| Chinese | 0.90 (0.52, 1.56) | 0.86 (0.45, 1.66) | 0.83 (0.42, 1.64) |
| Korean | 0.70 (0.36, 1.33) | 0.89 (0.40, 1.97) | 1.05 (0.49, 2.26) |
| African American | 0.66 (0.28, 1.56) | 0.63 (0.25, 1.58) | 0.39 (0.13, 1.22) |
| English Interview (Ref: Non-English) | 1.00 (0.56, 1.76) | -- | -- |
| HS Diploma or more (Ref: no HS diploma) | 0.78 (0.51, 1.20) | -- | -- |
| Born in U.S. (Ref: Foreign-born) | 0.75 (0.36, 1.56) | -- | -- |
| Age | 0.98 (0.95, 1.01) | ||
|
| |||
| Adolescent Girl | |||
|
| |||
| Age | |||
| 9 to 10 years | **0.11 (0.03, 0.37) | ***0.12 (0.03, 0.42) | ***0.11 (0.02, 0.31) |
| 11 to 12 years | 1.05 (0.61, 1.81) | 1.0 | 1.0 |
| 13–18 years | *2.17 (1.32, 3.57) | 1.27 (0.71, 2.26) | 1.10 (0.61, 1.98) |
| Insurance status | |||
| Uninsured | *0.42 (0.25, 0.70) | *0.41 (0.20, 0.81) | *0.43 (0.22, 0.86) |
| Public | *2.40 (1.50, 3.83) | 1.0 | 1.0 |
| Private | 0.70 (0.33, 1.53) | *0.39 (0.16, 0.96) | 0.42 (0.17, 1.05) |
| Have a Usual Source of Care (Ref: No) | *2.16 (1.32, 3.57) | 1.30 (0.66, 2.57) | 1.37 (0.67, 2.77) |
Only results for multivariate models with travel distance or public transportation time as the measure for geographic access are presented. Results were similar for models using straight-line distance, clinic within 3 miles, and driving time. Significance level of odds ratios:
p <0.05,
p<0.01,
p<0.001
DISCUSSION
For the most part, HPV vaccination services via safety-net clinics are geographically accessible for low-income, ethnic minority girls in this county hotline sample. Our findings reveal that 80% of, or 8 out of every 10, low-income adolescent girls with mothers who routinely call the Office of Women’s Health hotline live within three miles of a nearby clinic where they can access the HPV vaccine for free or low cost. These findings suggest HPV vaccination services are geographically accessible to populations who rely on safety-net facilities in Los Angeles County. While increased proximity to pediatric health services was linked to increased service use among urban, low-income populations in prior studies [17, 20], we did not find a similar relationship. Low perceived awareness of available HPV vaccination services, as opposed to a lack of existing vaccination services, may be a possible reason for low uptake. In addition, findings may stem from selection issues and lack of participant heterogeneity. The low-income mothers who called our hotline are presumably more motivated than low-income mothers from similarly underserved communities who do not use hotline services to seek health care for themselves or their daughters. Perhaps these motivational factors also compress the variation in our sample. Future research should test the hypothesis that intrinsic motivation may overcome geographic access barriers, and the corollary hypothesis that persons who are less motivated may be more severely affected by access barriers.
We found very low reports of HPV vaccine initiation in our sample of low-income, ethnic minority girls. These rates were much lower than nationally reported rates for low-income adolescent girls (51.9%) in 2009 [30], the same year this study was conducted, and well below the national 80% target immunization goal for adolescents in 2020 [9]. We also found rates of initiation to be equally low among older girls (13–18 years) and girls in the recommended age group (11–12 years). Low uptake may be due to lack of information about HPV, preventing mothers from seeking the HPV vaccine at safety-net clinics for their daughters. Rates of HPV and HPV vaccine awareness were only moderate within our study sample. Furthermore, our prior analyses have shown that needing more information about the vaccine and not knowing where to get the vaccine for their daughters were reported as potential correlates of low vaccine uptake [25]. These results reinforce studies showing a large proportion of parents report needing more information about the vaccine as a reason for not having their daughter vaccinated [14, 25, 31, 32]. Our findings, supportive of current literature, suggest even among mothers currently accessing county health services, additional education about HPV vaccines as well as where to access the vaccines would be beneficial.
Results also suggest health care coverage and clinical interactions with health care providers may be worth exploring in future research. Girls with public health insurance had higher rates of initiation compared to those with both private and no insurance coverage. For low-income adolescent girls, Medicaid coverage could lead to stronger ties with a usual source of care that improve continuity of care [33] as well as a greater chance to receive a physician recommendation for the HPV vaccines [34]. Lower rates of vaccine initiation among privately insured girls may be a result of the increasing cost-sharing and out-of-pocket costs for adolescent vaccines under private health insurance plans [35]. Prior studies indicate families at or near the poverty level are faced with disproportionate out-of-pocket costs that limit vaccine uptake [36]. The elimination of out-of-pocket costs for all recommended immunizations under the Affordable Care Act will help to ameliorate the individual cost burden to low-income parents of adolescent girls in the future [37].
Our study found that proximity safety-net clinics varied somewhat across race/ethnicity. The magnitude of differences for distance and time to nearest clinic between groups, however, were small (i.e. estimated driving time for Latina girls is on average 3 minutes shorter than for Chinese girls). Racial/ethnic differences related to other organizational and system aspects of care, such as access to clinic appointments, language concordant care, and preferences for other clinic attributes, may also impact HPV initiation and warrant further investigation [38–40]. Clinic-based factors such as targeted services for specific communities or the availability for racially or linguistically concordant providers may be stronger than the influence of distance on service use and therefore require further investigation [40, 41]. If this is the case, the limited English proficient mothers in our sample may be more inclined to have their daughters vaccinated at clinics within their ethnic community centers despite having to travel further than their nearest safety-net clinic. Future research should explore multiple dimensions of access (i.e. geographic, organizational) that influence vaccine uptake.
These study results should be considered in light of some important limitations. As mentioned above, our null findings could be a result of selection issues and lack of participant heterogeneity as mothers in our study are already a motivated health seeking group. All participants in the study were voluntary users of a county health hotline and may not be generalizable to all low-income mothers. Furthermore, this study had a limited number of non-Latino white, non-Latino African American and multiracial mothers, which could be due to hotline outreach and community activities that are promoted in the non-English language hotline communities (e.g. Latino, Chinese, Korean).
The locations of where girls received the HPV vaccine were not available in our dataset. For some groups, health services may be obtained at locations closer to a school or workplace. We based our analysis on proximity to the closest safety-net immunization clinic, but did not assess mother’s awareness of these clinics. In addition, our list of safety-net clinics, while comprehensive, may not include all points of HPV vaccine access. Private providers may also enroll in the VFC program and provide the vaccine for free or low cost to eligible girls, but are not included in this study. Nonetheless, the clinics used in our study were derived from the LACDPH Immunization Program’s referral list and therefore target the study population. Limited information is available for this study, however, about the hours of operation, additional vaccine administration fees, language capacity, or other services provided at these clinics. Further investigation regarding operational factors at the clinic level that influence timely vaccine uptake is warranted.
Proxy-reported vaccination history by mothers raises questions about response bias. A recent study, however, showed that parental reporting of HPV vaccination had the highest validity in the National Immunization Survey compared to parental reporting of any other adolescent vaccines [42]. Lastly, the cross-sectional nature of the data limits our ability to make causal inferences. Nevertheless, the unique sample of low-income girls and information on the exact residential and safety-net clinics provide practitioners provides actionable information for informing and targeting HPV promotion efforts.
Our study results point to the need to further examine factors that hinder and facilitate access to vaccination services among underserved populations. The idea of geographic barriers to care has long been discussed in the literature, but only recently have more studies attempted to empirically test this idea. We employed techniques to estimate not only simple proximity, but also to estimate the “realistic” travel distance and travel time to reach a clinic. Hence, our study is among the few to systematically examine clinic proximity as a primary correlate of HPV vaccine initiation. Our findings indicate interventions aimed to reduce geographic barriers may not be as urgent as increasing outreach for existing services within this large urban area. Future studies, however, should continue to investigate health system factors (e.g. administration fees, clinic hours and wait times) related to HPV vaccine access for underserved groups. In addition, future interventions for vaccine uptake should focus on increasing awareness on where to access the vaccine as well as other safety-net system factors that could improve access to HPV vaccines for underserved populations and ultimately reduce cervical cancer disparities.
Highlights.
We focus on an underserved population of low-income, ethnic minority girls
We examine geographic proximity to HPV vaccination services within safety-net clinics
Over 80% of girls live near a clinic with HPV vaccination services for free or low cost
Distance and transportation time to nearest clinic differ by race/ethnicity
Age of adolescent girl and insurance status remain important correlates of vaccine initiation
Acknowledgments
We gratefully acknowledge Laurel Fowler, Deputy Director of the Los Angeles County Department of Public Health Immunization Program for providing information about immunization services in Los Angeles County. We also thank the Office of Women’s Health Hotline operators and Kathleen Yu from the UCLA Division of Cancer Prevention and Control Research for assisting data collection and data entry. This work was supported by the UCLA Jonsson Cancer Center Foundation pre-doctoral fellowship, NIH/NCI R25 Cancer Education and Career Development Program, and the AHRQ Grants for Health Services Research Dissertation Program (1-R36-HS020172-01).
Footnotes
Abbreviations: HPV = human papillomavirus; LAC = Los Angeles County; LACDPH = Los Angeles County Department of Public Health; OWH = Office of Women’s Health; VFC = Vaccines for Children
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Freeman HP, Wingrove BK. Excess Cervical Cancer Mortality: A Marker for Low Access to Health Care in Poor Communities. National Cancer Institute, Center to Reduce Cancer Health Disparities; Rockville, MD: 2005. [Google Scholar]
- 2.Yin D, et al. Does socioeconomic disparity in cancer incidence vary across racial/ethnic groups? Cancer Causes Control. 2010 doi: 10.1007/s10552-010-9601-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NCI. State Cancer Profiles: Incidence Rates for California, 2002–2006, Cervix, All Races (including Hispanic) 2010 [cited 2010 01–25–2010]; Available from: www.statecancerprofiles.cancer.gov.
- 4.Cockburn M, Liu L, Deapen D. Los Angeles Cancer Surveillance Program. University of Southern California; Los Angeles, CA: 2009. Cancer in Los Angeles County: Trends by Race/Ethnicity, 1976–2006. [Google Scholar]
- 5.Garland SM, et al. Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N Engl J Med. 2007;356(19):1928–43. doi: 10.1056/NEJMoa061760. [DOI] [PubMed] [Google Scholar]
- 6.CDC. MMWR. Centers for Disease Control and Prevention; 2010. FDA Licensure of Bivalent Human Papillomavirus Vaccine (HPV2, Cervarix) for Use in Females and Updated HPV Vaccination Recommendations from the Advisory Committee on Immunization Practices (ACIP) pp. 626–629. [PubMed] [Google Scholar]
- 7.CDC. Vaccines for Children Program. 2010 Apr 13; [cited 2010; Available from: http://www.cdc.gov/vaccines/programs/vfc/default.htm.
- 8.U.S. Department of Health and Human Services. Recommended Preventive Services. Healthcare.gov. 2012 [cited 2012 November 7]; Available from: http://www.healthcare.gov/law/resources/regulations/prevention/recommendations.html.
- 9.U.S. Department of Health and Human Services. Healthy People 2020: Immunization and Infectious Diseases. 2012 Mar 1; [cited 2012 March 15]; Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=23.
- 10.Gerend MA, Magloire ZF. Awareness, knowledge, and beliefs about human papillomavirus in a racially diverse sample of young adults. J Adolesc Health. 2008;42(3):237–42. doi: 10.1016/j.jadohealth.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 11.Tiro JA, et al. What do women in the U.S. know about human papillomavirus and cervical cancer? Cancer Epidemiol Biomarkers Prev. 2007;16(2):288–94. doi: 10.1158/1055-9965.EPI-06-0756. [DOI] [PubMed] [Google Scholar]
- 12.Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med. 2007;45(2–3):107–14. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 13.Dempsey AF, et al. Factors that are associated with parental acceptance of human papillomavirus vaccines: a randomized intervention study of written information about HPV. Pediatrics. 2006;117(5):1486–93. doi: 10.1542/peds.2005-1381. [DOI] [PubMed] [Google Scholar]
- 14.Cates JR, et al. Racial differences in HPV knowledge, HPV vaccine acceptability, and related beliefs among rural, southern women. J Rural Health. 2009;25(1):93–7. doi: 10.1111/j.1748-0361.2009.00204.x. [DOI] [PubMed] [Google Scholar]
- 15.Reiter PL, et al. Correlates of receiving recommended adolescent vaccines among adolescent females in North Carolina. Hum Vaccin. 2011;7(1) doi: 10.4161/hv.7.1.13500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127–40. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Fu LY, et al. Spatial accessibility to providers and vaccination compliance among children with medicaid. Pediatrics. 2009;124(6):1579–86. doi: 10.1542/peds.2009-0233. [DOI] [PubMed] [Google Scholar]
- 18.Elkin EB, et al. Geographic access and the use of screening mammography. Med Care. 2010;48(4):349–56. doi: 10.1097/MLR.0b013e3181ca3ecb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taylor SL, et al. ZIP code correlates of HIV-testing: a multi-level analysis in Los Angeles. AIDS Behav. 2006;10(5):579–86. doi: 10.1007/s10461-005-9064-4. [DOI] [PubMed] [Google Scholar]
- 20.Teach SJ, et al. Spatial accessibility of primary care pediatric services in an urban environment: association with asthma management and outcome. Pediatrics. 2006;117(4 Pt 2):S78–85. doi: 10.1542/peds.2005-2000E. [DOI] [PubMed] [Google Scholar]
- 21.Mobile Health Clinics Association. 2012 [cited 2013 January 12]; Available from: http://www.mobilehealthclinicsnetwork.org/index.html.
- 22.Mobile Health Map. 2012 [cited 2013 January 15]; Available from: http://www.mobilehealthmap.org/about.php.
- 23.Oriol NE, et al. Calculating the return on investment of mobile healthcare. BMC Med. 2009;7:27. doi: 10.1186/1741-7015-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Groom H, et al. Qualitative Analysis of Immunization Programs With Most Improved Childhood Vaccination Coverage From 2001 to 2004. Journal of Public Health Management and Practice. 2010;16(1):E1–E8. doi: 10.1097/PHH.0b013e3181b0b8bc. [DOI] [PubMed] [Google Scholar]
- 25.Bastani R, et al. Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer Epidemiol Biomarkers Prev. 2011;20(7):1463–72. doi: 10.1158/1055-9965.EPI-11-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Los Angeles County Department of Public Health Immunization Program. Immunization Program Referral List. 2009 [cited 2009 January 20]; Available from: http://publichealth.lacounty.gov/ip/IZclinics/clinics.htm.
- 27.Cordasco KM, et al. English language proficiency and geographical proximity to a safety net clinic as a predictor of health care access. J Immigr Minor Health. 2010;13(2):260–7. doi: 10.1007/s10903-010-9425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.CDC. MMWR Early Release. Centers for Disease Control and Prevention; 2007. Quadrivalent Human Papillomavirus Vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP) pp. 1–24. [PubMed] [Google Scholar]
- 29.Logan W Zhang, Alba RD. Immigrant Enclaves and Ethnic Communities in New York and Los Angeles. American Sociological Review. 2002;67(2):299–322. [Google Scholar]
- 30.CDC. National, state, and local area vaccination coverage among adolescents aged 13–17 years - United States, 2009. Morbidity Mortality Weekly Report. 2010:1018–23. [PubMed] [Google Scholar]
- 31.Hughes J, et al. Disparities in how parents are learning about the human papillomavirus vaccine. Cancer Epidemiol Biomarkers Prev. 2009;18(2):363–72. doi: 10.1158/1055-9965.EPI-08-0418. [DOI] [PubMed] [Google Scholar]
- 32.Yeganeh N, Curtis D, Kuo A. Factors influencing HPV vaccination status in a Latino population; and parental attitudes towards vaccine mandates. Vaccine. 2010;28(25):4186–91. doi: 10.1016/j.vaccine.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 33.Szilagyi PG, et al. Delivering adolescent vaccinations in the medical home: a new era? Pediatrics. 2008;121(Suppl 1):S15–24. doi: 10.1542/peds.2007-1115C. [DOI] [PubMed] [Google Scholar]
- 34.Smith PJ, et al. The association between having a medical home and vaccination coverage among children eligible for the vaccines for children program. Pediatrics. 2005;116(1):130–9. doi: 10.1542/peds.2004-1058. [DOI] [PubMed] [Google Scholar]
- 35.Smith PJ, et al. Underinsurance and adolescent immunization delivery in the United States. Pediatrics. 2009;124(Suppl 5):S515–21. doi: 10.1542/peds.2009-1542K. [DOI] [PubMed] [Google Scholar]
- 36.Molinari NA, et al. Out-of-pocket costs of childhood immunizations: a comparison by type of insurance plan. Pediatrics. 2007;120(5):e1148–56. doi: 10.1542/peds.2006-3654. [DOI] [PubMed] [Google Scholar]
- 37.US-DHHS. Recommended Preventive Services. Healthcare.gov. 2011 [cited 2011 November 7]; Available from: http://www.healthcare.gov/law/resources/regulations/prevention/recommendations.html.
- 38.Guerrero AD, et al. Racial and ethnic disparities in pediatric experiences of family-centered care. Med Care. 2010;48(4):388–93. doi: 10.1097/MLR.0b013e3181ca3ef7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weech-Maldonado R, et al. Racial and ethnic differences in parents’ assessments of pediatric care in Medicaid managed care. Health Serv Res. 2001;36(3):575–94. [PMC free article] [PubMed] [Google Scholar]
- 40.Ngo-Metzger Q, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007;22(Suppl 2):324–30. doi: 10.1007/s11606-007-0340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Traylor AH, et al. The predictors of patient-physician race and ethnic concordance: a medical facility fixed-effects approach. Health Serv Res. 2010;45(3):792–805. doi: 10.1111/j.1475-6773.2010.01086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dorell CG, Jain N, Yankey D. Validity of parent-reported vaccination status for adolescents aged 13–17 years: National Immunization Survey-Teen, 2008. Public Health Rep. 2011;126(Suppl 2):60–9. doi: 10.1177/00333549111260S208. [DOI] [PMC free article] [PubMed] [Google Scholar]